Abstract
Much attention on the spread and impact of the ongoing pandemic has focused on institutional factors such as government capacity along with population-level characteristics such as race, income, and age. This paper draws on a growing body of evidence that bonding, bridging, and linking social capital - the horizontal and vertical ties that bind societies together - impact public health to explain why some U.S. counties have seen higher (or lower) excess deaths during the COVID19 pandemic than others. Drawing on county-level reports from the Centers for Disease Control and Prevention (CDC) since February 2020, we calculated the number of excess deaths per county compared to 2018. Starting with a panel dataset of county observations over time, we used coarsened exact matching to create smaller but more similar sets of communities that differ primarily in social capital. Controlling for several factors, including politics and governance, health care quality, and demographic characteristics, we find that bonding and linking social capital reduce the toll of COVID-19 on communities. Public health officials and community organizations should prioritize building and maintaining strong social ties and trust in government to help combat the pandemic.
Keywords: COVID19, Disaster, Social capital, Excess deaths, Coarsened exact matching, Policy
1. Introduction
Since its well-publicized spread from Wuhan, China to the Diamond Princess cruise ship anchored off Japan's coast in January 2020 and beyond, coronavirus disease 2019 (COVID-19) has taken lives, upended economies, and changed rhythms of daily life for billions of people. As of June 2021, COVID-19 has spread to over 173 million confirmed cases since early 2020 and caused more than 3.7 million deaths worldwide, with more than 597,000 verified fatalities in the United States alone (New York Times, 2021). Much research has examined variation in pandemic outcomes from factors such as the capacity of states and health care systems (Farag et al., 2012; Schoenbaum et al., 2011), individual behavior, and mobility (Barrios et al., 2020; Ding et al., 2020), and social vulnerability (Chin-Hong et al., 2020; Karaye and Horney, 2020). However, a growing body of evidence has pointed instead to the role of social ties, trust, and cohesion during crises and disasters (Kawachi et al., 2008; Iwasaki et al., 2017). Communities with stronger ties can more effectively spread actionable and accurate information, encourage the implementation of health-promoting behaviors, mediate stress, and positively engage with health authorities and their advice (Szreter and Woolcock, 2004; Jean-Baptiste et al., 2020). Building on initial research connecting social ties and the pandemic (Borgonovi and Andrieu, 2020; Varshney and Socher, 2020; Sharkey, 2020; for more, see Table 1 ), this study seeks to explain why some communities experienced higher excess death rates from COVID-19 than others.
Table 1.
Past findings about social capital and COVID-19.
| Study | Sample | Concept | Measure | Effect | Outcome |
|---|---|---|---|---|---|
| Elgar et al. (2020) | 84 countries | Trust | World Values Survey | Increase | Deaths |
| Group affiliations | Increase | ||||
| Civic engagement | Decrease | ||||
| Trust in government | Decrease | ||||
| Borgonovi and Andrieu (2020) | U.S. Counties | Overall Social Capital |
Rupasingha et al. (2006)'s Index |
Decrease | Mobility |
| Borgonovi et al. (2020) | U.S. Counties | Overall Social Capital | USJEC Index | Decrease | Case Rates |
| Durante et al. (2021) | Italian provinces | Civic Capital | Blood Donor Rate | Decrease | Mobility |
| Trust (Survey) | |||||
| Newspaper Readership | |||||
| Arachchi and Managi (2021) | Individuals in 37 countries | Community Attachment | Single Survey Items (5-pt Likert Scale) | Increase | Deaths |
| Social Trust | |||||
| Family Bond | Decrease | Deaths | |||
| Neighborhood Security | |||||
| Wu (2021) | U.S. States | Social Capital | Putnam Index, USJEC Index | Increase | Testing Rate |
| Kuchler et al. (2020) | U.S. counties Italian Provinces |
Social connectedness | Facebook Data | Increase | Case Rates |
| Varshney and Socher (2020) | U.S. counties U.S. States |
Social Capital | USJEC Index | Decrease | Case & Growth Rates |
| Makridis and Wu (2020) | U.S. counties | Social Capital | USJEC Index | Decrease | Case & Growth Rates |
| Bai et al. (2020) | U.S. counties | Civic Norms | Rupasingha et al. (2006)'s indices | Increase | Social Distancing |
| Social Network Density | Decrease | ||||
| Fraser and Aldrich 2020 | Japanese prefectures | Linking Social Capital | Fraser (2020) Social Capital Indices | Increase | Case Rates in Hotspots |
| Decrease | Case Rates Overall | ||||
| Bartscher et al. (2020a) | European country regions | Bridging Social Capital | Voter Turnout | Increase-then-decrease | Cumulative Cases |
| Bartscher et al. (2020b) | Decrease | Excess Deaths Mobility |
|||
| Barrios et al. (2020) | Individuals, Counties, E.U. regions | Civic Duty | Voter Turnout, USJEC Index | Increase | Social distancing |
| Ding et al. (2020) | U.S. Counties | Community engagement | USJEC Rupasingha et al. (2006) |
Decrease | Social distancing |
| Individual commitment to norms | Increase | ||||
| Milani (2021) | 41 Countries | Social Connectedness | Facebook Data | Increase | Infections, Risk Perception, Social Distancing |
| Yanagisawa et al. (2021) | U.S. Counties | Social/emotional support | Behavioral Risk Factor Surveillance System Index | Decrease | Case Rates Deaths |
| Civic engagement | Petris Index | Weak decrease | |||
| Rupasingha et al. (2006) | Increase |
Drawing on county-level reports from the Centers for Disease Control and Prevention (CDC) since February 2020, we calculated the number of excess deaths per county compared to a five-year average from 2015 to 2019 (Centers for Disease Control and Prevention, 2021). We produced panels datasets of county observations over time and used coarsened exact matching to find communities to compare as similar as possible except for their differing levels of social capital. We find consistent evidence across several months that bonding and linking social capital can reduce the toll of COVID-19 on communities, emphasizing the effectiveness of both horizontal and vertical social ties in pandemic response.
This study makes two major contributions to the literature. First, early analyses of community drivers of COVID-19 often relied on case rates; that approach remains challenging as cases have been underreported in the U.S. and correlate with testing rates, which vary for many reasons (Varshney and Socher, 2020). Similarly, case fatality rates adjust for the number of recognized cases, but this too may miss cases that were not identified as COVID-19 but had health consequences (Borgonovi and Andrieu, 2020; Borgonovi et al., 2020; Zhang et al., 2020). Researchers suspect that more deaths due to COVID had occurred than were initially reported (Banerjee et al., 2020; Kontis et al., 2020; Woolf et al., 2020), so by examining excess death rates, that is, the number of additional or fewer deaths per 100,000 persons in a community in 2020 compared to in the preceding five years on average, we can better capture the toll of COVID-19 on U.S. communities. Excess deaths do also reflect changes in how many people die in a given period due to COVID-19 related behavioral changes (e.g. fewer road accidents, higher cancer/heart-related deaths because of lack of critical care or seeking critical care). This challenge aside, they offer a much clearer glimpse of COVID-19's toll that traditional COVID death rates, which are often marred by limited testing capacity. While Bartscher et al. (2020a, b) examined the effect of overall social capital on excess mortality in Europe, the authors are unaware of any such research in the U.S.
Second, we find further support for the distinction between bonding, bridging, and linking social capital in its impacts on health outcomes (Szreter and Woolcock, 2004; Aldrich et al., 2018; Aldrich, 2019). While overall measures of social capital were not significantly associated with excess death rates, bonding and linking social capital were both separately and strongly associated with lower excess death rates. Further, we did not find evidence of a Janus-faced effect, where social capital levies substantial negative outcomes on out-groups (Aldrich, 2012; Aldrich et al., 2018). However, recent studies of COVID-19 in Japan suggest that trust in government, for example, can lead to mixed effects if government officials do not enforce quality health policy (Fraser and Aldrich, 2021). Our data suggest that in the current COVID-19 pandemic, vertical and horizontal social capital are both frequently associated with lower rates of excess deaths over time.
2. Literature review
Why do some communities experience higher rates of excess deaths than others during the pandemic? Excess deaths have been used after past disasters to more accurately capture deaths due to crisis that may have been miscategorized, misdiagnosed, or never recognized among patients with other overlapping conditions, or when records are lost, like after Hurricane Maria hit Puerto Rico in 2018 (Santos-Burgoa et al., 2018; Rivera and Rolke, 2019). Pandemic scholars have applied the same technique to capture deaths obfuscated by comorbidities and weak state and health care system capacity (Banerjee et al., 2020). Past scholars suggest four main explanations for why some communities suffer worse COVID-19 related mortality than others: mobility, health care quality, quality of health, social vulnerability, political partisanship, and social capital, which we discuss below.
First, communities might see worse outbreaks if they face greater population movement, spreading the outbreak further, as occurred during SARS (Bowen and Laroe, 2006) and Avian Flu (Smallman-Raynor and Cliff, 2008). On average, infected persons develop symptoms within five days of exposure, with a range of 1–14 days (Lauer et al., 2020). However, many people spread COVID asymptomatically, making it especially difficult to track the spread of COVID. Early evidence already suggests that mobility matters to COVID-19 spread (Zhang et al., 2020).
Another set of explanations ties community risk during COVID-19 to health conditions and behaviors. Obesity, diabetes, smoking, drinking, and physical inactivity are all associated with higher rates of mortality from COVID-19 (Townsend et al., 2020). These conditions might not increase mobility and exposure (often, mobility is reduced in communities with a high prevalence of individuals with health problems). However, if infected with COVID-19, individuals with such pre-existing conditions are considerably more likely to die. These health conditions make COVID spread especially costly to human life.
Alternatively, some communities might face worse outbreaks because their health care systems are more easily overwhelmed. Even in non-outbreak conditions, communities tend to see lower mortality rates due to better hospital quality and health care policy (Schoenbaum et al., 2011), of which the physician workforce is an important part (Baicker and Chandra, 2004; Goodman and Grumbach, 2008). Similarly, governments' capacity to step in, coordinate response, purchase protective equipment, and provide assistance to residents might affect pandemic impact (Farag et al., 2012). Further, persons lacking health insurance are especially vulnerable during COVID; states might see fewer excess deaths when governments have more robust health policies and have worked to get more people insured (Miller et al., 2020). Communities with more substantial government capacity were more effective in implementing lockdown policies and ensuring compliance with mobility restrictions (Bonaccorsi et al., 2020).
However, some communities might see greater excess deaths because their elected officials choose not to implement mask mandates, encourage physical distancing, or require school closures or lockdowns and because they themselves have adopted behaviors encouraged by those leaders. Recent research suggests that Americans' political preferences are greatly shaping adherence to new health behaviors, with Republican residents and elected officials resisting mask usage and social distancing while Democratic residents and officials have more readily adopted these new habits (Grossman et al., 2020; Painter and Qiu, 2020). As a result, grassroots political partisanship may greatly shape COVID outcomes.
However, some communities might face greater excess deaths due to having a high share of socially vulnerable residents. Socially vulnerable residents tend to see worse disaster outcomes and worse recovery over time, because they face financial limitations, mobility constraints, or abject discrimination by neighbors or public officials (Cutter et al., 2003). Residents tend to be more socially vulnerable to disaster residents if they are racial, religious, or ethnic minorities (Elliott et al., 2010), elderly (Salvati et al., 2018), women or single parents (Enarson, 1998), or face health conditions, disabilities, mobility challenges, unemployment, or poverty (Cutter et al., 2003). In the case of COVID, the most vulnerable demographics appear to be Black Americans (Chin-Hong et al., 2020), men, and the elderly (Mallapaty, 2020).
Finally, some communities, even socially vulnerable communities, might develop lower excess death rates due to the strength of social ties in their community. Social capital refers to the social ties that connect residents and enable reciprocity and collective action, and these come in three types: bonding, bridging, and linking social capital (Szreter and Woolcok, 2004). Bonding social capital describes ties between friends, family, and members of the same social groups, building trust and mutual reliance (Cox and Perry, 2011; Lee, 2019). In contrast, bridging social capital describes associational ties between members of different social groups, often built through volunteering groups, unions, parent-teacher organizations, and colleagues (Putnam, 2000). Bridging ties help residents find common ground and shared stake in their community, facilitating collective action, civic engagement, and closer collaboration during and after disasters (Smiley et al., 2018; Lee and Fraser, 2019; Ye and Aldrich, 2019). Last, linking social capital describes vertical ties that connect residents, elected officials, and decision-makers, helping residents petition for key public goods and responsive governance during and after crisis (Aldrich 2012, 2019).
These three kinds of social capital often carry trade-offs (Aldrich et al., 2018): communities with an excess of bonding social ties while lacking bridging ties may see hoarding of resources during a crisis (Smiley et al., 2018), while communities with strong bonding and linking ties may benefit at 'others' expense, as occurred when wealthy white neighborhoods offloaded unwanted-but-necessary FEMA trailers into poorer, Black neighborhoods (Aldrich and Crook, 2007). Similarly, one kind of social capital may be more effective for a policy goal than another. For example, studies of past epidemics found that information from trusted personal ties was more effective than centralized information campaigns (Funk et al., 2009; Tai and Sun, 2007; Vinck et al., 2019). Disasters and pandemics often face different challenges, namely physical devastation versus containing viral spread; social distancing, for example, has created social isolation challenges in exchange for stopping the spread of the virus. Despite their differences, we expect social capital is influential in both crises.
Most recently, scholars have linked social capital to COVID-19 in several ways, summarized in Table 1. Several scholars found that social capital was associated with decreasing mobility and more social distancing during the pandemic (Borgonovi and Andrieu, 2020; Bai et al., 2020; Ding et al., 2020; Barrios et al., 2020), while others directly linked it to decreases in case rates and mortality (Yanagisawa et al., 2021; Arachchi and Managi, 2021, Elgar et al., 2020; Varshney and Socher, 2020, Makridis and Wu, 2020, Bartscher et al., 2020a, b), while others linked social ties to increases in both case rates and social distancing behaviors (Milani, 2021). More often, scholars have highlighted using differing terms social capital trade-offs, where insular ties were liked to risky behavior, increases in mobility, and rising case and death rates, while trust in government or commitment to civic norms were related to declines in these outcomes (Elgar et al., 2020; Arachchi and Managi, 2021; Bai et al., 2020; Ding et al., 2020). And recent studies of COVID-19 spread in Japan suggest that linking social capital can be a double-edged sword; communities with strong trust in government can become worse off if those governments do not respond properly to the pandemic (Fraser and Aldrich, 2021). Some preliminary evidence suggests that bridging ties, which typically aid communities, might facilitate gatherings and resultant infections instead during COVID-19 (Yanagisawa et al., 2021).
These studies drew on several measures of social ties, including specific individual-level surveys (Elgar et al., 2020; Arachchi and Managi, 2021), the United States Congress Joint Economic Council's (USJEC, 2018) Social Capital Index (Wu et al., 2020; Varshney and Socher, 2020; Makridis and Wu, 2020; Barrios et al., 2020; Ding et al., 2020), Rupasingha et al.'s's (2006) social capital index (Borgonovi and Andrieu, 2020; Bai et al., 2020; Ding et al., 2020), as well as indices derived from Kyne and Aldrich's (2020) framework for measuring social capital (Fraser and Aldrich, 2021).
However, few studies have controlled for bonding (in-group), bridging (inter-group), and linking (vertical) social ties, all at the same time, and many have relied on case rates, which depend on testing capacity. This study tests the bonding, bridging, and linking social capital framework, to identify each's distinct impact. We test (1) whether bonding social capital still produces beneficial effects after controlling for bridging and linking ties, and (2) whether certain types of social capital were more effective at reducing COVID mortality earlier or later in the pandemic. By clarifying whether and how social capital affects the impacts of COVID-19, this study aims to increase awareness of the roles of different kinds of social ties in pandemic response.
3. Methods
This study examined why some U.S. counties experience higher excess death rates during the COVID-19 pandemic than others. Excess death rates refer to how many additional deaths per 100,000 residents occurred in a time-period in 2020 compared to the same period in 2018. As discussed above, excess death rates are among the best ways to measure the impact of a disaster whose impacts are not readily visible (Woolf et al., 2020; Santos-Burgoa et al., 2018). We focus on the case of U.S. counties, the smallest unit of analysis for which mortality data in 2020 is currently available. This granular approach helps us see the effects of community level traits, as compared to past state or nation-level studies (Banerjee et al., 2020; Woolf et al., 2020).
3.1. Data
This analysis used panel datasets to determine to what degree social capital was associated with COVID-19 outcomes. Our analytical strategy includes 1) modeling a complete unbalanced panel of county excess death rates over six time-periods, 2) modeling just our balanced panel of 286 counties over time, and 3) modeling matched samples over time, which we describe further below.
First, we tabulated excess death rates as an unbalanced panel of up to 947 counties over six time-periods. Later time-periods had more data available, creating an unbalanced panel dataset. Fig. 1 maps the geography of this dataset, highlighting counties based on their first observation available. Early time-period skew urban (e.g., New York, Detroit, and Los Angeles), while later observations tended to include rural and suburban counties, as COVID spread throughout the U.S.
Fig. 1.
Map of Counties in original Unbalanced Panel Dataset.
Fig. 2 highlights histograms of excess death rates in this unbalanced panel dataset. Here, we compare those excess death rates, showing the difference in 2020 deaths rates compared to prior death rates based on 1-year, 3-year averages, and 5-year averages. Their transparent distributions overlap almost perfectly as virtually identical measures, showing dark orange where overlapping. Each version is highly correlated with the other, with a Pearson's r correlation coefficient of 0.98, as shown in Appendix Figure A4, and they produce nearly identical correlations with our key variables of interest in Figure D3.
Fig. 2.
Distribution of county excess death rates over 6 study time periods.
Second, as robustness tests, we identified a balanced panel of 286 counties with observations for all six time-periods, because unbalanced panels alone are not ideal for estimating causal effects. Violin plots in Appendix Figure A5 show that unbalanced and balanced panels share surprisingly similar distributions with the full population of U.S. counties in terms of 19 key covariates. (The main exceptions are that counties from the unbalanced and balanced panels tend to be slightly more densely settled, Democrat-leaning, or highly educated than the population; see Appendix.) However, this balanced panel also carried drawbacks, leaving out counties that later experienced COVID cases.
Third, as further robustness tests, we employed matched samples. We refined this dataset by creating five matched datasets, including counties as similar as possible except that some had higher levels of specific types of social capital than others, described further below. The number of counties in each dataset is summarized in Table 2 . Below, we summarize our proxies and models.
Table 2.
U.S. Counties with observable excess death rates over time.
| Type of Sample | # Counties Observed per Time Period 1 |
Total Obs. |
|||||
|---|---|---|---|---|---|---|---|
| 2/1 to 4/25 | 4/26 to 5/16 | 5/17 to 5/23 | 5/24 to 8/22 | 8/23 to 8/29 | 8/30 to 9/26 | ||
| Unbalanced Panel | 287 | 287 | 461 | 524 | 923 | 947 | 3429 |
| Balanced Panel | 286 | 1716 | |||||
| Panel Matched for Overall Social Capital | 51 | 306 | |||||
| Panel Matched for All (Bonding, Bridging, & Linking Social Capital) | 64 | 384 | |||||
| Panel Matched for Bonding Social Capital | 64 | 384 | |||||
| Panel Matched for Bridging Social Capital | 58 | 348 | |||||
| Panel Matched for Linking Social Capital | 80 | 480 | |||||
Note:1 for all except Unbalanced Panel, this number is constant.
3.2. Proxies
This study used several proxies to model excess death rates. We list them briefly here, and discuss them at length in Appendix Section A1 Proxies. First, to represent the effect of social capital, we used Kyne and Aldrich's (2020) Social Capital Indices of U.S. counties, which includes three validated indices representing bonding, bridging, and linking social capital, as well as an overall measure of social capital which averages these three subtypes. We use a revised version of their bonding social capital index, measuring bonding ties via a proxy of community similarity, since people tend to make bonding ties among members of the same societal groups (see Appendix).
Second, we measured political factors, including the density of Democratic voters and government capacity, via the density of municipal employees. Next, we controlled for the capacity of health care systems by averaging two indicators, and the quality of health in each county by averaging seven indicators of health, supplemented by the rate of people with health insurance. Finally, we controlled for socioeconomic vulnerability using median household income and college education rates, the share of residents (1) over age 65, (2) who are women, and (3) who are Black, and population density. Each covariate is described at length in Appendix A, including sources and justifications, with descriptive statistics in Figure A3. Finally, this study does not control for mobility, but rather conceptualizes mobility as one of several ways that social capital changes resident behaviors and might ultimately shape excess death rates. We encourage future scholars to investigate more fully the relationship between pandemic mobility, mobility restrictions, and types of social capital.
3.3. Unbalanced panel models
To model excess death rates, we used ordinary least squares models. We compared several kinds of models. First, we modeled the unbalanced panel using (1) fixed effects for each period, and then repeated these models using (2) linear mixed models with random effects for each time-period. We also used (3) generalized estimating equation (GEE) models with an exchangeable or AR-1 correlation structure and robust standard errors as a robustness test. The correlation structure was selected based on which produced the lowest quasi-likelihood criterion. These estimation strategies (particularly fixed/random effects) help take care of the temporal variation due to the length or other characteristics of the time-period observed. We chose to use fixed/random effects for time-periods, rather than counties, to (1) account for the different dynamics of the pandemic over time, (2) make inferences among communities, not time-periods, and (3) maintain a small number of fixed effects given the large number of covariates and limited degrees of freedom in a statistical model. Together, these three modeling techniques help verify that our results are not due to statistical noise; we draw our conclusions from model coefficient effects which frequently occur across two or more types of models (as exemplified in Figure D4). These models are reported in Table B1.
3.4. Balanced panel models
Then, after the primary unbalanced panel models, we employed several robustness checks to confirm whether the direction of model estimates remained consistent. As our first robustness check, we narrowed into just the balanced panel, comparing (4) fixed effects, (5) random effects, and (6) GEE models. We generated these six models controlling for overall social capital, and then generated a second set of six models controlling for each social capital subtype in Table C1.
These balanced models revealed the same effects as unbalanced panel models for bonding, bridging, and linking social capital on excess death rates, albeit with less statistically significant results. The effect of bonding social capital (as represented by community similarity) was statistically significant at just p = 0.10, as opposed to p < 0.10 in the unbalanced models. However, our models are of population-level data, not random samples, so the random sampling error that p-values and statistical significance measure not a direct concern in this study. Instead, in population-level studies, statistically significant results flag particularly strong associations given sample size.
3.5. Matched panel models
Next, we performed a second robustness check with matching. To create more meaningful samples, we used coarsened exact matching to identify five different matched samples of counties. These counties were as similar as possible in terms of (1) the median household income, (2) the percentage of residents with some college education or more, (3) the percentage of residents over age 65, (4) population density per 1000 residents, and the (5) percentage of the population that is Black, except that some counties had social capital above the median in that sample while others did not. Coarsened exact matching is a widely used method for making causal inferences (Iacus et al., 2011), often used in health care studies (Azoulay et al., 2011; King et al., 2011; Sidney et al., 2015). More recently, it is preferred over propensity score matching, because it estimates causal effects with the least bias among sample sizes (Brandt et al., 2010; King et al., 2011).
We made five matched samples, each with a key difference. The key differences were as following, using the Kyne & Aldrich indices, for the first through fifth samples: (1) some had overall social capital (average of bonding, bridging, and linking social capital indices) greater than the median; (2) some had all social capital subtypes (bonding, bridging, and linking) score all over the median; (3) some had bonding social capital over the median; (4) some had bridging social capital over the median; and (5) some had linking social capital over the median. Appendix Figure D2 presents diagnostic plots and highlights how matching greatly improves the balance of matching covariates in our data.
In our matched models, sample sizes were smaller, so statistically significant coefficients were rarer. Further, ouro models did not suffer from problematic collinearity, and all variance inflation factors remained under 10. To reduce collinearity when present, we simplified several covariates into 8 or 6 quantiles and regressed these covariates as numeric variables; this helps retain the data's original shape while eliminating collinearity. For some models, these transformations were applied to covariates, including health quality, health care capacity, the share of women and Black residents, college completion rates, and income. Where applicable, all transformations are clearly listed at the bottom of each model table in the Appendix. In the appendix, we present model tables for the unbalanced panel (Table B1), the balanced panel (Table C1), and matched panels (Tables D5 & D6). Finally, to further explore these trends, we modeled our counties with separate models for each time-period (Table E1), and repeated this process for each time-period on matched samples (Tables E3-E4).All tables report standardized effects on excess death rates, describing the expected increase in deaths per 100,000 persons as each covariate increases by 1 standard deviation. Because effects were standardized, they can be compared across covariates.
3.6. Validation
Finally, despite our considerable base of evidence from unbalanced panel, balanced panels, matched samples, and individual time-steps, what if the social capital indices used in this study did not capture social capital as exactly as intended? To validate our results, we repeated our entire methodology using several other common county-level measures of social capital. To compare results about overall social capital, we use (1) Rupasingha and colleagues' (2006) social capital index hosted by Penn State University's Northeast Regional Center for Rural Development (last updated in 2014), as well as (2) the United States Congress Joint Economic Committee's (USJEC, 2018) Social Capital Index. To compare results about social capital subtypes, we use USJEC's four subindices (last updated in 2018), which include family unity (representing bonding ties), collective efficacy (a slightly different type of bonding ties, measured by violent crime rates), community health (an associational measure representing bridging ties), and institutional health (representing linking ties). In short, alternative indices frequently produce the same results, where measures related to bonding social capital were very consistently associated with decreases in excess deaths. We outline these results in depth in Appendix Section A6, summarizing consistent results in Table A7.
4. Results
This study examined why some communities experienced higher excess death rates than others during the COVID-19 pandemic. We analyzed excess deaths through unbalanced panel models, balanced panel models, matched models, models of each time step, and matched models of each time step.
4.1. Bonding social capital associated with lower excess death rates
First, this study finds consistent evidence of a strong association between excess death rates and bonding social capital, measured by community similarity. Communities with higher bonding social capital saw fewer excess deaths over time, in our unbalanced panel models (beta = −2.64, p < 0.10, Table B1). These results were confirmed in our balanced panel models (beta = −2.51, p = 0.10, Table C1), as well as several matched models. These included models on counties as similar as possible except for their level of overall social capital (beta = −7.81, p < 0.05, Table D6). This effect persisted even when modeling counties matched to be as similar as possible except for their level of bonding social capital specifically (beta = −7.81, p < 0.05, Table D5), indicating strong consistency across modeling strategies.
Fig. 3 visualizes the strong, negative effect of bonding social capital in our matched sample (Table D5) using statistical simulation in the Zelig package in R (King et al., 2000; Choirat et al., 2017). Holding all other covariates constant at their means and modes, we varied the level of bonding social capital, represented by community similarity, by two standard deviations above and below the sample mean. Using these conditions, we simulated the expected effect of bonding social capital on excess death rates using 1000 simulations. The straight white line in Fig. 3 depicts the median expected effect, while the bands show the varying projections for excess death rates given different levels of confidence (90, 95, 99, and 99.9%). These trends are consistent across models, as depicted in Figure D4.
Fig. 3.
Higher bonding social capital associated with decreases in excess deaths.
Bonding social capital's ameliorating effect was strongest early on in the pandemic, shortly after stay at home order were made in several states, including between February 1 and April 25 (beta = −10.45, p < 0.10, Table E1), as well as February 26 and May 16 (beta = −2.70, p < 0.10, Table E2). When we zoomed into the individual time steps of the matched sample, we saw a strong negative effect between February 1 and April 25 (beta = −36.39, p < 0.05, Table E4). Further, while the sample size was too small to achieve statistically significant results for other periods (n = 59 for the sample matched for bonding social capital), the first 4 time-periods all demonstrated strong negative effects (beta = −0.06 to −36.39, Table E4). Similarly, when matching for social capital overall, bonding social capital displayed strong negative effects between February 1 and April 25 (beta = −25.10, p < 0.10, Table E3), April 26 and May 16 (beta = −5.27, p < 0.10, Table E3), and May 24 to August 22 (beta = −21.46, p < 0.10, Table E3).
Finally, while bonding social capital was strongly related to excess deaths, overall social capital generally was not. We find some limited evidence that social capital overall was also negatively associated with excess deaths, but only for our models matched using overall social capital (beta = −4.72, p < 0.10, Table D6). However, the bulk of this study's evidence focuses on subtypes of social capital, for which effects were much clearer. While some past studies have found correlations with overall social capital and COVID outcomes (Borgonovi and Andrieu, 2020, for example), several have indicated that subtypes of social capital had diverging effects (Elgar et al., 2020; Arachchi and Managi, 2021; Fraser and Aldrich, 2021).
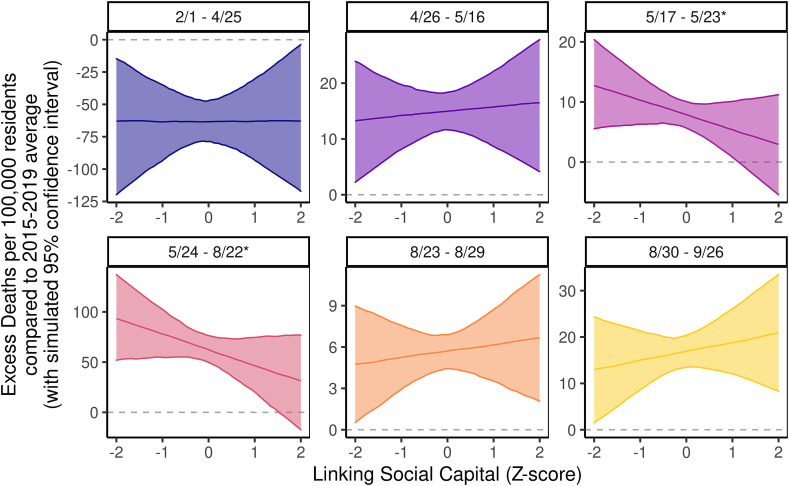
4.2. Linking social capital correlates weakly with declining excess death rates
Second, we found that after matching for overall social capital, communities with stronger linking social capital tended to see lower excess death rates (beta = −3.41, Table D6), although the effect was not statistically significant at convention levels. Instead, this effect was strong and more statistically significant in our models of matched samples by individual time-periods: Linking social capital was negatively associated with excess death rates between May 17 and 23 (beta = −3.40, p < 0.10) as well as May 24 and August 22 (beta = −19.23, p < 0.10), when matched for overall social capital (Table E3).
In Fig. 4 , we visualized the association between linking social capital and overall excess death rates, using the same methodology as in Fig. 3. We repeated this procedure across each of the six time-slices for our models of counties matched by overall social capital, where linking social capital had a statistically significant effect twice (5/17–5/23 and 5/24–8/22). We see that midway through the pandemic, linking capital's negative effect on excess deaths was quite large; trust in and connection to the government was deeply associated with COVID spread.
Fig. 4.
Effect of linking social capital on excess death rates. In sample matched by overall social capital by time-period.
Fig. 5 visualizes these effects descriptively using the difference in mean excess death rates among counties with social capital above and below the median in each time-period, with 95% confidence intervals. In the unbalanced panel, counties with linking social capital above the median tend to have higher excess death rates than those with low linking social capital. However, after zooming into more comparable cases, the effect gradually grows more negative. When comparing counties as similar as possible except that some have high bonding, bridging, and linking social capital while the others have low bonding, bridging, or linking social capital, descriptively, linking social capital becomes increasingly inversely related with excess death rates (although not statistically significant in this visual).
Fig. 5.
Difference in excess death rates in counties with high and low social capital.
Finally, this study also examined the effect of bridging social capital. We found some evidence of a positive association between bridging social capital and excess death rates in unbalanced panel models (beta = 2.61, p < 0.01, Table B1) and balanced panel models (beta = 1.41, Table C1, although statistically insignificant). This was complicated when we examined matched models of individual time-steps. We found strong bridging ties were linked to greater mortality early on (beta = 2.45, p < 0.05, Table E4), but lower mortality later in the pandemic (beta = −3.24, p < 0.10, Table E4). However, future verification is still needed to explain why. One possible explanation for the positive effect of bridging social capital may be the following: After accounting for any beneficial effects of trust in government through linking ties and close ties and social norms through bonding social capital, perhaps the associational ties used to represent bridging social capital in this study led to more gatherings and sites of infection. This contrasts with bridging social capital's usual beneficial effects on community resilience (Aldrich and Meyer, 2015) but matches with recent findings by Yanagisawa et al. (2021). Future studies should investigate more deeply the seemingly divergent relationship of bonding and bridging social capital in COVID-19 outcomes.
5. Discussion
This study examined why some U.S. counties saw higher death rates during the COVID-19 pandemic than we would expect, drawing from county-level excess death rates comparing the years 2020 and a five-year average of 2015–2019. We used available county-level data provided at regular intervals by the CDC to create panel datasets of county observations over six time-periods, and we applied coarsened exact matching to model counties as similar as possible except that they have different levels of social capital. This study found that counties with strong bonding social ties saw fewer excess deaths per 100,000 residents, while counties with strong linking social ties also saw fewer excess deaths overall, especially early in the pandemic.
This study contributes to our understanding of social capital and pandemic response in three ways. First, we showed that social capital subtypes, like bonding, bridging, and linking social ties, were related to COVID-19 outcomes, but overall social capital showed few consistent associations. This strongly suggests that pandemic scholars should discern between each type of social capital, rather than examining overall social capital. This is a strong endorsement for past work on these social capital subtypes (Szreter and Woolcock, 2004; Hawkins and Maurer, 2010; Aldrich and Meyer, 2015; Aldrich et al., 2018; Fraser and Aldrich, 2021).
Second, we showed the critical importance of looking beyond standard snapshots of data which often dominate in analyses of crises and disasters (Hacker and Pierson, 2004). Here, the relationship between social capital and COVID-19 outcomes varied over time. While linking social capital showed statistically significant effects in early-to-middle time-periods (May through August 2020), these effects were too muted to produce statistical significance in later time-periods (August through September 2020). Similarly, bonding social capital was strongly correlated between February and May 2020. This might suggest that trust in government and vertical ties mattered earlier in the crisis than later; after several months, we might expect that information disperses widely, or that people's opinions about social distancing, mask-wearing, and new behaviors become set. As we embark on a course of action, the fewer the options we encounter, solidifying and hardening over actions and preferences over time (Pierson, 2000). This matches with past findings by Bartscher et al. (2020a, b), who found that social capital's effect on case rates, excess deaths, and mobility also varied over time in European jurisdictions.
Alternatively, these effects may have remained statistically insignificant because matching reduced the size of our sample to below 100 counties per time-period. As more data becomes available, future studies should investigate whether these trends persist over wider timespans. However, it is worth noting that despite small samples, many trends were statistically significant, and, as shown in Fig. 2, Fig. 3, produced meaningful differences in excess deaths, matching past findings on social capital's ameliorating effect on case rates and death rates (Borgonovi and Andrieu, 2020; Varshney and Socher, 2020; Makridis and Wu, 2020).
Finally, this study faces several limitations. First, we could not compare across all counties, because the CDC has only provided overall death tallies for counties with at least 1 confirmed death from COVID. Fortunately, our panels closely resemble the full population of U.S. counties, as depicted in Figure A5, which implies that we may cautiously compare these results with other cases. Further, our matching approach allows us to compare communities as similar as possible, making our causal inference stronger.
Second, this study relies purely on aggregate data, not individual data. Future studies should examine qualitative accounts from residents of how social ties shaped their response to the pandemic. Third, because past death data was released monthly, while 2020 death data was released on various dates, we had to estimate past deaths on each date using daily averages of monthly death data. This is a necessary limitation of our excess deaths data, but future analyses should compare against daily data from local coroners' offices where available.
Finally, this study could not examine the association between Hispanic and Latinx ethnicity and excess death rates, because this was highly collinear with bonding social capital, as approximated by community similarity. This implies that these communities shared similarly high levels of bonding social capital, but future studies should compare more specifically the experiences of Hispanic and Latinx communities in their response to COVID.
6. Conclusion
In summary, this study examined why some communities have seen greater excess death rates than others during the COVID-19 pandemic, highlighting the ameliorating effect of bonding and linking social capital on excess death rates. We used a novel matched panel dataset of U.S. counties to model variation in excess death rates using publicly available data. We found that counties with higher bonding social capital tended to see fewer excess deaths per 100,000 residents, especially in the first few months of the pandemic, while linking social capital was associated with a decrease in excess death rates midway through the pandemic.
These findings underscore the importance of social ties in pandemic response. Facing overwhelmed health care systems and lacking federal guides, communities with strong, close-knit social ties and strong linking ties saw fewer excess deaths than comparable communities. Future studies should examine whether bridging social capital would show similar effects given a larger sample size as more data becomes available. Likewise, future studies should examine whether and how linking social ties aided pandemic response. Similarly, past studies indicated that sometimes social capital conveys negative effects on community resilience to crisis (Aldrich et al., 2018); future studies should investigate under what conditions social capital conveyed unintended effects. By clarifying the degree and ways that social capital shaped residents' behaviors, reciprocity, and collective action, we hope this study provokes further opportunities to leverage communities' social capital to combat the pandemic.
Data sharing
All data and complete replication code for this aggregate-level study will be shared immediately following publication, with no end date, for public access and replication. Data are available indefinitely on the Harvard Dataverse at https://doi.org/10.7910/DVN/JTTNKO.
Author credit statement
Timothy Fraser: Formal analysis; Investigation, Data curation, Methodology, Writing – original draft. Daniel P. Aldrich: Conceptualization, Methodology, Writing – review & editing. Courtney Page-Tan: Conceptualization, Methodology, Writing – review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114241.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aldrich D.P. University of Chicago Press; 2012. Building Resilience: Social Capital in Post-disaster Recovery. [Google Scholar]
- Aldrich D.P. University of Chicago Press; 2019. Black Wave: How Networks and Governance Shaped Japan's 3/11 Disasters. [Google Scholar]
- Aldrich D.P., Crook K. Strong civil society as a double-edged sword. Polit. Res. Q. 2007;61(3):379–389. [Google Scholar]
- Aldrich D.P., Meyer M.A. Social capital and community resilience. Am. Behav. Sci. 2015;59(2):254–269. [Google Scholar]
- Aldrich D.P., Page-Tan C., Fraser T. In: Lausanne, CH: EPFL International Risk Governance Center. Trump B.D., editor. 2018. A Janus-faced resource: social capital and resilience trade-offs. [Google Scholar]
- Arachchi I., Managi S. The role of social capital in COVID-19 deaths. BMC Publ. Health. 2021;21:434. doi: 10.1186/s12889-021-10475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay P., Graff Zivin Joshua S., Sampat B.N. National Bureau of Economic Research Working Paper; 2011. The Diffusion of Scientific Knowledge across Time and Space: Evidence from Professional Transitions for the Superstars of Medicine; p. 16683. [Google Scholar]
- Bai J.J., Jin W., Wan C. The impact of social capital on individual responses to COVID-19 pandemic: evidence from social distancing. 2020 (Social Science Research Network) [Google Scholar]
- Baicker K., Chandra A. Medicare spending, the physician workforce, and beneficiaries' quality of care. Health Aff. 2004;23:W4–W197. doi: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- Banerjee A., Pasea L., Harris S., Gonzalez-Izquierdo A., Torralbo A., Shallcross L., et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395(10238):1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrios J.M., Benmelech E., Hochberg Y.V., Sapienza P., Zingales L. Civic capital and social distancing during the covid-19 pandemic. Stigle Center Study Econ. State Work. Pap. Ser. 2020;44:1–45. [Google Scholar]
- Bartscher A.K., Seitz S., Siegloch S., Slotwinski M., Wehrhöfer N. The role of social capital in the spread of covid-19. VoxEu CEPR. 2020 doi: 10.1016/j.jhealeco.2021.102531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartscher A.K., Seitz S., Siegloch S., Slotwinski M., Wehrhöfer N. IZA Institute of Labor Economics; 2020. Social capital and the spread of COVID-19: insights from European countries. 13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonaccorsi G., Pierri F., Cinelli M., Flori A., Galeazzi A., Porcelli F., et al. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(27):15530–15535. doi: 10.1073/pnas.2007658117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgonovi F., Andrieu E. Bowling together by bowling alone: social capital and covid-19. COVID Econ. 2020;17:73–96. doi: 10.1016/j.socscimed.2020.113501. [DOI] [PubMed] [Google Scholar]
- Borgonovi F., Andrieu E., Subramanian S.V. Community level social capital and COVID-19 infections and fatality in the United States. COVID Econ. 2020;32:110–126. [Google Scholar]
- Bowen J.T., Laroe C. Airline networks and the international diffusion of severe acute respiratory syndrome (SARS) Geogr. J. 2006;172(2):130–144. doi: 10.1111/j.1475-4959.2006.00196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt S., Gale S., Tager I.B. Estimated effect of asthma case management using propensity score methods. Am. J. Manag. Care. 2010;16(4):257–264. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Provisional COVID-19 Death Counts in the united states by County.https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-in-the-United-St/kn79-hsxy [Google Scholar]
- Centers for Disease Control and Prevention . 2021. Underlying Causes of Death Database 1999-2019.https://wonder.cdc.gov/ucd-icd10.html Retrieved March 15, 2021 from. [Google Scholar]
- Chin-Hong P., Alexander K.M., Haynes N., Albert M.A., The Association of, Black Cardiologists. Pulling at the heart: COVID-19, race/ethnicity and ongoing disparities. Nat. Rev. Cardiol. 2020;17(9):533–535. doi: 10.1038/s41569-020-0416-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choirat C., Honaker J., Imai K., King G., Lau O. 2017. Zelig: Everyone's Statistical Software.http://zeligproject.org/ version 5.1.4.90000. [Google Scholar]
- Cox R.S., Perry K.E. Like a fish out of water: reconsidering disaster recovery and the role of place and social capital in community disaster resilience. Am. J. Community Psychol. 2011;48(3–4):395–411. doi: 10.1007/s10464-011-9427-0. [DOI] [PubMed] [Google Scholar]
- Cutter S.L., Boruff B.J., Shirley L.W. Social vulnerability to environmental hazards. Soc. Sci. Q. 2003;84(2):242–261. [Google Scholar]
- Ding W., Levine R., Lin C., Xie W. National Bureau of Economic Research Working Paper; 2020. Social Distancing and Social Capital: Why U.S. Counties Respond Differently to COVID-19; p. w27393. [Google Scholar]
- Durante R., Guiso L., Gulino G. Asocial capital: civic culture and social distancing during COVID-19. J. Publ. Econ. 2021;194:104342. doi: 10.1016/j.jpubeco.2020.104342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar F.J., Stefaniak A., Wohl M.J.A. The trouble with trust: time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc. Sci. Med. 2020;263:113365. doi: 10.1016/j.socscimed.2020.113365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott J.R., Haney T.J., Sams-Abiodun P. Limits to social capital: comparing network assistance in two new orleans neighborhoods devastated by hurricane katrina. Socio. Q. 2010;51(4):624–648. doi: 10.1111/j.1533-8525.2010.01186.x. [DOI] [PubMed] [Google Scholar]
- Enarson E. Through women's eyes: a gendered research agenda for disaster social science. Disasters. 1998;22(2):157–173. doi: 10.1111/1467-7717.00083. [DOI] [PubMed] [Google Scholar]
- Farag M., Nandakumar A.K., Wallack S., Hodgkin D., Gaumer G., Erbil C. Health expenditures, health outcomes and the role of good governance. Int. J. Health Care Finance Econ. 2012;13(1):33–52. doi: 10.1007/s10754-012-9120-3. [DOI] [PubMed] [Google Scholar]
- Fraser T., Aldrich D.P. The dual effect of social ties on COVID-19 spread in Japan. Sci. Rep. 2021;11(1596):1–12. doi: 10.1038/s41598-021-81001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk S., Gilad E., Watkins C., Jansen V.A.A. The spread of awareness and its impact on epidemic outbreaks. Proc. Natl. Acad. Sci. Unit. States Am. 2009;106(16):6872–6877. doi: 10.1073/pnas.0810762106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman D.C., Grumbach K. Does having more physicians lead to better health system performance? Jama. 2008;299(3):335–337. doi: 10.1001/jama.299.3.335. Retrieved 10/21/2020. [DOI] [PubMed] [Google Scholar]
- Grossman G., Kim S., Rexer J., Thirumurthy H. Social Science Research Network; 2020. Political partisanship influences behavioral responses to 'governors' recommendations for COVID-19 prevention in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker J., Pierson P. Princeton University Press; Princeton, NJ: 2004. Politics in Time: History, Institutions, and Social Analysis. [Google Scholar]
- Hawkins R.L., Maurer K. Bonding, bridging and linking: how social capital operated in New OrleansNO following Hurricane Katrina. HK Br. J. Soc. Work. 2010;40:1777–1793. [Google Scholar]
- Iacus S.M., King G., Porro G. Causal inference without balance checking: coarsened exact matching. Polit. Anal. 2011;20(1):1–24. [Google Scholar]
- Iwasaki K., Sawada Y., Aldrich D.P. Social capital as a shield against anxiety among displaced residents from fukushima. Nat. Hazards. 2017;89(1):405–421. [Google Scholar]
- Jean-Baptiste C., Herring R.P., Beeson W.L., Dos Santos H., Banta J.E. Stressful life events and social capital during the early phase of COVID-19 in the U.S. Soc. Sci. Human. Open. 2020;2(1):100057. doi: 10.1016/j.ssaho.2020.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaye I.M., Horney J. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am. J. Prevent. Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Subramanian S.V., Kim D. Springer; New York: 2008. Social Capital and Health. [Google Scholar]
- King G., Tomz M., Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. Am. J. Polit. Sci. 2000;44(2):347. [Google Scholar]
- King G., Nielsen R., Coberley C., Pope J.E., Wells A. Avoiding randomization failure in program evaluation, with application to the medicare health support program. Popul. Health Manag. 2011;14(S1):11–22. doi: 10.1089/pop.2010.0074. [DOI] [PubMed] [Google Scholar]
- Kontis V., Bennett J.E., Rashid T., Parks R.M., Pearson-Stuttard J., Guillot M., et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat. Med. 2020 doi: 10.1038/s41591-020-1112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuchler T., Russel D., Stroebel J. The geographic spread of COVID-19 correlates with structure of social networks as measured by Facebook. 2020 doi: 10.1016/j.jue.2020.103314. (NBER Working Paper) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyne D., Aldrich D.P. Capturing bonding, bridging, and linking social capital through publicly available data. Risk Hazards Crisis Publ. Pol. 2020;11(1):61–86. [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Bonding and bridging social capital and their associations with self‐evaluated community resilience: a comparative study of East Asia. J. Community Appl. Soc. Psychol. 2019;30(1):31–44. [Google Scholar]
- Lee J., Fraser T. How do natural hazards affect participation in voluntary association? the social impacts of disasters in Japanese society. Int. J. Disaster Risk Reduct. 2019;34:108–115. [Google Scholar]
- Makridis C.A., Wu C. Social Science Research Network; 2020. Ties that bind (and social distance): how social capital helps communities weather the COVID-19 pandemic. [Google Scholar]
- Mallapaty S. The coronavirus is most deadly if you are older and male — new data reveal the risks. Nature. 2020;585:16–17. doi: 10.1038/d41586-020-02483-2. [DOI] [PubMed] [Google Scholar]
- Milani F. COVID-19 outbreak, social response, and early economic effects: a global VAR analysis of cross-country interdependencies. J. Popul. Econ. 2021;34:223–252. doi: 10.1007/s00148-020-00792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I.F., Becker A.D., Grenfell B.T., Metcalf C.J. Disease and healthcare burden of COVID-19 in the United States. Nat. Med. 2020;26(8):1212–1217. doi: 10.1038/s41591-020-0952-y. [DOI] [PubMed] [Google Scholar]
- New York Times . 2021. The COVID-19 Pandemic.https://www.nytimes.com/news-event/coronavirus June 8. [Google Scholar]
- Painter M., Qiu T. Social Science Research Network; 2020. Political beliefs affect compliance with COVID-19 social distancing orders. [Google Scholar]
- Pierson P. Increasing returns, path dependence, and the study of politics. Am. Polit. Sci. Rev. 2000;94(2):251–267. [Google Scholar]
- Putnam R.D. Simon and Schuster; New York: 2000. Bowling Alone. The Collapse and Revival of American Community. [Google Scholar]
- Rivera R., Rolke W. Modeling excess deaths after a natural disaster with application to Hurricane Maria. Stat. Med. 2019;38(23):4545–4554. doi: 10.1002/sim.8314. [DOI] [PubMed] [Google Scholar]
- Rupasingha A., Goetz S.J., Freshwater D. The production of social capital in U.S. counties. J. Soc. Econ. 2006;35:83–101. [Google Scholar]
- Salvati P., Petrucci O., Rossi M., Bianchi C., Pasqua A.A., Guzzetti F. Gender, age and circumstances analysis of flood and landslide fatalities in Italy. Sci. Total Environ. 2018;610–611:867–879. doi: 10.1016/j.scitotenv.2017.08.064. [DOI] [PubMed] [Google Scholar]
- Santos-Burgoa C., Sandberg J., Suárez E., Goldman-Hawes A., Zeger S., Garcia-Meza A., et al. Differential and persistent risk of excess mortality from Hurricane Maria in Puerto Rico: a time-series analysis. Lancet Planet. Health. 2018;2(11):e478–e488. doi: 10.1016/S2542-5196(18)30209-2. [DOI] [PubMed] [Google Scholar]
- Schoenbaum S.C., Schoen C., Nicholson J.L., Cantor J.C. Mortality amenable to health care in the United States: the roles of demographics and health systems performance. J. Publ. Health Pol. 2011;32(4):407–429. doi: 10.1057/jphp.2011.42. [DOI] [PubMed] [Google Scholar]
- Sharkey P. 2020. The U.S. Has a Collective Action Problem That's Larger than the Coronavirus Crisis. April 10. Vox. [Google Scholar]
- Sidney J.A., Coberley C., Pope J.E., Wells A. Extending coarsened exact matching to multiple cohorts: an application to longitudinal well-being program evaluation within an employer population. Health Serv. Outcome Res. Methodol. 2015;15:136–156. [Google Scholar]
- Smallman-Raynor M., Cliff A.D. The geographical spread of avian influenza A (H5N1): panzootic transmission (December 2003-May 2006), pandemic potential, and implications. Ann. Assoc. Am. Geogr. 2008;98(3):553–582. [Google Scholar]
- Smiley K.T., Howell J., Elliott J.R. Disasters, local organizations, and poverty in the USA, 1998 to 2015. Popul. Environ. 2018;40(2):115–135. [Google Scholar]
- Szreter S., Woolcock M. Health by association? social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 2004;33(4):650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Tai Z., Sun T. Vol. 9. New Media & Society; 2007. Media dependencies in a changing media environment: the case of the 2003 SARS epidemic in China; pp. 987–1009. 6. [Google Scholar]
- Townsend M.J., Kyle T.K., Stanford F.C. Outcomes of COVID-19: disparities in obesity and by ethnicity/race. Int. J. Obes. 2020;44(9):1807–1809. doi: 10.1038/s41366-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USJEC (Senator Mike Lee) 2018. The Geography of Social Capital in america. (United States Congress Joint Economic Committee) [Google Scholar]
- Varshney L.R., Socher R. COVID-19 growth rate decreases with social capital. medRxiv. 2020 2020.04.23.20077321. [Google Scholar]
- Vinck P., Pham P.N., Bindu K.K., Bedford J., Nilles E.J. Institutional trust and misinformation in the response to the 2018-19 Ebola outbreak in North Kivu, D.R. Congo: a population-based survey. Lancet Infect. Dis. 2019;19(5):529–536. doi: 10.1016/S1473-3099(19)30063-5. [DOI] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, march-april 2020. Jama. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. Retrieved 10/21/2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C. Social capital and COVID-19: a multidimensional and multilevel approach. Chin. Sociol. Rev. 2021;53(1):27–54. [Google Scholar]
- Wu C., Wilkes R., Fairbrother M., Giordano G. 2020. Social Capital, Trust, and State Coronavirus Testing. (Contexts) [Google Scholar]
- Yanagisawa M., Kawachi I., Scannell C.A., Oronce C.I.A., Tsugawa Y. Association between county-level social capital and the burden of COVID-19 cases and deaths in the United States. Ann. Epidemiol. 2021;59:21–23. doi: 10.1016/j.annepidem.2021.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye M., Aldrich D.P. Substitute or complement? how social capital, age and socioeconomic status interacted to impact mortality in Japan's 3/11 tsunami. SSM - Popul. Health. 2019;7:100403. doi: 10.1016/j.ssmph.2019.100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S., et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368(6498):1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.