Abstract
Background
The COVID-19 pandemic has a worldwide impact on all health services, including childhood immunizations. In Canada, there is limited data to quantify and characterize this issue.
Methods
We conducted a descriptive, cross-sectional study by distributing online surveys to physicians across Ontario. The survey included three sections: provider characteristics, impact of COVID-19 on professional practice, and impact of COVID-19 on routine childhood immunization services. Multivariable logistic regression identified factors associated with modification of immunization services.
Results
A total of 475 respondents answered the survey from May 27th to July 3rd 2020, including 189 family physicians and 286 pediatricians. The median proportion of in-person visits reported by physicians before the pandemic was 99% and dropped to 18% during the first wave of the pandemic in Ontario. In total, 175 (44.6%) of the 392 respondents who usually provide vaccination to children acknowledged a negative impact caused by the pandemic on their immunization services, ranging from temporary closure of their practice (n = 18; 4.6%) to postponement of vaccines in certain age groups (n = 103; 26.3%). Pediatricians were more likely to experience a negative impact on their immunization services compared to family physicians (adjusted odds ratio [aOR] = 2.64, 95% CI: 1.48–4.68), as well as early career physicians compared to their more senior colleagues (aOR = 2.69, 95% CI: 1.30–5.56), whereas physicians from suburban settings were less impacted than physicians from urban settings (aOR = 0.62, 95% CI: 0.39–0.99). Some of the proposed solutions to decreased immunization services included assistance in accessing personal protective equipment, dedicated centers or practices for vaccination, universal centralized electronic immunization records and education campaigns for parents.
Conclusions
COVID-19 has caused substantial modifications to pediatric immunization services across Ontario. Strategies to mitigate barriers to immunizations during the pandemic need to be implemented in order to avoid immunity gaps that could lead to an eventual increase in vaccine preventable diseases.
Keywords: Immunization coverage, COVID-19, Health systems, Cross-sectional survey, Pediatrics, Primary care and family medicine
Abbreviations: aOR, Adjusted Odds Ratio; CDC, Centers for Disease Control; CI, Confidence Interval; COVID-19, Coronavirus Disease 2019; GTA, Greater Toronto Area; HPV, Human Papillomavirus; IQR, Interquartile range; PPE, Personal Protective Equipment; REDCap, Research Electronic Data Capture; PHAC, Public Health Agency of Canada; US, United States; VPDs, Vaccine Preventable Diseases
1. Background
The coronavirus disease 2019 (COVID-19) pandemic is causing an unprecedented impact on the delivery of healthcare services at all levels, including on routine childhood immunizations [1], [2], [3]. Studies from France and the Centers for Disease Control (CDC) in the United States (US) have revealed declines of up to 70% in routine childhood vaccine coverage since the beginning of the COVID-19 pandemic [4], [5], [6]. Disruptions to immunizations secondary to outbreaks of infectious diseases other than COVID-19 have previously resulted in increased rates of vaccine preventable diseases (VPDs), highlighting the current risks to Canadian children and their communities [7], [8]. Some low- and middle-income countries have also reported reduced access to mass vaccination programs and an increase in cases of measles attributed to COVID-19 [9], [10]. In response to the pandemic, various public health and governmental institutions in Canada have recommended that routine immunizations constitute an essential health service that should not be deferred [11], [12].
In Canada, about half of the hospitalized children who tested positive for SARS-CoV-2 were admitted for reasons other than COVID-19, with SARS-CoV-2 being incidentally detected. Aside from cases of multisystem inflammatory syndrome in children (MIS-C) and its temporal association with COVID-19, which remains poorly understood, children and young adults are generally mildly affected by the disease when compared to adults [13], [14]. The indirect impacts of the COVID-19 pandemic on access to medical services, including routine immunizations, represent an important burden on children’s health that may outweigh the burden of the infection itself [15].
In Ontario, school-based immunization of adolescents with hepatitis B vaccine (HBV), human papillomavirus (HPV) vaccine and meningococcal quadrivalent vaccine is delivered by public health units, but all other routine infant and childhood vaccines are most often administered in primary care clinics by family physicians and pediatricians. Some of the publicly funded vaccines can also be administered by pharmacists, but only for individuals older than five years old [16]. While there are anecdotal reports of caregivers not bringing their children to primary care providers for immunizations and of clinicians that have ceased to provide these services due to perceived risk of COVID-19, there are currently limited data to quantify the magnitude of this issue and identify contributing factors. Furthermore, whether the COVID-19 pandemic has impacted access to immunization differentially for specific groups of children is not known. The scarcity of data on vaccination practices in Canada during the COVID-19 pandemic precludes any specific evidence-based recommendations regarding best practices in safely maintaining routine childhood immunization. The purpose of this study is to rapidly generate data to better understand the impact of COVID-19 on physicians’ immunization practices in Ontario.
2. Methods
This is a descriptive cross-sectional study consisting of a self-administered online survey. The survey was distributed electronically to pediatricians and family physicians across the province of Ontario. Emails were initially sent to a listserv of 347 pediatricians from the Greater Toronto Area (GTA) on May 27, 2020. An email was then sent on June 15, with reminders on June 22 and 29, to the Pediatricians Alliance of Ontario listserv, which comprises 1,313 pediatricians working in Ontario, including the 347 pediatricians from the GTA listserv. The survey was also distributed concomitantly on June 12 and 25 to family physicians using a listserv from the University of Toronto Department of Family and Community Medicine, which comprises 1,983 family physicians throughout the GTA and beyond. After having completed the survey, the respondents were given an individual link to another independent survey, where they could provide their name and email address to participate in an incentive draw for one of three $100 gift cards. The goal was to maximise participation and ensure adequate external validity and representation from the target population [17]. Participants could decide not to opt in for the incentive draw if they wished to keep their responses completely anonymous. The collected emails and names were not linked with the participants’ responses to maintain confidentiality. Approval from The Hospital for Sick Children Research Ethics Board (REB) was obtained for this study (REB 1000070361).
2.1. Survey instrument
The survey instrument was developed with input from hospital and community-based physicians from general pediatrics, infectious diseases and family medicine. The survey incorporated previously published questionnaires on immunization practices of healthcare providers (HCP) and studies on HCP characteristics associated with up-to-date vaccination coverage of their patients. The survey was designed using Research Electronic Data Capture (REDCap) software (version 10.0.4; Vanderbilt University) and distributed by email as previously described. It was pilot tested with select pediatricians and family physicians from the target study population to ensure clarity of questions and instructions, ease of navigation and time for completion. The survey included three main sections: (1) HCP socio-demographic and practice characteristics, (2) impact of COVID-19 on clinical practice, and (3) impact of COVID-19 on immunization services.
Physician’s characteristics collected in the first section of the survey included physician’s specialty (family physician, general pediatrician or pediatric subspecialist), sex (male, female or prefer not to say), years in practice (<5 years, 5–20 years or > 20 years) and country of medical training (Canada or outside Canada). Practice characteristics collected included setting (urban, suburban or rural), type of practice site (community solo practice, community group practice, family health team or hospital), practice forward sortation area (defined by the three first characters of the practice’s postal code), proportion of patients < 19 years of age (for family physicians only), as well as availability of personal protective equipment (PPE) in physicians’ practices. These questions were selected based on previously published studies documenting HCP characteristics that may be associated with adequate on-time immunization coverage of their patients [18].
The second section of the survey aimed to quantify the impact of the COVID-19 pandemic on physician’s clinical practice. Respondents were asked if the pandemic caused the physical closure of their practice, and if so, the specific reasons associated with closure. If their practice had remained open, respondents were asked to indicate the proportion of visits conducted in-person before the pandemic and during the pandemic.
The third section of the survey included questions aiming to assess the impact of COVID-19 on the provision of immunization services. Respondents were asked to select from a list of what they felt were significant barriers to their immunization services during the pandemic. The survey also included questions on respondents’ attitudes towards vaccines during the pandemic, such as if they felt it was preferable to postpone routine childhood immunizations to limit the spread of COVID-19 and risk for HCP. Answers for these questions were based on a five-point Likert scale (strongly agree, agree, neutral, disagree or strongly disagree). Participants were also asked if they provided vaccines to patients who were referred from other clinics, and how they managed their patients who have missed immunizations due to school closures. Lastly, the survey included two open-ended questions prompting respondents to describe any further barriers to the delivery of immunization services, as well as ideas and solutions on how routine childhood immunizations could be safely maintained during the COVID-19 pandemic. Physicians who reported not administering vaccines to children or teenagers in their regular practice, or family physicians who do not see children in their usual practice, were only asked the questions on attitudes regarding vaccines, as well as the open-ended question about potential solutions to maintain childhood immunization services. The detailed survey instrument can be found in the supplementary material (Appendix 1).
2.2. Statistical analysis
Survey responses were analysed using Microsoft Excel (Office 365, Microsoft corp., Washington, USA) and Stata version 16.1. Socio-demographic and practice characteristics of respondents were summarized using frequencies and percentages. Logistic regression was performed to identify HCP-associated predictors of a negative impact from the COVID-19 pandemic on immunization services. A negative impact on immunization practices was reported as a binary variable (impact or no impact) and defined as a modification in immunization practices or complete closure of the practice of a respondent who usually provides immunization to children. Covariates for the multivariable model were selected a priori and independent of univariate analyses, based on expert opinion and previous research documenting an association with on-time immunization coverage. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were calculated, and p-values < 0.05 were considered statistically significant. Violin plots with medians and interquartile ranges (IQR) were generated using Python’s seaborn package to visualize changes in the proportion of in-person visits before versus during the pandemic. In respect to respondents’ qualitative input from the open-ended questions, thematic content analysis was performed by the first author. Respondents’ answers were clustered under emerging themes, and the number of comments within each theme was reported using frequencies and percentages.
3. Results
3.1. Participant characteristics
A total of 475 responses were received from throughout Ontario, including 286 pediatricians (21.8% response rate) and 189 family physicians (9.5% response rate) within a 5-week period, from May 27 to July 3, 2020 (14.4% total response rate), a time frame that corresponded with the first wave of COVID-19 cases in Ontario. In total, 392 respondents (83%) reported usually providing vaccines to children and teenagers. In the pediatrician group, 239 (84%) were general pediatricians and 47 (16%) were pediatric subspecialists. From the subspecialist group, 21 respondents (44%) reported usually providing routine childhood immunization. In the family physician group, the vast majority reported usually seeing children as part of their practice (n = 183, 97%) and providing vaccines to children (n = 181, 96%), with children accounting for 26.2% of their patients on average (standard deviation of 16.8%). With respect to PPE, a majority of respondents had access to gloves (n = 457, 96%), surgical masks (n = 452, 95%), eye protection (n = 399, 84%) and gowns (n = 350, 74%), and about half of respondents reported having access to N95 respirators (n = 220, 46%). Most respondents reported that their clinic was responsible for buying PPE (n = 361, 76%), with fewer respondents receiving PPE from donations (n = 78, 16%) or the government (n = 65, 14%). All respondent characteristics are detailed in Table 1 . Basic demographic characteristics of all pediatricians from the PAO are similar to the survey’s respondents (41.8% male, 58.2% female) with a majority of respondents aged over 40 years old and practicing in urban settings, including the city of Toronto and the GTA, Ottawa and Niagara (PAO, personal communication, May 18th, 2021). For family physicians, there was a larger proportion of female physicians who responded to our survey than throughout the province of Ontario (70% compared to 49.5%), but a similar proportion of physicians who trained outside Canada (21% compared to 25.3%), with a majority of physicians aged over 40 years old [19]. A map of the province with an overview of the number of respondents by forward sortation area was also created (Fig. 1 ). Of note, the initial 102 respondents from the GTA pediatrician listserv were not asked their practices’ forward sortation area and are therefore not represented on this map.
Table 1.
Characteristics of respondents.
| Specialty | Total [n, (%)] |
Pediatricians [n, (%)] |
Family physicians [n, (%)] |
|---|---|---|---|
| 475 (1 0 0) | 286 (60) | 189 (40) | |
| Subspecialty | |||
| Family physician | 186 (39) | – | 186 (98) |
| Emergency physician | 3 (1) | – | 3 (2) |
| General pediatrician | 239 (50) | 239 (94) | – |
| Pediatric subspecialist | 47 (10) | 47 (16) | – |
| Number of years into practice | |||
| Less than 5 years | 55 (12) | 35 (12) | 20 (11) |
| 5 – 20 years | 209 (44) | 119 (42) | 90 (48) |
| More than 20 years | 211 (44) | 132 (46) | 79 (42) |
| Place of medical training | |||
| Canada | 334 (70) | 166 (58) | 168 (89) |
| Outside Canada | 141 (30) | 120 (42) | 21 (11) |
| Sex | |||
| Female | 304 (64) | 172 (60) | 132 (70) |
| Male | 168 (35) | 111 (39) | 57 (30) |
| Prefer not to say | 3 (1) | 3 (1) | 0 |
| Setting of practice | |||
| Urban | 313 (66) | 187 (65) | 126 (67) |
| Suburban | 145 (31) | 91 (32) | 54 (28) |
| Rural or remote | 17 (3) | 8 (3) | 9 (5) |
| Type of practice site | |||
| Community solo practice | 114 (24) | 100 (35) | 14 (7) |
| Community group practice | 208 (44) | 129 (45) | 79 (42) |
| Academic practice (Family Health teams, etc.) | 98 (21) | 6 (2) | 92 (49) |
| Hospital | 55 (11) | 51 (18) | 4 (2) |
| Seeing children in practice | |||
| Yes | – | – | 183 (97) |
| No | – | – | 5 (3) |
| Usually providing vaccines | |||
| Yes | 392 (83) | 211 (74) | 181 (96) |
| No | 83 (17) | 75 (26) | 8 (4) |
Fig. 1.
Number of survey respondents by forward sortation area.
3.2. Impact on physicians’ practices
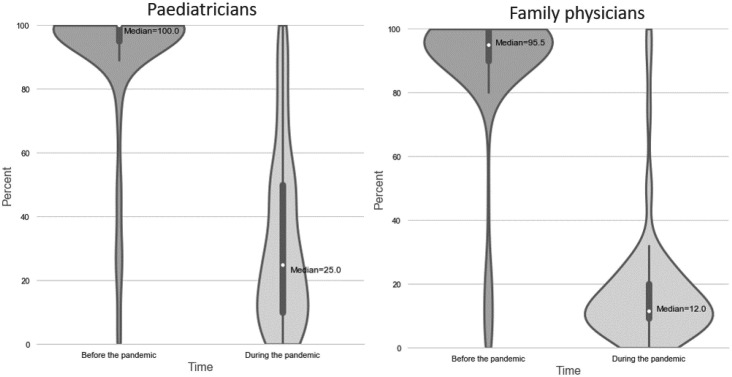
In total, 18 respondents (4%) reported that the COVID-19 pandemic caused a temporary closure of their practice, with the lack of PPE being the main reason for the closure (n = 11, 61%). The median proportion of in-person visits reported by family physicians was 95.5% (IQR 90.0%-100.0%) before the pandemic and dropped to 12.0% (IQR 9.3%-20.0%) during the pandemic. Similarly, for pediatricians, the median proportion of in-person visits was 100.0% (IQR 95.0%-100.0%) before the pandemic and dropped to 25.0% (IQR 10.0%-50.0%) during the pandemic. The distribution of in-person visits before and during the pandemic is displayed in Fig. 2 .
Fig. 2.
Violin plots of the proportion of in-person visits (%) before and during the pandemic for pediatricians and family physicians.
3.3. Impact on physicians’ immunization services
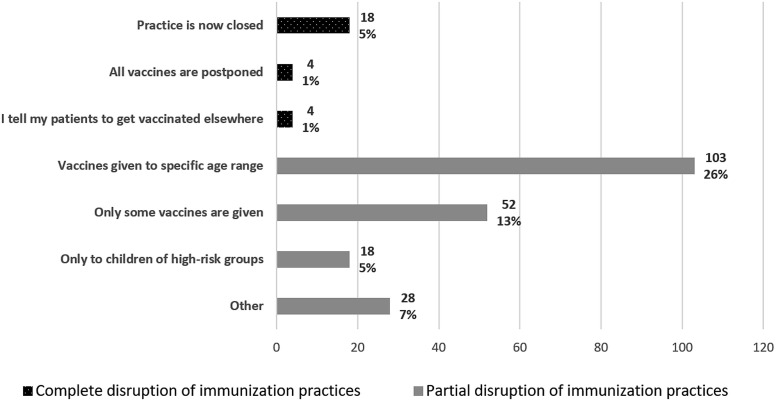
In total, 175 (45%) of the 392 respondents who usually provide vaccination to children acknowledged a negative impact caused by the pandemic on their immunization services, including 18 respondents (5%) having closed their practice, 4 (1%) postponing all vaccines and 4 (1%) telling their patients to get vaccinated in another clinic. Most respondents reported only providing immunizations to children of a specific age (n = 103; 26%), with the majority of this group continuing the vaccination of children aged 18 months and less (n = 97, 94%), and postponing vaccination for children aged 4–6 years old (n = 79, 77%) and teenagers (n = 100, 97%). Fewer respondents reported only postponing specific vaccines (n = 52, 13%), especially the rotavirus vaccine (n = 33, 63%), the influenza vaccine (n = 41, 79%), and the HPV vaccine (n = 44, 85%). Fig. 3 represents the reported impact of COVID-19 on immunization practices. In total, 118 respondents (30%) reported providing immunizations to patients from other clinics that were not offering this service anymore because of the pandemic, either frequently (n = 19, 5%), occasionally (n = 69, 18%) or rarely (n = 30, 7%). A majority of respondents (n = 271, 57%) reported that they did not have a system in place to keep track of their patients who may have missed vaccine doses. Regarding vaccines usually given in school settings (HBV, HPV and meningococcal quadrivalent vaccine), many of the survey participants reported not providing these vaccines and instead leaving the missed doses to be given in the schools when they would re-open (n = 111, 28%) or to public health clinics (n = 74, 19%).
Fig. 3.
Bar chart representing the impact of COVID-19 on physicians’ immunization services for children. NB percentages are based on physicians who usually provide vaccines to children (n=392).
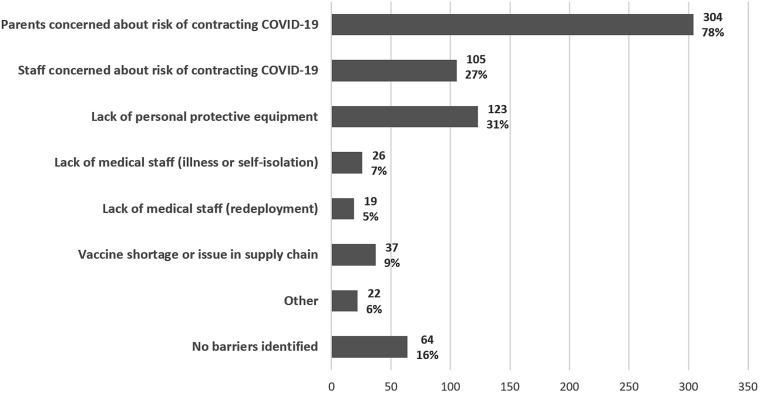
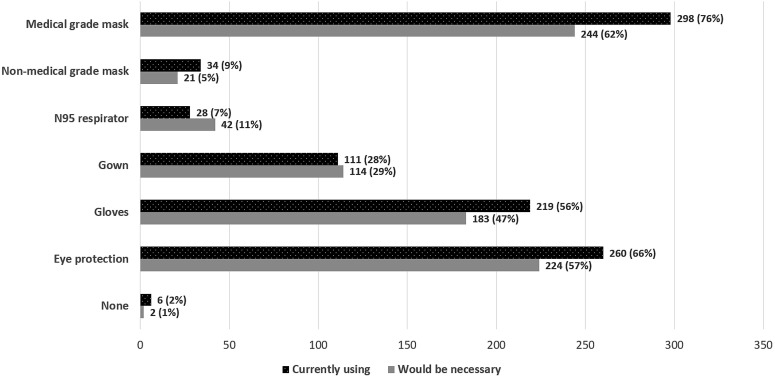
Most respondents were in disagreement or strong disagreement with the following statements: “I feel it is safe to postpone routine childhood immunizations because current physical distancing measures decrease the risk of vaccine preventable diseases” (n = 430, 91%); “I feel it is preferable to postpone routine childhood immunizations to limit the spread of COVID-19” (n = 434, 91%); and “I feel it is preferable to postpone routine childhood immunizations to limit the risk of COVID-19 exposure for healthcare workers” (n = 419, 88%). A majority of respondents acknowledged that there were significant barriers to the delivery of immunization services pertaining to the COVID-19 pandemic (n = 328, 84%). The most frequently identified barriers are shown in Fig. 4 . Fig. 5 shows the PPE elements used by physicians to vaccinate asymptomatic children, as well as the elements that they think would be truly necessary.
Fig. 4.
Bar chart representing the identified barriers to childhood routine immunization during the COVID-19 pandemic. NB percentages are based on physicians who usually provide vaccines to children (n=392).
Fig. 5.
Bar chart representing the PPE elements currently used by HCP for vaccination of asymptomatic children, and which elements they think would be necessary. NB percentages are based on physicians who usually provide vaccines to children (n=392).
3.4. Factors associated with decreased immunization services
In the multivariate logistic regression analysis, pediatricians were more likely to report that COVID-19 negatively impacted their delivery of immunizations than family physicians (aOR = 2.08, 95% CI 1.31–3.30), while physicians based in suburban practices were less likely to report a negative impact than physicians in urban practices (aOR = 0.61, 95% CI 0.39–0.97). Physicians in practice for less than five years were also more likely to report impacted immunization services compared to physicians in practice for 5–20 years (aOR = 2.69, 95% CI 1.30–5.56). There was no statistically significant association between impacted immunization services and either physician’s sex or country of medical training. All associations, with odds ratio from the univariate analysis and adjusted odds ratio from the multivariate analysis are displayed in Table 2 .
Table 2.
Multivariable logistic regression of practitioner-level predictors of overall COVID-19 negative impact* on routine childhood immunization services.
| Characteristics | Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|
| OR (95% CI) | p-value | aOR (95% CI) | p-value | |
| Specialty | ||||
| Family physician | ref | --- | ref | --- |
| Pediatrician | 1.73 (1.16–2.60) | 0.008 | 2.08 (1.31–3.30) | 0.002 |
| Site of primary practice | ||||
| Community solo practice | ref | --- | --- | --- |
| Community group practice | 0.91 (0.56–1.48) | 0.714 | --- | --- |
| Academic practice (family health team) |
0.90 (0.51–1.60) | 0.726 | --- | --- |
| Hospital | 0.98 (0.28–3.42) | 0.973 | --- | --- |
| Years of practice | ||||
| <5 years | 2.53 (1.24–5.16) | 0.011 | 2.69 (1.30–5.56) | 0.008 |
| 5–20 years | ref | --- | ref | --- |
| >20 years | 0.89 (0.58–1.36) | 0.589 | 0.75 (0.47–1.18) | 0.208 |
| Physician's sex | ||||
| Female | ref | --- | ref | --- |
| Male | 1.06 (0.69–1.63) | 0.796 | 1.25 (0.80–1.97) | 0.327 |
| Country of medical training | ||||
| Canada | ref | --- | ref | --- |
| Outside canada | 1.06 (0.69–1.63) | 0.796 | 0.72 (0.44–1.18) | 0.192 |
| Setting of primary practice | ||||
| Urban | ref | --- | ref | --- |
| Suburban | 0.65 (0.42–1.01) | 0.055 | 0.61 (0.39–0.97) | 0.037 |
| Rural or remote | 0.78 (0.24–2.53) | 0.682 | 1.10 (0.33–3.68) | 0.873 |
| Practice in gta | ||||
| No | ref | --- | --- | --- |
| Yes | 1.25 (0.83–1.89) | 0.283 | --- | --- |
Responses of two physicians (0.5%) were excluded from the regression analyses due to missing data points.
Impact defined as a modification in physicians’ immunization practices or complete closure of the practice.
3.5. Thematic content analysis of open-ended questions
The first open-ended question from the survey pertained to further barriers identified by respondents regarding provision of childhood immunization services during the COVID-19 pandemic. In total, 137 (35%) of the 392 respondents usually administering vaccines provided answers to this question. The most frequently identified themes and barriers to immunizations was “school closures” (n = 28, 20%), followed by “vaccine supply issues” (n = 21, 15%) and “parental concerns” (n = 20, 15%). Identified barriers from the respondents’ answers are listed in Table 3 , with an associated representative quote. All survey respondents were also asked to provide suggestions to safely maintain childhood immunizations throughout the COVID-19 pandemic in a second open-ended question. In total, 189 (40%) of the total 475 respondents provided answers. The most frequent suggestions were: “assistance in providing personal protective equipment to practices” (n = 65, 34%), “reorganization of patient flow” (n = 48, 25%), “dedicated centers or practices for vaccination” (n = 41, 22%), as well as “parental education and campaigning” (n = 31, 16%). %). Identified suggestions from the respondents’ answers are listed in Table 4 , with an associated representative quote.
Table 3.
Barriers and impact to routine childhood immunization from respondents’ qualitative input.
| Barriers to immunizations | Number of related comments [n, (%)] | Illustrative comments |
|---|---|---|
| School closures | 28 (20)* | School immunizations are impossible to keep up as no contact with public health about what is missed or started. Plus we do not have those immunizations in the office. |
| Vaccine supply issue | 21 (15) | It has brought the fragmentation of our system to the forefront- e.g. we have continued, schools haven't, families are confused. Public health reduced our vaccine quantities even though we maintained full service. This was an unnecessary barrier we had to expend time and energy to overcome. |
| Parental concerns | 20 (15) | Government puts such a fear into people of COVID-19 that parents can’t see beyond one illness at present. |
| Lack of PPE | 17 (13) | Initially had minimal to no PPE with closure of clinic to virtual visits only, eventually bought PPE to offer immunizations prioritizing 18 months under. |
| Significant delays for older children | 16 (12) | We aren’t able to bring in the older kids because we want to keep the office clean and safe for the newborns and infants. We have made this a priority because our group recognizes how important it is to vaccinate these children. |
| Reduced office hours | 14 (10) | Immunization may be delayed because parents do not want to come to the clinic and because I have limited the hours in my clinic |
| Unpreparedness | 14 (10) | At the start of the pandemic we didn't have a set way to deal with patients but as things evolved, we now have a smoother system. |
| Lack of support (Government, public health, etc.) | 11 (8) | I do not feel the government has supported physicians at all. As well public health continues to send the important message to families about vaccinating children yet they are not supporting offices either with respect to PPE or even stepping up to provide vaccines to older children (ages 4–6) or the grade 7 cohort. |
| Visits taking longer | 10 (7) | It takes me about 30–45 min per visit, because I disinfect the room between patients and have parents wait in the car. |
| Lack of public awareness / knowledge | 7 (5) | PPE and staff safety are the major concerns, as well as lack of education for parents regarding immunization and COVID 19 risks. |
| Concerns for staff safety | 7 (5) | Postponement may occasionally be necessary to protect me and staff if enquiry indicates that the parent(s), the patient, or house-hold members carry a risk of having Covid19 infection. |
| Practices’ closure | 6 (4) | Our government agencies and medical associations were very slow from the start making it clear that many pediatric offices remained open and that immunizations were still important. Many GP offices in our community were shut down and remain so. There was a local assumption by many that we were as well. |
| Total number of comments | 137 (35)** |
Percentages were calculated based on number of free text comments received for this question.
Percentage was calculated based on the number of respondents who usually provide vaccines for children and were presented with this question
Table 4.
Suggestions from respondents to safely maintain immunization coverage for children throughout the COVID-19 pandemic.
| Possible solutions | Number of related comments [n, (%)] | Illustrative comments |
|---|---|---|
| Assistance in providing PPE to practices | 65 (34)* | I have written letters to local businesses, the government and the OMA requesting assistance with obtaining PPE and have received no assistance or replies. Our clinic is supporting several other clinics in the area by providing pediatric care for their patients when other offices close. Without PPE, our office will also have to close. |
| Reorganising patient flow | 48 (25) | One parent per child. Parents are called the previous day by me and I go through the child's development and answer all their questions. The following day is then only for the actual vaccination. It works about 85% of the time. |
| Dedicated centers or practices for vaccination | 41 (22) | Trying to establish a community hospital site for routine vaccinations to make sure that primary care providers with closed offices have a simple alternative. I would love to see all childhood immunizations given at a centralized location and NOT in pediatrician's offices. |
| Education campaigns targeting parents | 31 (16) | The phone calls really help. We actively call parents and explain our precautions, and that we feel strongly that immunization should not be delayed. |
| Patient screenings | 28 (15) | The patients appreciate when we screen them over the phone and go through the protocol used, bring reassurance that we are taking the appropriate measures. |
| Centralized guidance | 14 (7) | Better guidance from groups like the CPS which has been virtually completely lacking during this pandemic. In addition, guidance for the next wave of COVID-19, and for the next pandemic, both of which will come. |
| Masking of patients and parents | 12 (6) | Mom and dads must be masked when they come in, distancing, plexiglass at our reception. |
| Vaccines given outside of practices (e.g. drive-thru) | 9 (5) | We offer vaccine administration in the parking lot where they can wait in their car after the shot to ensure no reaction. This option is appealing to most parents. |
| Subsidies for practices | 7 (4) | We should reimburse pediatricians offices for the extra time and cost encountered by them to provide such service. I suggest adding Covid surcharge in amount of 30% to all immunization related visits |
| Ensure adequate vaccine supply | 7 (4) | A centralized provincial clearinghouse for ordering vaccines and mailing of vaccines directly to our offices would decrease likelihood of shortages and delays in vaccine administration. |
| Simplify vaccine schedule | 6 (3) | Give varicella and Pediacel during the same visit for 15–18 months old instead of 2 separate office visits. Give the 4–6 year-old vaccines at the same time as flu vaccine. |
| Centralized immunization record | 4 (2) | Centralize the immunization data (should have already been done years ago, would be really helpful about now), so everybody knows accurately where they stand re: vaccines. Nobody should have to call a doctor’s office to “find out” if their vaccines are up to date. |
| Total number of comments | 189 (40)** |
Percentages were calculated based on number of free text comments received for this question.
Percentage was calculated based on the total of survey respondents.
4. Discussion
This survey study aimed to evaluate and quantify the impact of the COVID-19 pandemic on childhood immunization practices in Canada and to identify the possible practitioner-level predictors of this impact. Our findings can further inform the implementation of policies to mitigate a decrease in immunization coverage during future waves of the COVID-19 pandemic and avoid a potential surge of VPDs later on.
In our study, close to half of the participating physicians reported a negative impact of the COVID-19 pandemic on their immunization services, with a few HCP even postponing all of their patients’ vaccines. Other provinces in Canada have also described similar interruptions to vaccination services, including in Alberta, where a 20-per-cent decline in overall vaccinations between March and April 2020 has been reported in the city of Calgary [11], [12]. A pan-Canadian environmental scan involving key informant structured interviews with public health leaders between August-October 2020 has also revealed that all provinces had changes to their routine immunization programs during the early stages of the pandemic, with programs being affected to varying degrees. School immunization programs have been most affected by these disruptions, with a few Canadian provinces or territories also experiencing temporary suspension of infant and preschool programs, particularly in the regions with highest COVID-19 incidence [20]. These disruptions to immunization services are aligned with trends seen in other countries [21], [22]. An international pulse poll aiming to better characterize disruptions to immunization globally in May 2020 was conducted by the World Health Organization, Gavi and UNICEF. Of the 65 surveyed countries, seven countries (11%) reported a complete interruption of their immunization program, and 38 countries (58%) reported a partial disruption [22]. Fortunately, three quarters of respondents have also indicated that catch-up plans were being implemented, with main topics of guidance addressing specific safety procedures to carry out routine immunization sessions, decision-making considerations and dissemination of educational messages to the community [22].
In Canada, some of the solutions to the disruption of immunization services that have been implemented since the beginning of the pandemic have included additional clinics for immunization services, reorganization of patient flow with shortened appointment times and opportunistic immunization at other appointments, guidance documents on immunization services during the pandemic and public health released communications for HCP [20]. Many of these strategies are aligned with the findings from our survey, with respondents suggesting a reorganisation of patient flow, patient screenings, centralized guidance documents and dedicated centers or practices for vaccination in order to maintain immunization services for children. In addition, most respondents have highlighted the importance of support programs to access PPE in order to continue to safely provide vaccines. A majority of respondents acknowledged that they do not have a system in place allowing them to keep track of patients that may have missed immunization doses, which causes significant challenges in planning catch-up immunization schedules. The implementation of a universal centralized electronic immunization record in Ontario could facilitate the identification of immunity gaps and the organization of catch-up programs [23]. The experience from the COVID-19 vaccination campaign should be leveraged and the COVID-19 immunization electronic record could be expanded to the other publicly funded immunizations. Parental concerns about contracting COVID-19 in healthcare settings were also identified as the most significant barrier to immunization services for children; therefore, public health units and governmental bodies should invest in education campaigns for parents with a focus on vaccine effectiveness and the safety of getting vaccines in healthcare settings. Parents and patients should be informed that measures aiming to mitigate the transmission of COVID-19 have been implemented and that benefits from vaccination outweigh the minimal risks of contracting COVID-19 in healthcare settings.
In Ontario, prior to the COVID-19 pandemic, immunization coverage estimates remained below the 2025 Canadian national goal of 95% coverage of a regimen of five doses of DTaP, four doses of polio vaccine and two doses of measles, mumps and rubella vaccine by seven years of age. For the 2018–2019 school year, coverage of a two-doses regimen of the measles vaccine was estimated at 86.6% in seven-year-old children throughout Ontario, with a few areas of the province reporting a vaccination coverage as low as 50% [24]. Because of the highly contagious nature of the measles virus, near-perfect vaccination coverage (herd immunity of 93–95%) is required to effectively protect against a resurgence of measles [25]. Public health units with a measles coverage below 80% should therefore further emphasize public messaging around the importance of maintaining routine childhood immunizations during the pandemic and implement previously discussed strategies to avoid sustained disruption in immunizations that may translate into future measles outbreaks. Fortunately, there have been no cases of measles or increase in VPDs reported by Public Health Ontario in 2020 compared to previous years [26]. Moreover, there has been a significant decrease in non-SARS-CoV-2 respiratory viruses throughout Canada during the 2020–21 season compared to previous seasons, with a virtual absence of influenza detection [27]. Although increased demand for influenza vaccines was reported at the start of the season, the Canadian Seasonal Influenza Immunization Coverage Survey has reported similar vaccine coverage compared to the 2019–20 season, at 32% among adults aged 18 to 64 years throughout Canada [28], [29]. The stability of this estimate indicates that strategies to mitigate disruption in immunization services during the second wave of the COVID-19 pandemic may have been successfully implemented, and that the observed decline in communicable diseases other than COVID-19 is most likely secondary to the indirect impact from public health measures aiming to mitigate the spread of COVID-19. However, as physical distancing measures and travel restrictions are lifted, the possibility of a delayed surge of VPDs in cohorts of under-vaccinated children needs to be closely monitored.
Our study also found that the immunization services provided by pediatricians, as well as HCP from urban settings and the ones who have been in practice for a shorter period of time, were significantly more impacted by the pandemic. While this may inform which HCP should be preferentially supported in their efforts to continue providing immunizations to children, our study did not explore the possible reasons behind these findings. In Ontario, given that a substantial proportion of COVID-19 cases have been diagnosed in populous cities, it is not surprising that urban settings would be more impacted than suburban or rural settings. On the other hand, the reasons for preferential negative impact on pediatricians and early-career physicians immunisation practice are unknown. Previous studies have found that more recently graduated physicians had decreased odds of believing vaccines are efficacious and safe compared to graduates from a previous 5-year period, and it is possible that some recent graduates did not prioritise immunisation visits as much as their more experienced colleagues did. It is also possible that early-career physicians had been redeployed to other clinical tasks related to the COVID-19 pandemic more frequently than their more senior colleagues, which could have impacted their immunization practices [30].
Our study has several limitations. First, the low response rate and the potential introduction of selection bias due to the convenience sampling of respondents can limit the external validity and generalizability of our study results. Additionally, practice size and the number of children seen in each practice was not collected from the survey respondents, which limits the quantification of the impact on vaccine coverage at a population-level. Also, while physicians represent a substantial proportion of the HCP providing vaccines to children in Ontario, we have not evaluated the impact on the immunization services provided by nurse practitioners, nurses, and pharmacists. Lastly, in view of the cross-sectional nature of the study, we were only able to capture the immunization practices of physicians within a limited timeframe during the first wave of the COVID-19 pandemic, well before vaccines against COVID-19 were available.
5. Conclusion
Our survey study reports that COVID-19 has caused substantial modifications to physicians’ pediatric immunization services across Ontario in the initial wave of the pandemic, which suggests that there could be cohorts of under-vaccinated children at increased risk of VPDs when public health measures aiming to mitigate the transmission of COVID-19 are relaxed. The survey respondents have identified multiple solutions to maintaining childhood immunizations, including assistance in accessing personal protective equipment, dedicated centers or practices for vaccination, universal centralized electronic immunization records and education campaigns for parents. Concerted efforts by HCP, public health units and government bodies are required to ensure appropriate provision of routine childhood immunizations throughout the COVID-19 pandemic, catch-up of any missed vaccines, and education of parents and caregivers about the importance of maintaining vaccine coverage for their children.
Funding
This study was supported by a Creative Professional Activity grant from the Department of Paediatrics at The Hospital for Sick Children, Toronto.
CRediT authorship contribution statement
Pierre-Philippe Piché-Renaud: Conceptualization, Methodology, Data curation, Formal analysis, Funding acquisition, Writing - original draft. Catherine Ji: Conceptualization, Methodology, Funding acquisition, Resources, Writing - original draft. Daniel S. Farrar: Data curation, Formal analysis, Software, Writing - original draft. Jeremy N. Friedman: Conceptualization, Methodology, Funding acquisition, Writing - review & editing. Michelle Science: Conceptualization, Funding acquisition, Writing - review & editing. Ian Kitai: Conceptualization, Funding acquisition, Writing - review & editing. Sharon Burey: Resources, Writing - review & editing. Mark Feldman: Conceptualization, Methodology, Resources, Funding acquisition, Writing - review & editing. Shaun K. Morris: Supervision, Conceptualization, Methodology, Funding acquisition, Writing - review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [SKM has participated on an advisory board for Pfizer, is an investigator on an investigator-led project funded by Pfizer and received personal fees from GlaxoSmithKline outside the submitted work. SB, JNF, CJ, PPPR and MS are investigators on an investigator-led project funded by Pfizer outside of the submitted work.].
Acknowledgement
We would like to acknowledge all pediatricians and family physicians who participated in this survey study. We would also like to thank Robyn Neville-Kett from the Pediatricians’ Alliance of Ontario and the Department of Family and Community Medicine at the University of Toronto for their help with the distribution of the survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.05.094.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.WHO. Guiding principles for immunization activities during the COVID-19 pandemic: Interim Guidance. World Health Organization; March 26th, 2020.
- 2.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020 doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li H., Yu G., Duan H., Fu J., Shu Q. Changes in Children's Healthcare Visits During Coronavirus Disease-2019 Pandemic in Hangzhou. China J Pediatr. 2020;224:146–149. doi: 10.1016/j.jpeds.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffman J. Vaccine Rates Drop Dangerously as Parents Avoid Doctor’s Visits. [Cited 2020 August 18]; Available from: https://www.nytimes.com/2020/04/23/health/coronavirus-measles-vaccines.html.
- 5.Weill A., Drouin J., Desplas D., Cuenot F., Dray-Spira R., Zureik M. Usage des médicaments de ville en France durant l’épidémie de Covid-19 – point de situation après 5 semaines de confinement (jusqu’au 19 avril 2020) EPIPHARE - Groupement d’intérêt scientifique (GIS) ANSM-CNAM. 2020 [Google Scholar]
- 6.Santoli J.M., Lindley M.C., DeSilva M.B., et al. Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration — United States, 2020. MMWR Morb Mortal Wkly Rep. ePub. 2020 doi: 10.15585/mmwr.mm6919e2external. [DOI] [PubMed] [Google Scholar]
- 7.Suk J.E., Paez Jimenez A., Kourouma M., et al. Post-Ebola Measles Outbreak in Lola, Guinea, January-June 2015(1) Emerg Infect Dis. 2016;22(6):1106–1108. doi: 10.3201/eid2206.151652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wesseh C.S., Najjemba R., Edwards J.K., Owiti P., Tweya H., Bhat P. Did the Ebola outbreak disrupt immunisation services? A case study from Liberia. Public Health Action. 2017;7(Suppl 1):S82–S87. doi: 10.5588/pha.16.0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poudel A. Measles outbreaks reported in five districts including in Kathmandu and Lalitpur in last one month. [Cited 2020 August 18]; Available from: https://kathmandupost.com/national/2020/04/29/measles-outbreaks-reported-in-five-districts-including-in-kathmandu-and-lalitpur-in-last-one-month.
- 10.Médecins Sans Frontières. Measles is a steady, silent killer among COVID-19. [Cited 2020 August 18]; Available from: https://www.msf.org/measles-steady-silent-killer-among-covid-19.
- 11.Canadian Pediatric Society. Stick to immunization schedule during the COVID-19 pandemic, paediatricians urge. [Cited 2020 August 18]; Available from: https://www.cps.ca/en/media/stick-to-immunization-schedule-during-the-covid-19-pandemic.
- 12.Public Health Agency of Canada (PHAC). Interim guidance on continuity of immunization programs during the COVID-19 pandemic. [Cited 2020 September 7]; Available from: https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/interim-guidance-immunization-programs-during-covid-19-pandemic.html.
- 13.Jiang L., Tang K., Levin M., et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30651-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitano T., Kitano M., Krueger C., et al. The differential impact of pediatric COVID-19 between high-income countries and low- and middle-income countries: A systematic review of fatality and ICU admission in children worldwide. PLoS ONE. 2021;16(1):e0246326. doi: 10.1371/journal.pone.0246326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chanchlani N., Buchanan F., Gill P.J. Addressing the indirect effects of COVID-19 on the health of children and young people. CMAJ. 2020;192(32):E921–E927. doi: 10.1503/cmaj.201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ontario College of Pharmacists. Administering Injections. [Cited 2020 August 18]; Available from: https://www.ocpinfo.com/practice_resource/administering-injections/.
- 17.Singer E, Ye C. The Use and Effects of Incentives in Surveys. 2013;645(1):112-41
- 18.Guttmann A., Manuel D., Dick P.T., To T., Lam K., Stukel T.A. Volume matters: physician practice characteristics and immunization coverage among young children insured through a universal health plan. Pediatrics. 2006;117(3):595–602. doi: 10.1542/peds.2004-2784. [DOI] [PubMed] [Google Scholar]
- 19.Glazier R.H., Green M.E., Wu F.C., Frymire E., Kopp A., Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193(6):E200–E210. doi: 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sell H, Assi A, Driedger SM, et al. Continuity of routine immunization programs in Canada during the COVID-19 pandemic. 2021: 2021.03.22.21254121. [DOI] [PMC free article] [PubMed]
- 21.Harris R.C., Chen Y., Cote P., et al. Impact of COVID-19 on routine immunisation in South-East Asia and Western Pacific: Disruptions and solutions. Lancet Reg Health West Pac. 2021:100140. doi: 10.1016/j.lanwpc.2021.100140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO. Special feature: immunization and COVID-19. [Cited 2021 May 14]; Available from: https://www.who.int/immunization/monitoring_surveillance/immunization-and-covid-19/en/.
- 23.Wilson S.E., Quach S., MacDonald S.E., et al. Immunization information systems in Canada: Attributes, functionality, strengths and challenges. A Canadian Immunization Research Network study. Can J Public Health. 2017;107(6):e575–e582. doi: 10.17269/CJPH.107.5679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Public Health Ontario. Immunization Coverage Report for School Pupils in Ontario 2018–19 School Year. [Cited 2021 May 15]; Available from: https://www.publichealthontario.ca/-/media/documents/i/2020/immunization-coverage-2018-19.pdf?la=en.
- 25.Paules C.I., Marston H.D., Fauci A.S. Measles in 2019 - Going Backward. N Engl J Med. 2019;380(23):2185–2187. doi: 10.1056/NEJMp1905099. [DOI] [PubMed] [Google Scholar]
- 26.Public Health Ontario. Monthly Infectious Diseases Surveillance Reports. [Cited 2021 May 15]; Available from: https://www.publichealthontario.ca/en/data-and-analysis/infectious-disease/infectious-diseases-monthly.
- 27.Groves H, Piché-Renaud P, Peci A, et al. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada. 2021: 2021.04.15.21255591. [DOI] [PMC free article] [PubMed]
- 28.Global News. Demand for flu shot up 500% at Ontario pharmacies compared to 2019. [Cited 2021 May 15]; Available from: https://globalnews.ca/news/7434935/demand-up-500-per-cent-ontario-pharmacies-flu-shot.
- 29.Public Health Agency of Canada (PHAC). Flu (influenza): FluWatch surveillance. [Cited 2021 May 15]; Available from: https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance.html#a1.
- 30.Coughlan C., Nafde C., Khodatars S., et al. COVID-19: lessons for junior doctors redeployed to critical care. Postgrad Med J. 2020 doi: 10.1136/postgradmedj-2020-138100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.