Abstract
Background
The rapid spread of coronavirus disease 2019 in the United States led to a variety of mandates intended to decrease population movement and “flatten the curve.” However, there is evidence some are not able to stay-at-home due to certain disadvantages, thus remaining exposed to both coronavirus disease 2019 and trauma. We therefore sought to identify any unequal effects of the California stay-at-home orders between races and insurance statuses in a multicenter study utilizing trauma volume data.
Methods
A posthoc multicenter retrospective analysis of trauma patients presenting to 11 centers in Southern California between the dates of January 1, 2020, and June 30, 2020, and January 1, 2019, and June 30, 2019, was performed. The number of trauma patients of each race/insurance status was tabulated per day. We then calculated the changes in trauma volume related to stay-at-home orders for each race/insurance status and compared the magnitude of these changes using statistical resampling.
Results
Compared to baseline, there was a 40.1% drop in total trauma volume, which occurred 20 days after stay-at-home orders. During stay-at-home orders, the average daily trauma volume of patients with Medicaid increased by 13.7 ± 5.3%, whereas the volume of those with Medicare, private insurance, and no insurance decreased. The average daily trauma volume decreased for White, Black, Asian, and Latino patients with the volume of Black and Latino patients dropping to a similar degree compared to White patients.
Conclusion
This retrospective multicenter study demonstrated that patients with Medicaid had a paradoxical increase in trauma volume during stay-at-home orders, suggesting that the most impoverished groups remain disproportionately exposed to trauma during a pandemic, further exacerbating existing health disparities.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic spread rapidly across the United States, leading to a variety of state-issued actions intended to “flatten the curve.”1 , 2 Though differing in duration and stringency, mandates requiring most citizens to stay home were issued and led to a decrease in population movement.3 , 4
Unfortunately, both the COVID-19 virus and subsequent restrictions impacted certain groups disproportionately.5, 6, 7, 8, 9, 10 For example, stay-at-home (SAH) orders may be less effective for people with lower income as they are less likely to be able to work from home.11 , 12 Similarly, people of color comprise a larger portion of the essential workforce and are more likely to continue working despite SAH orders.13 , 14 These disparities pose a significant threat to the groups of people who are unable to stay “safer at home” and subsequently have more exposure to the COVID-19 virus.15
In addition, people unable to SAH have increased exposure to traumatic injury (ie, work-related, motor vehicle collision during commute, etc), the third leading cause of death in the United States.16 Therefore, trauma data represent a unique fund of information that could identify groups with continued exposure to both COVID-19 and trauma. Though some studies have detailed a large decrease in total trauma volume resulting from SAH orders despite increases in firearm-related penetrating trauma, none have described any differences by race or socioeconomic status.17, 18, 19, 20, 21
Thus, we sought to describe the effects of the state of California’s March 19, 2020, SAH orders on trauma volume for each race and insurance status in a multicenter study across 7 counties in Southern California.22 We hypothesized that Black and Latino patients, as well as uninsured and Medicaid patients, would have less of a decline in trauma volume after SAH orders compared to other races and insurance types.
Methods
A posthoc multicenter retrospective analysis of all trauma patients presenting to 11 American College of Surgeons (ACS) level I and II trauma centers across Southern California was performed between the dates of January 1, 2020, and June 30, 2020, and January 1, 2019, and June 30, 2019.20 This study was approved by the Institutional Review Board of the University of California, Irvine, as well as all other participating institutions and was deemed exempt from the need for consent. Included in this study were all patients within each institution’s trauma registry, comprised of both trauma activations and trauma consults where a trauma surgeon evaluated the patient after arrival. The primary outcomes were race and insurance status. Race was self-reported and included White, Black, Asian, Latino, and other. Insurance status included Medicare, Medicaid, private, or uninsured.
First, the total number of trauma patients presenting across all institutions per day was tabulated. To improve the signal-to-noise in our data analysis, we applied a smoothing operation. We chose a Gaussian kernel for smoothing for its favorable minimization of truncation effects compared to a simple sliding window average. The width of the Gaussian kernel function was chosen as small as possible to respect the signal in the raw data while eliminating the presentation of stochastic daily variations. The daily trauma data for 2019 and 2020 was plotted with a Gaussian smoothing width of 3 days. The fewest number of patients presenting per day in 2020 was identified. This value was compared to a 60-day average from January 1, 2020, to February 29, 2020, (2020 baseline) to calculate the drop from baseline.
Next, the number of trauma patients of each race and insurance status were tabulated per day. Gaussian smoothing was again performed with the width of the smoothing set to a standard deviation of 7 days. A mean of 2020 baseline was calculated for each group and the data was normalized using this value, allowing for visual comparison. The normalized and smoothed data was plotted by race and insurance status in separate plots. The furthest percentage drop below baseline was calculated for each group. The amount of time spent below 75% of baseline for each group was also identified to provide a temporal description of these changes.
We then sought to compare the change in trauma volume across different insurance statuses and races. First, the baseline proportion of trauma volume for each group was established using the 2020 baseline period. Then, the proportional change in average daily trauma volume from the 2020 baseline to March 1, 2020, to June 1, 2020, the period when trauma volume appeared most affected, was calculated for each group. We estimated the uncertainties in these quantities using statistical resampling. Ten thousand random trials were simulated for each group by sampling with replacement on daily visit values. Standard deviations were calculated using those random samples. For each trial, the percentage change in average daily trauma volume between periods was compared between each group. A P value for a presumptive difference between groups was then estimated by the number of trials wherein the values for 1 group exceeded that for the other.
Next, to further confirm proportional changes in trauma volume during the SAH period, the 2020 SAH period was compared to the same period in 2019. The proportion of each group between March 1, 2019, and June 1, 2019, was compared to the proportion between March 1, 2020, and June 1, 2020, using a χ2 analysis.
Finally, we evaluated for any disproportionate changes in penetrating trauma rates for each insurance status and race. That is, the penetrating trauma rates between January 1, 2020, to February 29, 2020, and March 1, 2020, to June 1, 2020, were compared for each group using a χ2 analysis. We also looked specifically at the Medicaid population for any other significant changes in mechanism of injury over time. Rates of ground level falls, falls from height, pedestrians struck, motorcycle collisions, motor vehicle collisions, assaults, sports injuries, gunshot wounds, and stab wounds were compared between these 2 time periods using a χ2 analysis. P values were 2-tailed. All analysis and figure creation were performed using Python 3.8.
Results
Overall trauma volume
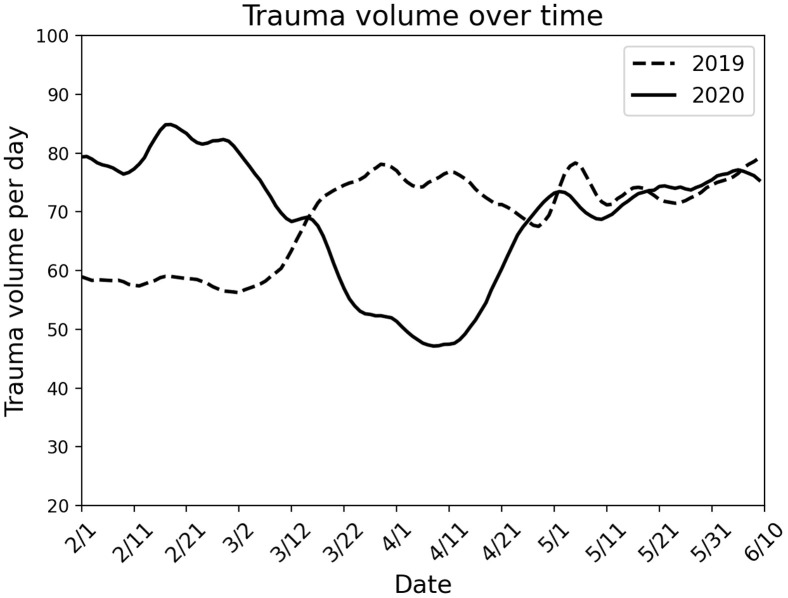
Between January 1, 2019, and June 30, 2019, 12,316 trauma patients were identified; 12,744 patients were identified between January 1, 2020, and June 30, 2020. The 2020 baseline was 78.8 trauma activations per day. The lowest smoothed number of trauma activations per day across all institutions was 47.2, representing a 40.1% drop from the 2020 baseline, and occurred on April 8, 2020, 20 days after SAH orders. The number of trauma activations per day returned to 90% of baseline on April 29, 2020 (Fig 1 ).
Fig. 1.
Comparison of trauma volume from February through June in 2020 and 2019. Total cases per day were accumulated across 11 participating sites. California stay-at-home orders were initiated on March 19, 2020. The curves were subjected to a smoothing function (see Methods).
Trauma volume by insurance status
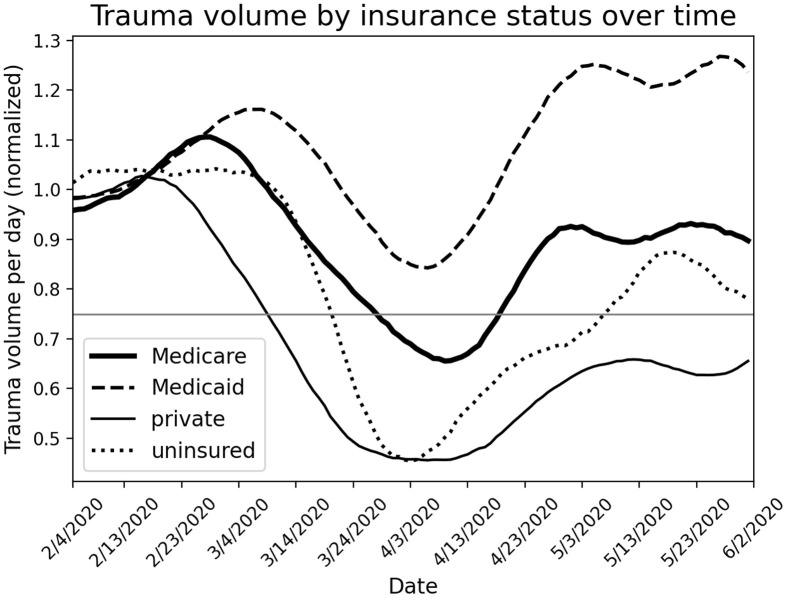
Description over time
The daily volume of trauma patients with Medicaid dropped to 15.7% below baseline at its lowest and rebounded to above baseline at the end of the study period. Medicare daily volume dropped to 34.5% below baseline and persisted below 75% of baseline for 22 days. Uninsured volume dropped to 54.6% below baseline and stayed below 75% of baseline for 50 days. The volume of patients with private insurance dropped to 54.4% below baseline and did not return to 75% of baseline during the study period (Fig 2 ).
Fig. 2.
Comparison of trauma volume over time as a function of patient insurance. The trauma volume numbers were normalized to a value of 1 for all insurance types over an initial time period (20 days). The curves were subjected to a smoothing function (see Methods). The horizontal line highlights the condition of 25% reduction from initial volume.
Comparison between time periods
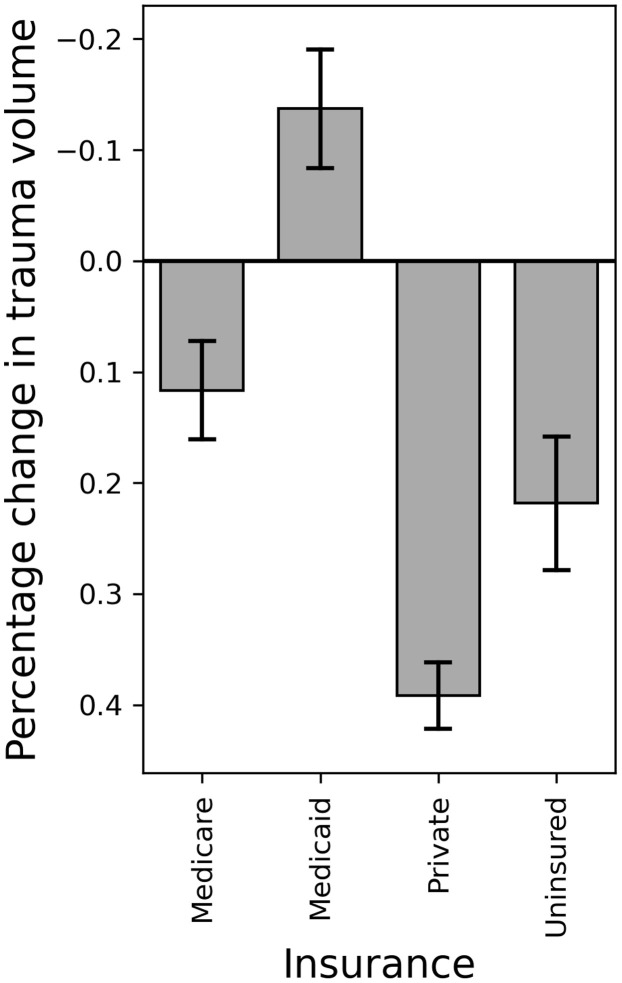
From January 1, 2020, through February 29, 2020, to March 1, 2020, through June 1, 2020, the average daily trauma volume decreased 11.7 ± 4.4% for Medicare patients, 39.1 ± 3.0% for private insurance patients, and 21.8 ± 6.0% for patients without insurance. The average daily trauma volume of Medicaid patients increased by 13.7 ± 5.3% (Fig 3 ).
Fig. 3.
Changes in daily trauma volume between pre and post stay-at-home orders (January 1, 2020, to February 29, 2020, versus March 1, 2020 to June 1, 2020) according to insurance type. Positive values (downward pointing bars) indicate a drop in volume during the stay-at-home period. The error bars indicate the uncertainty in the percentage drop expressed as a root mean square deviation from the observed value across random statistical resampling simulations (see Methods).
From March 1, 2019, through June 1, 2019, to March 1, 2020, through June 1, 2020, the proportion of trauma patients with Medicare (19.1% vs 21.7%, P = .004) and Medicaid (19.7% vs 35.2%, P < .001) increased. The proportion of patients with private insurance (40.7% vs 29.0%, P = .001) decreased. The proportion of patients with no insurance was similar between time periods (P = .06) (Table I ).
Table I.
Comparison of proportional trauma volume by race and insurance statuses between March 1, 2019, through June 1, 2019, and March 1, 2020 through June 1, 2020
| Characteristic | 2019 (n = 6687) | 2020 (n = 6014) | P value |
|---|---|---|---|
| Insurance status | |||
| Medicare | 1280 (19.1%) | 1305 (21.7%) | .004 |
| Medicaid | 1987 (29.7%) | 2115 (35.2%) | <.001 |
| Private | 2722 (40.7%) | 1747 (29.0%) | .001 |
| Uninsured | 484 (7.2%) | 487 (8.1%) | .069 |
| Race | |||
| White | 3258 (48.7%) | 2780 (46.2%) | .005 |
| Black | 537 (8.0%) | 518 (8.6%) | .235 |
| Asian | 340 (5.1%) | 275 (4.6%) | .180 |
| Latino | 1936 (29.0%) | 2001 (33.3%) | <.001 |
Comparison between insurance statuses
From January 1, 2020–February 29, 2020, to March 1, 2020–June 1, 2020, the trauma volume of Medicaid patients decreased significantly less when compared to patients with Medicare, private insurance, and no insurance (all P < .05). The volume of patients with private insurance decreased significantly more compared to patients with Medicare and no insurance (all P < .05). No other significant differences between groups were found (Table II ).
Table II.
Comparison of changes in daily trauma volume from January 1, 2020, through February 29, to March 1, 2020, through June 1, 2020, across insurance statuses
| Medicare | Medicaid | Private | Uninsured | |
|---|---|---|---|---|
| Medicare | 11.7% vs –13.7% P < .001 |
11.7% vs 39.1% P <.001 |
11.7% vs 21.8% P = .084 |
|
| Medicaid | –13.7% vs 39.1% P < .001 | –13.7% vs 21.8% P < .001 | ||
| Private | 39.1% vs 21.8% P = .002 |
|||
| Uninsured |
Displayed as average drop per insurance status in column vs average drop per insurance status in row.
Trauma volume by race
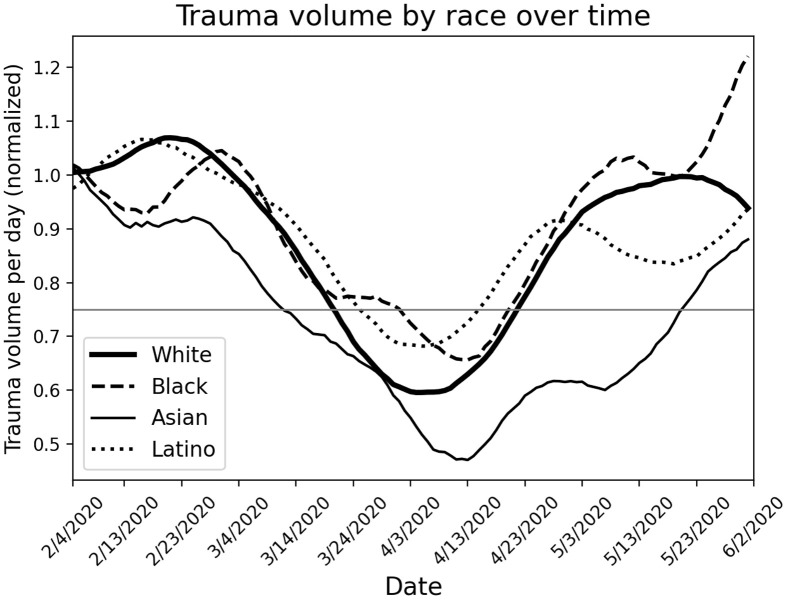
Description over time
The daily volume of trauma patients of Black race dropped to 34.4% below baseline at its lowest and persisted below 75% of baseline for 20 days. The daily volume of Latino patients dropped to 31.8% below baseline and stayed below 75% of baseline for 21 days. The daily volume of White patients fell to 40.4% below baseline and stayed below 75% of baseline for 32 days. The volume of Asian patients fell to 53.0% below baseline at its lowest and stayed below 75% of baseline for 70 days (Fig 4 ).
Fig. 4.
Comparison of trauma volume over time as a function of patient race. The trauma volume numbers were normalized to a value of 1 for all races over an initial time period (20 days). The curves were subjected to a smoothing function (see Methods). The horizontal line highlights the condition of 25% reduction from initial volume.
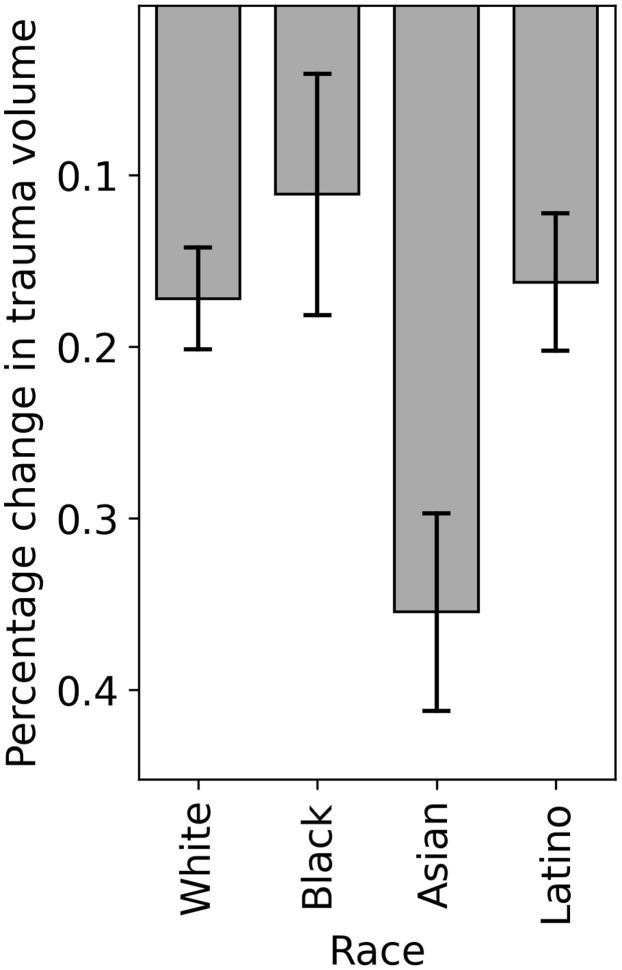
Comparison between time periods
From January 1, 2020, through February 29, 2020, to March 1, 2020, through June 1, 2020, the average daily trauma volume dropped 17.2 ± 3.0% for White patients, 11.1 ± 7.1% for Black patients, 35.5 ± 5.8% for Asian patients, and 16.2 ± 3.9% for Latino patients (Fig 5 ).
Fig. 5.
Changes in daily trauma volume between pre and post stay-at-home orders (January 1, 2020, to February 29, 2020 versus March 1, 2020 to June 1, 2020) according to patient race. Positive values (downward pointing bars) indicate a drop in volume during the stay-at-home period. The error bars indicate the uncertainty in the percentage drop expressed as a root mean square deviation from the observed value across random statistical resampling simulations (see Methods).
From March 1, 2019, through June 1, 2019, to March 1, 2020, through June 1, 2020, the proportion of Latino patients increased (29.0% vs 33.3%, P < .001) and the proportion of White patients decreased (48.7% vs 46.2%, P = .005). The proportion of Black and Asian patients was similar between time periods (all P > .05) (Table I).
Comparison between races
The trauma volume for Asian patients showed a significantly greater reduction when compared to that of White, Black, and Latino patients (all P < .05). Other comparisons between groups were not significant (Table III ).
Table III.
Comparison of changes in daily trauma volume from January 1, 2020, through February 29, 2020, to March 1, 2020, through June 1, 2020 across races
| White | Black | Asian | Latino | |
|---|---|---|---|---|
| White | 17.2% vs 11.1% P = .207 |
17.2% vs 35.5% P = .004 |
17.2% vs 16.2% P = .419 |
|
| Black | 11.1% vs 35.5% P = .003 |
11.1% vs 16.2% P = .260 | ||
| Asian | 35.5% vs 16.2% P = .005 |
|||
| Latino |
Displayed as average drop per race in column versus average drop per race in row.
Penetrating trauma rates over time
By insurance status
From January 1, 2020, through February 29, 2020 to March 1, 2020, through June 1, 2020, penetrating trauma rates decreased significantly for patients with Medicare (6.8% vs 2.8%, P < .001), but increased for those with Medicaid (16.6% vs 21.1%, P = .002). Penetrating trauma rates were similar across both time periods for patients with private and no insurance (all P > .05) (Table IV ).
Table IV.
Comparison of penetrating trauma rates by insurance status and race between January 1, 2020, through February 29, 2020, and March 1, 2020, through June 1, 2020
| Characteristic | 1/1/2020–2/29/2020 | 3/1/2020–6/1/2020 | P value |
|---|---|---|---|
| Insurance status | |||
| Medicare | 66/976 (6.8%) | 36/1293 (2.8%) | <.001 |
| Medicaid | 204/1228 (16.6%) | 445/2113 (21.1%) | .002 |
| Private | 160/1894 (8.4%) | 163/1729 (9.4%) | .301 |
| Uninsured | 67/416 (16.1%) | 88/475 (18.5%) | .342 |
| Race | |||
| White | 113/2166 (5.2%) | 230/2780 (8.3%) | <.001 |
| Black | 93/376 (24.7%) | 111/518 (21.4%) | .245 |
| Asian | 18/275 (6.5%) | 19/275 (6.9%) | .865 |
| Latino | 214/1541 (13.9%) | 370/2001 (18.5%) | <.001 |
By race
From January 1, 2020, through February 29, 2020, to March 1, 2020, through June 1, 2020, penetrating trauma rates increased significantly for both White (5.2% vs 8.3%, P < .001) and Latino patients (13.9% vs 18.5%, P < .001). Penetrating trauma rates were similar across both time periods for Black and Asian patients (all P > .05) (Table IV).
Changes in traumatic mechanism over time for Medicaid patients
Among patients with Medicaid, from January 1, 2020, through February 29, 2020, to March 1, 2020, through June 1, 2020, there was a significant decrease in the rates of blunt trauma (83.4% vs 78.9%, P = .002) and pedestrians struck (11.2% vs 8.2%, P = .005) but an increase in rates of penetrating trauma (16.6% vs 21.1%, P = .002) and gunshot wounds (5.3% vs 7.5%, P = .015). The rates of all other mechanisms were similar between the 2 time periods (all P > .05).
Comparing the racial compositions across insurance statuses
Of those presenting between March 1, 2020, and June 1, 2020, the Medicaid population had a significantly higher percentage of Black and Latino patients compared to the non-Medicaid population (57.1% vs 33.6%, P < .001).
Discussion
The COVID-19 pandemic and subsequent restrictions on populations have resulted in a number of reported racial and socioeconomic disparities.5, 6, 7, 8, 9 , 12, 13, 14 This posthoc analysis of a multicenter study demonstrated the overall trauma volume decreased after SAH orders, with the magnitude of the effect varying substantially according to insurance status. The trauma volume of Medicaid patients, and to a smaller degree Medicare and uninsured patients, was less affected than those with private insurance who became less involved in traumatic injuries, supporting our hypothesis. Black and Latino patients experienced similar changes in trauma volume compared to White patients, at least within the bounds of statistical significance, contrary to our original hypothesis.
The COVID-19 SAH orders have had an unequally harsh impact on the poor.11 , 12 This study on trauma patients further affirms this as the trauma volume of patients with Medicaid, reserved for those with low and very low incomes, was the least affected (ie, least protected) by SAH.23 In fact, Medicaid patients were the only group in this study to have an increase in daily trauma volume related to SAH orders. This further supports location data demonstrating that more impoverished people are less likely to benefit from SAH orders in the United States.12 We believe this is most likely due to the inability of lower income individuals to either work from home or stop working for an extended period of time.11 Though we lack occupational data needed to prove this conjecture, it is partially supported by our Medicaid population having a significantly larger percentage of Black and Latino patients, who make up a disproportionately large amount of the essential workforce, compared to our non-Medicaid population.13 Additionally, further analysis of the changes in traumatic mechanism before and after SAH orders within our Medicaid population showed no difference in rates of motor vehicle collisions, which likely reflects continued commutes to work during the SAH period. Also, important to note is that Medicaid was the only insurance status with a significant increase in penetrating trauma rates after SAH orders, suggesting that the poorest segment of our population was most affected by the spikes in violent crime.20 , 21 Interestingly, Medicare patients were the second least affected by SAH orders. This may be related to the mechanism of injury in this population being predominantly ground level falls, which can occur at home and thus may not be affected by SAH orders.24 , 25 In addition, this population is also more likely to require ongoing medical care and thus may actually still be leaving home. Surprising to the authors, by inference from the trauma volume data, uninsured patients may represent the next most able to stay at home. This could be due to the diversity of the uninsured population, which spans self-employed patients (including people who already work from home) of higher income who choose not to purchase insurance to undocumented patients.26 , 27 Overall, our findings suggest that the most impoverished groups remain exposed to not only COVID-19 but also traumatic injury, potentially due to their inability to SAH.28 , 29 These economic disparities should be acknowledged and addressed to allow for equal protection of all socioeconomic groups during a pandemic.
The COVID-19 pandemic has also resulted in a number of health and economic disparities across races.5, 6, 7, 8, 9 , 12 , 14 Although Black and Latino patients appeared less protected by SAH orders than White and Asian patients by some metrics, their change in trauma volume compared to White patients was not significant. This pushes against the notion that people of color are more likely to disregard SAH orders.30, 31, 32 The absence of a statistically significant finding by race could be due to a variety of factors. Patterns of injury and trauma care utilization are driven by a complex interplay of epidemiological risk factors, access challenges, and care-seeking behaviors, among others, and teasing these out are beyond the scope of this study. Moreover, limitations of the study design may have prevented us from detecting a difference when in fact one truly exists. Regardless, pandemic-related racial disparities must be urgently addressed via financial support, community outreach, and other novel programs.
Predicting trauma volume accurately is important for hospital staffing and resource allocation, especially during a pandemic that has considerably stressed hospital systems.19 , 33 At the lowest point, we identified a 40% decrease in total trauma volume, which is similar to the 43% decrease described by Leichtle et al in a single center study in Virginia.17 Interestingly, the lowest trauma volume our region experienced was 20 days after SAH orders, perhaps indicating that large-scale behavioral changes take a considerable amount of time to take effect. The overall trauma volume rebounded to near baseline 41 days after SAH orders were issued, likely due to a combination of partial reopening and waning compliance for the continued restrictions.22 Surprisingly, this rebound occurred and was sustained as new COVID-19 cases were increasing in California (Apr 29, 2020–2,000 cases/day, Jun 30, 2020–8,000 cases/day), indicating that disease burden in the region is less important than SAH orders with regards to predicting trauma volume.34 We suggest that healthcare organizations and trauma systems take into account the volume reduction and timing of changes seen in this study when planning for future SAH orders.
There are a number of limitations to this study. First, this study utilized multiple trauma registries, making it susceptible to missing information and misclassification, such as data on patients with traumatic injuries who presented to nontrauma hospitals. It is also unclear how different registries handled categorization of multi-ethnic/racial patients. Second, although initial SAH orders applied to the entire state, restrictions were partially lifted in different counties to varying degrees in the following months due to differences in local infection rates. In addition, given the wide variations in race and socioeconomic status across Southern California counties, these lightened restrictions could have affected our results. Also, as mentioned previously, we evaluated outcomes with respect to insurance status, which is not an adequate proxy for socioeconomic status or class, and thus represents a heterogeneous population.35 Future research, which controls for factors related to socioeconomic status and/or class would help further elucidate the exact causes for disparities observed in this study. We therefore suggest that future trauma registry data include variables that more accurately depict socioeconomic status, such as occupation, place of residence, level of education, and household income, amongst others.36
In conclusion, this retrospective multicenter study demonstrated a paradoxical increase in the trauma volume of patients with Medicaid during California SAH orders, suggesting they are the least able to SAH. Evidently, the most impoverished groups remain disproportionately exposed to trauma even during a pandemic, further exacerbating existing health disparities. This highlights the importance of addressing economic health disparities before and during a pandemic or other disaster.
Funding/Financial support
The authors received no funding or financial support for this study.
Conflict of interest/Disclosure
The authors have no related conflicts of interest to declare.
References
- 1.Matrajt L., Leung T. Evaluating the Effectiveness of Social Distancing Interventions to Delay or Flatten the Epidemic Curve of Coronavirus Disease. Emerg Infect Dis. 2020;26:1740–1748. doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Conference of State Legislatures State action on coronavirus (COVID-19); 2021. https://www.ncsl.org/research/health/state-action-on-coronavirus-covid-19.aspx
- 3.Moreland A., Herlihy C., Tynan M.A., Sunshine G., McCord R.F., Hilton C., et al. Timing of state and territorial covid-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1198–1203. doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobsen G.D., Jacobsen K.H. Statewide COVID-19 Stay-at-home orders and population mobility in the United States. World Med Health Policy. 2020;12:347–356. doi: 10.1002/wmh3.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owen W.F., Jr., Carmona R., Pomeroy C. Failing Another national stress test on health disparities. JAMA. 2020;323:1905–1906. doi: 10.1001/jama.2020.6547. [DOI] [PubMed] [Google Scholar]
- 7.Subbaraman N. How to address the coronavirus's outsized toll on people of colour. Nature. 2020;581:366–367. doi: 10.1038/d41586-020-01470-x. [DOI] [PubMed] [Google Scholar]
- 8.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 10.Cleveland Manchanda E., Couillard C., Sivashanker K. Inequity in crisis standards of care. N Engl J Med. 2020;383:e16. doi: 10.1056/NEJMp2011359. [DOI] [PubMed] [Google Scholar]
- 11.Center for Economic and Policy Research VOXEU. The large and unequal impact of COVID-19 on workers; 2020. https://voxeu.org/article/large-and-unequal-impact-covid-19-workers Updated 8 April, 2020. Accessed 7 October 2020.
- 12.The New York Times Location data says it all: staying at home during coronavirus is a luxury; 2020. https://www.nytimes.com/interactive/2020/04/03/us/coronavirus-stay-home-rich-poor.html Updated 3 April, 2020. Accessed 25 November 2020.
- 13.U.S. Bureau of Labor Statistics Labor force characteristics by race and ethnicity, 2018. https://www.bls.gov/opub/reports/race-and-ethnicity/2018 Updated October 2020. Accessed 20 November 2020.
- 14.Economic Policy Institute Black workers face two of the most lethal preexisting conditions for coronavirus—racism and economic inequality; 2020. https://www.epi.org/publication/black-workers-covid Updated June 1, 2020. Accessed November 20, 2020.
- 15.County of Los Angeles Public Health Temporary targeted safer at home health officer order for control of COVID-19: tier 1 substantial surge response; 2020. http://publichealth.lacounty.gov/media/coronavirus/docs/HOO/HOO_SaferatHome_SurgeResponse.pdf Updated 28 November 2020. Accessed 1 December 2020.
- 16.Centers for Disease Control and Prevention Leading causes of death; 2020. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm Updated 30 October 2020. Accessed 1 December 2020.
- 17.Leichtle S.W., Rodas E.B., Procter L., Bennett J., Schrader R., Aboutanos M.B. The influence of a statewide "Stay-at-Home" order on trauma volume and patterns at a level 1 trauma center in the United States. Injury. 2020;51:2437–2441. doi: 10.1016/j.injury.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forrester J.D., Liou R., Knowlton L.M., Jou R.M., Spain D.A. Impact of shelter-in-place order for COVID-19 on trauma activations: Santa Clara County, California, March 2020; 2020. Trauma Surg Acute Care Open. 2020;5 doi: 10.1136/tsaco-2020-000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherman W.F., Khadra H.S., Kale N.N., Wu V.J., Gladden P.B., Lee O.C. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res. 2021;479:266–275. doi: 10.1097/CORR.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yeates E.O., Grigorian A., Barrios C., Schellenberg M., Owattanapanich N., Barmparas G., et al. Changes in traumatic mechanisms of injury in southern california related to COVID-19: penetrating trauma as a second pandemic. J Trauma Acute Care Surg. 2020 doi: 10.1097/TA.0000000000003068. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly M.R., Barie P.S., Grigorian A., Kuza C.M., Schubl S., de Virgilio C., et al. New York State and the nation: trends in firearm purchases and firearm violence during the COVID-19 pandemic. Am Surg. 2020 doi: 10.1177/0003134820954827. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.COVID19.CA.GOV Latest news on COVID-19; 2020. https://covid19.ca.gov/latest-news Updated 3 October 2020. Accessed 3 October 2020.
- 23.Benefits.gov California Medicaid; 2020. https://www.benefits.gov/benefit/1620 Updated 1 December 2020. Accessed 4 December 2020.
- 24.Sterling D.A., O'Connor J.A., Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–119. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharya B., Maung A., Schuster K., Davis K.A. The older they are the harder they fall: Injury patterns and outcomes by age after ground level falls. Injury. 2016;47:1955–1959. doi: 10.1016/j.injury.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen K.H., Sommers B.D. Access and quality of care by insurance type for low-income adults before the affordable care act. Am J Public Health. 2016;106:1409–1415. doi: 10.2105/AJPH.2016.303156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Commonwealth Fund Who are the remaining uninsured, and why do they lack coverage?; 2019. https://www.commonwealthfund.org/publications/issue-briefs/2019/aug/who-are-remaining-uninsured-and-why-do-they-lack-coverage Updated 28 August 2019. Accessed 6 December 2020.
- 28.Hu T., Yue H., Wang C., She B., Ye X., Liu R., et al. Racial segregation, testing site access, and COVID-19 incidence rate in Massachusetts, USA. Int J Environ Res Public Health. 2020;17:E9528. doi: 10.3390/ijerph17249528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maroko A.R., Nash D., Pavilonis B.T. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97:461–470. doi: 10.1007/s11524-020-00468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ProPublica Early data shows black people are being disproportionally arrested for social distancing violations; 2020. https://www.propublica.org/article/in-some-of-ohios-most-populous-areas-black-people-were-at-least-4-times-as-likely-to-be-charged-with-stay-at-home-violations-as-whites Updated 8 May 2020. Accessed 26 December 2020.
- 31.Brookings Social distancing in Black and white neighborhoods in Detroit: a data-driven look at vulnerable communities; 2020. https://www.brookings.edu/blog/fixgov/2020/05/19/social-distancing-in-black-and-white-neighborhoods-in-detroit-a-data-driven-look-at-vulnerable-communities Updated 19 May 2020. Accessed 25 November 2020.
- 32.Boise State University The Blue Review. Who is most likely to voluntarily comply with COVID-19 public health recommendations?; 2020. https://www.boisestate.edu/bluereview/who-is-most-likely-to-voluntarily-comply-with-covid-19-public-health-recommendations Updated 3 April 2020. Accessed 26 December 2020.
- 33.Dennis B.M., Stonko D.P., Callcut R.A., Sidwell R.A., Stassen N.A., Cohen M.J., et al. Artificial neural networks can predict trauma volume and acuity regardless of center size and geography: a multicenter study. J Trauma Acute Care Surg. 2019;87:181–187. doi: 10.1097/TA.0000000000002320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The New York Times California coronavirus map and case count; 2020. https://www.nytimes.com/interactive/2020/us/california-coronavirus-cases.html Updated 26 January 2021. Accessed 26 January 2021.
- 35.Braveman P.A., Cubbin C., Egerter S., Chideya S., Marchi K.S., Metzler M., et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 36.Baker E.H. In: The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society. Cockerham W.C., Dingwall R., Quah S., editors. Wiley-Blackwell; Hoboken (NJ): 2014. Socioeconomic Status, Definition. [Google Scholar]