Abstract
Videoconferencing platforms have recently gained wide attention due to the COVID-19 pandemic, both within and outside of the medical community. This article reviews various applications of online meeting technology to the radiologic community, not only in response to the recent pandemic but also thereafter. Various platform features are outlined and discussed, specifically with respect to collaboration, training, and patient care. Platforms reviewed are GoToMeeting, Microsoft Teams, Skype, WebEx, and Zoom.
Keywords: Collaboration, Radiology, Videoconferencing
1. Introduction
The practice of social distancing and a shift towards working remotely across a gamut of professions have resulted from the global coronavirus disease 2019 (COVID-19) pandemic.1 The capability to remain connected to coworkers despite distance, particularly in a work from home scenario, has been facilitated through the use of online meeting applications.2 Collective efforts and learning from a distance had already gained increased attention in the radiologic community prior to the COVID-19 pandemic.3 It is only natural that radiology departments adjust by incorporating online conferencing software into daily practice during the COVID-19 pandemic, by introducing increased collaboration amongst educational institutions and medical practices in various disparate locations. This manuscript discusses the utility of specific online meeting platforms (e.g., GoToMeeting, WebEx, and Zoom) to several aspects of radiologic workflow including teamwork, training, and patient care. The discussion will be framed to review recent trends in utilization of specific applications as it relates to these categories of radiologic workflow.
2. Definition and major platforms
A webinar, an event in which a group of people have a real time discussion online,4 uses transmitted video and audio signals.5 Webinars can also be presented as replays as well as one-way didactic live content without two-way interaction. The practice has evolved with technology and is now often performed using software that allows users to communicate with audio and/or video as well through text. Additionally, many applications include screen sharing functionality, allowing participants to share information from their individual software applications. Platforms chosen for this review (Zoom, Skype, WebEx, GoToMeeting and Microsoft Teams) were listed by G2.com in March to June 2020 as the top 5 of 10 videoconferencing platforms. G2 scored and ranked platforms based on data incorporated from user reviews, online sources, and social networks.6 Selected online conferencing platforms are summarized below and in Table 1 .The information presented in Table 1 reflects features available as of June 2020.
Table 1.
Summary of select videoconferencing platforms.
| Platform | Package | Max # of participants | Monthly cost (per host) | Screen sharing | Control sharing | Chat feature | Multi-source audio | Recording | Annotation tools | HIPAA compliant | Mobile device compatibility | Desktop compatibility | Time limit |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |
Professional | 150 | $14.00 | ✓ | ✓ | ✓ | ✓ | ✓ |
|
|
|||
| Business | 250 | $19.00 |
|
✓ | |||||||||
| Enterprise | 3000 | Custom rate |
|
||||||||||
 |
Requires Office 365 subscription | 250 | Included w/ Office 365 | ✓ | ✓ | ✓ | ✓ |
|
✓ |
|
|
||
 |
Free | 100 | Free | ✓ |
|
✓ | ✓ |
|
✓ | ✓ |
|
|
24 h |
| Starter | 50 | $14.95 |
|
||||||||||
| Plus | 100 | $19.95 | |||||||||||
| Business | 200 | $29.95 |
|
||||||||||
 |
Basic | 100 | Free | ✓ | ✓ | ✓ | ✓ |
|
✓ |
|
|
40 min | |
| Pro | 100 | $14.00 |
|
24 h | |||||||||
| Business | 300 | $19.99 |
|
||||||||||
| Enterprise | 500 | $19.99 |
|
||||||||||
| Healthcare | $200 (for 10 hosts) |
|
|
✓ |
|
||||||||
 |
50 | Free | ✓ | ✓ | ✓ | Dial in for additional fee |
|
|
|
2.1. GoToMeeting
GoToMeeting by LogMeIn is a videoconferencing platform that offers 3 packages available for purchase. Features of GoToMeeting include high definition video, screen sharing, note taking, recording, and meeting transcription. GoToMeeting is compatible with many desktop programs as well as mobile devices and has no time limit for length of sessions (LogMeIn, Inc., Boston, MA).7
2.2. Microsoft Teams
Microsoft's videoconferencing platform, Microsoft Teams, offers many features including screen sharing, recording, transcription ability, and many more. The suite offers the advantage of being well-integrated with other Microsoft 365 programs like Outlook. Although it does not boast of annotation features, users can easily sync/share meeting content, agendas, and schedules to Outlook and Teams App (Microsoft Corporation, Redmond, WA).8 , 9
2.3. WebEx
Cisco's WebEx is a videoconferencing platform that includes screen sharing, HD video, recording, and annotation. WebEx meeting participants can share their screen without requesting control from the host. WebEx is widely compatible; meetings can be launched from other programs like Microsoft Teams, Slack, Moodle, Canvas, amongst others.10 , 11
2.4. Zoom
Zoom (Zoom Video Communications, Inc., San Jose, CA) is a cloud-based software application designed for online conferencing with text, audio, video and screen sharing, and recording functionality. This application can be operated along a range of devices with internet access including mobile and nonmobile computer operating systems as well as smartphones.12 , 13 Zoom allows for screen sharing without requesting control from the host.
2.5. Skype
Skype (Skype; Microsoft, Redmond, WA) is a type of voice over internet protocol (VoIP) application that can be accessed across myriad devices via the internet ranging from mobile phones to smart watches to computers and even gaming consoles. It allows for communication via audio only or audio and video with instant text messaging capability.14
3. Applications of online conferencing tools
3.1. Collaboration
The use of videoconferencing software presents a valuable opportunity to promote interprofessional communication and teamwork within the radiologic community. By permitting communication between physically distant groups in real time, collaboration can occur not only within the local medical community but also with those outside of it, in particular industry specialists, medical researchers, and basic scientists. Team members can quickly communicate in a way that respects the time of all attendees, requires very little planning, and can save substantial cost and time associated with travel.7Research and departmental seminars can similarly be held, recorded, and distributed for both students, faculty, attendees and non-attendees to later stream, reference, or use for training purposes.7
Moreover, real time discussions and consensus reading of studies can be accomplished using online conferencing platforms. This activity could enhance the quality and depth of the collaborating entities15 that are no longer constrained by geographic limitations. Some institutions have used this technology to conduct clinical trial reviews. Remote “expert” readers at various sites can review clinical study data within real time access to images.7 Collaborative features like polling and breakout rooms, offered by platforms like Zoom, can be enabled to stimulate discussion and peer learning. Breakout rooms allow the host to divide participants into smaller groups, up to fifty.16 Polling participants with either single or multiple choice questions can provide hosts with valuable feedback, and can even be conducted anonymously.17 Thus, by using this technology, field experts that may otherwise be unable to work together due to physical distance can connect and collaborate more readily.
Videoconferencing can also be utilized in the form of virtual peer learning conferences which can be beneficial supplements to traditional audit-based peer review. Under the peer review model, radiologists numerically score peer mistakes to monitor individual performance and competency. Conversely in a peer learning model, numerical scoring is not implemented and individual performance is not graded; cases are reviewed categorically in a way to foster collaborative learning from error.18 In one survey of perceptions of peer review, only 32% of radiologists felt that the in-place peer review model decreased medical error and 46% of radiologists reported that they participated only because it was mandatory.19 Many groups have transitioned from peer review to supplementation with peer learning for these reasons, and to promote collegiality and collaborative learning from error.18 A virtual peer learning program implemented exclusively using videoconferencing, may enhance participation amongst radiologists. Without exclusive use of videoconferencing, physically present participants engage more than remote participants; a standardized experience promotes equal participation and group sharing amongst team members. A virtual peer learning model is also beneficial to radiologists as it demands less than 1 h per month of administrative time. In one example, this approach allowed radiologists, residents, fellows, and medical students from 14 institutions in 10 states to engage in valuable peer feedback, improvement, and learning.20 Furthermore, in order to gain an even wider audience, meetings were recorded and posted via YouTube (Google, San Bruno, CA) for streaming across the globe.18 Considering that videoconferencing is easy to implement, low cost and saves time, its use may attract more participants towards a peer learning approach and help promote a culture of improvement with wide reaching audiences.
3.2. Training
Many aspects of medical education have been affected by the recent COVID-19 pandemic,21 and videoconferencing offers a potential solution to some of these challenges now and in the future. While many medical schools had previously adopted virtual learning for 1st and 2nd year students,22 the recent pandemic highlights the need for similar improvement in other areas of medical education.
Prior to the COVID-19 pandemic, efforts in the use of online conferencing software such as Webex have demonstrated a favorable perception of educational value by preclinical student participants as compared to in person formats. However, at Harvard Medical School, participants noted a perceived decreased quality of communication using Webex compared to live simulation sessions. This may have been related to a relatively decreased availability of viewing angles to the simulation laboratory. Camera placement could potentially provide different (or multiple) angles to mitigate this shortcoming.10
In response to the COVID-19 pandemic, many 3rd and 4th year medical school curricula developed infrastructure for a sudden shift to remote learning. Conferencing platforms were used at some institutions to simulate clinical experiences for students; however, it was uncertain if there was a sufficient volume of simulated online experiences to satisfy a full typical rotation. As a temporary alternative some schools implemented online elective opportunities in the 4th year until the 3rd year rotations recommenced.21 In one example, a completely virtual radiology rotation was successfully designed and implemented for one hundred and eleven medical students. The course, prepared in only two weeks, consisted of both large group didactic lectures in addition to small group sessions. When surveyed, 84% of responding students rated the course as excellent and 95% reported the course allowed them to master core knowledge related to radiology.23 For post-graduate students, videoconferencing is being used in place of in-person teaching and group learning sessions for residents21 for example with Grand Rounds and Morbidity and Mortality conferences. The virtual nature of such meetings provides an accessible forum for a wider audience base including 3rd and 4th year students practicing physical distancing.
Some radiology residency programs are using this method for both mentor-guided image interpretation and formal didactic lectures. “Screen share” features enable attendees (residents) to view the host's (faculty member) picture archiving and communication systems (PACs) screen remotely. Multiple monitors can be shared at once. The collaborative features offered by these applications (Table 1) allow traditional radiology read-out and “hot seat” style case conferences to occur similar to how they would traditionally. Annotation features of some platforms (e.g., Zoom) allow residents to illustrate on the host's screen and can be useful for questions and quizzes.24 Messaging features of some platforms may also allow trainees to post questions or seek further information.
With respect to utility after the COVID-19 pandemic is over, online conferencing software also presents a potential solution to mitigation of the academic radiology community's concerns regarding the possible negative impact on resident education by the burgeoning trend of 24 hour radiology attending coverage.25 Building on former efforts in the utility of remote radiology resident supervision from the early 2000s,26 the Department of Radiology from the Medical College of Wisconsin, has reported promising outcomes in their implementation of Skype into overnight emergency radiology workflow. Enhanced teamwork and the ability to educate were also reported using Skype with an overall impression that the incorporation of online telecommunication software aids in the restoration of balance to the loss of resident autonomy in the growing paradigm shift towards continuous attending radiology coverage.27
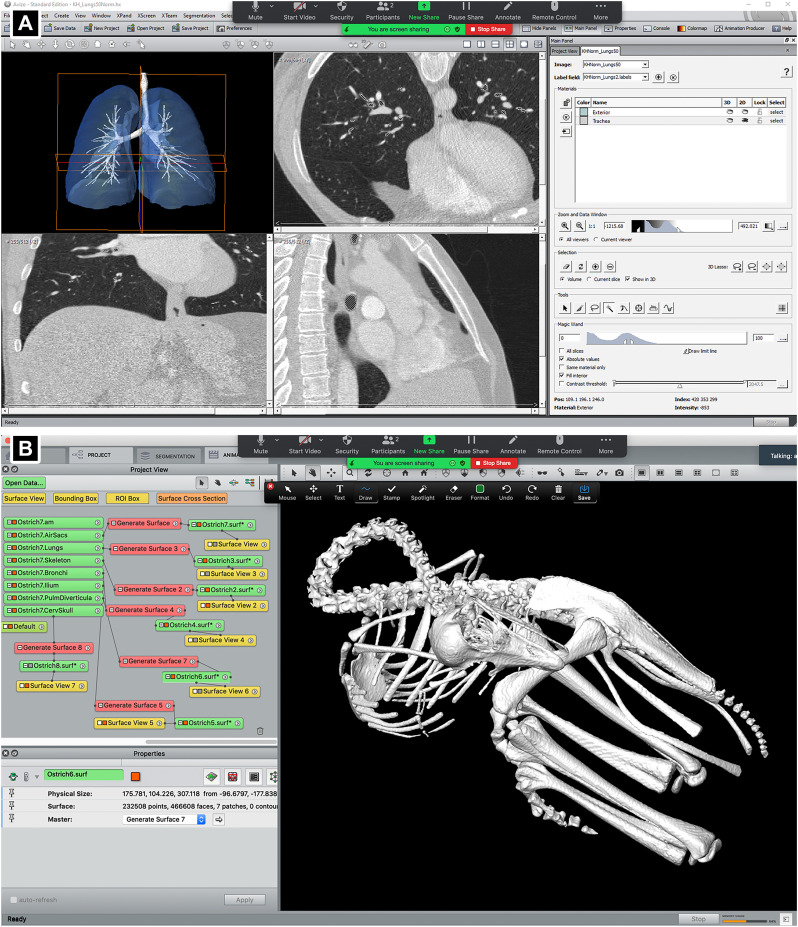
One of the most useful aspects of the videoconferencing programs that can be used for work from home training of medical students, residents, and even other radiologists is the shared screen tool. This has been highly effective in supporting cooperative training partnerships between our radiology department and the Department of Cell Biology and Anatomy given interdepartmental distance and recent COVID-19 related social distancing needs (Fig. 1 ). This can be easily used to teach students, residents, or colleagues how to use cutting-edge three-dimensional (3D) modeling programs for rendering and segmenting surface models from CT and MR image data. Many of these programs, e.g., Mimics, VGSTUDIO, Avizo (Fig. 1) can be challenging to learn, but through various videoconferencing software programs (Table 1), screen sharing, and control sharing can be used to facilitate training. Control sharing permits the instructor to both demonstrate the various steps on how to build and edit a model, as well as manipulate the computer of the student that they are teaching.
Fig. 1.
Screen shots of Zoom during two screen shares (clinical and basic science projects) demonstrating the use of the scientific visualization program Avizo (Thermofisher Scientific, Waltham, MA). A) The Avizo 7.1 segmentation module with a 3D model of an adult human lung and associated axial (top right), coronal (bottom left), and sagittal (bottom right) slices. B) The Avizo 9.1 main GUI with a 3D segmented surface model of a juvenile ostrich skeleton (Struthio camelus), and multiple rendered surface models deselected.
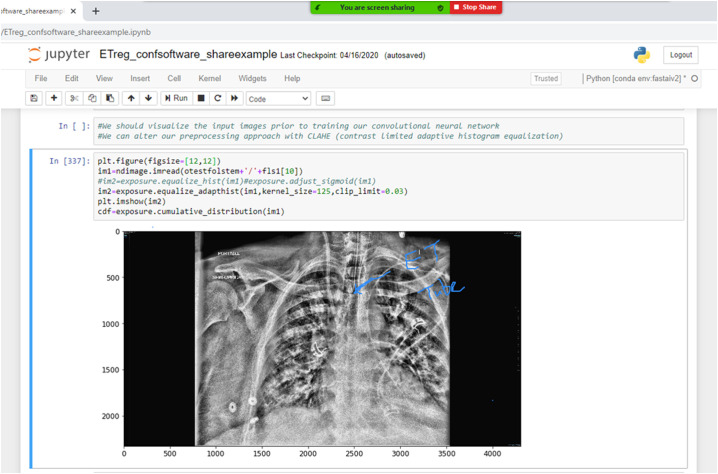
In a similar vein, conferencing software paired with Jupyter notebooks (https://jupyter.org/) can be used to teach basic computer programming techniques as they relate to radiology-focused artificial intelligence application development. Fig. 2 shows a Zoom screenshot of a Jupyter notebook for training a convolutional neural network to detect endotracheal tube position. In this figure, the discussion leader has used Zoom's annotation tools to highlight the endotracheal tube position on a chest radiograph for an intubated patient with COVID-19. The radiograph in the screenshot has been manipulated with Contrast Limited Adaptive Histogram Equalization (CLAHE), and different participants can adjust these parameters in the notebook with control sharing.
Fig. 2.
Example Zoom screenshot of a shared session explaining a Jupyter notebook being developed to investigate support device detection using a convolutional neural network for COVID-19 cases. Annotations can be used to highlight key findings in the images modified with digital processing.
While videoconferencing holds many solutions to the problems medical education faces today during the COVID19 pandemic, its use can continue to be of value in future education models. Geographically isolated radiology residents can attend courses hosted by their program even when they are not rotating at the institution's main location. Similarly, new or rural programs which may lack local instructors to deliver course content can gain access to facilitators not otherwise available to them. In one such example, the majority of residents and facilitators would not have been able to participate in a course without the use of videoconferencing technology. Residents reported this technology did not hinder their ability to discuss topics as a group. However, visual quality and technical difficulties are important to lecture effectiveness28 and therefore must be considered when choosing between platforms.
3.3. Patient care
Incorporation of online conferencing applications into the clinical arena has been an effective tool for radiologists to improve patient care through enhanced connectivity with clinicians.29 In one example, a virtual tumor board was implemented using Microsoft Teams and perceptions were surveyed. The virtual multidisciplinary conference was attended by a wide array of physicians and graduate medical trainees, and radiologic images were easily viewed by all participants at the start by using screen share features.8 The majority of participants preferred a virtual to in-person tumor board, and almost 80% of participants preferred to continue the virtual format even after in-person restrictions are lifted.8 At our institution, Zoom continues to be used for all tumor boards as well as subspecialty interdisciplinary conferences, and we anticipate that its usage will also be favored once physical distancing precautions are relaxed. In another example, investigators successfully employed Skype into virtual radiology rounds. Each session consisted of a micro-lecture and review of patient cases by both clinicians and radiologists. In 89% of cases presented virtually, radiologists responded with an increase in confidence in their diagnosis/interpretation, and in 56% of cases, radiologists revised their report and interpretation. Radiologists reported that clinician input and discussion with the referring clinician to better understand the context of the imaging exam, made accessible by videoconferencing, improved their interpretation of image.30
Another advantage of the use of teleconferencing platforms is to interact with patients and answer their questions while they are having an imaging procedure.31 Currently this activity is performed in person and requires visiting the scanning room. At times this may be inconvenient, inefficient, or not feasible if the imaging suite is at different location.
4. Cautionary considerations
Virtual platforms have allowed us to connect from afar in much more efficient ways. However, all users, including radiologists, other physicians, and patients, should approach videoconferencing with caution concerning privacy and data sharing. In recent news, Zoom has been criticized for many of its privacy policies. Claims of Zoom selling user data to third parties, such as Facebook, and of “Zoom-bombers” hijacking meetings have received an extensive amount of attention in the media and even by the Federal Bureau of Investigation (FBI).32 While Zoom received most of the scrutiny about privacy, a deeper look reveals little difference between privacy policies of Zoom and that of other platforms. Data collected while videoconferencing, as is routinely done, can potentially be used by platforms to generate consumer profiles and develop facial recognition software.33 Not only is sensitive data at risk for being shared without the knowledge of attendees, but it is also being shared to the platform itself.34 Hijackers can gain access to meeting IDs and passwords causing major disruption to sessions. An even more serious threat, however, are those that enter meetings undetected, gaining access to data presented and to the individual data of the participants. Hackers tend to follow market trends, and with a spike in videoconferencing technology use, a new wave of security threats to this technology is created.35
Experts recommend that users take steps to educate themselves on proper videoconferencing conduct and to ensure privacy. Meeting recordings, most likely accessed from cloud storage servers, have been found on the internet.34 , 35 A highly recommended strategy to mitigate against un-wanted meeting hijackers is to have hosts utilize waiting room features in addition to meeting IDs and high-strength passwords. Some virtual platforms allow users joining the meeting to authenticate prior to joining in an effort to improve security. Links to virtual meetings should be shared with each attendee in a secure fashion, never on social media by either the host or attendees. Experts warn against using consumer-grade software that may lack sufficient privacy tools necessary for professional meetings. Users should update software regularly to ensure the product is always utilizing the most up-to-date privacy and security features.33 It is important to remember, the default software settings are not always configured for highest privacy and may need to be manually changed.35
With respect to patient data and privacy, the Office for Civil Rights at the U.S. Department of Health and Human Services has modified Health Insurance Portability and Accountability Act (HIPAA) enforcement policies in alignment with the use of telehealth services during the COVID-19 pandemic. The office has chosen not to “impose penalties for noncompliance with the regulatory requirements under the HIPAA Rules against covered health care providers in connection with the good faith provision of telehealth during the COVID-19 nationwide emergency”.36 With this notice, it explicitly mentioned to not use public facing video applications such as Facebook Live (Facebook, Menlo Park, CA) and TikTok (ByteDance, Ltd., Haidian District, Beijing, China), in the provision of telehealth. However, a number of vendors (including the ones mentioned here) provide HIPAA-compliant video communication and will enter into a Business Associate Agreement. Business Associate Agreements are important to create a bond of liability that binds two parties and should be established with anyone who maintains or transmits Personal Health Information (PHI). All providers should inform patients if their chosen platform does not meet HIPAA compliance and may put his/her PHI at risk during a telehealth visit.
5. Conclusion
The practice of radiology is defined by a technologically driven communicative partnership with other healthcare professionals as well as patients. With the variety of online conferencing software available, there is opportunity to enhance cooperative efforts, and there is potential to capitalize on the benefits of virtual platforms for radiologic teamwork, training and patient care that were implemented during physical distancing requirements in 2020 and 2021.
Funding information
None.
Notation of prior abstract publication/presentation
None.
Declaration of competing interest
None.
References
- 1.Coronavirus disease 2019 (COVID-19) 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
- 2.Gonzales-Zamora J.A., Alave J., De Lima-Corvino D.F., Fernandez A. Videoconferences of Infectious Diseases: an educational tool that transcends borders. A useful tool also for the current COVID-19 pandemic. Infez Med. 2020;28(2):135–138. Ahead of print Jun 1. [PubMed] [Google Scholar]
- 3.Gupta S., Johnson E.M., Peacock J.G., et al. Radiology, mobile devices, and internet of things (IoT) J Digit Imaging. Jan 2 2020 doi: 10.1007/s10278-019-00311-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webinar Updated November 24. 2020. https://dictionary.cambridge.org/us/dictionary/english/webinar
- 5.Videoconferencing 2020. https://www.merriam-webster.com/dictionary/videoconferencing Updated November 24.
- 6.G2 Best video conferencing software. 2020. https://www.g2.com/categories/video-conferencing Updated November 23.
- 7.Poon D.P., Langkals J.W., Giesel F.L., Knopp M.V., von Tengg-Kobligk H. Internet-based videoconferencing and data collaboration for the imaging community. J Comput Assist Tomogr. Nov–Dec 2011;35(6):753–761. doi: 10.1097/RCT.0b013e3182345aeb. [DOI] [PubMed] [Google Scholar]
- 8.Dharmarajan H., Anderson J.L., Kim S., et al. Transition to a virtual multidisciplinary tumor board during the COVID-19 pandemic: University of Pittsburgh experience. Head Neck. 2020;42(6):1310–1316. doi: 10.1002/hed.26195. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Microsoft Teams 2020. https://www.microsoft.com/en-us/microsoft-365/microsoft-teams/group-chat-software
- 10.Hayden E.M., Navedo D.D., Gordon J.A. Web-conferenced simulation sessions: a satisfaction survey of clinical simulation encounters via remote supervision. Telemed J E Health. Sep 2012;18(7):525–529. doi: 10.1089/tmj.2011.0217. [DOI] [PubMed] [Google Scholar]
- 11.Cisco Webex https://www.webex.com/
- 12.Kay D., Pasarica M. Using technology to increase student (and faculty satisfaction with) engagement in medical education. Adv Physiol Educ. 2019;43(3):408–413. doi: 10.1152/advan.00033.2019. [DOI] [PubMed] [Google Scholar]
- 13.About Zoom. https://zoom.us/about
- 14.Armfield N.R., Bradford M., Bradford N.K. The clinical use of Skype—for which patients, with which problems and in which settings? A snapshot review of the literature. Int J Med Inform. Oct 2015;84(10):737–742. doi: 10.1016/j.ijmedinf.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Hofvind S., Lee C.I. Consensus reads: the more sets of eyes interpreting a mammogram, the better for women. Radiology. 2020;295(1):42–43. doi: 10.1148/radiol.2020192746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Enabling breakout rooms. https://support.zoom.us/hc/en-us/articles/206476093-Enabling-breakout-rooms
- 17.Pooling for meetings. https://support.zoom.us/hc/en-us/articles/213756303-Polling-for-meetings
- 18.Chow R.A., Tan N., Henry T.S., Kanne J.P., Sekhar A. Peer learning through multi-institutional case conferences: abdominal and cardiothoracic radiology experience. Acad Radiol. Feb 12 2020 doi: 10.1016/j.acra.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Eisenberg R.L., Cunningham M.L., Siewert B., Kruskal J.B. Survey of faculty perceptions regarding a peer review system. J Am Coll Radiol. Apr 2014;11(4):397–401. doi: 10.1016/j.jacr.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Haas B.M., Mogel G.T., Attaya H.N. Peer learning on a shoe string: success of a distributive model for peer learning in a community radiology practice. Clin Imaging. Feb 2020;59(2):114–118. doi: 10.1016/j.clinimag.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Newman N.A., Lattouf O.M. Coalition for medical education-a call to action: a proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. J Card Surg. 2020;35(6):1174–1175. doi: 10.1111/jocs.14590. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sattar M.U., Palaniappan S., Lokman A., Hassan A., Shah N., Riaz Z. Effects of Virtual Reality training on medical students’ learning motivation and competency. Pak J Med Sci. 2019;35(3):852–857. doi: 10.12669/pjms.35.3.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Durfee S.M., Goldenson R.P., Gill R.R., Rincon S.P., Flower E., Avery L.L. Medical student education roadblock due to COVID-19: virtual radiology core clerkship to the rescue. Acad Radiol. 2020;27(10):1461–1466. doi: 10.1016/j.acra.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li C.H., Rajamohan A.G., Acharya P.T., et al. Virtual read-out: radiology education for the 21st century during the COVID-19 pandemic. Acad Radiol. 2020;27(6):872–881. doi: 10.1016/j.acra.2020.04.028. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruno M.A., Duncan J.R., Bierhals A.J., Tappouni R. Overnight resident versus 24-hour attending radiologist coverage in academic medical centers. Radiology. 2018;289(3):809–813. doi: 10.1148/radiol.2018180690. Dec. [DOI] [PubMed] [Google Scholar]
- 26.Steckel R.J., Batra P., Goldin J.G., Zucker M., Sayre J.W., Johnson S.L. Supervision of residents by faculty radiologists using home workstations. Emerg Radiol. Dec 2003;10(3):121–125. doi: 10.1007/s10140-003-0283-6. [DOI] [PubMed] [Google Scholar]
- 27.Vagvala S.H., Tolat P.P., Hohenwalter M.D., Duvnjak P. Skype as a tool for resident education on call. J Am Coll Radiol. 2020;17(1 Pt A):75–77. doi: 10.1016/j.jacr.2019.08.012. Jan. [DOI] [PubMed] [Google Scholar]
- 28.O’Regan K., Marsden P., Sayers G., et al. Videoconferencing of a national program for residents on evidence-based practice: early performance evaluation. J Am Coll Radiol. 2010;7(2):138–145. doi: 10.1016/j.jacr.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Fefferman N.R., Strubel N.A., Prithiani C., Chakravarti S., Caprio M., Recht M.P. Virtual radiology rounds: adding value in the digital era. Pediatr Radiol. 2016;46(12):1645–1650. doi: 10.1007/s00247-016-3675-y. Nov. [DOI] [PubMed] [Google Scholar]
- 30.Zember J., Saul D., Delgado J., Boyer D., Reid J. Radiology rounds in the intensive care units through a telepresence model. J Am Coll Radiol. 2018;15(11):1655–1657. doi: 10.1016/j.jacr.2018.06.014. Nov. [DOI] [PubMed] [Google Scholar]
- 31.Shailam R., Botwin A., Stout M., Gee M.S. Real-time electronic dashboard technology and its use to improve pediatric radiology workflow. Curr Probl Diagn Radiol. Jan-Feb 2018;47(1):3–5. doi: 10.1067/j.cpradiol.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Fung B IR IR. Zoom, the Video Conferencing App Everyone is Using, Faces Questions Over Privacy. 2020.
- 33.It's not just Zoom: Google Meet, Microsoft Teams, and Webex have privacy issues, too. 2020. https://www.consumerreports.org/video-conferencing-services/videoconferencing-privacy-issues-google-microsoft-webex/ Updated November 24.
- 34.Dealing with privacy issues in your next video conference. 2020. https://www.casamo.com/dealing-with-privacy-issues-in-your-next-video-conference/ Updated November 23.
- 35.Do's and don'ts of videoconferencing security. 2020. https://www.computerworld.com/article/3535924/do-s-and-don-ts-of-videoconferencing-security.html Updated April 7.
- 36.Notifiication of enforcement discreition for telehealth remort communications during the COVID-19 nationwide public health emergency. 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Updated March 30.