Abstract
Caregiver mental health is crucial to the wellbeing of children. This is most apparent when caregivers face high levels of stress or life adversity. To study this phenomenon in the current global context, this study examined the relation between stress/disruption from the COVID-19 pandemic and the mental health of female and male caregivers. Pre-pandemic childhood adversity was considered as a moderator of this association. A multi-national sample (United Kingdom, 76%; United States, 19%; Canada, 4%, and Australia, 1%) was recruited in May 2020, of whom 348 female and 143 male caregivers of 5–18 year-old children provided data on the constructs of interest. At this time, caregivers reported on their history of adverse childhood experiences (ACEs) and COVID stress/disruption. About two months later (July 2020) caregiver mental health was evaluated. We examined differences between female and male caregivers on ACEs, COVID stress/disruption, and mental health (distress, anxiety, substance use, and posttraumatic stress). Main and interactive effects of ACEs and COVID stress/disruption on each mental health outcome were examined. Female caregivers reported higher COVID stress/disruption, more ACEs, and greater distress, anxiety, and posttraumatic stress symptoms compared to male caregivers. Among female caregivers, higher COVID stress/disruption and more adverse childhood experiences (ACEs) independently predicted all mental health outcomes, consistent with a stress accumulation model. Among male caregivers, a pattern of interactions between COVID stress/disruption and ACEs suggested that the effects of COVID stress/disruption on mental health was stronger for those with higher ACEs, especially for substance use, consistent with a stress sensitization model. Higher levels of stress and mental health difficulties among female caregivers suggests a disproportionate burden due to pandemic-related disruption compared to male caregivers. Findings speak to the disparate effects of COVID-19 on the mental health of female compared to male caregivers, and the role of pre-existing vulnerabilities in shaping current adaptation.
Keywords: Mental health, Caregivers, COVID-19, Pandemic, Early adversity, ACEs
1. Introduction
Caregiver mental health is critical to the adjustment of children. Under conditions of stress, changes in caregiver behavior, emotional availability, and psychological functioning may have a cascading effect on the wellbeing of children (Masarik and Conger, 2017). According to the family stress model, external stressors may permeate the family unit and undermine the adaptive caregiving processes that are essential for children's development (Conger et al., 2010). While the family stress model focuses primarily on economic hardship as a source of external stress, this model has recently been re-formulated and applied to the ongoing COVID-19 pandemic (Prime et al., 2020). According to this framework, pandemic-related stress and disruption—including job loss, financial insecurity, crowding, resource depletion, widespread social distancing, and extended quarantine/confinement—may exert its impact on children via changes in family processes, structure, and organization (Prime et al., 2020). Central to this model is the wellbeing of caregivers, whose physical and mental health is crucial to engage in effective leadership, coping, and meaning-making during the pandemic. In effect, caregivers serve as a funnel through which stress and disruption from the pandemic impact overall family functioning and child adjustment.
The capacity of caregivers to provide nurturance, safety, guidance, and protection to their children under conditions of stress depends, in part, on their own mental health. Children of caregivers with mental health difficulties are at an increased risk of abuse and neglect, poor social and academic functioning, and more emotional, behavioral, and physical health problems (Ayers et al., 2019; Leijdesdorff et al., 2017; Pierce et al., 2020a, 2020b). During COVID-19, reports of heightened adult mental health problems in the general public have been reported cross-nationally (Rajkumar, 2020; Serafini et al., 2020; Shi et al., 2020; Vindegaard and Benros, 2020; Xiong et al., 2020). Caregivers have an added burden during the pandemic, including increased parenting stress, concerns about accessing (and safety of) childcare, the added responsibility of homeschooling, stress about repeated school closures and re-integration, concerns about the physical health of their children, and worries about their children's social and emotional development due to prolonged separation from peers and teachers (e.g., Neece et al., 2020). Recent reports among caregivers with children at home indicate more frequent use of alcohol as a coping strategy during the pandemic as compared to non-caregivers, which in turn is related to more alcohol problems (Wardell et al., 2020). Moreover, in a recent survey, caregivers with children in the home were more likely to report feeling depressed than adults without children (Centre for Addiction and Mental Health, 2020). These findings highlight the unique mental health needs of caregivers during the pandemic.
Currently, very few studies have focused solely on the processes involving caregiver wellbeing and child adjustment. In one study, parents of children with mental and physical difficulties reported more burnout, less perceived social support, and negative changes in their parenting style (Fontanesi et al., 2020). Another study showed that parents who lost their jobs during the pandemic reported higher depression and more psychological mistreatment of their children, as well as a greater risk of physical abuse when their capacity to engage in cognitive reframing was low (Lawson et al., 2020). In addition to financial stress, caregiver anxiety and depression is associated with higher child abuse potential during the pandemic (Brown et al., 2020). Finally, a recent study suggested that 27% of parents of children age <18 years reported worsening mental health and, for 1 in 10 families, this was accompanied by worsening behavioral functioning of children (Patrick et al., 2020). These declines were associated with multiple stressors such as heightened risk of food insecurity, loss of childcare, and changes in insurance status. All told, these studies suggest that COVID-related stress and disruption is having a negative impact on caregivers, with harmful downstream consequences for children and the overall functioning of families (Prime et al., 2020).
Inclusion of male caregivers in family-based research is imperative to elucidating the complexity of parenting within a family systems framework (Cabrera et al., 2018). However, no study has examined the disparate impact of the COVID-19 pandemic on the wellbeing of female versus male caregivers. This may be partly due to the general underrepresentation of male caregivers in family research studies (Phares et al., 2005). Although a modest trend for greater involvement of male caregivers in family-based research has occurred over the last decade, it remains a challenge recruiting sufficient numbers of male caregivers to make appropriate comparisons with female caregivers (Parent et al., 2017). In the current study, we recruited a relatively large sample of female (n = 348) and male (n = 143) caregiver of children aged 5–18 years to examine the disparate effects of COVID-19 stress and disruption on caregiver mental health.
Finally, in keeping with theoretical models suggesting that not all individuals will be impacted by the pandemic in the same way (Prime et al., 2020), we examined the role of pre-pandemic adversity on the mental health of female and male caregivers. One of the strongest risk factors for mental health difficulties in adulthood is a history of childhood maltreatment and family dysfunction, collectively referred to as adverse childhood experiences (ACEs). Childhood maltreatment accounts for about 30% of psychiatric disorders in adulthood (Kessler et al., 2010), and a greater number of ACEs is associated with an increased risk of multiple physical and mental health problems over the life course, including alcohol use, smoking, cancer, heart disease, sexual risk-taking, suicidal behavior, and psychiatric disorders (Bellis et al., 2014; Hughes et al., 2017). The contribution of ACEs to the mental health of caregivers during the COVID-19 pandemic is unknown. Thus, we test two competing models on the role of ACEs and COVID-specific stress in shaping caregiver mental health outcomes. The first is the stress accumulation model for understanding how early childhood adversity and adult stress exposure operate with respect to one another. This suggests that childhood adversity and adult stress exposure are additive and independent (Hostinar et al., 2015). Statistically, stress accumulation manifests as main effects for COVID-19 stress/disruption and ACEs on mental health, with no interaction between them. This pattern would indicate that individuals with both higher levels of COVID-19 stress/disruption and higher levels of ACEs would have poorer mental health.
The second model of the way in which early adversity and adult stress exposure operate together is a stress sensitization model. This model posits that the effects of recent stress on mental health are most pronounced among those with a history of adversity (McLaughlin et al., 2010). In other words, although recent pandemic stress may have a negative impact on the wellbeing of many caregivers, this effect may be greater among those who have also experienced prior adversity. An assumption of the stress sensitization model is that COVID-19 stress/disruption and ACEs have a multiplicative effect on mental health problems (Hostinar et al., 2015). Statistically, this manifests as a significant interaction between COVID-19 stress/disruption and ACEs in the prediction of caregiver mental health problems. This pattern would indicate that the influence of COVID-19 stress/disruption on caregiver mental health outcomes would depend, in part, on their pre-existing ACEs.
At present, there exists limited support for each of these models in the context of COVID-19. A recent study of adolescents showed that elevations in posttraumatic stress symptoms as a function of greater COVID-19 exposure (self- or other-exposure) was greater for those with a history of maltreatment than those with no such history (Guo et al., 2020). This study also demonstrated an independent and additive effect of fear of COVID-19 exposure and ACEs on both posttraumatic stress symptoms and anxiety, and a marginal interaction between these constructs in predicting anxiety. This study therefore provides mixed evidence for the stress accumulation and sensitization models, depending on the constructs investigated and the mental health outcome of interest. Further examination of stress accumulation and stress sensitization models in the context of COVID-19 is warranted in order to better elucidate the ways in which COVID-19 stress/disruption may manifest, particularly for caregivers.
Examining differences between female and male caregivers in terms of COVID stress/disruption, ACEs, and mental health is important to effectively respond to the mental health needs of subgroups that may be more negatively impacted by the pandemic. For instance, the unique impact of the pandemic on women has been highlighted previously (Connor et al., 2020; Gausman and Langer, 2020), as has the impact on caregivers specifically (Russell et al., 2020). This interaction between sex and caregiver role may reveal important patterns that can inform policies and programs to address the unique needs of female and male caregivers, respectively. This may ultimately help to prevent the widening of mental health disparities and ensure adequate access to appropriate gender-based health and social services.
In the current study, we examine the disparate effects of COVID-19 stress/disruption and ACEs on the mental health of female and male caregivers in four domains: distress, anxiety, substance use, and posttraumatic stress symptoms. We examine mean differences between female and male caregivers, and test for the main and interactive effects of COVID-19 stress/disruption and ACEs on mental health in a cross-national sample from May 2020 to July 2020. We hypothesize the following: (i) compared to male caregivers, female caregivers will report more ACEs, consistent with large pre-pandemic epidemiological studies that have demonstrated more ACEs (or greater likelihood of individual ACEs) in women compared to men (Keyes et al., 2012; Merrick et al., 2018); (ii) compared to male caregivers, female caregivers will report more mental health difficulties on average, especially distress-related psychopathology (depression, anxiety, posttraumatic stress), consistent with higher rates of mental health difficulties in these domains among women both prior to the pandemic (e.g., Olff et al., 2007; Steel et al., 2014) and during the pandemic (e.g., Daly et al., 2020; Xiong et al., 2020); (iii) the relation between COVID stress/disruption and mental health difficulties will be stronger among female compared to male caregivers. This hypothesis derives from two findings in the extant literature: first is that, compared to men, women assume a disproportionate level of caregiving responsibility and experience more caregiving stress in general (Pinquart and Sörensen, 2006), and are experiencing more multifactorial stress during the pandemic (Connor et al., 2020). Second is that, broadly speaking, there are sex differences in stress responsiveness that are, at least in part, hormonally- and neurobiologically-mediated (Bale and Epperson, 2015; Bangasser and Valentino, 2014; Heck and Handa, 2019). This increase in stressors and responsiveness to stress may result in greater risk of mental health difficulties among female compared to male caregivers during the ongoing pandemic. Notwithstanding the expectation of a stronger relation between COVID stress/disruption and mental health difficulties among female caregivers, we did not hypothesize differences between female and male caregivers in stress accumulation versus stress sensitization, as there are limited prior studies on which to base this hypothesis. Thus, this remained an exploratory question in the current study.
2. Methods
2.1. Participants and procedure
The current study is part of a prospective cohort of 549 caregivers (M age = 41.33, SD age = 6.329) designed to understand the effects of COVID-19 stress and disruption on family wellbeing. The current study draws on data from the baseline assessment in May 2020 (Time 1) and the first follow-up assessment in July 2020 (Time 2). Respondents were recruited via Prolific®, an online research panel company. Recruitment was limited to caregivers with at least two children per family (aged 5–18 years), as other objectives of the broader project were to evaluate within-family differences in family processes in the context of COVID-19. Caregivers were mostly married/common-law (90%), White-European (73%), females (68%), who resided in either the United Kingdom (76%), United States (19%), Canada (4%) or Australia (1%). Following recruitment, participants completed online questionnaires via Qualtrics®, which included measurement of stressful events and disruptions related to COVID-19, early adversity, and current mental health (see Measures section). For the current study, caregivers reported on their own mental health, history of childhood adversity, and COVID stress/disruption. There were 491 participants with complete data on these constructs. The analyses were conducted on this final sample. Ethics approval was received from all listed institutions.
2.2. Measures
COVID Stress/Disruption. At T1, multiple stressors related to the pandemic were assessed that covered disruption across numerous aspects of life, including finances, basic needs, personal and family welfare, career/education, and household responsibilities. Participants rated how applicable each stressor was to their households on a three-point scale: “Not True” (1), “Somewhat True” (2) and “Very True” (3). The full scale is presented in the Supplementary Materials. Participants completed this measure at baseline (May 2020). Principal components analyses revealed that a single component explained 23.95% (λ = 5.99) of the variation and the items demonstrated strong internal consistency, overall (α = 0.85). Internal consistency for female (α = 0.84) and male (α = 0.87) caregivers was equally strong.
Adverse Childhood Experiences (ACEs). At T1, caregivers reported on their history of adversity using the revised version of the Adverse Childhood Experiences Questionnaire developed by Finkelhor et al. (2015). Caregivers responded to a number of items related to childhood maltreatment and family dysfunction, including childhood abuse, neglect, peer victimization, exposure to community violence, socioeconomic status, etc. Items were endorsed as either present (1) or absent (0) and then summed into an ACEs index that ranged from 0 to 14 (mean = 2.72, median = 2).
Caregiver Mental Health. At T2, four domains of caregiver mental health were assessed using validated questionnaires. First, psychological distress was measured using the Kessler Psychological Distress Scale (K10; Kessler et al., 2002). The K10 is a widely utilized 10-item questionnaire that yields a global measure of distress related to depression and anxiety symptoms. Items assess feelings experienced in the past 30 days, with response options ranging from “None of the time” (1) to “All of the time” (5). We used the continuous version of the scale. Internal consistency in the current sample was good (Cronbach's ɑ = 0.93). Second, anxiety was assessed using the short-form of the Patient-Reported Outcomes Measurement Information System (PROMIS®; v1.0, 4-item; PROMIS Health Organization, 2016). Caregivers responded to 4 items assessing fear, worries, and anxiety over the past 7 days, with response options ranging from “Never” (1) to “Always” (5). Internal consistency in the current sample was good (Cronbach's ɑ = 0.92). Third, substance use was assessed using the Tobacco, Alcohol, Prescription Medication, and other Substance use Tool (TAPS; McNeely et al., 2016). Caregivers responded to 4 items assessing alcohol, tobacco, marijuana, and other prescriptions and non-prescription drug use over the past month, with response options ranging from “Everyday” (1) to “Never” (6). Internal consistency in the current sample was acceptable (Cronbach's ɑ = 0.61). The scale was reverse coded such that higher scores reflected more substance use. Finally, posttraumatic stress was evaluated using the Trauma Screening Questionnaire (TSQ; Brewin et al., 2002). Caregivers responded to 10 yes/no items assessing symptoms or behaviors indicative of a trauma response. Example items included: “Upsetting thoughts or memories about the event that have come into your mind against your will”, “Feeling upset by reminders of the event”, and “Heightened awareness of potential dangers to yourself or others.” Internal consistency in the current sample was good (Cronbach's ɑ = 0.88).
2.3. Analytic plan
We analyzed data with SPSS Version 21.0 and Mplus version 8. When comparing female and male caregivers on the outcomes of interest, normally-distributed data were evaluated using t-tests, while non-normally distributed data were evaluated using the nonparametric Mann-Whitney U test in SPSS. To examine the relation between COVID-19 stress/disruption, ACEs, and their interaction in relation to caregiver mental health, multiple linear regression models were tested in Mplus, with main and interactive effects entered simultaneously into the model. In these models, COVID-19 stress/disruption and ACEs were mean-centered and their interaction was computed on these centered variables. A maximum likelihood estimator with robust standard errors (MLR) was used, which yields parameter estimates with standard errors and a chi-square that are robust to non-normality of data. Unstandardized (B) coefficients with 95% confidence intervals (CIs) are reported, along with a measure of effect size (β). A direct comparison of the regression parameters between female and male caregivers was made by testing the difference between them using a z-test in Mplus.
3. Results
Bivariate correlations and descriptive statistics (means, SDs, and variable ranges) across the entire sample are presented in Table 1 . Notable associations include the positive relation between COVID stress/disruption and ACEs, and the association between each of these variables with all four mental health outcomes. Moreover, all four mental health outcomes were correlated to different degrees, with the strongest association between distress and anxiety, and the weakest association between substance use and anxiety.
Table 1.
Bivariate correlations and descriptive statistics for study variables for the entire sample.
| 1. | 2. | 3. | 4. | 5. | M | SD | Range | |
|---|---|---|---|---|---|---|---|---|
| 1. COVID stress/disruption | – | 38.87 | 7.70 | 25–67 | ||||
| 2. ACEs | .35∗∗∗ | – | 2.72 | 3.13 | 0–14 | |||
| 3. Distress | .50∗∗∗ | .35∗∗∗ | – | 19.14 | 7.83 | 10–46 | ||
| 4. Anxiety | .43∗∗∗ | .29∗∗∗ | .82∗∗∗ | – | 7.42 | 3.66 | 4–20 | |
| 5. Substance use | .20∗∗∗ | .18∗∗∗ | .18∗∗∗ | .13∗∗ | 2.06 | 3.38 | 0–20 | |
| 6. PTSS | .47∗∗∗ | .36∗∗∗ | .61∗∗∗ | .66∗∗∗ | .18∗∗ | 2.58 | 2.92 | 0–10 |
∗∗∗p < .001. ∗∗p < .01. ∗p < .05.
PTSS – Posttraumatic stress symptoms.
There were significant overall differences between female and male caregivers on COVID-19 stress/disruption. Female caregivers (M = 39.85, SD = 7.53) reported higher COVID stress/disruption compared to male caregivers (M = 36.49, SD = 7.49), t (489) = 4.50, p < .001. Female caregivers (median = 2.00) also reported higher ACEs compared to male caregivers (median = 1.00), U = 28,232, p = .017.
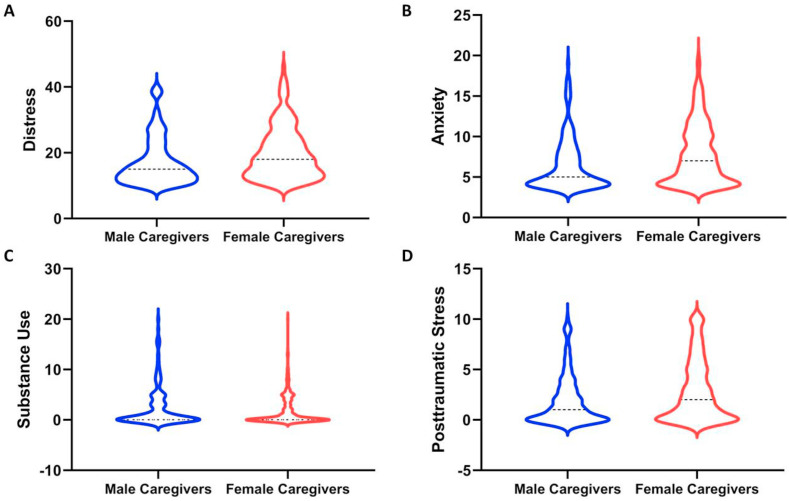
There were also significant differences between female and male caregivers with respect to the extent of mental health difficulties they reported. These differences are illustrated in Fig. 1 . On average, female caregivers reported more distress, U = 30,558, p < .001, anxiety, U = 29,858, p < .001, and posttraumatic stress, U = 29,244, p = .002 compared to male caregivers. While there was a trend for greater substance use among male caregivers, this difference was not significant, U = 22,879, p = .12. Thus, on average, female caregivers demonstrate more distress-related mental health difficulties compared to male caregivers during the current pandemic.
Fig. 1.
Mental health differences between female (red) and male (blue) caregivers on distress (A), anxiety (B), substance use (C), and posttraumatic stress (D). Plots are violin plots with the dashed line representing the median value for female and male caregivers on each outcome. Significantly elevated levels of distress, anxiety, and posttraumatic stress were observed for female compared to male caregivers, as reported in the main text. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Table 2 presents results from the multiple-group regression analysis with COVID stress/disruption, ACEs, and their interaction predicting each of the four mental health outcomes (distress, anxiety, substance use, and posttraumatic stress), as well as a direct comparison of differences in these parameters between female and male caregivers. For female caregivers, higher COVID stress/disruption and more ACEs were independently associated with higher distress, anxiety, substance use, and posttraumatic stress. An examination of effect sizes suggested that the effects of COVID stress/disruption was greater than the effect of ACEs for female caregivers’ distress, anxiety, and posttraumatic stress, whereas the effect of ACEs was greater than COVID stress/disruption for substance use. There was no significant interaction between COVID stress/disruption and ACEs for any mental health outcome. Thus, for female caregivers, the impact of COVID stress/disruption and ACEs on mental health is additive.
Table 2.
Regression models with COVID stress/disruption, ACEs, and their interaction predicting caregiver mental health outcomes.
| Distress |
Anxiety |
Substance use |
PTSS |
|||||
|---|---|---|---|---|---|---|---|---|
| Female Caregivers | Male Caregivers | Female Caregivers | Male Caregivers | Female Caregivers | Male Caregivers | Female Caregivers | Male Caregivers | |
| COVID Stress | ||||||||
| B 95% CI β |
.49∗∗∗ [.37,.60] .46 |
.28∗∗ [.12,.45] .29 |
.20∗∗∗ [.15,.26] .40 |
.10∗ [.02,.17] .22 |
.06∗ [.01,.10] .14 |
.12∗∗ [.03,.20] .21 |
.16∗∗∗ [.11,.20] .38 |
.11∗∗∗ [.05,.16] .33 |
| Difference |
p = .046 |
p = .032 |
p = .24 |
p = .20 |
||||
| ACEs | ||||||||
| B 95% CI β |
.50∗∗∗ [.25,.76] .20 |
.45∗ [.03,.88] .18 |
.20∗∗ [.08,.32] .17 |
.11 [-.07,.29] .10 |
.18∗∗ [.06,.30] .19 |
.14 [-.05,.32] .09 |
.23∗∗∗ [.13,.32] .24 |
.13∗ [.02,.24] .15 |
| Difference |
p = .85 |
p = .41 |
p = .74 |
p = .19 |
||||
| COVID∗ACEs | ||||||||
| B 95% CI β |
.00 [-.02,.03] .01 |
.03 [-.03,.09] .09 |
.00 [-.01,.02] .02 |
.02† [.00,.05] .18 |
.00 [-.01,.01] .02 |
.05∗∗∗ [.03,.07] .27 |
.00 [-.01,.01] .02 |
.02† [.00,.03] .15 |
| Difference | p = .43 | p = .16 | p < .001 | p = .19 | ||||
∗∗∗p < .001. ∗∗p < .01. ∗p < .05. †p < .10.
PTSS – Posttraumatic stress symptoms.
Note. The main effects and interaction were computed using the continuous (centered) COVID stress/disruption and ACEs scores.
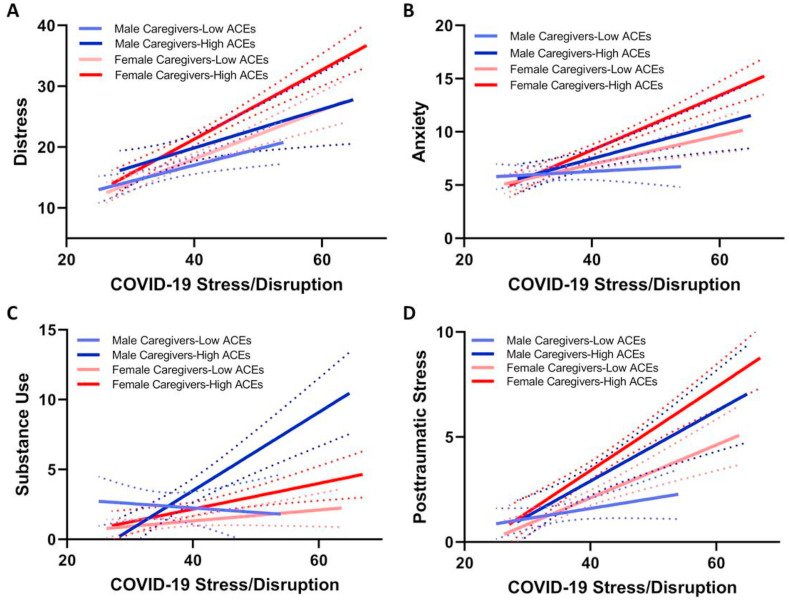
For male caregivers, results varied by mental health outcome. For distress, the pattern was similar as that seen for female caregivers, with higher COVID stress/disruption and more ACEs independently predicting higher distress, with no interaction. For anxiety and substance use, there was a main effect of COVID stress/disruption but not ACEs; and for posttraumatic stress, both COVID stress/disruption and ACEs were positive predictors. Similar to female caregivers, the effect of COVID stress/disruption was generally larger than that for ACEs across mental health outcomes. Unlike female caregivers, however, there was a significant interaction between COVID stress/disruption and ACEs in predicting male caregivers’ substance use, and marginal interactions for anxiety and posttraumatic stress. The pattern of these associations can be seen in Fig. 2 . As depicted, for male caregivers with low ACEs, COVID stress/disruption exerted a relatively small effect on mental health. In contrast, for male caregivers with higher ACEs, COVID stress/disruption was more strongly associated with substance use, anxiety, and posttraumatic stress. Thus, for male caregivers, the effects of COVID stress/disruption and ACEs are at least partially multiplicative, with the effect of COVID stress/disruption being contingent on the level of early adversity they experienced.
Fig. 2.
Associations between recent COVID stress/disruption and parental mental health as a function of caregivers' history of adverse childhood experiences (ACEs) for distress (A), anxiety (B), substance use (C), and posttraumatic stress (D). Dotted lines are the 95% confidence bands around each association. Light-colored lines show associations between COVID stress/disruption and mental health for those with low levels of ACEs, while dark-colored lines show associations between COVID stress/disruption and mental health for those with high levels of ACEs. High versus low ACEs were categorized based on a median split for these plots (low = 0 or 1; high = 2+). In the main text, the interactions were conducted on the continuous ACEs and COVID stress/disruption variables. As detailed in Table 2, this figure shows a largely additive contribution of ACEs and COVID stress/disruption for female caregivers, and a multiplicative relation for male caregivers (shown by the interaction).
4. Discussion
The current study examined the effects of stress and disruption due to the COVID-19 pandemic on the mental health of female and male caregivers, and how this interfaced with caregivers' history of adversity (ACEs). Three primary results emerged from this study. First, consistent with study hypotheses and prior research, female caregivers are, on average, considerably more burdened than male caregivers in terms of their experience of COVID stress and their self-reported history of childhood adversity. Second, and also consistent with study hypotheses, female caregivers report significantly more mental health problems than male caregivers in the domains of distress, anxiety, and posttraumatic stress. Finally, there are differences between female and male caregivers in how COVID stress/disruption and ACEs together confer risk for psychopathology. For female caregivers, the pattern of effects was largely suggestive of stress accumulation, wherein COVID stress/disruption and ACEs exert independent and additive effects on mental health problems. Conversely, for male caregivers, the pattern was more multiplicative, wherein the effect of COVID stress/disruption on mental health—in particular substance use—was dependent on their ACEs, consistent with the notion of stress sensitization. This study provides evidence of disparities in mental health between female and male caregivers during the ongoing pandemic, and differences in the role that early adversity plays in shaping caregivers’ responsiveness to stress during this unprecedented time.
The overall pattern of higher COVID stress/disruption among female compared to male caregivers is consistent with recent work demonstrating a disproportionate impact of the COVID-19 pandemic on women versus men (Connor et al., 2020). For instance, in the United States, women have reported more stress-inducing events from the pandemic compared to men (Park et al., 2020). The added burden faced by women is manifold, and includes an inequitable loss of job security and income, overrepresentation in health care jobs for which risk of infection is heightened, and the increased likelihood of caring for a family member with long-term healthcare needs. In general, women are more likely than men to experience caregiver burden by caring for another adult (Adelman et al., 2014), a circumstance that may be worsened during a public health crisis. In addition to caring for other adults, women often shoulder more of the childcare load than men. Not only do mothers spend more time overall than fathers caring for their children, but they engage in more physical care, multitasking, solo care, routine and non-routine care, and take on more responsibility for their children (Craig, 2006; Craig and Mullen, 2011). Globally, women devote 2–10 times more time on unpaid care work (housework, care of persons, and community work) than men, a finding that cuts across income levels and geographic regions (Ferrant Pessando and Nowacka, 2014). These inequalities in unpaid care work may be intensified by COVID-19, as school and childcare closures have resulted in greater caregiving and educational responsibilities for parents (Graves, 2020; Power, 2020). Our results cohere with these findings by showing that female caregivers report significantly greater stress and disruption from the pandemic compared to male caregivers. The fact that caregivers experience more overall psychological distress than non-caregivers (Bird, 1997) suggests that women caring for children may represent a group that is particularly susceptible to stress and disruption emanating from the pandemic.
In addition to caregiver differences in the experience of COVID stress and disruption, we also demonstrate a higher mental health burden among female compared to male caregivers. Female caregivers in our study reported more distress, anxiety, and posttraumatic stress than male caregivers. Multiple reports from Spain (González-Sanguino et al., 2020), China (Liu et al., 2020), Italy (Mazza et al., 2020), Iran (Moghanibashi-Mansourieh, 2020), Turkey (Özdin and Bayrak Özdin, 2020), and Denmark (Sønderskov et al., 2020) have reported elevated levels of mental health difficulties among women compared to men during COVID-19. Nationally-representative surveys in the United Kingdom have shown that females are more likely to report psychological distress or meet the threshold for a psychiatric disorder during the pandemic compared to men (Daly et al., 2020; Li and Wang, 2020), and that individuals caring for children report more mental health problems than those without children (Pierce et al., 2020b). Our results dovetail with these previous findings by showing that female caregivers appear to be disproportionately burdened by mental health difficulties during the ongoing pandemic relative to male caregivers.
Finally, building on prior large-scale mental health surveys, the current results show that the relation between COVID stress/disruption and mental health difficulties follows a somewhat different pattern for female and male caregivers. In particular, for females, the pattern was consistent with the notion of stress accumulation, which postulates that the deleterious effects of stressful events combine linearly across the life course (Evans et al., 2013). This model is consistent with the concept of allostatic load, wherein persistent activation of stress systems results in cumulative wear and tear on the body and deterioration of physical and mental health (Danese and McEwan, 2012). With respect to sex and gender differences, recent systematic reviews suggest that the association between allostatic load and mental health difficulties may be greater in women compared to men, even though men may have higher allostatic load on average (Kerr et al., 2020). Thus, elevated levels of mental health problems among female caregivers during the pandemic may reflect a progressive aggregation of stressful events that erodes mental wellbeing via a mechanism of increased allostatic load. Moreover, the relation between recent COVID stress/disruption and distress and anxiety was stronger for female compared to male caregivers, consistent with large epidemiological surveys showing that women report more stressful events, and that the link between stressful events and mental health problems is greater for women compared to men (Armstrong et al., 2018). Sex and gender differences in stress experience and responsiveness may be exacerbated by the current pandemic as a function of greater social isolation, resource insecurity, and caregiving burden, as well as elevated risk of intimate partner violence that is disproportionately experienced by women (Connor et al., 2020).
In contrast to female caregivers, the pattern of association between COVID stress/disruption and mental health difficulties in male caregivers followed that of stress sensitization, albeit not consistently across outcomes. Here, male caregivers with relatively higher levels of childhood adversity (ACEs) demonstrated a greater increase in mental health problems as the level of COVID stress/disruption increased, whereas those with lower ACEs were less responsive to the effects of COVID stress/disruption. This effect was most prominent for substance use problems, and was only marginally significant for anxiety and posttraumatic stress and not significant for psychological distress. This suggests a greater vulnerability for stress-related substance use during the COVID-19 pandemic among male caregivers who experienced early adversity. This may be due to lower distress tolerance, more positive expectancies about substance use, or greater avoidant coping in men compared to women (Nolen-Hoeksema, 2004), perhaps especially for individuals with a history of early adversity. Indeed, male caregivers reported fewer mental health difficulties in all other domains compared to female caregivers, suggesting that male caregivers may use substances to cope with other emotional difficulties that have arisen during the pandemic (Wardell, 2020). Previous studies examining gender differences in stress sensitization have reported mixed findings. For example, McLaughlin et al. (2010) found that fewer recent stressors were required to trigger stress sensitization effects for posttraumatic stress among women compared to men, whereas fewer recent stressors were required to trigger depression in men compared to women. Other studies have demonstrated greater sensitization to depression in women compared to men (Colman et al., 2013). For substance use—the outcome for which stress sensitization was most strongly observed among male caregivers in the current study—some previous studies have shown greater sensitization for women (Myers et al., 2014; Young-Wolff et al., 2012). In contrast, recent large-scale epidemiological surveys do not show gender differences in stress sensitization when examining general risk of psychopathology (Albott et al., 2018). It is plausible that these effects depend on the nature of early adversity, the recent stressors experienced, and unique sample characteristics. Notwithstanding the need for replication in diverse samples, our results are consistent with the notion that male caregivers who have experienced high levels of ACEs may reflect another group that is particularly vulnerable to poor mental health outcomes during the pandemic.
From a family systems perspective, the negative impact of COVID stress and disruption on caregiver mental health may spill over into many other aspects of family life, ultimately compromising the wellbeing of children and relationships across the family unit. Female caregivers may experience more stress than male caregivers in part due to their greater involvement in childcare during the pandemic; and this added caregiving stress likely has a recursive impact on children. The mechanisms that account for this transmission of risk have yet to be explored in the context of COVID-19, but theoretical models posit that changes in caregiver-child interactions, marital functioning, and sibling relationships are likely mediators of these effects (Prime et al., 2020). Also unknown is how sources of resilience within families can safeguard against poor outcomes for caregivers and children. While some families will be more susceptible to the impact of stress and disruption due to any number of pre-existing and/or recent vulnerabilities, others may emerge with greater cohesion and wellbeing. The factors that foster this type of resilience within families have yet to be explored during the COVID-19 pandemic, but may include the capacity for relationship-building, meaning-making, adaptive coping, and predictable home environments (e.g., Glynn et al., 2021). Additional research is urgently needed to better understand these complex pathways to caregiver, child, and family resilience during the ongoing pandemic.
The current results should be considered in light of several limitations. First, caregiver mental health was based solely on their own self-reports, and caregivers also reported on their own history of adversity and current COVID stress/disruption. This raises the possibility of shared method bias that could inflate some of the associations reported herein. Future studies that include observation or direct assessment (e.g., clinical interviews) would help to determine the robustness of these effects. Second, these findings are cross-sectional; thus, we cannot ascertain the directionality of the relation between COVID stress/disruption and mental health. Indeed, it may be that there is a bi-directional effect in which increases in mental health problems also contribute to more stress and disruption during the pandemic. We are collecting additional waves of data over the coming months and will be able to examine fluctuations in caregiver mental health over a longer duration to examine how this is related to changes in COVID stress/disruption. Third, although we were able to recruit a relatively large sample of female and male caregivers, the number of male caregivers recruited was still less than half the number of female caregivers. There is a long-recognized challenge in detecting statistical interactions using continuous variables in multiple regression analyses (Shieh, 2009). Thus, the current study may have been somewhat underpowered to detect subgroup differences in the relation between COVID stress/disruption and caregiver mental health. Moreover, the larger sample of female caregivers may have skewed the results towards larger effects of ACEs and COVID stress/disruption on mental health for female relative to male caregivers. Future studies with larger and more equal samples of female and male caregivers are encouraged based on this initial report. Additionally, we cannot rule out the possibility that differences in the level of COVID stress/disruption and mental health between female and male caregivers reflect a reporting bias between groups. For instance, there is some evidence that men may under-report mental health symptoms under certain conditions (Berger et al., 2012; Sigmon et al., 2005), though these reporting biases do not entirely account for the gender gap in mental health difficulties such as depression (Hyde and Mezulis, 2020). Nonetheless, the mental health differences between female and male caregivers documented in the current study may be somewhat inflated based on these reporting biases. Furthermore, the current study also did not assess gender as a social construct (including the option for gender-diverse identities) and was limited to the assessment of caregiver-reported sex. As sex and gender do not perfectly correlate, a more thorough assessment of sex and gender—and their interaction with the social role of caregiving—is warranted. Finally, this sample was relatively homogeneous in terms of ethnicity, race, and the sociodemographic background of participants. This limits generalizability of the current findings and means that we may not have adequately captured risk of mental health difficulties among some populations that have been disproportionately impacted by the pandemic. Future studies with more diverse samples are strongly encouraged.
5. Conclusions
The current study highlights the disparate effect of the ongoing COVID-19 pandemic on the mental health of female and male caregivers. In comparison to male caregivers, female caregivers are significantly more burdened in terms of their experience of COVID stress and disruption and their mental health. Among male caregivers, those with a history of childhood adversity also appear to be experiencing more mental health difficulties as a function of increased COVID stress and disruption, especially substance use problems. These results support initiatives to increase the availability, accessibility, and use of telepsychology services to meet the mental health needs of caregivers during and after the pandemic. Indeed, the use of such services has increased dramatically during the pandemic, especially among women and to address issues specific to women (Pierce et al., 2020a). Online recovery support for substance use difficulties has also increased significantly during the pandemic and may help to address this growing concern (Bergman et al., 2021). For caregivers specifically, group-based telepsychology services to address behavioral concerns of children have been shown to have high fidelity in the context of COVID-19, including for high-risk families who may be experiencing considerable disruption (Fogler et al., 2020; James Reigler et al., 2020). Such supports are likely to prove critical not only in the short term, but as psychological services transform in the aftermath of COVID-19 to include telepsychology as a standard delivery format to manage ongoing stress and promote recovery from the disruption brought about by COVID-19.
Funding
The Canada Research Chair program (950-232347) provided unconditional funds to the senior author which were used to develop this study. The funder had no role in the design, collection of data, analyses, or decision to publish the study.
Credit author statement
Mark Wade: Analysis, Writing, and Revisions; Heather Prime: Reviewing and Editing; Dylan Johnson: Reviewing and Editing; Shealyn S. May: Data Collection and Management, Reviewing; Jennifer M. Jenkins: Reviewing and Editing; Dillon T. Browne: Conceptualization, Methodology, Data Collection, Reviewing and Editing.
Declaration of competing interest
The authors have no financial interests or conflicts to disclose.
Acknowledgements
We would like to thank the participants who contributed to this study for their time and dedication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.113801.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adelman R.D., Tmanova L.L., Delgado D., Dion S., Lachs M.S. Caregiver burden: a clinical review. JAMA - J. Am. Med. Assoc. 2014;311:1052–1059. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- Albott C.S., Forbes M.K., Anker J.J. Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Netw. Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.5354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong J.L., Ronzitti S., Hoff R.A., Potenza M.N. Gender moderates the relationship between stressful life events and psychopathology: findings from a national study. J. Psychiatr. Res. 2018;107:34–41. doi: 10.1016/j.jpsychires.2018.09.012. [DOI] [PubMed] [Google Scholar]
- Ayers S., Bond R., Webb R., Miller P., Bateson K. Perinatal mental health and risk of child maltreatment: a systematic review and meta-analysis. Child Abuse Neglect. 2019;98:104172. doi: 10.1016/j.chiabu.2019.104172. [DOI] [PubMed] [Google Scholar]
- Bale T.L., Epperson C.N. Sex differences and stress across the lifespan. Nat. Neurosci. 2015;18(10):1413–1420. doi: 10.1038/nn.4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangasser D.A., Valentino R.J. Sex differences in stress-related psychiatric disorders: neurobiological perspectives. Front. Neuroendocrinol. 2014;35(3):303–319. doi: 10.1016/j.yfrne.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis M.A., Lowey H., Leckenby N., Hughes K., Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J. Publ. Health. 2014;36(1):81–91. doi: 10.1093/pubmed/fdt038. [DOI] [PubMed] [Google Scholar]
- Berger J.L., Addis M.E., Reilly E.D., Syzdek M.R., Green J.D. Effects of gender, diagnostic labels, and causal theories on willingness to report symptoms of depression. J. Soc. Clin. Psychol. 2012;31(5):439–457. [Google Scholar]
- Bergman B.G., Kelly J.F., Fava M., Evins A.E. Online recovery support meetings can help mitigate the public health consequences of COVID-19 for individuals with substance use disorder. Addict. Behav. 2020;113:106661. doi: 10.1016/j.addbeh.2020.106661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird C.E. Gender differences in the social and economic burdens of parenting and psychological distress. J. Marriage Fam. 1997;59(4):809. doi: 10.2307/353784. [DOI] [Google Scholar]
- Brewin C.R., Rose S., Andrews B., Green J., Tata P., McEvedy C., et al. Brief screening instrument for post-traumatic stress disorder. Br. J. Psychiatry. 2002;181(AUG):158–162. doi: 10.1017/s0007125000161896. [DOI] [PubMed] [Google Scholar]
- Brown S.M., Doom J.R., Lechuga-Peña S., Watamura S.E., Koppels T. 2020. Stress and Parenting during the Global COVID-19 Pandemic. Child Abuse and Neglect. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabrera N.J., Volling B.L., Barr R. Fathers are parents, too! Widening the lens on parenting for children's development. Child Dev. Perspect. 2018;12(3):152–157. doi: 10.1111/cdep.12275. [DOI] [Google Scholar]
- Colman I., Garad Y., Zeng Y., Naicker K., Weeks M., Patten S.B., et al. Stress and development of depression and heavy drinking in adulthood: moderating effects of childhood trauma. Soc. Psychiatr. Psychiatr. Epidemiol. 2013;48(2):265–274. doi: 10.1007/s00127-012-0531-8. [DOI] [PubMed] [Google Scholar]
- Conger R.D., Conger K.J., Martin M.J. Socioeconomic status, family processes, and individual development. J. Marriage Fam. 2010;72(3):685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J., Madhavan S., Mokashi M., Amanuel H., Johnson N.R., Pace L.E., Bartz D. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc. Sci. Med. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig L. Does father care mean fathers share? Gend. Soc. 2006;20(2):259–281. doi: 10.1177/0891243205285212. [DOI] [Google Scholar]
- Craig L., Mullan K. How mothers and fathers share childcare. Am. Socio. Rev. 2011;76(6):834–861. doi: 10.1177/0003122411427673. [DOI] [Google Scholar]
- Daly M., Sutin A., Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK household longitudinal study. Psychol. Med. 2020;1–10 doi: 10.31234/OSF.IO/QD5Z7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A., McEwen B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Evans G.W., Li D., Whipple S.S. Cumulative risk and child development. Psychol. Bull. 2013;139(6):1342. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Ferrant G., Pesando M., Nowacka K. 2014. Unpaid Care Work: the Missing Link in the Analysis of Gender Gaps in Labour Outcomes. [Google Scholar]
- Finkelhor D., Shattuck A., Turner H., Hamby S. A revised inventory of adverse childhood experiences. Child Abuse Neglect. 2015;48:13–21. doi: 10.1016/j.chiabu.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Fogler J.M., Normand S., O'Dea N., Mautone J.A., Featherston M., Power T.J., Nissley-Tsiopinis J. Implementing group parent training in telepsychology: lessons learned during the COVID-19 pandemic. J. Pediatr. Psychol. 2020;45(9):983–989. doi: 10.1093/jpepsy/jsaa085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S.D., Roma P., Verrocchio M.C. The effect of the COVID-19 lockdown on parents: a call to adopt urgent measures. Psychol. Trauma: Theor. Res. Pract. Pol. 2020;12(S1):S79. doi: 10.1037/tra0000672. [DOI] [PubMed] [Google Scholar]
- Gausman J., Langer A. Sex and gender disparities in the COVID-19 pandemic. J. Wom. Health. 2020;29(4):465–466. doi: 10.1089/jwh.2020.8472. [DOI] [PubMed] [Google Scholar]
- Glynn L.M., Davis E.P., Luby J.L., Baram T.Z., Sandman C.A. A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiol. Stress. 2021:100291. doi: 10.1016/j.ynstr.2020.100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graves L. 2020. Women's Domestic Burden Just Got Heavier with the Coronavirus. Retrieved November 4, 2020, from the Guardian Website.https://www.theguardian.com/us-news/2020/mar/16/womens-coronavirus-domestic-burden [Google Scholar]
- Guo J., Fu M., Liu D., Zhang B., Wang X., van IJzendoorn M.H. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse and Neglect. 2020;110:104667. doi: 10.1016/j.chiabu.2020.104667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck A.L., Handa R.J. Sex differences in the hypothalamic–pituitary–adrenal axis’ response to stress: an important role for gonadal hormones. Neuropsychopharmacology. 2019;44(1):45–58. doi: 10.1038/s41386-018-0167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar C.E., Lachman M.E., Mroczek D.K., Seeman T.E., Miller G.E. Additive contributions of childhood adversity and recent stressors to inflammation at midlife: findings from the MIDUS study. Dev. Psychol. 2015;51(11):1630–1644. doi: 10.1037/dev0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C., et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lanc. Publ. Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Hyde J.S., Mezulis A.H. Gender differences in depression: biological, affective, cognitive, and sociocultural factors. Harv. Rev. Psychiatr. 2020;28(1):4–13. doi: 10.1097/HRP.0000000000000230. [DOI] [PubMed] [Google Scholar]
- James Riegler L., Raj S.P., Moscato E.L., Narad M.E., Kincaid A., Wade S.L. Pilot trial of a telepsychotherapy parenting skills intervention for veteran families: implications for managing parenting stress during COVID-19. J. Psychother. Integrat. 2020;30(2):290. [Google Scholar]
- Kerr P., Kheloui S., Rossi M., Désilets M., Juster R.P. Allostatic load and women's brain health: a systematic review. Front. Neuroendocrinol. 2020;59 doi: 10.1016/j.yfrne.2020.100858. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L.T., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., McLaughlin K.A., Green J.G., Gruber M.J., Sampson N.A., Zaslavsky A.M., et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br. J. Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Eaton N.R., Krueger R.F., McLaughlin K.A., Wall M.M., Grant B.F., Hasin D.S. Childhood maltreatment and the structure of common psychiatric disorders. Br. J. Psychiatry. 2012;200(2):107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson M., Piel M.H., Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020:104709. doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijdesdorff S., Van Doesum K., Popma A., Klaassen R., Van Amelsvoort T. Prevalence of psychopathology in children of parents with mental illness and/or addiction: an up to date narrative review. Curr. Opin. Psychiatr. 2017;30:312–317. doi: 10.1097/YCO.0000000000000341. [DOI] [PubMed] [Google Scholar]
- Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatr. Res. 2020;291:113267. doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatr. Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masarik A.S., Conger R.D. Stress and child development: A review of the Family Stress Model. Curr. Opin. Psychol. 2017;13:85–90. doi: 10.1016/j.copsyc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the covid-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Publ. Health. 2020;17(9) doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Conron K.J., Koenen K.C., Gilman S.E. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol. Med. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J., Wu L.T., Subramaniam G., Sharma G., Cathers L.A., Svikis D., et al. Performance of the tobacco, alcohol, prescription medication, and other substance use (TAPS) tool for substance use screening in primary care patients. Ann. Intern. Med. 2016;165(10):690–699. doi: 10.7326/M16-0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick M.T., Ford D.C., Ports K.A., Guinn A.S. Prevalence of adverse childhood experiences from the 2011-2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038–1044. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 2020;51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B., McLaughlin K.A., Wang S., Blanco C., Stein D.J. Associations between childhood adversity, adult stressful life events, and past-year drug use disorders in the national epidemiological study of alcohol and related conditions (NESARC) Psychol. Addict. Behav. 2014;28(4):1117–1126. doi: 10.1037/a0037459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neece C., McIntyre L.L., Fenning R. Examining the impact of COVID‐19 in ethnically diverse families with young children with intellectual and developmental disabilities. J. Intellect. Disabil. Res. 2020;64(10):12769. doi: 10.1111/jir.12769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin. Psychol. Rev. 2004;24(8):981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Olff M., Langeland W., Draijer N., Gersons B.P.R. Gender differences in posttraumatic stress disorder. Psychol. Bull. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Özdin S., Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatr. 2020;66(5):504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent J., Forehand R., Pomerantz H., Peisch V., Seehuus M. Father participation in child psychopathology research. J. Abnorm. Child Psychol. 2017;45(7):1259–1270. doi: 10.1007/s10802-016-0254-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J. Gen. Intern. Med. 2020;35(8):2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2020-0836. [DOI] [PubMed] [Google Scholar]
- Phares V., Fields S., Kamboukos D., Lopez E. Still looking for poppa. Am. Psychol. 2005;60:735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- Pierce B.S., Perrin P.B., Tyler C.M., McKee G.B., Watson J.D. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in US mental health care delivery. Am. Psychol. Adv. Online Publ. 2020;76(1):14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- Pierce M., Hope H.F., Kolade A., Gellatly J., Osam C.S., Perchard R., et al. Effects of parental mental illness on children's physical health: systematic review and meta-analysis. Br. J. Psychiatry. 2020;217:354–363. doi: 10.1192/bjp.2019.216. [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sorensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006;61(1):P33–P45. doi: 10.1093/geronb/61.1.P33. [DOI] [PubMed] [Google Scholar]
- Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustain. Sci. Pract. Pol. 2020;16(1):67–73. doi: 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- PROMIS . 2016. PROMIS Item Bank v1.0 – Emotional Distress - Anxiety – Short Form 4a. Health Measures. Retrieved from.https://www.healthmeasures.net/explore-measurement-systems/promis/obtain-administer-measures [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B.S., Hutchison M., Tambling R., Tomkunas A.J., Horton A.L. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent–child relationship. Child Psychiatr. Hum. Dev. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113:229–235. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Lu Z., Que J., Huang X., Liu L., Ran M., et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shieh G. Detecting interaction effects in moderated multiple regression with continuous variables power and sample size considerations. Organ. Res. Methods. 2009;12(3):510–528. doi: 10.1177/1094428108320370. [DOI] [PubMed] [Google Scholar]
- Sigmon S.T., Pells J.J., Boulard N.E., Whitcomb-Smith S., Edenfield T.M., Hermann B.A., et al. Gender differences in self-reports of depression: the response bias hypothesis revisited. Sex. Roles. 2005;53(5–6):401–411. [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020;1 doi: 10.1017/neu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z., Marnane C., Iranpour C., Chey T., Jackson J.W., Patel V., Silove D. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int. J. Epidemiol. 2014;43(2):476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Centre for Addiction and Mental Health . 2020. COVID-19 National Survey Dashboard. Retrieved November 4, 2020, from the Centre for Addiction and Mental Health Website.https://www.camh.ca/en/health-info/mental-health-and-covid-19/covid-19-national-survey [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Kempe T., Rapinda K.K., Single A., Bilevicius E., Frohlich J.R., et al. Drinking to cope during COVID‐19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin. Exp. Res. 2020;44(10):2073–2083. doi: 10.1111/acer.14425. [DOI] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young-Wolff K.C., Kendler K.S., Prescott C.A. Interactive effects of childhood maltreatment and recent stressful life events on alcohol consumption in adulthood. J. Stud. Alcohol Drugs. 2012;73(4):559–569. doi: 10.15288/jsad.2012.73.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.