Abstract
Background
Caring for children with cerebral palsy (CP) for many aspects of their lives may affect caregiver’s psychological health. Emergence of COVID-19 put added pressure on caregivers.
Aims
The aim of this study was to investigate the psychological health of Iranian caregivers of children with CP and associated risks during a lockdown period.
Methods
Using online snowball sampling, 160 caregivers of children with CP participated in this web-based cross-sectional study. The Hospital Anxiety and Depression Scale (HADS), Perceived Stress Scale (PSS-4), Caregiver Difficulties Scale (CDS), and a demographic questionnaire were administered. Hierarchical multiple linear regression analysis was applied to identify risk factors related to caregiver psychological health.
Outcomes and results
Mental health problems were prevalent; (depression = 45.0% and anxiety = 40.6%). Significant correlations were found between CDS and HADS-Anxiety (r = 0.472, P < 0.001), HADS-depression (r = 0.513, P < 0.001), and perceived stress (PSS) related to COVID-19 (r = 0.425, P < 0.001). After controlling for demographic and clinical variables, burden (CDS) was found to significantly predict caregiver anxiety, depression and stress. Furthermore, several demographic characteristics (being married, low educational level and low income) were significantly related to high HADS Anxiety scores. For depression, only having a physical problem was significantly related to HADS among demographic variables. No significant correlations were found between PSS-4 and demographic variables.
Conclusions and implications
During COVID-19 outbreak, the mental health of caregivers of children with CP is affected by multiple factors such as burden of care and demographic characteristics. Due to the importance of well-being among caregivers of disabled children, a comprehensive plan including psychological consultation, remote education, or in-person handouts for the self-care or handling of the children and adequate distance support may enable better mental health for these caregivers.
Keywords: Neurodevelopmental disorders, Anxiety, Depression, Burden of care, COVID-19, Caregiver
What this paper adds?
-
•
During COVID-19, depression and anxiety are prevalent among caregivers of children with CP.
-
•
Burden of care is a significant predictor of mental health problems during the outbreak.
-
•
Income, education, marital and physical status of the caregivers can affect their mental state.
1. Introduction
COVID-19 is a life-threatening illness in millions of people across the world that may cause symptoms such as fever, cough or acute respiratory disease (Boldrini, Bernetti, Fiore, & Committee, 2020; Boyle, Fox, Havercamp, & Zubler, 2020). The incidence of the COVID-19 pandemic significantly affects individuals and families which in turn can deteriorate public health and health care (Courtenay & Perera, 2020). One of the endangered populations during this pandemic may be children with developmental disabilities (Leocani, Diserens, Moccia, & Caltagirone, 2020). Disability is not currently associated with a higher risk of being affected by COVID-19 or being subject to more severe conditions, although factors or particular complications related to disabilities may increase these threats (Leocani et al., 2020). In public health research, children with cerebral palsy (CP) are a vulnerable population that require attention. Previous studies have shown that children with CP have a higher prevalence of particular comorbidities (e.g., hypertension, heart disease, respiratory disease and diabetes), which are identified as risk factors for poor COVID-19 outcomes (Leocani et al., 2020; Turk, Landes, Formica, & Goss, 2020). Some studies have investigated COVID-19 trends among children with CP which are part of the Intellectual and Developmental Disability (IDD) population (Turk & McDermott, 2020; Turk et al., 2020).
CP is the most prevalent disability starting in early childhood characterized as a series of difficulties caused by central nervous system lesions (Farajzadeh, Maroufizadeh, & Amini, 2020). There are similarities in the incidence rate of CP reported in Iran and other countries (Johnson, 2002; Yeargin-Allsopp et al., 2008), with the rate of about 2 per 1000 live births (Joghataei, Mohammad, Rahgozar, & Siadaty, 2002). CP-related symptoms have adverse effects on many aspects of these children’s and their parents' lives (e.g., physical, socio-economic, psychological, and behavioral) (Farajzadeh et al., 2020; Khayatzadeh, Rostami, Amirsalari, & Karimloo, 2013; Ones, Yilmaz, Cetinkaya, & Caglar, 2005). Due to their disability-related limitations, children with CP may require long-term care and effective treatments to become as independent as possible (Ones et al., 2005). Parents are primarily responsible for caring for and helping children with CP (Farajzadeh et al., 2020). Owing to the emotional and physical demands, caregiving for a child with long lasting functional problems is a demanding responsibility which results in a burden of care (Khayatzadeh et al., 2013). Caregivers' physical, psychosocial, and mental health is negatively affected by the burden of care, resulting in low quality of care and unmet client needs (Farajzadeh et al., 2020; Khayatzadeh et al., 2013). In Iran, the first hit COVID-19 Middle-Eastern country, medical activities and rehabilitation services were postponed to allow shifting of staff and facilities to intensive care for infected people by coronavirus. These disturbances may place an already vulnerable caregiver at higher risk for mental health issues.
While a quarantine and social distancing have been crucial to prevent transmission of COVID-19, caregivers may face further burden and negative psychological consequences such as fear of infecting their children. As a result, their assistance with their child’s personal care makes caregivers unable to respect physical distancing. Socioeconomic imbalance resulting from job losses or other circumstances can exacerbate the burden imposed on caregivers who had financial difficulties before the outbreak of the new virus. Burden of caregiving accompanied with stressors such as fear of transmitting the virus to their child, separation or loss of relatives because of COVID-19, economic uncertainty due to job losses and financial insecurity all place caregivers in a more at-risk position. The prolonged exposure to burden due to the lockdown and the lack of support from relatives, medical and rehabilitation teams or government may also contribute to an increase in psychological distress (Boldrini et al., 2020). Therefore, emphasis should be placed on how to tailor possible ways and guarantee service access for caregivers. To do that, we first need to evaluate the amount and factors impacting caregiving burden on the psychological health of caregivers. During the pandemic, it is imperative to recognize risk factors associated with depression, anxiety and stress among caregivers. Comprehending their health and well-being is important now, as it sets the stage for later actions.
Currently the global emphasis is on introducing social distancing initiatives while the psychosocial well-being of parents is an important concern as a prerequisite for stable life for both caretaker and care recipient. Therefore, identifying factors affecting the psychological wellbeing of caregivers of children with CP would also help identify effective supporting measures for this vulnerable group. Despite studies in other disabled populations such as autism or IDD (Colizzi et al., 2020; Turk & McDermott, 2020; Turk et al., 2020), there is no research on the caregivers of children with CP. Therefore, this research aimed to identify potential factors that lead to mental health outcomes among caregivers of children with CP during the COVID-19 pandemic in Iran.
2. Methods
2.1. Recruitment and Study Population
In the present study 165 caregivers of children with CP were recruited through virtual snowball sampling (Baltar & Brunet, 2012; Dusek, Yurova, & Ruppel, 2015). An Iranian free web-based platform was used 1 (Porsline.ir) for developing the online questionnaires. We first sent the survey E-link to CP virtual communities and pediatric rehabilitation therapists/managers by email or other communicative media (WhatsApp, Telegram, SMS) and asked them to share it with caregivers of CP children within reach. At the beginning of the online survey, an informed consent was recruited from the participants. The privacy and anonymity of caregivers in the survey was assured. The inclusion criteria for caregivers were; age ≥18 years, having a child with CP within 2–14 years of age, being the main caregiver responsible for the daily provision of care to the child with CP, living with the child with CP in the same place, being a native Persian speaker and able to read and write in Persian, and having an education level of grade five or higher. Caregivers were excluded from this study if there were other disabled children in the family and/or if they had additional caregiving responsibilities apart from their usual parenting care.
2.2. Ethical considerations
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Ethical Code: IR.IUMS.REC.1399.821), and online consent was provided for the participants.
2.3. Instruments
2.3.1. Demographic variables
Demographic information including caregiver`s age, educational level, employment status, marital status, any illnesses, income level and the type and age of their child with CP were collected.
2.3.2. Hospital Anxiety and Depression Scale (HADS)
The HADS is a self-rated 14 item scale evaluating psychological distress in non-psychiatric patients. It assesses symptoms of anxiety and depression in two subscales comprising 7 items for the anxiety subscale (HADS Anxiety) and seven for the depression subscale (HADS Depression). The main concentration of HADS Anxiety is on symptoms of generalized anxiety disorder, but HADS Depression focuses on the main symptom of depression called anhedonia. Each item is scored with four possible options with a range between 0–3. After reversing the scores of six items, to calculate the two subscales all responses have to be summed. According to Zigmond & Snaith recommended cut-off scores are 8–10 for doubtful cases and ≥11 for definite cases (Zigmond & Snaith, 1983). Using a cut-off score of 8 or above, an appropriate balance between sensitivity and specificity was negotiated for both HADS Anxiety and HADS Depression (Zigmond & Snaith, 1983). Anxiety and depression items have to be summed separately, reporting a score between 0–21 for each category. The higher score explains a more severe state of depression or anxiety in the participant. Satisfactory psychometric properties is reported for the Persian version of this scale (Amini, Maroufizadeh, & Samani, 2017). The Cronbach’s alpha coefficient of the HADS-A and HADS-D were 0.820 and 0.673, respectively.
2.3.3. Perceived Stress Scale-4 item (PSS-4)
The PSS-4 is a self-report scale that measures the degree to which situations in one’s life over the past month (here the COVID-19 pandemic) are appraised as unpredictable, uncontrollable and overloading. Items are designed to detect stress experienced within the last month on a 5-point Likert scale, ranging from 0 (never) to 4 (very often). Scoring is obtained by reverse scoring of some items and summing across all item scores. Greater scores indicates higher levels of perceived stress (Cohen, Kamarck, & Mermelstein, 1983). The Persian version of this scale is reported to have satisfactory psychometric properties (Maroufizadeh, Zareiyan, & Sigari, 2014, 2018). Although we used the 4-items version of PSS-4 in the present study, there are the 14-items and 10-items versions available regarding this scale. The Cronbach’s alpha coefficient of the PSS-4 was 0.723 in this survey.
2.3.4. Caregiver Difficulties Scale (CDS)
The Caregiver Difficulties Scale (CDS) is self-administered and has 25 items. It has been developed using a combined qualitative-quantitative approach. The four domains of the scale are; concern for the child (8 items), impact on self (7 items), support for caregiving (5 items), and social and economic strain (5 items). Caregivers have to score each item on a 5-point scale ranging from 0 to 4 that declares the frequency and extent of their perceived caregiving experience. The final total score ranges from 0 to 100 with higher scores denoting greater effects of the encountered burden of care on the caregivers lives (Wijesinghe, Fonseka, & Hewage, 2013). The Persian translation of CDS is reported to have satisfactory psychometric properties in mothers of children with CP (Farajzadeh, Amini, Maroufizadeh, & Wijesinghe, 2018). The reported Cronbach’s alpha coefficient of the CDS was 0.860.
2.4. Statistical Analysis
In this study, continuous variables were reported as mean (±standard deviation (SD)) and categorical variables as frequency (percentage). In univariable analysis, the relationships between demographic variables and HADS-A and HADS-D scores were examined by using independent samples t-test, one-way ANOVA, and Pearson correlation coefficients. To investigate the relationship of HADS-A, HADS-D, and PSS-4 scores with CDS scores the Pearson correlation coefficient was used. In multivariable analysis, hierarchical multiple linear regression was used to investigate the relationship of HADS-A, HADS-D, and PSS-4 scores with CDS scores, controlling for demographic variables. In this approach, two steps were performed: the demographic variables were entered in the block 1, and the CDS score was inserted to the block 2. Data analysis was undertaken using SPSS for windows, version 16.0 (SPSS Inc., Chicago, IL, USA) and statistical significance (P) was interpreted as <0.05.
3. Results
3.1. Caregivers characteristics
The demographic characteristics of the caregivers are presented in Table 1 . According to the exclusion criteria, data of five caregivers were excluded. The mean age of the caregivers was 35.47 (SD = 6.59) years. Of the 160 caregivers, 84.4 % were female, 95.0 % were married, 20.0 % were employed, and 49.4 % had a university education.
Table 1.
Demographic characteristics of the caregivers (n = 160).
| Mean (SD) or n (%) | |
|---|---|
| Age (years), Mean (SD) | 35.47 (6.59) |
| Sex | |
| Male | 25 (15.6) |
| Female | 135 (84.4) |
| Marital status | |
| Single | 8 (5.0) |
| Married | 152 (95.0) |
| Education | |
| Elementary | 13 (8.1) |
| High school | 68 (42.5) |
| University | 79 (49.4) |
| Occupation | |
| Employed | 32 (20.0) |
| Unemployed | 128 (80.0) |
| Income | |
| < 40,000,000 Rials | 139 (86.9) |
| ≥ 40,000,000 Rials | 21 (13.1) |
| Caregiver mental illness | |
| No | 117 (73.1) |
| Yes | 43 (26.9) |
| Caregiver physical illness | |
| No | 143 (89.4) |
| Yes | 17 (10.6) |
| Type of CP | |
| Hemiplegic | 40 (25.0) |
| Diplegic | 35 (21.9) |
| Quadraplegic | 85 (53.1) |
| Other disease | |
| No | 68 (42.5) |
| Yes | 92 (57.5) |
| Child’s age (y) | 7.93 (4.55) |
SD: Standard Deviation; CP: Cerebral Palsy.
3.2. Distribution of HADS and CDS scores
The mean HADS-A and HADS-D scores for all caregivers were 7.88 (SD = 3.94) and 7.43 (SD = 4.25), respectively. Using a cut-off value of >8 for both subscales, the prevalence of anxiety, depression, and comorbid anxiety-depression were 45.0% (n = 47), respectively. The mean CDS score was 58.51 (SD = 13.87).
3.3. Relationship of HADS-A and HADS-D scores with demographic variables
Table 2 shows the relationships between the HADS-A and HADS-D scores and demographic variables among caregivers of children with CP using univariable analysis. The mean HADS-A score in caregivers with low incomes was significantly higher than the caregivers with high incomes (P = 0.013). Caregivers who had elementary education obtained higher HADS-A scores compared to caregivers who had a high school/university education (P = 0.044). The mean HADS-A score in married participants was higher than the single participants, although this difference was not statistically significant (P = 0.064).
Table 2.
Relationship of anxiety and depression with demographic variables and burden of care in parents of children with CP during the COVID-19 pandemic.
| Anxiety |
Depression |
Stress |
||||
|---|---|---|---|---|---|---|
| Mean (SD) or r | P | Mean (SD) or r | P | Mean (SD) or r | P | |
| Age (y) | −0.083 | 0.298 | −0.097 | 0.223 | −0132 | 0.095 |
| Sex | 0.224 | 0.029 | 0.531 | |||
| Male | 7.00 (3.45) | 5.72 (3.53) | 6.40 (2.89) | |||
| Female | 8.04 (4.01) | 7.74 (4.31) | 6.81 (3.06) | |||
| Marital status | 0.064 | 0.292 | 0.232 | |||
| Single | 5.38 (4.14) | 5.88 (4.36) | 5.50 (3.55) | |||
| Married | 8.01 (3.89) | 7.51 (4.25) | 6.82 (3.00) | |||
| Education | 0.044 | 0.345 | 0.711 | |||
| Elementary | 10.46 (4.07) | 9.08 (4.33) | 7.38 (2.93) | |||
| High school | 7.78 (4.14) | 7.25 (4.40) | 6.76 (3.16) | |||
| University | 7.54 (3.62) | 7.30 (4.11) | 6.63 (2.96) | |||
| Occupation | 0.245 | 0.038 | 0.697 | |||
| Employed | 7.16 (4.02) | 6.03 (3.80) | 6.56 (2.95) | |||
| Unemployed | 8.06 (3.91) | 7.77 (4.30) | 6.80 (3.06) | |||
| Income | 0.013 | 0.664 | 0.954 | |||
| < 40,000,000 R | 8.18 (3.98) | 7.48 (4.34) | 6.76 (3.10) | |||
| ≥ 40,000,000 R | 5.90 (3.06) | 7.05 (3.69) | 6.71 (2.55) | |||
| Caregiver Mental Illness | 0.102 | 0.184 | 0.271 | |||
| No | 7.57 (4.03) | 7.15 (4.22) | 6.59 (3.05) | |||
| Yes | 8.72 (3.57) | 8.16 (4.30) | 7.19 (2.96) | |||
| Caregiver Physical Illness | 0.435 | 0.041 | 0.541 | |||
| No | 7.80 (3.92) | 7.19 (4.19) | 6.70 (3.07) | |||
| Yes | 8.59 (4.15) | 9.41 (4.37) | 7.18 (2.77) | |||
| Type of CP | 0.642 | 0.695 | 0.094 | |||
| Hemiplegic | 7.50 (4.59) | 7.90 (4.69) | 5.92 (3.24) | |||
| Diplegic | 7.66 (3.74) | 7.43 (4.27) | 7.40 (2.81) | |||
| Quadroplegic | 8.15 (3.70) | 7.20 (4.06) | 6.87 (2.96) | |||
| Child’s Other Disease | 0.519 | 0.884 | 0.916 | |||
| No | 7.65 (3.43) | 7.37 (4.18) | 6.78 (2.74) | |||
| Yes | 8.05 (4.28) | 7.47 (4.33) | 6.73 (3.24) | |||
| Child’s age (y) | 0.059 | 0.460 | −0.017 | 0.832 | −0.030 | 0.710 |
SD: Standard Deviation; CP: Cerebral Palsy, r: Pearson correlation coefficient.
Compared to males, females had higher scores on HADS-D (P = 0.029). Unemployed caregivers exhibited higher scores of HADS-D compared to employed caregivers (P = 0.038). Caregivers who had a physical illness obtained higher scores on HADS-D compared to those who had no physical illness (P = 0.041). As presented in Table 2, stress was not significantly related to demographic variables (all P > 0.05).
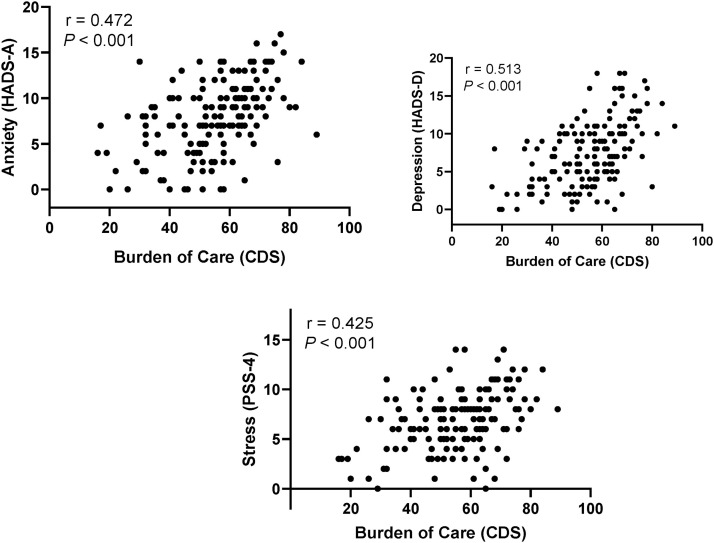
As shown in Fig. 1 , there were significant positive correlations between CDS scores and measures of anxiety (r = 0.472, P < 0.001), depression (r = 0.513, P < 0.001), and stress (r = 0.425, P < 0.001).
Fig. 1.
Relationship of burden of care with measures of anxiety, depression, and stress among parents of children with CP during the COVID-19 pandemic.
HADS: Hospital Anxiety and Depression Scale; PSS-4: Perceived Stress Scale-4 item; CDS: Caregiver Difficulties Scale.
3.4. Multiple linear regression analysis
Hierarchical multiple linear regression analyses were performed to examine the variables related to the anxiety, depression, and stress scores (Table 3 ). Regarding anxiety, in block 1, being married, low educational level and low income were significantly related to high HADS-A scores (Table 3). When the demographic variables were included in the model, the model R2 was equal to 0.122, indicating that 12.2 % of the variance in the HADS-A score was explained by the demographic variables. In block 2, CDS score was positively correlated with HADS-A score (b = 0.14, P < 0.001). A one-point increase in the CDS score was associated with a 0.14-point increase in the HADS-A score. When the CDS measure was added to the model, there was a considerable improvement in the model (ΔR2 = 21.4 %). More specifically, an additional 21.4 % of the variance in the HADS-A score was explained by the CDS score.
Table 3.
The results of the hierarchical multiple linear regressions for the factors related to the psychological status of the caregivers of children with cerebral palsy.
| Anxiety |
Depression |
Stress |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | P | b | SE | P | b | SE | P | |
| Block 1: Demographics | |||||||||
| Age (y) | −0.04 | 0.06 | 0.563 | −0.07 | 0.07 | 0.302 | −0.08 | 0.05 | 0.106 |
| Sex (female vs male) | −1.11 | 1.18 | 0.346 | −1.45 | 1.28 | 0.258 | 0.05 | 0.93 | 0.959 |
| Marital status (Married vs Single) | 3.45 | 1.47 | 0.020 | 2.32 | 1.60 | 0.150 | 1.11 | 1.17 | 0.345 |
| Education | |||||||||
| High school vs elementary | −2.65 | 1.21 | 0.030 | −2.52 | 1.31 | 0.057 | −0.64 | 0.96 | 0.504 |
| university vs elementary | −2.18 | 1.22 | 0.077 | −1.63 | 1.33 | 0.221 | −0.60 | 0.97 | 0.535 |
| Occupation (unemployed vs employed) | −0.43 | 1.07 | 0.686 | 0.85 | 1.16 | 0.467 | 0.15 | 0.85 | 0.858 |
| Income (≥ 40,000,000 R vs < 40,000,000 R) | −2.08 | 0.99 | 0.038 | 0.22 | 1.08 | 0.837 | 0.37 | 0.79 | 0.636 |
| Caregiver Mental Illness (yes vs no) | 0.78 | 0.82 | 0.345 | 0.24 | 0.90 | 0.790 | 0.43 | 0.65 | 0.509 |
| Caregiver Physical Illness (yes vs no) | 0.32 | 1.16 | 0.782 | 2.53 | 1.26 | 0.046 | 0.57 | 0.92 | 0.533 |
| Type of CP | |||||||||
| diplegic vs hemiplegic | −0.11 | 0.91 | 0.907 | −0.27 | 0.99 | 0.785 | 1.49 | 0.72 | 0.042 |
| quadriplegic vs hemiplegic | −0.16 | 0.82 | 0.848 | −1.41 | 0.89 | 0.117 | 0.62 | 0.65 | 0.344 |
| Child’s Other Disease (yes vs no) | 0.07 | 0.67 | 0.922 | 0.10 | 0.73 | 0.892 | −0.22 | 0.53 | 0.673 |
| Child’s age (y) | 0.07 | 0.08 | 0.431 | 0.04 | 0.09 | 0.641 | 0.04 | 0.07 | 0.582 |
| Model characteristics | R2 = 12.2%, F = 1.56, P = 0.104 | R2 = 11.1%, F = 1.40, P = 0.164 | R2 = 6.8%, F = 0.82, P = 0.637 | ||||||
| Block 2: CDS | |||||||||
| Burden of care | 0.14 | 0.02 | <0.001 | 0.17 | 0.02 | <0.001 | 0.10 | 0.02 | <0.001 |
| Model characteristics | R2 = 33.5%, ΔR2 = 21.4%, F = 5.23, P < 0.001 | R2 = 36.9%, ΔR2 = 25.8%, F = 6.06, P < 0.001 | R2 = 22.9%, ΔR2 = 16.1%, F = 3.08, P < 0.001 | ||||||
b: regression coefficient; SE: Standard Error; CDS: Caregiver Difficulties Scale.
Regarding depression, in block 1, among demographic variables, only having a physical illness was significantly related to HADS-D scores (b = 2.53, P = 0.046). The HADS-D score in caregivers with a high school education was lower than the caregivers with an elementary education, although this difference was not statistically significant (b=−2.52, P = 0.057). The model R2 in this step was 0.111. In block 2, the CDS score was positively correlated with the HADS-D score (b = 0.17, P < 0.001). When the CDS measure was added to the model, there was a considerable improvement in the model (ΔR2 = 25.8 %).
Regarding stress, in block 1, the PSS-4 score in caregivers of children with diplegic CP was higher than caregivers of children with hemiplegic CP (b = 1.49, P = 0.042). The model R2 in this step was 0.068, suggesting that 6.8 % of the variance in the PSS-4 score was explained by the demographic variables. In block 2, the CDS score was positively correlated with the PSS-4 score (b = 0.10, P < 0.001). When the CDS measure was added to the model, there was a considerable improvement in the model (ΔR2 = 16.8 %).
4. Discussion
Our study aimed to describe the mental health of caregivers of children with CP in a lockdown period associated with the COVID-19 outbreak. We surveyed the factors that might have impacts on the psychological status of caregivers with the goal of providing a picture of influential factors on caregivers’ psychological status for the healthcare team when faced with this situation.
We found that approximately half of caregivers (45 %) reported symptoms of anxiety. Based on the results of the HADS-D, forty percent of caregivers also reported being depressed, which is concordant with an Iranian study (Sajedi, Alizad, Malekkhosravi, Karimlou, & Vameghi, 2010). Sajedi et al. reported that 44 percent of 43 mothers of disabled children had mild to severe depressive symptoms. Nearly, one-third of caregivers had both signs of anxiety and depression at the same time which indicates the demanding essence of caregiving. This issue has to be considered as an important subject, because weak psychological health of caregivers affects the quality of caregiving and could lead to worsening the physical difficulties of the children (Farajzadeh et al., 2020; Garip et al., 2017; Khayatzadeh et al., 2013). Also, with continuing COVID-19 lockdown there may be an early discontinuation of care in the home. Therefore, we recommend that healthcare professionals should look at the caregivers not always as only a healthcare team member, but also as a potential patient (Moghimi, 2007).
As expected in demographic characteristics there was a predominance of females in the caregiving process which is consistent with the study by Dalvand et al. (2015), Nobakht, Rassafiani, Hosseini, and Hosseinzadeh (2020). They reported that main caregivers of children with CP in Iran are mothers. The mothers of children with disabilities are in danger of experiencing depression symptoms (Manuel, Naughton, Balkrishnan, Paterson Smith, & Koman, 2003; Ones et al., 2005; Sajedi et al., 2010), and our study confirmed that the depressive state was more common in female caregivers than male ones.
Another key finding was a lack of correlation between type of CP and psychological status of the parents, which is concordant with previous studies that reported the severity and the type of CP are not associated with maternal depression (Garip et al., 2017; Manuel et al., 2003; Ones et al., 2005; Sajedi et al., 2010; Unsal-Delialioglu, Kaya, Ozel, & Gorgulu, 2009). However, there was a significant association between amount of anxiety reported by caregivers and their incomes. In other words, anxiety among low-income caregivers was higher than their high-income counterparts. Lack of social support such as financial resources from governmental and non-governmental agencies in Iran before the pandemic prevalence imposed pressure on families with a child with a physical disability (Khayatzadeh et al., 2013). Emergence of COVID-19, followed by a cross-country lockdown, have devastated most of the businesses and multiplied the financial difficulties of low-income families, resulting in higher amounts of anxiety (Moghanibashi-Mansourieh, 2020).
In this study, education level was also discovered to be associated with anxiety. Our findings indicated that higher levels of education may help caregivers identify more coping strategies to deal with setbacks during lockdown. In fact, having higher education levels may help caregivers to solve the unexpected and never encountered problems (Farajzadeh et al., 2020).
A significant correlation was also found between employment and depression symptoms. Employed caregivers who could count on their salaries during lockdown obtained lower scores of depression than unemployed caregivers, who lost their jobs due to the pandemic outbreak or did not have a job before. So, it seems that having a well-paid or at-least fair salaried job during the time that all businesses are closed might be correlated with the physical or psychological well-being of caregivers and result in lower financial burden and finally fewer psychological life stressors.
The results of the multiple regression analysis revealed that low income, low educational level and being married, are three demographic factors that predicted anxiety among caregivers. This might be because the lockdown situation decreased the income level of people significantly, people with lower education had a lower knowledge to confront this new situation. Also, fear of losing the job or reduction in salary induced anxiety in many individuals which may have affected their marital relationships (Maiti, Singh, Innamuri, & Hasija, 2020). Since low income, low level of education and unemployment can negatively affect the family's access to educational facilities and new communication technologies, these suggest policy-making needs. In addition to policies guiding job opportunities for caregivers and support and healthcare for families with disabled children, policies need to address simpler, more accessible and cheaper ways to educate the parents of these children – including during critical situations such as lockdowns and pandemics. Therapists and professionals involved in the health system and education of the disabled, can provide printed brochures, regular telephone calls or periodic visits to caregivers' homes in compliance with health protocols – all of which can play an effective role in reducing the care burden of these caregivers.
According to the results of hierarchical regression, burden of care was the main predictor of anxiety, depression and stress. This is in line with the study of Cacioppo, in which mental load was claimed as the greatest difficulty of caregivers during the COVID-19 pandemic (Cacioppo et al., 2020). We found that caregiver burden (CDS) predicted more than one-fifth of anxiety experienced by caregivers whereas the demographic characteristics which were significantly correlated with HADS-A, predicted almost twelve percent of that. Similarly, CDS predicted more of depression in comparison with demographic characteristics. COVID-19 perceived related stress was not correlated with demographic features. However, burden had a significant relationship with the perceived stress and predicted it by 16 percent. It can be concluded that burden would significantly predict the caregivers’ psychological problems above and beyond their demographic characteristics, therefore focusing on the burden of caregivers may decrease their mental load.
The more burden imposed to caregivers, the higher psychological symptoms were manifested in caregivers. Diminished participation in social activities due to the pandemic could consequently result in a greater proportion of time caregivers spend on caregiving, encountering fewer positive emotions and an enhanced occurrence of depressive symptoms. These were demanding situations for caregivers even before the pandemic emerged. In fact, there was a lack of adequate educational systems and integrated medical and rehabilitation services and more radically a lack of continuity of rehabilitation care, practical social networks, and suitable social insurance systems for caregivers of children with CP in Iran (Dalvand et al., 2015; Khayatzadeh et al., 2013). Cross-country lockdown made the situation even worse by nearly disrupting the contact between caregivers and health professionals. It has been reported that during COVID-19 a main concern of parents was their children’s rehabilitation (Cacioppo et al., 2020). So this situation suggests the need for providing more information for families relating to using equipment, nursing, and rehabilitation issues especially in children with severe physical disabilities. In addition, healthcare professionals, especially rehabilitation teams in Iran do not have enough knowledge and experience of working with children and caregivers in a virtual atmosphere to decrease the burden imposed on caregivers although emerging attempts have been made recently (Nobakht et al., 2020). Therefore, in order to improve rehabilitation recovery processes and achieve better results for these children, healthcare teams, including occupational and speech therapists and others, have to be armed with enough knowledge to train caregivers in a similar crisis, including the use of telehealth. There also should be a movement toward family-centered services, in which the caregivers work and consult with service providers including rehabilitation members to make them ready to cope with unexpected situations such as burden of care in quarantines due to a pandemic situation. This could support caregivers and therapists and reduce challenges related to child care at home in a lockdown.
There were some limitations to this study. First, many of the participants had low educational status, therefore they may not have had proper access to online services to take part in the survey. Second, since this survey was a cross-sectional study, the mental problems seen in caregivers during the pandemic may have been the results of that situation only and not due to ongoing caregiving situations. Third, we didn’t have a control group consisting of caregivers of normally developing children, so we cannot claim that the COVID-19 crisis had a greater impact on the caregivers of children with CP. Based on the limitations listed, we recommend to encounter families with low incomes and with low usage of communicative technologies through more available data gathering methods such as telephone interviews. To discover the exact difference of caregivers’ mental state before and during the pandemic, retrospective surveys may clarify any differences. Lastly, a study comparing mental health issues in caregivers of children with CP and caregivers of normally developing children would be useful for planning for pandemics.
5. Conclusion
In the current study, the significant predictive effect of burden on caregivers of children with CP during a pandemic was confirmed. We found out burden is the most important predictor of psychological well-being among caregivers, implying that measures by healthcare professions especially rehabilitation teams should lay emphasis on the empowerment of family caregivers. It could be fulfilled by providing suitable virtual or in-person training and facilitating access to necessary resources by supporting caregivers to manage the burden of care better in a time that families have a less access to resources. Policy making and financial facilities to provide caregivers with social communities and to expand caregivers' support network may also have a positive effect on the enhancement of caregivers' sense of competence and control. Future studies are needed to find the healthcare team competency in providing interventions and investigate the effect of those virtual interventions on quality of life and the psychological health of caregivers. The COVID-19 pandemic also had some benefits in terms of changing our view toward the undeniable role of caregivers in healthcare-related jobs. Our data confirm that healthcare teams should understand that instead of just focusing on the child as the only client, it is better to consider a family- centered approach to help the whole family.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Ata Farajzadeh: Conceptualization, Investigation, Writing - original draft, Writing - review & editing. Moslem Dehghanizadeh: Conceptualization, Investigation, Validation, Writing - review & editing. Saman Maroufizadeh: Formal analysis, Visualization, Writing - original draft. Malek Amini: Methodology, Validation, Writing - review & editing. Aryan Shamili: Supervision, Conceptualization, Methodology, Investigation, Validation, Writing - review & editing.
Acknowledgements
The proposal of this study was appraised by Iran University of Medical Sciences (99-1-27-18322). We would also like to acknowledge caregivers of children with cerebral palsy who participated in this study.
Footnotes
Porsline-Online questionnaire software service. (2020). https://survey.porsline.ir/ Accessed from 18th March to 20th May 2020.
References
- Amini P., Maroufizadeh S., Samani R.O. Evaluating the factor structure, item analyses, and internal consistency of hospital anxiety and depression scale in Iranian infertile patients. International Journal of Reproductive BioMedicine. 2017;15(5):287. [PMC free article] [PubMed] [Google Scholar]
- Baltar F., Brunet I. Social research 2.0: Virtual snowball sampling method using Facebook. Internet Research. 2012 [Google Scholar]
- Boldrini P., Bernetti A., Fiore P., Committee S.E. Impact of COVID-19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER) European Journal of Physical and Rehabilitation Medicine. 2020;56(3):316–318. doi: 10.23736/S1973-9087.20.06256-5. [DOI] [PubMed] [Google Scholar]
- Boyle C.A., Fox M.H., Havercamp S.M., Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disability and Health Journal. 2020;13(3) doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo M., Bouvier S., Bailly R., Houx L., Lempereur M., Mensah-Gourmel J., Vagnoni J. Emerging health challenges for children with physical disabilities and their parents during the COVID-19 pandemic: the ECHO French survey. Annals of Physical and Rehabilitation Medicine. 2020 doi: 10.1016/j.rehab.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983:385–396. [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sciences. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay K., Perera B. COVID-19 and people with intellectual disability: Impacts of a pandemic. Irish Journal of Psychological Medicine. 2020;37(3):231–236. doi: 10.1017/ipm.2020.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalvand H., Hosseini S.A., Rassafiani M., Samadi S.A., Khankeh H.R., Kelly G. Co-occupations: The caregiving challenges of mothers of children with cerebral palsy. The British Journal of Occupational Therapy. 2015;78(7):450–459. [Google Scholar]
- Dusek G.A., Yurova Y.V., Ruppel C.P. Using social media and targeted snowball sampling to survey a hard-to-reach population: A case study. International Journal of Doctoral Studies. 2015;10(1):279–299. [Google Scholar]
- Farajzadeh A., Amini M., Maroufizadeh S., Wijesinghe C.J. Caregiver difficulties scale (CDS): Translation and psychometric evaluation among Iranian mothers of cerebral palsy children. Occupational Therapy in Health Care. 2018;32(1):28–43. doi: 10.1080/07380577.2017.1422607. [DOI] [PubMed] [Google Scholar]
- Farajzadeh A., Maroufizadeh S., Amini M. Factors associated with quality of life among mothers of children with cerebral palsy. International Journal of Nursing Practice. 2020;26(3) doi: 10.1111/ijn.12811. e12811. [DOI] [PubMed] [Google Scholar]
- Garip Y., Ozel S., Tuncer O.B., Kilinc G., Seckin F., Arasil T. Fatigue in the mothers of children with cerebral palsy. Disability and Rehabilitation. 2017;39(8):757–762. doi: 10.3109/09638288.2016.1161837. [DOI] [PubMed] [Google Scholar]
- Joghataei M.T., Mohammad K., Rahgozar M., Siadaty S. Prevalence of some paralysis and limb amputation disabilities in Iran national epidemiological survey. Journal of Rehabilitation. 2002 [Google Scholar]
- Johnson A. Prevalence and characteristics of children with cerebral palsy in Europe. Developmental Medicine and Child Neurology. 2002;44(9):633–640. [PubMed] [Google Scholar]
- Khayatzadeh M.M., Rostami H.R., Amirsalari S., Karimloo M. Investigation of quality of life in mothers of children with cerebral palsy in Iran: Association with socio-economic status, marital satisfaction and fatigue. Disability and Rehabilitation. 2013;35(10):803–808. doi: 10.3109/09638288.2012.708818. [DOI] [PubMed] [Google Scholar]
- Leocani L., Diserens K., Moccia M., Caltagirone C. Disability through COVID‐19 pandemic: Neurorehabilitation cannot wait. European Journal of Neurology. 2020 doi: 10.1111/ene.14320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiti T., Singh S., Innamuri R., Hasija M.A.D. 2020. Marital distress during COVID-19 pandemic and lockdown: A brief narrative. [Google Scholar]
- Manuel J., Naughton M.J., Balkrishnan R., Paterson Smith B., Koman L.A. Stress and adaptation in mothers of children with cerebral palsy. Journal of Pediatric Psychology. 2003;28(3):197–201. doi: 10.1093/jpepsy/jsg007. [DOI] [PubMed] [Google Scholar]
- Maroufizadeh S., Zareiyan A., Sigari N. Reliability and validity of Persian version of perceived stress scale (PSS-10) in adults with asthma. Archives of Iranian Medicine. 2014;17(5) 0-0. [PubMed] [Google Scholar]
- Maroufizadeh S., Foroudifard F., Navid B., Ezabadi Z., Sobati B., Omani-Samani R. The Perceived Stress Scale (PSS-10) in women experiencing infertility: A reliability and validity study. Middle East Fertility Society Journal. 2018;23(4):456–459. [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghimi C. Issues in caregiving: The role of occupational therapy in caregiver training. Topics in Geriatric Rehabilitation. 2007;23(3):269–279. [Google Scholar]
- Nobakht Z., Rassafiani M., Hosseini S.A., Hosseinzadeh S. A web-based daily care training to improve the quality of life of mothers of children with cerebral palsy: A randomized controlled trial. Research in Developmental Disabilities. 2020;105:103731. doi: 10.1016/j.ridd.2020.103731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ones K., Yilmaz E., Cetinkaya B., Caglar N. Assessment of the quality of life of mothers of children with cerebral palsy (primary caregivers) Neurorehabilitation and Neural Repair. 2005;19(3):232–237. doi: 10.1177/1545968305278857. [DOI] [PubMed] [Google Scholar]
- Sajedi F., Alizad V., Malekkhosravi G., Karimlou M., Vameghi R. Depression in mothers of children with cerebral palsy and its relation to severity and type of cerebral palsy. Acta Medica Iranica. 2010:250–254. [PubMed] [Google Scholar]
- Turk M.A., McDermott S. The Covid-19 pandemic and people with disability. Disability and Health Journal. 2020 doi: 10.1016/j.dhjo.2020.100944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk M.A., Landes S.D., Formica M.K., Goss K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disability and Health Journal. 2020;13(3):100942. doi: 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unsal-Delialioglu S., Kaya K., Ozel S., Gorgulu G. Depression in mothers of children with cerebral palsy and related factors in Turkey: A controlled study. International Journal of Rehabilitation Research. 2009;32(3):199–204. doi: 10.1097/MRR.0b013e32832607b6. [DOI] [PubMed] [Google Scholar]
- Wijesinghe C., Fonseka P., Hewage C. The development and validation of an instrument to assess caregiver burden in cerebral palsy: Caregiver difficulties scale. The Ceylon Medical Journal. 2013;58(4) doi: 10.4038/cmj.v58i4.5617. [DOI] [PubMed] [Google Scholar]
- Yeargin-Allsopp M., Braun K.V.N., Doernberg N.S., Benedict R.E., Kirby R.S., Durkin M.S. Prevalence of cerebral palsy in 8-year-old children in three areas of the United States in 2002: A multisite collaboration. Pediatrics. 2008;121(3):547–554. doi: 10.1542/peds.2007-1270. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]