Abstract
Rationale
Understanding how health has changed in response to the COVID-19 pandemic is critical to recovering from the pandemic.
Objective
This study focused on how sleep characteristics in the United States may be different from before to during the COVID-19 pandemic.
Methods
To this end, the sleep characteristics of a nationally representative sample of U.S. adults collected before the COVID-19 outbreak (i.e., 2018 National Health Interview Survey, n = 19,433) were compared to the sleep characteristics of a nationally representative sample of U.S. adults recruited via Luc.id, an online survey sampling company, during the COVID-19 outbreak (i.e., 2020 Luc.id, n = 2059).
Results
While average sleep duration did not change between 2018 and 2020, the prevalence of both shorter and longer than recommended sleep duration were greater in 2020. Moreover, the number of days with difficulty falling asleep, difficulty staying asleep, and not feeling rested was greater in 2020 than 2018. Adults younger than 60 had larger differences than those 60 or older.
Conclusions
Sleep health in U.S. adults was worse in 2020 than in 2018, particularly in adults younger than 60. Findings highlight sleep as target in future research and interventions seeking to understand and reduce the effects of the COVID-19 pandemic.
Keywords: COVID-19, Coronavirus, Sleep health, National health interview survey, United States, Sleep duration, Sleep difficulties, Sleep problems
1. Introduction
The typical operations of everyday life have been substantially altered since the emergence and spread of COVID-19 in the U.S. In March 2020, U.S. government officials began to issue stay-at-home orders to prevent the spread of the virus. Accompanying these orders were major changes and restrictions in education, business operations, recreation, and socialization (Cheng et al., 2020; Haffajee and Mello, 2020). Educational, business, and recreation establishments across the country closed, began work/learn-from-home practices, or substantially restricted work hours and how many people could be in their physical space at once (Abouk and Heydari, 2020; Baldwin and Weder di Mauro, 2020; Bartik et al., 2020). These changes, along with the uncertainty and stress surrounding the virus, have posed massive challenges to the U.S. population. Understanding how the physical and mental health of the U.S. has changed in response to the spread of COVID-19 is crucial to reducing and recovering from the pandemic.
Sleep is one such factor likely to have changed due to the spread of COVID-19. Understanding how sleep has changed during this time is important because sleep plays a critical role in maintaining and promoting both mental and physical health (Buysse, 2014; Gallicchio and Kalesan, 2009; Goldstein and Walker, 2014). Notably, it plays a central role in the functioning of the immune system; healthy sleep is critical to prevent and recover from illnesses (Lange et al., 2010; Prather et al., 2015). Unfortunately, as outlined by Altena and colleagues, changes in work and home life, increased stress, and home confinement during the spread of COVID-19 are likely to impair sleep (Altena et al., 2020). In support of these assertions, recent findings show unusually high proportions of people reporting sleep disturbances or poor sleep quality in Italian, Chinese, Belgian, French, and Greek populations (Cellini et al., 2020, Cellini et al., 2021; Huang and Zhao, 2020; Xiao et al., 2020; Voitsidis et al., 2020; Casagrande et al., 2020; Beck et al., 2021). However, a recent study in U.S. adults identified that not everyone experienced worse sleep as a composite measure of sleep was not impacted in this sample, and even showed a trend toward improvement (Gao and Scullin, 2020). Indeed, only approximately 25% of the sample experienced a decline in sleep health. This evidence corroborates with other findings that some people, particularly younger populations who have biologically driven later sleep-wake schedules, tended to have increased sleep duration during the COVID-19 pandemic, likely as a result of relaxed school/work schedules after quarantine and work-from-home orders were instituted (Leone et al., 2020; Sinha et al., 2020; Roenneberg et al., 2003). Evidence from Belgian and Italian samples suggest that students and remote workers experience in.
Altogether this evidence suggests that the COVID-19 pandemic has not ubiquitously deteriorated all sleep characteristics for all populations. To better understand the effects of the COVID-19 pandemic on sleep, it is necessary to examine how sleep characteristics in different populations are being affected. While prior evidence implicates younger populations may experience less detriments or even improvements in sleep during the pandemic, it is unknown whether the sleep of particular racial groups may be differentially affected. Minority racial groups routinely face discrimination and social, healthcare, and many other disadvantages, and these experiences may exacerbate the negative effects of the COVID-19 pandemic on sleep (Hardeman and Medina, 2019; Howard and Navarro, 2016; Slopen et al., 2016). Identifying whether particular age or racial groups are more or less affected by the pandemic can help provide evidence for targeted future research and intervention.
In addition to considering how different populations may have been affected by the pandemic, the above evidence also suggests that it is necessary to examine how different sleep characteristics may have been impacted. For instance, while general theorizing focuses on negative consequences of the pandemic, particular sleep characteristics, such as sleep duration may have actually improved (Altena et al., 2020). Sleep duration may have increased because quarantine and work-from-home orders may relax rigid early morning work/school start times that can conflict with a person's natural sleep schedule and curtail sleep duration. The relaxation of work/school times during the pandemic may allow for a greater sleep opportunity and allow for people to obtain a longer, more sufficient sleep duration, particularly in younger populations who have later sleep schedules which frequently conflict with early work/school schedules. In contrast to sleep duration, stressors and negative affect associated with the pandemic may have impaired other sleep characteristics, such as sleep onset latency or awakenings during the night. Because the pandemic may have differentially affected sleep characteristics, prior studies utilizing composite indices of sleep health or sleep quality may provide limited or obscured insight into how sleep is being affected, thus research is needed that looks at the effects of the pandemic on distinct sleep characteristics.
Finally, while findings from other countries likely extend to the U.S., it is unknown how sleep in the U.S. has been affected. To better understand how sleep may have changed in the U.S. during the COVID-19 pandemic, this study uses similar methods as Casagrande and colleagues who compared the sleep characteristics of a large sample of Italian adults during quarantine to the sleep characteristics of normative samples of the general Italian population before quarantine (Casagrande et al., 2020). Similarly, the current study compared the sleep characteristics of a large sample of U.S. adults in 2020 to the sleep characteristics of a large nationally representative sample U.S. adults taken in 2018 (the National Health Interview Survey). Importantly, the current study improves upon the methodology used in Casagrande et al. (2020) by a.) using a normative comparison sample that is much closer in time to provide a clearer understanding of how sleep changed from before to during the pandemic, and by b.) recruiting a sample that is matched with the normative comparison samples on socio-demographic variables, thereby ruling out many socio-demographic factors as confounds.
Using this methodology, this study examined if different sleep characteristics (i.e., sleep duration, difficulties falling asleep, difficulties staying asleep, and feelings of restedness) may have changed during the pandemic. The large and diverse size of each sample further allow for a highly powered examination of what age and racial groups may or may not be particularly experiencing impairments in sleep since the onset of the COVID-19 pandemic.
2. Methods
2.1. Participants
The 2018 National Health Interview Survey (NHIS) was conducted to track the health of the general U.S. population. The 2018 survey is a publicly available data set (available here) and was selected because it was the most recent NHIS survey administered before the global spread of COVID-19 (which began in 2019). The NHIS uses a multistage area probability design to draw a representative sample of noninstitutionalized U.S. citizens each month over a year. Data from a total of 25,417 participants were collected through a personal household interview conducted by trained U.S. Census Bureau employees. NHIS is approved by the Research Ethics Review Board of the National Center for Health Statistics and the U.S. Office of Management and Budget. All NHIS respondents provided oral consent before participation. The annual response rate for the survey in the mid-2010s was approximately 70%, though response rates appear to have declined over time (Czajka and Beyler, 2016). Because all data from the 2020 U.S. sample was collected via an online survey (see below), only participants from the 2018 NHIS sample who reported that they use the internet (n = 19,433) were included to increase comparability between the samples.
The 2020 national sample of U.S. adults was recruited via Luc.id, an online survey panel that collects nationally representative samples for social science research using advance screening for gender, race, age, and region. This recruiting platform aims to recruit samples matched on census demographics, producing samples that are more comparable than MTurk on demographic and psychosocial characteristics to nationally representative surveys such as the American National Election Survey (Coppock and McClellan, 2019). Luc.id has previously been used for COVID-19 related research (Burszytyn et al., 2020). After reading the consent form for the study, 97.5% agreed to participate. Participants earned approximately $1 for completing the survey. The 2020 survey was reviewed by the San Diego State University Institutional Review Board and declared exempt, and informed consent was obtained from participants. All Luc.id 2020 data was collected on April 27, 2020 (n = 2060), which was approximately one month since many states issued stay-at-home orders and several months since the rise of COVID-19 as a global health concern. As a testament to the representativeness of this sample to the general U.S. adult population, the demographic characteristics of the 2020 Luc.id sample were extremely similar to the demographic characteristics of the 2018 NHIS sample (see Table 1 ).
Table 1.
Demographic characteristics of NHIS 2018 sample of internet users (n = 19,433) and Luc.id April 2020 online nationally representative sample (n = 2059).
| NHIS 2018 | Luc.id 2020 | |
|---|---|---|
| Age | 48.16 (17.22) | 48.16 (17.22) |
| Age group | ||
| 18-29 | 17.6% | 22.5% |
| 30-44 | 27.1% | 28.6% |
| 45-59 | 25.4% | 25.1% |
| 60+ | 30.0% | 23.8% |
| Gender: Percentage female | 54.6% | 51.1% |
| Education | ||
| Did not finish high school | 5.8% | 2.5% |
| High school or GED | 20.5% | 20.3% |
| Some college or 2-year degree | 32.7% | 28.9% |
| Bachelor's degree | 25.4% | 29.1% |
| Graduate or professional degree | 15.5% | 19.2% |
| Race | ||
| White | 81.4% | 73.6% |
| Black | 10.8% | 11.4% |
| Asian | 5.7% | 6.8% |
| Other | 1.8% | 8.2% |
| Hispanic | 11.1% | 12.0% |
| Region | ||
| Northeast | 17.2% | 20.4% |
| Midwest | 22.5% | 18.6% |
| South | 36.1% | 37.4% |
| West | 24.1% | 23.6% |
| Living with significant other: Percentage yes | 52.6% | 55.2% |
| Living with children under 18: Percentage yes | 27.0% | 35.7% |
2.2. Measures
Demographic characteristics. Both surveys collected demographic information on participants, including age, gender, education, race, Hispanic ethnicity, U.S. region, living with a significant other in the household, and the presence of children under age 18 in the household. See Table 1 for demographics of both samples.
Sleep. Participants reported the number of days in the past week they (1) had trouble falling asleep, (2) had trouble staying asleep, and (3) woke up feeling rested. The number of days participants reported feeling rested was reverse scored to reflect number of days not feeling rested. In addition, participants reported, on average, how many hours of sleep they get in a 24-h period. All sleep questions were worded the same way in both the 2018 NHIS and Luc.id 2020 samples. However, response options for sleep duration ranged in whole numbers from 1 to 24 h in the 2018 NHIS sample and ranged in whole numbers from 1 to 16+ hours in the Luc.id 2020 sample. Sleep duration responses were capped at 4 on the lower end of the scale and 12 at the higher end of the scale in both samples (75 observations in Luc.id 2020 and 138 observations in NHIS 2018) to reduce the influence of outliers and erroneous answers.
In addition to the above sleep variables, additional dichotomous clinically relevant sleep variables were created to evaluate if differences in mean levels of sleep characteristics between 2018 and 2020 may have clinical importance. Based upon the National Sleep Foundation's recommendation for adult sleep duration, the prevalence of shorter than recommended sleep duration was calculated by dichotomizing reported sleep duration into 7 h of sleep or more (0) and less than 7 h of sleep (1) (Hirshkowitz et al., 2015). Additionally, a variable representing the prevalence of longer than the National Sleep Foundation's recommended sleep duration (greater than 9 h for adults between 18 and 64 and greater than 8 h for adults 65+) was created wherein 1 represented exceeding the recommended sleep duration and 0 represented meeting the recommended sleep duration (Hirshkowitz et al., 2015). To examine whether the number of people experiencing any sleep disturbances differed between 2018 and 2020 and to facilitate interpretation of findings with prior work examining these sleep characteristics in the NHIS data (Hisler et al., 2019) the number of days over the past week than participants reported difficulty falling asleep, difficulty staying asleep, and not feeling rested were each dichotomized into variables reflecting zero days (0) and one or more days (1). Note that sleeping less than the recommended hours, experiencing difficulties falling asleep, staying asleep, and not feeling rested can suggest symptoms of sleep disorders, particularly insomnia. Thus, effects on these binary variables directly model increases in the number of people sleeping fewer hours than recommended and beginning to experience sleep difficulties, thereby providing a translation of the practical and clinical significance of observed effects on the continuous variables (Funder and Ozer, 2019; Rosenthal and Rubin, 1982).
2.3. Analytic strategy
Comparisons between the mean levels of each continuous sleep characteristic in 2018 vs. 2020 U.S. adult national samples were conducted via analysis of covariance (ANCOVA). In addition, the clinical significance of the differences between the samples was evaluated by predicting the prevalence of each clinically relevant sleep variables in a series of logistic regression. Finally, to explore whether particular sociodemographic factors may be associated with greater differences in sleep between 2018 and 2020, age (categorized into bins of age 18–29, 30–44, 45–59, and 60+) and race (categorized into White, Black, Asian, and Other racial groupings) were examined as moderators in ANCOVA and logistic regression analyses when estimating the difference in sleep characteristics between 2018 and 2020. The false-positive rate was set to 0.01 (i.e., α = 0.01) as opposed to .05 to provide increased protection from false positives associated with multiple hypothesis testing. Note that because the NHIS 2018 data was collected over the course of a year whereas the Luc.Id 2020 data was collected all in April, seasonal effects on sleep outcomes were controlled for by including a set of dummy coded variables indicating the month the assessment (using January as the reference category) in analyses.
2.4. Missing data
Missing data on any sleep variable was extraordinarily low in both the NHIS 2018 and Luc.id 2020 samples (182 cases out of 19,433 in NHIS 2018 & 21 cases out of 2060). To investigate whether missing data may bias results, we used the NHIS data to conduct binary regressions examining if demographic or individual sleep variables were related to probability of having missing data on any sleep variables (this was not examined in Luc.id 2020 because sample of missing data was so small, i.e., 21 cases). Only the variable of not living with significant other was associated with an increased likelihood of having missing data on any sleep variables (B = 0.71, p < .001). Thus, because 1.) missingness in either large sample is less than 0.9%, 2.) probability of missingness on these variables was largely unrelated to any other study variable, and 3.) the sample size in both datasets is large and losing cases will not demonstrably affect the power or precision of the study, pair-wise deletion was used in instances of missing data.
3. Results
3.1. Differences in sleep characteristics of U.S. adults between 2018 and 2020
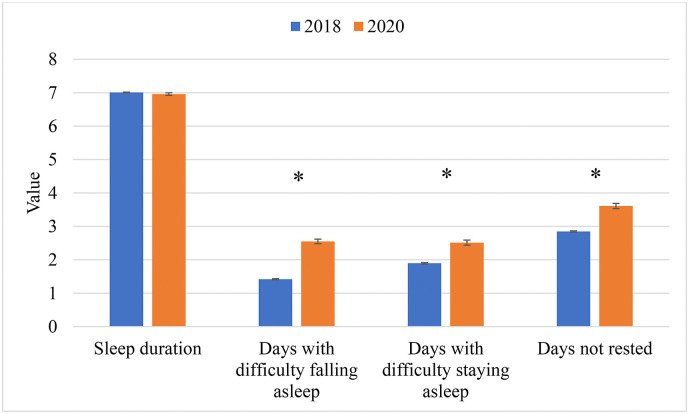
Results from ANCOVAS comparing sleep characteristics for U.S. adults in the NHIS 2018 and Luc.id 2020 samples are presented in Table 2 and results are depicted in Fig. 1 . There was a small, but not statistically significant difference in sleep duration between the 2018 and 2020 samples (M diff = −0.05, 99% CI = −0.17 to 0.09, d = −0.02, F (1, 21,415) = 1.17). In contrast, mean levels of number of days with difficulty falling asleep (M diff = 1.13, 99% CI = 0.93 to 1.32, d = 0.35, F (1, 21,416) = 230.92) difficulty staying asleep (M diff = 0.62, 99% CI = 0.39 to 0.84, d = 0.17, F (1, 21,414) = 52.18), and not feeling rested (M diff = 0.76, 99% CI = 0.54 to 0.98, d = 0.21, F (1, 21,377) = 80.03) were larger in 2020 than in 2018. Thus, in comparison to 2018, U.S. adults in 2020 reported approximately one more day a week with difficulty falling asleep, staying asleep, and not feeling rested.
Table 2.
Mean level comparisons of sleep characteristics in NHIS 2018 sample of internet users vs. Luc.id April 2020 online nationally representative sample.
| NHIS 2018 |
Luc.id 2020 |
||||
|---|---|---|---|---|---|
| M (SE) n | M (SE) n | Mdiff (99% CI) | d (99% CI) | F (df) | |
| Sleep duration | 7.01 (.01) 19,369 | 6.96 (.04) 2059 | −0.05 (−0.17 to 0.09) | −0.02 (−0.06 to 0.02) | 1.17 (1, 21,415) |
| Days with difficulties falling asleep | 1.42 (.02) 19,381 | 2.55 (.07) 2048 | 1.13 (0.93–1.32) | 0.35 (0.32–0.39) | 230.92 (1, 21,416) |
| Days with difficulties staying asleep | 1.90 (.02) 19,373 | 2.51 (.08) 2054 | 0.62 (0.39–0.84) | 0.17 (0.13–0.21) | 52.18 (1, 21,414) |
| Days feeling not rested | 2.85 (.02) 19,333 | 3.61 (.08) 2057 | 0.76 (0.55–0.93) | 0.21 (0.17–0.24) | 80.03 (1, 21,377) |
Note. Positive Mdiff values reflect increases in variable from 2018 to 2020. d = Cohen's d adjusted for uneven group sample sizes.
Fig. 1.
Sleep characteristics in 2018 vs. 2020. Error bars indicate standard error of the mean. * indicates statistically significant difference.
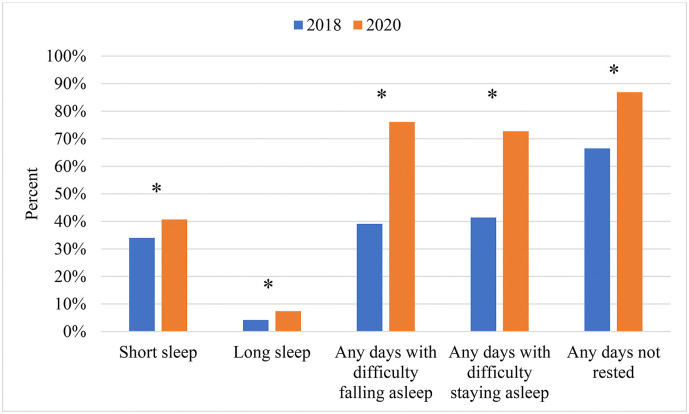
Logistic regressions predicting differences in the prevalence of clinically relevant sleep characteristics for U.S. adults in the NHIS 2018 vs. Luc.id 2020 samples are presented in Table 3 and results are depicted in Fig. 2 . More U.S. adults in 2020 reported shorter than recommended sleep duration than in 2018 (40.7% vs. 34.0%, respectively, OR = 1.36, 99% CI = 1.14 to 1.62). Interestingly, more U.S. adults in 2020 reported longer than recommended sleep duration than in 2018 (7.4% vs. 4.2%, respectively, OR = 2.32, 99% CI = 1.55 to 3.48). Additionally, nearly twice as many adults reported days with difficulties falling asleep (39.1% vs. 76.1%, respectively, OR = 4.55, 99% CI = 3.80 to 5.46) and staying asleep (41.4% vs. 72.7%, respectively, OR = 2.98, 99% CI = 2.50 to 3.55) in 2020 than in 2018. Moreover, substantially more adults reported days not feeling rested in 2020 (2018: 66.5% vs. 2020: 86.9%, OR = 3.21, 99% CI = 2.59 to 3.98).
Table 3.
Results from logistic regressions predicting clinical sleep characteristics of NHIS 2018 sample of internet users vs. Luc.id April 2020 online nationally representative sample.
| NHIS 2018 |
Luc.id 2020 |
||
|---|---|---|---|
| % yes (total N) | % yes (total N) | OR (99% CI) | |
| Shorter than recommended sleep duration | 34.0% (19,369) | 40.7% (2059) | 1.36 (1.14–1.62) |
| Longer than recommended sleep duration | 4.2% (19,369) | 7.4% (2059) | 2.32 (1.55–3.48) |
| 1+ days of difficulty falling asleep | 39.1% (19,381) | 76.1% (2048) | 4.55 (3.80–5.46) |
| 1+ days of difficulty staying asleep | 41.4% (19,373) | 72.7% (2054) | 2.98 (2.50–3.55) |
| 1+ days of not feeling rested | 66.5% (19,333) | 86.9% (2057) | 3.21 (2.59–3.98) |
Note. OR = Odds ratio. OR over one indicates increase in risk for outcome from 2018 to 2020.
Fig. 2.
Percentage of participants reporting clinically relevant sleep characteristics in 2018 vs. 2020. * indicates statistically significant difference.
Finally, because different states implemented responses to COVID-19 at different timelines and magnitudes, analyses were reconducted after accounting for region of the U.S. the participant lived in. Although participants who lived in Southern states reported more days with difficulties falling asleep in 2020 than participants from other states, accounting for region of the U.S. did not alter results nor their interpretation.
3.2. Differences in sleep characteristics of U.S. age groups between 2018 and 2020
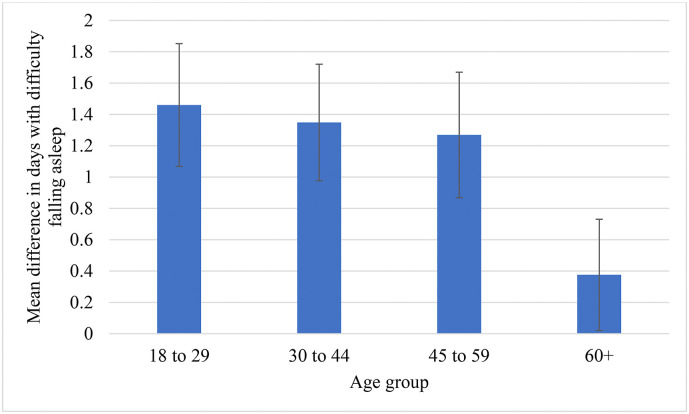
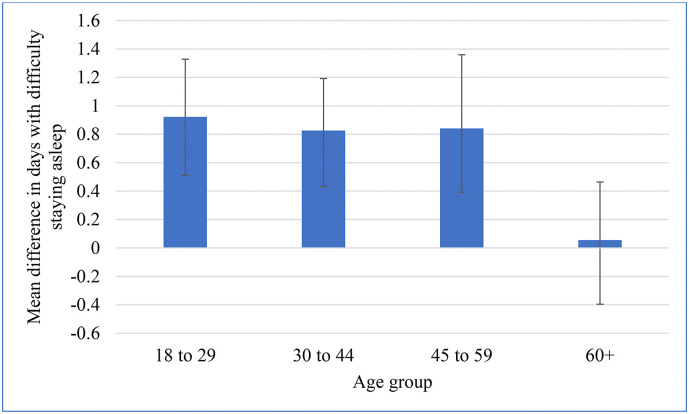
When examining whether age group moderated differences in sleep characteristics between the 2018 and 2020 samples, age group significantly moderated the differences in difficulties falling asleep (Wald = 18.73, df = 3, p < .001) and difficulties staying asleep (Wald = 12.44, df = 3, p < .001) between 2018 and 2020. Probing these interactions revealed that for difficulties falling asleep, the 60+ age group had significantly smaller differences between 2018 and 2020 than all other age groups as demonstrated by non-overlapping confidence intervals around mean difference point estimates (see Fig. 3 ). For difficulties staying asleep, the 60+ age group did have any differences in difficulties staying asleep between 2018 and 2020 (M diff = 0.06, 99% CI = −0.40 to 0.46), which tended to be a smaller difference than other age groups, though this was only statistically significant with the 18- to 29-year-old age group as evident by non-overlapping confidence intervals (see Fig. 4 ).
Fig. 3.
Mean difference between 2020 and 2018 in number of days with difficulty falling asleep across age groups. Positive values reflect increases from 2018 to 2020. Error bars represent 99% confidence interval.
Fig. 4.
Mean difference between 2020 and 2018 in number of days with difficulty staying asleep across age groups. Positive values reflect increases from 2018 to 2020. Error bars represent 99% confidence interval.
In terms of clinically relevant sleep characteristics, age group also moderated differences in the prevalence of exceeding recommendations for sleep length (Wald = 29.50, df = 3, p < .001), experiencing any difficulties falling asleep (Wald = 17.21, df = 3, p = .001), and experiencing any difficulties staying asleep (Wald = 17.21, df = 3, p = .001). Probing these interactions revealed that for the 60+ age group had smaller increases in the prevalence of exceeding recommendations for sleep length (OR = 0.31, 99% CI: 0.17 to 0.58), any days experiencing difficulty falling asleep (OR = 0.35, 99% CI: 0.23 to 0.53), and any days experiencing difficulty staying asleep (OR = 0.38, 99% CI: 0.26 to 0.56) between 2018 and 2020 in comparison to the other age groups.
3.3. Differences in sleep characteristics of U.S. Racial groups between 2018 and 2020
When examining differences in sleep characteristics between 2018 and 2020 across racial groups, no clear patterns emerged.
4. Discussion
Multiple sleep characteristics of U.S. adults were different in the 2020 sample as opposed to the 2018 sample, suggesting that sleep may have changed during the spread of COVID-19 (see Fig. 1, Fig. 2). On average, sleep duration was not statistically significantly shorter in 2020 than in 2018; however, U.S. adults reported approximately one more day a week of difficulty falling asleep, staying asleep, and not feeling rested in 2020. Furthermore, these mean level differences translated into differences on clinically relevant sleep characteristics. More adults either slept less or exceeded the National Sleep Foundation recommendations for sleep duration in the 2020 sample than in the 2018 sample (Hirshkowitz et al., 2015). Moreover, the number of U.S. adults experiencing any difficulties falling asleep and staying asleep nearly doubled from 2018 to 2020. Finally, the number of adults reporting any days not feeling rested was also substantially greater in 2020 than in 2018. These findings converge with cross-sectional findings of greater sleep disturbances and poorer sleep quality during the pandemic in Chinese, Greek, and Italian populations (Casagrande et al., 2020; Cellini et al., 2020; Huang and Zhao, 2020; Xiao et al., 2020; Voitsidis et al., 2020). The current findings provide an important advancement to these prior studies by a.) examining sleep characteristics in another distinct population using larger and more representative samples, but also b.) provide insight into the extent to which U.S. sleep characteristics may differ from before to during the COVID-19 pandemic.
At first glance, it may be surprising that mean sleep duration did not show a statistically significant difference when large differences in difficulties in falling asleep and staying asleep emerged. However, the effects of the pandemic may depend on individual characteristics, such as sleep/circadian timing. For instance, stay-at-home orders relaxed morning work/school schedules which may provide greater sleep opportunity for people with later sleep timing, such as adolescents and young adults, and counteract negative effects of the pandemic on sleep duration (Cellini et al., 2020; Sinha et al., 2020; Leone et al., 2020). This possibility dovetails with findings that even individuals such as students and remote workers had a longer sleep opportunity (i.e., longer time in bed) during quarantine, there was not a corresponding increase in sleep duration, speculatively because of co-occurring difficulties falling asleep and staying asleep (Cellini et al., 2021). Examining the effects of the pandemic across individual differences in sleep/circadian timing may reveal more nuanced effects on sleep duration. Additionally, it may seem counterintuitive that larger differences in sleep duration were not observed given the sizeable changes in difficulties falling asleep and staying asleep. This may also be explained by greater flexibility in school/work schedules. Assuming a rigid morning wake-up time, a night in which someone experiences difficulty falling asleep or staying asleep should lead to similar decreases sleep duration; still, relaxation or lack of work/school obligations during the COVID-19 pandemic may allow for a person to sleep-in on a night with such difficulties, thereby buffering the impact of these difficulties on sleep duration. Finally, the proportion of people either not meeting or exceeding the National Sleep Foundation's sleep duration recommendations was greater in 2020 than 2018. More people sleeping less than recommended and more people sleeping more than recommended may obscure differences between the samples when examining mean level changes.
While mean levels of sleep duration appear to have only been slightly different from before to during the COVID-19 pandemic, difficulties falling asleep and staying asleep were greater in 2020 than 2018. Yet, adults aged 60 and older showed smaller differences than younger age groups (see Fig. 3, Fig. 4). Though this study cannot directly speak to why these groups are less and more affected, respectively, possible speculations are offered. Older adults already have greater difficulty falling asleep and staying asleep than younger adults; thus, there may be less room for their sleep to be further impacted by other factors such as COVID-19 (Ohayon et al., 2004). Additionally, older adults may already be living more sheltered lives and may be more habituated to the side effects of stay-at-home orders. Interestingly, results from a population study in France reported that adults under the age of 65 experienced the most improvements in sleep problems after confinement mandates were lifted. Given that results from the current study show that adults over the age of 65 may be experiencing the least changes in sleep during the COVID-19 pandemic, it may be that these limited effects on sleep curtail any detectable improvement in sleep once quarantine mandates are lifted (Beck et al., 2021).
4.1. Limitations
While the current findings provide an important advancement in understanding how sleep characteristics may different from before to during the COVID-19 pandemic, there are important limitations to consider. First, while both the NHIS 2018 and Luc.id 2020 samples were designed to be representative of the U.S. adult population and the samples were extremely similar in socio-demographic variables, it cannot be ruled out that other sociodemographic, psychological, or methodological differences may account for any observed differences in sleep between the two samples. This limitation is notable as other health factors related to sleep, such as weight, physical activity, or substance use, may differ across the two samples and influence differences in sleep between the two samples. Future longitudinal studies will be necessary to rule out such an alternative explanation. Despite this alternative explanation, this study makes a contribution by identifying sleep as a factor that future studies should examine given possible declines in the sleep health of U.S. adults and the importance of sleep for health (Buysse, 2014). Second, this study examined differences between two different samples, each of which were collected on different years. Any detected differences in sleep characteristics may reflect other factors influencing sleep between 2018 and 2020. For instance, Hisler and colleagues previously reported trends in increased difficulty falling asleep and staying asleep from 2013 to 2017 in the U.S. NHIS data (Hisler et al., 2019). The deteriorations in these sleep characteristics observed between the NHIS 2018 and Luc.id 2020 samples may solely reflect this time trend rather than effects of the COVID-19 pandemic. Yet, given that magnitude of changes observed in this prior study were much smaller (i.e., increases in prevalence of sleep difficulties by ~1–3% from 2013 to 2017) than the magnitude of changes in the current study, this factor seems extremely unlikely to fully account for observed differences in this study. Third, all sleep measures were self-reported and are therefore subject to self-report biases and limitations. Future studies using non-self-report measures, such as actigraphy, are needed to reinforce findings from this study. Fourth, this study was not able to separately examine effects on weekday and weekend sleep. Because some of the effects the pandemic on sleep may be due to changes in work/school, which typically occur on weekdays, examining the separate influence on weekday vs. weekends may provide further nuanced insight into how the pandemic and changes in social obligations affect sleep. Finally, analyses looking at particular age and race groups may be less precise and less reliable due to smaller sample sizes when examining subgroups in comparison to full sample analyses. Future work should continue examining how the COVID-19 pandemic impacted people across different sociodemographic groups and seek to replicate our finding that adults over 60 experienced less effects of the pandemic on their sleep characteristics.
5. Conclusions and implications
These findings implicate reductions in the sleep health of the U.S. adult population since the spread of COVID-19. In particular, the prevalence of people having difficulties falling asleep, staying asleep, and not feeling rested, and not meeting recommendation sleep duration guidelines may have increased, especially among adults 18 to 59. The overall picture is that sleep has deteriorated during the pandemic; given that sleep plays an important role in biological and psychological health, such deteriorations implicate concomitant deteriorations in other aspects of health or may foreshadow them. For instance, emerging studies suggest that mental health has declined during the COVID-19 pandemic(Casagrande et al., 2020; Rajkumar, 2020). Because mental health and sleep are tightly connected, changes in mental and sleep health during the pandemic are likely to be associated with each other and intervening on one aspect of health may improve the other (Casagrande et al., 2020; Freeman et al., 2017; Rajkumar, 2020). Moreover, given that insomnia is characterized by difficulty falling asleep, difficulty staying asleep, and not feeling rested, these findings suggest that the prevalence of insomnia symptoms may have increased during the pandemic and may be more prevalent in adults under age 60. Finally, these findings highlight particular populations and sleep characteristics that may warrant extra consideration by clinicians and should be targeted in future research.
Author credit statement
Garrett Hisler: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Jean Twenge: Conceptualization, Methodology, Writing – review & editing, Supervision.
References
- Abouk R., Heydari B. The immediate effect of covid-19 policies on social distancing behavior in the United States. 2020. https://ssrn.com/abstract=3571421 Available at: SSRN. [DOI] [PMC free article] [PubMed]
- Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., Schlarb A., Frase L., Jernelov S., Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Baldwin R., Weder Di Mauro B. CEPR Press; 2020. Economics in the Time of COVID-19. [Google Scholar]
- Bartik A.W., Bertrand M., Cullen Z., Glaeser E.L., Luca M., Stanton C. The impact of COVID-19 on small business outcomes and expectations. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117:17656. doi: 10.1073/pnas.2006991117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck F., Leger D., Cortaredona S., Verger P., Peretti-Watel P., Seror V., Cortaredona S., Fressard L., Launay O., Raude J. Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burszytyn L., Rao A., Roth C., Yanagizawa-Drott D. University of Chicago, Becker Friedman Institute for Economics Working Paper; 2020. Misinformation during a Pandemic; pp. 2020–2044. [Google Scholar]
- Buysse D.J. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. SSRN Abstract Database; 2020. The Enemy Who Sealed the World: Effects Quarantine Due to the COVID-19 on Sleep Quality, Anxiety, and Psychological Distress in the Italian Population. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Giovanna M., Costa S. Changes in sleep pattern, sense of time, and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020;29:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Conte F., De Rosa O., Giganti F., Malloggi S., Reyt M., Guillemin C., Schmidt C., Muto V., Ficca G. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Barceló J., Hartnett A.S., Kubinec R., Messerschmidt L. COVID-19 government response event dataset (CoronaNet v.1.0) Nature Human Behaviour. 2020;4:756–768. doi: 10.1038/s41562-020-0909-7. [DOI] [PubMed] [Google Scholar]
- Coppock A., Mcclellan O.A. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Research & Politics. 2019;6 2053168018822174. [Google Scholar]
- Czajka J.L., Beyler A. Declining response rates in federal surveys: trends and implications (background paper) Mathematica Policy Research. 2016:1–86. [Google Scholar]
- Freeman D., Sheaves B., Goodwin G.M., Yu L.-M., Nickless A., Harrison P.J., Emsley R., Luik A.I., Foster R.G., Wadekar V., Hinds C., Gumley A., Jones R., Lightman S., Jones S., Bentall R., Kinderman P., Rowse G., Brugha T., Blagrove M., Gregory A.M., Fleming L., Walklet E., Glazebrook C., Davies E.B., Hollis C., Haddock G., John B., Coulson M., Fowler D., Pugh K., Cape J., Moseley P., Brown G., Hughes C., Obonsawin M., Coker S., Watkins E., Schwannauer M., Macmahon K., Siriwardena A.N., Espie C.A. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. The Lancet Psychiatry. 2017;4:749–758. doi: 10.1016/S2215-0366(17)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funder D.C., Ozer D.J. Evaluating effect size in psychological research: sense and nonsense. Advances in Methods and Practices in Psychological Science. 2019;2:156–168. [Google Scholar]
- Gallicchio L., Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J. Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- Gao C., Scullin M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020;73:1–10. doi: 10.1016/j.sleep.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A.N., Walker M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014;10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffajee R.L., Mello M.M. Thinking globally, acting locally — the U.S. Response to covid-19. N. Engl. J. Med. 2020;382:e75. doi: 10.1056/NEJMp2006740. [DOI] [PubMed] [Google Scholar]
- Hardeman R.R., Medina E.M. In: Promoting Health Equity Among Racially and Ethnically Diverse Adolescents: A Practical Guide. Barkley L., Svetaz M.V., Chulani V.L., editors. Springer International Publishing; Cham: 2019. Structural racism and critical race theory: contributions to adolescent health inequities and outcomes. [Google Scholar]
- Hirshkowitz M., Whiton K., Albert S.M., Alessi C., Bruni O., Doncarlos L., Hazen N., Herman J., Adams Hillard P.J., Katz E.S., Kheirandish-Gozal L., Neubauer D.N., O'donnell A.E., Ohayon M., Peever J., Rawding R., Sachdeva R.C., Setters B., Vitiello M.V., Ware J.C. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep health. 2015;1:233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Hisler G., Muranovic D., Krizan Z. Changes in sleep difficulties among the U.S. population from 2013 to 2017: results from the National Health Interview Survey. Sleep Health. 2019;5:615–620. doi: 10.1016/j.sleh.2019.08.008. [DOI] [PubMed] [Google Scholar]
- Howard T.C., Navarro O. Critical race theory 20 Years later: where do we go from here? Urban Educ. 2016;51:253–273. [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange T., Dimitrov S., Born J. Effects of sleep and circadian rhythm on the human immune system. Ann. N. Y. Acad. Sci. 2010;1193:48–59. doi: 10.1111/j.1749-6632.2009.05300.x. [DOI] [PubMed] [Google Scholar]
- Leone M.J., Sigman M., Golombek D.A. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr. Biol. 2020;30:R930–r931. doi: 10.1016/j.cub.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon M.M., Carskadon M.A., Guilleminault C., Vitiello M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- Prather A.A., Gurfein B., Moran P., Daubenmier J., Acree M., Bacchetti P., Sinclair E., Lin J., Blackburn E., Hecht F.M., Epel E.S. Tired telomeres: poor global sleep quality, perceived stress, and telomere length in immune cell subsets in obese men and women. Brain Behav. Immun. 2015;47:155–162. doi: 10.1016/j.bbi.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian journal of psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T., Wirz-Justice A., Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythm. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- Rosenthal R., Rubin D.B. A simple, general purpose display of magnitude of experimental effect. J. Educ. Psychol. 1982;74:166–169. [Google Scholar]
- Sinha M., Pande B., Sinha R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: a national survey. Journal of Public Health Research. 2020;9 doi: 10.4081/jphr.2020.1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- slopen N., Lewis T.T., Williams D.R. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. doi: 10.1016/j.sleep.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voitsidis P., Gliatas I., Bairachtari V., Papadopoulou K., Papageorgiou G., Parlapani E., Syngelakis M., Holeva V., Diakogiannis I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr. Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 Days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. : international medical journal of experimental and clinical research. 2020;26:e923921. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]