Abstract
Especially individuals with mental disorders might experience an escalation of psychopathological symptoms during the COVID-19 pandemic. Therefore, we investigated the role of anxiety, depressive, and other mental disorders for levels and longitudinal changes of COVID-19-related fear, anxiety and depressive symptoms during the first months of the COVID-19 pandemic in Germany. In a longitudinal observational design with four assessment waves from March, 27th until June, 15th 2020, a total of 6,551 adults from Germany was assessed. 4,175 individuals participated in one, 1,070 in two, 803 in three, and 503 in all four waves of data collection. Multilevel analyses revealed that across all assessment waves, COVID-19-related fear, anxiety, and depressive symptoms were significantly higher in individuals with vs. without anxiety, depressive, and other mental disorders. All symptoms decreased on average over time, and this decrease was significantly stronger in individuals with vs. without anxiety disorders, and particularly driven by individuals with generalized anxiety disorder. Our findings suggest that individuals with mental disorders, especially anxiety disorders – and in particular those with a generalized anxiety disorder – seem to be vulnerable to experience psychological strain in the context of the pandemic, might likely overestimate potential threat, and should be targeted by preventive and therapeutic interventions.
Keywords: SARS-CoV-2, Corona, Mental health, Distress, Mental strain, Vulnerability
1. Introduction
A growing body of research around the globe suggests that the COVID-19 pandemic relates to increased mental health impairments (Bäuerle et al., 2020; Cooke, Eirich, Racine, & Madigan, 2020; Feng et al., 2020; Mazza et al., 2020; Ozamiz-Etxebarria, Dosil-Santamaria, Picaza-Gorrochategui, & Idoiaga-Mondragon, 2020; Petzold, Bendau, Plag, Pyrkosch, Mascarell Maricic, Betzler et al., 2020; Sibley et al., 2020; Tan et al., 2020; Taylor et al., 2020a; Twenge & Joiner, 2020; Wang et al., 2020). For example, in a general population sample of adults from the US (Twenge & Joiner, 2020), heightened anxiety and depressive symptoms were three times more frequent during the initial phase of the pandemic in early 2020 as compared to 2019. Recent data of a longitudinal study with adults from Germany (Bendau, Petzold et al., 2020; Bendau, Plag et al., 2020) showed that anxiety and depressive symptoms were particularly high in early 2020, but attenuated in the following months of the pandemic. Overall, these findings are in line with previous evidence that mental health problems tend to be highly prevalent during times of crises (e.g., wars and natural disasters) (Bonanno, Brewin, Kaniasty, & La Greca, 2010).
The risk to experience mental health issues when facing adversities considerably varies between individuals (Bonanno et al., 2010). Vulnerability-stress models (Ingram & Luxton, 2005; Zuckerman, 1999) and previous studies (Norris et al., 2002; North, 2013) suggest that specific vulnerabilities (e.g., pre-existing mental disorders) predispose to respond with psychopathological symptoms to times of crises and stress. In line with symptom-progression models (Shear, Bjelland, Beesdo, Gloster, & Wittchen, 2007; Wittchen et al., 2014), previous research has shown that psychopathology typically unfolds gradually over time (Asselmann, Wittchen, Lieb, Höfler, & Beesdo-Baum, 2014; Beesdo, Knappe, & Pine, 2009) and that past and current mental disorders rank among the top risk factors for a further escalation of mental health problems (Asselmann, Wittchen, Lieb, & Beesdo-Baum, 2018; Beesdo et al., 2007). It is thus plausible to assume that individuals with pre-existing mental disorders not only experience higher levels of psychopathological symptoms, but also more unfavorable symptom changes during the COVID-19 pandemic.
In a general population sample of adults from Canada and the US, pre-existing depressive and anxiety disorders were associated with higher COVID-19-related distress (Asmundson et al., 2020; Taylor et al., 2020b). Anxiety disorders were associated with even higher COVID-19-related distress and anxiety symptoms as compared to depressive disorders. However, it has not been investigated yet if changes in psychopathological symptoms such as depressive and anxiety symptoms during the initial phase of the COVID-19 pandemic differed between individuals with and without specific pre-existing mental disorders as well as how the psychological reaction of those groups develop over time in the pandemic as a phase of constant changes. Such research requires longitudinal study designs with multiple waves of assessment throughout the first months of the COVID-19 pandemic.
Anxiety and depressive disorders belong to the most frequent mental disorders (Jacobi et al., 2015; Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). Examining their role for COVID-19-related fear, depressive, and anxiety symptoms during the COVID-19 pandemic is thus particularly crucial. Although anxiety and depressive disorders are similar and often co-occur (Goldberg, Krueger, Andrews, & Hobbs, 2009), both diagnostic classes partially differ with respect to their etiology, progress, and outcomes (Asselmann, Hertel et al., 2018; Beesdo, Pine, Lieb, & Wittchen, 2010; Hettema, 2008). Therefore, it is essential to examine whether levels and changes in COVID-19-related fear, depressive, and anxiety symptoms differ between individuals with pre-existing anxiety and depressive disorders (in their pure and comorbid form). Moreover, anxiety disorders are a phenotypically highly heterogeneous group of disorders (Craske et al., 2009). For this reason, assessing the role of individual diagnoses of anxiety disorders for symptom changes during the pandemic is additionally important. Such research promises to considerably improve an early recognition of individuals who are at increased risk for a vicious cycle of psychopathological symptoms during (and after) the COVID-19 pandemic and might thus benefit from targeted prevention and early intervention.
In this study, we used data from a general population sample of 6,551 adults, who were prospectively followed up in up to four waves from March (when COVID-19 became a serious health concern in Germany) until June 2020. We longitudinally examined the predictive role of mental disorders in spring 2020 for levels and changes of COVID-19-related fear, depressive, and anxiety symptoms during the following months. In addition, we tested for diagnostic specificity, examined the role of individual anxiety disorder diagnoses (agoraphobia, panic disorder, social anxiety disorder, generalized anxiety disorder, and other anxiety disorders according to DSM-5) and considered the role of additional diagnostic features (e.g., number of disorders and perceived worsening of existing anxiety disorders).
2. Method
2.1. Design
Our data comes from a general population sample with a total of 6,551 adults from Germany, which were assessed repeatedly at up to four waves using an online survey (SoSci-Survey) to examine the role of current mental disorders for the course of mental health problems during the first months of the COVID-19 pandemic (Bendau, Petzold et al., 2020; Petzold, Bendau, Plag, Pyrkosch, Mascarell Maricic, Betzler et al., 2020). The study was approved by the ethics committee of the Charité - Universitätsmedizin Berlin (EA1/071/20) and pre-registered at clinicaltrials.gov (NCT04331106). Participants were recruited via social media platforms (Twitter, Facebook, Instagram), news portals, and the homepage of the Charité - Universitätsmedizin Berlin. Only individuals who were 18 years or older, were currently living in Germany, and had sufficient language skills to complete the survey in German were included. All participants provided written informed consent before inclusion in the study.
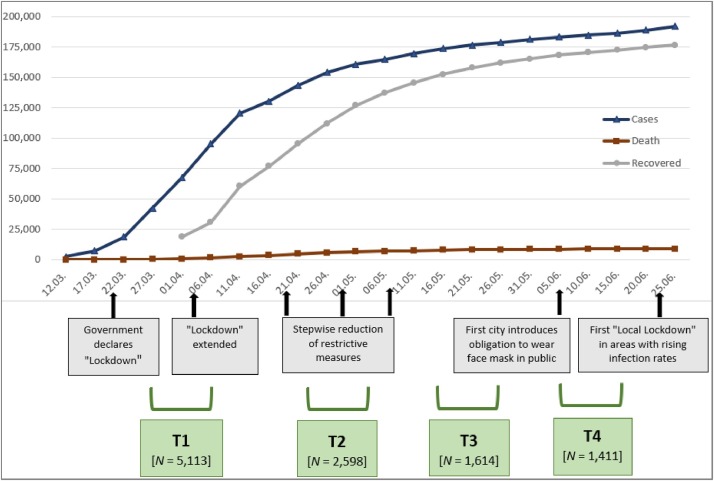
The first wave (T1) took place from March 27th to April 6th, the second wave (T2) from April 24th to May 4th, the third wave (T3) from May 15th to May 25th, and the fourth wave (T4) from June 5th to June 15th 2020. A total of 4,175 individuals participated in one, 1,070 in two, 803 in three, and 503 in all four waves of data collection. T1 was conducted at the time when COVID-19 became a serious health concern in Germany and several public health measures (e.g., “lockdown”, social distancing, etc.) were taken to prevent a further spread of the virus (see Fig. 1 ). In the following months, infection rates increased slower. At this time, some measures were removed, whereas others were introduced (e.g., wearing a mask in public places).
Fig. 1.
Development of the COVID-19 pandemic in Germany at the time when the four assessments took place, including information on specific public health measures that were taken at different time points (Bendau, Plag et al., 2020) and the number of participants (N) at each assessment. (p. 19).
2.2. Assessment of current mental disorders
The presence of a diagnosed anxiety disorder (“Are you currently suffering from a diagnosed anxiety disorder” – “if yes, which one(s)?” – selection fields with different anxiety disorders) and other diagnosed mental disorders (“Are you currently suffering from a diagnosed other mental disorder” – “if yes, which one(s)?” – free-text fields) in the present was queried at the first assessment. The free-text fields were transformed into ICD-10 F-codes and clustered into depressive disorders and other mental disorders (mostly adjustment disorders, personality disorders, and eating disorders). At baseline, participants were also asked whether they received professional help due to psychological problems (psychotherapy, pharmacotherapy, or other).
2.3. Assessment of COVID-19-related fear, depressive, and anxiety symptoms
At each wave, COVID-19-related fears were assessed with the COVID-19-Anxiety Questionnaire (C-19-A), a modified and validated version of the DSM-5 Severity-Measure-For-Specific-Phobia-Adult-Scale (Petzold, Bendau, Plag, Pyrkosch, Mascarell Maricic, Rogoll et al., 2020), which includes ten items, rated on a 5-point Likert scale from 0 (“never”) to 4 (“all the time”). Moreover, depressive and anxiety symptoms were assessed with the validated ultra-brief screening scale of the Patient Health Questionnaire-4 (PHQ-4) (Löwe et al., 2010). The PHQ-4 includes four items, rated on a 4-point Likert scale from 0 (“not at all”) to 3 (“nearly every day”). Two items refer to anxiety (GAD-2) and two items to depressive (PHQ-2) symptoms.
At each wave, individuals who had reported to currently suffer from an anxiety disorder when they entered the study were asked to indicate whether their anxiety symptoms had worsened due to the pandemic from the last until the current assessment (rated on a 6-point Likert scale from 1 (“not true at all”) to 6 (“totally true”)).
2.4. Data analysis
Stata 16 was used for the analyses. We applied multilevel analyses with measurement occasions (Level 1) nested within persons (Level 2). We built separate models per symptom scale (C-19-A, PHQ-4, PHQ-2, and GAD-2) and modeled the effects as fixed effects. The alpha level was set at .05. Because our multilevel approach enables to deal with missing data at individual waves our models refer to all participants who did or did not take part in all four waves.
First, we regressed the respective standardized symptom score as outcome (C-19-A, PHQ-4, PHQ-2, or GAD-2) on gender (Level 2; female, male, diverse), age (Level 2; in years), any other mental disorder (Level 2; yes vs. no), any depressive disorder (Level 2; yes vs. no), any anxiety disorder (Level 2; yes vs. no), and a symptom change variable (Level 1) as multiple predictors. The symptom change variable was coded with 0 at T1, with 1 at T2, with 1.75 at T3, and with 2.5 at T3 to represent how the four waves were temporally related to each other (in months; T2 was conducted about 1 month after T1, T3 about 1.75 months after T1, and T4 about 2.5 months after T1). The variable was used to indicate symptom changes over time (from T1 to T4). Moreover, two interaction terms were included (symptom change * any depressive disorder and symptom change * any anxiety disorder) to investigate whether symptom changes differed between individuals with and without any depressive or any anxiety disorder, respectively.
To test for diagnostic specificity, we repeated our first set of analyses. However, instead of any depressive and any anxiety disorder (and their interactions with the symptom change variable), we added a categorical variable (Level 2) with the following mutually exclusive groups as predictor: (1) no anxiety and no depressive disorder (no DA), (2) depressive but no anxiety disorder (pure D), (3) anxiety but no depressive disorder (pure A), and (4) comorbid depressive and anxiety disorder (comorbid DA). We also included an interaction term of this new variable with the symptom change variable. We repeated this regression three times, using category 1, 2, or 3 of this categorical variable as reference category.
To examine the role of individual diagnoses of anxiety disorders, we repeated our first set of analyses, but instead of any anxiety disorder (and its interaction with the symptom change variable), we added individual diagnoses of anxiety disorders as predictors (Level 2; agoraphobia, panic disorder, social anxiety disorder, generalized anxiety disorder, and other anxiety disorder; yes vs. no, respectively). We also included interaction terms of these new variables with the symptom change variable. Furthermore, we repeated these analyses and used the information on whether anxiety symptoms had subjectively worsened due to the pandemic as outcome (unstandardized score). Because only individuals with a self-reported anxiety disorder were asked this question and some of these individuals did not provide respective information, these analyses were only conducted in a subsample.
Finally and to examine the role of a higher number of baseline diagnoses of anxiety disorders, we repeated our first set of analyses and included an additional predictor, which coded the number of anxiety disorders (Level 2). An interaction term of this new variable with the symptom change variable was included as well.
3. Results
3.1. Sample characteristics
Sample characteristics for the total sample and by different mental disorders are shown in Tables 1 and S1 (in the Supplement). The total sample (N = 6,551) included 4,662 (71.2 %) women and 1,846 (28.2 %) men. The mean age was 36.94 years (SD = 11.70 years). 953 individuals (14.5 %) reported a secondary education or lower, 1,904 (29.1 %) a higher education entrance qualification, and 3,404 (52.0 %) a university degree. 1,045 participants (16.0 %) currently worked in a medical context. 650 individuals (9.9 %) suffered from a severe physical illness.
Table 1.
Basic sociodemographic characteristics (age and gender) of the total sample and separated for the different disorder types.
| N | Age: M (SD) | Gender: N (%) | Therapy: N (%) | |
|---|---|---|---|---|
| Total | 6,551 | 36.94 (11.70) | f = 4,663 (71.2) | |
| m = 1,846 (28.2) | ||||
| d = 43 (0.7) | ||||
| Depressive disorder | 656 | 34.13 (11.15) | f = 521 (79.4) | Therapy: 432 (65.9) |
| m = 116 (17.7) | ||||
| d = 19 (2.9) | ||||
| Other mental disorders | 386 | 32.61 (10.72) | f = 325 (84.2) | Therapy: 280 (72.5) |
| m = 53 (13.7) | ||||
| d = 8 (2.1) | ||||
| Anxiety disorder | 893 | 34.58 (10.72) | f = 696 (77.9) | Therapy: 453 (50.7) |
| m = 183 (20.5) | Psychotherapy: 375 (42.0) | |||
| d = 14 (1.6) | Pharmacotherapy: 247 (27.7) | |||
| Agoraphobia | 75 | 33.60 (9.29) | f = 57 (76.0) | Therapy: 34 (45.3) |
| m = 17 (22.7) | Psychotherapy: 25 (33.3) | |||
| d = 1 (1.3) | Pharmacotherapy: 18 (24.0) | |||
| Panic disorder | 351 | 35.83 (11.08) | f = 282 (80,3) | Therapy: 188 (59.7) |
| m = 68 (19.4) | Psychotherapy: 147 (41.9) | |||
| d = 1 (0.3) | Pharmacotherapy: 113 (32.2) | |||
| Social anxiety disorder | 307 | 31.23 (9.60) | f = 227 (73.9) | Therapy: 160 (52.1) |
| m = 70 (22.8) | Psychotherapy: 141 (45.9) | |||
| d = 10 (3.3) | Pharmacotherapy: 87 (28.3) | |||
| Generalized anxiety disorder | 424 | 35.89 (11.11) | f = 338 (79.7) | Therapy: 250 (59.0) |
| m = 77 (18.2) | Psychotherapy: 205 (48.3) | |||
| d = 9 (2.1) | Pharmacotherapy: 137 (32.2) | |||
| Any other anxiety disorder | 132 | 34.83 (10.78) | f = 100 (75.8) | Therapy: 38 (28.8) |
| m = 29 (22.0) | Psychotherapy: 35 (26.5) | |||
| d = 3 (2.3) | Pharmacotherapy: 13 (9.8) |
Note. f = female, m = male, d = diverse (participants with diverse gender expressions and/or identities that are not exclusively masculine or feminine).
615 individuals (9.4 %) of the total sample reported a pure anxiety disorder, 378 (5.8 %) a pure depressive disorder, and 278 (4.2 %) both an anxiety and a depressive disorder. 5,299 participants (79.8 %) reported neither an anxiety nor a depressive disorder.
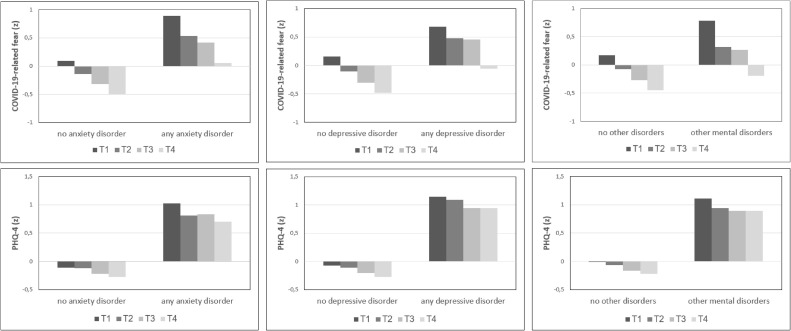
3.2. Anxiety, depressive, and other mental disorders
As shown in Table 1, men experienced lower COVID-19-related fear, depressive, and anxiety symptoms compared to women. Moreover, older individuals experienced higher COVID-19-related fears, but lower depressive and anxiety symptoms compared to younger individuals. Averaged across waves, all symptoms were higher in individuals with (vs. without) any other, depressive, or anxiety disorder. Moreover, all symptoms decreased over time, and this decrease was higher in individuals with (vs. without) any anxiety disorder, but did not vary by depressive disorders (Fig. 2 ).
Fig. 2.
Symptom changes in COVID-19-related fear (C-19-A), anxiety, and depressive symptoms (PHQ-4) from T1 until T4 for different disorder groups (any anxiety, depressive, and other mental disorder).
3.3. Diagnostic specificity
To detangle the role of current anxiety and depressive disorders, we further compared the observed symptom levels and changes between individuals with no DA, pure D, pure A, and comorbid DA (Table S2).
-
(1)
All symptoms were higher in individuals with pure D, pure A, or comorbid DA vs. no DA. Moreover, all symptoms more strongly decreased in individuals with pure A vs. no DA. However, individuals with pure D and comorbid DA did not differ from those with no DA with respect to their symptom changes. The only exception was that depressive symptoms decreased more strongly in individuals with pure D vs. no DA.
-
(2)
All observed symptoms were higher in individuals with pure A and comorbid DA vs. pure D. The only exception was that the total score of depression and anxiety symptoms (PHQ-4) and depressive symptoms (PHQ-2) were lower in individuals with pure A vs. pure D. Furthermore, all symptoms more strongly decreased in individuals with pure A vs. pure D. However, symptom changes did not differ between individuals with comorbid DA and pure D.
-
(3)
All symptoms were higher in individuals with comorbid DA vs. pure A. However, symptoms less strongly decreased in individuals with comorbid DA vs. pure A.
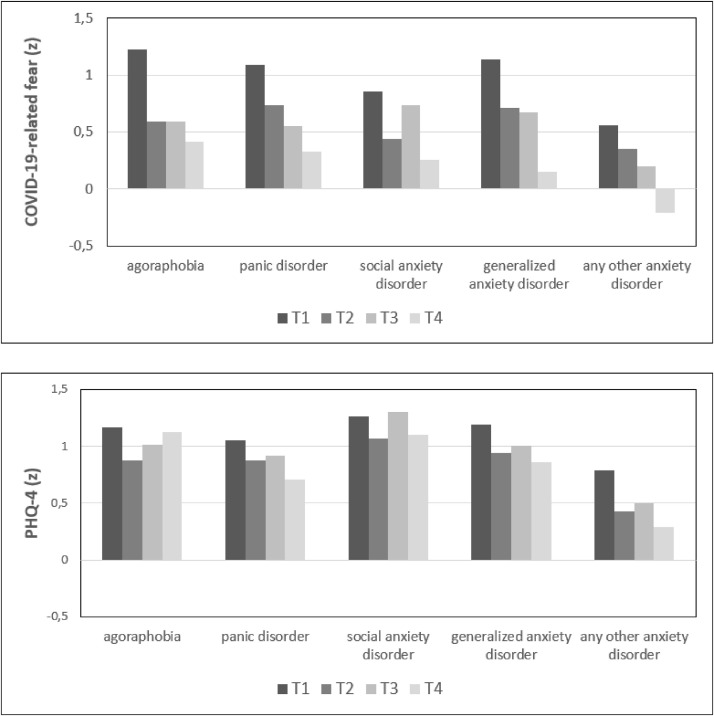
3.4. The role of individual anxiety disorder diagnoses
Investigating the role of individual diagnoses of anxiety disorders revealed the following results (Table 2 ): All observed symptoms were higher in individuals with each of the assessed anxiety disorders. The only exceptions were that agoraphobia was only associated with higher COVID-19-related fears (but not with depressive and anxiety symptoms) and other anxiety disorders were only associated with higher depressive and anxiety symptoms (but not with COVID-19-related fears).
Table 2.
Associations of current mental disorders with levels and changes of COVID-19-related fear, depressive, and anxiety symptoms over time.
| COVID-19- related fear (C-19-A) | Depressive and anxiety symptoms (PHQ-4) | Depressive symptoms (PHQ-2) | Anxiety symptoms (GAD-2) | |
|---|---|---|---|---|
| Number of observations | 10,667 | 10,624 | 10,624 | 10,625 |
| Coefficient | b (SE) | b (SE) | b (SE) | b (SE) |
| Gender | ||||
| Male vs. female | −0.161** (0.025) | −0.138** (0.023) | −0.053* (0.024) | −0.200**(0.023) |
| Diverse vs. female | −0.142 (0.140) | −0.002 (0.128) | 0.057 (0.131) | −0.069 (0.129) |
| Diverse vs. male | 0.020 (0.142) | 0.136 (0.130) | 0.110 (0.132) | 0.130 (0.130) |
| Age | 0.005** (0.001) | −0.007** (0.001) | −0.009** (0.001) | −0.003** (0.001) |
| Other mental disorder | 0.216** (0.050) | 0.524** (0.045) | 0.445** (0.046) | 0.524** (0.045) |
| Depressive disorder | 0.279**(0.042) | 0.813** (0.039) | 0.865** (0.040) | 0.640** (0.039) |
| Anxiety disorder | 0.687**(0.036) | 0.794** (0.034) | 0.598** (0.035) | 0.866** (0.034) |
| Symptom change | −0.256**(0.007) | −0.073** (0.008) | −0.036** (0.008) | −0.095** (0.008) |
| Symptom change * depressive disorder | 0.015 (0.022) | 0.010 (0.023) | −0.020 (0.025) | 0.042 (0.024) |
| Symptom change * anxiety disorder | −0.104** (0.020) | −0.084** (0.021) | −0.067** (0.023) | −0.088** (0.022) |
Note. b = coefficient from multilevel mixed-effect models. Standard errors are in parenthesis. Significance levels: ** p < 0.01, * p < 0.05.
Furthermore, individuals with (vs. without) a generalized anxiety disorder experienced a higher decrease of COVID-19-related fear, depressive, and anxiety symptoms over time (C-19-A, PHQ-4, and GAD-2) (Table 2 and Fig. 3 ). Individuals with (vs. without) any other anxiety disorder (rest category) experienced a higher decrease of depressive and anxiety symptoms over time (PHQ-4 and PHQ-2). However, symptom changes did not differ between individuals with and without agoraphobia, panic disorder, or social anxiety disorder.
Fig. 3.
Symptom changes in COVID-19-related fear (C-19-A), anxiety, and depressive symptoms (PHQ-4) from T1 until T4 for different anxiety disorders.
Moreover, supplemental analyses revealed that a higher number of comorbid anxiety disorders was associated with higher overall levels but also a higher decrease of COVID-19-related fear, depressive, and anxiety symptoms over time (Table S3).
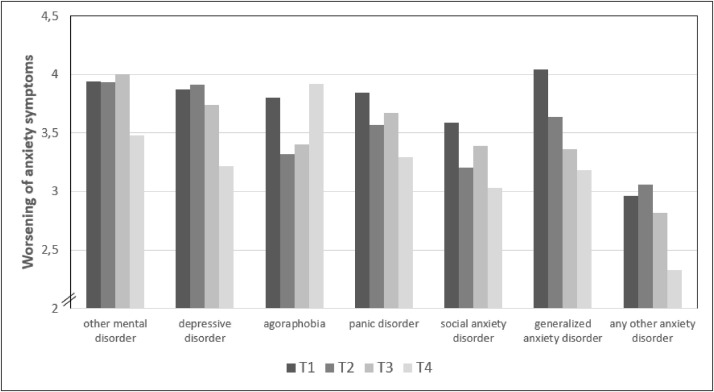
As displayed in Table 3 and Fig. 4 , the course of subject’s perceived worsening of symptoms differed with respect to the different anxiety disorders. Participants with generalized anxiety disorder demonstrated the most distinctive pattern in this context. Across all waves, those individuals perceived on average that their symptoms had worsened most strongly (from the last until the current wave), followed by participants with panic disorder (Table 3). At the same time, this perception attenuated clearly over time in individuals with generalized anxiety disorder, whereas the course of the perceived worsening of anxiety symptoms showed mixed trends in the other anxiety disorder groups (Fig. 4).
Table 3.
Associations of individual diagnoses of anxiety disorders with levels and changes of COVID-19-related fear, anxiety, and depressive symptoms over time as well as subjectively perceived worsening of anxiety symptoms over time (in individuals with anxiety disorders only; last column).
| COVID-19- related fear (C-19-A) | Depressive and anxiety symptoms (PHQ-4) | Depressive symptoms (PHQ-2) | Anxiety symptoms (GAD-2) | Worsening of symptoms | |
|---|---|---|---|---|---|
| n Observations | 10,667 | 10,624 | 10,624 | 10,625 | 1,469 |
| Coefficient | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) |
| Gender | |||||
| Male vs. female | −0.160** (0.025) | −0.140** (0.023) | −0.057* (0.024) | −0.200** (0.023) | −0.009 (0.139) |
| Diverse vs. fem. | −0.141 (0.140) | −0.036 (0.129) | 0.019 (0.132) | −0.094 (0.129) | −0.235 (0.446) |
| Diverse vs. male | 0.019 (0.141) | 0.104 (0.130) | 0.076 (0.133) | 0.106 (0.130) | −0.226 (0.461) |
| Age | 0.005** (0.001) | −0.007** (0.001) | −0.009** (0.001) | −0.004** (0.001) | −0.001 (0.005) |
| Other mental disorder | 0.199** (0.050) | 0.507** (0.046) | 0.433** (0.046) | 0.506** (0.046) | 0.397** (0.141) |
| Depressive disorder | 0.290** (0.040) | 0.815** (0.037) | 0.846** (0.038) | 0.662** (0.037) | 0.385** (0.124) |
| Agoraphobia | 0.325** (0.115) | 0.078 (0.107) | 0.044 (0.111) | 0.100 (0.108) | 0.055 (0.215) |
| Panic disorder | 0.527** (0.057) | 0.460** (0.053) | 0.307** (0.055) | 0.541** (0.054) | 0.485** (0.131) |
| Social anxiety disorder | 0.224** (0.059) | 0.498** (0.055) | 0.495** (0.057) | 0.428** (0.055) | 0.120 (0.145) |
| Generalized anxiety disorder | 0.627** (0.052) | 0.614** (0.049) | 0.376** (0.050) | 0.753** (0.049) | 0.853** (0.133) |
| Other anxiety disorders | 0.143 (0.084) | 0.342** (0.078) | 0.343** (0.080) | 0.291** (0.079) | −0.214 (0.185) |
| Symptom change | −0.257** (0.007) | −0.075** (0.008) | −0.041** (0.008) | −0.095** (0.008) | −0.235* (0.104) |
| Symptom change * Agoraphobia | −0.076 (0.073) | 0.085 (0.076) | 0.084 (0.083) | 0.054 (0.080) | 0.059 (0.168) |
| Symptom change * Panic disorder | −0.023 (0.033) | −0.017 (0.035) | −0.025 (0.038) | −0.008 (0.037) | 0.110 (0.092) |
| Symptom change * Social anxiety disorder | −0.009 (0.032) | −0.007 (0.034) | −0.023 (0.037) | 0.012 (0.036) | −0.028 (0.097) |
| Symptom change * Generalized anxiety disorder | −0.116** (0.028) | −0.079** (0.029) | −0.047 (0.032) | −0.093** (0.031) | −0.202* (0.095) |
| Symptom change * other anxiety disorder | −0.037 (0.041) | −0.097* (0.044) | −0.099* (0.047) | −0.088 (0.046) | 0.001 (0.120) |
Note. b = coefficient from multilevel mixed-effect models (the values of the variable worsening were computed in a separate model with only the participants which stated to have a anxiety disorders, because only those answered the item). Standard errors are in parenthesis. Significance levels: ** p < 0.01, * p < 0.05.
Fig. 4.
Perceived worsening of anxiety symptoms (rated on a 6-point Likert scale from 1 (not at all) to 6 (totally)) at the four waves (T1-T4) separated for different disorder types.
4. Discussion
4.1. Summary and interpretation of the results
This longitudinal study investigated the role of depressive, anxiety, and other mental disorders for differences in levels and changes of COVID-19-related fear, depressive, and anxiety symptoms during the first months of the COVID-19 pandemic among adults from Germany. We found that COVID-19-related fear, depressive, and anxiety symptoms were on average higher in individuals with (vs. without) depressive, anxiety or other mental disorders, which is consistent with previous studies (Asmundson et al., 2020; Hao et al., 2020). Possibly, individuals with current psychiatric disorders experienced higher psychological distress as compared to healthy individuals during the initial phase of the COVID-19 pandemic (e.g., due to a higher vulnerability to worrying about the news and less effective coping strategies (Bendau, Petzold et al., 2020; Hao et al., 2020)). Furthermore, patients with current mental disorders might have had more difficulties (e.g., due to public health measures such as physical distancing) to attend appointments with their treating clinician or to get other support from the health care system, resulting in a further escalation of psychopathological symptoms.
More specifically, comparing anxiety and depressive disorders revealed that individuals with anxiety disorders experienced higher COVID-19-related fear and anxiety symptoms, whereas individuals with depressive disorders experienced higher depressive symptoms. We further found that all symptoms decreased in the total sample over time. These results are in line with findings on symptom changes during previous epidemics (Chong et al., 2004) and after community disasters (Bonanno et al., 2010) and might be explained by the possibility that most people became used to and managed to cope with the challenging new situation over time.
However, importantly, all types of symptoms more strongly decreased in individuals with anxiety vs. depressive disorders. These findings partially contradict our assumptions that especially individuals with depressive and anxiety disorders should experience more unfavorable symptom changes (i.e., a lower symptom reduction) over time. One might speculate whether our findings were partially due to ceiling effects: Individuals with current anxiety disorders experienced more severe COVID-19-related threat and anxiety symptoms during the initial phase of the pandemic and thus had more room to improve over time. These particularly high levels of initial fear and anxiety among individuals with anxiety disorders might be explained by an elevated tendency to overestimate threat – a transdiagnostic marker of anxiety disorders (Abramowitz & Blakey, 2020). After the initial phase of the pandemic, a range of public health measures and governmental rules were removed or loosened in Germany. These changes might have signaled normality and safety especially to individuals with anxiety disorders and enabled them to continue specific treatment measures (e.g., psychotherapy sessions in person), leading to a further symptom improvement.
Investigating the role of individual diagnoses of anxiety disorders revealed that the symptom decrease over time among individuals with anxiety disorders was primarily driven by individuals with generalized anxiety disorder. This finding is consistent with the core symptomatology of generalized anxiety disorder: The presence of excessive anxiety and worry about various topics, events, or activities, which is difficult to control and may easily shift to other topics (American Psychiatric Association, 2013). Especially at the beginning of the COVID-19 pandemic, the knowledge about COVID-19 was low, the further course of the pandemic unsecure, and the presence of the topic in the media very high, which might have promoted an escalation of fears and anxieties especially among individuals with generalized anxiety disorder at the beginning of the COVID-19 pandemic. However, at the same time, it has to be noted that anxiety symptoms in this study were assessed with the PHQ4, which particularly focuses on generalized anxiety.
4.2. Strengths and limitations
Our study has several advantages: We prospectively followed up a large general population sample of adults in multiple waves during the first months of the COVID-19 pandemic in Germany. COVID-19-related fear, depressive, and anxiety symptoms were repeatedly assessed with well-established scales. Moreover, participants were initially asked about their current mental health status, which allowed us modeling the predictive role of pre-existing depressive and anxiety disorders for subsequent symptom changes during the COVID-19 pandemic.
However, our study is not without limitations. First, our sample was collected via convenience sampling methods and may not be fully representative of the general population in Germany. For example, a relatively large proportion was young and female, which might limit the generalizability of our results (e.g., to men and older individuals).
Second, current mental disorders were collected by single self-report items, but no structured or standardized clinical diagnostic interview was used to validate the diagnoses according to DSM or ICD criteria. Furthermore, information about the onset, duration, and severity of individual symptoms and disorders was not recorded and we ascertained whether the participants were in therapy (psychotherapy, pharmacotherapy, other) only at baseline but not at the follow-ups. Additional studies are necessary to assess the role of these and other clinical characteristics in greater detail.
Third, depressive and anxiety symptoms were assessed with the PHQ-4, a brief screening instrument, which primarily focuses on symptoms of generalized anxiety. Additional studies with more comprehensive assessments appear thus useful to focus on more nuanced changes with respect to other anxiety (e.g., social and phobic anxiety) and additional symptoms (e.g., externalizing psychopathology). Furthermore, the item which assessed the perceived worsening of anxiety symptoms might have been subject to recall biases and not reflected exactly changes in symptom severity.
Fourth, the C-19-A is an adapted phobia questionnaire and might not reflect all possible symptoms of COVID-19-related fear (e.g., symptoms commonly observed in illness anxiety such as checking oneself for symptoms, seeking reassurance, and seeking medical attention or advice). However, preliminary research suggests that the C-19-A has good psychometric properties, for example, in terms of internal consistency (α = 0.86) and convergent validity (Petzold, Bendau, Plag, Pyrkosch, Mascarell Maricic, Rogoll et al., 2020).
Fifth, the sample size at the first assessment period was considerably higher than the sample sizes at the follow ups and 4,175 participants of the total sample (N = 6551) took only part in one assessment. This drop-out might reduce the generalizability and comparability of the results. Nevertheless, our survey provides remarkable sample sizes with 2,376 individuals that participated repeatedly in two or more measurement periods
4.3. Conclusions
Our findings suggest that individuals with depressive disorders, other mental disorders and, in particular, anxiety disorders experienced severe COVID-19-related fears and anxieties during the first months of the COVID-19 pandemic in Germany, which improved over time. More specifically, these symptom changes were particularly driven by individuals with generalized anxiety disorder. Individuals with anxiety disorders – particularly generalized anxiety disorder – might have tended to overestimate the potential threat due to the COVID-19 panic at its early stage, when several issues concerning the virus were unclear and the situation seemed to be particularly unpredictable. This highlights the need for adequate health risk communication and information management during evolving crises such as the COVID-19 pandemic, especially toward vulnerable people, who might likely overestimate potential threat and thus experience severe mental health impairments. Future research may replicate our findings and investigate the role of anxiety, depressive and other mental disorders for the further course and outcome of psychopathology during and after the current pandemic.
Author contributions
Antonia Bendau: Literature research, conceptualization of the study, questionnaire construction, data collection, data preparation, data interpretation, writing.
Stefanie Kunas: Literature research, data preparation, data analysis, data interpretation, writing.
Sarah Wyka: Literature research, data interpretation, writing.
Moritz Bruno Petzold: Literature research, conceptualization of the study, questionnaire construction, data collection, critical review.
Jens Plag: Literature research, conceptualization of the study, ethics committee communication, questionnaire construction, data collection, critical review.
Eva Asselmann: Literature research, conceptualization of the methods, data preparation, data analysis, data interpretation, writing.
Andreas Ströhle: Primary conceptualization of the study, ethics committee communication, questionnaire construction, data interpretation, critical review
We would like to thank Lena Pyrkosch, Julia Große, Lea Mascarell Maricic, Janina Rogoll and Felix Betzler for their support in conceptualizing and realizing the project. Furthermore, many thanks to the Sonnenfeld-Stiftung for supporting our efforts.
Role of the funding source
This work was supported by the Sonnenfeld-Stiftung(grant for Antonia Bendau). The funding source had no involvement in the conceptualization and realization of the project or the manuscript.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Data availability
Data are available from the corresponding author on reasonable request.
Declaration of Competing Interest
The authors report no declarations of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.janxdis.2021.102377.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Abramowitz J.S., Blakey S.M. Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms. American Psychological Association; Washington, DC, US: 2020. Overestimation of threat; pp. 7–25. [DOI] [Google Scholar]
- American Psychiatric Association . 5th ed. 2013. Diagnostic and statistical manual of mental disorders. Washington, DC, US. [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Landry C.A., Rachor G.S., McKay D., Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselmann E., Wittchen H.‑U., Lieb R., Höfler M., Beesdo-Baum K. Associations of fearful spells and panic attacks with incident anxiety, depressive, and substance use disorders: A 10-year prospective-longitudinal community study of adolescents and young adults. Journal of Psychiatric Research. 2014;55:8–14. doi: 10.1016/j.jpsychires.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Asselmann E., Hertel J., Schmidt C.‑O., Homuth G., Nauck M., Beesdo-Baum K., Pané-Farré C.A. Interplay between RGS2 and childhood adversities in predicting anxiety and depressive disorders: Findings from a general population sample. Depression and Anxiety. 2018;35(11):1104–1113. doi: 10.1002/da.22812. [DOI] [PubMed] [Google Scholar]
- Asselmann E., Wittchen H.‑U., Lieb R., Beesdo-Baum K. Sociodemographic, clinical, and functional long-term outcomes in adolescents and young adults with mental disorders. Acta Psychiatrica Scandinavica. 2018;137(1):6–17. doi: 10.1111/acps.12792. [DOI] [PubMed] [Google Scholar]
- Bäuerle A., Teufel M., Musche V., Weismüller B., Kohler H., Hetkamp M.…Skoda E.‑M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. Journal of Public Health (Oxford, England) 2020 doi: 10.1093/pubmed/fdaa106. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K., Bittner A., Pine D.S., Stein M.B., Höfler M., Lieb R.…Wittchen H.‑U. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Archives of General Psychiatry. 2007;64(8):903. doi: 10.1001/archpsyc.64.8.903. [DOI] [PubMed] [Google Scholar]
- Beesdo K., Knappe S., Pine D.S. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K., Pine D.S., Lieb R., Wittchen H.‑U. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Archives of General Psychiatry. 2010;67(1):47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- Bendau A., Petzold M.B., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J.…Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. European Archives of Psychiatry and Clinical Neuroscience. 2020 doi: 10.1007/s00406-020-01171-6. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors in the COVID-19 pandemic in Germany. Brain and Behavior. 2020 doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Brewin C.R., Kaniasty K., La Greca A.M. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010 doi: 10.1177/1529100610387086. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Chong M.‑Y., Wang W.‑C., Hsieh W.‑C., Lee C.‑Y., Chiu N.‑M., Yeh W.‑C., Chen C.‑L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry. 2004;(185):127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Cooke J.E., Eirich R., Racine N., Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Research. 2020;292 doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske M.G., Rauch S.L., Ursano R., Prenoveau J., Pine D.S., Zinbarg R.E. What is an anxiety disorder? Depression and Anxiety. 2009;26(12):1066–1085. doi: 10.1002/da.20633. [DOI] [PubMed] [Google Scholar]
- Feng L.‑s., Dong Z.‑j., Yan R.‑y., Wu X.‑q., Li Zhang L., Ma J.…Zeng Y. Psychological distress in the shadow of the COVID-19 pandemic: Preliminary development of an assessment scale. Psychiatry Research. 2020;291 doi: 10.1016/j.psychres.2020.113202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.P., Krueger R.F., Andrews G., Hobbs M.J. Emotional disorders: Cluster 4 of the proposed meta-structure for DSM-V and ICD-11. Psychological Medicine. 2009;39(12):2043–2059. doi: 10.1017/S0033291709990298. [DOI] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J.M. The nosologic relationship between generalized anxiety disorder and major depression. Depression and Anxiety. 2008;25(4):300–316. doi: 10.1002/da.20491. [DOI] [PubMed] [Google Scholar]
- Ingram R.E., Luxton D.D. Development of psychopathology: A vulnerability-stress perspective. Sage Publications, Inc; Thousand Oaks, CA, US: 2005. Vulnerability-stress models; pp. 32–46. [DOI] [Google Scholar]
- Jacobi F., Michael Höfler M., Strehle J., Mack S., Gerschler A., Scholl L., Wittchen H.‑U. Twelve-months prevalence of mental disorders in the German Health Interview and Examination Survey for Adults - Mental Health Module (DEGS1-MH): a methodological addendum and correction. International Journal of Methods in Psychiatric Research. 2015;24(4):305–313. doi: 10.1002/mpr.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Petukhova M., Sampson N.A., Zaslavsky A.M., Wittchen H.‑U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K.…Brähler E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders. 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C.…Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health. 2020;17(9) doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris F.H., Friedman M.J., Watson P.J., Byrne C.M., Diaz E., Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;3(65):207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- North C.S. Rethinking disaster mental health response in a post-9/11 world. The Canadian Journal of Psychiatry. 2013;58(3):125–127. doi: 10.1177/070674371305800301. [DOI] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos De Saude Publica. 2020;36(4) doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F.…Ströhle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID‐19 pandemic in Germany. Brain and Behavior. 2020 doi: 10.1002/brb3.1745. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L.M., Rogoll J.…Ströhle A. Development of the COVID-19-Anxiety Questionnaire and first psychometric testing. BJPsych Open. 2020;6(5):e91. doi: 10.1192/bjo.2020.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear M.K., Bjelland I., Beesdo K., Gloster A.T., Wittchen H.‑U. Supplementary dimensional assessment in anxiety disorders. International Journal of Methods in Psychiatric Research. 2007;16(S1):S52–S64. doi: 10.1002/mpr.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley C.G., Greaves L.M., Satherley N., Wilson M.S., Overall N.C., Lee C.H.J., Barlow F.K. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. American Psychologist. 2020;75(5):618–630. doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., Sharma V.K. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Annals of Internal Medicine. 2020 doi: 10.7326/M20-1083. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Covid stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37(8):706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. U.S. Census Bureau‐assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID‐19 pandemic. Depression and Anxiety. 2020 doi: 10.1002/da.23077. da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S.…Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen H.‑U., Knappe S., Andersson G., Araya R., Banos Rivera R.M., Barkham M.…Schumann G. The need for a behavioural science focus in research on mental health and mental disorders. International Journal of Methods in Psychiatric Research. 2014;23(Suppl. 1):28–40. doi: 10.1002/mpr.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. American Psychological Association; Washington, DC, US: 1999. Vulnerability to psychopathology: A biosocial model. Vulnerability to psychopathology: A biosocial model. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available from the corresponding author on reasonable request.