Abstract
This study is to compare ibuprofen and ketorolac for children with trauma-related acute pain. We conducted a multicentre randomized, double-blind, controlled trial in the Paediatric Emergency Department setting. We enrolled patients aged 8 to 17 who accessed the emergency department for pain related to a limb trauma that occurred in the previous 48 h. At the admission, patients were classified based on numeric rating scale-11 (NRS-11) in moderate (NRS 4–6) and severe (NRS 7–10) pain groups. Each patient was randomized to receive either ibuprofen (10 mg/kg) or ketorolac (0.5 mg/kg) and the placebo of the not given drug in a double dummies design. NRS-11 was asked every 30 min until 2 h after drug and placebo administration. The primary outcome was NRS-11 reduction at 60 min. Among 125 patients with severe pain, NRS-11 reduction after 60 min from drug administration was 2.0 (IQR 1.0–4.0) for ibuprofen and 1.0 (IQR 1.0–3.0) for ketorolac (p = 0.36). Ibuprofen was significantly better, considering secondary outcomes, at 90 min with a lower median of NRS-11 (p 0.008), more patients with NRS-11 less than 4 (p 0.01) and a reduction of pain score of more than 3 NRS-11 points (p 0.01). Among 87 patients with moderate pain, the NRS-11 reduction after 60 min from drug administration was 1.63 (± 1.8) for ibuprofen and 1.8 (± 1.6) for ketorolac, with no statistically significant difference.
Conclusions: Oral ibuprofen and ketorolac are similarly effective in children and adolescents with acute traumatic musculoskeletal pain.
Trial registration: ClinicalTrial.gov registration number: NCT04133623.
| What is Known: |
| • Limb trauma is one of the most common causes of paediatric emergency department visits. Non-steroidal anti-inflammatory drugs are the most frequently used analgesics in this clinical setting. In particular ibuprofen is the first over the counter non-steroidal anti-inflammatory drug in terms of use. Ketorolac is considered the most effective non-steroidal anti-inflammatory drug for severe pain. |
| What is New: |
| • This study directly compared oral ibuprofen and ketorolac for moderate and severe acute traumatic pain in children and adolescents. Both drugs were similarly effective in children and adolescents with severe pain, and ketorolac was not superior to Ibuprofen for moderate pain. |
Keywords: Ibuprofen, Ketorolac, Paediatric, Paediatric Emergency Medicine, Pain, Trauma
Introduction
Musculoskeletal injuries are a significant source of acute pain and a common reason for children and adolescents to access the paediatric emergency department (PED) [1].
The harmful effects of inadequate pain treatment in childhood are well known, and several drugs are available to manage acute traumatic pain in children [2].
Non-steroidal anti-inflammatory drugs (NSAIDs) and opioids are the families of analgesics most frequently employed in this clinical setting. A recent meta-analysis considering the trials that compared the effectiveness of NSAIDs and opioids for the management of acute traumatic pain in children showed the non-inferiority of NSAIDs [3].
On the other hand, comparisons among different NSAIDs in this context are lacking.
Ibuprofen is THE most commonly used and studied NSAIDs [3, 4]. Ketorolac is a potent NSAID for the short-term management of severe acute pain in adults [5]. It is still not indicated for paediatric use [5], except for post-operative pain. However, a growing number of studies suggest good safety and efficacy in children in different settings, particularly for acute musculoskeletal pain [6, 7].
This study aims to compare the effectiveness of ibuprofen and ketorolac for acute traumatic moderate and severe pain in children and adolescents.
Materials and methods
This investigation was a multicentre randomized, double-blind, double-dummy, controlled trial.
The study protocol was approved by the independent bioethics committee of the Institute for Maternal and Child Health IRCCS Burlo Garofolo of Trieste, Italy, and by the Italian pharmacological agency (AIFA), Eudract code: 2018-004,057-25. It was recorded at ClinicalTrial.gov before the enrolment of the first participant, registration number NCT04133623.
The study was conducted at the PEDs of the Institute for Maternal and Child Health IRCCS Burlo Garofolo of Trieste, Italy (a tertiary-level university teaching children’s hospital) and the Santa Maria degli Angeli hospital of Pordenone, Italy.
Children and adolescents aged 8 to 17 who accessed the PED complaining of moderate to severe pain related to a limb trauma that occurred in the previous 48 h were considered eligible for the study. Patients self-reported their pain through the numeric rating scale-11 (NRS-11), in which patients verbally rate their pain from 0 to 10 (0 no pain, 10 worst imaginable pain) [8].
Scores from 4 to 6 were considered moderate pain, and scores from 7 to 10 were severe.
Patients with at least one of the following features were excluded from the research: administration of any analgesic within the previous 8 h; known allergy to ibuprofen or ketorolac; chronic use of analgesics; known hepatopathy or nephropathy, history of thrombocytopenia or coagulation disturbance; known chronic neurological or metabolic diseases, history of gastritis or esophagitis in the previous 30 days; clinical suspicion of violence or pregnancy; polytrauma; and inability to self-report pain related to intellectual disability, moderate-severe hearing loss or communication limitations or language difficulties.
Eligible children were enrolled and randomly assigned to receive a dose of 10 mg/kg oral ibuprofen syrup (maximum of 600 mg) or a dose of 0.5 mg/kg oral drops of ketorolac (maximum of 10 mg), after obtaining written informed consent from a parent or legal guardian.
Using a computerized method by an independent epidemiologist at the Clinical Epidemiology and Public Health Research Unit at the IRCCS Burlo Garofolo Institute, we generated two separate randomization lists, one for patients with severe pain and one for patients with moderate pain, stratified per centre, with a fixed block size of 4.
Each list randomly assigned patients to receive ibuprofen or ketorolac and the placebo of the not-given drug in a double dummies fashion. Drug kits were produced, consecutively numbered and labelled to be assigned to subjects with moderate or severe pain. They were designed to be used for a single patient. Each kit contained two vials closed into opaque envelopes, containing (1) a maximum extractable volume of 15 ml of ibuprofen syrup (40 mg/ml) and oral ketorolac placebo or (2) a maximum extractable volume of 5 ml of ketorolac drops (2 mg/ml) and oral ibuprofen placebo. Each vial reported the ml pro/kg dose and maximum ml dose to administer. Each drug and its corresponding placebo were indistinguishable in aspect, taste and flavour.
Consequently, each subject received one dose of active drug (ibuprofen or ketorolac) and one dose of placebo. Patients, nurses and clinicians were double-blinded on the drug and placebo administered. After the drug administration, the patients were asked to self-report their pain through the NRS-11 scale every 30 min until 2 h and to report the onset of new symptoms, especially: headache, nausea, vomiting, dyspepsia, hitching, somnolence, abdominal pain or dizziness. If patients considered their pain poorly controlled after 1 h, acetaminophen was offered as a rescue drug. If rescue therapy was asked before 1 h, it was considered as failures.
The primary study outcome was the difference in NRS-11 score reduction between the ketorolac and ibuprofen groups after 60 min of drug administration. The secondary results were the difference in NRS-11 score reduction between groups at 30-60-120 min, the number of patients achieving NRS-11 score < 4 and the number of patients reaching an NRS-11 reduction > 3 points at each time point between groups and the number of patients asking for rescue analgesics in the two groups.
We hypothesized that ketorolac would be more effective than ibuprofen for severe pain and as effective as ibuprofen for moderate pain. According to the first hypothesis of ketorolac superiority over ibuprofen, based on the available literature indicating a one-point reduction in the NRS scale, a difference of minimal clinical importance for patients [9], we estimated a study population of 130 patients (65 for each group) to achieve a difference of 1 point between T0 and T60 in the NRS-11 score (with a standard deviation of 2) between the two groups with an alpha and beta error of 0.05 and 0.20, respectively. The second hypothesis concerns the non-inferiority of ibuprofen compared to ketorolac in managing moderate to acute trauma-related pain. For the non-inferiority hypothesis, assuming a pain reduction of 1 point in the difference between T0 and T60 on the NRS-11 score as the minimum clinically significant reduction, we set the non-inferiority threshold at 50% of this value (0.5 points) (refs) [10]. The study needs 120 patients (60 for each group) according to the established non-inferiority threshold, a standard deviation of 1 point with an alpha and beta error of 0.05 and 0.20, respectively. We will consider non-inferiority confirmed if the upper limit of the 95% confidence interval of the difference between the mean of ibuprofen and ketorolac is less than the non-inferiority threshold. Both samples’ sizes were calculated for a 1:1 ratio between groups.
Statistical analysis
The statistical analysis was blinded and performed by the Clinical Epidemiology and Public Health Research Unit of the IRCCS Burlo Garofolo. Data for the two study hypotheses (superiority of ketorolac and non-inferiority of ibuprofen) were analysed separately. For the hypothesis of superiority, we planned analysis by intention-to-treat, while for the hypothesis of non-inferiority per protocol.
Continuous variables were reported as a median and interquartile range, based on data distribution, while categorical variables as numbers and percentages.
We used the Mann-Whitney test, based on data distribution, to evaluate the difference in NRS-11 score between the ibuprofen group and the ketorolac group 60 min after drug administration (primary study result). We calculated the 95% confidence interval of the difference between the two drugs and confirmed the non-inferiority of ibuprofen if the upper limit of the confidence interval remains below the defined non-inferiority threshold.
For secondary outcomes, differences were assessed with the Mann-Whitney test for the continuous variables and the chi-square test (or Fisher’s exact test where appropriate) for the categorical variables. Each time was evaluated separately. If the patient required another pain medication, it was evaluated as study drug failure, not as dropping out. A p value < 0.05 was considered statistically significant.
Results
From November 2019 to September 2021, 307 patients were eligible for this study. Of these, 53 patients refused to participate, and 42 were excluded: 28 with polytrauma, 10 with language difficulties, 2 with intellectual disability, 1 with known nephropathy and 1 with an allergy to ibuprofen. We enrolled a total of 212 patients, 125 with severe pain (63 randomized to ibuprofen and 62 to ketorolac) and 87 with moderate pain (43 randomized to ibuprofen and 44 to ketorolac). There were no dropouts at follow-up, and all randomized subjects were analysed.
Table 1 shows the main demographical and clinical characteristics of the enrolled patients. There were no statistically significant differences between groups regarding demographical features, duration of symptoms, site of trauma or prevalence of fractures.
Table 1.
Patients’s characteristics at enrolment
| Severe | Moderate | |||||
|---|---|---|---|---|---|---|
| Ibuprofen | Ketorolac | p | Ibuprofen | Ketorolac | p | |
| (n = 63) | (n = 62) | (n = 43) | (n = 44) | |||
| Age: years, median (IQR) | 12.1 (10.1–14.2) | 12.8 (10.7–14.8) | 0.27 | 12.1 (10.0–14.6) | 13.2 (10.1–16.1) | 0.39 |
| Male sex, n (%) | 29 (46.0) | 29 (46.8) | 0.93 | 26 (60.5) | 33 (75.0) | 0.15 |
| Weight: kg, median (IQR) | 50.0 (38.0–62.0) | 53.0 (39.8–63.0) | 0.63 | 48.0 (40.0–60.0) | 52.0 (40.5–60.8) | 0.46 |
| Duration of symptoms, median (IQR) | 12.0 (2.0–18.0) | 12.0 (2.0–18.0) | 0.88 | 15.0 (5.3–21.3) | 12.0 (2.0–24.0) | 0.48 |
| Location of trauma, n (%) | ||||||
| - Upper limb | 40 (63.5) | 39 (62.9) | 0.95 | 26 (60.5) | 29 (65.9) | 0.6 |
| - Lower limb | 23 (36.5) | 23 (37.1) | 17 (39.5) | 15 (34.1) | ||
| Limb deviation, n (%) | 4 (6.3) | 8 (12.9) | 0.21 | 5 (11.6) | 2 (4.5) | 0.27a |
| Diagnosis, n (%) | 0.7 | 0.17 | ||||
| - Bone fracture | 34 (54.0) | 38 (61.3) | 27 (62.8) | 19 (43.2) | ||
| - Contusion | 20 (31.7) | 17 (27.4) | 11 (25.6) | 18 (40.9) | ||
| - Sprain | 9 (14.3) | 7 (11.3) | 5 (11.6) | 5 (11.4) | ||
| - Dislocation | 0 | 0 | 0 | 2 (4.5) | ||
| Outcome, n (%) | 0.62a | 44 (100.0) | ||||
| Discharge from PED | 62 (98.4) | 60 (96.8) | 43 (100.0) | - | ||
| Hospital admission | 1 (1.6) | 2 (3.2) | ||||
| NRS-11 at arrival, median (IQR) | 8.0 (7.0–8.0) | 8.0 (7.0–9.0) | 0.06 | 6.0 (5.0–6.0) | 5.0 (5.0–6.0) | 0.5 |
aFisher exact test
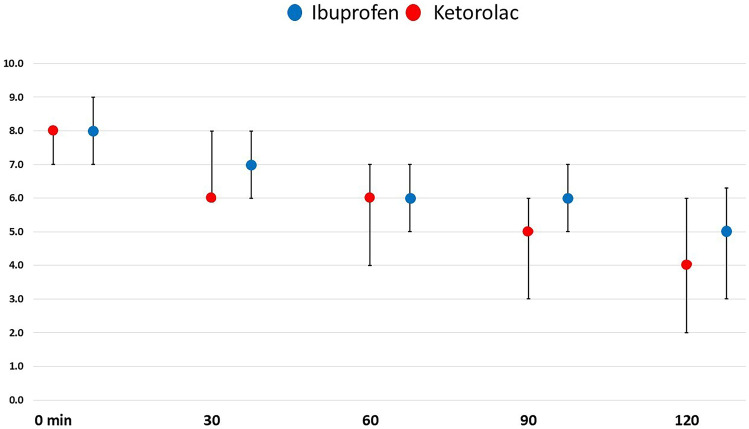
Table 2 presents the main results of the study. No statistically noteworthy differences were found in the median pain score differences T0–T60 between patients receiving ibuprofen or ketorolac, 2.0 (1.0–4.0) and 1.0 (1.0–3.0), respectively, p = 0.36, considering patients with severe pain. The median disparity of the pain scores was not statistically different also in the other time points analysed. Figure 1 demonstrates the change in pain score during the 120 min follow-up in children with severe and moderate pain receiving ibuprofen versus ketorolac.
Table 2.
NRS trend every 30 min after ibuprofen or ketorolac administration
| Pain scores NRS-11 | Severe | Moderate | ||||
|---|---|---|---|---|---|---|
|
Ibuprofen (n = 63) |
Ketorolac (n = 62) |
p |
Ibuprofen (n = 43) |
Ketorolac (n = 44) |
p | |
| Difference T0-T60, median (SD) | 2.0 (1.0–4.0) | 1.0 (1.0–3.0) | 0.36 | 1.0 (0.0–3.0) | 1.5 (1.0–2.0) | 0.49 |
| Difference T0-T30, median (IQR) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.78 | 0.0 (0.0–1.0) | 1.0 (0.0–2.0) | 0.22 |
| Difference T0-T90, median (IQR) | 3.0 (1.0–5.0) | 2.0 (1.0–3.3) | 0.06 | 2.0 (1.0–4.0) | 2.0 (1.0–3.8) | 0.71 |
| Difference T0-T120, median (IQR) | 3.0 (1.0–6.0) | 3.0 (1.0–5.0) | 0.29 | 3.0 (1.0–4.0) | 2.0 (2.0–4.0) | 0.96 |
| Pain scores at T30, median (IQR) | 6.0 (6.0–8.0) | 7.0 (6.0–8.0) | 0.08 | 5.0 (4.0–6.0) | 5.0 (4.0–5.0) | 0.24 |
| Pain scores at T60, median (IQR) | 6.0 (4.0–7.0) | 6.0 (5.0–7.0) | 0.03 | 4.0 (3.0–5.0) | 4.0 (2.0–5.0) | 0.44 |
| Pain scores at T90, median (IQR) | 5.0 (3.0–6.0) | 6.0 (5.0–7.0) | 0.008 | 3.0 (2.0–5.0) | 3.0 (2.0–4.0) | 0.58 |
| Pain scores at T120, median (IQR) | 4.0 (2.0–6.0) | 5.0 (3.0–6.3) | 0.12 | 3.0 (1.8–4.0) | 3.0 (1.3–4.0) | 0.58 |
| Pain score decrease > 3 at T30, n (%) | 2 (3.2) | 1 (1.6) | 1.00a | 3 (7.0) | 1 (2.3) | 0.36a |
| Pain score decrease > 3 at T60, n (%) | 18 (28.6) | 11 (17.7) | 0.15 | 7 (16.3) | 9 (20.5) | 0.62 |
| Pain score decrease > 3 at T90, n (%) | 29 (46.0) | 15 (24.2) | 0.01 | 11 (25.6) | 11 (25.0) | 0.95 |
| Pain score decrease > 3 at T120, n (%) | 30 (47.6) | 26 (41.9) | 0.52 | 12 (27.9) | 15 (34.1) | 0.53 |
| Pain score < 4 points at T30, n (%) | 1 (1.6) | 0 | 1.00a | 8 (18.6) | 10 (22.7) | 0.64 |
| Pain score < 4 points at T60, n (%) | 11 (17.5) | 4 (6.5) | 0.06 | 15 (34.9) | 15 (34.1) | 0.94 |
| Pain score < 4 points at T90, n (%) | 21 (33.3) | 10 (16.1) | 0.03 | 22 (51.2) | 24 (54.5) | 0.75 |
| Pain score < 4 points at T120, n (%) | 24 (38.1) | 19 (30.6) | 0.38 | 26 (61.9) | 31 (70.5) | 0.40 |
aFisher exact test
Fig. 1.
Numeric rating scale-11 every 30 min since ibuprofen or ketorolac administration
Sixty and 90 min after the drug administration, the ibuprofen group revealed a lower median pain score (p = 0.03 and 0.008, respectively), and at 90 min, a higher proportion of patients with a pain score decrease > 3 points (p = 0.01), and with pain scores < 4 points (p = 0.03) compared to the ketorolac group.
Concerning patients with moderate pain, no statistically significative discrepancies were detected in the median pain score differences T0–T60 between patients receiving ibuprofen or ketorolac (Table 2). The mean change in score reduction between groups at T60 was 0.17 in ketorolac favour; the mean difference in the ibuprofen group was 1.63 with 1.8 SD and that of ketorolac 1.80 with 1.6 SD, with a 95% CI = −0.55 to 0.89. This cannot confirm the ibuprofen non-inferiority compared to ketorolac for our population with moderate pain although no between-group differences were seen at 60 min and for the other times and outcomes evaluated.
Table 3 displays the list of adverse events in the two groups of patients. Adverse events were mild, namely, nausea, headache and sleepiness, and rare in both parties. In the superiority study, five subjects experienced adverse events in the ibuprofen vs 2 in the ketorolac group (p = 0.44). In contrast, in the non-inferiority study, only 1 adverse event was reported in the ibuprofen group (p = 0.49).
Table 3.
Frequency and type of adverse events. The table reports the number of patients presenting each symptom
| Severe | Moderate | |||
|---|---|---|---|---|
| Ibuprofen (n = 63) | Ketorolac (n = 62) | Ibuprofen (n = 43) | Ketorolac (n = 44) | |
| Nausea, n | 2 | 2 | 0 | 0 |
| Headache, n | 2 | 0 | 1 | 0 |
| Sleepiness, n | 1 | 0 | 0 | 0 |
Discussion
This study proved that oral ketorolac was not superior to oral ibuprofen in children and adolescents with severe acute traumatic pain. However, it could not demonstrate that the oral ibuprofen was not not-inferior to oral ketorolac in patients with moderate acute traumatic pain.
Ibuprofen is the most widely used NSAID in children to manage acute pain. It is the only one licensed for use in children as young as 6 months [11] and the most studied NSAID for handling acute pain in children with trauma. The literature reveals that among oral medications, ibuprofen was not inferior to codeine [12], the combination of acetaminophen and codeine [13], morphine [14] and oxycodone [15]. When investigated, the combination of ibuprofen and opioids was not superior to using ibuprofen alone.
Despite being not licensed for paediatric age, ketorolac was reported as an effective analgesic alternative to opioids in neonates and children [16, 17].
According to a recent review, ketorolac was studied in children mainly for post-operative pain and administered intravenously [18]. Only a few trials investigated its employment in a PED setting. A trial examined the use of sublingual ketorolac in young patients with acute abdominal pain compared to sublingual tramadol and sublingual paracetamol. It showed that the three drugs were similarly effective in managing pain in this clinical context [19].
A single trial investigated ketorolac versus tramadol in children with acute traumatic pain in the emergency department [7]. In that trial, ketorolac was administered through the sublingual route and was as effective as tramadol for pain management.
To our knowledge, this is the first trial comparing ibuprofen and ketorolac for acute traumatic pain in the ED. Despite the experiences mentioned above with sublingual ketorolac, we decided to administer both ibuprofen and ketorolac via the oral route to avoid the possible bias of a different drug absorption related to the route of administration. Considering that ibuprofen is administered as a syrup and ketorolac as drops, we designed a double-blind, double-dummy randomized trial in which patients took both a dose of syrup and a dose of drops.
According to the recommended posology, and following the Italian Drug Agency (AIFA) indications, we decided to give a dose of 10 mg/kg of ibuprofen with a maximum of 600 mg [20] and 0.5 mg/kg of ketorolac with a maximum of 10 mg [6]. We are fully aware that the single dose of ketorolac may be 30 mg, as this was the maximum quantity administered in previous investigations that employed sublingual ketorolac [7, 19]. Nevertheless, we decided to use the maximum of 10 mg according to a previous trial performed in the ED setting in adult patients with moderate to severe acute pain, showing a similar decrease in subjects receiving 10 mg, 15 mg or 30 mg of intravenous ketorolac [21, 22].
This study has several limitations. First of all, we could not reach the planned sample size for patients with moderate pain. The outbreak of the COVID-19 pandemic and the related social distancing measures led to a reduction in the PED visits for trauma in our setting [23]. Moreover, for an extended period, the medical student responsible for the enrolment of patients was not allowed to be present in the PED. This study did not demonstrate the non-inferiority of ibuprofen compared to ketorolac for moderate traumatic pain. Although the mean difference of pain between groups at 60 min was slight (0.17), the 95% confidence interval was vast (−0.55 to 0.89), the upper limit exceeding the non-inferiority threshold. It is possible that by reaching the planned sample size, the confidence interval would have been different, thus demonstrating the non-inferiority of ibuprofen. Therefore, further and more extensive studies are needed to evaluate the non-inferiority of ibuprofen. Moreover, we considered a difference pain score of 1 point between groups as clinically important. The choice of other cut-offs could have influenced the study results. Second, we used a maximum dose of 10 mg of ketorolac; therefore, we cannot exclude that a higher dose would have influenced the results. In the same way, we used a maximum dose of 600 mg of ibuprofen even though a previous trial in adult patient with acute pain in the ED setting did not find a stronger effect of doses exceeding 400 mg (22). Third, the enrolment of patients was not continuous but associated with the presence of dedicated staff.
On the contrary, this study’s main strength is the solid methodological design and the idea of comparing the effectiveness of two commonly used NSAIDs for moderate and severe traumatic pain.
In conclusion, this randomized controlled trial showed the equivalence of oral ibuprofen and oral ketorolac in children and adolescents with severe acute traumatic pain. Future studies are needed to prove the equivalence of these two drugs for patients with moderate traumatic pain.
Acknowledgements
The authors thank Martina Bradaschia for the English revision of the manuscript.
Abbreviations
- AIFA
Italian Medicines Agency; Agenzia Italiana del Farmaco
- COVID-19
Corona virus induced disease-19
- ED
Emergency department
- IRCCS
Scientific Clinical Research Center; istituto di ricerca a carattere scientifico
- NRS
Numeric rating scale
- NSAIDs
Non-steroidal anti-inflammatory drugs
- PED
Paediatric emergency department
- SD
Standard deviation
Authors’ contributions
Sergio Ghirardo, Giorgio Cozzi, Matteo Trevisan, Alessandro Amaddeo, Laura de Nardi and Egidio Barbi designed the study and wrote the protocol and the article. Luca Ronfani made the statistical evaluation and revised the manuscript. Alessandra Maestro reviewed the protocol, made the registration of the protocol and revised the manuscript. Davide Zanon organized, prepared and supplied the drugs and placebo; he also contributed to the writing of the draft. Francesca Barbieri is responsible for the satellite centres and revised the manuscript.
Funding
The study was founded entirely by the Institute for Maternal and Child Health, IRCCS Burlo Garofolo, Trieste, Italy.
Data Availability
Data are available on request to the corresponding author.
Declarations
Ethical Approval
The protocol was approved by the independent bioethics committee of IRCCS Burlo Garofolo of Trieste, Italy, and by the Italian pharmacological agency (AIFA), Eudract code: 2018–004057-25. It was recorded at ClinicalTrial.gov before the enrolment of the first participant, registration number NCT04133623.
Consent to participate
All the parents/guardians gave the consent to participate on a dedicated written form; all the children gave their consent as well on written consent forms that were designed to be appropriate for patients aged 8–12 years and 12–18 years.
Consent for publication
All the authors gave the consent for the publication of the article in its current form.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whitfill T, Auerbach M, Scherzer DJ, Shi J, Xiang H, Stanley RM. Emergency care for children in the United States: epidemiology and trends over time. J Emerg Med. 2018;55(3):423–434. doi: 10.1016/J.JEMERMED.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 2.Weisman SJ, Bernstein B, Schechter NL. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152(2):147–149. doi: 10.1001/ARCHPEDI.152.2.147. [DOI] [PubMed] [Google Scholar]
- 3.Cortellazzo Wiel L, Poropat F, Barbi E, Cozzi G (2020) Is opioid analgesia superior to NSAID analgesia in children with musculoskeletal trauma? Arch Dis Child 105(12). 10.1136/ARCHDISCHILD-2020-319359 [DOI] [PubMed]
- 4.Kircher J, et al. Acute pediatric musculoskeletal pain management in North America: a practice variation survey. Clin Pediatr (Phila) 2014;53(14):1326–1335. doi: 10.1177/0009922814555972. [DOI] [PubMed] [Google Scholar]
- 5.FDA (2008) Toradol (Roche) Medication guide approved by the U.S. Food and Drug Administration only WARNING TORADOL. Reference ID: 3281582
- 6.Marzuillo P, Calligaris L, Amoroso S, Barbi E. Narrative review shows that the short-term use of ketorolac is safe and effective in the management of moderate-to-severe pain in children. Acta Paediatr. 2018;107(4):560–567. doi: 10.1111/apa.14189. [DOI] [PubMed] [Google Scholar]
- 7.Neri E, et al. Sublingual ketorolac versus sublingual tramadol for moderate to severe post-traumatic bone pain in children: a double-blind, randomised, controlled trial. Arch Dis Child. 2013;98(9):721–724. doi: 10.1136/archdischild-2012-303527. [DOI] [PubMed] [Google Scholar]
- 8.von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143(3):223–227. doi: 10.1016/J.PAIN.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Olsen MF et al (2017) Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med 15(1). 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed]
- 11.Poddighe D, Brambilla I, Licari A, Marseglia GL. Ibuprofen for pain control in children: new value for an old molecule. Pediatr Emerg Care. 2019;35(6):448–453. doi: 10.1097/PEC.0000000000001505. [DOI] [PubMed] [Google Scholar]
- 12.Clark E, Plint AC, Correll R, Gaboury I, Passi B. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119(3):460–467. doi: 10.1542/peds.2006-1347. [DOI] [PubMed] [Google Scholar]
- 13.Friday JH, Kanegaye JT, McCaslin I, Zheng A, Harley JR. Ibuprofen provides analgesia equivalent to acetaminophen-codeine in the treatment of acute pain in children with extremity injuries: a randomized clinical trial. Acad Emerg Med. 2009;16(8):711–716. doi: 10.1111/J.1553-2712.2009.00471.X. [DOI] [PubMed] [Google Scholar]
- 14.Poonai N, et al. Oral administration of morphine versus ibuprofen to manage postfracture pain in children: a randomized trial. CMAJ. 2014;186(18):1358–1363. doi: 10.1503/CMAJ.140907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koller DM, Myers AB, Lorenz D, Godambe SA. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23(9):627–633. doi: 10.1097/PEC.0B013E31814A6A39. [DOI] [PubMed] [Google Scholar]
- 16.Moffett BS, Wann TI, Carberry KE, Mott AR. Safety of ketorolac in neonates and infants after cardiac surgery. Pediatr Anesth. 2006;16(4):424–428. doi: 10.1111/J.1460-9592.2005.01806.X. [DOI] [PubMed] [Google Scholar]
- 17.Kingston P, Lascano D, Ourshalimian S, Russell CJ, Kim E, Kelley-Quon LI. Ketorolac use and risk of bleeding after appendectomy in children with perforated appendicitis. J Pediatr Surg. 2021 doi: 10.1016/J.JPEDSURG.2021.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooney MF. Pain management in children: NSAID use in the perioperative and emergency department settings. Paediatr Drugs. 2021;23(4):361–372. doi: 10.1007/S40272-021-00449-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giorgio C, et al. Title Administering analgesia sublingually is a suitable option for children with acute abdominal pain in the emergency department. Acta Paediatrica. 2019;108:143–148. doi: 10.1111/apa.14514. [DOI] [PubMed] [Google Scholar]
- 20.Krauss BS, Calligaris L, Green SM, Barbi E. Current concepts in management of pain in children in the emergency department. Lancet. 2016;387(10013):83–92. doi: 10.1016/S0140-6736(14)61686-X. [DOI] [PubMed] [Google Scholar]
- 21.Motov S, et al. Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med. 2017;70(2):177–184. doi: 10.1016/J.ANNEMERGMED.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Motov S, et al. Comparison of oral ibuprofen at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med. 2019;74(4):530–537. doi: 10.1016/J.ANNEMERGMED.2019.05.037. [DOI] [PubMed] [Google Scholar]
- 23.Cozzi G, et al. The impact of the COVID-19 lockdown in Italy on a pediatric emergency setting. Acta Paediatr. 2020;109(10):2157–2159. doi: 10.1111/APA.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on request to the corresponding author.