Abstract
Background
Patients awaiting surgical procedures often experience significant anxiety. Such anxiety may result in negative physiological manifestations, slower wound healing, increased risk of infection, and may complicate the induction of anaesthesia and impede postoperative recovery. To reduce patient anxiety, sedatives and anti‐anxiety drugs are regularly administered before surgery. However, these often have negative side effects and may prolong patient recovery. Therefore, increasing attention is being paid to a variety of non‐pharmacological interventions for reduction of preoperative anxiety such as music therapy and music medicine interventions. Interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. A systematic review was needed to gauge the efficacy of both music therapy and music medicine interventions for reduction of preoperative anxiety.
Objectives
To examine the effects of music interventions with standard care versus standard care alone on preoperative anxiety in surgical patients.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 7), MEDLINE (1950 to August 2012), CINAHL (1980 to August 2012), AMED (1985 to April 2011; we no longer had access to AMED after this date), EMBASE (1980 to August 2012), PsycINFO (1967 to August 2012), LILACS (1982 to August 2012), Science Citation Index (1980 to August 2012), the specialist music therapy research database (March 1 2008; database is no longer functional), CAIRSS for Music (to August 2012), Proquest Digital Dissertations (1980 to August 2012), ClinicalTrials.gov (2000 to August 2012), Current Controlled Trials (1998 to August 2012), and the National Research Register (2000 to September 2007). We handsearched music therapy journals and reference lists, and contacted relevant experts to identify unpublished manuscripts. There was no language restriction.
Selection criteria
We included all randomized and quasi‐randomized trials that compared music interventions and standard care with standard care alone for reducing preoperative anxiety in surgical patients.
Data collection and analysis
Two review authors independently extracted the data and assessed the risk of bias. We contacted authors to obtain missing data where needed. Where possible, results were presented in meta analyses using mean differences and standardized mean differences. Post‐test scores were used. In cases of significant baseline differences, we used change scores.
Main results
We included 26 trials (2051 participants). All studies used listening to pre‐recorded music. The results suggested that music listening may have a beneficial effect on preoperative anxiety. Specifically, music listening resulted, on average, in an anxiety reduction that was 5.72 units greater (95% CI ‐7.27 to ‐4.17, P < 0.00001) than that in the standard care group as measured by the Stait‐Trait Anxiety Inventory (STAI‐S), and ‐0.60 standardized units (95% CI ‐0.90 to ‐0.31, P < 0.0001) on other anxiety scales. The results also suggested a small effect on heart rate and diastolic blood pressure, but no support was found for reductions in systolic blood pressure, respiratory rate, and skin temperature. Most trials were assessed to be at high risk of bias because of lack of blinding. Blinding of outcome assessors is often impossible in music therapy and music medicine studies that use subjective outcomes, unless in studies in which the music intervention is compared to another treatment intervention. Because of the high risk of bias, these results need to be interpreted with caution.
None of the studies included wound healing, infection rate, time to discharge, or patient satisfaction as outcome variables. One large study found that music listening was more effective than the sedative midazolam in reducing preoperative anxiety and equally effective in reducing physiological responses. No adverse effects were identified.
Authors' conclusions
This systematic review indicates that music listening may have a beneficial effect on preoperative anxiety. These findings are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. Therefore, we conclude that music interventions may provide a viable alternative to sedatives and anti‐anxiety drugs for reducing preoperative anxiety.
Plain language summary
Can music interventions replace sedatives for reduction of preoperative anxiety?
People awaiting surgical procedures often experience high levels of anxiety. Such anxiety may result in negative bodily responses, such as increased blood pressure and heart rate, leading to slower wound healing and increased risk of infection. High anxiety may also affect the start of anaesthesia and slow down postoperative recovery. To reduce patient anxiety, sedatives and anti‐anxiety drugs are regularly administered before surgery. However, these often have negative side effects, such as causing drowsiness and breathing difficulties, and may interact with anaesthetic drugs to prolong patient recovery and discharge. Therefore, increasing attention is being paid to music therapy and music medicine interventions, amongst other non‐pharmacological interventions, for reduction of preoperative anxiety. Interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. A systematic review was needed to gauge the efficacy of both music therapy and music medicine interventions for reduction of preoperative anxiety.
The review included 26 trials with a total of 2051 participants. The findings suggested that music listening may have a beneficial effect on preoperative anxiety. Most trials presented some methodological weakness. Therefore, these results need to be interpreted with caution. However, these findings are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. Therefore, we conclude that music interventions may provide a viable alternative to sedatives and anti‐anxiety drugs for reducing preoperative anxiety.
Summary of findings
Summary of findings for the main comparison. Music interventions versus standard care for preoperative anxiety.
| Patient or population: patients with preoperative anxiety Settings: In‐patient Intervention: Music Comparison: standard care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Music | |||||
| Preoperative anxiety (STAI) STAI. Scale from: 20 to 80. | The mean preoperative anxiety (stai) ranged across control groups from 37.63 to 44.43 points | The mean preoperative anxiety (stai) in the intervention groups was 5.72 lower (7.27 to 4.17 lower) | 896 (13 studies) | ⊕⊕⊝⊝ low1 | ||
| Preoperative anxiety (non‐STAI) VAS, NRS | The mean preoperative anxiety (non‐stai) in the intervention groups was 0.60 standard deviations lower (0.9 to 0.31 lower) | 504 (7 studies) | ⊕⊕⊝⊝ low1,2 | |||
| Heart rate | The mean heart rate ranged across control groups from 70.06 to 86.44 beats per minute | The mean heart rate in the intervention groups was 2.77 lower (4.76 to 0.78 lower) | 1109 (16 studies) | ⊕⊝⊝⊝ very low1,3,4 | ||
| Heart rate variability LF/HF ratio | The mean heart rate variability ranged across control groups from 1.77 to 2.6 LF/HF ratio | The mean heart rate variability in the intervention groups was 0.37 lower (1.16 lower to 0.42 higher) | 241 (2 studies) | ⊕⊝⊝⊝ very low1,4,5 | ||
| Systolic blood pressure | The mean systolic blood pressure ranged across control groups from 125.87 to 152 mm Hg | The mean systolic blood pressure in the intervention groups was 4.82 lower (12.13 lower to 2.49 higher) | 809 (14 studies) | ⊕⊝⊝⊝ very low1,4,6 | ||
| Diastolic blood pressure | The mean diastolic blood pressure ranged across control groups from 74.5 to 90 mm Hg | The mean diastolic blood pressure in the intervention groups was 2.37 lower (4.03 to 0.71 lower) | 786 (13 studies) | ⊕⊝⊝⊝ very low1,4,7 | ||
| Respiratory rate | The mean respiratory rate ranged across control groups from 16 to 23.2 breaths per minute | The mean respiratory rate in the intervention groups was 0.97 higher (0.82 to 1.11 higher) | 375 (6 studies) | ⊕⊝⊝⊝ very low1,8 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 The majority of the trials were assessed as high risk of bias studies 2 All point estimates favour music although the magnitude of the effect differs across studies. 3 Results were inconsistent across studies as evidenced by I² =79%. 4 Wide confidence interval 5 Results were inconsistent across studies as evidenced by I² =69%. 6 Results were inconsistent across studies as evidenced by I² =98%. 7 Results were inconsistent across studies as evidenced by I² =82%. 8 Results were inconsistent across studies as evidenced by I² =96%.
Background
Description of the condition
Patients awaiting surgical procedures often experience significant anxiety in anticipation of events that are uncomfortable, uncertain, and that may include a health risk. High levels of anxiety result in negative physiological manifestations, such as elevated blood cortisol levels, and increased blood pressure and heart rate, leading to slower wound healing, diminished immune response, and increased risk of infection (Scott 2004). High anxiety may also complicate presurgical drug administration, adversely affect the induction of anaesthesia, and impede postoperative recovery (Kain 2000; Kiecolt‐Glaser 1998; Maranets 1999; Ozalp 2003; Scott 2004). To reduce patient anxiety, sedatives or antianxiety drugs are regularly administered before surgery. However, sedatives often have negative side effects, such as drowsiness and respiratory depression, and may interact with anaesthetic agents prolonging patient recovery and discharge (Agarwal 2005). Therefore, increasing attention is being paid to a variety of non‐pharmacological interventions for reduction of preoperative anxiety (Agarwal 2005; Leroy 2003; Norred 2000; Wright 2007).
Description of the intervention
Music has been used in different medical fields to meet physiological, psychological, and spiritual needs of patients. Research on the effects of music and music therapy for medical patients has burgeoned during the past 20 years and has included a variety of outcome measures in a wide range of specialty areas (Dileo 2005). Specifically, the anxiolytic effects of music have been studied in a variety of medical patients, including surgical (Daub 1988Kaempf 1989Koch 1998Mok 2003), cardiac (Bolwerk 1990; Hamel 2001; White 1999), and oncology patients (Frank 1985; Pfaff 1989).
It is important to make a clear distinction between music interventions administered by medical or healthcare professionals (music medicine) and those implemented by trained music therapists (music therapy). A substantive set of data (Dileo 2005) indicates that music therapy interventions with medical populations are significantly more effective than music medicine interventions for a wide variety of outcomes. This difference might be attributed to the fact that music therapists individualize their interventions to meet patients' specific needs, more actively engage the patients in the music making, and employ a systematic therapeutic process that includes assessment, treatment, and evaluation. As defined by Dileo (Dileo 1999), interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. These music experiences include:
listening to live, improvised, or pre‐recorded music;
performing music on an instrument;
improvising music spontaneously using voice or instruments, or both;
composing music; and
music combined with other modalities (e.g., movement, imagery, art) (Dileo 2007).
How the intervention might work
A common theory regarding the anxiety‐reducing effects of music is that music can help patients focus their attention away from stressful events to something pleasant and soothing (Mitchell 2003; Nilsson 2008). Even though this is an important mechanism in preoperative anxiety reduction, it is important to emphasize that music does more than refocusing patients’ attention. It provides the patient with an aesthetic experience that can offer comfort and peace while awaiting surgery. In music interventions provided by a trained music therapist, the music therapist furthermore adapts the live music interactions to the in‐the‐moment needs of the patients. This often provides a deeply humanizing and validating experience for the patient. The act of making music together can provide a strong sense of support. Moreover, the active and creative engagement in music making (for example, singing songs, improvising music) stands in stark contrast to passively submitting oneself to surgical procedures. This may result in an increased sense of control and empowerment.
On a neurophysiological level, it has been postulated that music induces relaxation through its impact on automated and central nervous responses (Gillen 2008; Lai 2006). More specifically, it is believed that the anxiolytic effect of music is achieved through its suppressive action on the sympathetic nervous system, leading to decreased adrenergic activity and decreased neuromuscular arousal (Chlan 1998; Gillen 2008). Music furthermore triggers the limbic system in the brain to release endorphins; these neurotransmitters play an important role in enhancing a sense of well‐being (Arslan 2008; Lee 2005). However, Gillen (Gillen 2008) has suggested that more research is needed to examine the physiological mechanisms that explain the anxiolytic effects of music.
Why it is important to do this review
Most research studies examining the anxiety‐reducing effects of music in presurgical patients have used music listening as the primary intervention. Several of these studies have found that exposure to music reduces preoperative anxiety. Several studies, however, have suffered from small sample size, making it nearly impossible to achieve statistically significant results. In addition, a number of individual factors that are likely to influence responses to music, including age, gender, emotional state, music preference, personal associations with the music, prior musical training, and culture, are likely to influence the outcomes (Dileo 2005; Pelletier 2004; Standley 1986; Standley 2000). A systematic review was needed to more accurately gauge the efficacy of both music medicine and music therapy for reduction of preoperative anxiety as well as to identify variables that may moderate the effects.
Objectives
To identify randomized controlled trials examining the effects of music therapy or music medicine interventions (as defined by the authors) on preoperative anxiety in surgical patients.
To compare the efficacy of participation in standard care combined with music therapy or music medicine interventions with standard care alone.
To compare the efficacy of patient‐preferred music with researcher‐selected music.
To compare the efficacy of different types of music interventions (music therapy versus music medicine).
Methods
Criteria for considering studies for this review
Types of studies
We included all randomized controlled trials (RCT) and controlled clinical trials (CCTs) with quasi‐randomized or systematic methods of treatment allocation in any language, published and unpublished.
We conducted a sensitivity analysis to assess the impact of the randomization method.
Types of participants
This review included all surgical patients that were inpatients, outpatients, emergency, non‐emergency, undergoing major as well as minor surgical procedures. Dental surgical patients and patients undergoing non‐surgical procedures were excluded. This review did not include family members of the participants. There were no restrictions as to age, gender, or ethnicity.
Types of interventions
The review included all studies in which standard care combined with music therapy or music medicine interventions (as defined by the authors) delivered during the preoperative period was compared with standard treatment alone. Studies that included a combination of operative periods (for example, preoperative, perioperative, postoperative) were considered only if data on the effects of music on anxiety during the preoperative period were reported.
Types of outcome measures
Primary outcomes
The primary outcome for this review was preoperative anxiety. Measures of anxiety included the State Anxiety scale of the State‐Trait Anxiety Inventory (STAI‐S) (Spielberger 1983), visual analogue scales (VAS), numerical rating scales (NRS), and the Zung Self‐Rating Anxiety Scale. We only included scales with established reliability and validity (that is, as evidenced in at least one prior published study in a peer‐reviewed journal).
Secondary outcomes
The secondary outcomes for this review were:
preoperative sedative drug intake;
physiological outcomes (e.g., heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, skin temperature) using post‐intervention or change scores to compare the treatment and control groups;
physical outcomes (e.g., infection rate, wound healing);
patient satisfaction.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases and trial registers:
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 7);
MEDLINE (Ovid) (1950 to August 2012);
EMBASE (1980 to August 2012);
CINAHL (1982 to August 2012);
PsycINFO (1967 to August 2012);
LILACS (1982 to August 2012);
AMED (1985 to April 2011; we no longer had access to AMED after this date);
Science Citation Index (1980 to August 2012);
The specialist music therapy research database at www.musictherapyworld.net (database is no longer functional) (1 March 2008);
CAIRSS for Music (August 2012);
Proquest Digital Dissertations (1980 to August 2012);
ClinicalTrials.gov (http://www.clinicaltrials.gov/) (2000 to August 2012);
Current Controlled Trials (http://www.controlled‐trials.com/) (1998 to August 2012);
National Research Register (http://www.nihr.ac.uk/Pages/NRRArchive.aspx) (2000 to August 2012).
We used the search strategy found in Appendix 2 for MEDLINE (Ovid) and adapted it for the other databases.
Searching other resources
We handsearched the following journals from their first available date:
Australian Journal of Music Therapy (August 2012);
Canadian Journal of Music Therapy (August 2012);
The International Journal of the Arts in Medicine (December 2007, latest issue was published in 1999);
Journal of Music Therapy (August 2012);
Musik‐, Tanz‐, und Kunsttherapie (Journal for Art Therapies in Education, Welfare and Health Care)(August 2012);
Musiktherapeutische Umschau (online index available until 2010);
Music Therapy (February 2012; latest issue published 1996);
Music Therapy Perspectives (August 2012);
Nordic Journal of Music Therapy (August 2012);
Music Therapy Today (online journal of music therapy) (December 2007; latest issue published December 2007);
Voices (online international journal of music therapy) (August 2012);
New Zealand Journal of Music Therapy (online index available until 2009);
British Journal of Music Therapy (August 2012).
In an effort to identify further published, unpublished, and ongoing trials we searched the bibliographies of relevant studies and reviews, contacted experts in the field, and searched available proceedings of music therapy conferences.
We imposed no language restrictions for either searching or trial inclusion.
Data collection and analysis
Selection of studies
One author (JB) scanned the titles and abstracts of each record retrieved from the search. If information in the abstract clearly indicated that the trial did not meet the inclusion criteria, we rejected the trial. When a title or abstract could not be rejected with certainty, JB and MS independently obtained and inspected the full article. We used an inclusion criteria form to assess the trial's eligibility for inclusion. We resolved any disagreements by discussion. If a trial was excluded, we kept a record of both the article and the reason for its exclusion.
Data extraction and management
JB and MS independently extracted data from the selected trials using a standardized coding form. We discussed and were able to resolve any differences in data extraction. We extracted the following data.
General information
Author
Year of publication
Title
Journal (title, volume, pages)
If unpublished, source
Duplicate publications
Country
Language of publication
Intervention information
Type of intervention (e.g., singing, song‐writing, music listening, music improvisation)
Music selection (detailed information on music selection in case of music listening)
Music preference (patient‐preferred versus researcher‐selected in the case of music listening)
Level of intervention (music therapy versus music medicine as defined by the authors in the background section)
Length of intervention
Frequency of intervention
Comparison intervention
Participants information
Total sample size
Number in experimental group
Number in control group
Gender
Age
Ethnicity
Type of surgery
Setting
Inclusion criteria
Outcomes
Pre‐test means, post‐test means, standard deviations, and sample sizes were extracted for the treatment group and the control group for the following outcomes (if applicable). For some trials only change scores, instead of post‐test scores, were available.
Preoperative anxiety.
Preoperative sedative drug intake.
Physiological outcomes (e.g., heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, skin temperature).
Physical outcomes (e.g., infection rate, wound healing).
Patient satisfaction.
Assessment of risk of bias in included studies
JB and MS assessed all included trials for risk of bias and were blinded to each other's assessments. Any disagreements were resolved by discussion. The authors used the following criteria for quality assessment.
Random sequence generation
Low risk
Unclear risk
High risk
Random sequence generation was rated as low risk if every participant had an equal chance to be selected for either condition and if the investigator was unable to predict which treatment the participant would be assigned to. Use of date of birth, date of admission, or alternation resulted in high risk of bias.
Allocation concealment
Low risk methods to conceal allocation include:
central randomization;
serially numbered, opaque, sealed envelopes;
other descriptions with convincing concealment.
Unclear risk, authors did not adequately report on method of concealment.
High risk (e.g., alternation methods were used).
Blinding of participants and personnel
Low risk
Unclear risk
High risk
Since participants cannot be blinded in a music intervention trial, studies were not downgraded for not blinding the participants. As for personnel, in music therapy studies music therapists cannot be blinded because they are actively making music with the patients. In contrast, in music medicine studies blinding of personnel is possible by providing control group participants with headphones but no music (e.g., blank CD). Therefore, downgrading for not blinding personnel was only applied in studies that used listening to pre‐recorded music.
Blinding of outcome assessors
Low risk
Unclear risk
High risk
Incomplete outcome data
We recorded the proportion of participants whose outcomes were analysed. We coded losses to follow‐up for each outcome as:
low risk, if fewer than 20% of patients were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
unclear risk, if loss to follow‐up was not reported;
high risk, if more than 20% of patients were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms.
Selective reporting
Low risk, reports of the study were free of suggestion of selective outcome reporting
Unclear risk
High risk, reports of the study suggest selective outcome reporting
Other sources of bias
Low risk
Unclear risk
High risk
Information on potential financial conflicts of interest was considered as a possible source of additional bias.
The above criteria were used to give each article an overall quality rating, based on the Cochrane Handbook for Systematic Reviews of Interventions Section 8.7 (Higgins 2011). A. Low risk of bias: all criteria met. B. Moderate risk of bias: one or more of the criteria only partly met. C. High risk of bias: one or more criteria not met.
Studies were not excluded based on a low quality score. We planned to use the overall quality assessment rating for sensitivity analysis. However, since most trials were at high risk of bias, we could not carry out this analysis.
Measures of treatment effect
All outcomes in this review were presented as continuous variables. We calculated standardized mean differences with 95% confidence intervals (CI) for outcome measures using results from different scales. When there were sufficient data available from various studies using the same measurement instrument (for example, Spielberger's State Anxiety Inventory) we computed a mean difference (MD) with 95% CI.
Unit of analysis issues
In all studies included in this review, participants were individually randomized to the intervention or the standard care control group. Post‐test values or change values on a single measurement for each outcome from each participant were collected and analysed.
Dealing with missing data
We did not impute missing outcome data. We analysed data on an endpoint basis, including only participants for whom final data point measurements were obtained (available case analysis). It was not assumed that participants who dropped out after randomization had a negative outcome.
Assessment of heterogeneity
We investigated heterogeneity using visual inspection of the forest plots as well as the I2 statistic (Higgins 2002).
Assessment of reporting biases
Publication bias using preoperative anxiety as the outcome was examined visually in the form of a funnel plot (Figure 1). The funnel plot did not show evidence of publication bias.
1.
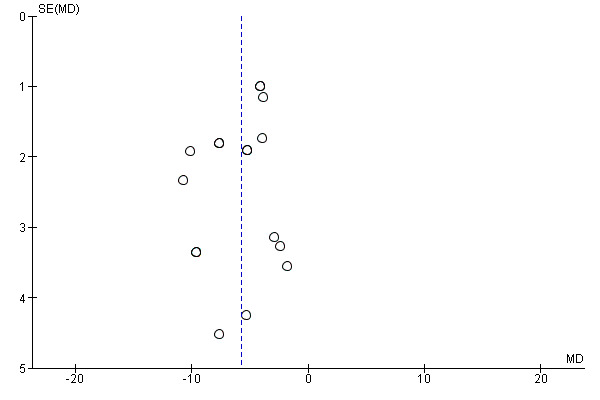
Funnel plot of comparison: 1 Music versus standard care, outcome: 1.1 State Anxiety STAI.
Data synthesis
We entered all trials included in the systematic review into Review Manager (RevMan 5.1). We anticipated that some individual studies would have used final scores whereas others might have used change scores. We combined these different types of analyses as mean difference (MD). We calculated pooled estimates using the more conservative random‐effects model. We determined the levels of heterogeneity by the I2 statistic (Higgins 2002).
The following treatment comparison was made: music interventions versus standard care alone.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were determined a priori, but these could not be carried out because of insufficient numbers of trials per subgroup:
a. music medicine with music therapy interventions; b. patient‐preferred music with researcher‐selected music; d. comparison of different types of music interventions (e.g., listening to music, active music making).
Sensitivity analysis
We examined the impact of sequence generation by comparing the results of including and excluding trials that used inadequate or unclear randomization methods.
Results
Description of studies
See Figure 2
2.
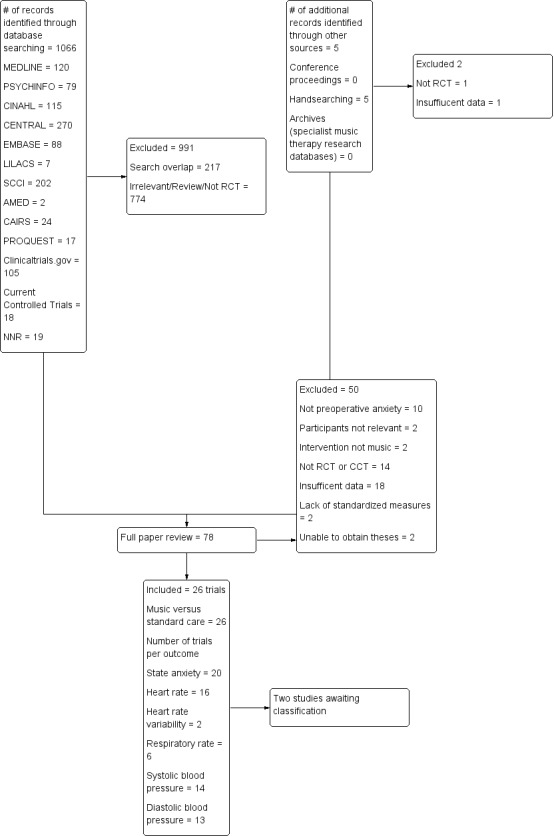
Excluded Study flow diagram.
Results of the search
The database searches and handsearching of conference proceedings, journals, and reference lists resulted in 1071 citations. Two authors (JB and MS) examined the titles and abstracts and identified 76 studies as potentially relevant, which were retrieved for further assessment. These were then independently screened by JB and MS.
We included 26 trials in this review (see Characteristics of included studies). Where necessary, we contacted the chief investigators to obtain additional information on study details and data.
Two studies (Berbel 2007; Dwita 2002) are awaiting classification. We were unable to obtain the study reports.
Included studies
We included 26 studies with a total of 2051 participants in this review. These studies examined the effects of music on preoperative anxiety in patients awaiting surgery. There was a balanced distribution of female (54%) and male (46%) participants in these studies. The mean age of participants was 48.74 years of age. Only five studies specified the ethnicity of the study participants (Augustin 1996; Hook 2008; Lee 2011; Yung 2002; Yung 2003). Nine studies were conducted in the USA (Allen 2001; Augustin 1996; Bringman 2009; Cassidy 2003; Cooke 2005; DeMarco 2012; Evans 1994; Gaberson 1995; Winter 1994); five in Taiwan (Chang 1996; Lee 2011; Lee 2012; Lin 2011; Ni 2011); three in Hong Kong (Szeto 1999; Yung 2002; Yung 2003); three in China (Guo 2005; Lee 2004; Li 2004); two in Poland (Miluk‐Kolasa 1996; Miluk‐Kolasa 2002); two in Turkey (Arslan 2008; Ganidagli 2005); one in Malaysia (Hook 2008); and one in Israel (Kushnir 2012). Trial sample size ranged from 9 to 327 participants with an average sample size of 78.9 (SD 64.36) participants.
The studies included many different types of surgery including general ambulatory (Augustin 1996), general (Bringman 2009; Cassidy 2003; Gaberson 1995; Hook 2008; Lee 2004; Lee 2011; Lee 2012; Miluk‐Kolasa 1996; Miluk‐Kolasa 2002; Ni 2011; Szeto 1999), endoscopic (Evans 1994), gynaecological or urogenital (Arslan 2008; Winter 1994; Yung 2002; Yung 2003), orthopaedic (Cooke 2005; Lin 2011), elective cosmetic (DeMarco 2012), elective caesarian (Kushnir 2012), cardiac (Chang 1996), ophthalmic (Allen 2001), septorhinoplastic (Ganidagli 2005), and gastric cancer (Li 2004).
Not all studies measured all outcomes identified for this review.
All included studies were categorized as music medicine studies (as defined by the review authors in the background section) and used listening to pre‐recorded music as the intervention. Some authors provided theoretical frameworks for the use of music to reduce anxiety including: (a) decreased adrenergic and sympathetic nervous system activity through entrainment of body rhythms with music (Arslan 2008; Lee 2004); (b) sedative music's capacity to reduce neuroendocrine activity (Lin 2011); (c) the influence of music listening on the limbic system of the brain by reducing the ability of neurotransmitters to relay uncomfortable feelings and by triggering the release of endorphins (Arslan 2008; Cooke 2005); (d) alteration of perceptual responses including the perception of time (Cooke 2005); and (e) music as a distracter, focusing the patient’s attention away from negative stimuli to something pleasant and encouraging (Lee 2011; Lee 2012). Robb and colleagues emphasize the need for researchers to specify a theoretical framework and "provide a rationale for the music selected and specify how qualities and delivery of the music are expected to impact targeted outcomes" (Robb 2011).
Most studies offered one 20 to 30‐minute music session to the participants during the preoperative waiting period. Two studies offered multiple music listening sessions, starting several days before surgery and continuing to the day of the surgery (Li 2004; Lin 2011).
Few studies provided detailed information about the music that was used (Bringman 2009; DeMarco 2012; Winter 1994). Most authors only reported the different styles of music that were offered to the participants (for example, jazz, easy listening, country and western, classical music) without any composition‐specific or performance‐specific information. Five studies indicated the tempo range of the music, namely between 60 to 80 beats per minute (bpm) (Chang 1996; Hook 2008; Lee 2011; Lee 2012; Lin 2011). The majority of the studies asked the participants to select their preferred music from a limited number of music offerings. In contrast, two studies used researcher‐selected music and did not take into account participant preference (DeMarco 2012; Li 2004). The decision to use patient‐selected music was based on the assumption that music preference plays an important part in the effectiveness of music relaxation. This assumption has been supported by a recent series of studies that found that music preference and familiarity with the music are positively correlated with the degree of relaxation obtained from listening to music (Tan 2012). It needs to be noted that, in the studies included in this review, participants could only select from a limited number of music styles presented by the researcher. It is likely that the preferred music of some of the participants was not included in the music selections offered and, even if it were, that they may not have liked the specific compositions or songs being played. In two studies, participants were asked to bring music of their own choice (Cassidy 2003; Ganidagli 2005).
Thirteen studies excluded patients who had received preoperative sedatives (Augustin 1996; Cooke 2005; DeMarco 2012; Evans 1994; Gaberson 1995; Lee 2004; Lee 2011; Lee 2012; Ni 2011; Szeto 1999; Winter 1994; Yung 2002; Yung 2003). In two studies, standard preoperative drugs, including midazolam hydrochloride and alfentanil hydrochloride, were administered to both the music intervention group and the standard care control group (Allen 2001; Ganidagli 2005). For a few studies, it was unclear whether participants received preoperative sedatives (Guo 2005; Hook 2008; Li 2004; Lin 2011). Five studies did not include any information on the use of preoperative drugs (Arslan 2008; Cassidy 2003; Kushnir 2012; Miluk‐Kolasa 1996; Miluk‐Kolasa 2002). Finally, one study compared a music intervention group who did not receive preoperative sedatives with a standard care control group who received midazolam (Bringman 2009). Because of the differences in preoperative drug administration between the two groups, this study could not be pooled with the other studies in this review. Instead, we included the results of this study in the narrative of this review.
One study's results (Miluk‐Kolasa 1996) could not be pooled with other studies because only percentage change scores were reported. These results are therefore presented in the narrative of the results section.
Details of the studies included in the review are shown in the table Characteristics of included studies.
Excluded studies
We excluded a total of 50 studies for the following reasons:
studies did not address preoperative anxiety; instead, the post‐test measurement of anxiety was administered after surgery (10 studies);
studies were not randomized controlled trials or controlled clinical trials (14 studies);
study participants did not meet the inclusion criteria (two studies);
insufficient data reporting (18 studies);
studies did not use standardized measures for anxiety (two studies);
studies did not use music (two studies); and
we were unable to obtain the studies (two studies).
The reasons for exclusion are listed in the table Characteristics of excluded studies.
Risk of bias in included studies
Allocation
We included 11 trials that used appropriate methods of randomization (for example, computer‐generated table of random numbers, a draw of lots, flip of coins), four trials that used alternate group assignment as the allocation method, four trials that used other forms of systematic allocation (for example, date of birth, day of surgery), and seven trials that reported using randomization but failed to state the randomization method.
Five trials used allocation concealment whereas eight trials did not. For the remainder of the trials, use of allocation concealment was not mentioned.
Blinding
In music intervention studies, participants cannot be blinded (unless they are in studies that compare different types of music interventions). Three studies reported blinding personnel. This was achieved by having both music group and control group participants wear headsets and listen to a CD. The control group listened to a blank CD. Twenty‐one studies did not blind personnel, and for two studies blinding of personnel was unclear.
Only seven trials reported blinding of the outcome assessors for objective measures. For 12 trials, the use of blinding was unclear. The other trials did not use blinding. However, it is important to point out that blinding of outcome assessors is not possible in the case of subjective measurement tools (for example, STAI (Spielberger 1983)) unless the participants are blinded to the intervention. We would like to point out that the assessment of risk of bias figure (Figure 3) lists three studies as having used blinding for subjective outcomes. However, these were studies that did not include subjective outcomes. A rating of low risk was assigned if studies did not include subjective outcomes.
3.
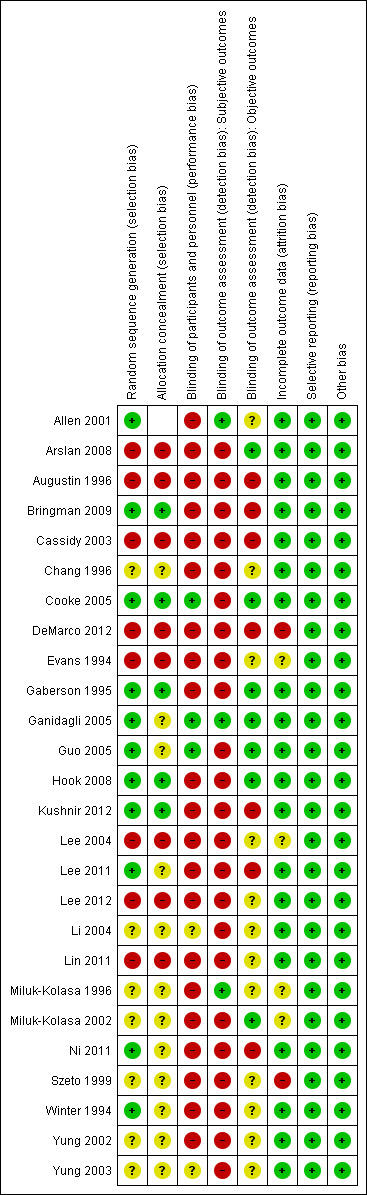
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Incomplete outcome data
The dropout rate was small for most trials, namely between 0% and 13%. Three trials reported dropout rates of more than 20%. For nine trials it was unclear whether there were any participant withdrawals. Most trials reported reasons for dropout. Detailed information on the dropout rate and reasons is included in the Characteristics of included studies table.
Selective reporting
We did not identify any issues related to selective reporting.
Other potential sources of bias
We did not identify any other potential sources of bias in the studies included in this review.
As a result of the risk of bias assessment, we concluded that two trials were at moderate risk of bias (Ganidagli 2005; Guo 2005). All other trials were at high risk of bias. The main reason for receiving a high risk of bias rating was the lack of blinding. As mentioned before, blinding is often impossible in music therapy and music medicine studies that use subjective outcomes, unless in studies where the music intervention is compared to another treatment intervention (for example, progressive muscle relaxation or different type of music intervention). Therefore, it appears impossible for these types of studies to receive a low or moderate risk of bias even if all other risk factors (for example, randomization, allocation concealment, etc.) have been adequately addressed.
It is worth noting that the Chinese trials were particularly problematic in terms of providing sufficient information regarding risk of bias. It is unclear, however, if this was due to incomplete translations or lack of detail in the original trial reports.
Risk of bias is detailed for each trial in the risk of bias tables included with the Characteristics of included studies table and the 'Risk of bias' summary (Figure 4). In addition, an overall assessment of risk of bias can be viewed in Figure 3.
4.
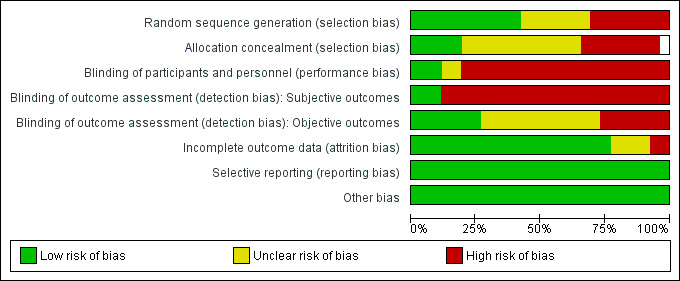
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
See: Table 1
Primary outcome
Preoperative anxiety
Twenty trials (N = 1400) examined the effects of music interventions on preoperative anxiety. Thirteen trials measured anxiety by means of the Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety scale (STAI‐S) (Allen 2001; Augustin 1996; Cassidy 2003; Cooke 2005; DeMarco 2012; Guo 2005; Lee 2004; Miluk‐Kolasa 2002; Ni 2011; Szeto 1999; Winter 1994; Yung 2002; Yung 2003). The STAI‐S is a validated and widely used instrument to measure patients' anxiety. It consists of 20 statements aimed at determining a patient's current anxiety level. The total score for STAI‐S ranges from 20 to 80. Seven trials reported mean anxiety measured by other scales such as a numeric rating scale and a visual analogue scale (Chang 1996; Gaberson 1995; Ganidagli 2005; Lee 2011; Lee 2012; Li 2004; Lin 2011). The data of one trial (Bringman 2009) could not be included in the meta‐analysis because, unlike the other studies, midazolam was withheld from participants in the music group but not from the control group. The results of this study are reported separately below.
A meta‐analysis of 13 trials that used the STAI‐S to examine state anxiety in 896 participants indicated significantly lower state anxiety in participants who received standard care combined with music interventions than those who received standard care alone (MD ‐5.72, 95% CI ‐7.27 to ‐4.17, P < 0.00001). The results were consistent across trials (I² = 43%) (Analysis 1.1). In the trial by Bringman (N = 327), participants in the non‐midazolam music listening group reported lower levels of anxiety at post‐test (mean 30, standard deviation (SD) 7.0) than those in the standard care midazolam group (mean 34, SD 7.0) and this difference was statistically significant (P < 0.001). A sensitivity analysis, removing those trials that used inadequate methods of randomization (Arslan 2008; Augustin 1996; Cassidy 2003; DeMarco 2012; Lee 2004) or for which the method of randomization was unclear (Miluk‐Kolasa 2002; Szeto 1999; Yung 2002; Yung 2003), resulted in similar findings (MD ‐5.76, 95% CI ‐7.94 to ‐3.57, P <.00001; I² = 38%) (Analysis 1.1).
1.1. Analysis.
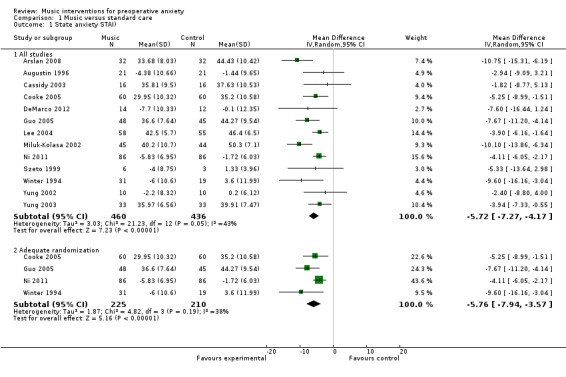
Comparison 1 Music versus standard care, Outcome 1 State anxiety STAI).
The standardized mean difference (SMD) of those trials that reported post‐test anxiety scores on measures different than the STAI‐S (N = 504) also suggested a moderate anxiety‐reducing effect of music (SMD ‐0.60, 95% CI ‐0.90 to ‐0.31, P < 0.0001) (Analysis 1.2). Statistical heterogeneity across the trials (I² = 61%) was due to some trials (Chang 1996; Li 2004; Lin 2011) reporting much larger beneficial effects of music interventions than others. A sensitivity analysis to examine the impact of randomization method, excluding the data of four trials (Chang 1996; Lee 2012; Li 2004; Lin 2011), resulted in a smaller SMD of ‐0.41 (95% CI ‐0.71 to ‐0.12, P = 0.006), but improved the homogeneity of the results (I² = 0%) (Analysis 1.2).
1.2. Analysis.
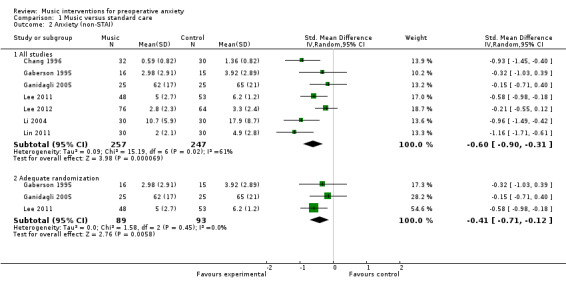
Comparison 1 Music versus standard care, Outcome 2 Anxiety (non‐STAI).
Secondary outcomes
Preoperative sedative drug intake
None of the studies in this review included preoperative sedative drug intake as an outcome variable. Instead, for most studies sedative drug intake was an exclusion criterion: patients who had received preoperative sedative drugs could not participate in the studies. One study (Bringman 2009) compared a non‐midazolam music listening group directly with a midazolam group and found that music listening was more effective than midazolam for preoperative anxiety reduction (see preoperative anxiety section).
Physiological responses
Heart rate (HR)
The pooled estimate of 16 studies (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; DeMarco 2012; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lee 2011; Lee 2012; Lin 2011; Ni 2011; Winter 1994; Yung 2002; Yung 2003) indicated that listening to music had a small effect on heart rate (MD ‐2.77, 95% CI ‐4.76 to ‐0.78, P = 0.006; I² = 79%). The results were inconsistent across studies (Analysis 1.3). Ten of these studies used inadequate methods of randomization or did not report the specific randomization method used. A sensitivity analysis excluding these studies from the analysis resulted in a similar MD of ‐2.44 (95% CI ‐5.95 to 1.07, P = 0.17). However, this effect size was no longer statistically significant and the heterogeneity of the studies increased (I² = 90%) (Analysis 1.3).
1.3. Analysis.
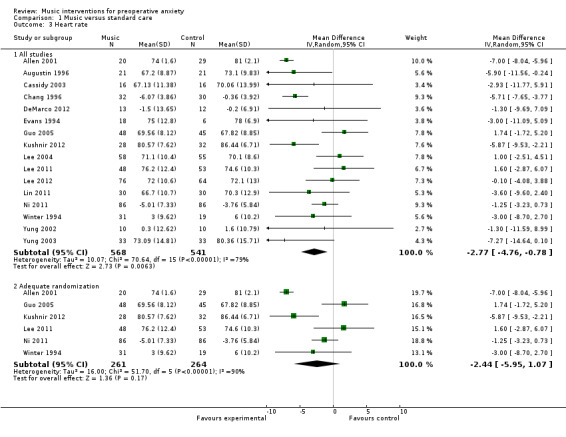
Comparison 1 Music versus standard care, Outcome 3 Heart rate.
Two studies (Lee 2011; Lee 2012) examined the impact of music listening on heart rate variability (HRV) in patients awaiting surgery. HRV is gaining acceptance as a measurement of cardiac parasympathetic activity and, therefore, an indicator of a relaxation response (Friedman 2007). Lee stated that "in the frequency‐domain of HRV, low frequencies (LFs; frequencies between 0.04 and 0.15 Hz) reflect mixed sympathetic and parasympathetic activities. High frequencies (HFs; frequencies between 0.15 and 0.4 Hz) reflect parasympathetic activity. High values of the low to high (LF/HF) ratio indicate a dominance of sympathetic activity while low values indicate a dominance of parasympathetic activity. Activation of the sympathetic nerves, as in anxiety, can cause the HR to increase, high frequencies to decrease, and low frequencies and the low‐to‐high ratio to increase" (Lee 2011, p1182). The pooled estimate of these two studies did not show evidence for an effect of music listening on HRV (LF/HF ratio) (MD ‐0.37, 95% CI ‐1.16 to 0.42, P = 0.36; I² = 69%) (Analysis 1.4).
1.4. Analysis.
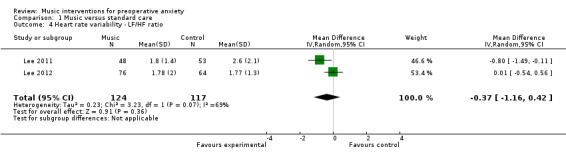
Comparison 1 Music versus standard care, Outcome 4 Heart rate variability ‐ LF/HF ratio.
The study by Bringman (Bringman 2009) did not find a statistically significant difference for HR between the music listening group (mean post‐test value of 67 bpm, SD 11) and the midazolam control group (mean post‐test value of 68 bpm, SD 10). However, given that the music listening group did not receive a preoperative sedative whereas the control group did means that music listening was able to achieve the same sedative effects as preoperative sedative drugs.
Finally, one study (Miluk‐Kolasa 1996) reported a ‐2.2% (SD 1.4) reduction from baseline HR for the music listening group (n = 50) and an 11.1% (SD 1.1) increase for the standard care control group (n = 50). In addition, this study measured the impact of music on cardiac output, the volume of blood being pumped by the heart. An increase in cardiac output can be attributed to an increase in HR and sympathetic nervous system activity. A reduction of 3.5% (SD 2.0) was reported in cardiac output for the music group whereas the control group's results indicated an increase of 10.9% (SD 2.1).
Blood pressure
Fourteen studies (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; DeMarco 2012; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lin 2011; Ni 2011; Szeto 1999; Winter 1994; Yung 2002) examined the effects of music listening on systolic blood pressure (SBP). Their pooled estimate indicated no strong evidence of effect for music listening (MD ‐4.82, 95% CI ‐12.13 to 2.49, P = 0.20; I² = 98%) (Analysis 1.5). A pooled estimate of ‐2.37 mm Hg (95% CI ‐4.03 to ‐0.71; 13 studies) was found for diastolic blood pressure (DBP) and this effect was statistically significant (P = 0.005) (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lin 2011; Ni 2011; Szeto 1999; Winter 1994; Yung 2002). However, the results were inconsistent across studies (I² = 98%) (Analysis 1.6).
1.5. Analysis.
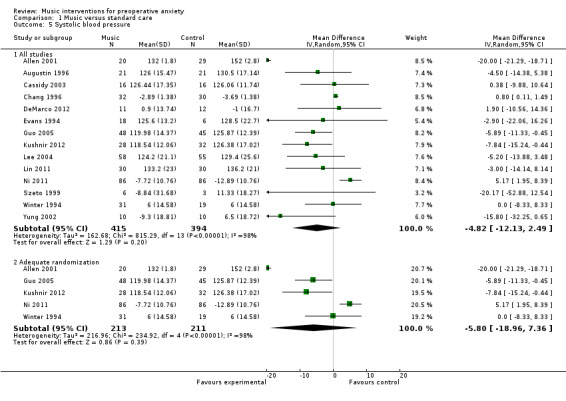
Comparison 1 Music versus standard care, Outcome 5 Systolic blood pressure.
1.6. Analysis.
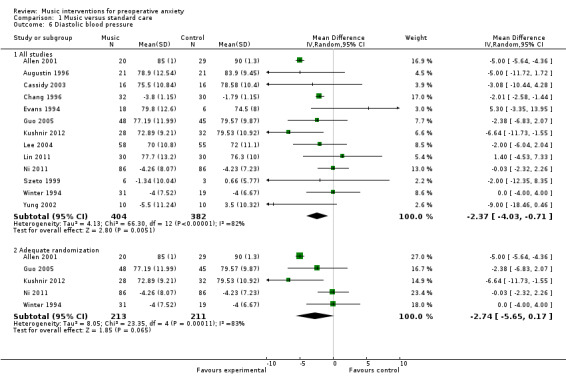
Comparison 1 Music versus standard care, Outcome 6 Diastolic blood pressure.
We conducted sensitivity analyses to assess the impact of inadequate randomization methods on the results. For SBP, the effect size remained non‐significant and heterogeneity persisted (MD ‐5.80, 95% CI ‐18.96 to 7.36, P = 0.39; I² = 98%) (Analysis 1.5). Likewise, for DBP excluding studies because of inadequate randomization method did not influence the effect size but the results were no longer statistically significant (MD ‐2.74, 95% CI ‐5.65 to 0.17, P = 0.06; I² = 83%) (Analysis 1.6).
A large study (N = 327) by Bringman (Bringman 2009) suggested that music listening can result in similar reductions in SBP and DBP compared with the administration of midazolam. Music listening resulted in mean post‐test values of 131 (SD 16) and 81 (SD 12), respectively, whereas midazolam intake resulted in mean post‐test values of 129 (SD 18) and 81 (SD 14), respectively.
The study by Miluk‐Kolasa (Miluk‐Kolasa 1996) reported a SBP change from baseline of ‐2.0% (SD 0.7) for the music group and 4.9% (SD 0.8) for the standard care control group. Similarly, a reduction in DBP was found for the music group (‐0.8%, SD 1) whereas the DBP in the control group increased by 3.8% (SD 1).
Respiratory rate
Listening to music had a clinically insignificant effect on respiratory rate, namely listening to music increased participants' respiratory rate by one breath per minute compared to standard care (6 studies; MD 0.97, 95% CI 0.82 to 1.11, P < 0.00001). Furthermore, the results were inconsistent across studies (I² = 96%) (Analysis 1.7).
1.7. Analysis.
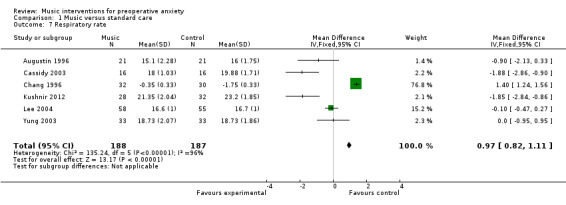
Comparison 1 Music versus standard care, Outcome 7 Respiratory rate.
Skin temperature and skin conductivity
Two studies (Chang 1996; Miluk‐Kolasa 1996) included skin temperature as an outcome variable. Increased skin temperature is related to a greater state of relaxation. The two studies could not be pooled because one study (Miluk‐Kolasa 1996) only reported percentage change scores. No difference in skin temperature between the two groups was found in the Chang study (N = 62) (music group mean post‐test value 33.62, SD 0.11; control group mean post‐test value 33.66, SD 0.11). In contrast, Miluk‐Kolasa (N = 100) reported an increase in skin temperature for the music group (4.3%, SD 0.4) and a decrease for the control group (‐3.1%, SD 0.3).
Guo (Guo 2005) included skin conductivity in a study examining the impact of music listening on the anxiety of 93 participants awaiting laparoscopic surgery. Skin conductivity refers to the electrical conductance of the skin, which varies with its moisture level. Because the sweat glands are controlled by the sympathetic nervous system, skin conductance is used as an indication of psychological or physiological arousal or stress response. Even though music group participants reported significantly less anxiety after music listening than control group participants, this self‐reported anxiety reduction was not reflected in the skin conductivity results with a mean post‐test value of 4.54 (SD 0.12) for the music group and 4.03 (SD 1.53) for the control group.
Salivary cortisol
Salivary cortisol is frequently used as a biomarker for psychological stress yet only one study in this review included this as an outcome (Guo 2005). Music listening (mean 3.11, SD 0.92) had a small, statistically significant effect on post‐intervention cortisol levels compared to the standard care control group (mean 3.61, SD 1.08).
Glucose count
Miluk‐Kolasa (Miluk‐Kolasa 1996) included plasma glucose concentrations as an outcome related to stress response in preoperative patients. An increase in blood glucose may be a function of increased stress. Listening to music preoperatively resulted in an average decrease in blood glucose of 6.9% (SD 1.9). In contrast, an average increase of 10.2% (SD 2.0) was found in the standard care control group.
Physical outcomes
None of the studies in this review included physical outcomes such as infection rate or wound healing. Some studies measured the effect of music on pain, but this outcome was not included in this review because of overlap with a published Cochrane review on music interventions for pain (Cepeda 2006).
Patient satisfaction
None of the studies included in this review included patient satisfaction as an outcome.
Discussion
Summary of main results
Preoperative anxiety
The results of 20 trials suggest that music listening may have a beneficial effect on anxiety in people awaiting surgery. Music listening resulted, on average, in an anxiety reduction that was 5.72 units greater than that of the standard care group, as measured by the STAI‐S. At this time, there is no consensus on what constitutes a clinically significant change in anxiety as measured by the STAI‐S. However, assessment of clinical significance is often determined using 0.5 standard deviation (SD) of the baseline measure as a guideline (Sloan 2005). Baseline SDs of studies included in this review ranged from 5.7 to 10.66, with a mean SD of 8.77. Based on the 0.5 SD rule, the difference between the treatment group and control group found in this review could therefore be considered clinically significant. Studies that used anxiety scales other than the STAI‐S resulted in a difference of ‐0.60 standardized units. Although the magnitude of the effect differed across the studies that used non‐STAI anxiety scales, the trials agreed on the direction of the point estimates. These anxiety‐reducing results are considered moderate in size according to interpretation guidelines put forth by Cohen (Cohen 1988). Cohen suggested that an effect size of 0.2 be considered a small effect, an effect size of 0.5 medium, and an effect size of 0.8 large.
Preoperative sedative drug intake
None of the studies in this review included preoperative sedative drug intake as an outcome variable. However, the results of one study that compared a non‐midazolam music listening group directly with a midazolam group found that music listening was more effective than midazolam for preoperative anxiety reduction.
Physiological responses
As for the effect of music on physiological responses, the results of 16 studies suggest that music listening has a small effect on heart rate, but these results were inconsistent across studies. No evidence was found for an effect of music listening on heart rate variability (HRV). However, the HRV result is based on two studies and more research is needed. One study reported that music listening significantly reduced cardiac output compared to a standard care control group.
Mixed results were found for blood pressure. Whereas no support for an effect of music was found for systolic blood pressure, those same studies did find support for an effect of music on diastolic blood pressure, although again the results were inconsistent across studies.
Listening to music had a clinically insignificant effect on respiratory rate, namely listening to music resulted in a respiratory rate that was faster by one breath per minute compared to the control group. The results were highly inconsistent across studies.
The results on the effect of music listening on skin temperature and skin conductivity were inconclusive with one study finding support for a beneficial effect and two studies failing to demonstrate such support.
Finally, single studies found a small, statistically significant effect of music on cortisol levels and blood glucose levels.
No studies were identified that addressed the other secondary outcomes listed in the protocol, namely physical outcomes and patient satisfaction.
Overall completeness and applicability of evidence
This review included 26 randomized and quasi‐randomized controlled trials. All trials used listening to pre‐recorded music as the music intervention. No music therapy trials, as defined by the authors in the background section, were included in this review. Although we found several music therapy studies that measured preoperative anxiety, these studies could not be included because they did not use a control group, suffered from insufficient data reporting, or failed to use standardized measures of anxiety.
In general, the trials that used listening to pre‐recorded music included limited information about the music selections used, except for mentioning general music styles (for example new age, classical music, easy listening, etc.). Music within each of these styles can vary widely and more detailed information would help clinicians make well‐informed decisions regarding music selections. More research is needed to evaluate the effect of music that is truly patient‐preferred, as well as the effect of music with different characteristics (tempo, timbre, harmony, emotional intensity, etc.) on patients during high anxiety situations such as when awaiting surgery.
Most trials used one music intervention session of 20 to 30 minutes. This clinical uniformity adds to the strength of this review, but also leaves several questions unanswered. First, the relationship between the frequency and duration of treatment and treatment effect remains unclear. Could it be that multiple music sessions before the onset of surgery, where feasible, result in greater benefit? Two studies (Li 2004; Lin 2011) did offer multiple music sessions starting with the first session several days before surgery and continuing to the day of the surgery. Compared to other studies, these two studies resulted in greater anxiety reduction. We would like to suggest that offering multiple music listening sessions allows for the patient to give feedback about the music, select different music if needed, and become more skilled in using music for relaxation purposes. Further investigation into the optimal frequency and duration of music interventions for presurgical patients is needed. In addition, since no music therapy interventions that use live music to meet specific in‐the‐moment needs of the patients were included in these studies, we were unable to determine whether these would be more effective than listening to pre‐recorded music.
Presently, no data can be provided regarding cost or cost‐effectiveness of the use of music interventions in the presurgical arena as these data were not included in the trials reviewed.
Because little information was provided in these studies about the ethnic make‐up of the patient samples, one can question the generalizability of these results to various ethnic groups. Persons' cultures may influence their music preferences and their potential acceptance and use of music as a therapeutic agent, especially during high‐stress medical situations such as surgery. This in turn may influence the anxiety‐reducing potential of music, to a greater or lesser degree.
Quality of the evidence
In general the quality of reporting was poor, with only 11 studies detailing the methods of randomization and allocation concealment, and level of blinding. The chief investigators of many studies needed to be contacted to provide additional methodological and statistical information. All but two studies received a high risk of bias rating.
Because of the large number of trials at high risk of bias, the findings of this review need to be interpreted with caution. It is important to be mindful that many studies received a high risk of bias because of lack of blinding. Often blinding of participants is not possible in music medicine or music therapy studies unless a comparative design is used (for example, comparing listening to pre‐recorded music with interactive music making with a therapist). When participants cannot be blinded to the intervention, there is definitely an opportunity for bias when participants are asked to report on subjective outcomes such as anxiety. However, this also means that trials that meet all other requirements for a low risk of bias rating are assigned a high risk of bias because of the inability to meet the blinding requirement for subjective outcomes.
For anxiety, consistent effects were obtained across studies. For the other outcomes included in the protocol, inconsistent results were obtained or not enough studies were available.
In summary, the quality of evidence was low (Table 1).
Potential biases in the review process
The strength of our review is that we searched all available databases and a large number of music therapy journals (English, German, and French language), checked reference lists of all relevant trials, contacted relevant experts for identification of unpublished trials, and included publications without restricting language. In spite of such a comprehensive search, it is still possible that we missed some published and unpublished trials. We requested additional data, where necessary, for all trials we considered for inclusion. This allowed us to get accurate information on the trial quality and data for most trials and helped us make well‐informed trial selection decisions.
It is possible that we did not identify some grey literature; however, it is doubtful that this would have had a significant impact on our results. Grey literature tends to include trials with relatively small numbers of participants and inconclusive results (McAuley 2000).
Agreements and disagreements with other studies or reviews
The findings of this review are consistent with the results of a review (26 studies) on the effects of music interventions on anxiety in patients awaiting minimally invasive procedures (Gillen 2008). Gillen and colleagues reported that music had a consistent and statistically significant effect on pre‐procedural anxiety. However, no consistent effects were found for physiological responses. Based on these results, they questioned the adequacy of current theories that link anxiety and the autonomic nervous system and the impact that music listening may have on these processes. Similarly, a review by Pittman and Kridli (Pittman 2011) (11 studies) found that music listening consistently reduced anxiety in patients awaiting surgery or invasive medical procedures. However, they reported inconsistent results regarding music’s effectiveness in lowering blood pressure, heart rate, and respiration in presurgical and pre‐procedural patients.
Authors' conclusions
Implications for practice.
Results of this review indicate that music listening may help reduce anxiety in patients awaiting surgery. These results are consistent with the findings of three other Cochrane systematic reviews on the use of music for anxiety reduction with coronary heart disease patients (Bradt 2009), mechanically ventilated patients (Bradt 2010), and cancer patients (Bradt 2011). Moreover, the results of one large study (Bringman 2009) indicated that music listening was more effective than midazolam for preoperative anxiety reduction and equally effective for reduction of heart rate and blood pressure. Given the support provided now by four Cochrane reviews for the anxiety‐reducing effects of music for medical patients, in addition to the fact that preoperative sedatives and anti‐anxiety drugs often have negative side effects and may prolong patient recovery and discharge, we suggest that music interventions should be offered to patients as an alternative to these drugs.
Although other Cochrane reviews have shown clear support for a beneficial though small effect of music on physiological responses in medical patients (Bradt 2009; Bradt 2010; Bradt 2011), the current review is less conclusive. Support was found for a small effect of music on heart rate and diastolic blood pressure although results were inconsistent across studies. Single studies reported a beneficial effect of music listening on salivary cortisol and blood glucose levels. This decrease in sympathetic nervous system and endocrine activation corresponds with the anxiety‐reducing effects found by subjective outcome measures in this review. However, this review did not provide evidence of such effect for respiratory rate, systolic blood pressure, or skin temperature. These conflicting findings regarding the impact of music on vital signs in presurgical patients may be related to the type and duration of music, as well as preoperative medication potentially masking physiological changes (Pittman 2011).
None of the studies included postoperative outcomes such as wound healing, infection rate, patient recovery and discharge, or patient satisfaction.
Implications for research.
This systematic review provides evidence that listening to pre‐recorded music may have beneficial effects on preoperative anxiety. However, randomized controlled trials (RCTs) are needed that examine the impact of other types of music interventions including live, interactive music experiences provided by professional music therapists. Music therapists are specially trained both clinically and academically to carefully select music interventions that actively engage patients and meet their specific needs. The act of making music together can provide a strong sense of support. Furthermore, the active and creative engagement in music making stands in stark contrast to passively submitting oneself to surgical procedures. This may result in an increased sense of control and empowerment. Future studies should examine the effects of active music therapy interventions and identify mediating variables such as social support, perceived level of control, and positive outlook.
Given the inconsistent changes in physiological responses in participants when listening to music during the preoperative period, more studies are needed to investigate the physiological mechanisms by which music reduces self‐reported anxiety. Consequently, some of the current theories on music's sedative impact through alteration of autonomic nervous system activity may need to be reconsidered (Gillen 2008).
Future trials that use listening to pre‐recorded music should report greater details related to the music selections made available to participants and exercise greater care in selecting music that reflects the patient's true preference (rather than just giving the patient the option to select from four or five general genres). In addition, more details concerning the delivery of the music are needed. We recommend that researchers consult the reporting guidelines for music‐based intervention developed by Robb, Burns, and Carpenter (Robb 2011). Finally, studies are needed that compare the effects of different frequencies and durations of music sessions.
Studies are urgently needed on the use of music interventions in paediatric surgical patients. All studies in this review included adult patients only.
Future studies should include important outcome variables such as preoperative sedative drug intake as well as postoperative outcomes including wound healing and recovery, infection rate, and time to discharge. Furthermore, given the promising results of the Bringman study (Bringman 2009), in which the effects of music listening were directly compared with the intake of a preoperative sedative, more studies are needed that make such direct comparisons. In addition, formal evaluation of the cost benefit of music interventions for preoperative anxiety reduction is needed.
Finally, researchers of future studies need to take greater care to design trials that meet current methodological standards (Bradt 2012) and adhere to CONSORT standards for reporting of RCTs (Schulz 2010) including detailing the randomization method, procedures for allocation concealment, blinding of personnel and outcome assessors, and attrition rate and reasons. Although blinding of participants is often not feasible in music medicine or music therapy trials, it is important that future trials meet those design aspects that minimize risk of bias.
History
Protocol first published: Issue 1, 2008 Review first published: Issue 6, 2013
| Date | Event | Description |
|---|---|---|
| 27 June 2008 | Amended | Converted to new review format. |
Notes
At the time of this review, we identified a published journal article (Beccaloni 2011) that plagiarized a section of the background text of the published protocol of this review (Dileo 2008). After an investigation, the following plan of action was agreed upon: the author will revise the abstract to include quotations around the directly quoted material as well as inclusion of the appropriate reference. This revision as well as an erratum addressing the issue will be published in the Journal of Perianesthesia Nursing 28(2):April 2013.
Acknowledgements
We would like to thank Nicola Petrucci (content editor), Nathan Pace (Statistical editor), Claire Ghetti, Fred J Schwartz (peer reviewers) and Ann Fonfa (consumer representative ) for their help and editorial advice during the preparation of this systematic review. We would like to thank and acknowledge Dr Nicola Petrucci (content editor), Dr Fred J Schwartz, Dr M Soledad Cepeda, Prof Bryan C Hunter, and Dr Megan Prictor (peer reviewers) for commenting on the protocol for the systematic review. Finally, we would like to thank Dr Kathleen Murphy for her assistance in retrieval of articles for this review.
Appendices
Appendix 1. Search strategy for CENTRAL, The Cochrane Library
#1 MeSH descriptor Anxiety explode all trees #2 MeSH descriptor Stress, Psychological explode all trees #3 MeSH descriptor Panic explode all trees #4 MeSH descriptor Fear explode all trees #5 (anxiety near (reduct* or alleviat*)) #6 anxiety:ti,ab #7 sedation or sedative #8 (anxioly* or stress or distress or fear):ti,ab #9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8) #10 surgery or surgical or preoperative #11 MeSH descriptor Surgical Procedures, Operative explode all trees #12 MeSH descriptor Preoperative Care explode all trees #13 (#10 OR #11 OR #12) #14 (#9 AND #13) #15 MeSH descriptor Anti‐Anxiety Agents explode all trees #16 MeSH descriptor Conscious Sedation explode all trees #17 MeSH descriptor Analgesia explode all trees #18 (#15 OR #16 OR #17) #19 (#14 OR #18) #20 MeSH descriptor Music explode all trees #21 MeSH descriptor Music Therapy explode all trees #22 (music near compos*) #23 music near rhythm* #24 music* or melod* #25 singing or sing or song or songs or improvis* #26 (#20 OR #21 OR #22 OR #23 OR #24 OR #25) #27 (#19 AND #26)
Appendix 2. MEDLINE search strategy (OvidSP)
1 exp anxiety/ 2 Stress, Physiological/ or Stress, Psychological/ 3 exp panic/ or exp fear/ 4 (anxiety adj5 (reduct$ or alleviat$)).tw. 5 anxiety.ab. 6 (sedation or sedative).tw. 7 (anxioly$ or stress or distress or fear).ab. 8 or/1‐7 9 (surgery or surgical or preoperative).tw. 10 exp surgery/ 11 exp Preoperative Care/ 12 or/9‐11 13 8 and 12 14 exp Anti‐Anxiety Agents/ 15 exp Conscious Sedation/ 16 exp analgesia/ 17 or/14‐16 18 13 or 17 19 exp music/ 20 exp music therapy/ 21 (music adj5 compos$).tw. 22 (music adj5 rhythm$).tw. 23 (music$ or melod$).tw. 24 (singing or sing or song or songs or improvis$).tw. 25 or/19‐24 26 randomized controlled trial.pt. 27 controlled clinical trial.pt. 28 randomized.ab. 29 placebo.ab. 30 clinical trials as topic.sh. 31 randomly.ab. 32 trial.ti. 33 or/26‐32 34 humans.sh. 35 33 and 34 36 18 and 25 and 35
Appendix 3. EMBASE search strategy (OvidSP)
1 exp Anxiety/ 2 exp Stress/ 3 exp Panic/ 4 exp Fear/ 5 (anxiety adj5 (reduct$ or alleviat$)).mp. 6 anxiety.ab. 7 (sedation or sedative).mp. 8 (anxioly$ or s! tress or distress or fear).ab. 9 or/1‐8 10 (surgery or surgical or preoperative).mp. 11 exp surgery/ 12 exp Preoperative Care/ 13 or/10‐12 14 13 and 9 15 exp Anxiolytic Agent/ 16 exp Conscious Sedation/ 17 exp Analgesia/ 18 or/15‐17 19 18 or 14 20 exp Music Therapy/ or exp Music/ 21 (music adj5 compos$).mp. 22 (music adj5 rhythm$).mp. 23 (music$ or melod$).mp. 24 (singing or sing or song or songs or improvis$).mp. 25 or/20‐24 26 25 and 19 27 (RANDOMIZED‐CONTROLLED‐TRIAL/ or RANDOMIZATION/ or CONTROLLED‐STUDY/ or MULTICENTER‐STUDY/ or PHASE‐3‐CLINICAL‐TRIAL/ or PHASE‐4‐CLINICAL‐TRIAL/ or DOUBLE‐BLIND‐PROCEDURE/ or SINGL! E‐BLIND‐PROCEDURE/ or (RANDOM* or CROSS?OVER* or FACTORIAL* or PLACEBO* or VOLUNTEER* or ((SINGL* or DOUBL* or TREBL* or TRIPL*) adj3 (BLIND* or MASK*))).ti,ab.) and human*.ec,hw,fs. 28 27 and 26
Appendix 4. CINAHL search strategy (EBSCOhost)
S1 MJ anxiety S2 MJ Stress S3 MJ panic S4 MJ fear S5 (anxiety and (reduct* or alleviat*)) S6 AB anxiety S7 sedation or sedative S8 AB anxioly* or stress or distress or fear S9 S8 or S7 or S6 or S5 or S4 or S3 or S2 or S1 S10 surgery or surgical or preoperative S11 MJ surgery S12 MJ Preoperative Care S13 S12 or S11 or S10 S14 S13 and S9 S15 MW AntiAnxiety Agents S16 MJ Conscious Sedation S17 MJ analgesia S18 S17 or S16 or S15 S19 S18 or S14 S20 MJ music S21 MJ music therapy S22 music and compos* S23 music and rhythm* S24 music* or melod* S25 singing or sing or song or songs or improvis* S26 S25 or S24 or S23 or S22 or S21 or S20 S27 S26 and S19
Appendix 5. PsycINFO search strategy (OvidSP)
1 exp anxiety/ 2 exp Stress/ 3 exp panic/ or exp fear/ 4 (anxiety adj5 (reduct$ or alleviat$)).tw. 5 anxiety.ab. 6 (sedation or sedative).tw. 7 (anxioly$ or stress or distress or fear).ab. 8 or/1‐7 9 (surgery or surgical or preoperative).tw. 10 exp surgery/ 11 exp Surgical Patients/ 12 or/9‐11 13 8 and 12 14 exp Tranquilizing Drugs/ 15 exp Sedatives/ 16 exp Analgesia/ 17 (conscious adj5 sedation).tw. 18 or/14‐17 19 13 or 18 20 exp music/ 21 exp music therapy/ 22 (music adj5 compos$).tw. 23 (music adj5 rhythm$).tw. 24 (music$ or melod$).tw. 25 (singing or sing or song or songs or improvis$).tw. 26 or/20‐25 27 empirical study.md. 28 followup study.md. 29 longitudinal study.md. 30 prospective study.md. 31 quantitative study.md. 32 "2000".md. 33 treatment effectiveness evaluation/ 34 exp hypothesis testing/ 35 repeated measures/ 36 exp experimental design/ 37 placebo$.ti,ab. 38 random$.ti,ab. 39 (clin$ adj25 trial$).ti,ab. 40 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).ti,ab. 41 or/27‐40 42 26 and 19 and 41 43 limit 42 to human
Appendix 6. LILACS search strategy (Virtual Health Library)
music [Words] and preoperative [Words]
music [Words] and surgery [Words]
music [Words] and surgical [Words]
music [Words] and presurgical [Words]
music [Words] and sedation [Words]
music [Words] and sedative [Words]
Appendix 7. AMED search strategy (OvidSP)
1 exp anxiety/ 2 exp Stress psychological/ 3 exp panic/ or exp fear/ 4 (anxiety adj5 (reduct$ or alleviat$)).tw. 5 anxiety.ab. 6 (sedation or sedative).tw. 7 (anxioly$ or stress or distress or fear).ab. 8 or/1‐7 9 (surgery or surgical or preoperative).tw. 10 exp surgery/ 11 exp Preoperative Care/ 12 or/9‐11 13 8 and 12 14 Anti‐Anxiety Agents.mp. 15 Conscious Sedation.tw. 16 exp analgesia/ 17 16 or 15 or 14 18 13 or 17 19 exp music/ 20 exp music therapy/ 21 (music adj5 compos$).tw. 22 (music adj5 rhythm$).tw. 23 (music$ or melod$).tw. 24 (singing or sing or song or songs or improvis$).tw. 25 or/19‐24 26 randomized controlled trial.pt. 27 controlled clinical trial.pt. 28 randomized.ab. 29 placebo.ab. 30 exp Clinical trials/ 31 trial.ti. 32 trial.ti. 33 or/26‐32 34 humans.sh. 35 33 and 34 36 18 and 25 and 35
Appendix 8. Social Science Citation Index search strategy (ISI)
#1 TS = anxiety or TS=stress or TS=(panic or fear) or TS=(anxiety SAME (reduct* OR alleviat*)) or TS = (sedation OR sedative) or TS = (anxioly* OR distress) #2 TS = (surgery or surgical or preoperative) or TS=(preoperative care) #3 #1 and #2 #4 TS = (anti‐anxiety agents) or TS=(Conscious Sedation) or TS = (analgesia or analgesic*) #5 #4 or #3 #6 TS = music or TS = (music therapy) or TS = (music SAME compos$) or TS = (music SAME rhythm*) or TS = (music* or melod*) or TS = (singing or sing or song or songs or improvis*) #7 #6 and #5 #8 TS=(random allocation) or TS=(controlled clinical trial$) or TS=(randomized controlled trial$) or TS=(double blind method$) or TS=(single‐blind method$) or TS=(Clinical trial$) or TS=placebo$ or TS=random$ or TS=(comparative study) or TS=(evaluation studies) or TS=(follow up studies) or TS=(prospective studies) or TS=(control$ or prospectiv$ or volunteer$) #9 #8 and #7
Appendix 9. The specialist music therapy research database search strategy
Research database is no longer functional. Archives of research reports, dissertations and conference proceedings were handsearched.
Appendix 10. CAIRSS for Music search strategy (Webvoyage)
(stress anxiety)[ in Keyword Anywhere ]AND(surgery surgical preoperative pre operative presurgical pre surgical sedative sedation)[ in Keyword Anywhere ]
Appendix 11. Proquest Digital Dissertations search strategy
("music therapy") AND (stress) AND (preoperative) OR (surgery)
cabs(music therapy) AND cabs(conscious sedation)
cabs(music therapy) AND (cabs(analgesic) OR cabs(sedation) OR cabs(sedative)) AND cabs(surgery)
cabs(music therapy) AND cabs(anxiety) AND (cabs(surgical) OR cabs(preoperative))
(cabs(song) OR cabs(singing) OR cabs(sing)) AND cabs(analgesia)
(cabs(listening) OR cabs(improvisation)) AND cabs(analgesia)
(cabs(listening) OR (improvisation)) AND cabs(anxiety) AND (cabs(preoperative) OR cabs(surgery))
(cabs(listening) OR cabs(improvisation)) AND (cabs(sedation) OR cabs(sedative))
(cabs(singing) OR cabs(sing) OR cabs(song)) AND (cabs(sedation) OR cabs(sedative))
(cabs(singing) OR cabs(sing) OR cabs(song)) AND cabs(conscious sedation)
(singing) OR (sing) OR (song) AND (preoperative) OR (surgery)
cabs(music) AND (cabs(anti anxiety agents) OR cabs(conscious sedation))
cabs(music) AND cabs(conscious sedation)
(music) AND ("preoperative") OR (surgery) AND (sedation) OR (sedative)
cabs(music) AND cabs(conscious sedation)
(music) AND cabs((anti anxiety agents OR conscious sedation))
(music)AND (anxiety) AND (preoperative) OR (surgery)
(music) AND (anxieties) OR (anti anxiety agent) OR (conscious sedation)
Appendix 12. ClinicalTrials.gov search strategy
Music
Appendix 13. Current Controlled Trials search strategy
Music
Appendix 14. National Research Register search strategy
Music and anxiety
Music and stress
Data and analyses
Comparison 1. Music versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 State anxiety STAI) | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All studies | 13 | 896 | Mean Difference (IV, Random, 95% CI) | ‐5.72 [‐7.27, ‐4.17] |
| 1.2 Adequate randomization | 4 | 435 | Mean Difference (IV, Random, 95% CI) | ‐5.76 [‐7.94, ‐3.57] |
| 2 Anxiety (non‐STAI) | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 All studies | 7 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.90, ‐0.31] |
| 2.2 Adequate randomization | 3 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 3 Heart rate | 16 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 All studies | 16 | 1109 | Mean Difference (IV, Random, 95% CI) | ‐2.77 [‐4.76, ‐0.78] |
| 3.2 Adequate randomization | 6 | 525 | Mean Difference (IV, Random, 95% CI) | ‐2.44 [‐5.95, 1.07] |
| 4 Heart rate variability ‐ LF/HF ratio | 2 | 241 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.16, 0.42] |
| 5 Systolic blood pressure | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 All studies | 14 | 809 | Mean Difference (IV, Random, 95% CI) | ‐4.82 [‐12.13, 2.49] |
| 5.2 Adequate randomization | 5 | 424 | Mean Difference (IV, Random, 95% CI) | ‐5.80 [‐18.96, 7.36] |
| 6 Diastolic blood pressure | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 All studies | 13 | 786 | Mean Difference (IV, Random, 95% CI) | ‐2.37 [‐4.03, ‐0.71] |
| 6.2 Adequate randomization | 5 | 424 | Mean Difference (IV, Random, 95% CI) | ‐2.74 [‐5.65, 0.17] |
| 7 Respiratory rate | 6 | 375 | Mean Difference (IV, Fixed, 95% CI) | 0.97 [0.82, 1.11] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 2001.
| Methods | Randomized controlled trial (RCT) 2‐arm parallel group design |
|
| Participants | Adult ambulatory surgical patients scheduled for ophthalmic surgery Diagnosis: 2 patients with glaucoma; all others: cataract removal Total N randomized: 40 N randomized to music group: 20 N randomized to control group: 20 N analysed in music group: 20 N analysed in control group: 20 Mean age: 75.5 years Sex: 30 (75%) females, 10 (25%) males Ethnicity: Not reported Setting: outpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music through headphones 2. Control group: resting quietly, no music Music provided: participants selected from 22 types of music including soft hits, classical guitar, chamber music, folk music or popular singers from the 1940s and 1950s Number of sessions: 1 Length of sessions: Not reported Categorized as music medicine |
|
| Outcomes | Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR): post‐test scores in preoperative period Stress: not included in this review since this outcome was measured only at baseline and postoperatively Coping: not included in this review since this outcome was measured only at baseline and postoperatively |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were sequentially selected from the patient rosters of two ophthalmic surgeons. Office assistants unaware of the study prepared patient rosters. On each day of data collection surgeons were randomly assigned to have their patients in the experimental or control group." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | This study used two subjective outcomes but these could not be included in this review because they did not pertain to preoperative anxiety. Therefore, a low risk of bias rating is given here. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | SBP, DBP and HR measurement were obtained by a Propaq Monitor and digitally recorded. It is unclear if the outcome assessor collecting the physiological responses was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | This research was supported in part by a grant from the Food and Drug Administration (FD‐T‐ 000889). No conflicts of interest identified. |
Arslan 2008.
| Methods | Controlled clinical trial (CCT) 2‐arm parallel group design |
|
| Participants | Adult patients undergoing urogenital surgery Diagnosis: urinary tract problems (n = 48, 75%); genital tract problems (n = 16, 25%) Total N randomized: 64 N randomized to music group: 32 N randomized to control group: 32 N analysed in music group: 32 N analysed in control group: 32 Mean age: 43.29 years Sex: 0 (0%) females, 64 (100%) males Ethnicity: Turkish (no detailed ethnicity information is reported) Setting: inpatient Country: Turkey |
|
| Interventions | Two study groups: 1. Music group: listening to preferred music through headphones plugged into a portable cassette player 2. Control group: standard care Music provided: participants selected from Turkish classical music, folk music, Turkish art music, or pop music Number of sessions: 1 Length of sessions: 30 minutes Categorized as music medicine |
|
| Outcomes | State anxiety (Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety form, STAI‐S): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Random assignment was achieved based on the day that patients underwent surgery. Patients who underwent surgery on Monday or Wednesday were assigned to the control group while patients who had their surgery on Tuesday or Thursday were assigned to the experimental group." |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Augustin 1996.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Adult patients scheduled for ambulatory surgery Type of surgery: arthroscopy (n = 12, 26%), herniorrhaphy (n = 8, 17%), orthopedic procedure (n = 6, 13%), urologic procedures (n = 5, 11%), nerve repairs (n = 4, 9%), endoscopic procedure (n = 3, 6%), laparoscopic procedures (n = 2, 4%), and breast biopsies (n = 2, 4%) Total N randomized: 42 N randomized to music group: 21 N randomized to control group: 21 N analysed in music group: 21 N analysed in control group: 21 Mean age: 47 Sex: 17 (40%) females, 25 (60%) males Ethnicity: 100% Caucasian Setting: inpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: preoperative instruction coupled with music listening 2. Control group: routine preoperative instruction Music provided: participants selected from classical, environmental, new age, western country, or general easy‐listening music Number of sessions: 1 Length of sessions: 15‐30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): change score HR, respiratory rate (RR), SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "When patients agreed to participate, we obtained their written informed consents and alternately assigned them to either the experimental or control group." |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded (personal communication with chief investigator) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | The outcome assessors were not blinded (personal communication with chief investigator) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss (personal communication with chief investigator) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Bringman 2009.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adults patients scheduled for an elective day or short‐stay surgery Type of surgery: laparotomy, hip replacement, laparoscopy, ventral hernia repair, inguinal hernia repair, arthroscopy, varicose vein, scrotal or vaginal surgery (number of participants per diagnosis not reported) Total N randomized: 372 N randomized to music group: 190 N randomized to control group: 182 N analysed in music group: 177 N analysed in control group: 150 Mean age: 50 years Sex: 198 (53%) females, 138 (47%) males Ethnicity: not reported Setting: inpatient Country: Sweden |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music. Patients in the music group did not receive pre‐medication midazolam solution. 2. Control group: standard pre‐medication midazolam solution orally Music provided: participants selected from classical, soft pop/film, soft jazz, nature sound, or instrumental music. CDs were compiled by a professional music therapist. Number of sessions: 1 Length of sessions: 17‐42 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test score HR, SBP, DBP, arterial pressure (AP): post‐test scores |
|
| Notes | Even though a professional music therapist helped with the selection of the music for this study, this study is categorized as a music medicine study because the patients listened to pre‐recorded music without the presence of a therapeutic process with the music therapist. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The music therapist randomized the patients through sealed envelopes immediately before the intervention" |
| Allocation concealment (selection bias) | Low risk | Quote: "[the music therapist] drew the first envelope in a row of previously randomly mixed envelopes consisting of an equal number of both allocations." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | The music therapist recorded the blood pressure and heart rate using a Riester fully automatic digital blood pressure monitor before and after the intervention. The music therapist was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 12%: 13 patients were excluded from experimental group due to logistic reasons (n = 12) and other reason (n = 1), and 23 patients were excluded from the control group due to logistic reasons (n = 19), and not receiving midazolam (n = 4). Quote: "The reasons for exclusion were logistic in the majority of cases, mainly due to a too early call to the operating room, which had the effect that the time between the intervention and the evaluation was too short. Hence, 177 patients in the music group and 159 in the midazolam group went through the study protocol; however, nine patients in the midazolam group were too sedated to be able to complete the second STAI X‐1." |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Cassidy 2003.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients scheduled for elective surgery Type of surgery: no details reported Total N randomized: 32 N randomized to music group: 16 N randomized to control group: 16 N analysed in music group: 16 N analysed in control group: 16 Mean age: 41.5 Sex: 21 (65.6%) females, 11 (34.4%) males Ethnicity: Not reported Setting: Outpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: standard care Music provided: Participants were asked to bring the music of their choice from home Number of sessions: 1 Length of sessions: 15 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores RR, pulse, SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The first patients was assigned to control group or intervention group by a coin toss. Each subsequent subject was assigned alternately to the control group or intervention group" |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | The researcher measured the pulse, respiration and blood pressure and was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Chang 1996.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients scheduled for surgery Type of surgery: open heart surgery including coronary artery bypass graft surgery (CABG) (n = 17, 27%) , valvular surgery (n = 33, 53%), and other (n = 12, 19%) Total N randomized: 62 N randomized to music group: 32 N randomized to control group: 30 N analysed in music group: 32 N analysed in control group: 30 Mean age: 51.8 Sex: 29 (47%) females, 33 (53%) males Ethnicity: not reported; most participants likely Taiwanese Setting: Inpatient Country: Taiwan |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: resting Music provided: music with 60‐72 beats per minute with bass tone and soft melody or religious music in a variety of languages including Chinese, Taiwanese, English and Japanese Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (VAS): post‐test scores HR, RR, SBP, DBP, pain, skin temperature: change scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for this study |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Cooke 2005.
| Methods | RCT 3‐arm parallel group design |
|
| Participants | Adult patients scheduled for day surgery Type of surgery: orthopaedic (n = 57, 32%), skin (n = 58,32%), breast (n = 15, 8%), urology (n = 24, 13%), general (n = 15, 8%), other (n = 11, 6%) Total N randomized: 180 (120 included in this review) N randomized to music group: 60 N randomized to control group: 60 N randomized to placebo group: 60 (not included in this review) N analysed in music group: 60 N analysed in control group: 60 N analysed in placebo group: 60 (not included in this review) Mean age: 55.7 years Sex: 90 (50%) females, 90 (50%) males Ethnicity: Not reported Setting: Outpatient Country: USA |
|
| Interventions | Three study groups: 1. Music group: listening to pre‐recorded music 2. Control group: standard nursing care 3. Placebo group: Wore headphones for 30 minutes with no sound. Music provided: patient‐selected pre‐recorded CD from one of the following genres, classical, jazz, country and western, new age, or easy‐listening Number of sessions: 1 Length of sessions: 30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): post‐test scores | |
| Notes | Standard deviations (SDs) are not reported in the research report but we were able to obtain the values from the investigator | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated list was used for permuted block random assignment to intervention, placebo or control groups by gender. That is, males and females were randomized separately so that equal numbers of each were assured in each group" |
| Allocation concealment (selection bias) | Low risk | Quote: "A biostatistician and research assistant who did not participate in data collection conducted the randomization procedures and prepared sequentially numbered sealed envelopes containing the random assignment for each consenting patient." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants was not possible. The nurses who provided care were blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The study did not address objective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. This research was supported by funding received from the Griffith University New Researcher Grant Scheme |
DeMarco 2012.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Adult patients undergoing elective cosmetic surgery Type of surgery: cosmetic surgery (no further details reported) Total N randomized: 38 N randomized to music group: 19 N randomized to control group: 19 N analysed in music group: 14 N analysed in control group:12 Mean age: 46.35 Sex: 24 (96%) females, 2 (4%) males Ethnicity: Not reported Setting: Outpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: listening to prerecorded music via headphones 2. Control group: standard care Music provided: CD selected by a music therapist: "Music for Unwinding". Music was composed by J Nagler, music therapist. The music style was identified as New Age Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | STAI: change scores HR, SBP: change scores |
|
| Notes | Even though a music therapist was involved with the music selection, the authors specifically state that this study did not use a music therapy intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients were randomized based on the day of their surgery using alternating placement in the control and experimental groups" |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessor was not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large subject loss: 32% (n = 12). Subject withdrawals are reported as follows: 38 participants consented and 26 completed all study requirements. Reasons for withdrawal included "patients cancelled the procedures, were taken into surgery early with no adequate time to complete all study requirements" |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No conflict of interest statement was reported |
Evans 1994.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Patients undergoing surgery under general anaesthesia Type of surgery: endoscopic cholecystectomy (n = 16, 67% ), endoscopic henorrhapsy (n = 7, 29% ), endoscopic appendectomy (n = 1, 4%) Total N randomized: 24 N randomized to music group: 18 N randomized to control group: 6 N analysed in music group: 18 N analysed in control group: 6 Mean age: 48.1 Sex: 14 (58%) females, 10 (42%) males Ethnicity: Not reported Setting: Inpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: receiving verbal reassurance Music provided: Participants selected from a variety of "easy listening" music that the medical staff had recorded. Number of sessions:1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI, Visual Analogue Anxiety Scale (VAAS)): could not be included in this review (see notes) SBP, DBP, HR: post‐test scores |
|
| Notes | State anxiety was measured before the music intervention, but not immediately after the music intervention. The post‐test was administered after the surgery. Therefore, this data could not be included. VAAS was administered before and immediately after the music intervention. However, because of insufficient data reporting, this outcome could not be included in this review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quotes: "The first 2 patients were assigned to the experimental group, and the third patient to the control group. This pattern was continued until 24 patients were enrolled." |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Gaberson 1995.
| Methods | RCT 3‐arm parallel group design |
|
| Participants | Adult patients scheduled for surgical procedures Type of surgery: general, orthopedic, gynaecologic, ophthalmic, otolaryngologic, and dental surgery (number of participants per type of surgery not specified) Total N randomized:46 (31 included in this review) N randomized to music group: 16 N randomized to humorous distraction group: 15 (not included in this review) N randomized to control group: 15 N analysed in music group: 16 N analysed in humorous distraction group:15 (not included in this review) N analysed in control group: 15 Mean age: 47.07 Sex: 27 (59%) females, 19 (41%) males Ethnicity: Not reported Setting: Inpatient Country: USA |
|
| Interventions | Three study groups: 1. Music group: listening to pre‐recorded music 2. Humorous distraction group: listening to a humorous tape 3. Control group: received no auditory distraction during the waiting period Music provided: An audiotape of slow, quiet, instrumental music (e.g., Omni Suite by Steven Bergman) Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (VAS): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each research assistant randomly assigned subjects by lottery to one of three groups" |
| Allocation concealment (selection bias) | Low risk | Draw by lots ensured allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for this study |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. This study was supported by an AORN Nurse Scientist Grant and a Duquesne University, Pittsburgh, Supplemental Faculty Development Grant. |
Ganidagli 2005.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients scheduled for surgical procedures Type of surgery: septorhinoplastic surgery Total N randomized:54 N randomized to music group: 28 N randomized to control group: 26 N analysed in music group: 25 N analysed in control group: 25 Mean age: 30 Sex: 21 (42%) females, 29 (58%) males Ethnicity: Not reported Setting: Inpatient Country: Turkey |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music through headphone 2. Control group: listening to a blank cassette or CD through headphone Music provided: Patients brought their own music Number of sessions: 1 Length of sessions: 50 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Observer’s Assessment of Alertness/Sedation Scales, Bispectral Index): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “they were assigned using a table of random numbers, to receive either music (music group) or no music (control group)" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants was not possible. Personnel were blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | This study did not address any subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | The outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 7 %(n = 4). Three patients from the music group and one patient from the control group were excluded from the study because of technical problems related to the music player. |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Guo 2005.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adults patients scheduled for laparoscopic surgery Type of surgery: laparoscopic surgery Total N randomized: 93 N randomized to music group: 48 N randomized to control group: 45 N analysed in music group: 48 N analysed in control group: 45 Mean age: 40.80 Sex: 54 (58%) females, 39 (42%) males Ethnicity: Not reported Setting: Not reported Country: China |
|
| Interventions | Two study groups: 1. Music group: listening to preferred music through headphone 2. Control group: wearing headphone without music Music provided: participants selected from six types of pre‐recorded music (classical music, light music, pop music, folk music, folk songs, and opera). Number of sessions: 1 Length of sessions: 30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): post‐test score HR, SBP, DBP, skin conductivity response, salivary cortisol: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants could not be blinded. Personnel were blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Outcome assessors were blinded by use of headphones in the control group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 7% (n = 7). Seven patients were excluded due to changing surgery, refusing to continue the study and environmental interference. Exact number of subject loss from each group is not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Hook 2008.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients undergoing surgery Type of surgery: Not specified Total N randomized: 108 N randomized to music group: 54 N randomized to control group: 54 N analysed in music group: 51 N analysed in control group: 51 Mean age: 40.3 Sex: 108 (100%) females, 0 males Ethnicity: 100% Malaysian Setting: Inpatient Country: Malaysia |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: standard care Music provided: Participants selected from Western, Malay or Chinese music that the medical staff had recorded. All music has a tempo of 60‐80 bpm Number of sessions: 8 Length of sessions: 30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI, Visual Analogue Scale for Anxiety (VASA)): Only VASA post‐test scores are included in this review (see notes) | |
| Notes | Both VASA and STAI were used to measure anxiety. But STAI post‐test scores were obtained after the surgery. VASA data were obtained at the start and the end of the music intervention prior to surgery. Therefore, only VASA data are used in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Subjects were randomly assigned, using the “envelope method,” to either the music therapy group or the control group” |
| Allocation concealment (selection bias) | Low risk | Use of sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study did not address objective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 6% (n = 6) The reasons for the subject loss were not reported. |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. This study was supported by Prince of Songkla University, Thailand. |
Kushnir 2012.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult women undergoing elective cesarean section because of medical reasons Type of surgery: caesarean section Total N randomized: 62 N randomized to music group: 30 N randomized to control group: 32 N analysed in music group: 28 N analysed in control group: 30 Mean age: 32.1 Sex: 60 (100%) females, 0 males Ethnicity: not reported Setting: Inpatient Country: Israel |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: bedrest with no music Music provided: Participants selected from three options: light popular music, light classical music, Israeli songs Number of sessions: 1 Length of sessions: 40 minutes Categorized as music medicine |
|
| Outcomes | Positive mood, negative mood, perceived threat of surgery: not used in this study HR, SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The researchers preprepared sealed envelopes, each containing a card with either "yes" or "no" in equal numbers. Each woman chose a sealed envelope. the women who had the yes card were included in the experimental group, those who had no were included in the control group". |
| Allocation concealment (selection bias) | Low risk | Participants were asked to draw and open a sealed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | The outcome assessor was not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two participants were excluded because of their music selection. Because these two participants were the only ones who selected popular music, the researchers decided to exclude them because analysis per music selection would not be possible with such a small subgroup. |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Lee 2004.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Adults undergoing surgery Type of surgery: cystoscopy, cauterisation or endoscopy Total N randomized: 113 N randomized to music group: 58 N randomized to control group: 55 N analysed in music group: 58 N analysed in control group: 55 Mean age: 51 Sex: 55 (49%) females, 58 (51%) males Ethnicity: 100% Hong Kong Chinese Setting: inpatient Country: China |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: participating in the usual pre‐procedural relaxing activities (e.g., reading or watching television) in the waiting rooms Music provided: participants selected from eastern and western style easy listening music or Chinese pop music Number of sessions: 1 Length of sessions: 20‐40 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): post‐test scores RR, pulse, SBP, DBP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients who had their procedure on Wednesday were assigned to the control group and patients who had their procedure on Thursday were assigned to the music group" |
| Allocation concealment (selection bias) | High risk | Alternate assignment prohibited allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. The study was supported by the Lee Hysan Foundation and grant from Chinese University of Hong Kong |
Lee 2011.
| Methods | RCT 3‐arm parallel group design |
|
| Participants | Adults undergoing surgery Type of surgery: orthopaedics (n = 23, 14%), general (n = 29, 17%), gynaecology (n = 44, 26%), urology (n = 16, 10%), neurosurgery (n = 20, 12%), other (n = 35, 21%) Total N randomized: 180 N randomized to music (headphone) group: 56 N randomized to music (broadcast) group: 66 N randomized to control group: 58 N analysed in music (headphone) group: 48 N analysed in music (broadcast) group: 66 (not used in this study) N analysed in control group: 53 Mean age: 49.36 Sex: 28 (55%) females, 23 (45%) males Ethnicity: not reported; it is likely that the majority of the participants were Taiwanese Setting: inpatient Country: Taiwan |
|
| Interventions | Three study groups: 1. Headphone group: Listening to music through headphone for 10 minutes 2. Broadcast group: Listening to music from an open speaker for 10 minutes 3. Control group: participants were told to rest and relax Music provided: Folk songs or pop music, played at a tempo of 60–80 beats per minute and a volume of 50–55 db Number of sessions: 1 Length of sessions: 10 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Numeric rating scale (NRS): post‐test scores HR and heart rate variability (HRV) (CheckMyHeart handheld HRV device): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random block sampling. Quote: "We applied random table to divide numbers 1–30 to three groups to determine each day of a month to be ‘headphone day,’ ‘broadcast day’ or ‘control day’" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used to assess the subjective outcome |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate 7% (n = 13). Eight patients from the experimental group were excluded due to HRV data incomplete or too much noise (n = 2), being sent to surgery before the end of measurement (n = 3), or refusing to take the measure (n = 3). Five patients from the control group were excluded due to HRV data were incomplete (n = 2) or being sent to surgery before the end of measurement (n = 3). |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Lee 2012.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adults undergoing surgery Type of surgery: Gynaecology (n = 41, 25%), orthopaedics (n = 29, 18%), general (n = 14, 8%), urology (n = 12, 7%), neurosurgery (n = 16, 10%), other (n = 25, 16%) Total N randomized: 161 N randomized to music group: 82 N randomized to control group: 79 N analysed in music group: 76 N analysed in control group: 64 Mean age: 49.63 Sex: 70 (50%) females, 70 (50%) males Ethnicity: Not reported Setting: inpatient Country: Taiwan |
|
| Interventions | Two study groups: 1. Music group: listening to10‐min session of music through headphones 2. Control group: receiving the VAS and HR measurements by the researcher at a 10‐min interval without a music intervention. Music provided: Patients selected from five kinds of music (folk songs or pop music), played at a tempo of 60–80 beats per minute and a volume of 50–55 db Number of sessions: 1 Length of sessions: 10 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (NRS): post‐test scores HR, HRV (CheckMyHeart): post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: “We assigned participants to groups using birthdays, placing those with even birth dates in the experimental group and those with odd birth dates in the control group.” |
| Allocation concealment (selection bias) | High risk | Systematic form of group allocation based on date of birth prevented allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used to assess the subjective outcome |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | HR measurement were obtained by CheckMyHeart HRV device. Unclear if outcome assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate: 12% (n = 19). Six patients from the experimental group were excluded due to HRV data incomplete or too much noise (n = 4), or being sent to surgery before the end of measurement (n = 2). Thirteen patients from the control group were excluded due to HRV data incomplete or too much noise (n = 7), being sent to surgery before the end of measurement (n = 4), or refusing to take the measure (n = 2). |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. There was no external financial support for this research |
Li 2004.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients undergoing surgery Diagnosis: gastric cancer Total N randomized: 60 N randomized to music group: 30 N randomized to control group: 30 N analysed in music group: 30 N analysed in control group: 30 Mean age: Not reported Sex: 23(38%) females, 37 (62%) males Ethnicity: Not reported Setting: Inpatient Country: China |
|
| Interventions | Two study groups: 1. Music group: listening to pre‐recorded music 2. Control group: receiving verbal support (explanation, guidance, encouragement and comfort) Music provided: Researcher‐selected Chinese classical music Number of sessions: 8 Length of sessions: 20‐30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Zung Self‐Rating Anxiety Scale (SAS)): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of participants was not possible. Blinding of personnel was not reported |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used to assess the subjective outcome |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Lin 2011.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adults undergoing surgery Type of surgery: Spinal surgery Total N randomized: 60 N randomized to music group: 30 N randomized to control group: 30 N analysed in music group: 30 N analysed in control group: 30 Mean age: 62.18 Sex: 29 (49.3%) females, 31 (51.7%) males Ethnicity: Not reported Setting: Inpatient Country: Taiwan |
|
| Interventions | Two study groups: 1. Music group: listening to preferred music through headphones 2. Control group: resting in bed undisturbed while the environment was kept quiet Music provided: Patients selected preferred music from Chinese pop music, classical music, nature sounds and sacred music that researchers provided. All music has a tempo between 6‐ and 72 beats per minute. Number of sessions: 4 sessions with measurements before and after each music session (evening before surgery, one hour before surgery, afternoon of first post‐operative day, and second post‐operative days). We used the one hour pre‐op time point for this review. Length of sessions: 30 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (VAS): post‐test score Pulse, DBP, SBP: post‐test score |
|
| Notes | Both STAI and VAS were used to measure anxiety but only VAS data are used because the STAI post‐test was administered after the surgery. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "All patients scheduled for surgery on Tuesdays and Thursdays were assigned to the study group, while those scheduled for surgery on Wednesdays and Fridays were assigned to the control group." |
| Allocation concealment (selection bias) | High risk | Systematic form of group allocation prevented allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for the subjective outcome |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases. This study was financially sponsored by the Taipei Veterans General Hospital (Grant No.V95B2‐004). |
Miluk‐Kolasa 1996.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Adult patients awaiting non‐orthopaedic surgeries Diagnosis: Laryngological surgery (n = 79, 79%), varicectomy (n = 21, 21%) Total N randomized: 100 N randomized to music group: 50 N randomized to control group: 50 N analysed in music group: 50 N analysed in control group: 50 Mean age: range between 20‐60 Sex: 28 (28%) females, 72 (72%) males Ethnicity: Not reported Setting: Inpatient Country: Poland |
|
| Interventions | Two study groups: 1. Music group: listening to individually composed music programs from Walkman‐type tape players. 2. Control group: standard care Music provided: Not reported Number of sessions: 1 Length of sessions: 1 hour Categorized as music medicine |
|
| Outcomes | SBP, DBP, HR, cardiac output, stroke volume, temperature, and glucose count: only percentage change scores are reported. These cannot be combined with post‐test/change scores in the meta‐analysis and therefore results are only presented in the narrative. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization method is not reported. Quote: "Subjects were randomly assigned to either group C or Group M" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | This study did not address any subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Outcomes were measured with electronic equipment. It is unclear if outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Miluk‐Kolasa 2002.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Patients awaiting for the crural varicectomy or laryngological surgeries Type of surgery: crural varicectomy (n = 19, 21%) or laryngological surgery (n = 70, 79%) Total N randomized: 89 N randomized to music group: 45 N randomized to control group: 44 N analysed in music group: 45 N analysed in control group: 44 Mean age: 40 Sex: 27 (30%) females, 62 (70%) males Ethnicity: Not reported Setting: Inpatient Country: Poland |
|
| Interventions | Two study groups: 1. Music group: listening to the music for 60 minutes 2. Control group: standard care Music provided: Not reported Number of sessions: 1 Length of sessions: 60 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization method was not reported. Quote: "Patients were allotted to groups at random" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | This study does not address objective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Ni 2011.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Adult patients admitted to outpatient surgery Type of surgery: neurosurgery (n = 29, 17%), obstetrics and gynaecology (n = 32, 7%), general clinic (n = 19, 11.1%), ear ‐ nose ‐ throat (n = 13, 7.6%), urology (n = 14, 8.2%), plastic surgery (n = 61, 35.7%), cardiovascular (n = 3, 1.8%) Total N randomized: 174 N randomized to music group: 87 N randomized to control group: 87 N analysed in music group: 86 N analysed in control group: 86 Mean age: 40.9 (11.8) Sex: 112 (65%) females, 60 (35%) males Ethnicity: Not reported Setting: Outpatient Country: Taiwan |
|
| Interventions | Two study groups: 1. Music group: listening to the music for 20 minutes via headphones 2. Control group: standard care Music provided: Investigator‐selected mini library of soothing popular Chinese and Taiwanese pop songs (low‐tone, slow rhythm ballads only). Participants selected music from this library Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | STAI: change scores HR, SBP, DBP: change scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer‐generated permuted block randomization was used to assign participants to either experimental or control group" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for the subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | High risk | Outcome assessor was not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Authors reported two withdrawals |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Szeto 1999.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Adult patients awaiting elective inpatient surgery Diagnosis: Not reported Total N randomized:12 N randomized to music group: 6 N randomized to control group: 6 N analysed in music group: 6 N analysed in control group: 3 Mean age: 58 Sex: Not reported Ethnicity: Not reported Setting: Inpatient Country: Hong Kong |
|
| Interventions | Two study groups: 1. Music group: listening to self‐selected music for 20 minutes 2. Control group: standard care Music provided: participants selected from slow rhythmical songs: Chinese or Western music. This music was determined to have sedative qualities by a panel of experts Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Chinese version STAI): change scores Tension (Subjective Unit of Tension Scale): change scores SBP, DBP: change scores |
|
| Notes | JB computed change scores because of large pre‐test differences | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: 33% (n = 3). Three patients from the control group could not complete the procedure, as they had to be sent to surgery |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Winter 1994.
| Methods | RCT 2‐arm parallel group design |
|
| Participants | Women undergoing elective gynaecological procedures Types of surgery: exploratory laparoscopies, laparoscopic tubal ligation, ovarian cysts excision, and intrauterine device removal Total N randomized: 50 N randomized to music group: 31 N randomized to control group: 19 N analysed in music group: 31 N analysed in control group: 19 Mean age: 37 Sex: 50 (100%) females, 0 (0%) males Ethnicity: Not reported Setting: Outpatient Country: USA |
|
| Interventions | Two study groups: 1. Music group: listening to music through headphones 2. Control group: standard care Music provided: Participants were asked to select from Schumann: Quartet for Piano and Strings in E‐Flat Major, Tchaikovsky: Symphony No. 6 in B minor (“Pathetique”), Beethoven: Symphony No. 2 in D Major (op. 36), Johnny Cash’s Greatest Hits, Willie Nelson’s Greatest Hits, The Beatles Part I, The Beatles Part II, Benny Goodman: Small Group 1941‐1945, Johnny Mathis: Better Together, Madonna: True Blue. The Temptations: 26th Anniversary, or The Mamas & The Papas: If You Can Believe Your Eyes Number of sessions: 1 Length of sessions: 50 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (STAI‐S): change scores HR, SBP, DBP: change scores |
|
| Notes | JB computed change scores and SD | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss. |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Yung 2002.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Chinese male surgical patients in an acute general hospital waiting to undergo inpatient surgery for transurethral resection of the prostate (TURP) Total N randomized: 30 (20 included in this review) N randomized to music group: 10 N randomized to nurse present group: 10 (not included in review) N randomized to control group: 10 N analysed in music group: 10 N analysed in nurse present group: 10 (not included in review) N analysed in control group: 10 Mean age: 67.67 Sex: 0 (0%) females, 30 (100%) males Ethnicity: 100% Chinese Setting: Inpatient Country: Hong Kong |
|
| Interventions | Three study groups: 1. Music group: listening to slow rhythm soft music via headphones 2. Nurse present group: A nurse stood with the patients while they were waiting in the holding area. The nurse was present, but there was minimal verbal interaction 3. Control group: No music intervention or nurse present Music provided: participants selected from slow rhythm songs, Chinese slow rhythm songs or Western slow rhythm songs Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Chinese version STAI): change scores HR, SBP, DBP: change scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects were randomly allocated to different conditions." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Self‐report measure was used for subjective outcome. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Yung 2003.
| Methods | CCT 2‐arm parallel group design |
|
| Participants | Patient awaiting urological surgery Type of surgery: TURP; Transurethral resection of the bladder (TURB); Cystolithotripsy; Herniorrhaphy; Laparoscopic cholecystectomy Total N randomized: 66 N randomized to music group: 33 N randomized to control group: 33 N analysed in music group: 33 N analysed in control group: 33 Mean age: 64.68 Sex: 0 (0%) females, 60 (100%) males Ethnicity: 100% Chinese Setting: Inpatient Country: Hong Kong |
|
| Interventions | Two study groups: 1. Music group: listening to music through headphones 2. Control group: standard care Music provided: Participants were given choice of 3 tapes approved by panel of 3 music instructors at the university level. The panel agreed that the music was sedative in that it possessed minimal rhythmic characteristics. Choices included: Chinese instrumental music, Western instrumental music, or Western and Chinese slow songs Number of sessions: 1 Length of sessions: 20 minutes Categorized as music medicine |
|
| Outcomes | Anxiety (Chinese version STAI): post‐test scores HR, RR, AP: post‐test scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were matched by type of operation into a music treatment group or a test control group." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The participants were not blinded. It is unknown whether the personnel were blinded |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | A self‐report measure was used to measure the subjective outcome |
| Blinding of outcome assessment (detection bias) Objective outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Other bias | Low risk | No indication of other biases |
Key to abbreviations:
AP ‐ Arterial pressure; BPM – beats per minute; CABG ‐ Coronary artery bypass graft surgery; CD – Compact disc; CCT ‐ Controlled clinical trial; DBP ‐ Diastolic blood pressure; HR ‐ Heart rate; HRV ‐ Heart rate variability; N ‐ Numbers; RCT – Randomized controlled trial; RR ‐ Respiratory rate; SAS ‐ Self‐Rating Anxiety Scale; SBP ‐ Systolic blood pressure; SD ‐ Standard deviations; TURB ‐ Transurethral resection of the bladder; TURP ‐ Transurethral resection of the prostate; VAS ‐ Visual analogue scale; VAAS ‐ Visual analogue anxiety scale; STAI ‐ State‐Trait Anxiety Inventory for adults
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aldrige 1993 | Not RCT or CCT |
| Aragon 2002 | Does not address preoperative anxiety; post‐test administered after the surgery |
| Arvelo Correa 1985 | No numerical data reported |
| Bansal 2010 | Does not address preoperative anxiety; music intervention provided during surgery |
| Beach 1991 | Insufficient data reporting |
| Beddows 1997 | Insufficient data reporting |
| Behl 1972 | Not RCT or CCT |
| Brunges 2003 | Insufficient data reporting |
| Chetta 1981 | Insufficient data reporting |
| Chu 2004 | Not RCT or CCT |
| Cirina 1994 | Not RCT or CCT |
| Cowan 1991 | Not RCT or CCT |
| Curtis 1987 | Unable to obtain Master's thesis from University |
| Dabu‐Bondoc 2010 | Use of binaural beat instead of music |
| Daub 1988 | Standard deviations not reported. Unable to obtain contact information for authors |
| Erickson 1989 | Insufficient data reporting |
| Gillen 2008 | Not RCT or CCT |
| Haun 2001 | Unclear if the study only included surgical biopsy patients. We contacted the authors but no response was received. As procedural patients (e.g., needle aspiration) are not included in this review, we decided to exclude this study |
| Jarred 2003 | Not population of interest. Participants were family members of surgical patients |
| Johnson 2012 | Did not address preoperative anxiety; post‐test administered after the surgery |
| Kaempf 1989 | Insufficient data reporting |
| Kain 2006 | Insufficient data reporting |
| Kamin 1982 | Insufficient data reporting |
| Kamin 1987 | Insufficient data reporting |
| Koch 1998 | Does not address preoperative anxiety; music intervention provided during surgery |
| Leardi 2007 | Does not address preoperative anxiety; music intervention provided during surgery |
| Lee 2002 | Did not use standardized measures (personal communication) |
| Madson 2010 | Does not address preoperative anxiety; music intervention provided after surgery |
| Miluk‐Kolasa 1994 | Insufficient data reporting |
| Mok 2003 | Does not address preoperative anxiety; music intervention provided during surgery |
| Moss 1987 | Does not address preoperative anxiety; music intervention provided during surgery |
| Murphree 1988 | Not RCT or CCT |
| Nilsson 2009 | Does not address preoperative anxiety; music intervention provided during surgery |
| Nix 1963 | Not RCT or CCT |
| Oyama 1987 | Insufficient data reporting |
| Padmanabhan 2005 | Use of binaural beat instead of music |
| Paradise 2001 | Not RCT or CCT |
| Park 2000 | Not RCT or CCT |
| Peristein 1994 | Unable to obtain master's thesis |
| Phillips 1997 | Insufficient data reporting |
| Robb 1995 | No standard deviations reported. Chief investigator could not provide us with this information |
| Sanderson 1986 | Not RCT or CCT |
| Scheve 2002 | Did not use standardized measures (personal communication) |
| Spintge 1982 | Insufficient data reporting |
| Staples 1993 | Insufficient data reporting |
| Tusek 1999 | Unacceptable allocation method: participants were assigned to the music intervention group based on availability of a CD player |
| Updike 1987 | Not RCT or CCT |
| Walters 1996 | Insufficient data reporting |
| Wang 2002 | Unclear post‐test data reporting. Post‐test values are expressed as percentages of pretest values but it is unclear how the standard deviations were computed |
| Zhan 2008 | Did not address preoperative anxiety; only reported data on postoperative anxiety |
Characteristics of studies awaiting assessment [ordered by study ID]
Berbel 2007.
| Methods | Unknown |
| Participants | Patients awaiting surgery |
| Interventions | Music versus midazolam |
| Outcomes | Preoperative anxiety |
| Notes | Unable to obtain article |
Dwita 2002.
| Methods | RCT |
| Participants | Patients awaiting surgery |
| Interventions | Music |
| Outcomes | Preoperative anxiety |
| Notes | Unable to obtain article |
Differences between protocol and review
The protocol title 'Music for preoperative anxiety' has been revised to 'Music interventions for preoperative anxiety'.
Contributions of authors
Conceiving the review: Cheryl Dileo (CD) and Joke Bradt (JB) Co‐ordinating the review: JB Undertaking manual searches: JB and research assistants Screening search results: JB and Minjung Shim (MS) Organizing retrieval of papers: JB Screening retrieved papers against inclusion criteria: JB and MS Appraising quality of papers: JB and MS Abstracting data from papers: JB and MS Writing to authors of papers for additional information: JB and MS Providing additional data about papers: JB Obtaining and screening data on unpublished studies: JB and MS Data management for the review: JB Entering data into Review Manager (RevMan 5.1): JB and MS RevMan statistical data: JB Other statistical analysis not using RevMan: JB Double entry of data: JB and MS Interpretation of data: JB and CD Statistical inferences: JB Writing the review: JB Securing funding for the review: CD Performing previous work that was the foundation of the present study: JB and CD Guarantor for the review (one author): JB Person responsible for reading and checking review before submission: JB and CD
Sources of support
Internal sources
No sources of support supplied
External sources
-
State of Pennsylvania Formula Fund, USA.
This grant only supported the protocol preparation work for this Cochrane review
Declarations of interest
JB and CD are music therapists.
MS: none known
New
References
References to studies included in this review
Allen 2001 {published data only}
- Allen K, Golden LH, Izzo JL, Ching MI, Forrest A, Niles R, et al. Normalization of hypertensive responses during ambulatory surgical stress by perioperative music. Psychosomatic Medicine 2001;63(3):487‐92. [PUBMED: 1138227] [DOI] [PubMed] [Google Scholar]
Arslan 2008 {published data only}
- Arslan S, Özer N, Özyurt F. Effect of music on preoperative anxiety in men undergoing urogenital surgery. Australian Journal of Advanced Nursing 2008;26(2):46‐54. [dn: 198783205186632] [Google Scholar]
Augustin 1996 {published data only}
- Augustin P, Hains A. Effect of music on ambulatory surgery patients' preoperative anxiety. Association of Perioperative Registered Nurses Journal 1996;63(4):750. [PUBMED: 8660020] [DOI] [PubMed] [Google Scholar]
Bringman 2009 {published data only}
- Bringman H, Giesecke K, Thorne A, Bringman S. Relaxing music as pre‐medication before surgery: A randomised controlled trial. Acta Anaesthesiologica Scandinavica 2009;53(6):759‐64. [PUBMED: 19388893] [DOI] [PubMed] [Google Scholar]
Cassidy 2003 {unpublished data only}
- Cassidy L. The effect of self‐selected music on elective surgical patients’ preoperative anxiety. Master’s thesis. Southern Illinois University at Edwardsville 2003.
Chang 1996 {published data only}
- Chang Y, Hwang SL, Lee MB, Shiu ST, Liao WS. Effects of music therapy on preoperative stress in patients facing open heart surgery. Chinese Psychiatry 1996;10:28‐37. [Google Scholar]
Cooke 2005 {published data only}
- Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. Journal of Advanced Nursing 2005;52(1):47‐55. [PUBMED: 16149980] [DOI] [PubMed] [Google Scholar]
DeMarco 2012 {published data only}
- DeMarco J, Alexander JL, Nehrenz G, Gallagher L. The benefit of music for the reduction of stress and anxiety in patients undergoing elective cosmetic surgery. Music and Medicine 2012;4(1):44‐8. [DOI: 10.1177/1943862111424416] [DOI] [Google Scholar]
Evans 1994 {published data only}
- Evans MM, Rubio PA. Music: a diversionary therapy. Today's OR‐Nurse 1994;16(4):17‐22. [PUBMED: 8066587] [PubMed] [Google Scholar]
Gaberson 1995 {published data only}
- Gaberson K. The effect of humorous and musical distraction of preoperative anxiety. Association of Perioperative Registered Nurses Journal 1995;62(5):784. [PUBMED: 8534077] [DOI] [PubMed] [Google Scholar]
Ganidagli 2005 {published data only}
- Ganidagli S, Cengiz M, Yanik M, Becerik C, Unal B. The effect of music on preoperative sedation and the bispectral index. Anesthesia and Analgesia 2005;101(1):103‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Guo 2005 {published data only}
- Guo J, Wang J. Study on individual music intervention to reduce preoperative anxiety on patients undergoing laparoscopic surgery. Chinese Journal of Nursing 2005;40(7):485‐8. [Google Scholar]
Hook 2008 {published data only}
- Hook L, Sonwathana P, Petpichetchian W. Music therapy with female surgical patients: Effect on anxiety and pain. Thai Journal of Nursing Research 2008;12(4):259‐71. [Google Scholar]
Kushnir 2012 {published data only}
- Kushnir J, Friedman A, Ehrenfeld M, Kushnir T. Coping with preoperative anxiety in cesarean section: Physiological, cognitive and emotional effects of listening to favorite music. Birth 2012;39(2):121‐7. [DOI] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Lee D, Henderson A, Shum D. The effect of music on preprocedural anxiety in Hong Kong Chinese day patients. Journal of Cinical Nursing 2004;13(3):297‐303. [PUBMED: 15009332] [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee KC, Chao YH, Yiin JJ, Chiang PY, Chao YF. Effectiveness of different music‐playing devices for reducing preoperative anxiety: A clinical control study. International Journal of Nursing Studies 2011;48(10):1180‐7. [PUBMED: 21565344] [DOI] [PubMed] [Google Scholar]
Lee 2012 {published data only}
- Lee KC, Chao YH, Yiin JJ, Hsieh HY, Dai WJ, Chao YF. Evidence that music listening reduces preoperative patients' anxiety. Biological Research for Nursing 2012;14(1):78‐84. [PUBMED: 21278165] [DOI] [PubMed] [Google Scholar]
Li 2004 {published data only}
- Li S. Applying Chinese classical music to treat preoperative anxiety of patients with gastric cancer. Chinese Nursing Research 2004;18(3B):471‐2. [Google Scholar]
Lin 2011 {published data only}
- Lin PC, Lin ML, Huang LC, Hsu HC, Lin CC. Music therapy for patients receiving spine surgery. Journal of Clinical Nursing 2011;20:960‐8. [PUBMED: 21320217] [DOI] [PubMed] [Google Scholar]
Miluk‐Kolasa 1996 {published data only}
- Miluk‐Kolasa B, Matejek M, Stupnicki R. The effects of music listening on changes in selected physiological parameters in adult pre‐surgical patients. Journal of Music Therapy 1996;33:208‐18. [1997‐07495‐002] [Google Scholar]
Miluk‐Kolasa 2002 {published data only}
- Miluk‐Kolasa B, Klodecka‐Rozalska, Stupnicki R. The effect of music listening on perioperative anxiety levels in adult surgical patients. Polish Psychological Bulletin 2002;33:55‐60. [2002‐11422‐007] [Google Scholar]
Ni 2011 {published data only}
- Ni CH, Tsai WH, Lee, LM, Kao CC, Chen YC. Minimising preoperative anxiety with music for day surgery patients ‐ a randomised clinical trial. Journal of Clinical Nursing 2011;21:620‐5. [DOI: 10.1111/j.1365-2702.2010.03466.x; PUBMED: 21332853] [DOI] [PubMed] [Google Scholar]
Szeto 1999 {published data only}
- Szeto C, Yung P. Introducing a music programme to reduce preoperative anxiety. British Journal of Theatre Nursing 1999;9(10):455. [PUBMED: 10646381] [DOI] [PubMed] [Google Scholar]
Winter 1994 {published data only}
- Winter MJ, Paskin S, Baker T. Music reduces stress and anxiety of patients in the surgical holding area. Journal of Post Anesthesia Nursing 1994;9(6):340‐43. [PUBMED: 7707258] [PubMed] [Google Scholar]
Yung 2002 {published data only}
- Yung P, Chui‐Kam S, French P, Chan T. A controlled trial of music and pre‐operative anxiety in Chinese men undergoing transurethral resection of the prostate. Journal of Advanced Nursing 2002;39(4):352‐9. [PUBMED: 12139647] [DOI] [PubMed] [Google Scholar]
Yung 2003 {published data only}
- Yung PMB, Kam SC, Lau BWK, Chan TMF. The effect of music in managing preoperative stress for Chinese surgical patients in the operating room holding area: a controlled trial. International Journal of Stress Management 2003;10:64‐74. [2003‐06067‐007] [Google Scholar]
References to studies excluded from this review
Aldrige 1993 {published data only}
- Aldridge K. The use of music to relieve pre‐operational anxiety in children attending day surgery. The Australian Journal of Music Therapy 1993;1:19‐35. [Google Scholar]
Aragon 2002 {published data only}
- Aragon D, Ferris C, Byers JF. The effects of harp music in vascular and thoracic surgical patients. Alternative Therapies in Health and Medicine 2002;8(5):52‐60. [PUBMED: 1223380] [PubMed] [Google Scholar]
Arvelo Correa 1985 {published data only}
- Arvelo Correa EJ, Daniel de Arvelo HE. Music hypnosis in children [Hipnosis musical em niños]. Revista de la Sociedad Médico‐Quirúrgico del Hospital de Emergencia 1985;20(2):71‐4. [Google Scholar]
Bansal 2010 {published data only}
- Bansal P, Kharod U, Patel P, Sanwatsarkar S, Patel H, Kamat H. The effect of music therapy on sedative requirements and haemodynamic parameters in patients under spinal anaesthesia: A prospective study. Journal of Clinical and Diagnostic Research 2002;4(4):2782‐9. [Google Scholar]
Beach 1991 {unpublished data only}
- Beach E, Cross W. The effect of music on preoperative anxiety in children. Master's thesis. Barry University 1991.
Beddows 1997 {published data only}
- Beddows J. Alleviating pre‐operative anxiety in patients: A study. Nursing Standard 1997;11:35‐8. [PUBMED: 9205339] [DOI] [PubMed] [Google Scholar]
Behl 1972 {unpublished data only}
- Behl VR. Effects of sedative music on pre‐operative patients as measured by changes in their blood pressure, heart rate, respirations and maacl scores. Master's thesis. University of Washington 1972.
Brunges 2003 {published data only}
- Brunges M, Avigne G. Clinical innovations. Music therapy for reducing surgical anxiety. Association of Perioperative Registered Nurses Journal 2003;78(5):816‐8. [PUBMED: 14621954] [DOI] [PubMed] [Google Scholar]
Chetta 1981 {published data only}
- Chetta HD. The effect of music and desensitization on preoperative anxiety in children. Journal of Music therapy 1981;18:74‐87. [PUBMED: 10252814] [DOI] [PubMed] [Google Scholar]
Chu 2004 {published data only}
- Chu JJ. Interactive music therapy for preoperative anxiety. The American Journal of Nursing 2004;104(9):72B. [PUBMED: 15105197] 15105197 [Google Scholar]
Cirina 1994 {published data only}
- Cirina C. Effects of sedative music on patient preoperative anxiety. Today's OR Nurse 1994;16(3):15‐8. [PubMed] [Google Scholar]
Cowan 1991 {published data only}
- Cowan DS. Music therapy in the surgical arena. Music Therapy Perspectives 1991;9:42‐5. [PUBMED: 8009576] 8009576 [Google Scholar]
Curtis 1987 {published data only}
- Curtis LD. Music: a method for anxiety reduction in the preoperative patient. Unpublished master's thesis. State University of New York at Buffalo 1987.
Dabu‐Bondoc 2010 {published data only}
- Dabu‐Bondoc S, Vadivelu N, Benson J, Perret D, Kain ZN. Hemispheric synchronized sounds and perioperative analgesic requirements. Anesthesia and Analgesia 2010;110(1):208‐10. [PUBMED: 19861358] [DOI] [PubMed] [Google Scholar]
Daub 1988 {published data only}
- Daub D, Kirschner‐Hermanns R. A study comparing music, Thalamonal and no premedication [Verminderung der preoperative angst. Vergleichende studie zwischen music. Thalamonal und ohne pramedikation]. Der Anaesthesist 37;9:594‐7. [PUBMED: 3056086] [PubMed] [Google Scholar]
Erickson 1989 {unpublished data only}
- Erickson WR. The anxiolytic effects of music in the preoperative environment. Unpublished master's thesis, University of Texas Health Science Center at San Antonio 1989.
Gillen 2008 {published data only}
- Gillen E, Biley F, Allen D. Effects of music listening on adult patients’ pre‐procedural state anxiety in hospital. International Journal of Evidence‐Based Healthcare 2008;6(1):24‐49. [2008‐02471‐003] [DOI] [PubMed] [Google Scholar]
Haun 2001 {published data only}
- Haun M, Mainous R, Looney S. Effect of music on anxiety of women awaiting breast biopsy. Behavioral Medicine 2001;27(3):127‐32. [2002‐13008‐004] [DOI] [PubMed] [Google Scholar]
Jarred 2003 {published data only}
- Jarred J. The effect of live music on anxiety levels of persons waiting in a surgical waiting room as measured by self‐report. Unpublished master's thesis, Florida State University 2003.
Johnson 2012 {published data only}
- Johnson B, Raymond S, Goss J. Perioperative music or headsets to decrease anxiety. Journal of Perianesthesia Nursing 2012;27(3):146‐54 . [PUBMED: 22612884] [DOI] [PubMed] [Google Scholar]
Kaempf 1989 {published data only}
- Kaempf G, Amodei M. The effect of music on anxiety: a research study. Association of Perioperative Registered Nurses Journal 1989;50(1):112. [PUBMED: 2751292] [DOI] [PubMed] [Google Scholar]
Kain 2006 {published data only}
- Kain ZN, Caldwell‐Andrews AA, Krivutza DM, Weinberg ME, Gaal D, Wabg SM, et al. Interactive music therapy as a treatment for preoperative anxiety in children: A randomized controlled trial. Anesthesia and Analgesia 2006;98:1260‐6. [PUBMED: 15105197] [DOI] [PubMed] [Google Scholar]
Kamin 1982 {published data only}
- Kamin A, Kamin H, Spintge R, Droh R. Endocrine effect of anxiolytic music and psychological counseling before surgery. In: Droh R, Spintge R editor(s). Angst, schmerz, music in der anasthesie. Basel: Editiones Roche, 1982:163‐6. [Google Scholar]
Kamin 1987 {published data only}
- Kamin A, Kamin H, Spintge R, Droh R. Musik als Beitrag zur Reduzierung pra‐ und postoperativer Angste in der Anasthesie. In: Spintge R, Droh R editor(s). Musik in der Medizin. Berlin: Springer‐Verlag, 1987. [Google Scholar]
Koch 1998 {published data only}
- Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music. Anesthesiology 1998;89:300‐6. [PUBMED: 9710387] [DOI] [PubMed] [Google Scholar]
Leardi 2007 {published data only}
- Leardi S, Pietroletti R, Angeloni G, Necozione S, Ranalletta G, Gusto B. Randomized clinical trial examining the effect of music therapy in stress response to day surgery. British Journal of Surgery 2007;94(8):943‐7. [PUBMED: 17636513] [DOI] [PubMed] [Google Scholar]
Lee 2002 {unpublished data only}
- Lee J. The effect of music therapy on levels of preoperative anxiety and ease of anesthesia induction in children undergoing surgery. Master's thesis. Temple University 2002.
Madson 2010 {published data only}
- Madson AT, Silverman MJ. The effect of music therapy on relaxation, anxiety, pain perception, and nausea in adult solid organ transplant patients. Journal of Music Therapy 2010;47(3):220‐32. [PUBMED: 21275333] [DOI] [PubMed] [Google Scholar]
Miluk‐Kolasa 1994 {published data only}
- Miluk‐Kolasa B, Obminskil A, Stupnicki R, Golec L. Effects of music treatment on salivary cortisol in patients exposed to pre‐surgical stress. Experimental and Clinical Endocrinology 1994;102:118‐20. [PUBMED: 8056055] [DOI] [PubMed] [Google Scholar]
Mok 2003 {published data only}
- Mok E, Wong KY. Effects of music on patient anxiety. AORN Journal 2003;52:396‐410. [PUBMED: 12619853] [DOI] [PubMed] [Google Scholar]
Moss 1987 {published data only}
- Moss V. The effect of music on anxiety in the surgical patient. Perioperative Nursing Quarterly 1987;3(1):9‐16. [PUBMED: 3645659] [PubMed] [Google Scholar]
Murphree 1988 {unpublished data only}
- Murphree JL. The effect of music therapy on anxiety in preoperative patients. Master’s thesis. Memphis State University 1988.
Nilsson 2009 {published data only}
- Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart and Lung: Journal of Acute and Critical Care 2009;38(3):201‐20. [PUBMED: 19486788] [DOI] [PubMed] [Google Scholar]
Nix 1963 {published data only}
- Nix PJ. Effects of music therapy and personal interaction on the preoperative patient. Unpublished master’s thesis, Loma Linda University 1963.
Oyama 1987 {published data only}
- Oyama T, Sato Y, Kudo T, Spintge R, Droh R. Effect of anxiolytic music on endocrine function in surgical patients. In: Spintge R. Droh R editor(s). Musik in der medizine/Music in Medicine. Berlin: Springer‐Verlag, 1987:169‐174. [Google Scholar]
Padmanabhan 2005 {published data only}
- Padmanabhan R, Hildreth AJ, Laws D. A prospective, randomised, controlled study examining binaural beat audio and pre‐operative anxiety in patients undergoing general anaesthesia for day case surgery. Anaesthesia 2005;60(9):874‐7. [PUBMED: 16115248] [DOI] [PubMed] [Google Scholar]
Paradise 2001 {published data only}
- Paradise CJ. An exploratory study of the effects of music as a preoperative nonpharmacologic anxiolytic in the surgical patient. Unpublished master's thesis, Mount Mary College Yankton, SD.
Park 2000 {published data only}
- Park SH, Park KS. The effects of music therapy on the preoperative anxiety of surgical patients. Journal of Korean Academy of Adult Nursing 2000;12(4):654‐5. [Google Scholar]
Peristein 1994 {published data only}
- Peristein RM. The effect of listening to music on preoperative anxiety in the patient admitted for same day surgery with general anesthesia. Unpublished master’s thesis, Albany Medical Center 1994.
Phillips 1997 {published data only}
- Phillips JR. Effect of preoperative music on anxiety in adult pre‐surgical patients. Master's thesis. University of Kansas 1997.
Robb 1995 {published data only}
- Robb SO, Nichols RJ, Rutan RL, Bishop BL. The effects of music assisted relaxation on preoperative anxiety. Journal of Music Therapy 1995;32:2‐21. [1995‐38255‐001] [Google Scholar]
Sanderson 1986 {published data only}
- Sanderson SK. The effect of music on reducing preoperative anxiety and postoperative pain and anxiety in the recovery room. Unpublished master’s thesis, Florida Sate University.
Scheve 2002 {unpublished data only}
- Scheve AM. The effect of music therapy intervention on pre‐operative anxiety of pediatric patients as measured by self‐report. Master’s thesis. Florida State University 2002.
Spintge 1982 {published data only}
- Spintge R, Droh R. The pre‐operative condition of 1910 patients exposed to anxiolytic music and Rohypnol (flurazepam) before receiving an epidural anesthetic. In: Droh R, Spintge R editor(s). Angst, schmerz, music in der anasthesie. Basel: Editiones Roche, 1982:77‐88. [Google Scholar]
Staples 1993 {unpublished data only}
- Staples SE. The effect of music listening on blood pressure, pulse rate, respiration rate, and anxiety state of patients in the preoperative room. Master's thesis. Florida State University 1993.
Tusek 1999 {published data only}
- Tusek DL, Cwynar R, Cosgrove DM. Effect of guided imagery on length of stay, pain and anxiety in cardiac surgery patients. Journal of Cardiovascular Management 1999;10(2):22‐8. [PUBMED: 10557909] [PubMed] [Google Scholar]
Updike 1987 {published data only}
- Updike P, Charles D. Music Rx: Physiological and emotional responses to taped music programs of preoperative patients awaiting plastic surgery. Annals of Plastic Surgery 1987;19:29‐33. [PUBMED: 3307595] [DOI] [PubMed] [Google Scholar]
Walters 1996 {published data only}
- Walters CL. The psychological and physiological effects of vibrotactile stimulation, via a Somatron, on patients awaiting scheduled gynecological surgery. Journal of Music Therapy 1996;33(4):261‐87. [1997‐03112‐003] [Google Scholar]
Wang 2002 {published data only}
- Wang S, Kulkarni L, Doley J, Kain Z. Music and preoperative anxiety: A randomized controlled study. Ambulatory Anesthesia 2002;94:1489‐94. [PUBMED: 12032013] [DOI] [PubMed] [Google Scholar]
Zhan 2008 {published data only}
- Zhan H, Yang N, He X. Influence of branchiplex anesthesia on analgesia effect by adopting music therapy. Chinese Nursing Research 2008;22(1B):108‐9. [Google Scholar]
References to studies awaiting assessment
Berbel 2007 {published data only}
- Berbel P, Moix J, Quintana S. Music versus diazepam to reduce preoperative anxiety: a randomized controlled clinical trial [Estudio comparativo de la eficacia de la musica frente al diazepam para disminuir la ansiedad prequiruirgica: un ensayo clinico controlado y aleatorizado]. Revista Espanola de Anestesiologia y Reanimacion 2007;54(6):355‐8. [PubMed] [Google Scholar]
Dwita 2002 {published data only}
- Dwita A, Natalia J. Effect of music on anxiety in patients undergoing cataract surgery [Pengaruh Musik Terhadap Kecemasan Penderita Katark Menjelang Operasi ]. ANIMA Indonesian Psychological Journal 2002;17(2):179‐95. [Google Scholar]
Additional references
Agarwal 2005
- Agarwal A, Ranjan R, Dhiraaj A, Lakra A, Kumar M, Singh U. Acupressure for prevention of pre‐operative anxiety:A prospective, randomised, placebo controlled study. Anaesthesia 2005;60:978–81. [DOI] [PubMed] [Google Scholar]
Beccaloni 2011
- Beccaloni AM. The medicine of music: A systematic approach for adoption into perianesthesia practice. Journal of Perianesthesia Nursing 2011;26(5):323‐30. [DOI] [PubMed] [Google Scholar]
Bolwerk 1990
- Bolwerk C. Effects of relaxing music on state anxiety in myocardial infarction patients. Critical Nurse Quarterly 1990;13:63‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bradt 2009
- Bradt J, Dileo C. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006577.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2010
- Bradt J, Dileo C, Grocke D. Music interventions for mechanically ventilated patients. Cochrane Database of Systematic Reviews 2010, Issue 12. [DOI: 10.1002/14651858.CD006902.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2011
- Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD006911.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2012
- Bradt J. Randomized controlled trials in music therapy: Guidelines for design and implementation. Journal of Music Therapy 2012;49(2):120‐49. [DOI] [PubMed] [Google Scholar]
Cepeda 2006
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004843.pub2] [DOI] [PubMed] [Google Scholar]
Chlan 1998
- Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart and Lung 1998;27(3):169‐76. [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd Edition. Hillsdale, NJ: Lawrence Earlbaum Associates, 1988. [Google Scholar]
Dileo 1999
- Dileo C. A classification model for music and medicine. Applications of Music in Medicine. Silver Spring: National Association for Music Therapy, 1999:1‐6. [Google Scholar]
Dileo 2005
- Dileo CD, Bradt J. Medical music therapy: A meta‐analysis & agenda for future research. Jeffrey Books, 2005. [Google Scholar]
Dileo 2007
- Dileo C, Bradt J. Music therapy: Applications to Stress Management. In: Lehrer PM, Woolfolk RL editor(s). Principles and Practice of Stress Management. 3rd Edition. New York: Guilford Press, 2007. [Google Scholar]
Dileo 2008
- Dileo C, Bradt J, Murphy K. Music for preoperative anxiety. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD006908] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frank 1985
- Frank JM. The effects of music therapy and guided visual imagery on chemotherapy‐induced nausea and vomiting. Oncology Nursing Forum 1985;12(5):47‐52. [MEDLINE: ] [PubMed] [Google Scholar]
Friedman 2007
- Friedman BH. An autonomic flexibility‐neurovisceral integration model of anxiety and cardiac vagal tone. Biological Psychology 2007;74(2):185‐99. [DOI] [PubMed] [Google Scholar]
Hamel 2001
- Hamel WJ. The effects of music intervention on anxiety in patients waiting for cardiac catheterization. Intensive & Critical Care Nursing 2001;17:279‐85. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (Editors). Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. [Available from www.cochrane‐handbook.org] [Google Scholar]
Kain 2000
- Kain ZN, Sevarino F, Alexander GM, Pincus S, Mayes LC. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated‐measures design. Journal of Psychosomatic Research 2000;49:417‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kiecolt‐Glaser 1998
- Kiecolt‐Glaser JK, Page G, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery: perspectives from psychoneuroimmunology. American Psychologist 1998;53(11):1209‐18. [DOI] [PubMed] [Google Scholar]
Lai 2006
- Lai HL, Chen CJ, Peng TC, Chang FM, Chen ML, Huang HY, Chang SC. Randomized controlled trial of music during kangaroo care on perinatal anxiety and preterm infants’ responses. International Journal of Nursing Studies 2006;43:139–46. [DOI] [PubMed] [Google Scholar]
Lee 2005
- Lee O, Chung Y, Chan M, Chan W. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: a pilot study. Journal of Clinical Nursing 2005;14(5):609‐20. [DOI] [PubMed] [Google Scholar]
Leroy 2003
- LeRoy S, Elixson EM, O'Brien P, Tong E, Turpin S, Uzark K. Recommendations for preparing children and adolescents for invasive cardiac procedures. Circulation 2003;108:2250. [DOI] [PubMed] [Google Scholar]
Maranets 1999
- Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesthesia and Analgesia 1999;89:1346‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
McAuley 2000
- McAuley L, Pham B, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta‐analyses?. Lancet 2000;356:1228‐31. [DOI] [PubMed] [Google Scholar]
Mitchell 2003
- Mitchell M. Patient anxiety and modern elective surgery: a literature review. Journal of Clinical Nursing 2003;12(6):806‐15. [DOI] [PubMed] [Google Scholar]
Nilsson 2008
- Nilsson U. The anxiety‐ and pain‐reducing effects of music interventions: a systemic review. AORN Journal 2008;87(4):780–807. [DOI] [PubMed] [Google Scholar]
Norred 2000
- Norred CL. Minimizing preoperative anxiety with alternative caring‐healing therapies. Association of Perioperative Registered Nurses Journal 2000;72(5):838‐40, 842‐3. [DOI] [PubMed] [Google Scholar]
Ozalp 2003
- Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N. Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiologica Scandinavica 2003;47:26‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pelletier 2004
- Pelletier CL. The effect of music on decreasing arousal due to stress: a meta‐analysis. Journal of Music Therapy 2004;41:192‐214. [DOI] [PubMed] [Google Scholar]
Pfaff 1989
- Pfaff VK, Smith KE, Gowan D. The effects of music assisted relaxation on the distress of pediatric cancer patients undergoing bone marrow aspiration. Children's Health Care 1989;18:232‐6. [Google Scholar]
Pittman 2011
- Pittman S, Kridli S. Music intervention and preoperative anxiety: an integrative review. International Nursing Review 2011;58:157‐63. [DOI] [PubMed] [Google Scholar]
RevMan 5.1 [Computer program]
- Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan).Version 5.1 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Robb 2011
- Robb SL, Burns DS, Carpenter JS. Reporting guidelines for music‐based interventions. Music and Medicine 2011;3(4):271‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Annals of Internal Medicine 2010;152(11):1‐8. [DOI] [PubMed] [Google Scholar]
Scott 2004
- Scott A. Managing anxiety in ICU patients: the role of pre‐operative information provision. Nursing in Critical Care 2004;9(2):72‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sloan 2005
- Sloan JA. Assessing the minimally clinically significant difference: scientific considerations, challenges and solutions. Journal of Chronic Obstructive Pulmonary Disease 2005;2(1):57–62. [DOI] [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD. Manual for the State‐Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press, 1983. [Google Scholar]
Standley 1986
- Standley JM. Music research in medical/dental treatment: a meta‐analysis and clinical implications. Journal of Music Therapy 1986;23:56‐122. [DOI] [PubMed] [Google Scholar]
Standley 2000
- Standley JM. Music research in medical treatment. Effectiveness of music therapy procedures: Documentation of research and clinical practice. 3rd Edition. Silver Spring: American Music Therapy Association, 2000:1‐64. [Google Scholar]
Tan 2012
- Tan X, Yowler CJ, Super DM, Fratianne RB. The interplay of preference, familiarity and psychophysical properties in defining relaxing music. Journal of Music Therapy 2012;49(2):150‐79. [DOI] [PubMed] [Google Scholar]
White 1999
- White JM. Effects of relaxing music on cardiac autonomic balance and anxiety after acute myocardial infarction. American Journal of Critical Care 1999;8(4):220‐30. [MEDLINE: ] [PubMed] [Google Scholar]
Wright 2007
- Wright KD, Stewart SH, Finley GA, Buffett‐Jerrott SE. Prevention and intervention strategies to alleviate preoperative anxiety in children: a critical review. Behavior Modification 2007;31(1):52‐79. [DOI] [PubMed] [Google Scholar]


