Abstract
Objective
Quality of life (QoL) is inversely associated with alcohol misuse and is a key measure by which recovery from alcohol use disorder (AUD) might be assessed. Yet, the determinants of QoL are scarcely known. The authors examined three ways through which demographic characteristics, familial and early life factors, and psychopathology conferred risks for QoL, including unique direct effects, developmental pathways, and clinical risk Profiles.
Methods
Cross‐sectional data from 1095 adults (50.4% without AUD; 49.6% with AUD) who participated in the NIAAA Natural History Protocol from January 2015 to March 2022 were analyzed. Multivariable regressions, path analysis, and latent Profile analysis were conducted.
Results
AUD was uniquely associated with lower QoL, and adverse effects of child maltreatment history and psychopathology symptoms on QoL were of similar or larger magnitudes. Mediation analysis indicated family history of AUD and child maltreatment history were indirectly associated with lower QoL through higher attention‐deficit/hyperactivity disorder symptoms, higher depressive symptoms, and positive AUD diagnosis. Latent Profile analysis of an enriched set of clinical characteristics identified four latent Profiles capturing the full range of alcohol use behavior. Latent Profiles with greater severity of familial and early life factors, psychopathology, and problematic drinking showed dose‐response associations with lower levels of physical, psychological, social, and environment QoL.
Conclusions
A constellation of developmental and clinical characteristics disproportionately affects individuals with AUD and is negatively associated with QoL domains. To improve QoL, prevention and intervention need to target multiple factors, including history of child maltreatment, comorbid psychopathology, and problematic drinking itself.
Highlights
Quality of life can be conceptualized as a multidimensional construct, encompassing the domains of physical, psychological, social, and environment quality of life. This study showed multiple ways early life factors and clinical characteristics could individually and collectively confer risk for low quality of life across these four domains.
Early life and familial factors were indirectly associated with lower quality of life through heightened psychopathology symptoms and alcohol use disorder. Four latent Profiles that captured the severity of developmental and clinical characteristics were inversely associated with domains of quality of life. Developmental risk factors and clinical indicators underlying the latent Profiles should be assessed to inform case conceptualization in the treatment of alcohol use disorder.
Several demographic characteristics, including older age, male gender, other marital status, fewer years of education, and lower household income, were linked to increased risk of membership in latent Profiles with greater clinical severity. These findings could inform targeted prevention and intervention efforts among at risk populations and highlight the importance of investigating health disparities in the context of alcohol and quality of life research.
Misuse of alcohol is a major disease burden accounting for 5.3% of deaths and 5.1% of disability‐adjusted life years worldwide (1). Alcohol use disorder (AUD) is common, with 13.9% and 29.1% of U.S. adults meeting current (past 12 months) and lifetime diagnoses respectively (2). AUD is associated with medical, social, and economic consequences that negatively influence individuals' wellbeing and quality of life (QoL) (3, 4). Recently, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) has developed a new definition of recovery that incorporates indicators such as “improvements in physical and mental health, quality of life, and other dimensions of well‐being.” (5) Therefore, a better understanding of developmental and clinical characteristics associated with dimensions of QoL is needed to inform AUD prevention and treatment.
QoL is a multidimensional construct capturing fulfillment of basic human needs and satisfaction in various aspects of life (6). The World Health Organization (WHO) identified four domains of QoL, namely physical, psychological, social, and environment QoL (7). Longitudinal analyses of National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) revealed inverse associations between changes in alcohol consumption and mental health‐related QoL over time (8). Among individuals with AUD in the multisite Combined Pharmacotherapies and Behavioral Interventions (COMBINE) study, reductions in drinking were associated with improvements in all four QoL domains (9). Besides drinking behaviors, externalizing and internalizing psychopathology such as attention‐deficit/hyperactivity disorder (ADHD) (10, 11) and depressive symptoms (12, 13) are associated with lower QoL among adults. Despite these findings, the unique associations between AUD and QoL domains after adjusting for other clinical characteristics on QoL have rarely been tested.
The externalizing and internalizing pathways to AUD are well‐documented (14, 15, 16). Generally, the externalizing pathway to AUD reflects vulnerability in behavioral inhibition and a propensity toward sensation seeking (15), whereas the internalizing pathway to AUD highlights the roles of negative affect and coping motives for alcohol use (16). Meta‐analytic data support externalizing and internalizing psychopathology as developmental precursors of AUD (17). Family history of AUD and history of child maltreatment are linked to elevated risk for AUD (18, 19), and may be distal factors that initiate externalizing and internalizing pathways to AUD. In a large‐scale longitudinal study, U.S. adults with adverse childhood experiences had lower life satisfaction and psychosocial well‐being than those who did not (20). Among adult women, the inverse associations between child maltreatment and health‐related QoL were partially mediated by psychosocial factors such as sleep problems and depressive symptoms (21, 22). These studies suggest possible developmental pathways linking early life factors to multiple QoL domains via psychopathology and AUD.
The examination of developmental pathways to QoL can be further enriched by exploring within‐person co‐occurrence of familial and early life factors, psychopathology symptoms, and alcohol‐related behaviors using latent Profile analysis (LPA). LPA is a person‐centered approach that has been increasingly used to capture heterogeneity in psychosocial functioning among heavy drinkers in recovery (23, 24, 25), but none of the prior studies had incorporated familial and early life factors as indicators. Latent Profiles identified through a combination of these factors and psychopathology symptoms would reflect both co‐occurrence and severity of multiple clinical characteristics that could inform personalized case conceptualization and treatment planning. The cumulative adverse effects of clinical characteristics on QoL domains could also be effectively examined through these empirically derived latent Profiles, resolving potential multicollinearity issues due to high correlations among clinical variables.
The goal of this study was to examine three ways through which demographic characteristics, familial and early life factors, and psychopathology conferred risks for multidimensional QoL. First, the unique direct effects of predictors on QoL domains were assessed using standardized multivariable regressions. We hypothesized that AUD along with externalizing and internalizing psychopathology would be uniquely and most strongly associated with all four QoL domains. Second, developmental pathways linking familial and early life factors to QoL domains via psychopathology (ADHD symptoms, depressive symptoms, and AUD) were evaluated using path analysis. We hypothesized that psychopathology would mediate the effects of familial and early life factors on QoL. Third, clinical risk Profiles of an enriched set of clinical characteristics, including obsessive drinking, compulsive drinking, and alcohol problems, were assessed using the person‐centered approach of LPA. We hypothesized that latent Profiles with greater clinical severity would be associated with lower QoL and that demographic differences in latent Profile membership would reveal health disparities.
METHOD
Data Source and Study Sample
Data were drawn from 1095 adults who participated in the NIAAA Natural History Protocol from January 2015 to March 2022. The objective of the NIAAA Natural History Protocol (ClinicalTrials.gov Identifier: NCT02231840) was to examine a broad range of traits among individuals with or without alcohol use problems and determine their potential eligibility for other research protocols conducted at the NIH Clinical Center. The study sample covered the full range of alcohol use behavior, including 552 participants without AUD (50.4%) and 543 participants with AUD (49.6%). Of those with AUD, 185 participants did not seek inpatient treatment at NIAAA (16.9% of study sample; “non‐treatment AUD”), whereas 358 participants sought inpatient treatment at NIAAA (32.7% of study sample; “treatment AUD”). The study protocol was approved by the National Institutes of Health Institutional Review Board. All participants provided written informed consent and completed a standardized battery of assessments and questionnaires.
Measures
Demographic Characteristics. Participants self‐reported age, sex, race, ethnicity, marital status, years of education, and annual household income.
Familial and Early Life Factors. Family history of AUD was measured using the Family Tree Questionnaire (26). A density score was calculated based on proportion of first‐ and second‐degree relatives identified as having an alcohol problem. History of child maltreatment was assessed using the Childhood Trauma Questionnaire‐Short Form (CTQ‐SF), a screening instrument validated in normative and clinical samples (27). With 25 clinical items and 5 response options for each item, the possible child maltreatment scores ranged from 25 to 125 (Cronbach's alpha [α] = 0.94 in the current sample).
Psychopathology. ADHD symptoms were assessed using the 6‐item screener version of the WHO Adult ADHD Self‐Report Scale (α = 0.77 in the current sample) (28). Depressive symptoms were assessed using the Montgomery Åsberg Depression Rating Scale (α = 0.91 in the current sample) (29). Alcohol Use Disorder was assessed using the Structured Clinical Interview for DSM‐IV (36.6% of the sample, n = 401) or DSM‐5 (63.4% of the sample, n = 694) (30).
Alcohol‐Related Measures. Three additional alcohol‐related variables were included in the LPA. Obsessive drinking (α = 0.95 in the current sample) and compulsive drinking (α = 0.95 in the current sample) were measured using the Obsessive Compulsive Drinking Scale (31). Alcohol problems were measured using the 10‐item Alcohol Use Disorders Identification Test (α = 0.95 in the current sample) (32).
Quality of Life. The WHO Quality of Life‐BREF (WHOQOL‐BREF) is a multidimensional measure of QoL, assessing physical health (e.g., ability to get around and work capacity), psychological health (e.g., meaningful and enjoyable life), social relationships (e.g., friend support and personal relationships), and environment QoL (e.g., safety, money, living conditions, access to health services, and mode of transportation) (7). These four domains of QoL were assessed using 24 items. This multidimensional measure has excellent psychometric properties (33). The Cronbach's alphas for the subscales in the current sample were 0.83 for physical, 0.87 for psychological, 0.77 for social, and 0.86 for environment QoL. Higher subscale scores represent better QoL.
Data Analyses
Three analytic methods were applied in this study. First, multivariable regressions with demographic characteristics, familial and early life factors, psychopathology, and AUD as unique predictors. These variables were standardized with a mean of 0 and standard deviation of 1 (i.e., z‐scores) to examine the relative strengths of the predictors' associations with the four QoL domains. Second, indirect effects of early life factors on QoL domains were modeled using path analysis to test possible underlying mechanisms through psychopathology symptoms and AUD. Third, LPA was utilized to capture within‐person co‐occurrence of early life factors, psychopathology symptoms, and alcohol‐related variables. To determine the optimal number of Profiles, a series of 7 latent Profile models were specified and compared based on information criteria, likelihood‐based tests, and interpretability of latent Profiles (34). Latent Profile differences in QoL domains and demographic characteristics were then examined. Statistical analyses were conducted in Stata 17.0 and Mplus 8.4.
RESULTS
Individual characteristics for the overall sample and by AUD status are presented in Table 1. Participants with AUD were more likely to be male, Black/African American, had other marital status, had fewer years of education, and had lower household income than participants without AUD. Participants with AUD also reported higher family history of AUD, higher child maltreatment, higher ADHD and depressive symptoms, and lower physical, psychological, social, and environment QoL than participants without AUD.
TABLE 1.
Characteristics of the overall sample, and participants with and without AUD
| Overall Sample (N = 1095) | Participants without AUD (n = 552) | Participants with AUD (n = 543) | χ 2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |||
| Sex | ||||||||
| Female | 466 | 42.6 | 285 | 51.6 | 181 | 33.3 | 37.5 | <0.001 |
| Male | 629 | 57.4 | 267 | 48.4 | 362 | 66.7 | ||
| Race | ||||||||
| White | 489 | 44.7 | 242 | 43.8 | 247 | 45.5 | 12.3 | 0.002 |
| Black/African | 438 | 40.0 | 205 | 37.1 | 233 | 42.9 | ||
| Other | 168 | 15.3 | 105 | 19.0 | 63 | 11.6 | ||
| Ethnicity | ||||||||
| Not Hispanic/Latino | 999 | 91.2 | 501 | 90.8 | 498 | 91.7 | 0.31 | 0.578 |
| Hispanic/Latino | 96 | 8.8 | 51 | 9.2 | 45 | 8.3 | ||
| Marital status | ||||||||
| Single | 749 | 68.4 | 396 | 71.7 | 353 | 65.0 | 36.2 | <0.001 |
| Married | 213 | 19.5 | 121 | 21.9 | 92 | 16.9 | ||
| Other a | 133 | 12.2 | 35 | 6.3 | 98 | 18.1 | ||
| Mean | SD | Mean | SD | Mean | SD | t | p | |
|---|---|---|---|---|---|---|---|---|
| Age | 40.4 | 13.4 | 37.1 | 13.5 | 43.8 | 12.4 | −8.5 | <0.001 |
| Years of education | 14.9 | 3.27 | 15.9 | 3.32 | 13.9 | 2.91 | 10.3 | <0.001 |
| Household income b | 5.41 | 2.65 | 6.11 | 2.40 | 4.69 | 2.69 | 9.2 | <0.001 |
| Family history of AUD | 0.09 | 0.14 | 0.04 | 0.09 | 0.14 | 0.16 | −12.2 | <0.001 |
| Child maltreatment | 38.5 | 15.7 | 34.3 | 11.1 | 42.8 | 18.3 | −9.3 | <0.001 |
| ADHD symptoms | 1.37 | 1.69 | 0.62 | 1.04 | 2.13 | 1.87 | −16.5 | <0.001 |
| Depressive symptoms | 6.64 | 9.50 | 0.99 | 2.13 | 12.4 | 10.6 | −24.8 | <0.001 |
| Physical QoL | 78.2 | 17.1 | 86.5 | 11.2 | 69.7 | 17.8 | 18.8 | <0.001 |
| Psychological QoL | 70.0 | 20.0 | 79.8 | 13.2 | 60.1 | 20.9 | 18.7 | <0.001 |
| Social QoL | 66.3 | 23.4 | 74.4 | 19.5 | 58.1 | 24.2 | 12.4 | <0.001 |
| Environment QoL | 70.5 | 18.5 | 78.8 | 14.6 | 62.0 | 18.4 | 16.8 | <0.001 |
Other marital status included divorced (n = 88), separated (n = 30), widowed (n = 11), and other marital status (n = 4).
Response options for annual household income were: 1 = “<$5000”; 2 = “$5000 ‐ $9999”; 3 = “$10000–$19999”; 4 = “$20000–$29999”; 5 = “$30000–$39999”; 6 = “$40000–$49999”; 7 = “$50000–$74999”; 8 = “$75000–$100000”; and 9 = “>$100000”.
Figure 1 shows the standardized regression coefficients from multivariable regressions with four QoL domains as dependent variables. Panel A shows that older age (b = −0.07, p = 0.004), history of child maltreatment (b = −0.13, p < 0.001), ADHD symptoms (b = −0.22, p < 0.001), depressive symptoms (b = −0.31, p < 0.001), and AUD diagnosis (b = −0.12, p < 0.001) were associated with lower physical QoL, whereas higher household income was protective (b = 0.10, p < 0.001). Panel B shows that Black/African American participants had higher psychological QoL (b = 0.16, p < 0.001) compared with White participants, whereas history of child maltreatment (b = −0.13, p < 0.001), ADHD symptoms (b = −0.28, p < 0.001), depressive symptoms (b = −0.32, p < 0.001), and AUD diagnosis (b = −0.16, p < 0.001) were associated with lower psychological QoL. Panel C shows that older age (b = −0.08, p = 0.004), fewer years of education (b = −0.07, p = 0.026), history of child maltreatment (b = −0.17, p < 0.001), ADHD symptoms (b = −0.13, p < 0.001), depressive symptoms (b = −0.25, p < 0.001) and AUD diagnosis (b = −0.07, p = 0.049) were associated with lower social QoL, whereas being married was protective (b = 0.07, p = 0.018). Panel D shows that being male (b = −0.08, p = 0.001), being Black/African American (b = −0.07, p = 0.017), history of child maltreatment (b = −0.20, p < 0.001), ADHD symptoms (b = −0.16, p < 0.001), depressive symptoms (b = −0.16, p < 0.001) and AUD diagnosis (b = −0.17, p < 0.001) were associated with lower environment QoL, whereas high household income was protective (b = 0.19, p < 0.001). Figure 1 shows that depressive symptoms had the strongest inverse associations with physical, psychological, and social QoL, and the effects of child maltreatment history and ADHD symptoms on the four QoL domains were of similar or larger magnitudes to those for AUD diagnosis.
FIGURE 1.
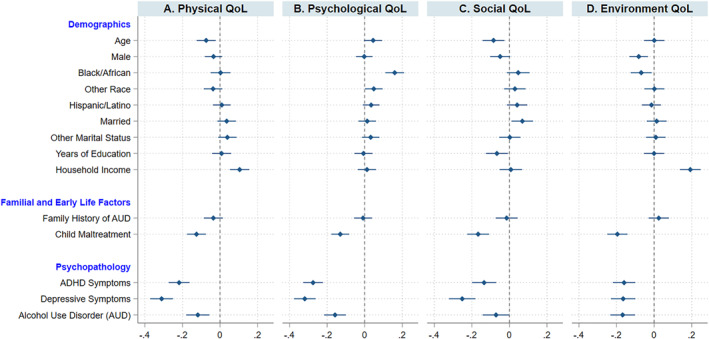
Effects of demographic, familial and early life, and psychopathology measures on four QoL domains, via multivariable regression analyses. Standardized regression coefficients, and 95% confidence intervals, are presented for multiple measures on four QoL domains: Physical, Psychosocial, Social, and Environment. The referent groups for sex, race, ethnicity, and marital status were female, White, not Hispanic/Latino and being single, respectively.
Figure 2 shows the path model where the effects of familial and early life factors were indirectly associated with multiple domains of QoL through increased psychopathology symptoms and AUD diagnosis. Family history of AUD was indirectly associated with higher ADHD and depressive symptoms, which in turn were associated with greater likelihood of positive AUD diagnosis and lower QoL across the four domains. As for history of child maltreatment, it was indirectly associated with greater likelihood of positive AUD diagnosis through higher ADHD and depressive symptoms, which in turn was associated with lower QoL domains. Three‐path mediation analyses indicated familial and early life factors conferred risks for ADHD and depressive symptoms, which in turn led to greater likelihood of positive AUD diagnosis and then to lower physical, psychological, and environment QoL (Supplemental Table 2), underscoring the crucial mediating role of AUD in pathways from familial and early life factors to lower QoL. Overall, the three mediators accounted for 78.8% to 100.0% of the total effect of family history of AUD on QoL domains and accounted for 33.2%–54.4% of the total effect of child maltreatment history on QoL domains (Supplemental Table 1).
FIGURE 2.
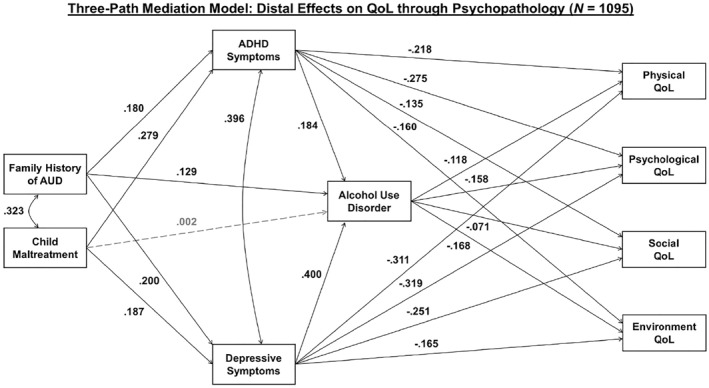
Path analysis linking family history of AUD and history of child maltreatment to QoL domains. Direct effects of family history of AUD and child maltreatment history on QoL domains and covariate effects (age, sex, race, ethnicity, marital status, years of education, and household income) were modeled but not shown in this Figure. Decomposition of direct and indirect effects is summarized in Supplemental Table 1. Three‐path mediation effects linking family history of AUD and history of child maltreatment to QoL domains are summarized in Supplemental Table 2. Correlations among QoL domains were positive and ranged from 0.371 to 0.588. Model fit statistics are as follow: Chi‐Square Statistic of Model Fit for the Baseline Model = 5295.548, Degrees of Freedom = 117, p < 0.0001; Chi‐Square Statistic of Model Fit = 0.000, Degrees of Freedom = 0, p = 0.0000; CFI = 1.000; TLI = 1.000; RMSEA = 0.000; SRMR = 0.000.
Expanding upon the path analysis, LPA was utilized to capture history of familial and early life factors and the co‐occurrence of an enriched set of clinical characteristics, including three alcohol‐related variables (obsessive drinking, compulsive drinking, and alcohol problems). These three alcohol‐related variables were not simultaneously modeled in the path analysis due to multicollinearity (Supplemental Figure 1). LPA can effectively model within‐person elevations in multiple correlated measures and capture both the range and severity of symptoms within a person‐centered framework. Panel A of Figure 3 shows the four‐class LPA which yielded the best fit to the data based on the likelihood ratio tests while referencing the Bayesian Information Criterion and considering the interpretability of latent Profiles (Supplemental Table 3). Overall, the four latent Profiles were differentiated by severity of clinical characteristics. Profile 1 (51.5%) had the lowest standardized mean scores across familial and early life factors, psychopathology symptoms, and alcohol‐related measures, and was labeled the “Minimal Risk” Profile. Profile 2 (17.6%) had standardized mean scores around zero for all early life factors and clinical characteristics and was labeled the “Low Risk” Profile. Profile 3 (18.4%) was like Profile 2 in terms of exposure to child maltreatment but was distinct in terms of family history of AUD and other clinical characteristics (labeled the “Moderate Risk” Profile). Profile 4 (12.5%) had the highest standardized mean scores across all early life and clinical characteristics and was labeled the “High Risk” Profile.
FIGURE 3.
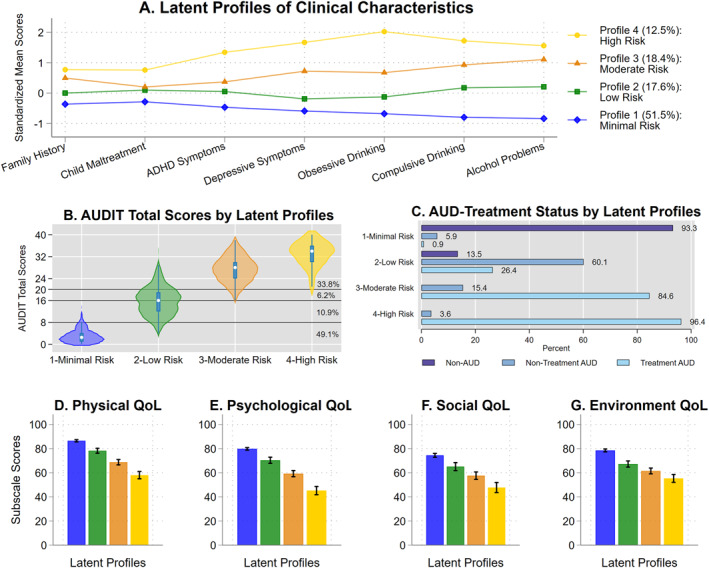
Latent Profiles capturing the spectrum of alcohol use behavior and dose‐response associations with QoL domains. Four latent Profiles were identified (Panel A) that were differentiated in terms of AUDIT total score and AUD‐treatment status (Panels B and C). In Panel B, the horizontal lines represent the WHO recommended clinical cutoffs for the AUDIT and the resulting proportions of each risk level groups were listed on the right (49.1% scored between 0 and 7; 10.9% scored between 8 and 15; 6.2% scored between 16 and 19; and 33.8% scored between 20 and 40) (32). Latent Profiles with more severe clinical characteristics had lower scores on all four domains of QoL (Panels D to G). Compared with latent Profile 1, the Cohen's d effect sizes for latent Profile 2 on QoL were 0.68 for physical domain, 0.66 for psychological domain, 0.46 for social domain, and 0.73 for environment domain. The Cohen's d effect sizes for latent Profile 3 relative to latent Profile 1 on QoL were 1.41 for physical domain, 1.41 for psychological domain, 0.84 for social domain, and 1.12 for environment domain. The Cohen's d effect sizes for latent Profile 4 relative to latent Profile 1 on QoL were 2.23 for physical domain, 2.36 for psychological domain, 1.30 for social domain, and 1.49 for environment domain.
The four empirically derived latent Profiles captured the full spectrum of alcohol use behavior. The violin plot (Panel B) illustrates increasing AUDIT total scores across the latent Profiles. These latent Profiles captured more than what is typically obtained through the AUDIT alone as they also factored into other familial and early life and clinical characteristics. Latent Profiles 2–4 provided better differentiation of individuals at the moderate to high clinical severity range than utilizing the conventional AUDIT cutoff scores of 8, 16, and 20 recommended by the WHO (32). Panel C shows all participants without AUD were in Profile 1 or Profile 2, whereas participants with AUD who did not seek inpatient treatment (non‐treatment AUD) were mostly in Profile 2, and participants with AUD who sought treatment (treatment AUD) were mostly in Profiles 3 and 4. These patterns of membership support the distinctiveness and clinical relevance of these four latent Profiles. Panels D‐G visually depict a consistent pattern in which Profiles with increasing clinical severity reported lower physical, psychological, social, and environment QoL in a stepwise, dose‐response fashion. The effect sizes of Profile 2 relative to Profile 1 on QoL domains were medium (Cohen's d ranged from 0.46 to 0.73). The effect sizes of Profiles 3 and 4 relative to Profile 1 on QoL domains were large (Cohen's d ranged from 0.84 to 2.36). The medium‐to‐large effect sizes highlight the advantage of using latent Profiles to capture co‐occurrence of early life adversity and clinical symptoms in predicting QoL.
Demographic differences in latent Profiles are presented in Figure 4. Participants in Profiles 2–4 were more likely to age 35 years or older, whereas those in Profile 1 were more likely to be under 35 years old (χ 2 (6) = 92.70, p < 0.001). Participants in Profiles 2 and 3 were more likely to be male (χ 2 (3) = 42.77, p < 0.001). Participants in Profiles 3 and 4 were less likely to be of Other Race (χ 2 (6) = 37.06, p < 0.001). Participants in Profiles 2–4 were more likely to report other marital status (χ 2 (6) = 43.15, p < 0.001). Finally, participants in Profiles 2–4 were more likely to report fewer years of education (χ 2 (6) = 127.49, p < 0.001) and lower household income (χ 2 (6) = 77.87, p < 0.001).
FIGURE 4.
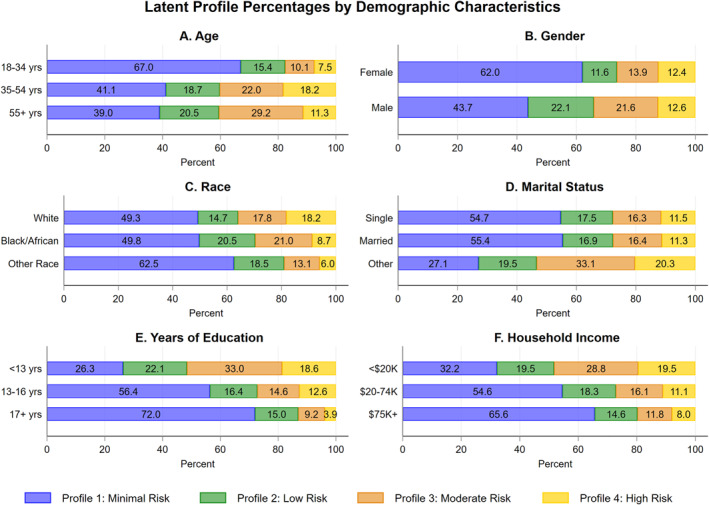
Demographic differences and health disparities in latent Profiles. In these analyses, age, years of education, and household income were categorized into three groups to facilitate data interpretation and visualization. Older and male participants were more likely than younger and female participants to be in latent Profiles with more severe clinical characteristics. Participants reported other marital status, fewer years of education, and lower household income were also more likely to be in latent Profiles with more severe clinical characteristics.
DISCUSSION
In adults across the spectrum of alcohol use behavior, AUD is inversely associated with QoL, especially for the physical, psychological and environment domains. Expanding upon prior research conducted among heavy drinkers in treatment settings (9, 35), this study revealed several domain‐specific demographic influences. For instance, physical and social QoL declined with age and lower environment QoL was observed among males and Blacks/African Americans. Relative to Whites, Blacks/African Americans reported higher psychological QoL, which based on prior literature may be related to higher social connectedness and religious involvement (36, 37). Household income was positively associated with higher physical and environment QoL, underscoring the role of socioeconomic resources in promoting specific domains of QoL (38).
Consistent with our first hypothesis, externalizing and internalizing psychopathology were uniquely associated with lower QoL and these inverse associations were of similar or larger magnitudes as the effects of AUD on QoL. These findings suggest that while AUD is an important risk factor for low QoL (9), interventions aimed at reducing externalizing and internalizing psychopathology may help promote QoL of AUD patients (10, 11, 12, 13), and thereby recovery as now defined (5). Consistent with our second hypothesis, significant indirect associations were also identified in the path analysis linking familial and early life factors to QoL domains via psychopathology symptoms and AUD. Notably, the three‐path mediation effects were significant for three out of four domains of QoL, such that family history of AUD and child maltreatment increased risks of externalizing and internalizing psychopathology, which in turn led to greater likelihood of positive AUD diagnosis and lower physical, psychological, and environment QoL. Although tested with retrospective data collected cross‐sectionally, the directions of these effects are consistent with longitudinal observations (17, 20, 39). The proposed developmental model could be of value to clinicians for case conceptualization and treatment planning (e.g., identifying externalizing and/or internalizing psychopathology as treatment targets and addressing early life trauma as clinically indicated) and should be further evaluated in prospective research.
LPA of early life factors, symptoms indicative of psychopathology, and alcohol‐related variables revealed four latent Profiles that varied by severity. These latent Profiles were cross validated against AUD and treatment‐seeking status and had dose‐response associations with all four QoL domains. Consistent with our third hypothesis, latent Profiles with greater clinical severity were associated with lower QoL domains. Specifically, the associations of the “Moderate Risk” and “High Risk” Profiles with QoL domains, relative to the “Minimal Risk” Profile were of large magnitude, with effect sizes (Cohen's d) ranging from 0.84 to 2.36. These Profile associations with QoL were larger in magnitude than the within‐person improvements in QoL domains observed based on changes in drinking levels across time (Cohen's d ranging from 0.22 to 0.52) (9). Therefore, while abstinence and reductions in drinking are critical to improve QoL, QoL among individuals in recovery may remain relatively low if other factors are not simultaneously addressed (40). More generally, our findings underscore the importance of addressing early life adversity, family history of AUD, and clinical characteristics across the spectrum of alcohol use behavior, as the factors driving greater clinical severity in Profiles 2–4 and lower QoL may be an obstacle to recovery and a driver of lapse and relapse. As expected, demographic differences in latent Profile membership further revealed health disparities. These findings may inform targeted intervention and outreach efforts to address health disparities experienced by older and disadvantaged individuals who are most vulnerable to experiencing low QoL in adulthood.
The strengths of this study include the heterogenous sample of 1095 participants representing the spectrum of alcohol use behavior, deep phenotyping including structured psychiatric interviews, the examination of multidimensional QoL including social and environment domains, the integration of familial and early life factors and psychopathology symptoms as risk factors for QoL within a developmental model, and the utilization of a person‐centered approach to classify multiple clinical characteristics into latent Profiles.
Despite these strengths, several limitations should be noted. First, retrospective reporting of child maltreatment, though assessed using the well‐validated CTQ‐SF questionnaire, is vulnerable to recall bias. Second, despite the use of measures with good psychometric properties, ADHD symptoms, depressive symptoms, alcohol problems, and QoL were measured based on self‐report and participants may have underreported undesirable symptoms. Third, alcohol‐related measures included in this study focused on current alcohol use behaviors and did not include onset of AUD or follow‐up data on relapse or remission of AUD, limiting our ability to assess for within‐person changes in QoL as a function of clinical characteristics and alcohol problems. Fourth, the use of cross‐sectional data limited inferences about cause and effect. For instance, although child maltreatment likely preceded psychopathology symptoms, and almost certainly preceded AUD and measures of QoL in adulthood, the relationships of psychopathology and AUD to QoL may be bi‐directional in nature, or connected via common underlying genetic predisposition. Longitudinal studies, incorporating genetic factors, are therefore needed to further our understanding of the dynamic associations between these variables over time.
In conclusion, the current study utilized a large and heterogeneous sample to establish support for a developmental model linking family history of AUD and history of child maltreatment to QoL domains via ADHD symptoms, depressive symptoms, and AUD diagnosis. The person‐centered approach of LPA captured how co‐occurrence and severity of multiple clinical characteristics in a stepwise fashion led to lower QoL in multiple domains. Because improvement in QoL is an integral part of recovery from AUD (5), future research should examine how drinking behavior and QoL may change during sensitive developmental periods from adolescence into young adulthood to inform prevention efforts. Longitudinal follow‐up of patients with AUD should address how stress and coping mechanisms may change over time and how interventions focused on psychosocial factors underling risk Profiles can aid recovery from AUD.
Supporting information
Supplementary Material 1
This study was supported by NIAAA Division of Intramural Clinical and Biological Research (Z1A AA 000130). The authors would like to thank Yvonne Horneffer, LaToya Sewell, and Tonette Vinson for their clinical work with the study participants, as well as Elizabeth Davis, Cheryl Jones, and the NIH postbaccalaureate Intramural Research Training Award fellows for their administrative support for this study protocol.
The authors do not have any conflicts of interest to disclose.
REFERENCES
- 1. World Health Organization . Global status report on alcohol and health 2018. World Health Organization; 2018. [Google Scholar]
- 2. Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM‐5 alcohol use disorder: results from the National Epidemiologic Survey on alcohol and related conditions III. JAMA Psychiatr. 2015;72(8):757–66. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eddie D, Greene MC, White WL, Kelly JF. Medical burden of disease among individuals in recovery from alcohol and other drug problems in the United States: findings from the National recovery Survey. J Addiction Med. 2019;13(5):385–95. 10.1097/adm.0000000000000512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kendler KS, Ohlsson H, Karriker‐Jaffe KJ, Sundquist J, Sundquist K. Social and economic consequences of alcohol use disorder: a longitudinal cohort and co‐relative analysis. Psychol Med. 2017;47(5):925–35. 10.1017/s0033291716003032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hagman BT, Falk D, Litten R, Koob GF. Defining recovery from alcohol use disorder: development of an NIAAA research definition. Am J Psychiatr. 2022:appiajp21090963. [DOI] [PubMed] [Google Scholar]
- 6. Costanza R, Fisher B, Ali S, Beer C, Bond L, Boumans R, et al. Quality of life: an approach integrating opportunities, human needs, and subjective well‐being. Ecol Econ. 2007;61(2–3):267–76. 10.1016/j.ecolecon.2006.02.023 [DOI] [Google Scholar]
- 7. World Health Organization. Development of the World Health Organization WHOQOL‐BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28(3):551–8. 10.1017/s0033291798006667 [DOI] [PubMed] [Google Scholar]
- 8. Imtiaz S, Loheswaran G, Le Foll B, Rehm J. Longitudinal alcohol consumption patterns and health‐related quality of life: results from the National Epidemiologic Survey on alcohol and related conditions. Drug Alcohol Rev. 2018;37(1):48–55. 10.1111/dar.12503 [DOI] [PubMed] [Google Scholar]
- 9. Witkiewitz K, Kranzler HR, Hallgren KA, O'Malley SS, Falk DE, Litten RZ, et al. Drinking risk level reductions associated with improvements in physical health and quality of life among individuals with alcohol use disorder. Alcohol Clin Exp Res. 2018;42(12):2453–65. 10.1111/acer.13897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Landes SD, London AS. Self‐reported ADHD and adult health in the United States. J Atten Disord. 2018;25(1):3–13. 10.1177/1087054718757648 [DOI] [PubMed] [Google Scholar]
- 11. Able SL, Johnston JA, Adler LA, Swindle RW. Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychol Med. 2007;37(1):97–107. 10.1017/s0033291706008713 [DOI] [PubMed] [Google Scholar]
- 12. Saatcioglu O, Yapici A, Cakmak D. Quality of life, depression and anxiety in alcohol dependence. Drug Alcohol Rev. 2008;27(1):83–90. 10.1080/09595230701711140 [DOI] [PubMed] [Google Scholar]
- 13. Quintero J, Morales I, Vera R, Zuluaga P, Fernández A. The impact of adult ADHD in the quality of life profile. J Atten Disord. 2019;23(9):1007–16. 10.1177/1087054717733046 [DOI] [PubMed] [Google Scholar]
- 14. Hardee JE, Cope LM, Martz ME, Heitzeg MM. Review of neurobiological influences on externalizing and internalizing pathways to alcohol use disorder. Curr Behav Neurosci Rep. 2018;5(4):249–62. 10.1007/s40473-018-0166-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Edwards AC, Gardner CO, Hickman M, Kendler KS. A prospective longitudinal model predicting early adult alcohol problems: evidence for a robust externalizing pathway. Psychol Med. 2016;46(5):957–68. 10.1017/s0033291715002457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol Addict Behav. 2011;25(3):390–404. 10.1037/a0024519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Meque I, Dachew BA, Maravilla JC, Salom C, Alati R. Externalizing and internalizing symptoms in childhood and adolescence and the risk of alcohol use disorders in young adulthood: a meta‐analysis of longitudinal studies. Aust N Z J Psychiatr. 2019;53(10):965–75. 10.1177/0004867419844308 [DOI] [PubMed] [Google Scholar]
- 18. Fenton M, Geier T, Keyes K, Skodol A, Grant B, Hasin D. Combined role of childhood maltreatment, family history, and gender in the risk for alcohol dependence. Psychol Med. 2013;43(5):1045–57. 10.1017/s0033291712001729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Enoch M.‐A. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology. 2011;214(1):17–31. 10.1007/s00213-010-1916-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mosley‐Johnson E, Garacci E, Wagner N, Mendez C, Williams JS, Egede LE. Assessing the relationship between adverse childhood experiences and life satisfaction, psychological well‐being, and social well‐being: United States Longitudinal Cohort 1995‐2014. Qual Life Res. 2019;28(4):907–14. 10.1007/s11136-018-2054-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lin HS, Naimi AI, Brooks MM, Richardson GA, Burke JG, Bromberger JT. Child maltreatment as a social determinant of midlife health‐related quality of life in women: do psychosocial factors explain this association? Qual Life Res. 2018;27(12):3243–54. 10.1007/s11136-018-1937-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lin HS, Naimi AI, Brooks MM, Richardson GA, Burke JG, Bromberger JT. Life‐course impact of child maltreatment on midlife health‐related quality of life in women: longitudinal mediation analysis for potential pathways. Ann Epidemiol. 2020;43:58–65. 10.1016/j.annepidem.2020.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pearson MR, Wilson AD, Richards DK, Witkiewitz K. Reconsidering alcohol treatment non‐responders: psychosocial functioning among heavy drinkers 3 years following treatment. Addiction. 2021;116(5):1262–9. 10.1111/add.15280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Witkiewitz K, Pearson MR, Wilson AD, Stein ER, Votaw VR, Hallgren KA, et al. Can alcohol use disorder recovery include some heavy drinking? A replication and extension up to 9 Years following treatment. Alcohol Clin Exp Res. 2020;44:1862–74. 10.1111/acer.14413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, Roos CR, et al. Profiles of recovery from alcohol use disorder at three years following treatment: can the definition of recovery be extended to include high functioning heavy drinkers? Addiction. 2019;114(1):69–80. 10.1111/add.14403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mann RE, Sobell LC, Sobell MB, Pavan D. Reliability of a family tree questionnaire for assessing family history of alcohol problems. Drug Alcohol Depend. 1985;15(1–2):61–7. 10.1016/0376-8716(85)90030-4 [DOI] [PubMed] [Google Scholar]
- 27. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–90. 10.1016/s0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- 28. Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–56. 10.1017/s0033291704002892 [DOI] [PubMed] [Google Scholar]
- 29. Svanborg P, Asberg M. A new self‐rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr Scand. 1994;89(1):21–8. 10.1111/j.1600-0447.1994.tb01480.x [DOI] [PubMed] [Google Scholar]
- 30. First MB. Structured clinical interview for the DSM (SCID). The encyclopedia of clinical psychology. 2014:1–6. 10.1002/9781118625392.wbecp351 [DOI] [Google Scholar]
- 31. Anton RF. Obsessive‐compulsive aspects of craving: development of the obsessive compulsive drinking scale. Addiction. 2000;95(Suppl 2):S211–217. 10.1046/j.1360-0443.95.8s2.9.x [DOI] [PubMed] [Google Scholar]
- 32. Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. In: AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. World Health Organization; 1992. [Google Scholar]
- 33. Kirouac M, Stein ER, Pearson MR, Witkiewitz K. Viability of the World Health Organization quality of life measure to assess changes in quality of life following treatment for alcohol use disorder. Qual Life Res. 2017;26(11):2987–97. 10.1007/s11136-017-1631-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model: A Multidiscip J. 2007;14(4):535–69. 10.1080/10705510701575396 [DOI] [Google Scholar]
- 35. Picci RL, Oliva F, Zuffranieri M, Vizzuso P, Ostacoli L, Sodano AJ, et al. Quality of life, alcohol detoxification and relapse: is quality of life a predictor of relapse or only a secondary outcome measure? Qual Life Res. 2014;23(10):2757–67. 10.1007/s11136-014-0735-3 [DOI] [PubMed] [Google Scholar]
- 36. Frazier C, Mintz LB, Mobley M. A multidimensional look at religious involvement and psychological well‐being among urban elderly African Americans. J Counsel Psychol. 2005;52(4):583–90. 10.1037/0022-0167.52.4.583 [DOI] [Google Scholar]
- 37. Warren‐Findlow J, Laditka JN, Laditka SB, Thompson ME. Associations between social relationships and emotional well‐being in middle‐aged and older African Americans. Res Aging. 2011;33(6):713–34. 10.1177/0164027511411928 [DOI] [Google Scholar]
- 38. Lee SB, Chung S, Seo JS, Jung WM, Park IH. Socioeconomic resources and quality of life in alcohol use disorder patients: the mediating effects of social support and depression. Subst Abuse Treat Prev Pol. 2020;15(1):13. 10.1186/s13011-020-00258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. VanMeter F, Nivison MD, Englund MM, Carlson EA, Roisman GI. Childhood abuse and neglect and self‐reported symptoms of psychopathology through midlife. Dev Psychol. 2021;57(5):824–36. 10.1037/dev0001169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tracy EM, Laudet AB, Min MO, Kim H, Brown S, Jun MK, et al. Prospective patterns and correlates of quality of life among women in substance abuse treatment. Drug Alcohol Depend. 2012;124(3):242–9. 10.1016/j.drugalcdep.2012.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1


