Abstract
Background
Lockdown measures during the COVID-19 pandemic are expected to have negative effects on mental health and relationship quality. However, little is known about the magnitude of these psychological effects on a population level and for vulnerable subgroups.
Methods
A representative sample (N = 2503; 50.2% female; mean age = 49.5) of the German population was assessed face-to-face during the COVID-19 pandemic (February 10-April 25, 2020). They were examined for differences in mental health (BSI-18) and relationship quality (PFB) in a pre-lockdown and lockdown subsamples. After testing and establishing the measurement models in confirmatory factor analyses, we added covariates as predictors of the factors to the regression model to investigate the impact of the lockdown measures.
Results
Overall, participants included after the introduction of lockdown measures reported significantly fewer mental health problems than participants included before the lockdown. Predictor analyses revealed that this effect was larger for participants of younger age and those with higher household income. There was no significant difference in relationship quality between pre-lockdown and lockdown. However, relationship quality improved for younger participants after the lockdown measures started, but deteriorated for older participants.
Conclusions
The German population was found to be largely resilient to the immediate effects of lockdown on mental health and relationship quality. Older participants and those with lower socio-economic status might constitute risk groups during times of lockdown. Further studies in countries affected by more drastic lockdown measures and the long-term consequences of the pandemic are needed to inform decision makers about the psychological effects of lockdown.
Keywords: COVID-19, Corona, Pandemic, Mental health, Relationship quality
1. Introduction
The ongoing COVID-19 pandemic is deemed to constitute a major public health care challenge worldwide. In Germany, the first coronavirus case (COVID-19) was confirmed on January 28, 2020. The sharp increase in newly confirmed cases in the population began in the first weeks of March shortly before the World Health Organization (WHO) declared the COVID-19 outbreak a global pandemic on March 11, 2020. In the following weeks, a whole series of lockdown measures were announced, starting with the cancellation of major events for more than 1000 participants on March 9, 2020. According to the agreement between the federal and state governments, social contacts in public places were restricted after March 16, 2020. This resulted in the closing of bars, theaters, exhibitions, sport facilities, schools, daycare centers for children, playgrounds, and retail sales points. On March 22, 2020 the federal and state governments agreed on the comprehensive restriction of social contacts in public and private settings, restrictions on freedom of movement in one federal state, and the closure of non-essential businesses.
This pandemic may have had a major impact on public mental health and we need to understand the scale of any such impact in different sections of the population (Hotopf, Bullmore, O'Connor & Holmes, 2020). A recent study, using the UK Household Longitudinal Study Waves, found that general psychological distress increased slightly during the pandemic (Pierce et al., 2020a). The risk factors associated with deterioration in general psychological distress were younger age, female gender, living with children, low income, and employment before the pandemic. Another study, which investigated the presence of psychiatric symptoms in the UK population, found higher levels of anxiety, depression, and posttraumatic stress disorder (PTSD) symptoms compared to previous population studies (Shevlin et al., 2020), but mean levels did not reach any clinical cut-offs. The presence of anxiety, depression, and symptoms of PTSD were predicted by younger age, presence of children in the household, and high estimates of personal risk. Anxiety and depression symptoms were also predicted by low income, loss of income, and pre-existing health conditions. Female gender, the presence of children in the household and estimates of personal risks of infection were predictive of specific COVID-related anxiety. A repeated cross-sectional study conducted in China reported that, although the number of confirmed COVID-19 cases increased sharply from the first to the second measurement time point, there were no clinically significant changes in the symptoms of anxiety, depression, and PTSD (Wang et al., 2020). However, the research context China might hardly be comparable to the UK due to several reasons such as the very different cultural and social context, and fundamental differences in handling of the pandemic. Therefore, it seems important to consider different pathways through which psychological distress and mental health can be affected in diverse cultural and political backgrounds while having the same or different lockdown measures.
In most countries worldwide, one strategy to reduce the spread of the virus is the introduction of lockdowns of cities, regions or entire nations. The consequences associated with these lockdown measures are expected to result in changes in the psychosocial environment in affected countries, and have profound negative effects on mental health (Fegert et al., 2020; Holmes et al., 2020). In fact, a recent online survey conducted at a university in Spain (N = 2530) during the COVID-19 outbreak found that participants reported a significant psychological impact during the first weeks of lockdown (Odriozola-González et al., 2020). In contrast, a longitudinal study on vulnerable groups (psychosocial and health-related risk factors and low socioeconomic position) conducted in the UK suggests that trajectories of depression were relatively stable during lockdown with little improvement (Frank et al., 2020). But depression symptoms were considerably higher among people experiencing limited social support, with a low socio-economic position, and among those with pre-existing mental and physical health conditions and/or a history of physical/psychological abuse (Frank et al., 2020).
Besides the potential psychological distress, the COVID-19 pandemic may also directly affect peoples’ relationships (Stanley and Markman, 2020). Reports of family violence including all violent behaviors within families that may be physical, sexual, psychological, or economic, including child abuse and intimate partner violence, have increased around the world since the lockdown measures came into force (Usher et al., 2020). However, despite growing evidence of the impact of lockdown on mental health, quantitative studies using psychometrically validated measures on the impact on relationship quality are missing. A deeper understanding of the psychological effects of lockdown on mental health and interpersonal relationships is crucial as this will allow governments to weigh their decisions regarding the psychological consequences of these lockdown measures.
To our knowledge, there are no representative population-based studies on the psychological impact of lockdown. So far, most of the research on mental health during the COVID-19 pandemic has used non-probability sampling (e.g. convenience sampling in online surveys). This can be particularly problematic for social and mental health research, as the persons excluded are often those most in need of help (Pierce et al., 2020b). Moreover, the current evidence is limited due to the use of non-validated mental health measures, and a lack of comparable, pre-Covid-19 or pre-lockdown baseline data.
The current study tries to fill these gaps in the literature by reporting the findings of a representative population-based survey which adopted a random route procedure during the COVID-19 pandemic in Germany. This is the first study to explore cross-sectional differences in psychological symptoms and relationship quality in a pre-lockdown and lockdown representative population-based sample, while adjusting for several well-known risk factors of mental health such as age, gender, low socio-economic status, and adverse childhood experiences (ACEs). Based on current literature, we hypothesize that lockdown results in an increase in psychological distress and a decrease in quality in intimate partner relationships. As one effect of the COVID-19 pandemic and lockdown is expected to be a widening of inequalities (Pierce et al., 2020b), we hypothesized that risk groups (young adults/older people, women, respondents with lower income, respondents with children in the household, and respondents with higher ACE burden) experienced greater psychological distress and lower quality of couple relationships in lockdown, compared with pre-lockdown participants. In doing so, we will allow for curvilinear effects by using squared predictors (e.g. younger individuals might be affected more strongly than middle aged adults because of a higher need for communion and belonging in young adolescence, compared to middle aged adults, who have more stable social networks in the form of family (i.e., partner and children) and co-workers. We also expect older participants to be more affected by the pandemic because of a higher risk to their health due to COVID-19 and a stronger isolation because of this fear, a decreased number of contacts with close family members and difficulty compensating for the lack of social interactions through virtual means.)
2. Method
2.1. Study design and participants
In cooperation with a professional demographics research institute (USUMA) a representative sample of the German population (age 14–95) was collected employing a random route approach. In a first step 258 German regional areas were predefined using the reference system for representative studies in Germany provided by the ADM-Sampling-System. Next, the target households within these regional areas were selected according to a random route procedure. For multi-person households, one person was randomly selected using the Kish selection grid technique. The population-based survey was conducted during the COVID-19 pandemic in the period from February 10 to April 25, 2020. This included a pandemic pre-lockdown and a pandemic lockdown time period. Face-to-face data collection was ongoing during the lockdown weeks. Participants were contacted by telephone to inform them in advance about the additional hygiene measures for the interviews and the self-report questionnaires (wearing masks, keeping distance, and disinfection of hands). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Ethics Committee of the University of Leipzig. Written and verbal informed consent was obtained from all respondents, who indicated their willingness to take part in the study. Anonymity in responses was guaranteed by deleting the link between the study code and the name of the participant after data entry. To qualify for inclusion in the survey, participants had to be at least 14 years of age and have sufficient German language skills. Prospective subjects were informed that the study was about psychological health and well-being. Out of the 5668 addresses used, 2503 responded indicating a utilization rate of 44.1%. The final sample consisted of N = 2503 respondents (50.2% female) with an average age of M = 49.5 years (SD = 17.5; range 14–95).
2.2. Measures
Sociodemographic information such as age, gender (female/male), number of children in the household, and equivalized household income (<EUR 1000 monthly was defined as a poverty risk), was assessed in face-to-face interviews with all respondents. Additionally, relationship status was assessed asking whether Person are living in a partnership (yes/no). By employing a random route approach, the sociodemographic characteristics of the target persons are not known before the assessment.
Mental health problems were measured using the short version of the Brief Symptom Inventory (BSI-18; Derogatis, 2000). This is a reliable and valid self-report measure assessing somatization, depression, and anxiety in different contexts and languages. Each item describes a symptom to be rated by respondents along a five-point scale according to how much they have been negatively impacted by the symptom during the previous week. As recent studies found high inter-correlations of the subscales and only fair reliability of the subscales, we tested different measurement models for further analyses. With a Cronbach α of 0.92 the BSI Global Severity Index (BSI-GSI) demonstrated excellent reliability in the current sample.
Intimate Partner Relationship Quality (RQ) was measured using the short form of the Partnership Questionnaire (PFB; Hahlweg, 1996; Kliem et al., 2012). It consists of three subscales (tenderness, communication, quarreling), each measured using three items. With a Cronbach α of 0.86 the PFB total score demonstrated good reliability in the current sample (n = 1548 (62%) answered the PFB and were in a relationship). Before including it as an outcome variable in our regression analyses, we tested different measurement models of the PFB to identify the number of latent variables that represent the data best. We then used these as dependent variables in the regression analyses.
Adverse childhood experiences (ACEs) were assessed using the German version of the ACE questionnaire (Felitti et al., 1998; Schäfer et al., 2009). The ACE questionnaire consists of ten items and assesses maltreatment and household dysfunction before the age of 18 using a yes/no answer format. The sum score (0–10) was used to investigate the differential effect of lockdown on respondents with different numbers of ACEs.
2.3. Statistical analyses
Lockdown measures in Germany were introduced in a series of actions beginning on March 9 up to March 23. To define the pre-lockdown and lockdown period, we chose the time of the agreement between the federal and state governments on restricting physical contacts in public place on March 16. This resulted in the pre-lockdown period (February 10-March 15, 2020, n = 1542) and the lockdown period (March 16-April 25, 2020; n = 961).
Model specification. We specified the measurement models of the BSI-18 and the PFB using confirmatory factor analysis (cfa-function of the R package lavaan; Rosseel, 2012). Since the items were ordinal and non-normally distributed, we used weighted least squares variance and means adjusted estimation. For the BSI, we first estimated a one-factor model with a general psychopathology factor loading on all 18 items. We compared this model to a three-factor model with each factor representing a BSI subscale (somatization, depression, and anxiety), measured using six items each. For the PFB we also compared a one-factor model with a general factor loading on all nine items, and a three-factor model with each factor representing a subscale (tenderness, communication, quarreling), with three items each. We evaluated overall model fit using a combination of the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR) based on common standards (good fit: CFI ≥ 0.95; RMSEA ≤ 0.06; SRMR ≤ 0.06; Bentler, 1990; Hu and Bentler, 1999).
Missing values. Of the full sample of N = 2503 participants, we excluded n = 115 participants (4.59%) because of missing values in the relevant demographic variables, resulting in a final sample size of N = 2388. The number of missing responses on the 18-item BSI was very low (0.06%), with only n = 22 participants (0.92%) not completing one or more responses. Of the n = 1551 respondents who stated to be in a relationship, n = 3 had at least one missing value on the 9-item PQ resulting in a total percentage of 0.19% missing values. We treated missing values on these questionnaires with pairwise missing deletion in the confirmatory factor analysis, resulting in a sample of n = 2366 for the BSI model and n = 1548 for the PFB PQ model.
Regression model. After testing and establishing the measurement models, we added the covariates as linear and squared predictors of the factors to the model. More specifically, we included lockdown measures (i.e., before versus after March 16, 2020), gender, age, ACE scores, equalized household income, and children living in the household as predictors of the factors in the models. All continuous variables (i.e., age, ACE scores, adjusted household income) were z-standardized and were included as both linear and squared predictors. Squared predictors were included based on our assumption that for example age might have a curvilinear effect on symptoms. To investigate whether the lockdown measures moderated the relationship between the other covariates and the BSI or PFB factors, we also specified interaction terms between lockdown and the other covariates (see online supplement Table 2 for an overview of all predictors). If the interaction terms are significant, this would suggest that lockdown affected the mental health or RQ of some subgroups in particular or in a different way/direction.
Table 2.
Mental Health (BSI-18) regression models (n = 2366).
| Mental Health (BSI) |
R2 |
β |
CI |
p |
Std. β |
|---|---|---|---|---|---|
| .280 | |||||
| Gender | 0.106 | [ 0.016; 0.196] | 0.021 | 0.136 | |
| Age | 0.128 | [ 0.081; 0.175] | 0.000 | 0.164 | |
| Age2 | 0.011 | [-0.030; 0.052] | 0.605 | 0.014 | |
| EHI | −0.091 | [-0.140;-0.042] | 0.000 | −0.117 | |
| EHI2 | 0.013 | [-0.018; 0.044] | 0.428 | 0.017 | |
| ACE | 0.403 | [ 0.327; 0.479] | 0.000 | 0.518 | |
| ACE2 | −0.031 | [-0.058;-0.004] | 0.024 | −0.040 | |
| Children | −0.017 | [-0.129; 0.095] | 0.769 | −0.021 | |
| Children2 | −0.008 | [-0.043; 0.027] | 0.666 | −0.010 | |
|
Lockdown |
−0.275 |
[-0.430;-0.120] |
0.000 |
−0.353 |
|
| Interaction effects | |||||
| Lockdown x Gender | 0.077 | [-0.066; 0.220] | 0.291 | 0.099 | |
| Lockdown x Age | 0.018 | [-0.055; 0.091] | 0.637 | 0.023 | |
| Lockdown x Age2 | 0.074 | [ 0.007; 0.141] | 0.028 | 0.096 | |
| Lockdown x EHI | −0.094 | [-0.172;-0.016] | 0.018 | −0.121 | |
| Lockdown x EHI2 | 0.060 | [ 0.007; 0.113] | 0.027 | 0.077 | |
| Lockdown x ACE | −0.039 | [-0.164; 0.086] | 0.546 | −0.050 | |
| Lockdown x ACE2 | −0.022 | [-0.071; 0.027] | 0.373 | −0.028 | |
| Lockdown x children | −0.031 | [-0.194; 0.132] | 0.710 | −0.039 | |
| Lockdown x children2 | 0.016 | [-0.029; 0.061] | 0.494 | 0.020 | |
Note. R2 = proportion of explained BSI; β = regression weight; CI = 95% confidence interval; Std. β = standardized regression weights (obtained by constraining the factor variance to 1); EHI = Equivalized Household Income; ACE = Adverse Childhood Experiences; BSI-18 = Brief Symptom Inventory.
2indicates squared predictors; significant predictors (p < 0.05) are marked in bold.
3. Results
Descriptive statistics.Table 1 and OS1 (Online Supplement Table 1) contain a detailed description of the total sample and the pre-lockdown and the lockdown sample. No significant differences between the pre-lockdown and the lockdown sample were found regarding all sociodemographic variables.
Table 1.
Sociodemographic characteristics of the total sample and comparison of the pre-lockdown and lockdown sample.
| Total (N = 2503) | Pre-Lockdown (n = 1542) | Lockdown (n = 961) | Test-statistic | |
|---|---|---|---|---|
| Age | 49.53 (17.51) | 49.80 (17.84) | 49.10 (16.95) |
t(2500) = 5.82 p = 0.334 |
| Gender (female) | 1256 (50.2) | 789 (51.2) | 467 (48.6) | Χ2(1) = 1.56, p = 0.211 |
| Living with partner | 418 (30.6) | 247 (30.1) | 171 (31.4) | Χ2(1) = 0.26, p = 0.612 |
| German citizenship | 2409 (96.2) | 1481 (96.0) | 928 (96.6) | Χ2(1) = 0.45, p = 0.504 |
| In a relationship | 1551 (62.0) | 967 (62.7) | 584 (60.8) | Χ2(1) = 0.95, p = 0.331 |
| Family status (n, (%)) | ||||
| Married, living together | 1108 (44.3) | 699 (45.3) | 409 (42.6) | Χ2(5) = 8.14, p = 0.149 |
| Married, living apart | 55 (2.2) | 41 (2.7) | 14 (1.5) | |
| Single | 734 (29.3) | 440 (28.5) | 294 (30.6) | |
| Divorced | 375 (15.0) | 217 (14.1) | 158 (16.4) | |
| Widowed | 226 (9.0) | 142 (9.2) | 84 (8.7) | |
| Not stated | 5 (0.2) | 3 (0.2) | 2 (0.2) | |
| Persons in household | ||||
| 1 | 862 (34.4) | 544 (35.3) | 318 (33.1) | Χ2(4) = 3.20, p = 0.525 |
| 2 | 986 (39.4) | 600 (38.9) | 386 (40.2) | |
| 3 | 371 (14.8) | 217 (14.1) | 154 (16.0) | |
| 4 | 218 (8.7) | 138 (8.9) | 80 (8.3) | |
| ≥5 | 66 (2.6) | 43 (2.8) | 23 (2.4) | |
| Children in the household | ||||
| 0 | 2065 (82.5) | 1268 (82.2) | 797 (82.9) | Χ2(4) = 4.18, p = 0.242 |
| 1 | 284 (11.3) | 168 (10.9) | 116 (12.1) | |
| 2 | 127 (5.1) | 87 (5.6) | 40 (4.2) | |
| ≥3 | 27 (1.1) | 19 (1.2) | 8 (0.8) | |
| Equalized disposable income | 1839.38 (726.08) | 1831.38 (737.64) | 1852.21 (737.64) |
t(2471) = 1.76 p = 0.488 |
| BSI Total Score | 4.51 (7.40) | 5.00 (7.93) | 3.73 (6.39) |
t(2473) = 4.18 p < 0.001 |
| PFB Total Score | 19.65 (4.67) | 19.27 (4.84) | 20.27 (4.31) |
t(1546) = 4.18 p < 0.001 |
Values are means (standard deviations) or n (%), as appropriate.
Model estimation. Model fit statistics are presented in Table 2 in the online supplement. The one-factor models had a considerably worse fit than the three-factor models for both the BSI and PFB. This was particularly the case for the PFB scale, which yielded unacceptable RMSEA and SRMR values. Because the three BSI factors were highly correlated (average r = 0.85; ps < 0.001), we added a common second-order factor loading on all three subscale factors (average λ = 0.92). The model fit was equivalent to the three-factor model. The three-factor PFB model fitted the data well, but the communication and tenderness factors were correlated by r = 0.97, whereas these factors only correlated by r = −0.45 and r = −0.36 with the quarreling factor. As such, we collapsed the two aforementioned scales into a common factor and specified a two-factor model (r = −0.40 between the factors). The two-factor model had a worse fit than the three-factor model (see Table 2 in the online supplement), but was theoretically more meaningful than the more complex model. We, therefore, used the higher-order BSI and two-factor PFB model for the subsequent analyses. The models are illustrated in Fig. 1 in the online supplement.
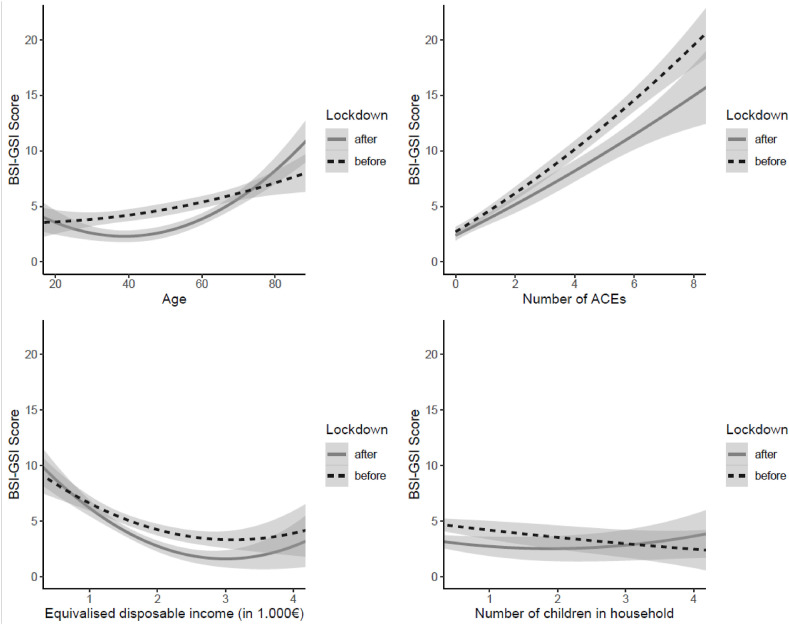
Fig. 1.
Pre-lockdown versus post-lockdown mental health patterns across the covariates.
The effect of covariates on BSI. As can be seen in Table 2, all covariates except for having children in the household had a significant effect on the BSI values pre-lockdown and lockdown. In summary, females, subjects who reported more ACEs, and older participants generally reported higher BSI values. The effects of gender and age were rather weak compared to the strong positive effect of ACEs on psychopathological symptoms. For each standard deviation on the ACE scale, reported psychopathological symptoms (BSI) increased by half a standard deviation.
Participants assessed during the lockdown reported significantly lower psychopathological symptoms, (pre-lockdown: M = 5.00; SD = 7.93; lockdown: M = 3.73, SD = 6.39) corresponding to an approximate mean-level difference of 1.27 points on the BSI scale, which reflects a small effect (d = 0.17). With regard to moderation effects of the lockdown variable, we found that the aforementioned negative relationship between psychopathological symptoms (BSI-18) and age, as well as adjusted household income were stronger in the lockdown than in the pre-lockdown sample. Fig. 1 illustrates these effects. Middle-aged adults yielded lower BSI values, whereas older adults (i.e., over the age of 70) reported higher psychopathological symptoms in lockdown. In regard to equivalized household income, participants with low socio-economic status (i.e., equivalized household income below EUR 1000) reported similar symptom endorsement throughout the entire assessment, which was comparatively high compared with participants with higher household income. The negative slope was steeper in lockdown, indicating that people with sufficient funds also reported lower psychopathological symptoms. The effect of the score of ACEs on psychopathological symptoms was equivalent both pre-lockdown and lockdown, despite somewhat lower BSI values overall (i.e., the main effect of lockdown).
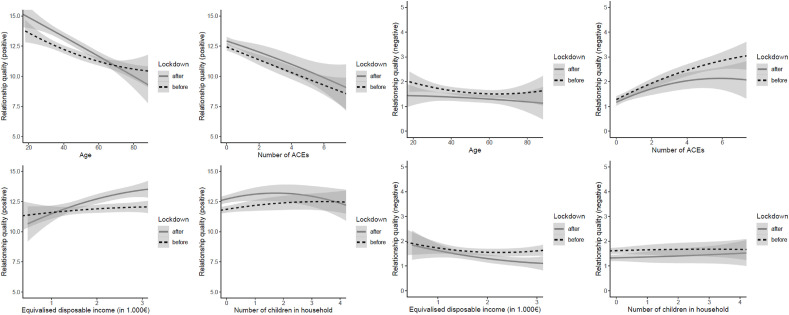
The effect of covariates on relationship quality (RQ).Table 3 shows the relationship between the covariates and the two factors of RQ (i.e., positive and negative RQ). Age and ACEs yielded a weak to moderate negative effect on the positive RQ factor pre-lockdown and lockdown. In contrast to the BSI, there were no significant differences between pre-lockdown and lockdown regarding RQ. However, the interaction effect with age was significant, suggesting that RQ improved in younger participants, but deteriorated for older participants in lockdown. With regard to low intimate partner RQ, only the accumulation of ACEs was a significant predictor with a moderate to strong positive effect on the frequency of conflicts (i.e., negative RQ). The findings suggest that a higher number of ACEs result in more frequent negative partnership behavior, independently of lockdown. Fig. 2 presents the effects of the covariates on RQ.
Table 3.
Relationship quality (PFB) regression models (n = 1548).
| Relationship quality positive | R2 | β | CI | p | Std. β |
| .179 |
|||||
| Gender | 0.049 | [-0.061; 0.159] | 0.379 | 0.056 | |
| Age | −0.228 | [-0.295;-0.161] | 0.000 | −0.258 | |
| Age2 | 0.048 | [-0.019; 0.115] | 0.165 | 0.054 | |
| EHI | 0.030 | [-0.037; 0.097] | 0.390 | 0.033 | |
| EHI2 | 0.009 | [-0.034; 0.052] | 0.677 | 0.010 | |
| ACE | −0.221 | [-0.317;-0.125] | 0.000 | −0.250 | |
| ACE2 | 0.004 | [-0.039; 0.047] | 0.856 | 0.004 | |
| Children | 0.008 | [-0.086; 0.102] | 0.865 | 0.009 | |
| Children2 | −0.009 | [-0.033; 0.015] | 0.480 | −0.010 | |
| Lockdown |
0.177 |
[-0.015; 0.369] |
0.069 |
0.200 |
|
| Interaction effects | |||||
| Lockdown x Gender | −0.117 | [-0.301; 0.067] | 0.213 | −0.133 | |
| Lockdown x Age | −0.137 | [-0.249;-0.025] | 0.017 | −0.155 | |
| Lockdown x Age2 | 0.002 | [-0.104; 0.108] | 0.974 | 0.002 | |
| Lockdown x EHI | 0.074 | [-0.048; 0.196] | 0.235 | 0.083 | |
| Lockdown x EHI2 | 0.014 | [-0.072; 0.100] | 0.741 | 0.016 | |
| Lockdown x ACE | 0.056 | [-0.122; 0.234] | 0.537 | 0.063 | |
| Lockdown x ACE2 | −0.009 | [-0.087; 0.069] | 0.826 | −0.010 | |
| Lockdown x children | 0.002 | [-0.155; 0.159] | 0.978 | 0.002 | |
| Lockdown x children2 |
−0.003 |
[-0.040; 0.034] |
0.860 |
−0.004 |
|
| Relationship quality negative | R2 | β | CI | p | Std. β |
| .111 |
|||||
| Gender | 0.024 | [-0.092; 0.140] | 0.686 | 0.031 | |
| Age | −0.051 | [-0.120; 0.018] | 0.142 | −0.067 | |
| Age2 | 0.034 | [-0.035; 0.103] | 0.330 | 0.044 | |
| EHI | 0.013 | [-0.058; 0.084] | 0.720 | 0.017 | |
| EHI2 | 0.008 | [-0.037; 0.053] | 0.733 | 0.010 | |
| ACE | 0.310 | [ 0.206; 0.414] | 0.000 | 0.405 | |
| ACE2 | −0.036 | [-0.079; 0.007] | 0.109 | −0.047 | |
| Children | 0.017 | [-0.085; 0.119] | 0.747 | 0.022 | |
| Children2 | −0.001 | [-0.030; 0.028] | 0.936 | −0.002 | |
| Lockdown |
0.138 |
[-0.068; 0.344] |
0.189 |
0.180 |
|
| Interaction effects | |||||
| Lockdown x Gender | −0.191 | [-0.387; 0.005] | 0.055 | −0.249 | |
| Lockdown x age | −0.011 | [-0.131; 0.109] | 0.863 | −0.014 | |
| Lockdown x age2 | −0.106 | [-0.222; 0.010] | 0.072 | −0.139 | |
| Lockdown x EHI | −0.109 | [-0.240; 0.022] | 0.103 | −0.142 | |
| Lockdown x EHI2 | −0.024 | [-0.110; 0.062] | 0.579 | −0.032 | |
| Lockdown x ACE | −0.040 | [-0.230; 0.150] | 0.679 | −0.053 | |
| Lockdown x ACE2 | −0.019 | [-0.095; 0.057] | 0.635 | −0.024 | |
| Lockdown x children | −0.037 | [-0.211; 0.137] | 0.681 | −0.048 | |
| Lockdown x children2 | −0.003 | [-0.050; 0.044] | 0.887 | −0.005 | |
Note. R2 = proportion of explained PFB variance; β = regression weight; CI = 95% confidence interval; Std. β = standardized regression weights (obtained by constraining the factor variance to 1); EHI = Equivalized Household Income; ACE = Adverse Childhood Experiences; PFB = Partnership Questionnaire; 2 indicates squared predictors; significant predictors (p < 0.05) are marked in bold.
Fig. 2.
Pre-lockdown versus lockdown relationship quality (positive: tenderness and communication/negative: quarreling) patterns across the covariates.
4. Discussion
This is the first representative population-based study to investigate the immediate effect of lockdown on mental health status and intimate partner relationships during the Covid-19 pandemic. In contrast to the results of recent studies and reviews of the negative psychological effects of social isolation (Leigh-Hunt et al., 2017) and quarantine (Brooks et al., 2020), our cross-sectional study on an aggregate population level evidenced fewer mental health problem in participants assessed during the first five weeks of the lockdown phase compared with participants assessed in the pandemic phase before the lockdown measures were introduced. This effect was stronger for younger participants and those with a higher household income, indicating that older persons and less well-off persons did not report better mental health in the lockdown sample compared with the pre-lockdown sample. One of the COVID-19 risk groups, people of advanced age (i.e. 70+), reported higher psychopathological symptoms in the lockdown sample compared with people of advanced age in the pre-lockdown sample.
Surprisingly, the number of children in the household did not affect mental health when comparing the pre-lockdown and lockdown sample. This might be explained by the fact that some companies were supportive in a sense that they would allow their employees to work from home while taking care of children. Several companies also offered high rates of short-time work compensation and short-time vacation in the beginning of the lockdown which enabled their employees to support their children with home schooling. Overall our results, therefore, run counter to the widespread belief that lockdown measures have an immediate negative impact on mental health (Fegert et al., 2020; Holmes et al., 2020). However, the study is based on the short term self-reported psychosocial effects, limited to the first weeks after the introduction of lockdown measures. At this stage, the population was still in an exploratory phase of the lockdown effects, with no knowledge nor prediction capability about how long these measures will be in act. In these uncertain conditions, people may tend to adopt a "propitiatory” attitude, and/or other attitudinal dispositions that help them cope with the related stressors. Thus, the fact that the subjects assert that there are no significant qualitative changes nor negative impact on mental health or relationship quality, may be influenced by the willingness to see and represent oneself in a propitiatory perspective, functional to cope with potentially longer challenging conditions.
In line with our results, a recent study on mental health conducted during the COVID-19 pandemic in China made the counterintuitive observation that there was no immediate impact of province-wide lockdown on psychological distress, whereas quarantine increased individuals’ anxiety, fear, and anger (Gan et al., 2020). Another study of the adult general population in the Republic of Ireland did not determine any marked differences in depression and anxiety in the first week of the nationwide quarantine compared with previous national prevalence studies in the UK (Hyland et al., 2020). Moreover, a study using a quota sample of N = 2025 UK adults found that anxiety, depression, and PTSD symptoms were not significantly higher compared with previous population-based studies. Within this study, the factors having children at home, loss of income, pre-existing health conditions, exposure to the virus, and high estimates of personal risk were associated with psychological distress. The authors conclude that the UK population, especially older citizens, were largely resilient in the early stages of the pandemic (Shevlin et al., 2020).
Our cross-sectional study demonstrates that in the first five weeks, on a population level, intimate partner RQ was not affected by the lockdown measures, indicating no differences in couples’ quarreling, communication, and tenderness. These results are in line with a recent poll by Monmouth University that included N = 808 adults aged 18 and older. It found that the vast majority (74%) of Americans with a romantic partner reported their relationship had not changed overall since the coronavirus outbreak. Specifically, 70% reported that the outbreak had not affected how often they argue or 77% reported no changes in their sex life. Among those who did report an outbreak-related change in their RQ, more reported a positive than a negative effect (Monmouth University Polling Institute, 2020). However, the interaction effect of the lockdown with age in our study was significant, suggesting that RQ improved for younger participants but deteriorated for older participants after the lockdown measures were introduced. This might be partly explained by the increase in mental health problems in older participants (+70) after lockdown measures were introduced. Another explanation for the age differences might be that the lockdown measures increase time availability at home, resulting in the possibility of family members to spend more time together and enjoy themselves in leisure activities in a domestic setting. This affects especially younger couples with higher rates of employment, while being a constant factor for retired persons. Surprisingly, the number of children in the household did not affect RQ when comparing the pre-lockdown and lockdown sample.
4.1. Strengths and limitations
One major strength of the study is that a random sampling procedure was applied, which reduced the risk of bias, and allowed quantification and exploration of the reasons of non-response (Pierce et al., 2020b). As most of the recent studies used convenience samples to describe the impact of the pandemic or lockdown, our study reports the first results of the impact of lockdown measures and the pandemic within a randomly selected population-based sample. A further strength is the continuation of the data collection during the lockdown made possible by adopting additional hygiene measures and intensifying telephone contacts prior to the interviews. Several limitations of this study need to be addressed. First, the study has a cross-sectional design which does not allow for a detailed analysis of change over time within populations or individuals. Cross-sectional data can only provide limited insights into population characteristics over a given time span, but it can be used to consider broader patterns of changes at an aggregate level (Rafferty et al., 2015). Although this study shows that there is no immediate severe effect of the lockdown measures in the German population, it might be important to consider that the levels of mental health difficulties, in light of the ongoing pandemic and rising number of COVID-cases, had increased within the German population already. As described in the introduction, some studies found that levels of anxiety, depression and PTSD increased during the pandemic. Hence, the lack of an immediate effect of the lockdown might be explained by generally higher levels of distress due to the pandemic. Second, there might be a significant self-selection bias as the utilization rate was only 44.1%. Hence, we cannot rule out a possible underutilization of particularly vulnerable groups during lockdown. This may have resulted in the underutilization of individuals with pre-existing (mental) health problems, as evidenced by the lower ACE load of the respondents in lockdown. Although we controlled for this difference in our analyses, the question remains whether there are further differential negative effects for vulnerable groups. While data collection was ongoing in the weeks of lockdown resulting in n = 918 respondents, interviewers reported more problems accessing the respondents during the lockdown. This may also have affected comparability between pre-lockdown and lockdown. However, demographic data were almost exactly equally distributed between the pre-lockdown and the lockdown sample. Third, the BSI-18 was found to have a highly left-skewed distribution within samples of the general population (Franke et al., 2017). This was also evident in our sample and may have resulted in a lack of sensitivity to detecting minor psychological distress on a population level. Fourth, our study is limited to the first weeks after introduction of the lockdown measures. Studies on the long-term psychosocial effects may identify a more severe impact on mental health and intimate partner relationships. Fourth, measures used in this study (ACE and PSB) are not validated in the subsample of 14–17-year-old adolescents but only for individuals at age 18 and older. Fifth, only participants who are at least 14 years of age and who had sufficient German language skills to understand the questionnaires were included in the study. Therefore, especially vulnerable groups such immigrants and refugees who are known to report higher levels of mental health difficulties compared to the general population (Fazel et al., 2005), and might thus be affected more by the lockdown measures, were excluded, which limits generalizability of the results. Sixth, since we neither assessed further characteristics of participants (e.g. sexual orientation), nor characteristics and forms of relationships (duration, sexual orientation, monogamous vs. polygamous, changing partners), the potential associations thereof with relationship quality and mental health could not be investigated. Seventh, from a global perspective, Germany introduced relatively mild lockdown measures (e.g., freedom of movement was only restricted in one federal state; people were allowed to do sports outside). It also provided powerful resources to mount a successful response to the pandemic (e.g. massive expansion of the number of intensive care beds, short-time work compensation, corona grants for self-employed persons). The results might thus not be generalizable to nations with more severe lockdown measures and limited responses to the pandemic.
Our study demonstrated that the lockdown measures introduced in Germany may not have had the immediate negative effects on mental health and quality in intimate partner relationships expected by the scientific and political community. The results may have crucial implications for political decisions on resources and interventions needed in future pandemics and possible periods of lockdown as well as for national recovery afterwards (Shevlin et al., 2020). With more and more research being published on the impact of the COVID-19 pandemic and the associated lockdown measures, the evidence is mounting that, on a population level, the immediate effects on mental health may not be as dramatic as expected. However, differential effects for specific vulnerable groups can be observed. Based on our results, especially older persons are at risk of being more negatively affected by lockdown measures regarding their mental health and relationship quality. They might therefore constitute a major target group for prevention strategies. Overall, the lockdown might not have an immediate or constant impact on mental health and relationships, but rather evolves over time. Therefore, future studies should focus on the longitudinal assessment of vulnerable groups as this will allow for more fine-grained analytical strategies. As the pandemic is ongoing, and Germany has had another lockdown, it is important to consider long-term effects on psychological distress and relationship quality. This seems crucial as the burden and strain on a personal level, but also on a population level, will become visible only after regular mental health services and child protections services, who had been restricted to emergency cases, return to normal care (Fegert et al., 2020). Future studies should also include in-depth investigations of factors that might explain our results, such as time availability at home or whether people tend to adopt a certain attitude or attitudinal dispositions, that help them cope with the pandemic and lockdowns measures in the short-term. More studies are urgently needed to study these processes in the ongoing pandemic and identify the evolving needs of different groups, and to then address these needs by means of appropriate (psychosocial) interventions.
Conflict of interest declaration
Over the last 5 years JMF has received research funding from the EU, DFG (German Research Foundation), BMG (Federal Ministry of Health), BMBF (Federal Ministry of Education and Research), BMG (Federal Ministry of Health), BMFSFJ (Federal Ministry of Family, Senior Citizens, Women and Youth), BMVg (Federal Ministry of Defence), several state ministries of social affairs, State Foundation Baden Württemberg, the UBS Foundation, Pontifical Gregorian University, Caritas, Diocese of Rottenburg-Stuttgart. Moreover, he received travel grants, honoraria and sponsoring for conferences and medical educational purposes from DFG, AACAP, NIMH / NIH, EU, Pro Helvetia, Janssen-Cilag (J&J), Shire, several universities, professional associations, political foundations and German federal and state ministries. The other authors have nothing to disclose.
Funding statement
The work was partly funded by The Independent Commissioner for Child Sexual Abuse Issues (JMF and MR). The funding source The Independent Commissioner for Child Sexual Abuse Issues had no role in the study design, data collection, analyses or interpretation of the data, writing the manuscript, or the decision to submit this paper for publication. The authors have not been paid to write this article by a pharmaceutical company or other agency. All authors had full access to all the data in the study and had final responsibility for the decision to submit the manuscript for publication.
Data availability
The data that support the findings of this study are available from the corresponding author, [CS], upon reasonable request.
Author contribution
CS, EB, and JMF designed the study. GO and CS were responsible for performing the statistical analyses and reporting the methods, and results. All authors (CS, GO, EP, EB, VC, MR, AW, JMF) made substantial contributions to the interpretation of data for this publication. CS, EP, and GO carried out the systematic literature searches, and they wrote the first draft of the manuscript. The remaining authors were involved in revising this draft critically in terms of important intellectual content. All authors (CS, GO, EP, EB, VC, MR, AW, JMF) are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.113954.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bentler P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L.R. NCS Pearson; Minneapolis, MN: 2000. Brief Symptom Inventory (BSI)-18: Administration, Scoring, and Procedures Manual. [Google Scholar]
- Fazel M., Wheeler J., Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatr. Ment. Health. 2020;14(20):1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Frank P., Iob E., Steptoe A., Fancourt D. Trajectories of depressive symptoms among vulnerable groups in the UK during the COVID-19 pandemic. medRxiv. 2020 doi: 10.1101/2020.06.09.20126300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke G.H., Jaeger S., Glaesmer H., Barkmann C., Petrowski K., Braehler E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Med. Res. Methodol. 2017;17(1):14. doi: 10.1186/s12874-016-0283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan Y., Ma J., Wu J., Chen Y., Zhu H., Hall B.J. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychol. Med. 2020;1–12 doi: 10.1017/S0033291720003116. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahlweg K. Hogrefe; Göttingen: 1996. Fragebogen zur Partnerschaftsdiagnostik (FPD). (Testmappe mit Handanweisung, Fragebogen PFB, Fragebogen FLP, Problemlisten I und II) [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotopf M., Bullmore E., O'Connor R.C., Holmes E.A. The scope of mental health research in the COVID-19 Pandemic and its aftermath. Br. J. Psychiatr. 2020:1–3. doi: 10.1192/bjp.2020.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model.: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- Kliem S., Job A.K., Kröger C., Bodenmann G., Stöbel-Richter Y., Hahlweg K., Brähler E. Entwicklung und Normierung einer Kurzform des Partnerschaftsfragebogens (PFB-K) an einer repräsentativen deutschen Stichprobe. Z. Klin. Psychol. Psychother. 2012;41(2):81–89. doi: 10.1026/1616-3443/a000135. [DOI] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Publ. Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Monmouth University Polling Institute . 2020. National: Relationships Weather the Pandemic - Few Report Love Life Changes during the Outbreak.https://www.monmouth.edu/polling-institute/documents/monmouthpoll_us_052120.pdf/ Retrieved August 06, 2020 from. [Google Scholar]
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatr. Res. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Jessop C., John A., Hotopf M., Ford T., et al. Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry. 2020;7(7):567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafferty A., Walthery P., King-Hele S. 2015. Analysing Change over Time: Repeated Cross- Sectional and Longitudinal Survey Data.https://www.ukdataservice.ac.uk/media/455362/changeovertime.pdf Retrieved August 06, 2020 from. [Google Scholar]
- Rosseel Y. Lavaan: an R package for structural equation modeling. J. Stat. Software. 2012;48(2):1–36. https://users.ugent.be/~yrosseel/lavaan/lavaanIntroduction.pdf Retrieved August 06, 2020 from: [Google Scholar]
- Schäfer I., Wingenfeld K., Spitzer C. 2009. ACE-D. Deutsche Version des “Adverse Childhood Experiences Questionnaire (ACE)https://zep-hh.de/wp-content/uploads/2015/05/ACE_Bogen.pdf Retrieved August 06, 2020 from. [DOI] [PubMed] [Google Scholar]
- Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L., et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6) doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley S.M., Markman H.J. Helping couples in the shadow of COVID‐19. Fam. Process. 2020 doi: 10.1111/famp.12575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. Family violence and COVID‐19: increased vulnerability and reduced options for support. Int. J. Ment. Health Nurs. 2020;29(4):549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, [CS], upon reasonable request.