Abstract
Background: In the beginning of 2020, Italy was the first European country to face the COVID-19 outbreak. Restrictions imposed during the pandemic, social isolation, and the cancellation of medical appointments likely resulted in stress that may have affected pregnant women adversely.
Aims: To determine the psychometric validity of the Italian version of the Pandemic-Related Pregnancy Stress Scale (PREPS) in assessing COVID-19-related stress in pregnant women and to examine correlations between PREPS scales and symptoms of anxiety and depression.
Methods: 232 pregnant women attending the Obstetric-Gynecologic Clinic of an Academic Hospital were assessed with the PREPS, the Revised Prenatal Distress Questionnaire (NuPDQ), the General Anxiety Disorder-7 (GAD-7), and the Patient Health Questionnaire-2 (PHQ-2). We analyzed the internal consistency and factor structure of the PREPS. Convergent validity was examined by comparison with the NuPDQ. PHQ-2 and GAD-7 were used to measure the association with depression and anxiety.
Results: Acceptable-to-good internal consistency was found for the three PREPS scales: Preparedness Stress (PS, α=0.760), Prenatal Infection Stress (PIS, α=0.857), and Positive Appraisal (PA, α=0.747). Correlations of the NuPDQ with both PREPS stress scale scores (PS and PIS) were statistically significant, but on multiple regression analysis only the PS scale was correlated with the NuPDQ. Prenatal infection stress predicted GAD-7 score, while Preparedness stress predicted PHQ-2 score.
Limitations: The main limitations were the small sample size and the cross-sectional design of the study.
Conclusion: The Italian PREPS exhibited good psychometric properties and associations with clinical symptoms of anxiety and depression.
Keywords: COVID-19, Pregnancy, Prenatal stress, PREPS, Anxiety, Depression
1. Introduction
In the beginning of 2020, Italy was the first country in Europe to be affected by the coronavirus 2019 disease (COVID-19) outbreak. Fear of infection, financial concerns, and isolation during the COVID-19 pandemic have heightened stress (Li et al., 2020), especially in vulnerable groups, including older people, children, and pregnant women (Brooks et al., 2020). Pregnant women have experienced additional limitations during the pandemic, such as the alteration or cancellation of medical appointments (Caparros-Gonzalez and Alderdice, 2020; Preis et al., 2020a; Saccone et al., 2020). Moreover, there has been a lack of definitive evidence about whether the SARS-CoV-2 virus can lead to life-threatening conditions during pregnancy, or whether it increases the risk of preterm delivery or other adverse childbirth outcomes (Hantoushzadeh et al., 2020; Zaigham and Andersson, 2020). Uncertainty about the potential impacts of the virus on oneself and on one's unborn child, fear of contagion, disruption of prenatal care, financial strain, and social isolation derived from restrictions imposed to limit the spread of the virus have been major sources of stress for childbearing women throughout the world (Caparros-Gonzalez and Alderdice, 2020; Ravaldi et al., 2020; Thapa et al., 2020). Stress related to the pandemic may coexist with and exacerbate pregnancy-specific stress (PSS), which originates from physical and psychological changes that occur during pregnancy (Ibrahim and Lobel, 2020). PSS is a known contributor to adverse maternal and neonatal outcomes including low birth weight, preterm delivery, pre-eclampsia, gestational diabetes, and unplanned caesarean section (Alderdice et al., 2012; Lobel and Dunkel Schetter, 2016). To evaluate COVID-19 pandemic-related stress in pregnant women, Preis and colleagues developed the Pandemic-Related Pregnancy Stress Scale (PREPS), which assesses two types of pandemic-related sources of stress: lack of preparedness for childbirth, and fears of infection – as well as a type of pandemic-related resilience, labelled positive appraisal (Preis et al., 2020c). Recent studies confirm that the PREPS exhibits strong psychometric properties in American, Polish, and German women (Ilska et al., 2021; Preis et al., 2020c; Schaal et al., 2020).
The aim of our study was to validate the Italian version of the PREPS. To analyze its convergent validity, we examined the associations of the PREPS with reliable, valid pregnancy-specific stress measures that have been shown previously to perform well in Italian pregnant women (Penengo et al., 2020). Moreover, we also evaluated correlations of stress, assessed by the PREPS subscales, with symptoms of anxiety and depression measured with validated instruments. Both anxiety and depression are known to be correlated with fear of childbirth (Dencker et al., 2019). We reasoned that during the COVID-19 pandemic, anxiety symptoms could be activated by fear of infection, and thus we hypothesized an association of the PREPS Infection scale with anxiety. In addition, because depressive symptoms often underlie low self-esteem (Orth and Robins, 2013), we hypothesized that depressive symptoms would be related to lack of confidence about one's ability to manage childbirth and postpartum as measured by the PREPS Preparedness scale.
2. Materials and method
2.1. Participants
The study was conducted between April 22nd and August 31st, 2020. We recruited 232 pregnant women who were receiving outpatient prenatal care at the Gynecology Clinic of the University Hospital of Udine. Inclusion criteria were current pregnancy, age over 18 years, and fluency in Italian language. All participants provided informed consent. The study was approved by the Medical Ethics Committee of Friuli Venezia Giulia region (CEUR-2018-Sper-027-ASUIUD).
2.2. Measures
Sociodemographic details and information about COVID-19 exposure and about pregnancy and prenatal care were collected via a questionnaire. It was organised in four sections (i.e., “Background Information”, with 17 questions; “COVID-19 Exposure”, 4 questions; “Your Pregnancy”, 11 questions; “Your Prenatal Care”, 7 questions). We also included an optional open-ended section about main concerns and resources in the face of the pandemic emergency (“Open-ended Prenatal and COVID-19 Concerns and Resilience Comments”, 2 questions). In addition, we administered the following self-report instruments:
PREPS: Pandemic-Related Pregnancy Stress Scale.
Preis et al. (2020c) developed and validated the Pandemic-Related Pregnancy Stress Scale (PREPS), an instrument designed to assess worries about preparedness for childbirth, concerns about COVID-19 infection, and positive appraisals of respondents in relation to being pregnant during the pandemic emergency. The PREPS includes 15 items rated on a five-point scale from 1 = “Very Little” to 5 = “Very Much”. The instrument consists of three subscales: PREPS-Preparedness Stress (PS), PREPS-Prenatal Infection Stress (PIS), and PREPS-Positive Appraisal (PA). The PS scale comprises seven items and evaluates the stress of feeling unprepared for childbirth or the postpartum due to the COVID-19 pandemic. The PIS scale (five items) assesses stress related to fear of infection of the mother or the fetus (Preis et al., 2020b, 2020c). Lastly, the PA scale (three items) measures a perception of personal growth (e.g., “being pregnant is giving me strength during the pandemic”) and it may reflect a specific way of coping. Scores on each of the three scales were calculated by averaging item responses. The original American version of the PREPS exhibited good psychometric properties (Preis et al., 2020c), both in terms of model fit (RMSEA=0.07, CFI=0.93, and TLI=0.91) and of internal consistency (PS: α=0.81, PIS: α=0.86, and PA: α=0.68). In this study, we considered average item scores ≥4 to be high (i.e., corresponding to a mean response of “Much” or “Very Much”).
The PREPS questionnaire was translated literally into Italian and then back-translated to the English language. No modifications to wording were made.
NuPDQ: Revised Prenatal Distress Questionnaire.
Lobel and colleagues developed the NuPDQ (Ibrahim and Lobel, 2020; Lobel et al., 2008), a revised version of the Prenatal Distress Questionnaire (Yali and Lobel, 1999). The NuPDQ includes 17 items that assess pregnancy-specific stress (PSS). Each item is scored on a three-point scale from 0 (“Never”) to 2 (“Very Often”). Items are summed obtaining a total score ranging from 0 to 34. The validity of the Italian version of the NuPDQ has been previously established (Penengo et al., 2020). Based on a recent review of 37 studies conducted with the NuPDQ (Ibrahim and Lobel, 2020), the average scale score of the 17-item version is 11.92 ±6.52. In the present study, we therefore defined scores ≥18.44 as high (i.e., greater than 1 SD above the general mean).
GAD-7: General Anxiety Disorder-7.
The GAD-7 assesses anxiety symptoms over the past two weeks. There are seven questions with response options ranging from 0 = “Not at All” to 4 = “Nearly Every Day” (Spitzer et al., 2006). The scale is considered an appropriate tool to measure anxiety in pregnancy. A total score equal to or greater than 7 has a sensitivity of 73.3% and specificity of 67.3% in detecting GAD in pregnant women (Zhong et al., 2015).
PHQ-2: Patient Health Questionnaire.
The PHQ-2 is a brief depression screening tool that assesses the frequency of major depressive disorder core symptoms (anhedonia and depressed mood) over two previous weeks. It consists of the first two items from the parent version, the PHQ-9. For each item, there are four possible responses: “Not at All”, “Several Days”, “Over Half the Days” and “Nearly Every Day”, which correspond to 0, 1, 2, and 3 points, respectively (Kroenke et al., 2003; Spitzer et al., 1999). Item responses are summed with a cut-off for depression defined as a score equal to or greater than 3. The PHQ-2 performs well as an initial screening of depression (Mitchell et al., 2016).
2.3. Data analysis
Means, medians, standard deviations, and interquartile ranges were calculated for continuously distributed measures. For categorical measures, frequencies and percentages were calculated.
Cronbach's coefficient alpha (ɑ) with a 95% confidence interval (CI) was used to estimate the internal consistency of PREPS scales, defined as acceptable when ɑ≥0.6 and good when ɑ≥0.8. The PREPS measurement model was tested using confirmatory factor analysis (CFA), with the diagonally weighted least squares estimator, suitable for five-level ordinal items, and a robust test. To test the goodness of fit of the model, χ2 and degrees of freedom (df), the root mean square error of approximation (RMSEA) with 90% CI, the comparative fit index (CFI), and Tucker-Lewis’ index (TLI) were calculated. Model fit was considered adequate with a χ2 to df ratio <2, an RMSEA ≤0.050, a CFI ≥0.950, and a TLI ≥0.090.
Pearson's product-moment correlation coefficients (r) were calculated to analyze the convergent validity and clinical correlates of PREPS scales. Also, Pearson's partial correlations (rP) were calculated to assess whether a single scale could account for the clinical associations of the PREPS scales.
All analyses were conducted using R-4.0.3 (R Development Core Team, 2021), and Lavaan 0.6-7 was used to conduct CFA (Rosseel, 2012).
3. Results
3.1. Sample characteristics
Of the 232 participants, 155 had a low-risk pregnancy, 77 had a high-risk pregnancy. Moreover, 135 women were in early pregnancy (first or second trimester), 97 were in late pregnancy (third trimester). One hundred and ten women were recruited in the first phase of the pandemic (between April and May 2020) and 122 in the second phase (between July and August 2020).
Sociodemographic and general characteristics of the sample are reported in Table 1 , together with participants’ scores on study instruments. The mean age of participants was 32.3 ±5.13 years, 36.1% of the sample lived in towns of more than 50,000 inhabitants, and 87.9% had access to the outdoors during the period of pandemic-related movement restrictions. About three-quarters of the sample (73.5%) reported having a planned pregnancy. Given the organization of Health Services in Italy, all participants received prenatal care from a general/family practitioner (at women's discretion) and an obstetrician (carried out usually every three months, or more frequent for high-risk pregnancies) during pregnancy. At the time of the research assessment, 48.4% of the participants had had a prenatal care appointment in the current week, 41.1% in the current month, and 5.5% two or more months before. About one-fifth of the sample (19.6%) reported having used online assistance during the pandemic (i.e., prenatal classes or courses, group therapies, and prenatal care appointments). Only two women were diagnosed with COVID-19, and another eight had indirect contact with infected people.
Table 1.
Total sample (N=258). Sample description.
| Measure | Count (%) / M ±SD; Md (IQR) |
| Age in years | 32.3 ±5.13; 33.0 (7.0) |
| Education in years | 15.1 ±3.62; 16.0 (5.0) |
| Current financial status: | |
| Below average | 29 (13.0%) |
| Average | 185 (83.0%) |
| Above average | 9 (4.0%) |
| Lost income due to COVID-19 | 71 (31.4%) |
| Employment status: | |
| Currently employed | 176 (76.5%) |
| Not employed | 38 (16.5%) |
| Student | 5 (2.2%) |
| Stable relationship | 229 (99.6%) |
| Number of children | 0.6 ±0.69; 0.0 (1.0) |
| High-risk pregnancy | 77 (33.2%) |
| Late pregnancy (3rd trimester) | 97 (41.8%) |
| NuPDQ | |
| Score | 11.6 ±5.07; 11.0 (7.0) |
| High (≥18.4) | 22 (9.9%) |
| PREPS – Preparedness Stress | |
| Score | 2.9 ±0.84; 2.9 (1.1) |
| High (≥ 4) | 21 (9.1%) |
| PREPS – Prenatal Infection Stress | |
| Score | 2.5 ±1.03; 2.6 (1.8) |
| High (≥ 4) | 23 (9.9%) |
| PREPS – Positive Appraisal score | 2.2 ±1.05; 2.0 (1.7) |
IQR: Interquartile range; M: Mean; Md: Median; NuPDQ: Revised Prenatal Distress Questionnaire; PIS: PREPS, Perinatal Infection Stress scale; PREPS: Pandemic-Related Pregnancy Stress Scale; PS: PREPS, Preparedness Stress scale; SD: Standard deviation.
3.2. Internal consistency
Acceptable-to-good internal consistency was found for the PS (α=0.760, 95% CI: [0.706; 0.803]), PIS (α=0.857, 95% CI: [0.823; 0.885]), and PA (α=0.747, 95% CI: [0.667; 0.810]) scales.
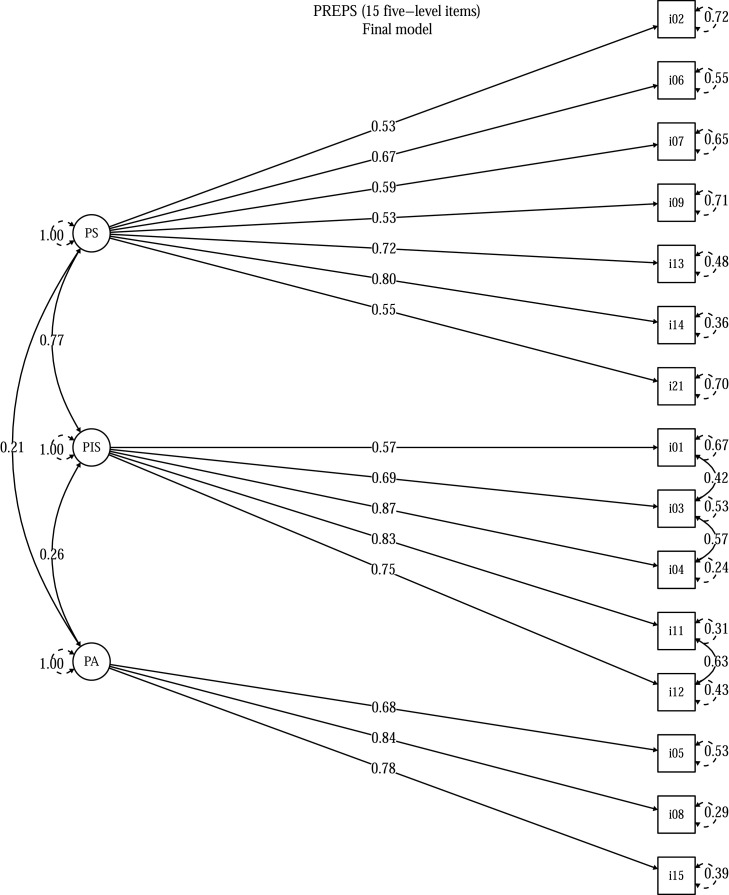
The proposed measurement model of the PREPS for the original English version (Preis et al., 2020b, 2020a, 2020c) was generally confirmed in the Italian sample, with minimal adjustment. All the items loaded on their expected factor. Correlated factors were considered, and some significant inter-item correlations were allowed (all within the PIS factor), obtaining a model with adequate fit: χ2 84=153.85 (χ2/df: 1.83), RMSEA=0.060 (90% CI: [0.045, 0.075], p(RMSEA≤0.050)=0.133), CFI=0.991, TLI=0.989. The adjusted model is displayed in Fig. 1.
Fig. 1.
Confirmatory factor analysis for the PREPS measurement model. PA: PREPS, Positive Appraisal scale; PIS: PREPS, perinatal infection stress scale; PREPS: Pandemic-Related Pregnancy Stress Scale; PS: PREPS, Preparedness Stress scale.
3.3. Convergent validity
Convergent validity of the PREPS stress scales (i.e., PS and PIS) was evaluated considering the correlations of each scale with the NuPDQ score. The correlations of PS with NuPDQ (r=+0.437, p<0.001) and of PIS with NuPDQ (r=+0.341, p<0.001) were moderate and statistically significant, whereas PA was uncorrelated with NuPDQ (r=+0.048, p=0.479). See Table 2 for details. After adjusting for the PS scale, the association between PIS and NuPDQ was no longer statistically significant (rP=+0.113, p=0.093), while the association between NuPDQ and PS remained significant (rP=+0.310, p<0.001) after controlling for PIS.
Table 2.
Pearson's bivariate correlations between scales (with their 95% confidence intervals in square brackets) and corresponding statistical significance.
| PS | +0.437 *** [+0.324, +0.537] | ||||
| PIS | +0.341 *** [+0.219, +0.452] | +0.591 *** [+0.500, +0.669] | |||
| PA | +0.048 ns [-0.084, +0.178] | +0.150 * [+0.021, +0.273] | +0.182 ** [+0.055, +0.304] | ||
| GAD-7 | +0.431 *** [+0.316, +0.533] | +0.251 *** [+0.123, +0.371] | +0.263 *** [+0.136, +0.382] | -0.030 ns [-0.161, +0.103] | |
| PHQ-2 | +0.397 *** [+0.280, +0.503] | +0.226 *** [+0.099, +0.347] | +0.204 ** [+0.075, +0.326] | +0.076 ns [-0.056, +0.204] | +0.604 *** [+0.513, +0.682] |
| NuPDQ | PS | PIS | PA | GAD-7 |
GAD-7: General Anxiety Disorder, 7 items questionnaire; NuPDQ: Revised Prenatal Distress Questionnaire; PA: PREPS, Positive Appraisal scale; PHQ-2: Patient Health Questionnaire, 2-item questionnaire; PIS: PREPS, Perinatal Infection Stress scale; PREPS: Pandemic-Related Pregnancy Stress Scale; PS: PREPS, Preparedness Stress scale. * = p<0.05, ** = p<0.01, *** = p<0.001, ns = not significant.
3.4. Clinical correlates
The PREPS PS and PIS stress scales were correlated with GAD-7 (respectively: r=+0.251, p<0.001; r=+0.263, p<0.001) and with PHQ-2 (r=+0.226, p<0.001; r=+0.204, p=0.002) scores. The PA scale was uncorrelated with the clinical scores (GAD-7: r=-0.030, p=0.663; PHQ-2: r=+0.076, p=0.259). See Table 2 for details.
After adjusting for the PIS scale, the association between PS and GAD-7 was no longer statistically significant (rP=+0.126, p=0.063), while the association between GAD-7 and PIS remained significant (rP=+0.150, p=0.027) after controlling for the PS scale. In contrast, after adjusting for the PS scale, the association between PIS and PHQ-2 was no longer statistically significant (rP=+0.092, p=0.169), while the association between PHQ-2 and PS remained significant (rP=+0.136, p=0.042) after adjusting for the PIS scale.
4. Discussion
The main goal of this study was to translate the PREPS for Italian-speaking women and to evaluate its psychometric properties. Results confirmed that the factor structure of the PREPS established in its American (RMSEA=0.07, CFI=0.93, TLI=0.91) (Preis et al., 2020c), German (RMSEA=0.073, CFI=0.920, TLI=0.902) (Schaal et al., 2020), and Polish (RMSEA=0.054, CFI=0.979, TLI=0.974) (Ilska et al., 2021) versions, also fit well in the Italian sample. Moreover, in the Italian version of the PREPS, the Preparedness Stress and Positive Appraisal scales exhibited acceptable internal consistency; the Infection Stress scale had good internal consistency. These results are in line with those found for the American (PS α=0.81, PIS α=0.86, PA α=0.68) (Preis et al., 2020c), Polish (PS α=0.824, PIS α=0.882, PA α=0.691) (Ilska et al., 2021), and German (PS α=0.81, PIS α=0.86, PA α=0.71) (Schaal et al., 2020) versions of the PREPS.
Both PREPS stress scales were individually correlated with pregnancy-specific stress as operationalized by the NuPDQ score, however, the model analyzing the independent contribution of all three PREPS scales found that PSS was associated with Preparedness stress but not with Prenatal infection stress and Positive appraisal. This pattern of findings resembles results observed in previous validation studies (Preis et al., 2020c; Schaal et al., 2020). In other words, in our sample, during the COVID-19 pandemic, pregnancy stress was related more strongly to practical concerns, such as not being able to receive sufficient help, being alone at delivery, or even being separated from the baby, than to fear of contracting an infection. This type of information is particularly useful in devising an effective intervention, for example, assuring a pregnant woman that her system of care during pregnancy continues to function despite the difficulties caused by the pandemic.
When considering the overall prevalence of stress in our sample, 9% of pregnant women reported high levels of Preparedness Stress and Prenatal Infection Stress. Schaal et al. (2020) found a similar prevalence of high stress of each type in their study of pregnant German women. In contrast, Preis et al. (2020c) reported a greater prevalence of COVID-19 related stress (27.2% and 29.1% for Preparedness Stress and Prenatal Infection Stress, respectively) among women in the US. It is possible that women in the US experienced higher pandemic-related stress than women from countries such as Italy and Germany with a nationalized health care system, assuring prenatal care and childbirth services for all, unlike the US (Boelig et al., 2020). Substantial civic unrest in the US since the emergence of COVID-19 may also have contributed to higher stress among pregnant American women.
As to the clinical correlates of stress related to the pandemic, our hypotheses were confirmed. Anxiety symptoms were related to fear of infection, whereas depressive symptoms were correlated with feeling unprepared for childbirth and for management of the puerperium. This could indicate that anxiety is directly related to an imminent uncontrollable danger such as infection damage, whereas depression may be related to feelings of personal insufficiency or abandonment while facing difficulties generated by the pandemic. The PREPS appears to capture the different sources of distress experienced by pregnant women and their association with anxiety and depression (Colli et al., 2021).
The main limitations of this study are its sample size and geographic homogeneity. These are attributable to the recruiting method we used: we enrolled only women who were attending prenatal care at a single site. This may also be a strength of the study, however, because in-person data collection eliminates some of the well known problems that can arise in online surveys, such as the inability to verify the status of respondents. Another limitation is the study's cross-sectional design; thus it was not possible to evaluate the test-retest reliability of the PREPS nor to ascertain the direction of association among variables. Moreover, a strength of the study is that it included women with high and low-risk pregnancies, women in various stages of pregnancy, and at different time periods during the pandemic, increasing the generalizability of results across these factors.
5. Conclusions
The Italian version of the PREPS has good psychometric properties. It is a reliable and valid instrument to evaluate worries about childbirth and postpartum, fear of infection, and to assess positive appraisal during the COVID-19 pandemic. Moreover, it enables identification of specific aspects of stress that are associated with anxious and depressive symptoms. Future studies are needed to investigate the impact of pandemic-related stress on pre- and post-natal outcomes (e.g., childbirth outcomes, maternal mental health, mother-newborn attachment, and infant development and health). The PREPS is a valuable tool that can be used to identify pregnant women who are experiencing high stress due to the COVID-19 pandemic and to aid in developing and tailoring targeted, effective interventions and treatments.
Funding
This research was not funded by agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
All procedures performed in this study involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. Approval for use of study assessment tools in pregnant women was granted by the Medical Ethics Committee of Friuli Venezia Giulia region (CEUR-2018-Sper-027-ASUIUD). Written informed consent was obtained from all participants included in the study.
Author statement
We confirm that this manuscript is the authors’ original work, and it has not been published elsewhere and is not under consideration by another journal.
All authors have approved the final manuscript and they agree with its submission to Journal of Affective Disorders.
All authors declare that they have no conflicts of interest.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgement
None.
References
- Alderdice F., Lynn F., Lobel M. A review and psychometric evaluation of pregnancy-specific stress measures. J. Psychosom. Obstet. Gynecol. 2012;33:62–77. doi: 10.3109/0167482X.2012.673040. [DOI] [PubMed] [Google Scholar]
- Boelig R.C., Saccone G., Bellussi F., Berghella V. MFM guidance for COVID-19. Am. J. Obstet. Gynecol. MFM. 2020;2:1–5. doi: 10.1016/j.ajogmf.2020.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caparros-Gonzalez R.A., Alderdice F. The COVID-19 pandemic and perinatal mental health. J. Reprod. Infant Psychol. 2020;38:223–225. doi: 10.1080/02646838.2020.1786910. [DOI] [PubMed] [Google Scholar]
- Colli C., Penengo C., Garzitto M., Driul L., Sala A., Degano M., Preis H., Lobel M., Balestrieri M. Prenatal stress and psychiatric symptoms during early phases of the COVID-19 pandemic in Italy. Int. J. Womens Health. 2021;2021:13:653–662. doi: 10.2147/IJWH.S315467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dencker A., Nilsson C., Begley C., Jangsten E., Mollberg M., Patel H., Wigert H., Hessman E., Sjöblom H., Sparud-Lundin C. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. 2019;32:99–111. doi: 10.1016/j.wombi.2018.07.004. [DOI] [PubMed] [Google Scholar]
- Hantoushzadeh S., Shamshirsaz A.A., Aleyasin A., Seferovic M.D., Aski S.K., Arian S.E., Pooransari P., Ghotbizadeh F., Aalipour S., Soleimani Z., Naemi M., Molaei B., Ahangari R., Salehi M., Oskoei A.D., Pirozan P., Darkhaneh R.F., Laki M.G., Farani A.K., Atrak S., Miri M.M., Kouchek M., Shojaei S., Hadavand F., Keikha F., Hosseini M.S., Borna S., Ariana S., Shariat M., Fatemi A., Nouri B., Nekooghadam S.M., Aagaard K. Maternal death due to COVID-19. Am. J. Obstet. Gynecol. 2020;223:109. doi: 10.1016/j.ajog.2020.04.030. .e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim S.M., Lobel M. Conceptualization, measurement, and effects of pregnancy-specific stress: review of research using the original and revised prenatal distress questionnaire. J. Behav. Med. 2020;43:16–33. doi: 10.1007/s10865-019-00068-7. [DOI] [PubMed] [Google Scholar]
- Ilska M., Kołodziej-Zaleska A., Brandt-Salmeri A., Preis H., Lobel M. Pandemic-related pregnancy stress assessment–Psychometric properties of the Polish PREPS and its relationship with childbirth fear. Midwifery. 2021;96 doi: 10.1016/j.midw.2021.102940. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The patient health questionnaire-2 validity of a two-item depression screener. Med. Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of covid-19 epidemic declaration on psychological consequences: a study on active weibo users. Int. J. Environ. Res. Public Health. 2020;17:1–9. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobel M., Cannella D.L., Graham J.E., DeVincent C., Schneider J., Meyer B.A. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008;27:604–615. doi: 10.1037/a0013242. [DOI] [PubMed] [Google Scholar]
- Lobel M., Dunkel Schetter C. In: 2nd Ed. Friedman Howard S., editor. Vol. 3. Elsevier; 2016. Pregnancy and prenatal stress; pp. 318–329. (Encyclopedia of Mental Health). [Google Scholar]
- Mitchell A.J., Yadegarfar M., Gill J., Stubbs B. Case finding and screening clinical utility of the patient health questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open. 2016;2:127–138. doi: 10.1192/bjpo.bp.115.001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orth U., Robins R.W. Understanding the link between low self-esteem and depression. Curr. Dir. Psychol. Sci. 2013;22:455–460. doi: 10.1177/0963721413492763. [DOI] [Google Scholar]
- Penengo C., Colli C., Garzitto M., Driul L., Cesco M., Balestrieri M. Validation of the Italian version of the revised prenatal coping inventory (NuPCI) and its correlations with pregnancy-specific stress. BMC Pregnancy Childbirth. 2020;20:1–14. doi: 10.1186/s12884-020-03159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the Coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM. 2020 doi: 10.1016/j.ajogmf.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc. Sci. Med. 2020;266:1–4. doi: 10.1016/j.socscimed.2020.113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Lobel M. Psychometric properties of the pandemic-related pregnancy stress scale (PREPS) J. Psychosom. Obstet. Gynecol. 2020;41:191–197. doi: 10.1080/0167482X.2020.1801625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team, 2021. R: a language and environment for statistical computing. R foundation for statistical computing.
- Ravaldi C., Wilson A., Ricca V., Homer C., Vannacci A. Pregnant women voice their concerns and birth expectations during the COVID-19 pandemic in Italy. Women Birth. 2020;1147:1–9. doi: 10.1016/j.wombi.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012;48:1–36. [Google Scholar]
- Saccone G., Florio A., Venturella R., De Angelis M., Bifulco G., Zullo F., Di Spiezio Sardo A. Psychological impact of coronavirus disease 2019 in pregnant women. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajog. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaal N., La Marca-Ghaemmaghami P., Preis H., Mahaffey B., Lobel M., Castro R. The German version of the pandemic-related pregnancy stress scale: a validation study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;256:40–45. doi: 10.1016/j.ejogrb.2020.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W. Validation and utility of a self-report version of PRIME-MD. The PHQ Primary Care Study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Thapa S.B., Mainali A., Schwank S.E., Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet. Gynecol. Scand. 2020;99:817–818. doi: 10.1111/aogs.13894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yali A.M., Lobel M. Coping and distress in pregnancy: an investigation of medically high risk women. J. Psychosom. Obstet. Gynecol. 1999;20:39–52. doi: 10.3109/01674829909075575. [DOI] [PubMed] [Google Scholar]
- Zaigham M., Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020;99:823–829. doi: 10.1111/aogs.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q.Y., Gelaye B., Zaslavsky A.M., Fann J.R., Rondon M.B., Sánchez S.E., Williams M.A. Diagnostic validity of the generalized anxiety disorder - 7 (GAD-7) among pregnant women. PLoS One. 2015;10:1–17. doi: 10.1371/journal.pone.0125096. [DOI] [PMC free article] [PubMed] [Google Scholar]