ABSTRACT
Patients with Chagas disease have reduced health-related quality of life (HRQoL). Hence, we aimed to identify the factors that mostly affected their HRQoL. This was a systematic review of qualitative studies. The Latin American and Caribbean Health Sciences Literature, Medical Literature Analysis and Retrieval System Online, Excerpta Medica Database, Web of Science, and SciVerse Scopus databases were searched for relevant studies without language or date restrictions. The search and data analysis were performed by independent reviewers; all qualitative studies that reported the factors that had an impact on the HRQoL of patients with Chagas disease were included. The risk of bias was assessed using the Critical Appraisal Skills Program Qualitative Study Checklist; confidence in the evidence was evaluated using the Grading of Recommendations Assessment, Development and Evaluation-Confidence in the Evidence from Reviews of Qualitative approach. Five studies were included in this review: four in Brazil and one in California, United States, with immigrants from Central and South America. The sample consisted of 207 patients with chronic Chagas disease. Stigma, physical limitations, work absenteeism, emotional or mental aspects, fear of treatment, and fear of the future had the strongest impact on the HRQoL. All items showed moderate confidence except for fear of treatment (low confidence). The physical, emotional, mental, and cultural aspects affected the HRQoL of patients with chronic Chagas disease. Identification of these factors is important in the development of strategies aimed at improving the HRQoL of this population.
Keywords: Chagas disease, Quality of life, Qualitative research, Systematic review
INTRODUCTION
Chagas disease (CD) was first described by the Brazilian scientist Carlos Chagas in 1909 1 , 2 . It remains a public health problem in Latin America 3 , with a potential expansion to non-endemic countries 4 . The acute phase is characterized by non-specific clinical manifestations 5 . Patients later progress to the chronic phase, which can present in indeterminate form (no specific signs and symptoms of disease) 6 , cardiac form (with heart disease), digestive form (with digestive impairment), or mixed form (simultaneous cardiac and digestive involvement) 7 .
Subjective health assessments have gained importance for clinicians, health policymakers, and researchers 8 , especially health-related quality of life (HRQoL). In the setting of CD, many studies have quantitatively evaluated the HRQoL of patients 9 - 13 . A recent state-of-the-art study 14 summarized the current findings and postulated that HRQoL is worse in patients with CD compared with that in healthy individuals. Moreover, HRQoL is more compromised in women with cardiovascular and gastrointestinal symptoms among patients with worse functional class, lower levels of physical activity, and worse cardiac function. Other studies have shown that HRQoL has potential value in screening patients with left systolic dysfunction 15 and identifying those at an increased risk of developing adverse cardiovascular events 13 , which highlights the value of HRQoL in the clinical follow-up of patients.
Despite evidence from previous studies, quantitative data are based on the participants’ response to the questionnaire-based survey with predefined questions, limiting the patient’s freedom of response. The major factors that affect the HRQoL of patients with CD should be determined. The identification of these factors can be carried out through qualitative interview 16 and can guide both clinicians and researchers in the selection of outcomes of patients’ management 17 - 19 . However, to the best of our knowledge, no qualitative studies have evaluated on the CD patients’ perception of the items that impact their HRQoL. Hence, the present study aimed to systematically review qualitative studies that investigated the items that has an impact on the HRQoL of patients with CD.
METHODS
Study design
This systematic review of qualitative studies aimed to identify the factors reported by CD patients that mostly affected their HRQoL and are part of the Caburé project (collaborative project focusing on social, historical, and geographical aspects of CD, which aims to create a specific instrument to assess patients’ HRQoL). The study was previously registered in the Open Science Framework (https://osf.io/4mk9u/) and edited following the Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines, an instrument used to describe the synthesis of qualitative research in health sciences 20 .
Peer review method
As recommended by Cochrane 21 , the screening of potentially eligible studies, data extraction, risk of bias assessment, and assessment of the quality of current evidence were performed by two independent reviewers: WTS and LFFO performed the screening of potentially eligible studies, data extraction, and risk of bias assessment, while WTS and DMX used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to assess the quality of current evidence. Discrepancies were resolved by consulting a third reviewer (HSC).
Searches and study selection
Potentially eligible studies were identified using a systematic search. The databases used were Latin American and Caribbean Health Sciences Literature (LILACS), Medical Literature Analysis and Retrieval System Online (MEDLINE), Excerpta Medica Database, Web of Science, and SciVerse Scopus for relevant studies. The search terms used were related to “Chagas disease,” “quality of life,” and “qualitative studies.” Each database was searched from the date of inception until November 2021 and updated in July 2022.
We manually reviewed the full-text versions of relevant systematic reviews and used a manual search to retrieve records from gray literature. The strategy used to search the MEDLINE database was [(“American Trypanosomiasis” OR “Trypanosomiasis, American” OR “Trypanosomiasis, South American” OR “South American Trypanosomiasis” OR “Trypanosoma cruzi Infection” OR “Infection, Trypanosoma cruzi” OR “Infections, Trypanosoma cruzi” OR “Trypanosoma cruzi Infections” OR “Chagas' Disease” OR “Cardiomyopathy, Chagas” OR “Trypanosomiasis, Cardiovascular” OR “Cardiovascular Trypanosomiasis” OR “Chagas Cardiomyopathy” OR “Cardiomyopathy, Chagas'” OR “Myocarditis, Chagas”) AND (“Quality of Life” OR “Life Quality” OR “Health-Related Quality Of Life” OR “Health-related Quality Of Life” OR “HRQOL”)]. More details about the search strategy are provided in the Supplementary Material (717.9KB, pdf) . After the search, the retrieved references were exported to Endnote®, and duplicate studies were removed. The authors screened the titles and abstracts and evaluated the full texts. Studies that met the eligibility criteria were included in this review.
Inclusion criteria
Primary qualitative studies that identified the factors that impact the HRQoL of individuals of both sexes, regardless of age, with at least two positive serological tests for Trypanosoma cruzi performed in any healthcare setting were included in this review. There were no restrictions on the language or year of publication.
Data extraction
Data on (a) the characteristics of the sample, (b) process of data collection and sources, (c) results of data analysis, and (d) main findings related to the HRQoL of patients were extracted. When data from a study were unavailable or unpublished, the original investigators were contacted to request the information. When necessary, the authors were contacted three times, with an interval of one week.
Risk of bias assessment
All included studies were assessed for risk of bias by reviewers using the Critical Appraisal Skills Program (CASP) Qualitative Study Checklist 22 . The CASP checklist composed of 10 questions, and the response options included “yes,” “no,” or “can’t tell” 23 .
Data analysis
The meta-synthesis method developed by Noblit and Hare was performed according to the instructions described by Britten et al. 24 . We present a meta-theory that demonstrates the analysis and interpretation of different theoretical and philosophical perspectives, sources, and assumptions shown in individual studies. Therefore, resynthesis was performed based on the meta-synthesis of the findings.
The characteristics and relationships between them were defined (location, sample characteristics, type of collection, and stage of disease). With information compiled based on the results of previous studies and researchers’ experience, the most frequent findings were grouped. Finally, the narrative summary technique was used, presenting the re-synthesis of the information collected and justifying the items that impact the HRQoL of patients with CD, as recommended by the Cochrane Handbook 25 .
The quality of current evidence was verified using the GRADE-Confidence in the Evidence from Reviews of Qualitative Research (GRADE-CERQual) approach 26 . According to this system, the evidence is classified as having high, moderate, low, or very low confidence. High-confidence evidence is related to a finding likely to be a reasonable representation of the phenomenon of interest, while low-confidence evidence shows that it remains unclear whether the finding is a representation of the phenomenon of interest, thus requiring further study 26 . More details regarding the confidence assessment are provided in the Supplementary Material (717.9KB, pdf) .
RESULTS
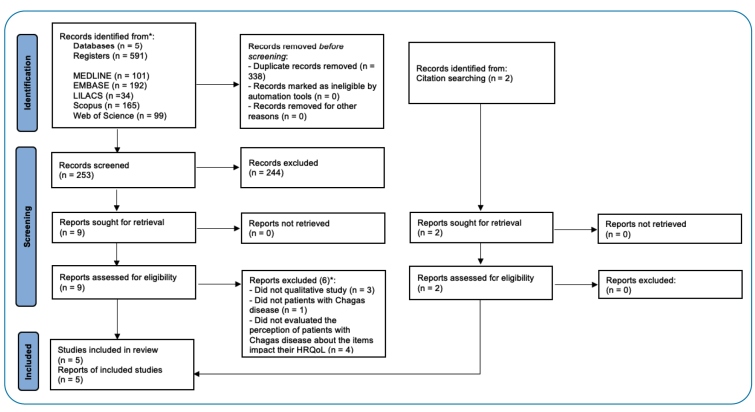
An electronic search strategy identified 591 relevant studies based on their titles and abstracts. Of these, 338 (57.2%) were duplicates. The remaining 253 studies were screened, and 9 references were selected as potentially eligible studies, of which 6 were excluded. After a manual search of previous reviews, we identified two other articles for full-text assessment, and both were included. Finally, five studies met the inclusion criteria 27 - 31 . Figure 1 outlines the process of selecting relevant articles for review.
FIGURE 1: Flowchart showing the process of selecting the studies for review. *Articles could be excluded for more than one reason.
The included studies were published between 2000 and 2021. Four were carried out in Brazil and one in California, United States, with immigrants from Central and South America. Among the included studies, the sample size ranged from 1 to 131 patients, and the total sample consisted of 207 individuals, all in the chronic phase of the disease. The ages of the patients ranged from 27 to 82 years.
The characteristics of the studies and their relationships are presented in Table 1. The meta-theory, with the main issues addressed by individual studies, is presented in Table 2. The details of the resynthesis (meta-synthesis) are described in the text. In summary, the issues that could impact the HRQoL of patients were grouped into 1) stigma, 2) mental health and/or emotional aspects, 3) physical limitations and work absenteeism, 4) fear of the future, and 5) fear of treatment. Results of the risk of bias assessment are shown in Table 3. Results of the assessment of the confidence of the findings for each thematic group performed using the GRADE-CERQual approach are shown in Table 4.
TABLE 1: Baseline characteristics of all included studies and the relationship between them (n=5).
| Study (year) | Country | Sample characteristics | Data collection | Disease stage |
|---|---|---|---|---|
| Araújo et al., 2000 27 | Brazil | n=131, aged from 31 years to 60 years, 62 men and 69 women | Individual interview | Chronic phase |
| Magnani, Oliveira, Gontijo, 2007 28 | Brazil | n=15, aged from 27 years to 75 years, 8 men and 7 women | Individual interview | Chronic phase |
| Ballester-Gil et al., 2008 29 | Brazil | n=1, aged 66 years, woman | Semi-structured individual interview | Chronic phase |
| Oliveira et al., 2010 30 | Brazil | n=10, aged from 51 years to 82 years, sex not reported | Semi-structured individual interview | Chronic phase |
| Forsyth et al., 2021 31 | United States | n=50, 17 men and 33 women | Semi-structured individual interview | Chronic phase |
TABLE 2: Interpretation of the different theoretical and philosophical perspectives (n=5).
| Study (year) | Theoretical and philosophical perspectives |
|---|---|
| Araújo et al., 2000 27 | It presents reports about the history of life and the disease, such as the existence of other cases in the family, what they felt when receiving the diagnosis, and impact on life after knowing the diagnosis. |
| Magnani, Oliveira, Gontijo, 2007 28 | It presents a theory about the symbology of Chagas disease in the lives of patients who are infected. |
| Ballester-Gil et al., 2008 29 | It presents the patient’s perceptions and knowledge about Chagas disease, which refer to the form of diagnosis; the feeling at the time of diagnosis; perceptions about the disease; perceptions about life in recent years; and perceptions about the forms of consultation and treatment. |
| Oliveira et al., 2010 30 | It presents information based on the patient’s perspective of the disease vector and on how they live and how they face the symptoms of the pathology. |
| Forsyth et al., 2021 31 | It presents the theory about patients’ knowledge of CD, impact of diagnosis (e.g., emotional), symptoms, access to treatment, strategies for treating the disease, sociopolitical context of CD, and adaptation to life in the United States, thus concluding the disease as neglected. |
TABLE 3: Risk of study bias.
| Risk of bias | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study (year) | 1) Was there a clear statement of the aims of the research? | 2) Is a qualitative methodology appropriate? | 3) Was the research design appropriate to address the aims of the research? | 4) Was the recruitment strategy appropriate to the aims of the research? | 5) Was the data collected in a way that addressed the research issue? | 6) Has the relationship between researcher and participants been adequately considered? | 7) Have ethical issues been taken into consideration? | 8) Was the data analysis sufficiently rigorous? | 9) Is there a clear statement of findings? | 10) How valuable is the research? |
| Araújo et al., 2000 27 | yes | Can’t tell | no | yes | no | no | yes | no | no | yes |
| Magnani, Oliveira, Gontijo, 2007 28 | yes | yes | yes | no | yes | no | yes | yes | no | yes |
| Ballester-Gil et al., 2008 29 | yes | yes | yes | no | yes | yes | yes | yes | no | yes |
| Oliveira et al., 2010 30 | yes | yes | yes | yes | yes | no | yes | yes | no | yes |
| Forsyth et al., 2021 31 | yes | yes | yes | yes | yes | yes | yes | yes | no | yes |
TABLE 4: Confidence in the evidence according to the GRADE-CERQual scores.
| Items that impact the HRQoL of patients with Chagas disease | CERQual Assessment of Confidence in the Evidence | Explanation of CERQual Assessment | Studies Contributing to the Review Finding |
|---|---|---|---|
| Stigma impacts the HRQoL of patients with CD. | Moderate confidence | Minor concerns in the methodological quality, coherence, data adequacy, and relevance | de Araújo et al., 2000 |
| Magnani et al., 2007 | |||
| Mental/emotional component impacts the HRQoL of patients with CD. | Moderate confidence | Minor concerns in the methodological quality and coherence; major concerns in the data adequacy and relevance | de Araújo et al., 2000 |
| Ballester-Gil et al., 2008 | |||
| Forsyth et al., 2021 | |||
| The physical component and work absenteeism impact the HRQoL of patients with CD. | Moderate confidence | Minor concerns in the methodological quality, coherence, data adequacy, and relevance | Ballester-Gil et al., 2008 |
| De Oliveira et al., 2010 | |||
| Forsyth et al., 2021 | |||
| Fear of the future impacts the HRQoL of patients with CD. | Moderate confidence | Minor concerns in the methodological quality, coherence, and relevance. Major concerns in the data adequacy | de Araújo et al., 2000 |
| Ballester-Gil et al., 2008 | |||
| Magnani et al., 2007 | |||
| Forsyth et al., 2021 | |||
| Fear of treatment impacts HRQoL of patients with CD. | Low confidence | Minor concerns in the methodological quality and relevance; major concerns in the data adequacy and coherence | Ballester-Gil et al., 2000 |
| Forsyth et al., 2021 |
Abbreviations: CD: Chagas Disease; CERQaul: Confidence in the Evidence from Reviews of Qualitative Research; HRQoL: Health-related quality of life.
Impact of stigma on HRQoL
Stigma is a situation in which the individual is aware of what is attributed to him by society and then begins to agree and apply negative stereotypes about the illness to oneself 32 . In the present review, two studies identified the impact of stigma on HRQoL 27 , 28 (moderate confidence).
In one study 27 , patients reported fear and shame, leading them to hide the disease from others: “Nobody knows at my job” and “Look, I am here now, but no one in my family knows I have this disease.” Another study 28 also described the interview response of an individual related to the stigma of sudden cardiac death: “People say these things: That Chagas disease... So-and-so died of Chagas disease, who would fall suddenly and die. This is how we heard about it. However, you know that even today, I still have it in my head from time to time. (...) This for me is death alone. Even that I think, do you understand? They say that whoever has Chagas disease, the person who is like this, falls and dies suddenly!”
Impact of mental health and/or emotional aspects on HRQoL
Three studies included interviews related to the mental health and/or emotional aspects of HRQoL (moderate confidence) 27 , 29 , 31 . One of the studies 27 demonstrated the emotional burden of having the disease: “Having Chagas disease for me is a problem.” In addition, other responses showed that the mental and/or emotional impact was detected since the diagnosis: “I love to dance, but after I found out I had Chagas disease I thought I had to go home, lie down, and wait for death...,” and “I felt very sad, lost, when I found out I had a disease that has no cure.”
Another study 29 reported the impact of CD on the mental and/or emotional aspects of HRQoL: “I feel very sad. I cry a lot. I am feeling down. I do not feel like talking or seeing anyone. I keep thinking that my heart is swollen and I feel more things than before. My life changed.”, and “I'm shaken, I don't want to talk to anyone. I am alone, thinking that I might die. I cry a lot every day, and I get out of control. I cry until I run out of air. I do not know how I had the strength to come today.” Finally, “this difficulty and pain caused me much sadness. I feel my heartbeat is fast.”
In a previous study 31 , the authors also verified the impact of mental and/or emotional factors on HRQoL: “I became depressed, I felt very sad, because you don’t know if you’re going to die tomorrow or what … I felt down, sad, without a desire to do anything….”
Impact of the physical component and work absenteeism on HRQoL
In several cases, patients with CD are removed from their jobs, particularly those with the cardiac form of the disease 33 , 34 . Physical limitations are one of the components that contribute to restriction in daily activities 35 , as observed in three studies 29 - 31 (moderate confidence).
In one of them, Ballester-Gil et al. 29 highlighted the impact of some physical factors related to body structure and function on patients’ HRQoL: “My heart is different. The patient’s blood pressure was high. I have trouble swallowing, and I have pain near my stomach. It feels like a hernia. I feel weak; I feel weak. When I eat, I feel weaker. When I eat. I have a hernia in my esophagus. An umbilical hernia. I have varicose ulcer. I have osteoporosis and arthrosis.”
Corroborating these findings, Forsyth et al. 31 interviewed individuals who reported physical complaints such as shortness of breath, weakness, and tiredness. The patients also reported that the presence of physical symptoms compromised their HRQoL: “There were strong palpitations that did not stop, and I felt my heart was very large. It is very uncomfortable because you do not have time to sleep or anything; you cannot relax with the constant jumping of your heart that is not at all normal.”
Another study 20 showed the impact of this disease on work activities and, consequently, on the patient’s HRQoL. The physical limitations are highlighted in the following statements: “[...] I cannot do anything I did before because everything tires me a lot and makes my chest feel tight and suffocate! If I didn’t have the disease, I would be working, I had to stop because of that”, “[...] Today I can’t work in the same way as before, it's exhausting, I feel weak and I have to rest.” and “Yes at home For hours, I cannot do things because of the pain; I feel unwell.”
Impact of fear of the future on HRQoL
Among the possible adverse events in patients with CD, sudden cardiac death may be the initial and/or most important manifestation of the disease 36 . Sudden cardiac death is the result of electrophysiological disturbances due to myocardial damage caused by the disease 37 . When people close to them who had CD suddenly died, patients with the disease experience extreme fear and insecurity about the future, especially of dying at any time, as reported in three studies 28 , 29 , 31 (moderate confidence).
One of the aforementioned studies 28 demonstrated reports about fear of the future: “Sometimes I was standing up like this and falling backward. This is Chagas disease. All the patients died suddenly. I would lie down to sleep, talk, and never get up,” or “I always heard: Chagas, Chagas (...) They say that whoever has Chagas, the person who is like that suddenly falls and dies! And it’s horrible! It’s like saying: ‘You have cancer!’ (...) It was like that for me at the time. Because I said: Gee, I’m doomed, I’m going to die soon,” and “People say these things: That Chagas... So-and-so died of Chagas, who would fall suddenly and die. This is how we heard about it. However, you know that even today, I still have it in my head from time to time. (...) This for me is death alone. Even that I think, do you understand? They say that whoever has Chagas, the person who is like this, falls down and dies suddenly!”
Ballester-Gil et al. 29 also reported some findings that corroborate the presence of fear of the future experienced by patients with CD: “I know this disease has no cure. I know I will die. I am sad; my life has changed since I got the result. I heard that Chagas disease has no cure, and I know I am going to die. The doctor explained how the disease and the exams were, but even though he was really polite and comforted me a lot, I know I am going to die.” Forsyth et al. 31 also observed interviews wherein patients with CD showed fear of the future and death: “I don’t want to die, I’m only 57. I want to see my family and my grandchildren grow.” and “Dying is what worries me. It has been 15 years since I am sick. I do not get better, but I do not die. But that’s my fear; I am getting on in age and I am always sick.”
Impact of Fear of treatment on HRQoL
CD tends to progress, and the available medications can be toxic and cause adverse side effects. Additionally, patients require permanent therapeutic measures, some of which are invasive, such as cardiac pacemakers. Two studies 29 , 31 highlighted the impact of fear of treatment on patients’ HRQoL (low confidence).
In a previous study 29 , the patients reported, “I’m all complicated. Where I am most nervous is because of this. I am afraid to put on a pacemaker. We see and hear on the television. I know that there is no cure. The pacemaker is a surgery to improve, but it has harmful effects. A pacemaker case can be a great success for a person, but it can also have serious consequences. Then, I get nervous about it. Besides, I have so many [problems] that if I did not have any of these businesses or other problems. If I were a healthy woman, and that's all, I would not have bothered to put a marker on. I am allergic, so I am afraid of everything and of putting a marker on that. And not feeling better and making my life worse.” And “Well, I asked the doctor and he said that tests are necessary, depending on the case and, in my case, depending on the state, I will have to put pacemaker. I know about the effects of the pacemaker on the person; it is very bad and the surgery is complicated.”
In addition to the fear of undergoing cardiac pacemaker implantation, drug treatment also caused fear in patients, as demonstrated in statements in the study of Forsyth et al. 31 : “From so much medicine you get scared, it frightens you, but you don’t want to die either, right? And sometimes I feel panicked, I feel scared, but the truth is I did the treatment because I do not want to die, I want to live, and thanks to it I have lived longer.”
DISCUSSION
This qualitative review is the first to identify the factors that impact the HRQoL of patients with CD, demonstrating that stigma, emotional and/or mental components, physical aspects and absence from work, fear of the future, and fear of treatment mostly affect the HRQoL of patients with chronic CD.
CD is among the neglected tropical diseases 38 . This phenomenon is caused by complex social, interpretive, and cultural processes 39 . Stigma is considered harmful to health and can cause intense psychosocial problems 40 , thus becoming a major concern of healthcare authorities and epidemiologists 41 . The stigma may be due to several sociocultural reasons that remain uncertain, but it may be related to work, where patients feel the fear of being terminated for having the disease or even insecurity of not being approved during the hiring interview. Studies on other health conditions have shown stigma as a marker of worse prognosis 42 - 44 , and people with CD have a greater tendency to be submissive and attacked by other people 45 . Therefore, due to the impact of stigma on the HRQoL of patients with CD, the present review reinforces the need to bring patients into the community, especially within the scope of primary healthcare. In addition to expanding public policies, encouraging conversations and health education strategies aimed at this neglected population should be implemented, particularly in endemic areas.
In addition to stigma, physical complaints and limitations at work can also affect the HRQoL of these patients. Physical limitations are noticeable in patients with the cardiac form of the disease, mainly due to progressive fatigue and dyspnea 46 . A systematic review and meta-analysis 47 showed that a reduction in exercise capacity is detectable from the early stages of heart disease; hence, it is necessary to stimulate strategies to improve the physical status of this population. Moreover, physical limitations are associated with worse levels of HRQoL 48 and are closely related to restrictions on activities and absence from work 34 . Workers with CD experience several adverse situations, such as a high rejection rate among job applicants and non-admission after showing positive results on pre-physical examinations or serological tests for the disease, regardless of the clinical status, in addition to being subject to dismissal without just cause 49 . Leaving from work predisposes patients with CD to future limitations as well as disability and marginalization, being part of a cycle between removal and increased inability to work 50 . International declarations consider work as a right for all and must be chosen by the individual under fair and favorable conditions 51 . However, this right has not been granted to the patients with CD 49 . In some cases, absence from work may occur as a result of physical impairments, which can affect the worker’s productivity and ability to perform work safely 35 .
Moreover, fear of the future can impact patients’ HRQoL. This can be explained by the prognosis of the condition, which may progress to megaesophagus, megacolon, esophageal motor disorders, diarrhea, and abdominal distension 52 , cardiac dysfunction 53 , functional impairment 47 , sudden cardiac death 36 , stroke, and heart transplantation 54 . With regard to fear of treatment, some patients reported fear of undergoing a device implantation such as a cardiac pacemaker. The implantation of a cardiac pacemaker may indicate having a weak heart or irregular beats 28 . Drug treatment was also pointed out as a reason for fear among this population, which is probably due to the possibility of severe adverse side effects caused by use of trypanocidal drugs (benznidazole and nifurtimox), such as cutaneous rash, gastrointestinal symptoms, and peripheral polyneuropathy 55 - 57 . In this scenario, communication is required between healthcare professionals and patients, especially regarding health education strategies. With empowerment and awareness of the prognosis and effects of treatment, patients can face the disease with a better HRQoL.
Finally, mental and/or emotional factors are important aspects of the HRQoL of patients with CD, as demonstrated by the high rate of depressive symptoms in the population 11 , 58 . The psyche is constructed through a complex interaction between the biological apparatus and social and cultural factors 59 . Stigma, fear of death, and inability to perform the activities of daily living are personal and environmental factors that can contribute to these symptoms 60 . Thus, the management of patients with chronic CD should not only involve the clinical but also the psychological aspects.
The present study has several strengths, limitations, and perspectives. In terms of strengths, the items that impact the HRQoL of patients with CD were systematically identified for the first time and the review was performed according to the suggested methodology. The results are of great clinical and scientific significance, as they can guide both the goals of clinical management and researchers’ choice of outcomes when performing new interventions in patients with CD.
As a limitation, all included studies selected patients in the chronic phase of the disease without stratifying the clinical form. Grouping patients with the indeterminate form together with patients with cardiac and digestive forms can be inappropriate because the needs, signs and symptoms, limitations, and prognoses can be different, which affects the HRQoL. Almost all studies were conducted in Brazil. Hence, further studies should be conducted in other Latin American countries, where the condition is highly prevalent and socioeconomic and cultural conditions are very heterogeneous 60 . Finally, one potentially eligible study was not evaluated owing to the lack of data for analysis. The author was contacted, but did not respond to the main researcher of the present review.
Therefore, a specific HRQoL assessment questionnaire for CD should be developed. Many of the factors identified in the present review that impact HRQoL, such as stigma and fear of treatment, were not addressed by the survey using generic questionnaires. Researchers have used generic questionnaires, such as the Short-Form Health Survey (SF-36), Abbreviated World Health Organization Quality of Life (WHOQoL-BREF), Minnesota Living with Heart Failure Questionnaire, Assessment of Quality of Life, and RELated Events 48 . Despite their wide use, they are not commonly used in assessing patients with CD. Therefore, the development of a specific questionnaire for assessing this disease is required to improve the assessment and monitoring of HRQoL in patients with CD.
Stigma, physical limitations, absence of work, mental and/or emotional aspects, fear of the future, and fear of treatment are factors cited by qualitative studies that most impact the HRQoL of patients with CD. Results showed moderate confidence and, despite these limitations, can help in clinical and scientific decision-making.
ACKNOWLEDGMENTS
None.
Footnotes
Ethics approval: The manuscript is a systematic review.
Financial Support: WTS was supported by a MSc. Studentship from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
REFERENCES
- 1.Kropf SP, Sá MR. The discovery of Trypanosoma cruzi and Chagas disease (1908-1909): tropical medicine in Brazil. Hist Cienc Saude Manguinhos. 2009;16(Suppl 1):13–34. doi: 10.1590/s0104-59702009000500002. [DOI] [PubMed] [Google Scholar]
- 2.Chagas C. Tripanosomiase americana: forma aguda da molestia. Mem Inst Oswaldo Cruz. 1916;8:37–60. [Google Scholar]
- 3.Perez-Molina JA, Molina I. Chagas disease. Lancet. 2018;391(10115):82–94. doi: 10.1016/S0140-6736(17)31612-4. [DOI] [PubMed] [Google Scholar]
- 4.Nunes MC, Dones W, Morillo CA, Encina JJ, Ribeiro AL. Council on Chagas Disease of the Interamerican Society of C. Chagas disease: an overview of clinical and epidemiological aspects. J Am Coll Cardiol. 2013;62(9):767–776. doi: 10.1016/j.jacc.2013.05.046. [DOI] [PubMed] [Google Scholar]
- 5.Rocha MO, Teixeira MM, Ribeiro AL. An update on the management of Chagas cardiomyopathy. Expert Rev Anti Infect Ther. 2007;5(4):727–743. doi: 10.1586/14787210.5.4.727. [DOI] [PubMed] [Google Scholar]
- 6.Ribeiro ALP, Rocha MOdC. Forma indeterminada da doença de Chagas: considerações acerca do diagnóstico e do prognóstico. Rev Soc Bras Med Trop. 1998;31(3):301–314. doi: 10.1590/s0037-86821998000300008. [DOI] [PubMed] [Google Scholar]
- 7.Andrade JPd, Marin-Neto J, Paola AAVd, Vilas-Boas F, Oliveira GMM, Bacal F, et al. I Diretriz Latino-Americana para o diagnóstico e tratamento da cardiopatia chagásica. Arq Bras Cardiol. 2011;97(2):01–48. [PubMed] [Google Scholar]
- 8.Renwick RE, Brown IE, Nagler ME. Quality of life in health promotion and rehabilitation: Conceptual approaches, issues, and applications. Illustrated edition. Sage Publications; Mar 26, 1996. [Google Scholar]
- 9.Gontijo EDG Tássia Nazareth, Magnani Cláudia, Paixão Gabriela Miana, Dupin Sanzio, Paixão Lúcia Miana. Qualidade de vida dos portadores de doença de Chagas. Rev Med Minas Gerais. 2009;19(4):281–285. [Google Scholar]
- 10.Oliveira BG, Abreu MNS, Abreu CDG, Rocha MOdC, Ribeiro AL. Health-related quality of life in patients with Chagas disease. Rev Soc Bras Med Trop. 2011;44(2):150–156. doi: 10.1590/s0037-86822011005000002. [DOI] [PubMed] [Google Scholar]
- 11.Ozaki Y, Guariento ME, de Almeida EA. Quality of life and depressive symptoms in Chagas disease patients. Qual Life Res. 2011;20(1):133–138. doi: 10.1007/s11136-010-9726-1. [DOI] [PubMed] [Google Scholar]
- 12.Pelegrino VM, Dantas RAS, Ciol MA, Clark AM, Rossi LA, Simões MV. Health-related quality of life in Brazilian outpatients with Chagas and non-Chagas cardiomyopathy. Heart & Lung. 2011;40(3):e25-e31. doi: 10.1016/j.hrtlng.2010.05.052. [DOI] [PubMed] [Google Scholar]
- 13.Costa HS, Lima MMO, Figueiredo PHS, Chaves AT, Nunes MCP, da Costa Rocha MO. The prognostic value of health-related quality of life in patients with Chagas heart disease. Qual Life Res. 2019;28(1):67–72. doi: 10.1007/s11136-018-1980-7. [DOI] [PubMed] [Google Scholar]
- 14.Almeida I, Oliveira LFL, Figueiredo PHS, Oliveira RDB, Damasceno TR, Silva WT, et al. The health-related quality of life in patients with Chagas disease: the state of the art. Rev Soc Bras Med Trop. 2022;55:e0657. doi: 10.1590/0037-8682-0657-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ávila MR, Figueiredo PHS, Lima VP, Silva WT, Vianna MVA, Fernandes LHC, et al. Accuracy of health-related quality of life in identifying systolic dysfunction in patients with Chagas cardiomyopathy. Trop Med Int Health. 2021;26(8):936–942. doi: 10.1111/tmi.13590. [DOI] [PubMed] [Google Scholar]
- 16.Juniper EF, Guyatt GH, Jaeschke R. Quality of life and pharamacoeconomics in clinical trials. 2nd Edition. Lippincott-Raven Publishers; Philadelphia: 1996. How to develop and validate a new health-related quality of life instrument; pp. 49–56. [Google Scholar]
- 17.Pope C, Van Royen P, Baker R. Qualitative methods in research on healthcare quality. BMJ Qual Saf. 2002;11(2):148–152. doi: 10.1136/qhc.11.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Busaidi ZQ. Qualitative research and its uses in health care. Sultan Qaboos Univ Med J. 2008;8(1):11–19. [PMC free article] [PubMed] [Google Scholar]
- 19.Whitehead AL, Sully BG, Campbell MJ. Pilot and feasibility studies: is there a difference from each other and from a randomised controlled trial? Contemp Clin Trials. 2014;38(1):130–133. doi: 10.1016/j.cct.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):1–8. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh J. Critical appraisal skills programme. J Pharmacol Pharmacother. 2013;4(1):76–76. [Google Scholar]
- 23.Programme CAS . CASP qualitative checklist. 2018. [2022 July 2022]. Available from: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf . [Google Scholar]
- 24.Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. Journal of health services research & policy. 2002;7(4):209–215. doi: 10.1258/135581902320432732. [DOI] [PubMed] [Google Scholar]
- 25.Higgins J. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2011. https://handbook-5-1.cochrane.org/ [Google Scholar]
- 26.Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. BioMed Central. 2018:1–10. doi: 10.1186/s13012-017-0688-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Araújo SMd, Andó MH, Cassarotti DJ, Mota DCGDA, Borges SMR, Gomes ML. Programa ACHEI: atenção ao chagásico com educação integral no município de Maringá e região noroeste do Paraná, Brasil. Rev Soc Bras Med Trop. 2000;33:565–572. doi: 10.1590/s0037-86822000000600008. [DOI] [PubMed] [Google Scholar]
- 28.Magnani C, Oliveira BG, Gontijo ED. Representations, myths, and behaviors among Chagas disease patients with pacemakers. Cad Saude Publica. 2007;23:1624–1632. doi: 10.1590/s0102-311x2007000700013. [DOI] [PubMed] [Google Scholar]
- 29.Ballester-Gil LM, Stotz EN, Hasslocher-Moreno AM, Azevedo BAd, Araújo-Jorge TCd. O saber do paciente chagásico sobre a sua doença: construção compartilhada de um instrumento para a pesquisa e teste de sua aplicabilidade. Cien Saude Colet. 2008;13:2199–2214. doi: 10.1590/s1413-81232008000900025. [DOI] [PubMed] [Google Scholar]
- 30.Oliveira APd, Gomes LF, Casarin ST, Siqueira HCHd. The life of the patient with chronic Chagas disease: possible nursing actions towards a healthy life. Rev Gaucha Enferm. 2010;31(3):491–498. doi: 10.1590/s1983-14472010000300012. [DOI] [PubMed] [Google Scholar]
- 31.Forsyth CJ, Hernandez S, Flores CA, Roman MF, Nieto JM, Marquez G, et al. “You Don’t Have a Normal Life”: Coping with Chagas Disease in Los Angeles, California. Med Anthropol. 2021;40(6):525–540. doi: 10.1080/01459740.2021.1894559. [DOI] [PubMed] [Google Scholar]
- 32.Nascimento LAd, Leão A. Estigma social e estigma internalizado: a voz das pessoas com transtorno mental e os enfrentamentos necessários. Hist Cienc Saude Manguinhos. 2019;26:103–121. doi: 10.1590/S0104-59702019000100007. [DOI] [PubMed] [Google Scholar]
- 33.Olivera MJ, Buitrago G. Economic costs of Chagas disease in Colombia in 2017: A social perspective. Int J Infect Dis. 2020;91:196–201. doi: 10.1016/j.ijid.2019.11.022. [DOI] [PubMed] [Google Scholar]
- 34.Lee BY, Bacon KM, Bottazzi ME, Hotez PJ. Global economic burden of Chagas disease: a computational simulation model. Lancet Infect Dis. 2013;13(4):342–348. doi: 10.1016/S1473-3099(13)70002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am. J. Card. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 36.Rassi A, Jr, Rassi SG, Rassi A. Morte súbita na Doença de Chagas. Arq Bras Cardiol. 2001;76(1):75–85. doi: 10.1590/s0066-782x2001000100008. [DOI] [PubMed] [Google Scholar]
- 37.Lopes ER. Sudden death in patients with Chagas disease. Mem Inst Oswaldo Cruz. 1999;94:321–324. doi: 10.1590/s0074-02761999000700061. [DOI] [PubMed] [Google Scholar]
- 38.Hofstraat K, van Brakel WH. Social stigma towards neglected tropical diseases: a systematic review. Int. Health. 2016;8(suppl_1):i53-i70. doi: 10.1093/inthealth/ihv071. [DOI] [PubMed] [Google Scholar]
- 39.Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: Adding moral experience to stigma theory. Soc Sci Med. 2007;64(7):1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 40.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Link B, Hatzenbuehler ML. Stigma as an unrecognized determinant of population health: Research and policy implications. J Health Polit Policy Law. 2016;41(4):653–673. doi: 10.1215/03616878-3620869. [DOI] [PubMed] [Google Scholar]
- 42.Austen E, Griffiths S. Weight stigma predicts reduced psychological wellbeing and weight gain among sexual minority men: A 12-month longitudinal cohort study using random intercept cross-lagged panel models. Body Image. 2022;40:19–29. doi: 10.1016/j.bodyim.2021.10.006. [DOI] [PubMed] [Google Scholar]
- 43.Bebell LM, Kembabazi A, Musinguzi N, Martin JN, Hunt PW, Boum Y, et al. Internalized stigma, depressive symptoms, and the modifying role of antiretroviral therapy: A cohort study in rural Uganda. SSM Ment Health. 2021;1:100034–100034. doi: 10.1016/j.ssmmh.2021.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nousak S. Cohorts & Perceived Social Stigma of Mental Illness by Education. 2015. https://etd.ohiolink.edu/apexprod/rws_olink/r/1501/10?clear=10&p10_accession_num=kent1585922193114882
- 45.Logie CH, Marcus N, Wang Y, Kaida A, O'Campo P, Ahmed U, et al. A longitudinal study of associations between HIV-related stigma, recent violence and depression among women living with HIV in a Canadian cohort study. Int J STD AIDS. 2019;22(7):e25341. doi: 10.1002/jia2.25341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Costa HS, Lima MMO, Figueiredo PHS, Lima VP, Avila MR, Menezes KKP, et al. Exercise tests in Chagas cardiomyopathy: an overview of functional evaluation, prognostic significance, and current challenges. Rev Soc Bras Med Trop. 2020;53:e20200100. doi: 10.1590/0037-8682-0100-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Costa HS, Lima MMO, Costa FSMd, Chaves AT, Nunes MCP, Figueiredo PHS, et al. Reduced functional capacity in patients with Chagas disease: a systematic review with meta-analysis. Rev Soc Bras Med Trop. 2018;51(4):421–426. doi: 10.1590/0037-8682-0158-2018. [DOI] [PubMed] [Google Scholar]
- 48.Sousa GR, Costa HS, Souza AC, Nunes MCP, Lima MMO, Rocha MOdC. Health-related quality of life in patients with Chagas disease: a review of the evidence. Rev Soc Bras Med Trop. 2015;48(2):121–128. doi: 10.1590/0037-8682-0244-2014. [DOI] [PubMed] [Google Scholar]
- 49.Guariento ME, Camilo MVF, Camargo AMA. Working conditions of Chagas' disease patients in a large Brazilian city. Cad Saude Publica. 1999;15(2):381–386. doi: 10.1590/s0102-311x1999000200022. [DOI] [PubMed] [Google Scholar]
- 50.Hultin H, Lindholm C, Möller J. Is there an association between long-term sick leave and disability pension and unemployment beyond the effect of health status?-a cohort study. PloS one. 2012;7(4):e35614. doi: 10.1371/journal.pone.0035614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morsink J. The Universal Declaration of Human Rights: Origins, Drafting, and Intent. University of Pennsylvania Press; 2010. pp. 282–329. [Google Scholar]
- 52.De Oliveira RB, Troncon LEA, Dantas RO, Meneghelli UG. Gastrointestinal manifestations of Chagas’ disease. Am J Gastroenterol. 1998;93(6):884–889. doi: 10.1111/j.1572-0241.1998.270_r.x. [DOI] [PubMed] [Google Scholar]
- 53.Ribeiro AL, Moraes RS, Ribeiro JP, Ferlin EL, Torres RM, Oliveira E, et al. Parasympathetic dysautonomia precedes left ventricular systolic dysfunction in Chagas disease. Am Heart J. 2001;141(2):260–265. doi: 10.1067/mhj.2001.111406. [DOI] [PubMed] [Google Scholar]
- 54.Pérez-Molina JA, Molina I. Chagas disease. The Lancet. 2018;391(10115):82–94. doi: 10.1016/S0140-6736(17)31612-4. [DOI] [PubMed] [Google Scholar]
- 55.Coronel MVP, Muñoz EC, Valle DK, Rojas DHFd. Adverse systemic reaction to benznidazole. Rev Soc Bras Med Trop. 2017;50(1):145–147. doi: 10.1590/0037-8682-0071-2016. [DOI] [PubMed] [Google Scholar]
- 56.Viotti R, Vigliano C, Lococo B, Alvarez MG, Petti M, Bertocchi G, et al. Side effects of benznidazole as treatment in chronic Chagas disease: fears and realities. Expert Rev Anti Infect Ther. 2009;7(2):157–163. doi: 10.1586/14787210.7.2.157. [DOI] [PubMed] [Google Scholar]
- 57.Vallejo M, Reyes PPA, Martinez Garcia M, Gonzalez Garay AG. Trypanocidal drugs for late-stage, symptomatic Chagas disease (Trypanosoma cruzi infection) Cochrane Database Syst Rev. 2020;(12) doi: 10.1002/14651858.CD004102.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Silva WT, Ávila MR, Oliveira LFFd, Figueiredo PHS, Lima VP, AdC Bastone, et al. Prevalence and determinants of depressive symptoms in patients with Chagas cardiomyopathy and predominantly preserved cardiac function. Rev Soc Bras Med Trop. 2020:53–53. doi: 10.1590/0037-8682-0123-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bodrova E, Leong DJ, Akhutina TV. When everything new is well-forgotten old: Vygotsky/Luria insights in the development of executive functions. New Dir Child Adolesc Dev. 2011;2011(133):11–28. doi: 10.1002/cd.301. [DOI] [PubMed] [Google Scholar]
- 60.Forsyth CJ. "I Cannot Be Worried": Living with Chagas Disease in Tropical Bolivia. PLoS Negl Trop Dis. 2017;11(1):e0005251. doi: 10.1371/journal.pntd.0005251. [DOI] [PMC free article] [PubMed] [Google Scholar]