Abstract
Background
Rural, poor, persons with HIV (PWH) and substance use are among the most vulnerable to SARS-CoV-2 and related health service disruptions. The objective of the study was to evaluate the health outcomes and utilization of PWH at an Outpatient-based Opioid Treatment (OBOT) Clinic.
Methods
We evaluated a clinic-based cohort at the University of Alabama at Birmingham HIV clinic from November 2018 to May 2021. We compared HIV outcomes of OBOT patients, who are highly vulnerable, to the overall clinic. We stratified OBOT patients according to comorbid stimulant use disorder and compared clinic utilization and viral load suppression in the 6 months before and after the safer at home mandate (May 2020) in Alabama.
Results
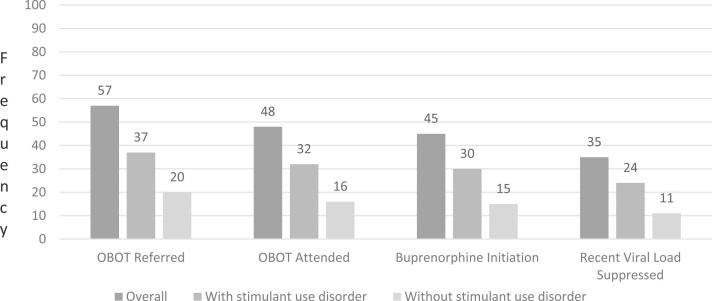
Of 3857 PWH, 57 were referred to OBOT, 48 attended, 45 were initiated on buprenorphine, and 35 had a VL< 200 in the last 6 months. Relative to the overall HIV clinic, OBOT patients were significantly less likely to remain VL suppressed (90% vs 78%, p = 0.01). More patients were suppressed after OBOT linkage (81%) than prior (73%). For those referred before May 2020, there was no change in viral suppression before and after the safer at home order (75%). Although new OBOT referrals did not increase during the pandemic, the number of visits attended per month did increase from a median of 3–4 per patient.
Conclusions
Unlike many PWH who faced access barriers, PWH receiving care at OBOT did not fall out of care but increased healthcare utilization and maintained viral suppression despite the public health emergency.
Keywords: Opioid use disorder, Opioid continuum of care, HIV, SARS-CoV-2
1. Background
Recent HIV outbreaks in persons who inject drugs highlight drug use as a persistent barrier to ending the HIV epidemic (Lerner and Fauci, 2019). This is especially problematic in hard hit rural areas where harm reduction measures, such as syringe service programs, are not legal. Substance use is common among persons with HIV (PWH): up to 25% of PWH report non-medical drug use in the last 2 months and 10% report non-medical opioid use in the last year (Edelman et al., 2014, Skalski et al., 2013). Substance use and, specifically, opioid use disorder reduces one’s ability to achieve and maintain viral load (VL) suppression. Further, HIV viremia plus substance use related behaviors- like transactional sex and sharing drug materials- contribute to HIV transmission in social and sexual networks (Cranston et al., 2019). As a result, the combined Opioid and HIV epidemics continue to drive HIV clusters and outbreaks across the US, halting progress along the HIV care continuum (Cranston et al., 2019, Van Handel et al., 2016). Since 2015, HIV clusters/outbreaks have been reported in PWID in Scott County, IN; Miami, FL; Boston, MA; Henepin and Ramsey Counties, MN; Multnomah County, OR; Philadelphia, PA; Seattle, WA; Cabbell County, WV; and Alaska(Centers for Disease Prevention and Control, Available at). The contemporary, so-called “fourth” wave of the opioid epidemic, involves stimulants like methamphetamines used in conjunction with opioids- a combination which increases both overdose and sexual risk behaviors (Ciccarone, 2021). This deadly polysubstance use trend escalated just as the largest pandemic of our lifetime, SARS-CoV-2, hit U.S. soil (Centers for Disease Prevention and Control, 2021a, Nerlander et al., 2018).
One year into the SARS-CoV-2 pandemic, this novel infection continues to add fuel to the Opioid and HIV syndemics. SARS-CoV-2 has disrupted non-medical drug use patterns, composition, and health care delivery for persons who use substances (Eaton and Clement, 2021, Grebely et al., 2020). Overdose events and deaths have exploded (Ciccarone, 2021, Centers for Disease Prevention and Control, 2021a, Czeisler et al., 2020). Between March 2020 and March 2021, overdose deaths rose 30%, reaching 96,779 deaths, an all-time high (Centers for Disease Prevention and Control, 2021b). Persons who use drugs cite boredom, anxiety, and stockpiling as contributors to increasing drug use (Addiction EMCfDaD, 2020). In addition, the drug supply, including non-opioid, non-medical drugs, is increasingly tainted with potent, synthetic opioids, namely fentanyl(Althoff et al., 2020). Lastly, many low barrier clinics serving persons with HIV and/or substance use have reduced staff, clinic hours or both (Grebely et al., 2020, Dawson and Kates, Available at, Peavy et al., 2020) in order to provide COVID-related service and/or move to telemedicine format. Although many changes were unavoidable, some service disruptions have reduced HIV testing, HIV pre-exposure prophylaxis (PrEP), and other harm reduction services like naloxone (Eaton and Clement, 2021).
This period has also been challenging for clinics treating opioid use disorder (OUD) including the UAB 1917 HIV Clinic Outpatient based Opioid Treatment (OBOT) Clinic, which opened in November 2019. OBOT is an integrated clinic that provides medication for OUD, specifically buprenorphine, to persons with HIV and OUD with the overall goal to retain patients in care, achieve and sustain VL suppression, and reduce harm. Clinic providers and staff can refer patients to OBOT clinic based on patient self-report or clinical diagnosis or concerns of OUD as long as the patient is agreeable. The clinic meets one half day weekly in the 1917 HIV clinic and is staffed by an HIV physician who is waivered to prescribe buprenorphine, a nurse, a social worker, and pharmacist. In addition to OUD services, the clinic provides HIV, STI, and routine health maintenance (e.g., vaccination) when indicated. Hence, patients receive an integrated approach to HIV, sexual health, and preventive services in conjunction with their OUD care. New patients are seen weekly and then move to a monthly or every 2–3-month clinic schedule pending progress with buprenorphine adherence, clinic retention, and HIV viral suppression.
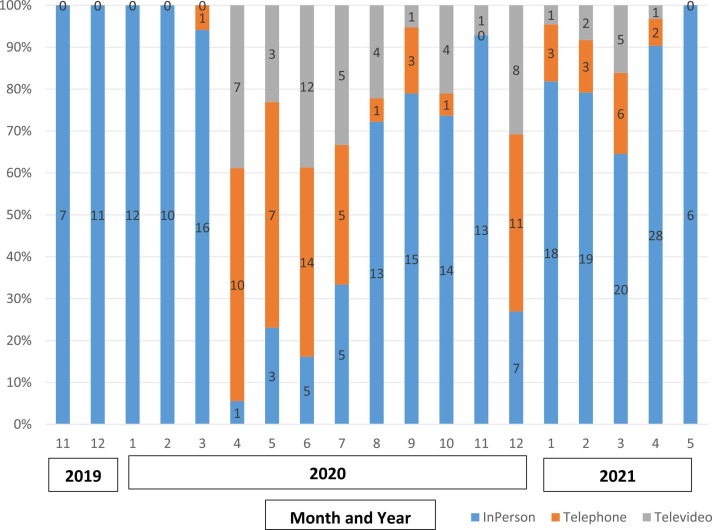
To continue services during the SARS-CoV-2 pandemic, the OBOT clinic began preparing for virtual encounters by training staff and providers on telemedicine in March 2020, and visits were expanded beyond routine clinic hours (Monday mornings) to accommodate high demand. In order to meet the needs of walk-in patients, the clinic never “shut down,” but following the safer at home order, clinic leadership advised all providers to move patient encounters to a telemedicine format unless an in-person visit was absolutely necessary (ie. acute illness requiring physical exam). The UAB eMedicine center scheduled all telemedicine visits including tele-video encounters in 30 min intervals. Due to competing life demands, many OBOT patients missed the pre-scheduled tele-video visits and others did not have access to a smartphone with video capabilities. Thus, most telemedicine visits occurred via telephone only. Other changes following the safer at home order included fewer laboratory visits for HIV viral load and toxicology assessments, fewer ad-hoc counseling and social work encounters integrated into in-person encounters, and more patients received the maximum supply of buprenorphine (30 days) rather than shorter courses. By the fall of 2020, most encounters returned to and remain in person at the brick and mortar clinic.
The objective of this study was to evaluate the OUD and HIV outcomes of OBOT patients during the pandemic. Unfortunately, the clinic was opened in November 2019, a few short months before the pandemic. Hence, disentangling the outcomes of the clinic with the pandemic is not possible. We previously described a significant increase in the UAB 1917 OBOT clinic utilization three months into the SARS-CoV-2 pandemic, which we attribute to the complex needs of PWH and OUD (Eaton et al., Virtual). We hypothesized that as the pandemic continued, OBOT patients would fall out of care (e.g., fewer visits) and experience more HIV viremia relative to the overall clinic population and that those with OUD plus stimulant use disorder would have the worst health outcomes. Because we anticipated that OBOT patients would be more vulnerable to poor health outcomes than others with HIV, we compared HIV outcomes among patients in the OBOT clinic, which is embedded in the 1917 HIV clinic, and the general clinic population.
2. Material and methods
This was a retrospective study of a clinic-based cohort of PWH receiving care at the University of Alabama at Birmingham 1917 HIV Clinic from November 1, 2018 until May 5, 2021. We quantified non-medical opioid use at the 1917 HIV Clinic, determined the number of patients referred to the OBOT clinic, the number receiving medications for OUD (MOUD), and those with HIV suppression. To quantify non-medical opioid use at the clinic level, we determined how many patients reported non-medical opioid use or were identified by providers as having non-medical use. We identified patient report using the ASSIST patient reported outcome assessment, which is conducted on all patients as part of usual care at our clinic every 4–6 months (Crane et al., 2021). We queried provider documentation in the patient’s problem list. In our electronic medical record, the problem list allows documentation of diagnoses, such as OUD, which are electronically linked to ICD9/10 codes, which are easy to query for clinical research. We defined referral to OBOT as any scheduled OBOT appointment (in person or telemedicine). MOUD initiation was defined as receiving a prescription for buprenorphine, and VL suppression was defined as < 200 copies/mL at the most recent assessment. We stratified the OUD continuum of care for those with and without comorbid stimulant disorder (OUD vs OUD+SUD).
Below, we refer to OBOT patients as anyone attending an OBOT visit. For patients attending OBOT clinic, we evaluated sociodemographic traits including age, race/ethnicity, gender, VL. We identified co-morbid stimulant use disorder (OUD + SUD) based on clinical criteria from chart abstraction conducted by a physician (EE). We explored changes in VL and clinic utilization at baseline and following the declaration of a SARS-CoV-2 safer at home mandate in Alabama (Ivey TOoAGKHome Order).
Descriptive statistics are reported as frequency with percentage or mean with standard deviation (SD). Care continuum outcomes expressed as frequency and percentages. Viral load suppression was compared between different groups as follows:
-
a)
Frequency and percentages of all PWH and OBOT attendees were compared using chi-square test of proportion,
-
b)
OBOT attendees were stratified into those with and without stimulant use disorder. “Recent VL” suppression was defined as VL suppression after May 2020 and was compared (frequency with percentages) using chi-square test of proportion,
-
c)
To examine the effect of safer at home order (May 2020), analysis was restricted to patients who attended OBOT clinic in the 6 months before the mandate (November 2019–April 2020). VL suppression was compared between this pre-period and the post-period of May 2020 to October 2020 using McNemar’s test for paired proportions,
-
d)
To examine the effect of OBOT utilization, VL at/prior to the first clinic visit was compared to VL within 180 days of the first visit using McNemar’s test for paired proportions.
Clinic utilization was quantified as visits per month. Trend over time for the number of visits was assessed using Mann-Kendall test; May 2021 was not included in this calculation only as data was closed May 5. Furthermore, sub-analysis was restricted to patients enrolled in the six months prior to May 2020. Number of visits for these patients were compared in the 6 months pre and post May 2020. Lastly, we quantified the frequency in-person visits to telehealth visits (e.g., telephone only and tele-video encounters) from January 2020 to June 2021.
Statistical significance was set at 0.05 (two-tailed). Analysis was conducted using SAS statistical software, version 9.4 (Cary, NC). This study was approved by the University of Alabama Institutional Review Board.
3. Results
A total of 3857 patients (31% white, 66% black, 75% men) received care in the UAB 1917 HIV clinic during the study period. A majority of patients (69%) are over forty years of age: 41–50 years (22%), 51–60 years (28%) and 61 and over (19%). Most are insured with commercial insurance 52%, followed by 37% public and 11% uninsured. Overall, 197 had documentation of non-medical opioid use based on self-report (i.e, PRO) or provider documentation in the patient’s problem list, and 4 were enrolled in a methadone treatment clinic. Of the 197, 41 were referred to OBOT. An additional 16 patients were referred following a clinical diagnosis or concern by their provider, which was not documented in the patient problem list. Overall 57 patients were referred to OBOT from November 2019 to May 2021, 48 attended a visit, 45 were initiated on buprenorphine and 35 (78%) had a recent VL < 200 ( Fig. 1). Of the 45 patients initiated on buprenorphine, 31 were white (69%) and 14 were black (31%), 23 (51%) were men, and mean age was 44 years (SD = 10 years).
Fig. 1.
The Opioid Continuum of Care for PWH at the UAB Outpatient Opioid Treatment Clinic Stratified by OUD alone versus OUD plus Stimulant Use Disorder (November 2019 to May 2021).
Overall, 37 OBOT patients had comorbid OUD and stimulant use disorder (OUD+SUD): 25 had methamphetamine use disorder with or without cocaine use and 12 had cocaine use disorder alone. Of them, 32 attended any visit, 30 were initiated on buprenorphine, and 24 (80%) had a recent VL < 200 (Fig. 1). Of the 20 patients without stimulant use disorder (OUD alone), 16 attended any visit, 15 were initiated on buprenorphine, and 11 (73%) had a recent VL < 200 (Fig. 1). Thus, no significant difference was found between those with and without stimulant use disorder with regard to their recent VL (p = 0.71).
When recent VL (post-May 2020) was compared between those attending OBOT and all 1917 HIV clinic patients, OBOT patients were significantly less likely to be suppressed (78% vs 90%, p = 0.01).
Of OBOT patients initiating buprenorphine (N = 45), 31 had at least one viral load available after OBOT linkage; the other 14 were recently enrolled (<180 days). Of the 31, 28 had a VL within 180 days of the first visit. Of the 28 patients, more patients (24, 86%) were suppressed after the clinic visit than prior to the visit (20, 71%), although not statistically significant (p = 0.10).
When comparing OBOT patients before and after safer at home order, 21 attended OBOT before, and, among them, 20 had a VL available both before and after May 2020. There was no change in the percentage (15, 75%) with VL suppression before and after this mandate.
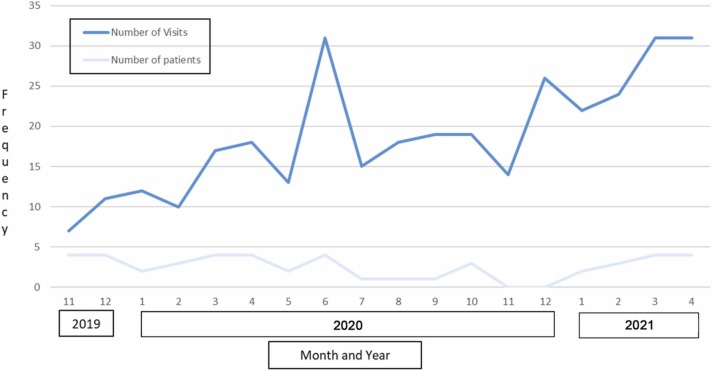
When comparing clinic utilization, the average number of new patients enrolled per month in OBOT did not increase during the study period: there were 4, 2, and 3 new patients per month in 2019, 2020, and 2021, respectively ( Fig. 2). The number of arrived visits per month increased in a clinically significantly manner from 9 to 18–27 visits in 2019, 2020, and 2021 respectively; this trend was also statistically significant (p < 0.001). To account for the accumulation of more OBOT enrollees over the study period, we examined whether there was any difference in number of visits for those enrolled (N = 21) prior to safer at home order in a paired test (signed rank test). In the 6 months before May 2020, there were 75 visits, and there were 73 during the May-October 2020 period. However, the number of visits attended per OBOT patient increased from a median of 3 visits (prior period) to a median of 4 visits following the safer at home order (p = 0.79). Lastly, the percentage of in-person and telehealth visits is summarized in Fig. 3.
Fig. 2.
Number of New Patients and Total Arrived Visits by Year and Month.
Fig. 3.
Percentage of In-person, Telephone, and Televideo encounters in the OBOT Clinic (Nov 2019–May 2021).
4. Discussion
The rapid growth of the UAB 1917 OBOT Clinic over the last 18 months highlights the acute need for addiction treatment in PWH, an urgency which predates the SARS-CoV-2 pandemic. The OBOT patient populations reflects the opioid crisis, which has been crippling for young women, both black and white communities, and middle age Americans. Whereas the overall 1917 HIV clinic population illustrates the HIV epidemic in America, which disproportionately affects black men. We anticipated that OBOT patients, due to psychosocial comorbidities, would experience loss to follow up and worsened HIV viremia as the pandemic marched on (Seo et al., 2021, Mehrotra et al., 2020, Fadul, 2020). However, patients fared better than expected: clinic visits per month increased significantly and the percent of OBOT patients with VL suppression remained stable at approximately 75% despite COVID-related changes in care delivery.
Due to reports of national mental health and overdose crises, we anticipated an increasing number of new OBOT patients in the context of the pandemic. However, the number of new referrals per month remained stable over the study period. At the same time, the number of OBOT encounters per patient increased from 3 to 4 visits per 6-month interval when comparing the period immediately before and after the safer at home order. In other words, patients actually attended more visits during the pandemic contrary to concerns that vulnerable patients would fall out of care.
Despite disruptions in traditional care, a majority of OBOT referrals engaged in care, received treatment, and were virally suppressed. Nonetheless, there are still opportunities for progress. A surprisingly low percentage of PWH reported non-medical opioid use on PROs, which likely underestimates the true OUD burden in our clinic located in central Alabama- an opioid hot spot (Van Handel et al., 2016). Approximately 30% of patients referred to OBOT did not report non-medical opioid use on PROs or have documentation of non-medical use, meaning a provider referred them based on clinical concerns rather than patient self-report. Unfortunately, underreporting is common and attributable, at least in part, to substance use stigma which is amplified in the Deep South (Browne et al., 2016). In order to rapidly identify and treat OUD, clinics must treat substance use disorder similar to HIV-as a chronic disease for which patients are supported and not shamed.
Telemedicine was not a service of the OBOT or 1917 Clinic prior to the SARS-CoV-2 pandemic. However, the risk of illness to patients and staff made it necessary for our clinic, along with many nationwide, to pivot to a virtual format. Although many of our patients lack smartphones, Wi-Fi, and media packages for tele-video, most have access to a telephone. Thus, telephone visits became the standard for many OBOT patients during the height of the first COVID-19 wave in Summer 2020. Through these encounters we learned that reaching patients during the prescheduled 30-minute encounter was challenging due to their chaotic lifestyles and competing demands, hence, multiple follow up calls were often necessary before successfully completing the encounter, and the phone encounter often occurred an hour or more after the scheduled visit. We also learned the importance of ad hoc visits when a patient arrived in person to the clinic outside of OBOT clinic hours. At times, a patient would arrive at our pharmacy or request social work services outside of routine OBOT hours (Monday mornings), and it was clear that the patient was in distress due to social or emotional stressors. On-site staff would often facilitate linkage to the OBOT provider, who was offsite, via a telephone encounter to allow for counseling, assessment, and medication adjustments when necessary. These examples demonstrate how a virtual clinic can extend the half-day clinic offerings, in terms of both time and space, to meet patients where they are. But, this type of flexibility is only possible with engaged providers, accommodating staff, and support from leadership.
Consistent with national trends, stimulant use disorder, and especially methamphetamine use, is prevalent among PWH with OUD in Alabama. Because stimulants may worsen treatment adherence and increase sexual behaviors, like chem-sex, stimulant use disorder is an additional obstacle to Ending the HIV Epidemic (Pufall et al., 2018). Further, because pharmacotherapies are only modestly effective, stimulant use disorder may be more difficult to treat and may compromise recovery for patients who successfully link to MOUD. Contrary to our hypothesis, those with comorbid stimulant use disorder (OUD + SUD) did not experience worse outcomes (Eaton et al., Virtual). Although the subset with OUD + SUD is a small sample size, this finding suggests that integrated HIV and OUD services may allow those with polysubstance use to improve HIV outcomes as well. We anticipate that the frequent and structured OBOT visits with both a clinician and social worker provided essential support for those with OUD + SUD keeping them engaged throughout the public health crisis.
This study of a single clinic-based cohort is limited due to the small sample size and lack of long-term follow up in a clinic which was just opened in 2019. Because the clinic was opened a few short months before the SARS-CoV-2 pandemic, it is challenging to determine to what extent patient outcomes are affected by engagement in OBOT care versus the pandemic. There are also unanswered questions around the low OBOT referral rate for patients identified as having non-medical opioid use. Reasons patients with non-medical opioid use may not be referred include: patient reported non-medical use but not meeting provider’s clinical OUD criteria, patient declined OBOT referral, patient receiving opioids for medical use and misinterpreted question. It is possible there is selection bias in terms of which patients were referred to OBOT; they may have more overt signs of OUD and may not reflect those with less obvious signs and symptoms of OUD. The study is limited by missing data on viral load after OBOT linkage as a significant percentage were linked to care within the last 6 months, and many providers only check viral load at 6 month intervals.
However, the results have important implications as we strive to return patient care to normalcy and minimize further disruptions to essential patient care. We must keep our clinic doors open as much as possible and provide virtual options when needed. We must train and employ ample numbers of addiction providers to fill this growing treatment gap. And HIV providers are uniquely suited to fill this roll. Like HIV, OUD is confounded by social determinants of health, chronic comorbidities, and intersectional stigma. Furthermore, like antiretroviral therapy for HIV, MOUD are highly effective, and, when retained in effective treatment, patients with OUD live long, healthy lives.
5. Conclusion
Developing OBOT care models and recruiting providers to staff them should be a priority for health systems serving PWH. As a pandemic-tested model of care, this innovative clinic has the potential to serve our most vulnerable and stigmatized patients through times of chaos and uncertainty- health care disruptions, civil unrest, and future public health crises.
Role of funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributors
EE developed the concept, chart review, and drafted manuscript; AT performed statistical analysis; WT assisted with regulartory documents, edited manuscript; JT assisted with concept development and editing; MS and KC assisted with study design, interpretation of results and editing.
Conflict of Interest
EE has received research funding to UAB on behalf of the Gilead HIV Research Scholarship. Other authors have no relevant conflicts of interest.
Acknowledgements
EFE has received research funding to her institution from NIH (1 R01 MH124633-01), SAMHSA (1H79SP082270-01), the Center for AIDS Research (P30 AI027767 Supplement), and the Gilead HIV Research Scholarship.
References
- Addiction EMCfDaD. European Drug Report 2020: Trends and Developments. Available at: 〈https://www.emcdda.europa.eu/publications/edr/trends-developments/2020_en〉. Accessed April 28, 2021 2021.
- Althoff K.N., Leifheit K.M., Park J.N., Chandran A., Sherman S.G. Opioid-related overdose mortality in the era of fentanyl: monitoring a shifting epidemic by person, place, and time. Drug Alcohol Depend. 2020;216 doi: 10.1016/j.drugalcdep.2020.108321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne T., Priester M.A., Clone S., Iachini A., DeHart D., Hock R. Barriers and facilitators to substance use treatment in the rural south: a qualitative study. J. Rural Health. 2016;32:92–101. doi: 10.1111/jrh.12129. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Prevention and Control. Recent HIV Clusters and Outbreaks Across the United States Among People Who Inject Drugs and Considerations During the COVID-19 Pandemic. Available at: 〈https://emergency.cdc.gov/han/2020/han00436.asp〉. Date 10/5/2020. Accessed 1/4/2022.
- Centers for Disease Prevention and Control. Overdose Deaths Accelerating During COVID-19. Available at: 〈https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html〉. Accessed April 7 2021a.
- Centers for Disease Prevention and Control. Provisional Drug Overdose Death Counts. Available at: 〈https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm〉. Accessed November 11 2021b.
- Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr. Opin. Psychiatry. 2021;34:34–350. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane H.M., Nance R.M., Whitney B.M., Ruderman S., Tsui J.I., Chander G., McCaul M.E., Lau B., Mayer K.H., Batey D.S., Safren S.A., Moore R.D., Eron J.J., Napravnik S., Mathews W.C., Fredericksen R.J., Hahn A.W., Mugavero M.J., Lober W.B., Saag M.S., Kitahata M.M., Delaney J.A.C. Drug and alcohol use among people living with HIV in care in the United States by geographic region. AIDS Care. 2021;33:1–8. doi: 10.1080/09540121.2021.1874274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranston K., Alpren C., John B., Dawson E., Roosevelt K., Burrage A., Bryant J., Switzer W.M., Breen C., Peters P.J., Stiles T., Murray A., Fukuda H.D., Adih W., Goldman L., Panneer N., Callis B., Campbell E.M., Randall L., France A.M., Klevens R.M., Lyss S., Onofrey S., Agnew-Brune C., Goulart M., Jia H., Tumpney M., McClung P., Dasgupta S., Bixler D., Hampton K., Amy B., Jaeger J.L., Buchacz K., DeMaria A Jr. Notes from the field: HIV diagnoses among persons who inject drugs - Northeastern Massachusetts, 2015-2018. MMWR Morb. Mortal. Wkly Rep. 2019;68:253–254. doi: 10.15585/mmwr.mm6810a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S. Mental HEalth, Substance Use, and Suicidal Ideation During the COVID-19 pandemic - United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson L., Kates J. Delivering HIV Care and Prevention in the COVID Era: A National Survey of Ryan White Providers. Available at: 〈https://www.kff.org/report-section/delivering-hiv-care-prevention-in-the-covid-era-a-national-survey-of-ryan-white-providers-issue-brief/〉. dec 16, 2020. Accessed 1/4/2022.
- Eaton E.F., Clement M.E. Wave the yellow flag: why we should prioritize routine human immunodeficiency virus and sexually transmitted infection care now. J. Infect. Dis. 2021;223:930–932. doi: 10.1093/infdis/jiab052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton EF, Hunt P., Turner O., Raper J., Saag MS. Opioid continuum of care for persons living with HIV: the first 8 months. In: IDweek. (Virtual). March 15, 2021.
- Edelman E.J., Tetrault J.M., Fiellin D.A. Substance use in older HIV-infected patients. Curr. Opin. HIV AIDS. 2014;9:317–324. doi: 10.1097/COH.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadul N. 112. A quality management project of a midwestern academic HIV clinic operation during COVID-19: implementation strategy and preliminary outcomes. Open Forum Infect. Dis. 2020;7:S184–S185. [Google Scholar]
- Grebely J., Cerdá M., Rhodes T. COVID-19 and the health of people who use drugs: what is and what could be. Int J. Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Handel M.M., Rose C.E., Hallisey E.J., Kolling J.L., Zibbell J.E., Lewis B., Bohm M.K., Jones C.M., Flanagan B.E., Siddiqi A.E., Iqbal K., Dent A.L., Mermin J.H., McCray E., Ward J.W., Brooks J.T. County-level vulnerability assessment for rapid dissemination of hiv or hcv infections among persons who inject drugs, United States. J. Acquir Immune Defic. Syndr. 2016;73:323–331. doi: 10.1097/QAI.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivey TOoAGK. Governor Ivey Issues Amended Safer at Home Order. https://governor.alabama.gov/newsroom/2021/03/governor-ivey-amends-safer-at-home-order-to-reflect-latest-cdc-guidance/. date march 22, 2021. Accessed 1/4/2022.
- Lerner A.M., Fauci A.S. Opioid injection in rural areas of the United States: a potential obstacle to ending the HIV epidemic. JAMA. 2019;322:1041–1042. doi: 10.1001/jama.2019.10657. [DOI] [PubMed] [Google Scholar]
- Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D., Schneider EC. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. Available at: 〈https://www.commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge〉. Accessed May 26 2021.
- Nerlander L.M.C., Hoots B.E., Bradley H., Broz D., Thorson A., Paz-Bailey G. HIV infection among MSM who inject methamphetamine in 8 US cities. Drug Alcohol Depend. 2018;190:216–223. doi: 10.1016/j.drugalcdep.2018.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peavy K.M., Darnton J., Grekin P., Russo M., Green C., Merrill J.O., Fotinos C., Woolworth S., Soth S., Tsui J.I. Rapid implementation of service delivery changes to mitigate COVID-19 and maintain access to methadone among persons with and at high-risk for HIV in an opioid treatment program. AIDS Behav. 2020;24:2469–2472. doi: 10.1007/s10461-020-02887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pufall E.L., Kall M., Shahmanesh M., Nardone A., Gilson R., Delpech V., Ward H., Positive Voices study g. Sexualized drug use (‘chemsex’) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med. 2018;19:261–270. doi: 10.1111/hiv.12574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo J.H., Kim S.J., Lee M., Kang J.I. Impact of the COVID-19 pandemic on mental health service use among psychiatric outpatients in a tertiary hospital. J. Affect. Disord. 2021;290:279–283. doi: 10.1016/j.jad.2021.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalski L.M., Sikkema K.J., Heckman T.G., Meade C.S. Coping styles and illicit drug use in older adults with HIV/AIDS. Psychol. Addict. Behav. 2013;27:1050–1058. doi: 10.1037/a0031044. [DOI] [PMC free article] [PubMed] [Google Scholar]