To the Editor:
Several studies report independent associations between obstructive sleep apnea (OSA) and cardiovascular disease (CVD). However, doubt has recently been cast on the ability of continuous positive airway pressure (CPAP) to mitigate these risks, and the culpability of OSA in promoting CVD. Randomized clinical trials of CPAP versus usual care (The Sleep Apnea Cardiovascular Endpoints [SAVE] study, Randomized Intervention with Continuous Positive Airway Pressure in CAD and OSA, and Impact of Sleep Apnea syndrome in the evolution of Acute Coronary syndrome) found no difference in rates of CVD-related events or death. As others have elaborated, these trials must be interpreted in the context of the cohorts enrolled (nonsleepy patients in their early 60’s with preexisting CVD), poor CPAP adherence, and relatively small sample sizes with composite outcomes (1). Hopefully, future studies can address whether CPAP has a role in the primary prevention of CVD in symptomatic younger patients. In the meantime, can we predict which OSA patients are susceptible to long-term cardiovascular sequelae?
To address this question, some investigators are exploring hypoxia metrics other than traditional frequency-based parameters such as apnea–hypopnea index (AHI) or oxygen desaturation index. These novel metrics capture the depth and length of desaturations by integrating the area above the oxygen saturation as measured by pulse oximetry (SpO2) trace within respiratory events. Kulkas and colleagues calculated the area under the pre-event baseline of each SpO2 desaturation up to the hypoxic nadir. Summing these areas and dividing by sleep time yielded the desaturation severity parameter (2). Azarbarzin and colleagues developed a similar metric termed the hypoxic burden. Hypoxic burden used different methods to define event onset/offset and included the SpO2 resaturation phase (3). Chazal and colleagues developed the respiratory event desaturation transient area (REDTA) which scales the analysis window based on event length, and then integrates the area below 100% and above the SpO2 tracing (4). Hypoxic burden and REDTA predicted CVD in several cohorts, more consistently than, or after adjustment for AHI or other hypoxia metrics. Interestingly, hypoxic burden was associated with CVD in a French sleep clinic population, while daytime sleepiness (gaining popularity as an at-risk OSA phenotype) was not (5). Have we discovered the holy grail of OSA risk stratification?
It is tempting to conclude that hypoxic burden (or similar SpO2 integrals) are the “right” way to assess OSA-associated hypoxia. However, we should evaluate what additional information is gleaned by these metrics beyond the AHI or mean oxygen saturation. Consider two patients, both with AHI 30, yet different values of hypoxic burden. Studies from the 1980s examining determinants of O2 desaturation illuminate potential differences between these patients. Sériès and colleagues performed pulmonary function tests and PSGs in OSA patients and calculated the desaturation area (similar to the hypoxic burden with minor boundary differences) under the SpO2 curve after apneas (6). The most important predictor of desaturation area they identified was the supine expiratory reserve volume (ERV). Similarly, Strohl and Altose measured rates of SpO2 decline in healthy adults during breath-holding and apneas (7) under hypoxic conditions. Reduced pre-apnea SpO2 was a robust predictor of the rate of post–apnea SpO2 decline, demonstrating the importance of pulmonary oxygen stores. Taken together, abdominal obesity leads to low functional residual capacity, which 1) reduces baseline SpO2 and lung oxygen stores (affecting parameters such as T90%), and 2) predisposes to deeper desaturations during apneas (affecting parameters such as hypoxic burden). Moreover, reduced baseline SpO2 contributes to faster desaturations, due to the steeper slope of the oxyhemoglobin dissociation at lower partial pressures of oxygen.
This physiology has critical CVD implications. Patients with metabolic syndrome and increased visceral adipose tissue (VAT) are at high risk for CVD, more so than BMI-matched persons with greater subcutaneous fat mass. Adipocytes in VAT are more lipolytically active and secrete more proinflammatory cytokines than those in subcutaneous fat. In addition, individuals with increased VAT are prone to airway obstruction because of fat accumulation in the neck and tongue. Additional increases in abdominal VAT further decrease lung volumes, leading to faster O2 desaturations. Therefore, associations between hypoxic burden or REDTA and CVD (3–5) may be mediated, at least in part, by visceral obesity. In an analysis of Sleep Heart Health Study data, Butler and colleagues surprisingly found that shorter event duration was associated with mortality (8). While authors interpreted this finding to reflect low arousal threshold, another explanation is worth considering. Patients with the shortest events would tend to have the most rapid O2 desaturation. In their analysis, these patients were more obese than those with longer respiratory events.
How should effects of VAT on lung function be accounted for in OSA studies? Ideally, we should use gold-standard methods such as CT scanning to quantify fat mass and distribution. However, these techniques are costly and require radiation exposure. As a result, most OSA-CVD association studies rely on body mass index (BMI) or waist circumference to “adjust for” the cardiovascular effects of obesity. Unfortunately, BMI correlates poorly with VAT mass, and it crudely predicts reductions in ERV. For example, in a community cohort, the coefficient of variation in ERV rose from 30 to 75% as BMI increased from 20 to >40 kg/m2 (9). Waist circumference, a composite metric of subcutaneous and visceral abdominal fat, outperforms BMI in predicting CVD risk, but its relation to VAT varies with age, sex, and race (10). Thus, VAT mass and lung volumes are important sources of unmeasured confounding that must be acknowledged in hypoxic burden-CVD associations.
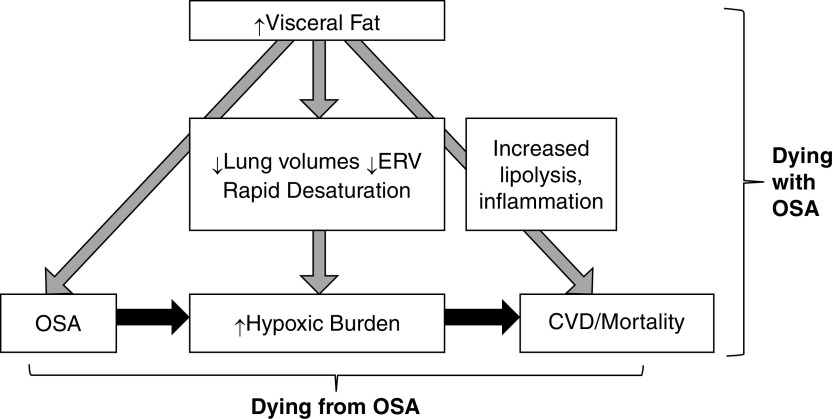
The point of this discussion is not to malign hypoxic burden or related metrics which carry prognostic information for populations with OSA. However, we cannot conclude that hypoxic burden is the cause of adverse outcomes until we have appropriately addressed the factors that contribute to its magnitude. We should maintain equipoise about whether patients are succumbing to complications of visceral obesity (dying with OSA), exposure to hypoxia when asleep (dying from OSA) or a combination of the two problems (Figure 1). This is a question with practical implications, since CPAP resolves hypoxic burden, but does not decrease harmful metabolic impacts of visceral adiposity. In research contexts, we advocate for acquiring lung volumes and fat distribution imaging to account for effects of VAT on pulmonary function and CVD, respectively. In clinical settings, we should recognize that a high hypoxic burden marks a patient who likely requires weight loss (not just CPAP use) to attenuate CVD risk.
Figure 1.
Schematic demonstrating how patients with obstructive sleep apnea (OSA) could be dying with OSA or from OSA. OSA induces hypoxemia, which, in turn, could contribute to mortality. On the other hand, this pathway may be confounded by the presence of visceral obesity. Visceral fat 1) predisposes to OSA, 2) decreases lung volumes, particularly expiratory reserve volume, leading to greater hypoxic burden, and 3) promotes cardiovascular disease and mortality. CVD = cardiovascular disease; ERV = expiratory reserve volume.
Footnotes
Supported by National Institutes of Health grant R01HL135483.
Originally Published in Press as DOI: 10.1164/rccm.202206-1052LE on August 8, 2022
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Javaheri S, Martinez-Garcia MA, Campos-Rodriguez F. CPAP treatment and cardiovascular prevention: we need to change the design and implementation of our trials. Chest . 2019;156:431–437. doi: 10.1016/j.chest.2019.04.092. [DOI] [PubMed] [Google Scholar]
- 2. Kulkas A, Tiihonen P, Eskola K, Julkunen P, Mervaala E, Töyräs J. Novel parameters for evaluating severity of sleep disordered breathing and for supporting diagnosis of sleep apnea-hypopnea syndrome. J Med Eng Technol . 2013;37:135–143. doi: 10.3109/03091902.2012.754509. [DOI] [PubMed] [Google Scholar]
- 3. Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J . 2019;40:1149–1157. doi: 10.1093/eurheartj/ehy624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Chazal P, Sadr N, Dissanayake H, Cook K, Sutherland K, Bin YS, et al. Predicting cardiovascular outcomes using the respiratory event desaturation transient area derived from overnight sleep studies. Annu Int Conf IEEE Eng Med Biol Soc . 2021;2021:5496–5499. doi: 10.1109/EMBC46164.2021.9630610. [DOI] [PubMed] [Google Scholar]
- 5. Trzepizur W, Blanchard M, Ganem T, Balusson F, Feuilloy M, Girault JM, et al. Sleep apnea-specific hypoxic burden, symptom subtypes, and risk of cardiovascular events and all-cause mortality. Am J Respir Crit Care Med . 2022;205:108–117. doi: 10.1164/rccm.202105-1274OC. [DOI] [PubMed] [Google Scholar]
- 6. Sériès F, Cormier Y, La Forge J. Role of lung volumes in sleep apnoea-related oxygen desaturation. Eur Respir J . 1989;2:26–30. [PubMed] [Google Scholar]
- 7. Strohl KP, Altose MD. Oxygen saturation during breath-holding and during apneas in sleep. Chest . 1984;85:181–186. doi: 10.1378/chest.85.2.181. [DOI] [PubMed] [Google Scholar]
- 8. Butler MP, Emch JT, Rueschman M, Sands SA, Shea SA, Wellman A, et al. Apnea-hypopnea event duration predicts mortality in men and women in the Sleep Heart Health Study. Am J Respir Crit Care Med . 2019;199:903–912. doi: 10.1164/rccm.201804-0758OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest . 2006;130:827–833. doi: 10.1378/chest.130.3.827. [DOI] [PubMed] [Google Scholar]
- 10. Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring) . 2011;19:402–408. doi: 10.1038/oby.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]