Abstract
Background
Cervical cancer is the commonest pelvic malignancy in the world, forth among women cancers, but 2nd commonest after breast cancer in the low & middle income countries. The disease is the second common in Ethiopia, with a prevalence of 13.4% with similar impact of cancer death. The aim of this study is to know the degree of cervical cancer among the suspected, & its associated factors among the women visiting the hospital for cervical cancer & precancer screening at specific period.
Methods and materials
A five years retrospective hospital based cross sectional study was conducted. All clients who came for screening with a visual inspection using acetic acid (VIA) & suspicious of cancer were included. Finally, every suspected woman with a complete chart was included. Data was coded and entered using Epi Data Version 3.1 then was exported to SPSS version 21 for analysis. Proportion, mean and standard deviation were used to describe the study variables. Then bivariate and multivariate logistic regression analyses were used to identify association between independent & outcome variables. Adjusted Odds Ratio (AOR) with 95% Confidence interval (CI) and p value (<0.05) were computed to assess the presence and degree of statistical association between dependent and independent variables.
Result
The prevalence of cervical cancer among the study women was 28%. Illiterate women suspicious with cervical cancer after positive test have five times increased odds of being diagnosed with cervical cancer than those who had formal education AOR 4.885(0.180, 0.741) 95%CI. Women with multiple sexual partners had eleven times increased odds of having cervical cancer than those with single sexual partner AOR 11.5 (1.273,24.34) 95%CI. Also, women who had referral for suspicious lesion for cervical cancer had significant association AOR 5.477(1.715–17.498) 95% CI.
Conclusion
This study has revealed a significant proportion of cervical cancer among the participants; and the factors associated with cervical cancer were multiple sexual partners, poor educational status (Illiterate), & those referred for suspected disease.
Keywords: VIA, Cervical cancer, Associated factors, Ethiopia
Highlights
-
•
This study revealed a higher level of cervical cancer.
-
•
Three quarter of the women were wrongly diagnosed with suspicious lesion for cervical cancer.
-
•
This leads to unnecessary referrals, stress, & expenditure.
-
•
So, the VIA test needs to be revisited,the health workers involved on client evaluation need to be supervised in regular basis, and may need refreshment training.
-
•
Multiple sexual partners, illiterate, referred from other health institutions were strongly associated.
1. Introduction
Cervical cancer is the commonest pelvic malignancies, & the fourth most common cancer among women globally, with 604 000 new cases and 342 000 deaths in 2020(2). About 90% of the new cases and deaths worldwide occurred in low- and middle-income countries, with second common women cancers after breast cancer in this part of the world, but in many countries of the sub-Saharan Africa (SSA) it is the commonest of all [[1], [2]]. In Ethiopia, the most commonly leading cancers among females were cancers of the breast (33%), Cervix uteri (17%) and Ovary (6%) [3]. According to GLOBOCAN report the one year incidence of cervical cancer in Ethiopia is 14.7% [[4], [5]]. Cervical cancer is slow progressing disease, from pre-invasive cervical intraepithelial neoplasia (CIN) to invasive lesion.Women living with HIV are 6 times more likely to develop cervical cancer compared with HIV negatives, & an estimated 5% of all cervical cancer cases are attributable to HIV [[1], [6]].
In low-and middle-income countries (LMICs), there is poor awareness & limited access towards preventative measures, and cervical cancer is often diagnosed at late stage when the women develop metastatic symptoms. In addition, access to treatment of cancerous lesions is also limited, resulting in a higher rate of death from cervical cancer [[1], [7]].
In 2020, there were around 10.0 million cancer deaths and 19.3 million new cases worldwide. Even though, 23.4% of the total cancer cases are diagnosed in Europe, death is higher in Asia and Africa relative to the incidence [4]. From all cancer cases 13% were related to infection, and HPV responsible for 690 000 from a total of 2.2 million new cases [8]. Among cancer in women, cervical cancer is still a major public health problem, ranking the fourth most common cause of cancer incidence and mortality globally [9].
Cervical cancer results from Human Papilloma Virus (HPV) infection. Seventy (70%) cervical cancers and pre-cancerous cervical lesions are attributed to HPV type 16 and18 [10]. More than 95% of cervical cancer lesions are associated with HPV [[1], [11]]. There are 15–20years time gap between the peak HPV infection and the peak of cancer incidence, but could happen faster & earlier (5–10years) in those with HIV/AIDS [10]. HPV vaccine for girls at age of 9–14 years, screening women starting at 30years with early treatment of the precancer would prevent the invasive cancer [10]. There are two peak age specific incidences of invasive cervical cancer at 30–40years, and at older age around 70–80years [12].
There are different histologic types of cervical cancer. Even if the world figures show low number, in a single report in Ethiopia squamous cell carcinoma of the cervix was 90% of all cases and adenocarcinoma account only for 3.85% of cases [12]. Cervical cancer is diagnosed histologically; surgery, chemotherapy and radiotherapy are the possible modes of treatment based on stage of the disease, patient status, & availability of the modalities [10].
There are several risk factors associated with cervical cancer. Age of the woman (40–49 years),multiparity more than two times, starting sexual intercourse before the age of 20 years, having multiple sexual partners, HIV infection, cigarette smoking, illiteracy, low socioeconomic status,& prolonged use of combined oral contraceptive pills [ 16–21].
There are multiple studies which showed the prevalence of cervical precancer & cancer detected using VIA, just to address some [13,14]. Similar studies also addressed referral of suspicious cases to higher health institution. They seem more interested on addressing suspicious high grade lesions, but don't specifically address the invasive cervical lesion. They addressed the extent of positive results, but didn't’ address the accuracy of these positive results on identification of the actual invasive disease. There are some studies which address Histopathologies for abnormal cervix, & show proportion of invasive lesion confirmed [15,16].But, both of these studies are not related to prior VIA test.
Implementing the multiple levels of prevention (vaccination, screening, & treating the precancers) & early treatment of the invasive lesion are very important for prevention. Currently, Ethiopia has been using VIA for screening & treatment of the positive women. Most of the positive results after the VIA test acquire the treatment right away, but suspicious lesions need further evaluation either biopsy, or referred to tertiary settings to make sure that the woman didn't have cervical cancer. Our hospital has its own cervical cancer screening clinic, & being tertiary hospital, accepts multiple suspicious referred cases from health centers & other hospitals.
We intended to know how common is invasive cervical cancer on those cases that have suspicious lesions for the malignancy. False positive results incur unnecessary interventions, referrals, & anxiety to the patients. Our study also addressed the association of the risk factors with cervical cancer. The results of this study serve as a baseline for other wider studies as well as for planning health intervention to reduce the incidence of cervical cancer and improve health of our women.
2. Methods
2.1. Study area and period
The study was conducted at HUCSH from January 1, 2015–december 31, 2019. Hawassa is the capital city of Sidama region located at 275 km south to Addis Ababa, the capital city of Ethiopia. The city has two government (one general and another comprehensive) and 4 private primary hospitals and a number of public and private clinics. HUCSH was established and started its full function in 2005. It is the only tertiary hospital in the region where many cases are referred from different health institutions, & also serving as a teaching hospital for Hawassa College of medicine and health sciences. Gynaecology and Obstetrics is one of the departments where laboring mothers, & other obstetrics and different gynecologic conditions are followed and managed accordingly. The hospital has a catchment population of about 18 million peoples. According to 2017 HIMS, there were about 106 012 and 11 103 patients of all types per year as outpatient and inpatient respectively. Gynecology and Obstetrics department has one gynecologic oncologist, ten Gynecologists and Obstetricians, four General practitioners and 93 midwives. There are also OBGYN residents at different years, medical interns and midwife master students on training in the department. It is one the referral center for suspicious cases of cervical cancer, & itself involved on cervical cancer screening.
2.2. Study design
Institutional based cross sectional study has been made. All women who have visited HUCSH from January 2015–december 2019, for cervical cancer screening & suspicious of malignancy (both referred & identified locally) were included. Three hundred ten charts were retrieved from the hospital registry, which had been suspected of having invasive cervical cancer after visual inspection using acetic acid. Only 279 (90%) charts were eligible for the study, the rest were excluded because of incomplete information. The study was registered at www.researchregistry.com with the UIN: researchregistry8021. This work is reported in line with STROCSS criteria from www.strocssguideline.com [17].
2.3. Data collection tools and procedures
The data was collected from medical records of the 279 charts retrieved from the hospital registry. The information was extracted using a structured check list by trained medical interns. The checklist was prepared by reviewing different literatures related to cervical cancer & associated factors. Data was collected from patient's chart after medical record numbers were obtained from log-books of the VIA screening unit, & pathology department. The check list was pretested, and all the collected checklists were checked for completeness and accuracy. Problems encountered during the data collection were reported to investigators for immediate action. In this study, several risk factors for cervical cancer including socio-demographic, reproductive, & behavioral characteristics, and co morbidity like HIV infection were considered.
2.4. Data quality management & analysis
Data collectors and supervisors were carefully trained about the objective of the study, the meaning of each, alternative answer and blank spaces and when to skip as necessary. The checklist was also carefully designed and prepared in english language and was used for data collection. The collected data was reviewed and checked for completeness and consistency by the principal investigator on a daily basis. Overall, the data collection process was strictly supervised by both the principal investigator and supervisors. To assure and control the quality; validated tool, pretest double data entry and cross checked system were implemented.
Information was coded and entered using Epi Data Version 3.1 then was exported to SPSS version 26 for further data cleaning and analysis. Proportion, mean and standard deviation were used to describe the study variables. Bi-variate and multi-variable logistic regression were also computed to assess statistical association between the outcome variable and independent variables. . Factors that are ≤0.25 significant levels in the bi-variate logistic regression analysis were considered in the multivariable logistic regression analysis. Adjusted Odds Ratio (AOR) with 95% Confidence interval (CI) and p value (<0.05) were computed to assess the presence and degree of statistical association between dependent and independent variables. To check for goodness of fit of the model Hosmer and Lemeshow test was checked. Variables in the Bivariate logistic regression found to be related to the outcome at p-value <0.25 were taken as a candidate variable to the multivariable logistic regression model for possible effect of confounders. Finally, variables having a p-value <0.05 were declared significant factors. Odds ratios with 95% CI are reported for significant variables associated with cervical cancer.
2.5. Study variables
2.5.1. Dependent variable
Cervix cancer.
2.5.2. Independent variable
Socio demographic factors.
Number of sexual partners.
History of family planning use.
HIV status.
Parity.
Age at first sexual intercourse.
History of sexual transmitted diseases.
Cigarette smoking.
History of cervical cancer screening.
Age of the women.
Income.
Marital status.
Educational level.
2.6. Operational definition
Multiple sexual partners: is when the woman has two and above sexual partners, & the same to her partner.
Early sexual intercourse: is practicing of sexual intercourse before 18 years old.
Multiparity: having two and above deliveries.
Grand multi para: woman who had five and above deliveries.
A precancerous cervical lesion: This is also called cervical intraepithelial lesion, is an abnormality on the cells of cervical tissue that can grow to cancer.
Cervical cancer: Histopathology confirmed malignancy of the cervix.
Visual inspection using acetic acid (VIA): is a visual examination of the uterine cervix by applying 3–5% of acetic acid.
VIA positive: presence of acetowhite area, usually near the transformation zone between the old & new squamo-columnar junction (SCJ).
VIA negative: presence of smooth, pink, uniform and featureless cervix.
Suspicious for cancer: presence of cervical ulcer; fungating/exophytic and bleeding mass; VIA-positive (aceto-white) with large (>75%) surface area.
Illiterate-Those women who can't read or write, with low educational status.
Literate-Those women who had formal education, can read & write.
3. Result
3.1. Socio-demographic characteristics
Of 310 cases 279 were eligible with a response rate of 90%, 31 cases were excluded due to incomplete chart. The age of the respondents ranges between 25 and 46 years with a mean age of 38.5 (Mean ± SD = 38.5 ± 9). Most of them (317, 77.8%) were above the age of 35 years. More than half of participants 146(52.3%) were from rural areas. Women who can't read and write were 103 (36.9%) and 277 (99.3%) were married. Regarding occupation and religion, majority (69.9%) were unemployed and 101 (36.2%) were Orthodox Christians respectively. One hundred fifty eight (56.6%) came by themselves, whereas 47 (38.8%) were referred from health centers, & almost half (49.1%) came from Oromia region (Table 1).
Table 1.
Socio-demographic characteristics among women visiting HUCSH for suspicious cervical cancer after VIA, from January 2015 to December 2019.
| Characteristics | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age (years) | 25–34 | 62 | 22.2 |
| ≥35 | 217 | 77.8 | |
| Educational status | Illiterate | 103 | 36.9 |
| Literate | 176 | 63.1 | |
| Marital status | Married | 277 | 99.3 |
| Single | 2 | 0.7 | |
| Occupation | Unemployed | 195 | 69.9 |
| Employed | 84 | 30.1 | |
| Residence | Urban | 132 | 47.3 |
| Rural | 147 | 52.7 | |
| Religion | Orthodox | 101 | 36.2 |
| Protestant | 87 | 31.2 | |
| Muslim | 91 | 32.6 | |
| Mode of referral | Self-referred | 157 | 56.3 |
| Referred | 122 | 43.7 | |
| Sources of referral | Health post | 6 | 5.0 |
| Health center | 47 | 38.8 | |
| District hospital | 43 | 35.5 | |
| Other | 25 | 20.7 | |
| Address(region) | Oromia | 137 | 49.1 |
| Sidama | 86 | 30.8 | |
| SNNPR | 56 | 20.1 |
3.2. Reproductive health related characteristics
In this study, 269 (96.4%) didn't have prior history of cervical cancer screening. Only 1(10%) was positive for cervical cancer among those who had screening. Most (92.1%) didn't use any artificial contraceptive methods; none of them used combined pills. The mean age of first pregnancy was 17.5 years (Mean ± SD = 17.5 ± 2.2), majority of them 19 (70.6%) of women get their first pregnancy at 14–18 years. Two hundred thirty nine (85.7%) were multiparous, while majority 211 (75.6%) were at premenopausal women (Table 2).
Table 2.
Reproductive Health Related characteristics among women visiting HUCSH for suspicious cervical cancer after VIA, from January 2015 to December 2019.
| Characteristics | Category | Frequency | Percentage (%) |
|---|---|---|---|
| History of cervical cancer screening | Yes | 10 | 3.6 |
| No | 269 | 96.4 | |
| Screened (VIA) with cervical cancer | Positive | 1 | 10.0(0.36) |
| Negative | 9 | 90.0(3.24) | |
| Ever used artificial contraceptives | Yes | 22 | 7.9 |
| No | 256 | 92.1 | |
| Contraceptive methods | Combined pills | 0 | 0 |
| Others | 22 | 100 | |
| Parity | Nullipara | 40 | 14.3 |
| Multipara | 239 | 85.7 | |
| Age at first pregnancy | 14–18 | 197 | 70.6 |
| ≥19 | 82 | 29.4 | |
| Menopausal status | Premenopause | 211 | 75.6 |
| Menopause | 68 | 24.4 |
3.3. Sexual behavior and life style factors
The mean age for sexual initiation was 16.9years (Mean ± SD = 16.9 ± 2.06). Two hundred sixteen (77.1%) started practicing sexual activity at age of 13–18 years. In our study, only 51 (18.3%) had multiple sexual partners. Even though 150 (53.8%) didn't have HIV test record, 16 (12.4%) were living with HIV and all of them were on ART. Only five (1.8%) of the study participants were drinking alcohol occasionally. While, none of the participants were cigarette smokers. (Table 3).
Table 3.
Sexual behavior & related life styles among women visiting HUCSH for suspicious cervical cancer after VIA, from January 2015 to December 2019.
| Characteristics | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age at first intercourse | 13–18 | 215 | 77.1 |
| ≥19 | 64 | 22.9 | |
| Sexual partners | Single | 228 | 81.7 |
| Multiple | 51 | 18.3 | |
| HIV test | Yes | 129 | 46.2 |
| No | 150 | 53.8 | |
| HIV test result | Negative | 113 | 87.6 |
| Positive | 16 | 12.4 | |
| Alcohol intake | Yes | 4 | 1.4 |
| No | 175 | 98.6 |
3.4. Prevalence of cervical cancer
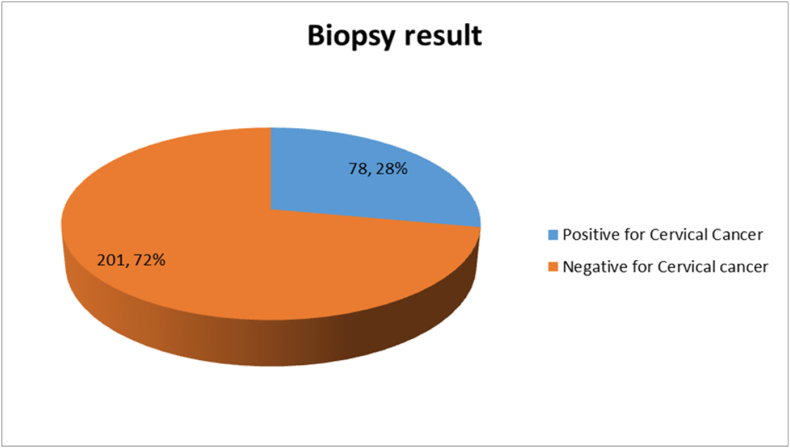
In this study 78 (28%) had a positive biopsy result for cervical cancer. From the positive result 71(91%) were squamous cell carcinoma, which makes it the most common type of cervical cancer. Adenosquamous was the second common 6(7.7%), & the rest 1(1.3%) goes to adenocarcinoma (Fig. 1).
Fig. 1.
Biopsy result of the cervix among women visiting HUCSH for suspicious cervical cancer after VIA, from January 2015 to December 2019.
3.5. Factors associated with cervical cancer
To identify factors associated with cervical cancer both bivariate and multivariate logistic regression analyses were done. Variables were checked if they are candidate for the multivariable model. The candidate variables were selected based on a p-value and those having p < 0.25 were taken to multivariate logistic regression mode. Eleven variables having p-value of less than 0.25 were taken to the multivariable model. Finally, three variables in the multivariate logistic regression model identified to have a statistically significant association with cervical cancer at P-value of <0.05. In this study, those women who are Illiterate and suspicious with cervical cancer after VIA positive test have five times increased odds of being diagnosed with cervical cancer than those who had formal education AOR 4.885(0.180, 0.741) 95%CI. Women with multiple sexual partners had eleven times increased odds of having cervical cancer than those with single sexual partner AOR 11.5 (1.273,24.34) 95%CI. Likewise, women who had been referred for suspicious lesion for cervical cancer had significant association AOR 5.477(1.715–17.498) 95% CI (Table 4).
Table 4.
Bivariate and Multivariate Logistic Regression analyses of factors associated with cervical cancer among women visiting HUCSH from January 2015 to December 2019.
| Cervical cancer | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Category | Yes, n (%) | No, n (%) | COR(95%CI) | P-value | AOR(95% CI) | P-value |
| Age category | 25–34 | 8(10.3) | 54(26.9) | 1 | |||
| ≥35 | 70(89.7) | 147(73.1) | 3.214(1.451–7.119) | .004* | .975(.229–4.157) | .973 | |
| Parity | Nullipara | 8(10.3) | 32(15.9) | 1 | |||
| Multipara | 70(89.7) | 169(84.1) | 1.657(.727–3.774) | .229* | .914(.192–4.355) | .910 | |
| Menopausal status | Premenopause | 45(57.7) | 166(82.6) | 1 | |||
| Post menopause | 33(42.3) | 35(17.4) | 3.478(1.950–6.203) | .000* | 1.805(.543–6.010) | .336 | |
| Educational status | Literate | 42(53.8) | 134(66.7) | 1 | |||
| Illiterate | 36(46.2) | 67(33.3) | 1.714(1.006–2.921) | .048* | 4.885(1.307–18.262) | .018** | |
| Sexual partners | Single | 48(61.5) | 180(89.6) | 1 | |||
| Multiple | 30(38.5) | 21(10.4) | 5.357(2.819–10.182) | .000* | 11.453(3.086–42.498) | .000** | |
| Age at first coitus | 13–18 | 71(91.0) | 144(71.6) | 4.015(1.742–9.252) | .001* | .820(.065–10.268) | .878 |
| ≥19 | 7(9.0) | 57(28.4) | 1 | ||||
| Age at first pregnancy | 14–18 | 11(14.1) | 71(35.3) | 3.327(1.652–6.700) | .001* | 4.896(.512–46.851) | .168 |
| ≥19 | 67(85.9) | 130(64.7) | 1 | ||||
| Hx of cervical screening | yes | 1(1.3) | 9(4.5) | 1 | |||
| No | 77(98.7) | 192(95.5) | 3.609(.450–28.973) | .227* | 1.812(.099–33.036) | .688 | |
| HIV test result | Negative | 26(76.5) | 87(91.6) | 1 | |||
| Positive | 8(23.5) | 8(8.4) | 3.346(1.144–9.789) | .027* | 2.543(.517–12.504) | .251 | |
| Mode of referral | Referred | 48(61.5) | 74(36.8) | 2.746(1.602–4.706) | .000* | 5.477(1.715–17.498) | .004** |
| Self-referral | 30(38.5) | 127(63.2) | 1 | ||||
| Current residence | Rural | 48(61.5) | 99(49.3) | 1.648(.967–2.810) | .066* | .953(.281–3.227) | .938 |
| Urban | 30(38.5) | 102(50.7) | 1 | ||||
NB: * show statistical significance at P-value <0.25.
** show strong statistical association at P-value <0.05 (statistically significant association).
4. Discussion
In this study, the prevalence of cervical cancer diagnosed by biopsy was 28%. The result shows difference with different studies. It is far lower compared to an hospital based histopathologies on symptomatic women in the same hospital [49.3%, 15], but higher than another similar study done in Nepal [4.11%, 10],and a population based study made in this country [4,18].The difference may have happened due to difference in study population,& the reasons of cervical sampling. Squamous cell carcinoma (SCC) is the most common histologic type (91%).It is comparable to other studies made in this country [12,16], but far higher to the global average & the Nepalese study [15].Even if there is no strong evidence on prognosis related to the cell types (SCC, adenocarcinomas, adenosquamous carcinoma), squamous cell carcinoma is still considered the better, with good out come when diagnosed & treated in early stage; precancers would have been picked early if screening implemented on eligible women.
Majority (77.8)of the women are at & older than 35 years with more than 89.7% of the total cases with cervical cancer, still the worst affected age (32.3%).Most (85.7%) of the study participants are multiparous with 70 (29.3%) affected, with 89.7% of the total cases with cervical cancer. It is comparable with another study made in Indonesia & India [19,20]. The disease progress happens to be slow, it may take 20–30years, & older women are expected to be diagnosed with the disease. With increasing parity the physiologic changes of the pregnancy & impact on general health affect the risk of infection with HPV & disease progression.
Most (269, 96.4%) of the women have never been screened for cervical cancer & precancer so far, & almost all (77, 98.72%) cancer cases are in this category, with high proportion diagnosed to have the disease (28.6%), than those who have been screened. Majority (150, 53.8%) of the women were not tested for HIV, and 44(56.4%) had been diagnosed to have the cancer, with high proportion of the disease (29.3%) than women with HIV test. It is universally accepted screening would prevent the invasive lesion, & seems expected the non-screened women are more affected than those who have been screened, even if they are few in number. Infection with HIV increases the risk of infection with HPV, persistence, & progression in to cancer. We never know, those not tested for HIV may be harboring the infection, which increases the risk of being affected by cervical cancer.
Most of the study participants (215, 77.1%) start to have sexual intercourse at the age range of 13–18 years. Almost all of the cancer cases are related with these age groups (71, 91%); with 33.0% of them have the disease. Similar result seen in another study made in India [20].The cervical changes (metaplasia) commonly happen in the adolescent girls, with an increased risk of high risk HPV infection. In the long run these people are vulnerable to develop cervical cancer.
Most of the women had single sexual partner in their life (228, 81.7%), but 29(56.9%) of the women with multiple partner have the disease, with 37.2% from the total cases. Women who have multiple sexual partners have a high risk of acquiring the disease [13].The possible justification might be due to the increased and repeated exposure to different HVP infections, which is the causative agent for the cancer, and if not screened and treated timely will perpetuate the cervical cancer. They are also at risk of acquiring other STIs including HIV, which activate the disease progress from infection with HPV to cancer. Almost all of them have been married (277, 99.3%), & 77(97.5%) of cancer cases are seen in this category; but 1(50%) of the single get diagnosed with the disease, even if we couldn't put a conclusion because of their low number.
The factors associated with cervical cancer were having multiple sexual partners, Illiterates (low educational level, can't read & write),referred to the hospital, diagnosed to have HIV infection, those who had their first pregnancy at the age range of 14–18 years, being in postmenopausal period, and those women who have never had screening for cervical precancer & cancer.
In this study having multiple sexual partners had statistical significant association with cervical cancer (AOR-11.453, P-value-0.000, 95% CI). This finding is concordant with a study in Ethiopia that showed statistical significant effect difference on cervical cancer prevalence between women having >1 sexual partners and women had 1 sexual partner [[13], [21]]. Also, in another study, those women who had two or more lifetime sexual partners and women whose husbands had two or more lifetime sexual partners had higher odds of cervical precancerous lesions [22]. Likewise, Ugandan women with STDs, with increased sexual partners, drink alcohol and smoke had increased risk of developing cancerous and precancerous lesion [23]. The possible justification for the similarity might be due to the increased and repeated exposure to different and multiple sexual partners will let the women to contract the HVP which is the causative agent for the cancer and if not screened and treated timely will eventually develop cervical cancer.
Our study also revealed those women who have low educational status(illiterate) has statistical significant association with cervical cancer (AOR 4.885, P-value 0.018, 95% CI). This finding was supported by another study, having low educational status is a strong factor for development of cervical cancer [24].Women who have formal education are expected to have good knowledge about different medical conditions, including cervical cancer. They also have the courage to seek medical intervention & being evaluated early. The different risk factors for cervical cancer tend to be less in these women. Those who are referred from other institutions had significant association with cervical cancer (AOR 5.477, P-value 0.004, 95% CI).This is most likely related with highly suspicious cases for cervical cancer get referred from the other health institution to the study hospital. So the possibility of diagnosing cervical cancer is higher than those who came for cervical screening & get suspected of having the cancer.
In this study, those women in the post-menopausal period & who have never been screened for cervical cancer have a two times increased odds of developing cervical cancer than their counter parts, even if didn't show statistical significant association. It is supported by other different studies in southern part of the country & Indonesia [16,19]. Women living with HIV have three times increased risk of being diagnosed with cervical cancer, & those who had pregnancy at early age (14–18 years) have five times risk of acquiring the disease. Other studies show similar report [1,25,21].The explanation could be older age & being in post menopause are a well-known risk for multiple pelvic malignancies. Infection with HIV and early age pregnancy increases the metaplastic changes of the cervix, extent of infection with HPV & its persistence, which encourage cellular change for the course of cervical cancer development. Those who have never been screened for cervical cancer & precancer might not have the knowledge & awareness about cervical cancer preventive measures & seeking early medical evaluation. They present to hospital when they get symptomatic with the cancer.
5. Conclusion
This study revealed a higher level of cervical cancer, but three quarter of the women were wrongly diagnosed with suspicious lesion for cervical cancer. This leads to unnecessary referrals, stress, & expenditure. So, the VIA test needs to be revisited,the health workers involved on client evaluation need to be supervised in regular basis, and may need refreshment training.The factors associated with cervical cancer were having multiple sexual partners, those women who are illiterate, referred from other health institutions for suspicious lesion of cervical cancer.
Ethical approval
Ethical approval was given by Hawassa university ethical review board.
Sources of funding
Hawassa university funded for data collectors.
Author contribution
SF & AZ Developed proposal, conduct the study, data interpretation and paper writing.
Registration of research studies
-
1.
Name of the registry: Research registry
-
2.
Unique Identifying number or registration ID: 8194
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry
Guarantor
Both authors.
Consent
The written and signed consent was obtain from the patients.
Declaration of competing interest
No conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104873.
Contributor Information
Shimelis Fantu Gebresilasie, Email: shimelisfantu@gmail.com.
Andualem Zegeye, Email: andualemz30@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO, Cancer 2018. https://www.who.int/news room/fact sheets/detail/cancer September 20 (available from:
- 2.Jedy-Agba E., Joko W.Y., Liu B., Buziba N.G., Borok M., Korir A., et al. Trends in cervical cancer incidence in sub-Saharan Africa. Br. J. Cancer. 2020;123(1):148–154. doi: 10.1038/s41416-020-0831-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.African Cancer Registry Network Ethiopia Addis Ababa City Cancer Reg. 2014 https://afcrn.org/index.php/membership/membership-list/100-addisababa [Available from: [Google Scholar]
- 4.Hyuna S., Bray F., Ferlay J., Soerjomataram I., Seigel R.L., Mathieu L., Jemal A. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 5.International Agency for Research on Cancer Global Cancer Observatory. 2018 https://gco.iarc.fr/today [Available from: [Google Scholar]
- 6.Megan J.H., Jennifer S., Jennifer M.Z., Karen S.M., George S., May M., Elizabeth A.B., Craig R.C. A randomized trial comparing the diagnostic accuracy of visual inspection with acetic acid to visual inspection with lugol's iodine for cervical cancer screening in HIV infected women. PLoS One. 2015;10(4):1–12. doi: 10.1371/journal.pone.0118568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shrestha A.D., Neupane D., Vedsted P., Kallestrup P. Cervical cancer prevalence, incidence and mortality in low and middle income countries: a systematic review. Asian Pac. J. Cancer Prev. APJCP. 2018;19(2):319–324. doi: 10.22034/APJCP.2018.19.2.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Martel C., Georges D., Bray H., Ferlay J., Clifford G.M. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Global Health. 2020;8(2):e180–e190. doi: 10.1016/S2214-109X(19)30488-7. [DOI] [PubMed] [Google Scholar]
- 9.Arbyn M., Weiderpass E., Bruni L., de Sanjose S., Saraiya H., Ferlay J. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Global Health. 2020;8(2):e191–w203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO Human Papillomavirus Cervical Cancer. 2020 https://www.who,int/news room/fact-sheets/detail/human papilloma virus-(hpv)-and cervical cancer November 11 (Available from: [Google Scholar]
- 11.Vanska S., Luostarinen T., Lagheden C., Eklund C., Kleppe S.N., Andrae B., et al. Differing age-specific cervical cancer incidence between different types of human papillomavirus: implications for predicting the impact of elimination programs. Am. J. Epidemiol. 2021;190(4):506–514. doi: 10.1093/aje/kwaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hailu H.E., Mondul A.M., Rozek L.S., Geleta T. Descriptive epidemiology of breast and gynecologic cancers among patients attending Saint Paul's millennium medical college,Ethiopia. PLoS One. 2020;15(3) doi: 10.1371/journal.pone.0230625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gebretsadik H., Hailay G., Tewolde W., Tsgehana G., Kidanemariam G., Mebrahtu T., Manaye K. Magnitude and associated factors of VIA positive test results for cervical cancer screening among refugee women aged 25-49 years in North Ethiopia. BMC Cancer. 2020;20:858. doi: 10.1186/s12885-020-07344-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen V.Q.H., Le M.T., Ngo V.Q.T., Dang C.T., Truong Q.V., Cao N.T., Linus C. The value of visual inspection with acetic acid and Pap smear in cervical cancer screening program in low resource settings: a population-based study. Gyneocol. Oncol. Rep. 2018;24:18–20. doi: 10.1016/j.gore.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parajuli G., Dawadi P., Khadka S. Prevalence of cervical cancer among cervical biopsies in a tertiary care center. J. Nepal Med. Assoc. JNMA. 2020;58(227):453–455. doi: 10.31729/jnma.5060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gemechu A., Fekade Y. Charactestics of cervical disease among symptomatic women with histopathological sample at Hawassa University referral hospital, southern Ethiopia. BMC Wom. Health. 2017;17:91. doi: 10.1186/s12905-017-0444-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ginimol M., Riaz A. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Ann Med. Surg. 2021;72 doi: 10.1016/j.amsu.2021.103026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Memirie S.T., Habtemariam M.K., Asefa M., Deressa B.T., Abayneh G., Tsegaye B., et al. Estimates of cancer incidence in Ethiopia in 2015 using population-based registry data. J. Global Oncol. 2018;4:1–11. doi: 10.1200/JGO.17.00175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Putri A.R., Khaerunnisa S., Yuliati I. Cervical cancer risk factors association in patients at the gynecologic-oncology clinic of dr. Soetomo hospital surabaya. Indonesia J. Cancer. 2019;13(4):104–109. [Google Scholar]
- 20.Sharma P., Pattanshetty S.M. A study on risk factors of cervical cancer among patients attending a tertiary care hospital: a case-control study. Clinic. Epidemiol. Global Health. 2018;6(2):83–87. [Google Scholar]
- 21.Asrat D.Z., Feleke B.E., Mihretie K.M. Prevalence and associated factors of cervical cancer among women in Ethiopia: a systematic review and meta-analysis. Res. Square. 2019 [Google Scholar]
- 22.Megan J.H., Jennifer S., George S., Karen S.M., May M., Naila A., Elizabeth A.B., Craig R.C. Accuracy of visual inspection with acetic acid to detect cervical cancer precursors among HIV-infected women in Kenya. Int. J. Cancer. 2015;136(2):392–398. doi: 10.1002/ijc.28996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrew L.O., Julius W., Anthony O., Emmanuel O. Prevalence of cancerous and pre-malignant lesions of cervical cancer and their association with risk factors as seen among women in the regions of Uganda. J. Clinic. Lab. Med. 2017;2(1) [Google Scholar]
- 24.Ngaon L.T., Yoshimura T. Parity and illiteracy as risk factors of cervical cancers in Viet Nam. Asian Pac. J. Cancer Prev. APJCP. 2001;2(3):203–206. [PubMed] [Google Scholar]
- 25.Stelzle D., Tanaka L.F., Lee K.K., Ibrahim Khalil A., Baussano I., Shah A.S.V., et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Global Health. 2021;9(2):e161–e169. doi: 10.1016/S2214-109X(20)30459-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.