Abstract
Background
In industrialised countries injuries (including burns, poisoning or drowning) are the leading cause of childhood death and steep social gradients exist in child injury mortality and morbidity. The majority of injuries in pre‐school children occur at home but there is little meta‐analytic evidence that child home safety interventions reduce injury rates or improve a range of safety practices, and little evidence on their effect by social group.
Objectives
We evaluated the effectiveness of home safety education, with or without the provision of low cost, discounted or free equipment (hereafter referred to as home safety interventions), in reducing child injury rates or increasing home safety practices and whether the effect varied by social group.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2009, Issue 2) in The Cochrane Library, MEDLINE (Ovid), EMBASE (Ovid), PsycINFO (Ovid), ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED), ISI Web of Science: Social Sciences Citation Index (SSCI), ISI Web of Science: Conference Proceedings Citation Index‐ Science (CPCI‐S), CINAHL (EBSCO) and DARE (2009, Issue 2) in The Cochrane Library. We also searched websites and conference proceedings and searched the bibliographies of relevant studies and previously published reviews. We contacted authors of included studies as well as relevant organisations. The most recent search for trials was May 2009.
Selection criteria
Randomised controlled trials (RCTs), non‐randomised controlled trials and controlled before and after (CBA) studies where home safety education with or without the provision of safety equipment was provided to those aged 19 years and under, and which reported injury, safety practices or possession of safety equipment.
Data collection and analysis
Two authors independently assessed study quality and extracted data. We attempted to obtain individual participant level data (IPD) for all included studies and summary data and IPD were simultaneously combined in meta‐regressions by social and demographic variables. Pooled incidence rate ratios (IRR) were calculated for injuries which occurred during the studies, and pooled odds ratios were calculated for the uptake of safety equipment or safety practices, with 95% confidence intervals.
Main results
Ninety‐eight studies, involving 2,605,044 people, are included in this review. Fifty‐four studies involving 812,705 people were comparable enough to be included in at least one meta‐analysis. Thirty‐five (65%) studies were RCTs. Nineteen (35%) of the studies included in the meta‐analysis provided IPD.
There was a lack of evidence that home safety interventions reduced rates of thermal injuries or poisoning. There was some evidence that interventions may reduce injury rates after adjusting CBA studies for baseline injury rates (IRR 0.89, 95% CI 0.78 to 1.01). Greater reductions in injury rates were found for interventions delivered in the home (IRR 0.75, 95% CI 0.62 to 0.91), and for those interventions not providing safety equipment (IRR 0.78, 95% CI 0.66 to 0.92).
Home safety interventions were effective in increasing the proportion of families with safe hot tap water temperatures (OR 1.41, 95% CI 1.07 to 1.86), functional smoke alarms (OR 1.81, 95% CI 1.30 to 2.52), a fire escape plan (OR 2.01, 95% CI 1.45 to 2.77), storing medicines (OR 1.53, 95% CI 1.27 to 1.84) and cleaning products (OR 1.55, 95% CI 1.22 to 1.96) out of reach, having syrup of ipecac (OR 3.34, 95% CI 1.50 to 7.44) or poison control centre numbers accessible (OR 3.30, 95% CI 1.70 to 6.39), having fitted stair gates (OR 1.61, 95% CI 1.19 to 2.17), and having socket covers on unused sockets (OR 2.69, 95% CI 1.46 to 4.96).
Interventions providing free, low cost or discounted safety equipment appeared to be more effective in improving some safety practices than those interventions not doing so. There was no consistent evidence that interventions were less effective in families whose children were at greater risk of injury.
Authors' conclusions
Home safety interventions most commonly provided as one‐to‐one, face‐to‐face education, especially with the provision of safety equipment, are effective in increasing a range of safety practices. There is some evidence that such interventions may reduce injury rates, particularly where interventions are provided at home. Conflicting findings regarding interventions providing safety equipment on safety practices and injury outcomes are likely to be explained by two large studies; one clinic‐based study provided equipment but did not reduce injury rates and one school‐based study did not provide equipment but did demonstrate a significant reduction in injury rates. There was no consistent evidence that home safety education, with or without the provision of safety equipment, was less effective in those participants at greater risk of injury. Further studies are still required to confirm these findings with respect to injury rates.
Plain language summary
Home safety education and providing safety equipment for injury prevention
Injuries are the leading cause of childhood death in industrialised countries. People living in disadvantaged circumstances are at greater risk of injury than those who are more advantaged. This review examined whether home safety education and providing safety equipment reduced injuries and increased safety behaviours and safety equipment use. It also looked at whether home safety education was more or less effective in disadvantaged families. The review authors found 98 studies involving 2,605,044 participants which reported many different safety behaviours, but relatively few studies included information on injuries.
The authors found that home safety interventions provided in the home may reduce injury rates, but more research is needed to confirm this finding. The results often varied between studies but, overall, families who received home safety interventions were more likely to have a safe hot tap water temperature, a working smoke alarm, a fire escape plan, fitted stair gates, socket covers on unused sockets, syrup of ipecac, poison control centre numbers accessible, and to store medicines and cleaning products out of reach of children. The authors found that home safety education was equally effective in the families whose children were at greater risk of injury.
Background
Every day more than 2000 children and teenagers die from unintentional injuries (WHO 2008). In industrialised countries injuries are the leading cause of child death, accounting for 40% of all child deaths between the ages of one to 14 years (Unicef 2001). The relative contribution of home, road traffic, leisure and other injuries varies by age and by country (WHO 2008). In the UK, for children under the age of five years, the majority of fatal and non‐fatal injuries occur in the home (Morrison 1999; ONS 2009). For older children, most fatal injuries occur as a result of a road traffic injury (ONS 2009), but injuries occurring at home account for 40% of medically attended injuries in five to nine year olds and 25% in 10 to 14 year olds (Morrison 1999).
Children's risk of injury is varied by a range of factors. These include age, gender, socioeconomic disadvantage, family type and size, maternal age, maternal educational level, ethnic group and neighbourhood of residence. The risk of home injury is greater amongst younger children than older children (Morrison 1999; ONS 2009; Roberts 1998), with the relationship between injury risk and age varying with the mechanism of injury (Roberts 1998). Boys have consistently been found to be at higher risk of injury than girls, with an increasing differential risk with increasing age (ONS 2009; Roberts 1998).
The burden of childhood injuries is greatest in low income countries and, within each country, injuries disproportionately affect children from low income families (WHO 2008). There are steep social gradients in injury mortality and morbidity for a range of injury mechanisms (Edwards 2006; Hippisley‐Cox 2002; Lyons 2003; Roberts 1996a; Roberts 1997). Other proxy indicators of disadvantage such as housing tenure (Alwash 1998; Kendrick 2005b), parental unemployment (Alwash 1998; Pomerantz 2001), income levels (Pomerantz 2001) and overcrowding (Alwash 1998) have also been found to be associated with child injury. Some work examining the effect of neighbourhood of residence has found a small but significant effect of living in a deprived neighbourhood that is independent of the characteristics of people living within neighbourhoods (Cubbin 2000b; Haynes 2003; Reading 1999; Reimers 2005).
The majority of studies examining the relationship between maternal age and child injury risk have found a greater risk of injury in children from families with younger rather than older mothers (Alwash 1998; Bijur 1988a; Reading 1999; Scholer 1999; Wicklund 1984). Children from single parent and step parent families have consistently been shown to be at higher risk of injury than those from two (natural) parent families (O'Connor 2000; Overpeck 1997; Reading 1999; Wadsworth 1983). Those children in larger families, especially where there are more older and fewer younger siblings, have been found to be at greater risk (Bijur 1988b; Reading 1999) as have those in families with lower levels of (usually maternal) education (Pomerantz 2001; Scholer 1999; Wicklund 1984). There are conflicting findings regarding the relationship between ethnicity and child injury rates. In the UK, the Health Survey for England (Erens 2001) and an ecological study of fracture clinic attendances and hospital admissions for child injury (Tobin 2002) found lower injury rates amongst South Asian groups, whilst a recent literature review of road traffic accident involvement of children from ethnic minorities suggests that Asian children may experience a higher risk of child pedestrian injury than their non‐Asian counterparts (DETR 2001). Conflicting findings have also emerged from US studies (Cubbin 2000a; Overpeck 1997; Pomerantz 2001).
Over recent years a series of systematic reviews have been undertaken examining the effect of interventions to reduce unintentional injuries amongst children, many of which report interventions aimed at reducing home injuries (DiGuiseppi 2000; DiGuiseppi 2001; Dowswell 1996; Elkan 2000; HIPRC 2005b; HIPRC 2005c; HIPRC 2005d; HIPRC 2005e; HIPRC 2005f; Kendrick 1994; Klassen 2000; Nilsen 2004; Pearson 2009; Pless 1993; Popay 1993; Roberts 1996b; Speller 1995; Spinks 2004; Spinks 2005; Ta 2006; Towner 1993; Towner 1996; Towner 2001; Towner 2002; Turner 2004; Turner 2011; Warda 1999). These have concluded that home safety education and the provision of safety equipment can be effective in increasing some, but not all, safety practices, including safety equipment possession, but that there is a paucity of evidence relating to the effect of such interventions in reducing injury rates. Evidence from observational studies demonstrates that families of children attending hospital following a baby walker related stairway fall were significantly less likely to own a stair gate than community controls (Elkington 1999); families of children attending hospital following a poisoning incident were significantly less likely to store poisonous substances safely than families of children attending hospital for reasons other than poisoning (Azizi 1994); and families of children attending accident and emergency (A&E) departments following a burn or scald were less likely to be safe for a range of practices related to burn and scald prevention than families of children attending A&E without a burn or scald (Petridou 1998). In addition, several observational studies have reported a lower risk of death in homes with smoke alarms than without (DiGuiseppi 1998; Marshall 1998; Runyan 1992). Few meta‐analyses have been undertaken in this area (DiGuiseppi 2000; DiGuiseppi 2001; Elkan 2000; Roberts 1996b). Two of these examined the effect of multi‐faceted home visiting programmes aimed at improving a range of maternal and child health outcomes, and both found that such programmes reduced childhood injuries (Elkan 2000; Roberts 1996b). The third examined the effect of interventions to increase smoke alarm ownership and found a non‐significant effect of counselling and educational interventions on owning an alarm or having a functional alarm. However, they did find a significant effect of interventions delivered during child health surveillance on either alarm ownership or having a functional alarm (DiGuiseppi 2001). The fourth examined the effect of interventions delivered in a clinical setting to increase smoke alarm ownership, promote a safe hot tap water temperature and to 'child proof' the home (DiGuiseppi 2000) and found interventions delivered in a clinical setting were effective in promoting a safe hot tap water temperature and in increasing smoke alarm ownership. In addition, intervention group families were 1.8 times more likely to store cleaning agents safely (95% CI or P value not reported). Only two of the studies included in this review reported injury outcomes and neither found that the intervention resulted in a significant reduction in injury occurrence. The review concluded that clinical counselling had little effect on most home safety practices designed to child proof the home and that the evidence about the impact of counselling on childhood injuries is limited. There is, therefore, a lack of evidence quantifying the effect of home safety education on a range of home safety practices and on childhood injury rates.
Concern has been expressed that educational interventions may either not address inequalities in childhood injury or may actually widen existing inequalities (Kendrick 2000; Towner 2005; van Weeghal 1997). This may occur either through inequalities in access to, uptake of, or differential effectiveness of interventions between social groups. Two systematic reviews specifically addressing social deprivation and childhood injury (Dowswell 2002; Mackay 1999) concluded that very few studies examined the impact of interventions in different social groups. A third review addressing inequalities in child injury by age, gender, social and economic factors, culture and ethnicity, place and specific vulnerable groups (Towner 2005) concluded that few intervention studies have explicitly addressed inequalities, and even fewer have attempted to take account of inequalities in the design and to report on the effect of the intervention in relation to these inequalities. This lack of evidence makes it difficult for policy makers and those designing and delivering interventions to know how best to design and deliver home safety interventions to increase home safety, reduce childhood injuries and address inequalities in child injury rates (Dowswell 2002).
Why it is important to do this review
At present none of the systematic reviews or the small number of meta‐analyses that have been published in the field of childhood home injury prevention have examined the effectiveness of such interventions by social group. As few injury prevention studies are large enough to have sufficient power for a subgroup analysis to adequately address this question, this is an ideal research question to be addressed through meta‐analysis. Furthermore, as meta‐regression analyses using summary data have limited power, it is also an ideal topic to be addressed by meta‐analyses combining IPD and summary data from published studies.
Objectives
The objectives of the review were to:
evaluate the effectiveness of home safety education, with or without the provision of low cost, discounted or free equipment (hereafter referred to as home safety interventions), in reducing child injury rates or increasing practices aimed at preventing childhood injuries in the home;
evaluate the effect of home safety interventions by social group.
Methods
Criteria for considering studies for this review
Types of studies
Individually and cluster randomised controlled trials (RCTs), non‐randomised controlled trials and controlled before and after (CBA) studies (studies with a concurrent control group which have data collected on outcome measures at baseline and follow‐up) were included.
Types of participants
Children and young people (aged 19 years and under) and their families.
For objective 2, studies were required to either report data on socio‐economic characteristics or have unpublished data on socio‐economic characteristics available for the review. The socio‐economic and demographic characteristics of interest were those previously found to be associated with an increased risk of childhood injury, which were explored in the 2007 version of this review. These included child age, gender, ethnic group, family type (single or two parent), housing tenure and parental unemployment.
Types of interventions
Home safety interventions provided by health or social care professionals, school teachers, lay workers, voluntary or other organisations to individual children or families, or groups of children or families, whose aim is to reduce home injuries or increase home safety practices or use of home safety equipment. Interventions offered in healthcare settings (primary care and secondary care, for example primary care practices, clinics, out‐patient departments, accident and emergency departments, hospital wards), schools and the homes of children and families were included. Interventions involving the provision of free, low cost or discounted safety equipment were included. Community‐based trials with multi‐faceted interventions were only eligible for inclusion if they included individual home safety interventions or group education.
We excluded multi‐faceted home visiting programmes aimed at improving a range of maternal and child health outcomes which reported injury outcomes but not possession and use of safety equipment or safety practices, as these are the subject of a Cochrane review currently undergoing revision (Bennett 2008). Those programmes reporting possession and use of safety equipment or safety practices were included. We excluded interventions aimed at improving safety behaviours which were not specific to the home environment, such as preventing insect or animal bites and promoting swimming safety in non‐domestic pools. We excluded studies promoting weapon safety and those aimed at reducing arson as our focus was on unintentional injury. We also excluded CBA studies where the control area contained the intervention area (for example, studies which compared injury rates in one area with those for the whole country). In our 2007 published review we included studies aimed at preventing chronic lead poisoning, however there has since been a Cochrane review evaluating household interventions aimed at preventing chronic lead poisoning (Yeoh 2008). We have, therefore, excluded these studies from the update and removed those that were included in our 2007 published review.
Types of outcome measures
The outcome measures we assessed were as follows.
Primary outcomes
Self reported or medically attended injury in children and young people aged 0 to 19 years.
Secondary outcomes
Possession and use of home safety equipment (stair gates, fireguards, smoke alarms, window locks, electrical socket covers, non‐slip bath mats, fire extinguishers, ipecac syrup, poison centre control number stickers).
Safety practices (storage of medicines, sharp objects, cleaning products, poisons and matches or lighters; use of baby walkers; safe hot water temperature; keeping hot foods or liquids, small objects and plants out of the reach of children; not leaving children alone in the bath, not leaving children alone on a high surface; checking smoke alarm batteries, having or practising a fire escape plan).
Search methods for identification of studies
Searches were not restricted by date, language or publication status.
Electronic searches
A search strategy was devised to identify randomised and non‐randomised studies (as defined above) using terms to identify injuries, safety equipment, practices and behaviours in the target population. We searched the following electronic databases:
Cochrane Central Register of Controlled Trials (CENTRAL) (2009, Issue 2) in The Cochrane Library;
MEDLINE (Ovid) (1950 to May 2009);
EMBASE (Ovid) (1980 to May 2009);
PsycINFO (Ovid) (1806 to May (week 3) 2009);
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to May 2009);
ISI Web of Science: Social Sciences Citation Index (SSCI) (1970 to May 2009);
ISI Web of Science: Conference Proceedings Citation Index‐ Science (CPCI‐S) (1990 to May 2009);
CINAHL (EBSCO) (1982 to May 2009);
Database of Abstracts and Reviews of Effectiveness (DARE) (2009, Issue 2) in The Cochrane Library;
NHS Economic Evaluation Database and the Health Technology Assessment Database (2009, Issue 2) in The Cochrane Library.
For the original review, all databases were searched from inception to July 2004.
Search strategies are reported in full in Appendix 1.
Searching other resources
We searched the following websites for published and unpublished research to June 2009:
Injury Prevention Research Centers at the Centers for Disease Control (USA);
Health Development Agency (UK) (up to March 2005);
National Institute for Health and Clinical Excellence (UK);
Children's Safety Network (USA);
International Society for Child and Adolescent Injury Prevention (International);
Child Accident Prevention Trust (UK);
Injury Control Resource Information Network (USA);
National Injury Surveillance Unit (Australia);
SafetyLit (USA);
The National Research Register (UK) (up to September 2007);
UKCRN Clinical Research Portfolio;
The metaRegister of controlled trials;
Index to theses.
We also handsearched the following sources to June 2009.
Abstracts from the 1st to 9th World conferences on injury prevention and control.
The journal "Injury Prevention" (to March 2009).
Reference lists of articles included in the review and of published systematic reviews.
We attempted to contact all authors of studies included in the review and asked for details of unpublished research for versions of this review through June 2004. In addition, for the previous version of this review (June 2004) we surveyed all Sure Start and Home Start schemes and Fire and Rescue Services in the UK, the Royal Society for the Prevention of Accidents, National Children's Homes and the Community Practitioners and Health Visitors Association (CPHVA) to ascertain if they had undertaken or participated in any evaluations of home safety programmes. These surveys were not repeated for the latest update.
Data collection and analysis
Selection of studies
Two authors (shared between DK, JS, CC, MW, AM‐J, CM, NI) independently scanned titles and abstracts to identify articles to retrieve in full. If an article appeared to be eligible based on the title but an abstract was unavailable, articles were retrieved in full. If there was disagreement between authors, a third author (DK or CM) reviewed the abstract and the article was retrieved in full if they considered it may fulfil the inclusion criteria. For studies where a review author was also an author of a study, other authors decided on inclusion of that study.
Data extraction and management
We attempted to obtain individual participant level data (IPD) for all eligible studies. If IPD were obtained, datasets were formatted across studies by recoding and labelling variables to ensure uniformity. Study authors who were unable or unwilling to provide IPD were asked to supply outcome data grouped by socio‐economic characteristics. If authors did not provide IPD or grouped outcome data, review authors (DK, JS, NI, PW) independently extracted data from published articles onto standard data extraction forms. We calculated numerators and denominators if study authors did not report this information and if we had the appropriate data. In these cases the odds ratios and confidence intervals we report may vary slightly from those in the published reports, due to rounding.
Data extraction was compared between authors for the first 53 articles. As there was a high level of agreement between authors (see results), data extraction on subsequent articles for the 2007 version of this review was undertaken by one author (DK) and by two authors (shared between DK, NI, PW) for the update of the review. Any discrepancies were identified and investigated by referral back to the original article by a senior member of the research team with prior experience of data extraction for systematic reviews and by consensus forming discussions. Following data extraction, multiple publications relating to the same study were identified to ensure results pertaining to the same individuals were not included more than once in analyses for each outcome.
Assessment of risk of bias in included studies
Two of a team of six authors (AM‐J, CM, SS, DK, NI, PW) independently assessed quality. If information regarding study quality was not available from publications or required clarification, we contacted study authors. For RCTs, allocation concealment, blinding of outcome assessment and completeness of follow‐up (80% or more in both treatment arms) were used as markers of trial quality.
Quality of randomisation was considered to be adequate when study authors mentioned the use of sealed opaque envelopes, automated computerised randomisation programmes, minimisation programmes or independent researchers using a computer generated list of random numbers. It was considered to be inadequate where randomisation was based on coin tossing or drawing from packs of cards. If insufficient data were provided to judge the adequacy of randomisation, it was categorised as unclear. Outcome assessment was considered to be blinded if authors stated this, and where it was not stated it was categorised as unclear. Outcomes assessed from self completed questionnaires were categorised as not blinded. The percentage follow‐up in each arm was calculated from the number allocated and the number with follow‐up data presented in each paper. This was frequently not reported for CBA studies, in which outcome assessment was often based on an injury surveillance system. In such cases, studies were categorised as having more than 80% follow‐up in each arm. Blinding of outcome assessment and the percentage of participants followed up was only recorded for those outcomes of relevance to this review.
For non‐randomised studies blinding of outcome assessment, completeness of follow‐up (80% or more in both treatment arms) and assessment of the distribution of confounders (baseline socio‐demographic or economic characteristics, safety practices or injury rates) were used as markers of quality. Studies were considered to be balanced in terms of confounders if the prevalence of these did not differ by more than 10% between the treatment arms. If studies reported that intervention and control groups were matched on various characteristics but did not provide data to judge the adequacy of this matching, the balance of confounders was categorised as unclear.
Kappa coefficients were calculated for the first 41 studies reviewed by both authors in the 2007 version of this review. Twenty of these studies were RCTs and 21 were non‐randomised studies. As a high level of agreement was not reached for all quality markers (see results) two authors extracted data on study quality for all included studies for the 2007 version and the update of the review. Disagreement between authors was resolved by referral back to the original article by a senior member of the research team with prior experience of quality assessment and by consensus forming discussion.
We examined the influence of individual aspects of study quality on effect sizes in a sensitivity analysis.
Measures of treatment effect
Combining treatment effects
Meta‐analyses were undertaken where three or more studies reported the same outcome. Where studies had three or more arms, data from each arm included in the meta‐analyses is described in the table 'Characteristics of included studies'. Where studies reported outcomes only for all ages combined (that is children and adults) they were not included in the meta‐analysis and their results are presented in the table of included studies.
For outcomes measured as rates, pooled incidence rate ratios (IRR) were estimated using summary data and random‐effects models. Effect sizes and standard errors were estimated from summary data from each study using Poisson regression in Stata (version 10) and meta‐analysis of effect sizes and standard errors was undertaken using the generic inverse variance option in Review Manager (version 5.1). If studies involved cluster randomisation, the number of events and the number of person years were adjusted for clustering using the variance inflation factor calculated using the formula given by Donner and Klar (Donner 2000). For studies for which we had IPD we calculated the coefficient of variation using the method described by Hayes and Bennett (Hayes 1999). For studies for which we did not have IPD we used a coefficient of variation of 0.25 (Hayes 1999). For CBA studies, we also estimated follow‐up injury rates adjusted for baseline rates using Poisson regression with a time by treatment arm interaction term. This represented the ratio of:
(Intervention arm follow‐up injury rate/Intervention arm baseline injury rate)/(Control arm follow‐up rate/Control arm baseline injury rate).
The regression coefficient (and the standard error) for this ratio of rates was used as the effect size (and the standard error) in the meta‐analysis adjusted for baseline injury rates.
For binary outcome measures, pooled odds ratios (OR) were estimated in a random‐effects model meta‐analysis using summary published data and if we had IPD, this was used to calculate appropriate summary data for those studies. If there was a zero in the 2 x 2 table for any study, 0.5 was added to each cell of that table before the meta‐analysis was performed. Studies with cluster allocation were adjusted for clustering by dividing the number of participants with and without an outcome by the design effect, calculated based on the intra‐class correlation coefficient (ICC) obtained from a range of sources (Kendrick 2006). For studies for which we had IPD we calculated the ICC from the IPD using one‐way analysis of variance. For studies that did not report an ICC for a particular outcome, but which had a similar allocation level to studies for which we had IPD, we used the ICC calculated from the IPD. If we calculated ICCs from more than one study for an outcome we used the midpoint of the range of ICCs. If we did not have IPD from which to calculate an ICC for an appropriate level of allocation we used the midpoint of a range of published ICCs (Adams 2004; DiGuiseppi 2002; Ukoumunne 1999). If these were available for injury outcomes at an appropriate allocation level we chose them in preference to those for other health related outcomes. The adjusted numbers of participants were included in the meta‐analysis as integers for analyses undertaken using Review Manager and as non‐integers for the analyses undertaken using Stata (version 10). The primary analyses for which forest plots are provided were undertaken using Review Manager (version 5.1). Analyses for outcomes using non‐integers, subgroup analyses and sensitivity analyses were undertaken using Stata (version 10). Effect sizes and confidence intervals, but not forest plots, are included in this review for these analyses.
Estimating the effect of interventions by social variables
Meta‐regression was undertaken to examine the effect of interventions by social group. Five covariates, previously shown to be associated with risk of injury (see introduction) were chosen as explanatory variables for the meta‐regression: child age (continuous), gender (binary), ethnic group (binary), single parent family (binary), residing in rented accommodation (binary) and at least one parent not in paid employment (binary).
The effect of covariates was assessed using IPD and study summary level data simultaneously, to minimise bias by including data from as many studies as possible and to maximise power for the meta‐regression (Lambert 2002). We developed a novel model which we used for this analysis, comprising five components (Sutton 2008).
Component 1
Logistic model to estimate effect sizes from non‐clustered studies for which IPD were available (Turner 2000) including a term for the interaction between treatment group and the binary covariate. If studies had small subgroup numbers precluding the estimation of effects by subgroups they were included in the analyses as summary data (see component 3).
Component 2
Random intercepts logistic model with participant at level one and cluster at level two for clustered studies for which IPD were available including a term for the interaction between treatment group and the binary covariate. If studies had small subgroup numbers precluding the estimation of effects by subgroups they were included in the analyses as summary data (see component 4).
Component 3
Random‐effects model meta‐regression of summary data from non‐clustered studies (Smith 1995) including a term for the covariate, expressed as the proportion of the study population with the covariate of interest.
Component 4
Random‐effects model meta‐regression of summary data from clustered studies where no adjustment for clustering had been made, including a term for the covariate, expressed as the proportion of the study population with the covariate of interest. Effect sizes were adjusted for clustering by inflating the variance by the design effect. A normal distribution, truncated at zero, was placed across likely values for the ICC. The mean ICC was obtained as described above and the standard deviation (SD) was equivalent to the difference between the maximum ICC for that outcome and the mean ICC divided by two. In such a distribution the mean ± 2 SD would encompass ICC values ranging from zero to the maximum ICC for that outcome.
Component 5
Meta‐analysis combining effect sizes from components 1 to 4. In the event that not all of the first four components of the model were required for a particular outcome, they were dropped accordingly. Due to possible ecological bias (where study‐level and patient‐level analyses give different results and the study‐level analysis is assumed to be biased), for analyses with sufficient IPD data available, we tested for potential ecological bias by splitting the variability between studies and within studies (in order to produce event‐risk estimates from the meta‐analysis more specific to individuals) (Riley 2008). Where the difference in the estimation of the treatment covariate interaction from both sources of variation was not statistically significantly different (at the 5% level) from each other, then the combined estimate is reported. Where it was significant, both estimates are noted.
The analysis strategy varied slightly to accommodate smaller amounts of data by reducing the complexity of the synthesis models, following the below criteria.
Five or more studies with at least one having IPD available: random‐effects model for simultaneously analysing IPD and summary‐level data, investigating splitting variance between and within studies.
Four studies with at least two having IPD available or five or more summary data only studies: random‐effects model for simultaneously analysing IPD and summary‐level data fireguards.
One IPD and two to four summary data only studies; two IPD and one summary data only studies; three IPD and no summary data only studies: fixed‐effect model for simultaneously analysing IPD and summary‐level data.
If only summary data were available, meta‐regression was undertaken only when five or more studies provided summary data.
In this model the IPD components estimate odds ratios comparing the treatment effect amongst those with and without the covariate of interest, whilst summary data components estimate regression coefficients for the change in treatment effect for a one unit change in the proportion of participants with the covariate of interest. In the summary data models a proportion of zero for the covariate estimates the treatment effect amongst those without the covariate of interest and a proportion of one will estimate the effect amongst those with the covariate of interest. Hence IPD and summary data models are estimating the same relationship between treatment effect and covariates (a similar situation exists for the continuous data (Riley 2008)).
We had IPD for one CBA study (Petridou 1997). However, we were unable to adjust for baseline values of the outcome using the IPD due to zero values in some subgroups. We were also unable to estimate the ICC as the variation between clusters was completely confounded by treatment group. Where possible, we therefore adjusted for the baseline prevalence of safety practices using a logistic model incorporating the baseline values as a covariate, unadjusted for clustering, and the regression coefficient and standard error were included in component 4 of the model and adjusted for clustering as described above.
All analyses were undertaken using a Bayesian Markov Chain Monte Carlo approach as implemented in the WinBUGS software (version 1.4.1) unless otherwise stated. All prior distributions were specified as vague unless otherwise stated.
Three studies provided IPD but were not included in the meta‐analyses. One reported outcomes that were reported by fewer than three studies (Schwebel 2009). Two had control groups that were not comparable to other studies included in the meta‐analysis (Kolko 2001; Rowland 2002) and, in addition, one also reported outcomes measured using a tool that differed from those of other studies reporting similar outcomes (Kolko 2001). One further study provided IPD on outcomes but not on social variables so was included in the meta‐analyses but was only included as summary data in the meta‐regressions (Swart 2008).
Unit of analysis issues
Outcome measures used in the analysis were as follows.
Injury rates for all injury mechanisms combined and for specific injury mechanisms.
Possession and use of home safety equipment (stair gates, fireguards, smoke alarms, window locks, electrical socket covers, non‐slip bath mats, fire extinguishers, ipecac syrup, poison centre control number stickers).
Safety practices (storage of medicines, sharp objects, cleaning products, poisons and matches or lighters; use of baby walkers; safe hot water temperature; keeping hot foods or liquids, small objects and plants out of the reach of children; not leaving children alone in the bath, not leaving children alone on a high surface; checking smoke alarm batteries, having or practising a fire escape plan).
Although studies reported a wide range of outcomes (see table 'Characteristics of included studies'), we restricted our analyses to injuries and to the most commonly and consistently reported safety practices in an attempt to limit the problems associated with multiple significance testing. The injury and safety practices outcomes used in the meta‐analyses are described in the table of included studies. Three injury outcomes were used in the meta‐analyses, poisonings, thermal injuries and all injuries, all of which were reported as rates. All safety practices used in the meta‐analyses were dichotomous.
Dealing with missing data
All cases with missing values were excluded from all analyses.
Assessment of heterogeneity
Heterogeneity between effect sizes of studies included in the review was described using forest plots, Chi2 (χ2) tests and the I2 statistic. We explored potential explanations for heterogeneity in two ways. Firstly we used meta‐regression to examine the effect of interventions by a range of demographic and social variables, using IPD and study summary level data simultaneously as described below. Other potential sources of heterogeneity were explored using subgroup analyses based on a priori explanations, which were whether the intervention included the provision of safety equipment, follow‐up period (up to and including three months and four or more months), whether the intervention was delivered in a clinical setting or in the home or community, use of a randomised or non‐randomised design, and study quality (allocation concealment, blinding of outcome assessment and at least 80% follow‐up in each treatment arm).
Assessment of reporting biases
In investigating publication and related biases for binary outcomes we followed the approach recommended in recent guidelines (Sterne 2011). Briefly, we only considered outcomes with 10 or more studies and produced contour enhanced funnel plots (Peters 2008) for examination. Given that there was heterogeneity for many outcomes we conducted the arcsine test proposed by Rucker (Rucker 2008) for funnel plot asymmetry. In order to investigate the impact of publication bias, a regression adjustment (the Egger‐D‐Var variant) was used as described by Moreno et al (Moreno 2009) for the outcomes we were concerned about. For meta‐analyses of injury rates where there were 10 or more studies we assessed publication bias using Egger's test.
Sensitivity analysis
The individual contribution of each study to the pooled result was assessed graphically and sensitivity analyses were undertaken to assess the effect of removing each study from each analysis. The robustness of the findings with respect to study quality was assessed by comparing treatment effects between randomised and non‐randomised studies and between RCTs with and without each of the three quality markers using subgroup analyses.
Results
Description of studies
Results of the search
Twelve thousand eight hundred and ninety‐seven records were found from searching bibliographic databases and 221 from other sources. In addition, for the original review we surveyed 443 Sure Start schemes, 198 (45%) of which replied; 356 Home Start schemes, of which 125 (35%) replied; 60 Fire and Rescue Services, of which 50 (83%) replied; eight Head Offices in the English Regions of the National Children's Homes charity, none of which replied; and the Head Offices for Wales, Scotland, Northern Ireland and England for the Royal Society for the Prevention of Accidents, one of which replied (25%). These surveys did not identify any studies meeting our inclusion criteria that had not already been identified from another source. The surveys were therefore not repeated for the update of the review.
Three hundred and sixty‐five articles (2.8%) from the 13,118 records were retrieved for more detailed evaluation.
Data were extracted by two authors on study design, participants, interventions, outcomes, subgroup analyses, adjustments for clustering and whether the author needed to be contacted for the first 53 studies identified for inclusion; 1386 of 1424 (97.3%) of these data items for the 53 studies were identical. Kappa coefficients for agreement on whether the study met the inclusion criteria in terms of study design (κ = 1.00), participants (κ = 1.00), interventions (κ = 0.85), outcomes (κ = 0.84) and overall whether the study met the inclusion criteria were high (κ = 1.00).
The PRISMA flow diagram shows the process of study identification and selection (Figure 1).
1.
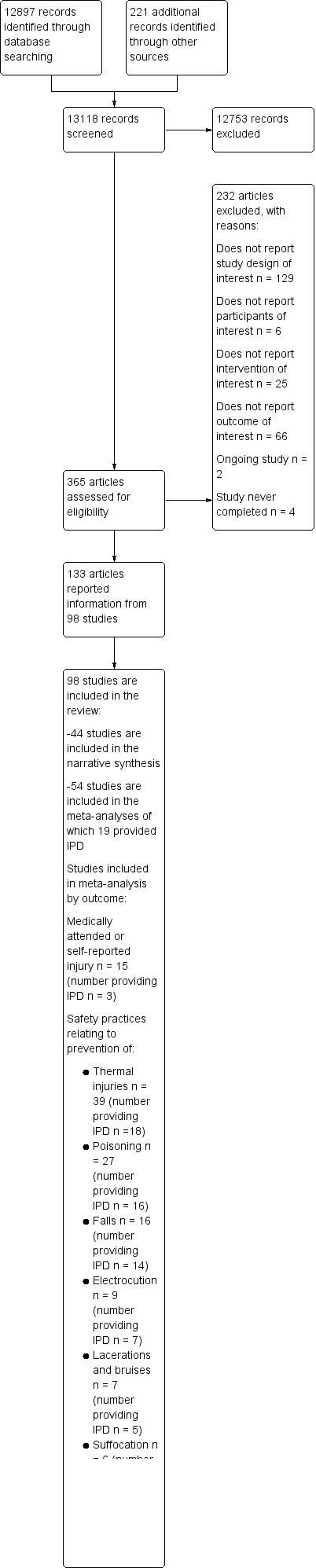
Study flow diagram.
Included studies
Ninety‐eight studies were included in the review. Fifty‐six (57%) were RCTs, 11 (11%) were non‐RCTs, 30 (31%) were CBAs and the design of one (1%) study was insufficiently described to distinguish between a non‐RCT and a CBA. Fifty‐four (55%) studies were included in at least one meta‐analysis (35 RCTs, 6 non‐RCTs and 13 CBAs) and 44 (45%) were summarised narratively. IPD were provided to us for 22 studies and data from 19 studies were included in at least one meta‐analysis. The most commonly reported outcomes related to thermal injuries, poisoning and falls.
Forty‐nine (50%) studies were from the USA, 14 from the UK (14%), six from Australia (6%), four (4%) each from Canada, South Africa and Sweden, three (4%) each from France and New Zealand, two (3%) each from Denmark and China, and one (1%) each from Singapore, Norway, Greece, Hong Kong, Israel, Italy and Mexico. Forty‐one (42%) provided interventions to families with children aged less than five years. Forty‐one (42%) provided low cost, discounted or free safety equipment and four (4%) provided information on financial help available for obtaining equipment or referral to centres where parents could obtain low cost equipment. Thirty‐six studies (36%) provided the intervention specifically to a disadvantaged population.
Twenty‐four studies reported outcomes related to the prevention of a range of medically attended or self reported injuries. Fifteen of these studies were included in the meta‐analyses, seven of which were RCTs, one was a non‐RCT and seven were CBAs. IPD were obtained from three studies.
Sixty‐four studies reported a range of outcomes related to thermal injury prevention. Thirty‐nine of these studies were included in at least one of the meta‐analyses of thermal injury prevention outcomes, 29 of which were RCTs, four were non‐RCTs and six were CBAs. IPD were obtained from 18 studies.
Forty‐five studies reported a range of outcomes related to poisoning prevention. Twenty‐seven of these studies were included in at least one of the meta‐analyses of poisoning prevention outcomes; 22 were RCTs, three were non‐RCTs and two were CBAs. IPD were obtained from 16 studies.
Twenty‐five studies reported a range of outcomes related to falls prevention. Sixteen of these studies were included in the meta‐analyses, 12 of which were RCTs, three were non‐RCTs and one was a CBA. IPD were obtained from 14 studies.
Sixteen studies reported a range of outcomes related to electrical injury prevention. Nine of these studies were included in the meta‐analyses, seven of which were RCTs and two were non‐RCTs. IPD were obtained from seven studies.
Twelve studies reported a range of outcomes related to the prevention of lacerations and bruising. Seven of these studies were included in the meta‐analyses, six of which were RCTs and one was a non‐RCT. IPD were obtained from five studies.
Twelve studies reported a range of outcomes related to the prevention of suffocation. Six of these studies were included in the meta‐analyses, all of which were RCTs. IPD were obtained from three studies.
Nine studies reported a range of outcomes related to the prevention of drowning. Five of these studies were included in the meta‐analyses, three of which were RCTs and two were non‐RCTs. IPD were obtained from four studies.
Nineteen studies reported home hazard scores or safety scores, none of which were included in a meta‐analysis.
Table 1 shows the demographic and socio‐economic variables reported by studies included in at least one of the meta‐regression analyses. If authors provided IPD, we have calculated the frequencies of these variables rather than using the published frequencies. The IPD datasets provided by some authors included all study participants regardless of whether follow‐up data were available for them, whilst others provided datasets containing only those participants for whom follow‐up data were available. Similarly, some authors report baseline data on all participants whilst others report baseline data only on those for whom follow‐up data were available. Consequently, the frequencies we report may differ from those reported by the authors in some cases. Twenty‐nine studies which were included in our meta‐analyses included data on child age. The mean or median age ranged from 0 to 13 years. Seventeen of the studies included in the meta‐analyses reported child gender. The percentage of males ranged from 46% to 63% across these studies. Fifteen studies reported the percentage of families residing in rented accommodation; this ranged from 13% to 100%. Twenty‐seven studies reported the percentage of single parent families; this ranged from 0% to 87%. Twenty‐nine studies reported the percentage of participants from a black or minority ethnic group; this ranged from 1% to 96%. Sixteen studies reported the percentage of families with at least one parent unemployed; this ranged from 11% to 81%.
1. Demographic and social characteristics of studies included in meta‐analyses (%).
| 1st Author | Mean/median age, years | Male | Non‐owner occupier | Single parents | BME group | Unemployment |
| Yorkston 2007 | ‐ | 51 | ‐ | ‐ | 9 | ‐ |
| Zhao 2006 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Phelan 2010 | 0 (prenatal mothers) | 46 | ‐ | 18 | 30 | 17 |
| Bulzachelli 2009 | 2.5 | 53 | ‐ | 70 | 96 | 53 |
| Sangvai 2007 | ‐ | ‐ | ‐ | ‐ | 48 | ‐ |
| Swart 2008 | ‐ | ‐ | ‐ | 52 | ‐ | 67 |
| Kendrick 2010 | ‐ | ‐ | 100 | 70 | 8 | 65 |
| Nansel 2008 | 1.2 | 52 | 71 | 32 | 66 | ‐ |
| Kendrick 2007 | 8.7 | 52 | ‐ | ‐ | ‐ | ‐ |
| Hwang 2006 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Gittelman 2007 | ‐ | ‐ | ‐ | ‐ | 84 | ‐ |
| Gielen 2007 | ‐ | 50 | ‐ | 69 | 93 | 48 |
| Carman 2006 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Babul 2007 | 1 | 52 | 39 | 11 | ‐ | ‐ |
| Dershewitz 1977 | ‐ | ‐ | ‐ | 0 | ‐ | 81 |
| Baudier 1988 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Campbell 2001 | 13 | 51 | ‐ | ‐ | ‐ | ‐ |
| Kendrick 2005 | 0.75 | ‐ | 20 | 5 | 4 | ‐ |
| McDonald 2005 | 0.81 | 48 | 83 | 54 | 93 | ‐ |
| Watson 2005 | 2.15 | 51 | 46 | 28 | 15 | 70 |
| Posner 2004 | 2.26 | 57 | 55 | ‐ | 84 | 34 |
| Kelly 2003 | ‐ | ‐ | ‐ | 13 | 93 | ‐ |
| Sznajder 2003 | 1.36 (youngest child) | ‐ | ‐ | 13 | ‐ | 34 |
| DiGuiseppi 2002 (smoke alarm ownership data only) | ‐ | ‐ | 100 | 13 | 18 | ‐ |
| Gielen 2002 | 0.25 | ‐ | ‐ | 87 | 94 | 77 |
| Hendrickson 2005 | 2 | 62 | ‐ | 27 | 88 | 74 |
| Nansel 2002 | 0.95 | 48 | 73 | 19 | 95 | ‐ |
| King 2001 | 2 | 59 | ‐ | ‐ | ‐ | ‐ |
| Johnston 2000 | 4.5 | 53 | ‐ | 56 | 30 | 57 |
| Clamp 1998 | 2.59 | ‐ | 21 | 10 | 1 | 12 |
| Waller 1993 | 2 | ‐ | ‐ | ‐ | ‐ | ‐ |
| Woolf 1992 | 1.92 | ‐ | ‐ | 11 | 10 | ‐ |
| Katcher 1989 | 8.5 | ‐ | ‐ | ‐ | 3 | ‐ |
| Barone 1988 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Williams 1998 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Matthews 1988 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Davis 1987 | 9 | ‐ | ‐ | ‐ | ‐ | ‐ |
| Kelly 1987 | 0.5 | ‐ | 89 | 81 | 95 | ‐ |
| Woolf 1987 | ‐ | ‐ | ‐ | 42 | 56 | 56 (maternal) |
| Thomas 1984 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Kendrick 1999 | 0.67 | 52 | 33 | 12 | 7 | 11 |
| Fergusson 1982 | 2 | ‐ | ‐ | 9 | 7 | ‐ |
| Miller 1982 | ‐ | ‐ | 13 | ‐ | ‐ | ‐ |
| Tan 2004 | 0.75 | ‐ | 79 | ‐ | ‐ | ‐ |
| Georgieff 2004 | 1.5 | ‐ | ‐ | 25 | 2 | ‐ |
| Mock 2003 | 6 | ‐ | ‐ | ‐ | ‐ | ‐ |
| Lindquist 1998, 1999, 2001, 2002, 2004 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Ytterstad 1995, 1998 | 2 | ‐ | ‐ | ‐ | ‐ | ‐ |
| Petridou 1997 | 9.5 | ‐ | ‐ | 4 | ‐ | ‐ |
| Bentzen 1997 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Svanstrom 1995 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Schwarz 1993 | ‐ | ‐ | ‐ | ‐ | 96 | ‐ |
| Guyer 1989, 1991 | ‐ | ‐ | 48 | ‐ | 8 | ‐ |
| Jenkins 1996 | ‐ | 63 | ‐ | 28 | 48 | 22 (paternal) |
Excluded studies
The Characteristics of excluded studies table gives the reason for exclusion of each excluded study.
Risk of bias in included studies
Our assessment of the risk of bias is given in the table 'Characteristics of included studies'. Of the 56 RCTs, 19 (34%) had adequate randomisation or allocation concealment, 18 (32%) had blinded outcome assessment, and 30 (54%) had follow‐up on at least 80% of participants in each treatment arm. Of the 11 non‐RCTs, none had blinded outcome assessment, six (55%) had follow‐up on at least 80% of participants in each treatment arm, and four (36%) were considered to be balanced in terms of confounders. Of the 30 CBAs, none had blinded outcome assessment, 18 (60%) had follow‐up on at least 80% of participants in each treatment arm, and eight (27%) were considered to be balanced in terms of confounders.
Twenty‐three (41%) of the RCTs, five (45%) of the non‐RCTs and 29 (97%) of the CBAs had a clustered design. The allocation level for clustered RCTs ranged from paediatricians to general practices and electoral wards, but also included several trials where allocation was based on time periods. The allocation level for the clustered non‐RCTs included one study allocated at the general physician (GP) practice level, but the remaining studies were allocated based on time periods. The allocation level for the clustered CBAs was generally larger, ranging from child health clinics to cities, islands, municipalities and counties. For the CBAs, where authors have described how the intervention and control communities were allocated this has been included in the comments section of the table.
Fifty‐four (55%) of the studies were included in at least one of the meta‐analyses. Thirty‐five (65%) of these were RCTs, six (11%) were non‐RCTs and 13 (24%) were CBAs. Nineteen (35%) of the studies included in the meta‐analysis provided IPD. In addition, a further three studies provided IPD which were not included in the meta‐analyses (Kolko 2001; Rowland 2002; Schwebel 2009). The first two studies had control groups that were not comparable to other studies included in the meta‐analysis and the outcomes measured in the third study were reported by fewer than three studies. None of the study authors provided us with unpublished subgroup analyses.
Effects of interventions
Different measures of effect are reported in this section, as follows.
Pooled incidence rate ratios (IRR) were calculated for injuries occurring during the study period. An effect size less than 1.0 means the intervention was beneficial.
Pooled odds ratios (OR) were calculated for protective outcomes, such as the uptake of safety equipment or safe practices. An effect size more than 1.0 means the intervention was beneficial.
For both measures, if the range of the 95% confidence interval (CI) falls on both sides of 1.0 then, statistically, the intervention has not been shown to work with certainty.
Medically attended and self reported injuries
Fifteen studies reporting medically attended or self reported injury were included in the meta‐analyses. The study by Kendrick was adjusted for clustering using a coefficient of variation of 0.30, calculated from the IPD. The study by Watson was not adjusted for clustering as the coefficient of variation calculated from the IPD was zero. The studies by Bentzen 1997; Carman 2006; Gittelman 2007; Guyer 1989; Lindqvist 1998a; Svanstrom 1995 and Yorkston 2007 were adjusted using a coefficient of variation of 0.25 as described above. After adjusting for clustering the effective combined sample size was 12,039 person years in the intervention arm and 12,367 person years in the control arm. Studies had very varied follow‐up time periods, ranging from six months (Sangvai 2007) to eight years (Svanstrom 1995).
In community injury prevention programmes, which were usually CBA studies, the intervention community or communities were often chosen because of their high injury rates. Five of the seven CBAs included in the meta‐analyses had considerably higher injury rates in the intervention than control arms at baseline (Carman 2006; Gittelman 2007; Guyer 1989; Lindqvist 1998a; Yorkston 2007). In view of this, we undertook analyses both adjusting and not adjusting CBA study follow‐up injury rates for baseline injury rates. Studies also reported outcomes at multiple follow‐up time periods. We chose the time period most consistent with that for other studies included in the meta‐analysis.
One study reported injury rates for 'potentially preventable injuries', that is those that could plausibly be prevented by the equipment provided as part of the intervention, and rates for all injuries (that is including those that were not plausibly preventable by the equipment provided in the trial) (Phelan 2010). We therefore undertook analyses including all injuries with a sensitivity analysis including only the potentially preventable injuries from the study by Phelan 2010.
Analyses unadjusted for baseline injury rates in controlled before and after (CBA) studies
Analysis 1.1. The pooled incidence rate ratio (IRR) was calculated.
1.1. Analysis.
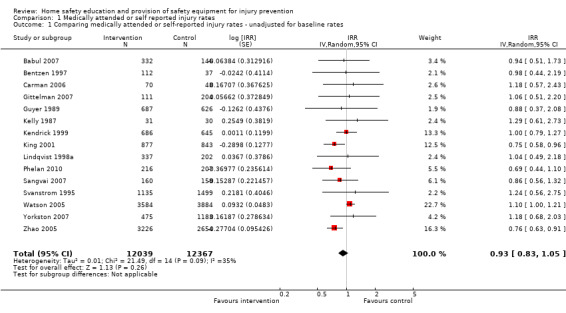
Comparison 1 Medically attended or self reported injury rates, Outcome 1 Comparing medically attended or self‐reported injury rates ‐ unadjusted for baseline rates.
Home safety interventions did not appear to be associated with a reduction in injury rates (IRR 0.93, 95% CI 0.83 to 1.05) and there was significant heterogeneity between effect sizes. Heterogeneity may be partly explained by the provision of safety equipment, with interventions providing equipment possibly being less effective (IRR 0.94, 95% CI 0.81 to 1.09) than those not providing equipment (IRR 0.85, 95% CI 0.72 to 0.99), with no significant heterogeneity between effect sizes in either subgroup. This difference may result from a single large school‐based study that did not provide equipment and which demonstrated a significant reduction in injury rates (Zhao 2005). Studies with non‐blinded outcome assessment also appeared to have a greater effect (IRR 0.76, 95% CI 0.64 to 0.90) than those with blinded outcome assessment (IRR 0.95, 95% CI 0.73 to 1.22), but significant heterogeneity remained in the latter subgroup analysis. Heterogeneity may also be partly explained by the setting in which the intervention was delivered, with possible evidence of a greater effect in those delivered in the home (clinical setting IRR 1.07, 95% CI 0.99 to 1.17; home IRR 0.83, 95% CI 0.68 to 1.01; community IRR 1.03, 95% CI 0.69 to 1.54). Heterogeneity did not appear to be explained by study design (RCTs IRR 0.87, 95% CI 0.71 to 1.07; other designs IRR 1.04, 95% CI 0.87 to 1.24), adequate allocation concealment (adequate concealment IRR 0.88, 95% CI 0.70 to 1.11; inadequate or unclear concealment IRR 0.87, 95% CI 0.55 to 1.37) or follow‐up of at least 80% of participants in each treatment arm (at least 80% follow‐up IRR 0.84, 95% CI 0.64 to 1.09; less than 80% follow‐up IRR 0.95, 95% CI 0.67 to 1.31). All analyses were robust to using only 'preventable' injuries from the study by Phelan 2010, except the finding of a significant effect in non‐blinded studies (IRR all injuries OR 0.76, 95% CI 0.64 to 0.90; preventable injuries only OR 0.71, 95% CI 0.47 to 1.07). Sensitivity analyses also indicated that findings were robust to excluding all studies in turn except Watson 2005, which resulted in a significant reduction in injury risk (IRR 0.86, 95% CI 0.77 to 0.96).
Analyses adjusted for baseline injury rates in controlled before and after (CBA) studies
Analysis 1.2. The pooled incidence rate ratio (IRR) was calculated.
1.2. Analysis.
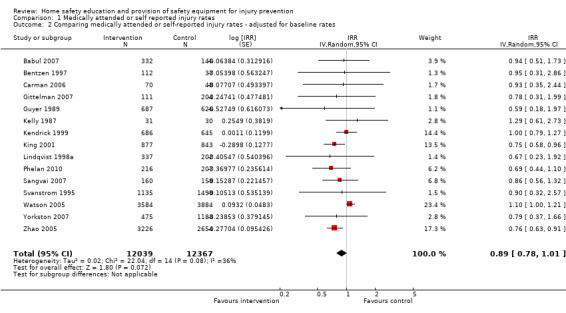
Comparison 1 Medically attended or self reported injury rates, Outcome 2 Comparing medically attended or self‐reported injury rates ‐ adjusted for baseline rates.
There was some evidence that home safety interventions may be associated with a reduction in injury rates (IRR 0.89, 95% CI 0.78 to 1.01) but there was significant heterogeneity between effect sizes. Heterogeneity may be partly explained by the setting in which the intervention was delivered with a significant effect found for interventions delivered in the home (IRR 0.75, 95% CI 0.62 to 0.91) compared to those delivered in clinical settings (IRR 1.07, 95% CI 0.99 to 1.17) or within the community (IRR 0.77, 95% CI 0.52 to 1.16), and no significant heterogeneity between effect sizes in any of these subgroup analyses. Interventions not providing equipment appeared to have a significant effect (IRR 0.78, 95% CI 0.66 to 0.92) whilst those providing equipment did not (IRR 0.92, 95% CI 0.79 to 1.08), with no significant heterogeneity between effect sizes in either subgroup analysis. Again, this difference may result from a single large school‐based study which did not provide equipment and which demonstrated a significant reduction in injury rates (Zhao 2005). Studies with non‐blinded outcome assessment may appear to be more effective (IRR 0.76, 95% CI 0.64 to 0.90) than those with blinded outcome assessment (IRR 0.95, 95% CI 0.73 to 1.22), but significant heterogeneity remained in the latter subgroup analysis. Heterogeneity did not appear to be explained by study design (RCTs IRR 0.89, 95% CI 0.76 to 1.06; other designs IRR 0.80, 95% CI 0.55 to 1.15). Restricting analyses to RCTs with adequate allocation concealment, blinded outcome assessment and follow‐up of at least 80% of participants in each arm excluded all CBAs and consequently resulted in the same subset of studies as for the analyses unadjusted for baseline rates presented above (that is adequate allocation concealment IRR 0.88, 95% CI 0.70 to 1.11; inadequate or unclear concealment IRR 0.87, 95% CI 0.55 to 1.37; blinded outcome assessment IRR 0.95, 95% CI 0.73 to 1.22; non‐blinded outcome assessment IRR 0.76, 95% CI 0.64 to 0.90; at least 80% follow‐up IRR 0.84, 95% CI 0.64 to 1.09; less than 80% follow‐up IRR 0.95, 95% CI 0.67 to 1.31). All analyses were robust to using only 'preventable' injuries from the study by Phelan 2010. Sensitivity analyses also indicated that findings were robust to excluding all studies in turn except Watson 2005, which resulted in a significant reduction in injury risk (IRR 0.82, 95% CI 0.74 to 0.92).
Data not included in the meta‐analysis
Nine studies reporting injury outcomes were not included in the meta‐analyses (Coggan 2000; Mackay 2002; Moller 1996; Ohn 2005; Ozanne‐Smith 2002; Ponce De Leon 2007; Rey 1993; Schelp 1987; Schlesinger 1966). Two of these reported significantly lower injury rates in the intervention group as compared to the control group (Coggan 2000; Moller 1996); neither however presented numerators and denominators. One study reported a significantly lower injury rate in the intervention group as compared to the control group for one subgroup only (domestic accidents) (Rey 1993). One study reported a significant reduction in hospital admission rate (compared to the rate for the rest of Sweden) in one of the five intervention areas (Lidkoping), a significant increase in one of the five intervention areas (Skovde) and no significant difference in three other intervention areas (Ponce De Leon 2007). Four studies did not find a significant difference in injury rates between intervention and control groups (Mackay 2002; Ohn 2005; Ozanne‐Smith 2002; Schlesinger 1966). One study (Schelp 1987) reported a significant reduction in injury rate post‐intervention compared to pre‐intervention but only presented this data for the intervention community.
Thermal injury prevention
Sixty‐four studies reported thermal injury prevention outcomes, 39 (61%) of which had at least one outcome included in at least one meta‐analysis.
Thermal injuries
Analysis 2.1. The pooled incidence rate ratio (IRR) was calculated.
2.1. Analysis.
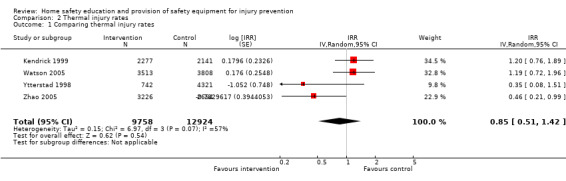
Comparison 2 Thermal injury rates, Outcome 1 Comparing thermal injury rates.
Only four studies reporting thermal injury rates (Kendrick 1999; Watson 2005; Ytterstad 1998; Zhao 2005) were included in the meta‐analysis. The study by Watson 2005 was adjusted for clustering using a coefficient of variation of 0.98 calculated from the IPD. The study by Kendrick was not adjusted for clustering as the coefficient of variation calculated from the IPD was zero. The study by Ytterstad 1998 was adjusted using a coefficient of variation of 0.25 as described above. The combined number of person years was 9758 and 12,924 in the intervention and control arms respectively. There was a lack of evidence that home safety interventions with or without the provision of safety equipment reduced thermal injuries (IRR 0.85, 95% CI 0.51 to 1.42) and there was significant heterogeneity between effect sizes. Adjusting the post‐intervention thermal injury rates for baseline rates for the study by Ytterstad 1998 had little impact on the results (IRR 0.94, 95% CI 0.59 to 1.49).
Safe hot tap water temperature
Analysis 4.1. The pooled odds ratio (OR) was calculated.
4.1. Analysis.
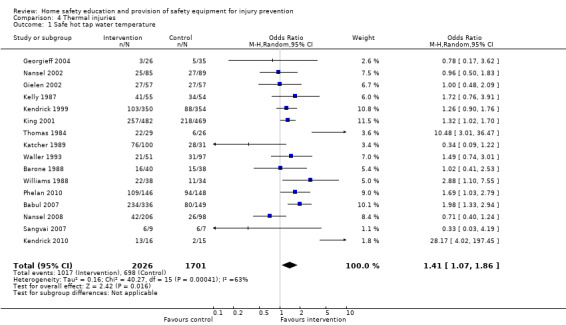
Comparison 4 Thermal injuries, Outcome 1 Safe hot tap water temperature.
Sixteen studies reporting safe hot tap water temperatures were included in the meta‐analysis (Babul 2007; Barone 1988; Georgieff 2004; Gielen 2002; Katcher 1989; Kelly 1987; Kendrick 1999; Kendrick 2010; King 2001; Nansel 2002; Nansel 2008; Phelan 2010; Sangvai 2007; Thomas 1984; Waller 1993; Williams 1988). These studies used varying definitions of a safe hot tap water temperature; less than 49 ºC (Georgieff 2004; Gielen 2002; Nansel 2002; Nansel 2008; Sangvai 2007), less than 52 ºC (Kelly 1987), less than or equal to 54 ºC (Katcher 1989; Kendrick 1999; King 2001; Phelan 2010; Thomas 1984) and less than 60 ºC (Waller 1993). Safe hot water was not defined in three studies (Babul 2007; Barone 1988; Williams 1988). Hot water temperatures were tested by observers in nine studies (Georgieff 2004; Gielen 2002; Kelly 1987; Kendrick 2010; King 2001; Phelan 2010; Sangvai 2007; Thomas 1984; Waller 1993) and were self reported in five (Babul 2007; Katcher 1989; Kendrick 1999; Nansel 2002; Nansel 2008) although one of the latter validated self reported temperatures by testing a sample of homes (Katcher 1989). Five were adjusted for clustering (Barone 1988; Georgieff 2004; Gielen 2002; Kendrick 1999; Williams 1988) and adjusted numerators and denominators were rounded to the nearest integer. The study by Georgieff was adjusted using an ICC of 0.00012 (DiGuiseppi 2002) and the studies by Kendrick, Gielen, Barone and Williams were adjusted using an ICC of 0.00159, which was calculated from IPD from the study by Kendrick (Kendrick 1999).
Families in the home safety interventions arms were more likely to have a safe hot tap water temperature than control group families (OR 1.41, 95% CI 1.07 to 1.86) and repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced identical results.
There was significant heterogeneity between effect sizes, which was not explained by the provision of thermometers for water temperature testing or the provision of thermostatic mixer valves as excluding studies providing either resulted in a similar effect size (OR 1.32, 95% CI 0.97 to 1.81) and significant heterogeneity between effect sizes remained. Some of the heterogeneity may be explained by study setting, with a significant effect seen only amongst those studies providing interventions in the home (OR 1.58, 95% CI 1.12 to 2.22) compared to those in clinical settings (OR 1.31, 95% CI 0.78 to 2.20). Some of the heterogeneity may also be explained by follow‐up period, with a significant effect seen only in studies with follow‐up of four or more months (OR 1.49, 95% CI 1.16 to 1.85) compared to those with follow‐up periods of three months or less (OR 1.40, 95% CI 0.57 to 3.46). Significant heterogeneity remained in the subgroup analyses by study setting and follow‐up period. Similar effect sizes were found when analyses were restricted to randomised studies (OR 1.58, 95% CI 1.14 to 2.20), those with adequate allocation concealment (OR 1.67, 95% CI 1.14 to 2.51), blinded outcome assessment (OR 1.33, 95% CI 1.04 to 1.69) and follow‐up of at least 80% participants in each arm (OR 1.62, 95% CI 1.04 to 2.53). Significant heterogeneity remained in the subgroup analyses for randomised studies and those with adequate allocation concealment and those with follow‐up of at least 80% of participants in each arm. Sensitivity analyses excluding each study in turn indicated that findings were robust to excluding any one study.
Functioning smoke alarms
Analysis 4.2. The pooled odds ratio (OR) was calculated.
4.2. Analysis.
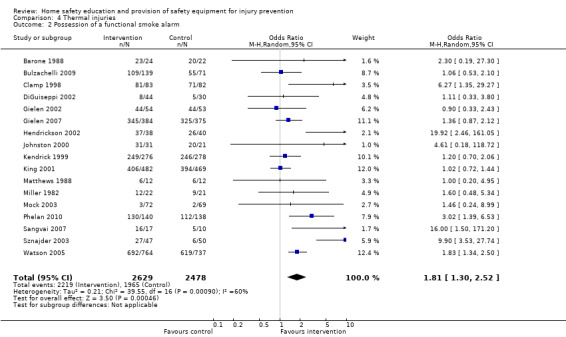
Comparison 4 Thermal injuries, Outcome 2 Possession of a functional smoke alarm.
Seventeen studies reporting possession of a functioning smoke alarm were included in the meta‐analysis (Barone 1988; Bulzachelli 2009; Clamp 1998; DiGuiseppi 2002; Gielen 2002; Gielen 2007; Hendrickson 2002; Johnston 2000; Kendrick 1999; King 2001; Matthews 1988; Miller 1982; Mock 2003; Phelan 2010; Sangvai 2007; Sznajder 2003; Watson 2005). Five were adjusted for clustering (Barone 1988; Gielen 2002; Johnston 2000; Kendrick 1999; Miller 1982) and adjusted numerators and denominators were rounded to the nearest integer. All studies were adjusted using an ICC of 0.033, calculated from IPD from the study by Kendrick 1999. The study by DiGuiseppi 2002 was not adjusted for clustering as the ICC calculated from the IPD provided from that study was extremely small (P < 0.00001).
Families in the home safety interventions arm were significantly more likely to possess a functioning smoke alarm than control group families (OR 1.81, 95% CI 1.30 to 2.52). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size of 1.83 (95% CI 1.28 to 2.50). Effect sizes varied significantly between studies and this heterogeneity may be partly explained by provision of smoke alarms, with a larger effect size in studies providing smoke alarms (OR 2.49, 95% CI 1.53 to 4.06) than those not providing alarms (OR 1.12, 95% CI 0.87 to 1.45), although significant heterogeneity still existed between effect sizes for studies providing smoke alarms. It may also be partly explained by the setting in which the intervention was delivered, with those in clinical settings (OR 1.56, 95% CI 1.14 to 2.13) possibly having a smaller effect size than those delivered in the home or community (OR 2.92, 95% CI 1.08 to 7.91), but significant heterogeneity remained in the analysis for interventions delivered in the home or community. Larger effect sizes were also seen in studies with follow‐up periods of three months or less (OR 2.66, 95% CI 1.27 to 5.89) than in those with longer follow‐up periods (OR 1.47, 95% CI 1.04 to 2.09), however significant heterogeneity was found between effect sizes in both subgroup analyses. Similar effect sizes were found when analyses were restricted to randomised studies (OR 2.25, 95% CI 1.43 to 3.55), those with adequate allocation concealment (OR 2.24, 95% CI 1.38 to 3.64) and those with follow‐up on at least 80% of participants in both arms (OR 3.13, 95% CI 1.49 to 6.58). Only three studies had blinded outcome assessment and the effect size may be smaller in these studies (OR 1.57, 95% CI 0.54 to 4.55) than in those without blinded outcome assessment (OR 2.64, 95% CI 1.55 to 4.51). However, care must be taken in interpreting this finding due to the small number of studies involved. Significant heterogeneity was found between treatment effects amongst randomised studies and amongst those randomised studies with and without adequate allocation concealment, with and without blinded outcome assessment, and with follow‐up on at least 80% of participants in both arms. Sensitivity analyses indicated that the findings were robust to the exclusion of any one study.
Seventeen studies reported smoke alarm ownership (Barone 1988; Clamp 1998; Davis 1987; DiGuiseppi 2002; Gielen 2007; Guyer 1989; Hendrickson 2002; Jenkins 1996; Kelly 1987; Kendrick 2007; King 2001; Matthews 1988; McDonald 2005; Nansel 2002; Nansel 2008; Posner 2004; Thomas 1984), 10 of which did not also report possession of a functional smoke alarm (Davis 1987; Guyer 1989; Jenkins 1996; Kelly 1987; Kendrick 2007; McDonald 2005; Nansel 2002; Nansel 2008; Posner 2004; Thomas 1984). Meta‐analysis of these 17 studies indicated that there was some evidence to suggest that intervention group families may be slightly more likely to have a smoke alarm (OR 1.17, 95% CI 0.97 to 1.42) and no significant heterogeneity was found between effect sizes.
Use of fire guards
Analysis 4.3. The pooled odds ratio (OR) was calculated.
4.3. Analysis.
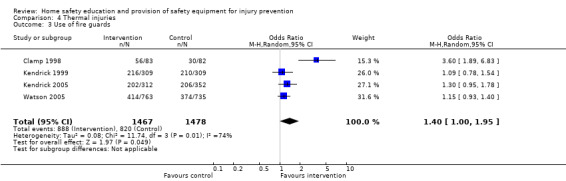
Comparison 4 Thermal injuries, Outcome 3 Use of fire guards.
Four studies reporting use of fire guards were included in the meta‐analysis (Clamp 1998; Kendrick 1999; Kendrick 2005b; Watson 2005). Two studies (Clamp 1998; Watson 2005) reported whether fire guards were fitted and always used; one study reported whether fire guards were used on some or all fires (Kendrick 2005b); and one whether fire guards were used on all fires (Kendrick 1999). If studies reported that fire guards were not required because families did not have any gas, electric, open or other fires these families were included as having fire guards as they were considered safe in terms of the risk of a thermal injury from such a source. Two studies (Kendrick 1999; Kendrick 2005b) were adjusted for clustering and adjusted numerators and denominators were rounded to the nearest integer. Both studies were adjusted for clustering using ICCs calculated from IPD from each respective study. An ICC of 0.01893 was used for Kendrick 1999 and 0.01119 for Kendrick 2005b.
There was some evidence that home safety interventions were effective in increasing the use of fire guards (OR 1.40, 95% CI 1.00 to 1.95). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size of 1.39 (95% CI 1.00 to 1.94). Effect sizes were significantly heterogeneous. All four studies provided fire guards and all provided interventions in clinical settings. A larger effect size was seen in the one study with a follow‐up period of three months or less (OR 3.60, 95% CI 1.89 to 6.84) than in those with longer follow‐up periods (OR 1.17, 95% CI 1.00 to 1.36); there was no significant heterogeneity between effect sizes for those studies with longer follow‐up periods. However, care must be taken in interpreting this finding due to the small number of studies involved. Restricting analyses to randomised studies, those with adequate allocation concealment, and with follow‐up on more than 80% of participants in both treatment arms did not alter the conclusions drawn from the main analysis. Only one randomised study had blinded outcome assessment. Sensitivity analyses excluding each study in turn indicated that the results were robust to the exclusion of any one study.
Keeping hot drinks or food out of reach of children
Analysis 4.4. The pooled odds ratio (OR) was calculated.
4.4. Analysis.
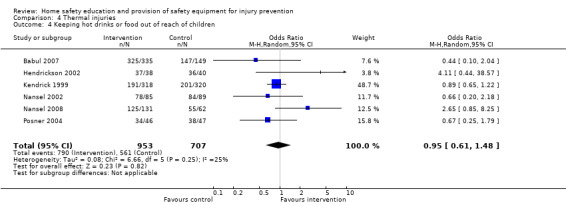
Comparison 4 Thermal injuries, Outcome 4 Keeping hot drinks or food out of reach of children.
Six studies reporting keeping hot drinks or food out of the reach of children (Babul 2007; Hendrickson 2002; Kendrick 1999; Nansel 2002; Nansel 2008; Posner 2004) were included in the meta‐analysis. The definitions of keeping hot food or drinks out of reach varied from never placing hot food or drinks on tablecloths or on edges of counters (Posner 2004), never holding a child whilst cooking or holding a hot liquid (Nansel 2002; Nansel 2008), never drinking hot drinks whilst holding a child (Kendrick 1999), hot liquids and hot foods placed out of a child's reach (Babul 2007), and hot food or drinks not observed to be accessible to a child on a home visit (Hendrickson 2002). The study by Kendrick was adjusted for clustering using an ICC of 0.01609 calculated from the IPD from that study and adjusted numerators and denominators were rounded to the nearest integer.
Families in the home safety interventions arms were not significantly more likely to keep hot drinks out of reach of children than control group families (OR 0.95, 95% CI 0.61 to 1.48) and there was no evidence of heterogeneity between effect sizes. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Storage of matches
Analysis 4.5. The pooled odds ratio (OR) was calculated.
4.5. Analysis.
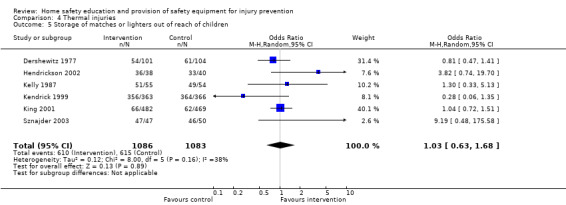
Comparison 4 Thermal injuries, Outcome 5 Storage of matches or lighters out of reach of children.
Six studies reporting storage of matches out of the reach of children were included in the meta‐analysis (Dershewitz 1977; Hendrickson 2002; Kelly 1987; Kendrick 1999; King 2001; Sznajder 2003). Five studies reported matches and lighters observed as out of reach of children on a home visit (Dershewitz 1977; Hendrickson 2002; Kelly 1987; King 2001; Sznajder 2003) and the sixth used self reported always keeping matches out of reach (Kendrick 1999). The ICC calculated from the IPD for the only clustered study (Kendrick 1999) was extremely small (P < 0.00001), hence the data from this study were not adjusted for clustering.
There was a lack of evidence that home safety interventions were effective in increasing the safe storage of matches (OR 1.03, 95% CI 0.63 to 1.68). There was no significant heterogeneity between effect sizes. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Possession of a fire extinguisher
Analysis 4.6. The pooled odds ratio (OR) was calculated.
4.6. Analysis.
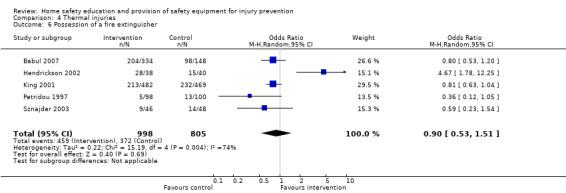
Comparison 4 Thermal injuries, Outcome 6 Possession of a fire extinguisher.
Five studies reporting possession of a fire extinguisher were included in the meta‐analysis (Babul 2007; Hendrickson 2002; King 2001; Petridou 1997; Sznajder 2003). This was defined as an easily accessible extinguisher that was in working order (Sznajder 2003), a fire extinguisher present (Hendrickson 2002; King 2001) and a functional fire extinguisher present (Babul 2007; Petridou 1997). The study by Petridou 1997 was adjusted for clustering using an ICC of 0.0024 (estimated as the midpoint of a range of ICCs published for health outcomes at the level of health authority, local authority or town (Kendrick 2006)) and the adjusted numerator and denominator were rounded to the nearest integer.
There was a lack of evidence that home safety interventions were effective in increasing possession of a fire extinguisher (OR 0.90, 95% CI 0.53 to 1.51). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size of 0.91 (95% CI 0.54 to 1.51). There was significant heterogeneity between treatment effects. The heterogeneity may be partly explained by the provision of fire extinguishers as studies not providing extinguishers had a smaller effect (OR 0.77, 95% CI 0.63 to 0.95) than the one study (Hendrickson 2002) that did provide extinguishers (OR 4.67, 95% CI 1.78 to 12.25). However, care must be taken in interpreting this finding due to the small number of studies involved. Sensitivity analyses including only randomised studies, those with adequate allocation concealment, and with follow‐up on more than 80% of participants in both treatment arms did not alter the conclusions drawn from the main analysis. Only one randomised study had blinded outcome assessment. Sensitivity analyses excluding each study in turn indicated that results were robust to the exclusion of any one study.
Having a fire escape plan
Analysis 4.7. The pooled odds ratio (OR) was calculated.
4.7. Analysis.

Comparison 4 Thermal injuries, Outcome 7 Has a fire escape plan.
Four studies reporting having or practising a fire escape plan were included in the meta‐analysis (Campbell 2001; Hwang 2006; Petridou 1997; Posner 2004). The study by Petridou 1997 was adjusted for clustering using an ICC of 0.0024 (estimated as the midpoint of a range of ICCs published for health outcomes at the level of health authority, local authority or town (Kendrick 2006)) and the adjusted numerator and denominator were rounded to the nearest integer. Home safety interventions were effective in increasing the proportion of families with a fire escape plan (OR 2.01, 95% CI 1.45 to 2.77) and there was no significant heterogeneity between effect sizes. Identical results were found when analyses were repeated using non‐integers for numerators and denominators for clustered studies. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Checking or changing smoke alarm batteries in the last six months
Analysis 4.8. The pooled odds ratio (OR) was calculated.
4.8. Analysis.
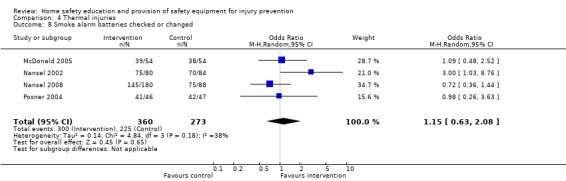
Comparison 4 Thermal injuries, Outcome 8 Smoke alarm batteries checked or changed.
Four studies reporting checking or changing smoke alarm batteries in the last six months were included in the meta‐analysis (McDonald 2005; Nansel 2002; Nansel 2008; Posner 2004). There was no evidence that home safety interventions were effective in increasing the proportion of families who had checked or changed smoke alarm batteries in the preceding six months (OR 1.15, 95% CI 0.63 to 2.08) and there was no significant heterogeneity between effect sizes. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Effect of covariates on thermal injury prevention practices
The effects of the interventions by child age, gender and social group are shown in Table 2. There was no evidence that interventions varied in effect by child age, gender or any of the social variables.
2. Odds ratios for thermal injury prevention practices (95% credible interval) by social variables.
| Social variables | Functional Smoke Alarm | Fire Guards | Keeping matches out of reach | Safe Hot Water | Keeping hot drinks and food out of reach | Fire extinguishers | Fire Escape Plans | Checking/changing smoke alarm batteries |
| GENDER | ||||||||
| Boys | 2.00 (0.55, 12.82) | N/A | N/A | 1.07 (0.63, 1.79) | 0.88 (0.36, 2.38) | 1.14 (0.50, 2.57)* | N/A | 2.12 (0.84, 5.68) |
| Girls | 1.88 (0.52, 12.22) | N/A | N/A | 1.66 (0.97, 2.79) | 1.02 (0.43, 2.84) | 0.64 (0.22, 1.91) | N/A | 1.11 (0.38, 3.34) |
| Interaction term (ratio of odds ratios) | 1.06 (0.63, 1.74) | N/A | N/A | 0.65 (0.38, 1.07) | 0.86 (0.48, 1.54) | 1.77 (0.27, 11.25) | N/A | 1.92 (0.37, 10.18) |
| ETHNIC GROUP | ||||||||
| Black and minority ethnic groups | 3.21 (0.94, 15.14) | 1.50 (0.41, 6.28) | 1.28 (0.01, 184.7) | 1.14 (0.51, 2.72) | 1.38 (0.36, 7.51) | N/A | N/A | 1.29 (0.80, 2.07) |
| White | 2.74 (0.89, 12.86) | 1.45 (0.43, 5.43) | 1.04 (0.01, 329.10) | 1.23 (0.54, 2.82) | 0.91 (0.19, 4.17) | N/A | N/A | 0.39 (0.08, 1.40) |
| Interaction term (ratio of odds ratios) | 1.16 (0.54, 2.50) | 1.02 (0.57, 1.86) | 1.04 (0.02, 28.40) | 0.94 (0.49, 1.83) | 1.58 (0.57, 5.02) | N/A | N/A | 3.33 (0.82, 18.15) |
| FAMILY TYPE | ||||||||
| Single parent family | 1.63 (0.66, 4.64) | 1.38 (0.83, 2.45) | N/A | 1.45 (0.45, 6.18) | 0.95 (0.16, 5.16) | 2.18 (0.27, 23.74)* | N/A | 1.10 (0.39, 2.99) |
| Two parent family | 1.99 (0.81, 5.42) | 1.20 (0.81, 1.87) | N/A | 1.64 (0.59, 7.91) | 1.06 (0.31, 4.64) | 0.86 (0.54, 1.36) | N/A | 1.11 (0.63, 1.98) |
| Interaction term (ratio of odds ratios) | 0.83 (0.51, 1.33) | 1.16 (0.76, 1.76) | N/A | 0.85 (0.42, 1.72) | 0.87 (0.22, 3.16) | 2.52 (0.24, 36.80) | N/A | 0.99 (0.26, 3.43) |
| HOUSING TENURE | ||||||||
| Non‐owner occupied | 1.73 (0.67, 4.99) | 1.39 (0.91, 2.32) | N/A | 1.70 (0.48, 7.48) | 0.94 (0.32, 2.53) | N/A | N/A | 1.75 (0.85, 3.65) |
| Owner occupied | 1.88 (0.72, 5.44) | 1.13 (0.77, 1.76) | N/A | 1.88 (0.54, 9.21) | 0.78 (0.27, 2.09) | N/A | N/A | 0.96 (0.23, 4.27) |
| Interaction term (ratio of odds ratios) | 1.09 (0.64, 1.90) | 1.22 (0.88, 1.71) | N/A | 0.89 (0.43, 1.83) | 1.20 (0.61, 2.36) | N/A | N/A | 1.82 (0.32, 10.14) |
| PARENTAL UNEMPLOYMENT | ||||||||
| 1 or more parent not in paid employment | N/A | N/A | N/A | N/A | N/A | 2.72 (1.14, 6.79)* | N/A | N/A |
| Both parents in paid employment | N/A | N/A | N/A | N/A | N/A | 0.76 (0.24, 2.32) | N/A | N/A |
| Interaction term (ratio of odds ratios) | N/A | N/A | N/A | N/A | N/A | 3.56 (0.84, 15.97) | N/A | N/A |
| AGE | ||||||||
| Odds ratio at age 0 | Model does not converge | 1.13 (0.70, 1.89) | Model does not converge | 1.36 (0.89, 1.93) | 1.37 (0.50, 4.99) | 1.12 (0.74, 1.69) | 1.37 (0.52, 3.69) | 1.35 (0.71, 2.57) |
| Odds ratio at age 4 | Model does not converge | 1.30 (0.79, 2.31) | Model does not converge | 1.22 (0.54, 3.02) | 0.35 (0.04, 2.56) | 0.93 (0.66, 1.29) | 1.55 (0.80, 3.06) | 0.61 (0.14, 2.32) |
| Interaction term (ratio of odds ratios) | Model does not converge | 1.04 (0.91, 1.16) | Model does not converge | 0.97 (0.75, 1.31) | 0.72 (0.38, 1.29) | 0.96 (0.82, 1.10) | 1.03 (0.94, 1.13) | 0.82 (0.52, 1.27) |
* Fixed effect model used
Studies not included in the meta‐analyses for thermal injury prevention
Twenty‐five studies were not included in any meta‐analyses and, in addition, 14 of the 39 studies included in the meta‐analyses reported other outcomes for which meta‐analyses were not undertaken. Two of the studies reported medically attended thermal injuries (Guyer 1989; McLoughlin 1982) and neither found a reduction in injury rates amongst intervention communities. Two studies reported fire related injuries and found a significant reduction in fire related injuries in the intervention area but not in the control area (Mallonee 1996; Schwarz 1993); a third study reported fire related injuries in all age groups and did not find a significant reduction in injuries in the intervention group (DiGuiseppi 2002).
Four studies reported testing hot tap water temperature (Katcher 1989; Mock 2003; Posner 2004; Shapiro 1987); three of which found a significantly higher proportion of the intervention group had tested their hot tap water temperature (Katcher 1989; Posner 2004; Shapiro 1987). Two studies reported possession of fitted fire guards (Coggan 2000; Paul 1994); one of which reported a significant effect favouring the intervention group (Coggan 2000). Three studies reported fire setting or match play incidents (Adler 1994; Franklin 2002; Kolko 2001); two of which (Franklin 2002; Kolko 2001) reported significant reductions in the incidence of fire setting or match play behaviour favouring the intervention groups. Two studies reported turning pan handles away from the edge of stoves (Nansel 2008; Posner 2004); neither of which found a significant difference between treatment groups.
The remainder of the outcomes were each reported by only one study and significant differences were reported between treatment groups only for 12 studies. Posner 2004 reported significantly more intervention group families had spout covers for the bath and used a hot water thermometer; Katcher 1989 reported that significantly more intervention group families had tested their hot water temperature; Colver 1982 reported that significantly more intervention group families made safety changes to their homes; Garcia 1996 reported that the intervention group parents showed a significant improvement in safety behaviour; Kendrick 2007 reported that significantly more intervention group children never used matches; Hwang 2006 reported that significantly more intervention arm families had identified a meeting place outside the house in case of fire; Chan 2004 reported that intervention group parents were significantly more likely to test the temperature of micro‐waved food and to 'child proof' boilers and rice cookers; and Blake 1993 reported that significantly more intervention group parents bought and installed smoke alarms.
Harvey 2004 reported that installing alarms resulted in a higher proportion of households having functional alarms than giving vouchers for free alarms. Rowland 2002 reported that smoke alarms with ionisation sensors were more likely to be working than those with optical sensors, and those with lithium batteries were more likely to be working than those with zinc batteries; Mueller 2008 reported that significantly more families who had photoelectric alarms installed had functioning alarms than those who had ionisation alarms, at both nine and 15 months; and Yang 2008 reported that families who had lithium battery smoke alarms were more likely to have functioning alarms than those with zinc battery alarms, and that photoelectric alarms resulted in significantly fewer false alarms than ionising alarms.
Poisoning prevention
Forty‐five studies reported poisoning prevention outcomes, 27 (60%) of which had at least one outcome included in at least one meta‐analysis.
Poisonings
Analysis 3.1. The pooled incidence rate ratio (IRR) was calculated.
3.1. Analysis.

Comparison 3 Poisoning injury rates, Outcome 1 Comparing poisoning rates.
Only four studies reporting poisoning rates (Fergusson 1982; Kendrick 1999; Watson 2005; Zhao 2005) were included in the meta‐analysis. The studies by Kendrick 1999 and Watson 2005 were not adjusted for clustering as the coefficients of variation calculated from the IPD data were zero. The study by Fergusson 1982 was adjusted for clustering using a coefficient of variation of 0.25 as described above. The combined number of person years was 9206 and 8791 in the intervention and control arms respectively. There was a lack of evidence that home safety interventions with or without the provision of safety equipment reduced the rate of poisoning (IRR 0.93, 95% CI 0.65 to 1.32) and there was no significant heterogeneity between effect sizes.
Storage of medicines
Analysis 5.1. The pooled odds ratio (OR) was calculated.
5.1. Analysis.
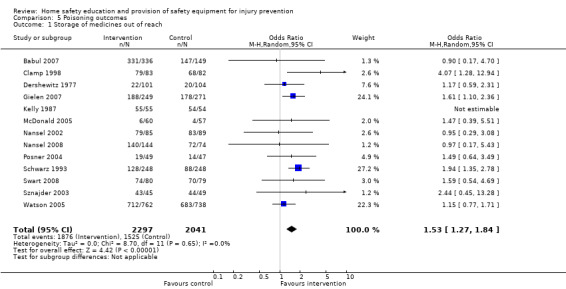
Comparison 5 Poisoning outcomes, Outcome 1 Storage of medicines out of reach.
Thirteen studies reporting storage of medicines either in locked cupboards, drawers or cabinets; stored at or above adult waist level or as being inaccessible to a child were included in the meta‐analysis (Babul 2007; Clamp 1998; Dershewitz 1977; Gielen 2007; Kelly 1987; McDonald 2005; Nansel 2002; Nansel 2008; Posner 2004; Schwarz 1993; Swart 2008; Sznajder 2003; Watson 2005). The study by Schwarz 1993 was adjusted for clustering using an ICC of 0.00012 (midpoint of a range of ICCs for injury at ward level (Kendrick 2006)) and that by Swart 2008 was adjusted using an ICC of 0.218 which was calculated from the IPD provided by the authors.
Families in the home safety interventions arms were significantly more likely to store medicines safely than control group families (OR 1.53, 95% CI 1.27 to 1.84). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an identical result. There was was no significant heterogeneity between effect sizes. Findings were robust to excluding each study in turn.
Storage of cleaning products
Analysis 5.2. The pooled odds ratio (OR) was calculated.
5.2. Analysis.
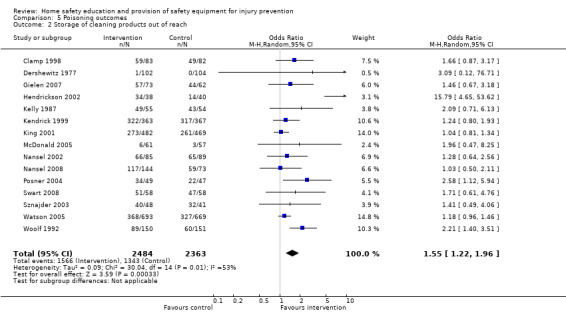
Comparison 5 Poisoning outcomes, Outcome 2 Storage of cleaning products out of reach.
Fifteen studies reporting safe storage of cleaning products, defined as for safe storage of medicines, were included in the meta‐analysis (Clamp 1998; Dershewitz 1977; Gielen 2007; Hendrickson 2002; Kelly 1987; Kendrick 1999; King 2001; McDonald 2005; Nansel 2002; Nansel 2008; Posner 2004; Swart 2008; Sznajder 2003; Watson 2005; Woolf 1992). The ICC for safe storage of cleaning products calculated from IPD for the study by Kendrick 1999 was extremely small (P < 0.00001), so this study was analysed unadjusted for clustering. The study by Swart 2008 was adjusted for clustering using an ICC of 0.359 calculated from the IPD provided by the authors.
Families in the home safety interventions arms were significantly more likely to store cleaning products safely than control group families (OR 1.55, 95% CI 1.22 to 1.96) but effect sizes varied significantly between studies. The heterogeneity may be partly explained by providing cupboard, drawer or cabinet locks, as opposed to providing education only, by study setting and follow‐up period. The effect appeared to be greater amongst studies providing locks (OR 1.87, 95% CI 1.28 to 2.72) than those providing education only (OR 1.13, 95% CI 0.92 to 1.40), although significant heterogeneity remained between effect sizes amongst studies which provided locks. Interventions delivered in clinical settings appeared to have a smaller effect (OR 1.29, 95% CI 1.10 to 1.51) than those delivered at home (OR 2.14, 95% CI 1.06 to 4.32), but the effect sizes were significantly heterogeneous amongst the latter subgroup. Heterogeneity may also be partly explained by the follow‐up period, with larger effect sizes seen in studies with follow‐up periods of three months or less (OR 1.88, 95% CI 1.33 to 2.66) than in those with longer follow‐up periods (OR 1.15, 95% CI 0.99 to 1.34); however, significant heterogeneity was found between effect sizes in those studies with shorter follow‐up periods.
Restricting the analyses to randomised studies made little difference to the findings in terms of effect size or heterogeneity (OR 1.68, 95% CI 1.26 to 2.22). Heterogeneity was partly explained by trial quality. There was some evidence that effect sizes were smaller and less heterogeneous in RCTs with adequate allocation concealment than in those without (adequate allocation concealment OR 1.21, 95% CI 1.04 to 1.40; inadequate or unclear allocation concealment OR 3.00, 95% CI 1.42 to 6.32), with significant heterogeneity in the latter subgroup. Effect sizes were similar in studies with and without blinding of outcome assessment (with blinded outcome assessment OR 1.71, 95% CI 1.10 to 2.67; without blinded outcome assessment OR 1.76, 95% CI 1.11 to 2.81), with significant heterogeneity in both subgroups. Both studies with (OR 1.77, 95% CI 1.15 to 2.71) and without (OR 1.45, 95% CI 1.03 to 2.04) follow‐up on at least 80% of participants demonstrated effects of a similar magnitude, with significant heterogeneity amongst studies with at least 80% follow‐up in both arms. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Possession of syrup of ipecac
Analysis 5.3. The pooled odds ratio (OR) was calculated.
5.3. Analysis.

Comparison 5 Poisoning outcomes, Outcome 3 Possession of syrup of ipecac.
Ten studies reporting possession of syrup of ipecac were included in the meta‐analysis (Gielen 2002; Johnston 2000; Kelly 1987; Kelly 2003; McDonald 2005; Nansel 2002; Petridou 1997; Schwarz 1993; Woolf 1987; Woolf 1992). Five were adjusted for clustering (Gielen 2002; Johnston 2000; Kelly 2003; Petridou 1997; Schwarz 1993) and adjusted numerators and denominators were rounded to the nearest integer. The study by Petridou 1997 was adjusted for clustering using an ICC of 0.0024 (estimated as midpoint of a range of ICCs published for health outcomes at the level of health authority, local authority or town). The studies by Gielen 2002; Johnston 2000 and Kelly 2003 were adjusted for clustering using an ICC of 0.0094 (midpoint of a range of ICCs calculated from IPD and from published injury outcomes at general practice, clinic, health professional level) and the study by Schwarz 1993 was adjusted for clustering using an ICC of 0.00012 (midpoint of a range of ICCs for injury at ward level) (Kendrick 2006).
Families in the home safety interventions arms were significantly more likely to possess syrup of ipecac than control group families (OR 3.34, 95% CI 1.50 to 7.44). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size OR of 3.34 (95% CI 1.50 to 7.41). Effect sizes varied significantly between studies. The heterogeneity may be partly explained by whether syrup of ipecac was provided or not, the setting in which the intervention was delivered, follow‐up period and study design. The effect size appeared to be larger in studies providing syrup of ipecac (OR 10.41, 95% CI 2.40 to 45.09) than those not providing it (OR 1.77, 95% CI 1.08 to 2.91), although significant heterogeneity remained between effect sizes for studies in both subgroups. There was some evidence that the effect size may be larger where the intervention is delivered at home (OR 5.45, 95% CI 1.22 to 24.32) as opposed to in a clinical setting (OR 2.02, 95% CI 1.08 to 3.75), although significant heterogeneity remained between effect sizes for studies in both subgroups. Smaller treatment effects were seen in studies with follow‐up periods of three months or less (OR 2.47, 95% CI 1.00 to 6.08) than in those with longer follow‐up periods (OR 4.38, 95% CI 1.36 to 14.31); however, significant heterogeneity was found between effect sizes in those studies with shorter follow‐up periods.
The effect size was much smaller amongst randomised (OR 2.25, 95% CI 1.26 to 3.99) than non‐randomised studies (OR 17.90, 95% CI 8.28 to 38.72), but there were similar effect sizes for RCTs with and without each of the quality criteria (effect sizes ranged from OR 1.60 to 3.46) and significant heterogeneity existed in five of the six subgroup analyses. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Poison control centre number accessible
Analysis 5.4. The pooled odds ratio (OR) was calculated.
5.4. Analysis.

Comparison 5 Poisoning outcomes, Outcome 4 Having a poison control centre sticker available.
Nine studies reporting having the poison control centre number accessible were included in the meta‐analysis (Hendrickson 2002; Kelly 2003; Nansel 2002; Nansel 2008; Petridou 1997; Phelan 2010; Posner 2004; Woolf 1987; Woolf 1992). One of these reported having the poison control centre number or the national emergency number (911) accessible (Hendrickson 2002). Two studies (Kelly 2003; Petridou 1997) were adjusted for clustering and adjusted numerators and denominators were rounded to the nearest integer. The study by Petridou 1997 was adjusted for clustering using an ICC of 0.0024 (estimated as midpoint of a range of ICCs published for health outcomes at the level of health authority, local authority or town) and the study by Kelly 2003 adjusted for clustering using an ICC of 0.0094 (midpoint of a range of ICCs calculated from IPD and from published injury outcomes at general practice, clinic, health professional level) (Kendrick 2006).
Families in the home safety interventions arm were significantly more likely to have the poison control centre number accessible (OR 3.30, 95% CI 1.70 to 6.39). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size OR of 3.31 (95% CI 1.70 to 6.43). The effect sizes varied significantly between studies. This heterogeneity may be partly explained by the provision of poison control centre stickers or the setting in which the education was delivered. Studies providing poison control centre stickers (OR 4.44, 95% CI 2.08 to 9.49) may have larger effect sizes to those not providing stickers (OR 2.66, 95% CI 0.93 to 7.67); effect sizes in both groups were heterogeneous. Education delivered in a clinical setting (OR 2.10, 95% CI 0.85 to 5.15) may have a smaller effect than that delivered at home (OR 5.99, 95% CI 2.08 to 17.26), but significant heterogeneity between effect sizes remained in both subgroups. Treatment effects appeared similar amongst studies with shorter (three months or less) (OR 3.54, 95% CI 1.36 to 9.22) and longer (four months or more) follow‐up periods (OR 2.98, 95% CI 1.09 to 8.09); however, significant heterogeneity was found between effect sizes in those studies with shorter follow‐up periods.
Restricting the analysis to RCTs slightly increased the effect size (OR 4.78, 95% CI 2.53 to 9.02) but made little difference to the degree of heterogeneity. There was evidence that the heterogeneity may be partly explained by trial quality and that effect sizes may be smaller in RCTs with adequate allocation concealment than in those without (adequate allocation concealment OR 2.52, 95% CI 0.92 to 8.69; inadequate or unclear allocation concealment OR 7.02, 95% CI 3.18 to 15.50), with significant heterogeneity amongst both subgroups. The effect size may be smaller amongst studies with blinded outcome assessment (OR 4.10, 95% CI 2.10 to 7.99) than amongst those without (OR 6.78, 95% CI 1.39 to 33.10) but significant heterogeneity remained in both subgroups. The effect size appeared to be larger in RCTs with follow‐up (OR 6.57, 95% CI 3.02 to 14.30) than without (OR 2.33, 95% CI 1.47 to 3.69) follow‐up of at least 80% of participants, although there was significant heterogeneity between effect sizes for RCTs in the former subgroup. Sensitivity analyses excluding each study in turn indicated that the findings were robust to the exclusion of any one study.
Storage of poisons out of reach
Analysis 5.5. The pooled odds ratio (OR) was calculated.
5.5. Analysis.
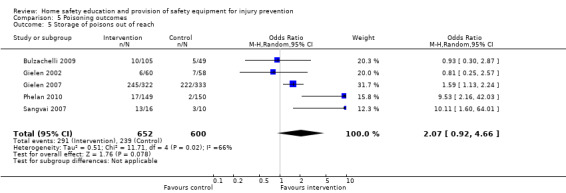
Comparison 5 Poisoning outcomes, Outcome 5 Storage of poisons out of reach.
Five studies reporting storing poisons out of reach were included in the meta‐analysis ( Bulzachelli 2009; Gielen 2002; Gielen 2007; Phelan 2010; Sangvai 2007). The study by Gielen 2002 was adjusted for clustering using an ICC of 0.0094 (midpoint of a range of ICCs calculated from IPD and from published injury outcomes at general practice, clinic, health professional level) (Kendrick 2006). Home safety interventions were not effective in increasing safe storage of poisons (OR 2.07, 95% CI 0.94 to 4.66) and there was significant heterogeneity between effect sizes. Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced an effect size OR of 2.08 (95% CI 0.92 to 4.68). The heterogeneity may be partly explained by providing cupboard, drawer or cabinet locks, as opposed to providing education only, by study setting and follow‐up period. Effect sizes may be larger in studies providing locks (OR 4.07, 95% CI 0.73 to 22.80) compared to those providing education only (OR 1.44, 95% CI 0.90 to 2.30); in those provided in the home or community (OR 2.66, 95% CI 0.22 to 31.67) than in a clinical setting (OR 1.84, 95 CI 0.75 to 4.52); and in those with longer (four months or more) (OR 3.93, 95% CI 0.64 to 23.94) rather than short (three months or less) follow‐up periods (OR 1.52, 95% CI 1.10 to 2.11). Significant heterogeneity remained in all subgroup analyses except for studies providing education only and those with shorter follow‐up periods. Restricting analyses to RCTs made little difference to the effect size (OR 2.69, 95% CI 0.96 to 7.57) or degree of heterogeneity. Heterogeneity may also be partly explained by study quality. Comparisons between RCTs with an without adequate allocation concelament or blinded outcome assessment were not possible as three of the four RCTs had adequate allocation concealment and three had unblinded outcome assessment. Effect sizes may be larger in studies with follow‐up of at least 80% of participants in each arm (OR 3.36, 95% CI 0.58 to 19.34) than without (OR 2.58, 95% CI 0.22 to 30.36). Signficant heterogeneity remained in all subgroup analyses. Sensitivity analyses excluding each study in turn indicated that findings became significant when the study by Gielen 2002 was excluded (OR 2.73, 95% CI 1.01 to 7.37).
Storage of plants out of reach
Analysis 5.6. The pooled odds ratio (OR) was calculated.
5.6. Analysis.
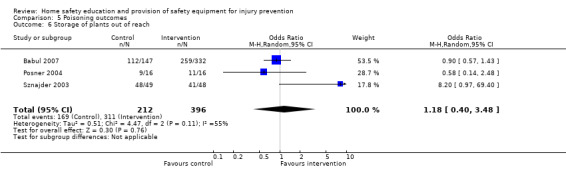
Comparison 5 Poisoning outcomes, Outcome 6 Storage of plants out of reach.
Three studies reporting storing plants out of reach (Babul 2007), plants not being accessible (Posner 2004), or not having any toxic plants in the home (Sznajder 2003) were included in the meta‐analysis. There was a lack of evidence that home safety education was effective in promoting safe storage of plants (OR 1.18, 95% CI 0.40 to 3.48) and there was no significant heterogeneity between effect sizes. Findings were robust to excluding each study in turn.
Effect of covariates on poisoning prevention outcomes
Table 3 shows the effect of the interventions by child age, gender and social group. Interventions to promote storage of poisons out of reach were significantly more effective in families with younger rather than older children. Families with employed parents were significantly more likely to possess syrup of ipecac than those with at least one parent not in paid employment. There was no evidence that interventions varied in effect with gender or the other social variables.
3. Odds ratios for poisoning prevention practices (95% credible interval) by social variables.
| Social variables | Storage of cleaning products out of reach | Possession of ipecac | Poison centre number | Storage of poisons out of reach | Storage of medicines out of reach | Plants* |
| GENDER | ||||||
| Boys | 1.63 (0.80, 3.76) | 3.21 (1.25, 8.63)* | 2.53 (0.05, 157.3) | 2.26 (0.04, 201.2) | 1.72 (0.76, 4.56) | N/A |
| Girls | 1.83 (0.89, 4.32) | 2.58 (1.02, 6.92) | 3.48 (0.07, 234.50) | 2.41 (0.04, 227.30) | 1.41 (0.64, 3.81) | N/A |
| Interaction term (ratio of odds ratios) | 0.89 (0.62, 1.27) | 1.23 (0.27, 5.83) | 0.72 (0.26, 2.00) | 0.93 (0.49, 1.75) | 1.22 (0.72, 2.00) | N/A |
| ETHNIC GROUP | ||||||
| Black and minority ethnic groups | 1.79 (1.05, 3.04) | 3.53 (1.10, 12.68) | 5.37 (1.42, 21.17) | 2.05 (0.38, 17.43) | 3.64 (0.98, 14.44) | N/A |
| White | 1.88 (1.16, 3.59) | 1.98 (0.28, 12.99) | 2.25 (0.50, 9.16) | 3.02 (0.42, 20.55) | 2.54 (0.62, 10.93) | N/A |
| Interaction term (ratio of odds ratios) | 0.94 (0.54, 1.54) | 1.79 (0.21, 17.04) | 2.40 (0.88, 7.12) | 0.73 (0.21, 2.43) | 1.43 (0.65, 3.23) | N/A |
| FAMILY TYPE | ||||||
| Single parent family | 1.74 (1.10, 3.08) | 2.67 (0.90, 8.07) | 3.64 (0.88, 15.65) | 1.59 (0.19, 16.07) | 2.60 (0.99, 7.06) | Model does not converge |
| Two parent family | 1.60 (1.09, 2.66) | 2.37 (1.00, 6.86) | 3.64 (1.04, 12.35) | 2.23 (0.22, 18.89) | 2.48 (0.99, 6.29) | Model does not converge |
| Interaction term (ratio of odds ratios) | 1.10 (0.73, 1.63) | 1.11 (0.30, 3.75) | 0.99 (0.38, 2.77) | 0.75 (0.37, 1.57) | 1.05 (0.59, 1.88) | Model does not converge |
| HOUSING TENURE | ||||||
| Non‐owner occupied | N/A | N/A | N/A | N/A | N/A | N/A |
| Owner occupied | N/A | N/A | N/A | N/A | N/A | N/A |
| Interaction term (ratio of odds ratios) | N/A | N/A | N/A | N/A | N/A | N/A |
| PARENTAL UNEMPLOYMENT | ||||||
| 1 or more parent not in paid employment | 2.00 (1.15, 3.86) | 0.38 (0.07, 2.00)* | 5.95 (0.21, 172.10) | 2.17 (0.31, 21.97) | 2.86 (0.97, 9.21) | N/A |
| Both parents in paid employment | 1.71 (1.02, 3.31) | 59.96 (4.37, 1001.00) | 6.15 (0.23, 202.90) | 2.35 (0.30, 20.73) | 2.27 (0.80, 7.56) | N/A |
| Interaction term (ratio of odds ratios) | 1.17 (0.80, 1.73) | 0.01 (0.00, 0.43) | 0.94 (0.27, 3.33) | 0.97 (0.47, 1.95) | 1.25 (0.72, 2.14) | N/A |
| AGE | ||||||
| Odds ratio at age 0 | 1.34 (0.95, 1.96) | 1.54 (0.57, 4.57) | 1.99 (0.24, 12.63) | 3.05 (0.38, 30.10) | 1.03 (0.56, 2.10) | 0.80 (0.18, 3.80) |
| Odds ratio at age 4 | 1.18 (0.84, 1.78) | 1.20 (0.38, 5.04) | 3.59 (0.44, 35.44) | 0.77 (0.09, 7.22) | 1.89 (1.02, 3.84) | 0.22 (0.01, 2.00) |
| Interaction term (ratio of odds ratios) | 0.97 (0.85, 1.10) | 0.94 (0.71, 1.26) | 1.17 (0.76, 1.84) | 0.71 (0.54, 0.93) | 1.16 (0.95, 1.43) | 0.73 (0.25, 1.53) |
* Fixed effect model used
Studies not included in the meta‐analyses for poisoning prevention outcomes
Eighteen studies were not included in any of the meta‐analyses and, in addition, 10 of the 27 studies included in the meta‐analyses also reported other outcomes for which meta‐analyses were not undertaken.
Seven studies reported poisonings (Guyer 1989; Krug 1994; Lindqvist 1998a; Scherz 1968; Steele 1985a; Steele 1985b; Woolf 1992); one of which found a significant reduction in kerosene ingestion in the intervention area as compared to the control area (Krug 1994), and a second reported a reduction in the proportion of aspirin poisonings occurring in the intervention area post‐intervention as compared to pre‐intervention but did not present denominators or a P value (Scherz 1968). The remaining five studies reported no significant difference in poisoning rates between the intervention and control groups.
Six studies reported possession of syrup of ipecac (Dawson 1989; Lacoutre 1978; LeBailly 1990; Paul 1994; Steele 1985a; Wissow 1989). Four found significant effects, three favouring the intervention group (Lacoutre 1978; LeBailly 1990; Paul 1994) and one favouring the control group (Wissow 1989). Four studies reported use of child resistant containers (CRCs) for storing medicines (Schwarz 1993), cleaning products (King 2001) or paraffin (Schwebel 2009; Swart 2008), with two finding no significant difference (King 2001; Schwebel 2009), one finding significantly more intervention group families storing paraffin in a CRC (Swart 2008), and one finding greater use of CRCs for medicines amongst control group families with borderline statistical significance (P = 0.08) (Schwarz 1993). Two studies reported possession of a carbon monoxide detector (Phelan 2010; Posner 2004) with one finding significantly more intervention group families possessed a detector (Phelan 2010).
The remaining outcomes were each reported by one study only. Six studies found a significant effect. Johnston 2000 found that the intervention group were significantly more likely to have removed poisons from their home than the control group; Schwebel 2009 found significantly more intervention group families stored paraffin away from food and were significantly less likely to store paraffin in drinks containers; Swart 2008 found that significantly more intervention group families stored beauty products safely and stored paraffin in properly labelled, tightly closed non‐glass containers; Paul 1994 found the intervention group was significantly more likely to have a lockable cabinet for storage of poisons in the kitchen post‐intervention compared to pre‐intervention; Steele 1985b found that the intervention group showed significantly more hazard reducing behaviour than the control group; and Garcia 1996 found that intervention group students showed a significant improvement in poison safety behaviour.
Falls prevention
Twenty‐five studies reported falls prevention outcomes, 16 (64%) of which had at least one outcome included in at least one meta‐analysis.
Fitted stair gates
Analysis 6.1. The pooled odds ratio (OR) was calculated.
6.1. Analysis.

Comparison 6 Falls outcomes, Outcome 1 Having a fitted stair gate.
Twelve studies reporting possessing a fitted stair gate were included in the meta‐analysis (Clamp 1998; Gielen 2002; Kendrick 1999; Kendrick 2005; King 2001; McDonald 2005; Nansel 2002; Nansel 2008; Phelan 2010; Posner 2004; Sznajder 2003; Watson 2005). Two studies reported whether stair gates were fitted and always used (Clamp 1998; Watson 2005), two reported whether stair gates or closed doors were used to prevent access to some or all stairways (Gielen 2002; McDonald 2005), and the remainder reported having at least one fitted stair gate. If studies reported that stair gates were not required because families did not have any stairs these families were included as having stair gates as they were considered safe in terms of the risk of a stairway fall. Three studies were adjusted for clustering (Gielen 2002; Kendrick 1999; Kendrick 2005) and adjusted numerators and denominators were rounded to the nearest integer. The studies by Kendrick were adjusted for clustering using ICCs of 0.0092 (Kendrick 2005) and 0.0065 (Kendrick 1999), both of which were calculated from the IPD. The study by Gielen 2002 was adjusted for clustering using an ICC of 0.0079 (midpoint of a range of ICCs calculated from IPD from studies by Kendrick 2005).
Families in the home safety interventions arms were significantly more likely to have a fitted stair gate than control group families (OR 1.61, 95% CI 1.19 to 2.17). Repeating analyses using non‐integers for numerators and denominators for clustered studies produced similar results (OR 1.61, 95% CI 1.18 to 2.18). There was significant heterogeneity between effect sizes. This heterogeneity may be partly explained by the provision of stair gates, with possibly larger effect sizes amongst studies providing (OR 2.05, 95% CI 1.08 to 3.89) than not providing gates (OR 1.26, 95% CI 0.96 to 1.64); but significant heterogeneity remained amongst studies providing gates. Studies providing the intervention in the home may also have larger effect sizes (OR 1.95, 95% CI 0.57 to 6.65) than those providing the intervention in a clinical setting (OR 1.30, 95% CI 1.19 to 1.60), but again significant heterogeneity was found amongst studies providing the intervention at home. Study design and adequate allocation concealment had little impact on findings (RCTs only OR 1.68, 95% CI 1.16 to 2.42; adequate allocation concealment OR 1.72, 95% CI 1.17 to 2.55, with significant heterogeneity in both analyses). Only two studies had blinded outcome assessment, and effect sizes were smaller amongst those studies (OR 0.92, 95% CI 0.71 to 1.18) than amongst studies without blinded outcome assessment (OR 1.97, 95% CI 1.28 to 3.04, with significant heterogeneity amongst effect sizes). Effect sizes were similar amongst studies with follow‐up on at least 80% of participants in each arm (OR 1.89, 95% CI 0.98 to 3.63, with significant heterogeneity amongst effect sizes) and those without (OR 1.46, 95% CI 1.20 to 1.76), and amongst those with shorter (three months or less) follow‐up periods (OR 1.78, 95% CI 1.22 to 2.60) and longer (four months or more) follow‐up periods (OR 1.52, 95% CI 1.00 to 2.31, with significant heterogeneity amongst effect sizes). Sensitivity analyses indicated findings were robust to excluding each study.
Possession and use of baby walker
Analysis 6.2. The pooled odds ratio (OR) was calculated.
6.2. Analysis.
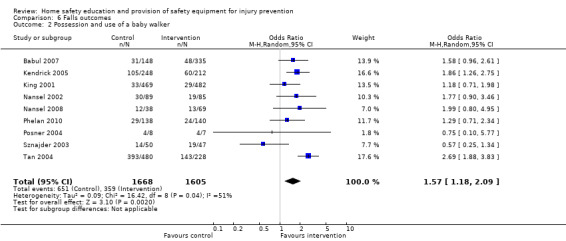
Comparison 6 Falls outcomes, Outcome 2 Possession and use of a baby walker.
Nine studies reporting baby walker possession (Kendrick 2005; King 2001; Nansel 2002; Nansel 2008; Phelan 2010) or use (Babul 2007; Posner 2004; Sznajder 2003; Tan 2004) were included in the meta‐analysis. It was considered appropriate to combine these two outcomes as a strong relationship between walker ownership and use was found in the one study that reported both outcomes for which we had IPD (Kendrick 2005). This study found that 94% of those owning a walker used it and 96% of those who used a walker owned one. The study by Kendrick 2005 was adjusted for clustering using an ICC of 0.0529 calculated from the IPD from that study and adjusted numerators and denominators were rounded to the nearest integer.
Families in the home safety interventions arms were less likely to have or use a walker than control group families (OR 1.57, 95% CI 1.18 to 2.09). Identical results were found when analyses were repeated using non‐integers for numerators and denominators for clustered studies. There was significant heterogeneity between effect sizes. This heterogeneity may be partly explained by the setting in which the intervention was delivered and the follow‐up period. Education delivered in clinical settings may be more effective in reducing walker possession and use (OR 0.46, 95% CI 0.37 to 0.59) than that delivered at home (OR 0.84, 95% CI 0.59 to 1.18), and the effect may be greater with follow‐up periods of four months or more (OR 0.58, 95% CI 0.43 to 0.79, with significant heterogeneity between effect sizes) compared to shorter follow‐up periods (OR 0.82, 95% CI 0.43 to 1.57).
Restricting analyses to randomised studies (OR 0.71, 95% CI 0.55 to 0.93) and those with adequate allocation concealment (OR 0.71, 95% CI 0.55 to 0.93) had little impact on the findings. There was some evidence that effects may be greater amongst studies without blinded outcome assessment (OR 0.69, 95% CI 0.50 to 0.96) than amongst the two studies with blinded assessment (OR 0.87, 95% CI 0.53 to 1.43) but this should be interpreted with caution due to small numbers of studies with blinded outcome assessment. Effect sizes were similar amongst those with follow‐up (OR 0.75, 95% CI 0.53 to 1.05) and without (OR 0.66, 95% CI 0.41 to 1.07) follow‐up on at least 80% of participants in each arm. Sensitivity analyses found that findings were robust to excluding each study in turn.
Possession of window locks or screens or windows with limited opening
Analysis 6.3. The pooled odds ratio (OR) was calculated.
6.3. Analysis.
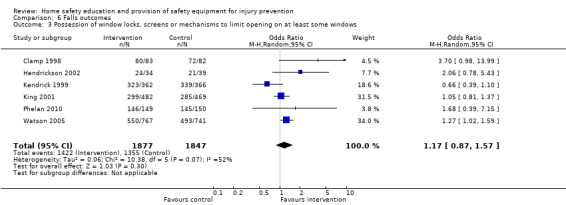
Comparison 6 Falls outcomes, Outcome 3 Possession of window locks, screens or mechanisms to limit opening on at least some windows.
Six studies reporting possession of window locks (Clamp 1998; Kendrick 1999; Watson 2005), screens (Hendrickson 2002), windows with opening limited to no more than six inches (King 2001) or working window guards, locks or restricted openings of less than 10 cm (Phelan 2010) were included in the meta‐analysis. The ICC for window locks calculated from the IPD for the study by Kendrick was extremely small (P < 0.00001) hence this study was not adjusted for clustering.
Families in the home safety interventions arms were not significantly more likely to possess window locks than control group families (OR 1.17, 95% CI 0.87 to 1.57) and effect sizes varied significantly between studies. Effect sizes were similar in studies providing window locks (OR 1.21, 95% CI 0.67 to 2.11, with significant heterogeneity between effect sizes) and those not providing locks (OR 1.24, 95% CI 0.71 to 2.18), and those delivered in clinical settings (OR 1.18, 95% CI 0.62 to 2.25, with significant heterogeneity between effect sizes) and those delivered at home (OR 1.12, 95% CI 0.87 to 1.45). The heterogeneity may be partly explained by follow‐up period, with a larger effect found in studies with follow‐up periods of three months or less (OR 2.52, 95% CI 1.15 to 5.52) than in those with longer follow‐up periods (OR 1.06, 95% CI 0.81 to 1.39). There was some evidence that interventions may be effective amongst RCTs (OR 1.26, 95% CI 1.00 to 1.59) including those with non‐blinded outcome assessment (OR 1.43, 95% CI 1.05 to 1.96). Effects were not significant for RCTs with adequate allocation concealment (OR 1.22, 95% CI 0.96 to 1.55) and those with follow‐up on at least 80% of participants (OR 1.53, 95% CI 0.87 to 2.68). Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Possession of non‐slip bath mats or decals
Analysis 6.4. The pooled odds ratio (OR) was calculated.
6.4. Analysis.
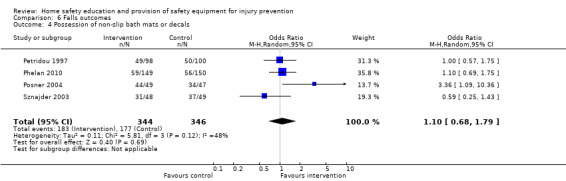
Comparison 6 Falls outcomes, Outcome 4 Possession of non‐slip bath mats or decals.
Three studies reporting possession of non‐slip bath mats (Petridou 1997; Phelan 2010; Sznajder 2003) and one reporting possession of non‐slip bath decals (Posner 2004) were included in the meta‐analysis. The study by Petridou was adjusted for clustering using an ICC of 0.0024 (estimated as the midpoint of a range of ICCs published for health outcomes at the level of health authority, local authority or town) (Kendrick 2006) and adjusted numerators and denominators were rounded to the nearest integer.
Intervention arm families were not significantly more likely to have non‐slip bath mats or decals (OR 1.10, 95% CI 0.68 to 1.79). Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced similar findings (OR 1.10, 95% CI 0.68 to 1.78). There was no significant heterogeneity between effect sizes. Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Does not leave child alone on high surface
Analysis 6.5. The pooled odds ratio (OR) was calculated.
6.5. Analysis.
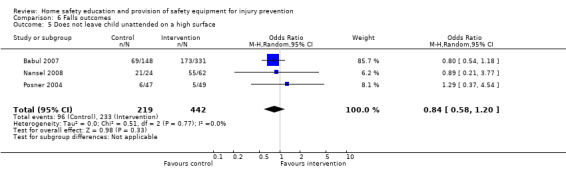
Comparison 6 Falls outcomes, Outcome 5 Does not leave child unattended on a high surface.
Three studies reported never leaving a child alone on a high surface (Babul 2007; Nansel 2008; Posner 2004). Intervention arm families were not significantly more likely to never have left a child alone on a high surface (OR 0.84, 95% CI 0.58 to 1.20) and there was no significant heterogeneity amongst effect sizes. Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Effect of covariates on falls prevention practices
Table 4 shows the effect of the interventions by child age, gender and social group. There was no evidence that the interventions varied in effect with child age, ethnic group or parental unemployment. Interventions were significantly more effective in increasing stair gate possession amongst families living in non‐owner occupied accommodation and in increasing window lock possession amongst families with male children. Analyses were not possible for baby walkers and high surfaces for child age due to the outcomes not being relevant to older children.
4. Odds ratios for falls prevention practices (95% credible interval) by social variables.
| Social variables | Fitted stair gate | No baby walker | Non‐slip bath mat | Window locks | Not leaving child unattended on high surfaces |
| GENDER | |||||
| Boys | 1.64 (0.85, 3.31) | 0.67 (0.32, 1.37) | N/A | 1.45 (0.80, 2.92) | N/A |
| Girls | 1.92 (0.99, 3.85) | 1.04 (0.49, 2.18) | N/A | 0.85 (0.46, 1.70) | N/A |
| Interaction term (ratio of odds ratios) | 0.86 (0.62, 1.18) | 0.64 (0.26, 1.59) | N/A | 1.72 (1.16, 2.57) | N/A |
| ETHNIC GROUP | |||||
| Black and minority ethnic groups | 1.98 (1.17, 3.34) | 0.77 (0.29, 2.49) | N/A | 1.58 (0.58, 5.11) | N/A |
| White | 1.65 (1.01, 2.76) | 1.03 (0.30, 2.59) | N/A | 1.36 (0.57, 3.43) | N/A |
| Interaction term (ratio of odds ratios) | 1.19 (0.77, 1.85) | 0.79 (0.33, 2.02) | N/A | 1.13 (0.62, 2.05) | N/A |
| FAMILY TYPE | |||||
| Single parent family | 2.03 (1.16, 3.62) | 0.89 (0.32, 2.46) | 0.60 (0.16, 1.99)* | 0.98 (0.37, 3.19) | N/A |
| Two parent family | 1.82 (1.12, 3.02) | 0.92 (0.41, 1.87) | 1.00 (0.69, 1.44) | 1.51 (0.63, 4.76) | N/A |
| Interaction term (ratio of odds ratios) | 1.11 (0.75, 1.65) | 0.99 (0.44, 2.24) | 0.60 (0.15, 2.14) | 0.65 (0.40, 1.05) | N/A |
| HOUSING TENURE | |||||
| Non‐owner occupied | 1.98 (1.48, 2.66) | 1.22 (0.48, 2.93) | N/A | 1.13 (0.03, 54.7)* | 0.44 (0.04, 3.65)* |
| Owner occupied | 1.22 (0.96, 1.61) | 1.36 (0.53, 3.34) | N/A | 1.48 (0.04, 75.5) | 2.51 (0.58, 13.06) |
| Interaction term (ratio of odds ratios) | 1.62 (1.18, 2.24) | 0.90 (0.54, 1.47) | N/A | 0.76 (0.50, 1.17) | 0.18 (0.003, 5.76) |
| PARENTAL UNEMPLOYMENT | |||||
| 1 or more parent not in paid employment | 2.08 (0.77, 5.86) | 0.39 (0.14, 1.04)* | 2.07 (0.91, 4.78)* | 1.40 (0.58, 4.23) | N/A |
| Both parents in paid employment | 1.82 (0.67, 5.01) | 0.87 (0.49, 1.51) | 0.91 (0.59, 1.42) | 1.40 (0.63, 4.49) | N/A |
| Interaction term (ratio of odds ratios) | 1.15 (0.77, 1.71) | 0.45 (0.14, 1.40) | 2.28 (0.88, 5.86) | 0.98 (0.62, 1.55) | N/A |
| AGE | |||||
| Odds ratio at age 0 | 1.40 (1.02, 2.06) | N/A due to age of walker use | 1.16 (0.80, 1.71)* | 1.00 (0.30, 4.87) | N/A due to age for leaving child on high surfaces |
| Odds ratio at age 4 | 1.26 (0.81, 2.02) | N/A due to age of walker use | 1.08 (0.78, 1.50) | 1.27 (0.35, 5.84) | N/A due to age for leaving child on high surfaces |
| Interaction term (ratio of odds ratios) | 0.97 (0.84, 1.13) | N/A due to age of walker use | 0.98 (0.90, 1.06) | 1.06 (0.90, 1.23) | N/A due to age for leaving child on high surfaces |
* Fixed effect model used
Data not included in the meta‐analysis
Nine studies were not included in any of the meta‐analyses and, in addition, seven of the 16 studies included in the meta‐analyses also reported other outcomes for which meta‐analyses were not undertaken.
Three studies reported the safety of balconies (Paul 1994; Petridou 1997; Sznajder 2003), none of which found a significant effect. Three reported use or acquisition of a stair gate (Coggan 2000; Emond 2002; Wissow 1989), two of which reported a significant effect favouring the intervention group (Coggan 2000; Emond 2002). Two reported having handrails on indoor or outdoor stairs (Hendrickson 2002; Paul 1994); having carpets or rugs fixed to floors (Kendrick 1999; Sznajder 2003); high chair safety (Paul 1994; Sznajder 2003); and limiting window opening widths (King 2001; Paul 1994), none of which demonstrated a significant effect. The remainder of the outcomes were reported by one study only. Chan 2004 demonstrated a significant effect favouring the intervention group for child proofing window frames and for avoiding staggered furniture layout and Paul 1994 demonstrated a significant effect favouring the intervention group for reducing accessibility of roof areas. One reporting outdoor stair safety (Petridou 1997) and one reporting the number of safety changes made to the home (Colver 1982) reported significant effects favouring the intervention group. No significant effects were demonstrated for any other outcomes.
Electrical injury prevention
Use of socket covers
Analysis 7.1. The pooled odds ratio (OR) was calculated.
7.1. Analysis.
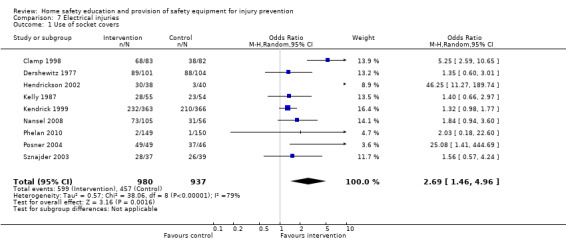
Comparison 7 Electrical injuries, Outcome 1 Use of socket covers.
Nine studies reported the use of socket covers (Clamp 1998; Dershewitz 1977; Hendrickson 2002; Kelly 1987; Kendrick 1999; Nansel 2008; Phelan 2010; Posner 2004; Sznajder 2003). This was defined as use of socket covers (Dershewitz 1977), use of socket covers on all unused outlets (Clamp 1998; Nansel 2008), often or always using socket covers on unused outlets (Kendrick 1999; Posner 2004), using socket covers on unused outlets (Kelly 1987; Sznajder 2003), or not having uncovered electrical outlets visible (Phelan 2010) or accessible to children (Hendrickson 2002). The ICC for using socket covers calculated from IPD for the study by Kendrick 1999 was extremely small (P < 0.00001) so this study was analysed unadjusted for clustering.
Families in the home safety interventions arms were significantly more likely to use socket covers than those not receiving home safety interventions (OR 2.69, 95% CI 1.46 to 4.96), and effect sizes varied significantly between studies. The heterogeneity was partly explained by the provision of socket covers, with studies providing covers appearing to have a greater effect (OR 3.54, 95% CI 1.45 to 8.64) than those not providing covers (OR 1.76, 95% CI 1.02 to 3.03), and RCTs appearing to have a greater effect (OR 3.68, 95% CI 1.47 to 9.20) than other designs (OR 1.39, 95% CI 1.06 to 1.83); but significant heterogeneity remained between effect sizes for studies providing locks and for RCTs. Interventions provided at home (OR 5.45, 95% CI 0.49 to 60.69) may have larger effect sizes than those provided in clinical settings (OR 2.01, 95% CI 1.18 to 3.40), but significant heterogeneity remained in both subgroup analyses. Studies with shorter follow‐up periods (three months or less) appeared to have a greater effect (OR 4.06, 95% CI 1.59 to 10.32) than those with longer follow‐up periods (four months or more) (OR 1.33, 95% CI 1.01 to 1.76), with significant heterogeneity in the former subgroup analysis. Effect sizes were similar in studies with (OR 3.53, 95% CI 1.35 to 9.19) and without adequate allocation concealment (OR 3.97, 95% CI 0.68 to 23.26). The same subset of studies had follow‐up on at least 80% of participants in each arm and non‐blinded outcome assessment, and effect sizes appeared larger in these studies (OR 5.44, 95% CI 1.39 to 21.24) than in those with lower levels of follow‐up and blinded outcome assessment (OR 1.76, 95% CI 0.72 to 4.34); with significant heterogeneity between effect sizes in the former group of studies. Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Effect of covariates on use of socket covers
Table 5 shows the effect of the interventions by child age, gender and social group. There was no evidence that the effect of interventions to increase use of socket covers varied by child age, gender or any of the social variables.
5. Odds ratios for use of socket covers (95% credible interval) by social variables.
| Social variables | Socket covers |
| GENDER | |
| Boys | 0.50 (0.00, 53.26) |
| Girls | 1.17 (0.00, 129.70) |
| Interaction term (ratio of odds ratios) | 2.36 (0.68, 8.27) |
| ETHNIC GROUP | |
| Black and minority ethnic groups | 1.96 (0.09, 29.00) |
| White | 1.25 (0.05, 18.05) |
| Interaction term (ratio of odds ratios) | 1.59 (0.56, 4.49) |
| FAMILY TYPE | |
| Single parent family | 2.15 (0.45, 11.07) |
| Two parent family | 2.58 (0.63, 11.85) |
| Interaction term (ratio of odds ratios) | 0.82 (0.33, 2.11) |
| HOUSING TENURE | |
| Non‐owner occupied | 0.68 (0.00, 111.70) |
| Owner occupied | 0.25 (0.00, 38.68) |
| Interaction term (ratio of odds ratios) | 2.76 (0.76, 11.09) |
| PARENTAL UNEMPLOYMENT | |
| 1 or more parent not in paid employment | Model does not converge |
| Both parents in paid employment | Model does not converge |
| Interaction term (ratio of odds ratios) | Model does not converge |
| AGE | |
| Odds ratio at age 0 | 0.86 (0.01, 32.12) |
| Odds ratio at age 4 | 0.38 (0.00, 14.98) |
| Interaction term (ratio of odds ratios) | 0.76 (0.51, 1.11) |
Data not included in the meta‐analysis
Seven studies reported a range of outcomes not included in the meta‐analysis. Three reported use of socket covers (Emond 2002; LeBailly 1990; Wissow 1989), with two studies (Emond 2002; LeBailly 1990) reporting that the intervention group was significantly more likely to have socket covers than the control group. Two reported use of circuit breakers (Paul 1994; Petridou 1997), with one study reporting a significant effect favouring the intervention group (Petridou 1997). The remaining outcomes were reported by one study only. Chan 2004 found intervention group parents were more likely to report child proofing electrical heating devices; but no effect of the intervention was found for the other outcomes reported by the other studies.
Prevention of lacerations and bruising
Storage of sharp objects
Analysis 8.1. The pooled odds ratio (OR) was calculated.
8.1. Analysis.
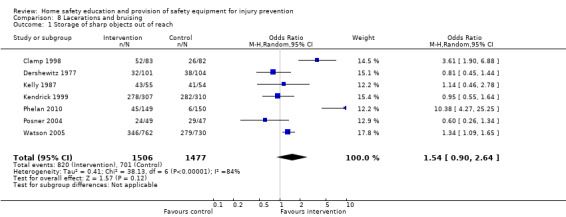
Comparison 8 Lacerations and bruising, Outcome 1 Storage of sharp objects out of reach.
Seven studies reporting storage of sharp objects were included in the meta‐analysis. This was defined as storage of sharp objects at or above adult eye level or in locked cupboards or drawers (Clamp 1998; Watson 2005), storage of sharp objects in locked cupboards or drawers (Posner 2004), always stores sharp objects out of reach (Kendrick 1999), unsafe storage of sharp objects (Phelan 2010), or knives not accessible (Kelly 1987) or stored out of reach (Dershewitz 1977). The study by Kendrick 1999 was adjusted for clustering using an ICC of 0.0094, calculated from the IPD from that study, and adjusted numerators and denominators were rounded to the nearest integer.
Families in the home safety interventions arms were not significantly more likely to store sharp objects safely than those in the control arms (OR 1.54, 95% CI 0.90 to 2.64). Identical results were found when analyses were repeated using non‐integers for numerators and denominators for clustered studies. There was significant heterogeneity between effect sizes. Six of the seven studies provided locks, six were also RCTs and six provided the intervention in clinical settings, so exploration of differential effects by the provision of locks, study design and setting was not possible. Studies with a longer follow‐up period (four or more months) (OR 1.85, 95% CI 0.86 to 3.96) may possibly have a slightly larger effect size than those with shorter follow‐up periods (three months or less) (OR 1.22, 95% CI 0.41 to 3.62), but significant heterogeneity remained in both subgroup analyses. RCTs with adequate allocation concealment (OR 2.27, 95% CI 0.88 to 5.87) may have a larger effect size than those without (OR 0.89, 95% CI 0.55 to 1.45), with significant heterogeneity in the former subgroup analysis. Those with non‐blinded outcome assessment (OR 3.47, 95% CI 1.09 to 11.11) appeared to have a larger effect size than those with blinded assessment (OR 0.80, 95% CI 0.53 to 1.22), with significant heterogeneity in the former subgroup analysis. Those with follow‐up on at least 80% of participants in each arm had a larger effect size (OR 5.86, 95% CI 2.06 to 16.64) than those without (OR 1.02, 95% CI 0.69 to 1.50), again with significant heterogeneity in the former subgroup analysis. Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Effect of covariates on storage of sharp objects
Table 6 shows the effect of the interventions by child age, gender and social group. There was no evidence that the effect of interventions to increase safe storage of sharp objects varied by child age, gender, ethnic group, housing tenure or parental unemployment. The effect of interventions by family type differed according to whether the variance within and between studies was modelled jointly or separately. Modelling the variance jointly indicated there was no significant difference in the intervention effect between single and two parent families. However, when the variance within and between studies was modelled separately, interventions appeared to be more effective in two parent families in the between variance model (OR single parent family 0.003, 95% CI 1.4 x 10‐5 to 0.18; OR two parent family 9.78, 95% CI 0.22 to 80.38), interaction term 2.3 x 10‐4 (95% CI 5.4 x 10‐6 to 0.01) than in the within variance model (OR single parent family 12.76, 95% CI 0.28 to 1045; OR two parent family 9.78, 95% CI 0.22 to 80.38), interaction term 1.30 (95% CI 0.84 to 2.00); difference between the within study variance and between study variance models 8.66 (95% CI 4.90 to 12.38). Caution should be exercised in interpreting these findings due to the small number of studies in these analyses (four IPD studies and two summary data only studies).
6. Odds ratios for storage of sharp objects out of reach (95% credible interval) by social variables.
| Social variables | Sharp objects |
| GENDER | |
| Boys | 0.56 (0.04, 7.78) |
| Girls | 0.49 (0.03, 6.79) |
| Interaction term (ratio of odds ratios) | 1.15 (0.78, 1.66) |
| ETHNIC GROUP | |
| Black and minority ethnic groups | 0.77 (0.16, 3.54) |
| White | 0.85 (0.18, 3.72) |
| Interaction term (ratio of odds ratios) | 0.92 (0.53, 1.58) |
| FAMILY TYPE* | |
| Single parent family | 0.95 (0.22, 4.11) |
| Two parent family | 0.85 (0.21, 3.58) |
| Interaction term (ratio of odds ratios) | 1.12 (0.72, 1.76) |
| HOUSING TENURE | |
| Non‐owner occupied | 1.58 (0.55, 4.54) |
| Owner occupied | 1.18 (0.40, 3.27) |
| Interaction term (ratio of odds ratios) | 1.36 (0.92, 2.02) |
| PARENTAL UNEMPLOYMENT | |
| 1 or more parent not in paid employment | 0.91 (0.11, 6.46) |
| Both parents in paid employment | 0.70 (0.09, 4.91) |
| Interaction term (ratio of odds ratios) | 1.29 (0.87, 1.93) |
| AGE | |
| Odds ratio at age 0 | 1.89 (0.50, 7.22) |
| Odds ratio at age 4 | 1.58 (0.41, 6.24) |
| Interaction term (ratio of odds ratios) | 0.96 (0.83, 1.09) |
* See text for odds ratios from modelling within and between study variance separately
Data not included in the meta‐analysis
Eight studies included a range of outcomes not included in the meta‐analysis. Three studies reported protecting sharp corners or edges of benchtops (Kelly 1987; Paul 1994; Sznajder 2003); two of which found a significant effect favouring the intervention group (Paul 1994; Sznajder 2003). One study reported storage of pins and needles out of reach (Dershewitz 1977) and one reported storage of sharp objects out of reach (Wissow 1989); neither demonstrated a significant effect. One study reported five outcomes related to lawn mower safety and found significant effects favouring the intervention group for not leaving the motor running and making children stay indoors whilst the lawn was being mowed (Mayer 1998). One study reported use of devices to prevent doors closing completely and found a significant effect favouring the intervention group (Clamp 1998). One study reported laceration injury rates pre‐ and post‐intervention for intervention and control areas (Bentzen 1997). Both pre‐ and post‐intervention rates varied greatly between areas, with exceedingly low rates in the control area at both timepoints; so it may not be reasonable to compare injury rates between areas. Other outcomes were reported by one study only and none found any significant effects.
Suffocation prevention
Keeping small objects out of reach of children
Analysis 9.1. The pooled odds ratio (OR) was calculated.
9.1. Analysis.
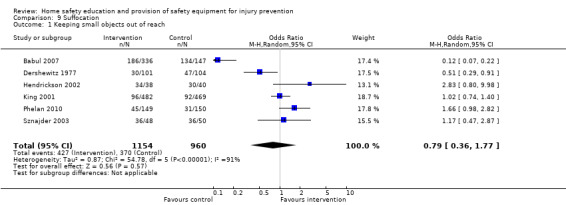
Comparison 9 Suffocation, Outcome 1 Keeping small objects out of reach.
Six studies reporting keeping small objects out of reach of children were included in the meta‐analysis. They defined out of reach as no small objects within a child's reach in the living room (King 2001), small objects usually (Sznajder 2003) or always (Babul 2007) kept out of a child's reach, coins out of reach (Dershewitz 1977), small items not accessible (Hendrickson 2002), and objects smaller than a ping‐pong ball visible on surfaces less than one metre from the floor (Phelan 2010).
There was a lack of evidence that home safety interventions were effective in encouraging parents to keep small objects out of reach of children (OR 0.79, 95% CI 0.36 to 1.77), with significant heterogeneity between effect sizes. All included studies were RCTs and all but one delivered the intervention at home, hence differential effects by study design and setting were not possible. Effect sizes were similar amongst studies with shorter (three months or less) (OR 1.05, 95% CI 0.41 to 2.69) and with longer follow‐up periods (four months or more) (OR 0.60, 95% CI 0.16 to 2.30), with significant heterogeneity amongst both subgroup analyses. Effect sizes were also similar amongst RCTs with (OR 0.70, 95% CI 0.24 to 2.07) and without (OR 1.10, 95% CI 0.21 to 5.81) adequate allocation concealment, with significant heterogeneity in the former subgroup analysis, and amongst those with (OR 0.76, 95% CI 0.39 to 1.47) and without (OR 0.87, 95% CI 0.19 to 4.00) blinded outcome assessment, with significant heterogeneity between effect sizes in both subgroup analyses. Effect sizes appeared larger in studies with follow‐up on at least 80% of participants in each arm (OR 1.29, 95% CI 0.90 to 1.85) than those without (OR 0.25, 95% CI 0.06 to 1.05), but there was significant heterogeneity between effect sizes in the latter subgroup analysis. Sensitivity analyses excluding each study in turn indicated that findings were robust to the exclusion of any one study.
Effect of covariates on storage of small objects
Table 7 shows the effect of the interventions by child age, gender and social group. The interventions were significantly more effective amongst families with older rather than younger children and were more effective amongst families where at least one parent was not in paid employment rather than families in which both parents were in paid employment. Interventions did not differ in effect by gender or family type.
7. Odds ratios for storage of small objects out of reach (95% credible interval) by social variables.
| Social variables | Storage of small objects out of reach |
| GENDER | |
| Boys | 0.35 (0.20, 0.62) |
| Girls | 0.14 (0.06, 0.27) |
| Interaction term (ratio of odds ratios) | 2.54 (0.86, 7.91) |
| ETHNIC GROUP | |
| Black and minority ethnic groups | N/A |
| White | N/A |
| Interaction term (ratio of odds ratios) | N/A |
| FAMILY TYPE | |
| Single parent family | 0.72 (0.19, 2.86) |
| Two parent family | 0.38 (0.28, 0.52) |
| Interaction term (ratio of odds ratios) | 1.90 (0.44, 8.31) |
| HOUSING TENURE | |
| Non‐owner occupied | N/A |
| Owner occupied | N/A |
| Interaction term (ratio of odds ratios) | N/A |
| PARENTAL UNEMPLOYMENT | |
| 1 or more parent not in paid employment | 1.90 (0.79, 4.89) |
| Both parents in paid employment | 0.63 (0.38, 1.04) |
| Interaction term (ratio of odds ratios) | 3.02 (1.06, 9.04) |
| AGE | |
| Odds ratio at age 0 | 0.03 (0.01, 0.08) |
| Odds ratio at age 4 | 43.43 (10.06, 179.00) |
| Interaction term (ratio of odds ratios) | 6.37 (3.43, 11.73) |
Data not included in the meta‐analysis
Nine studies reported outcomes not included in the meta‐analyses (Babul 2007; Campbell 2001; Dershewitz 1977; Hendrickson 2002; Kendrick 1999; Paul 1994; Pless 2007; Posner 2004; Zhang 2003). Only one study found any significant effects of home safety interventions, which were for preventing children from eating nuts and using a small parts tester (Posner 2004).
Drowning prevention
Never leaving child alone in the bath
Analysis 10.1. The pooled odds ratio (OR) was calculated.
10.1. Analysis.
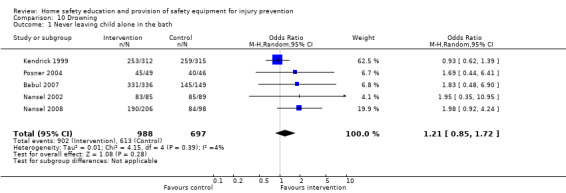
Comparison 10 Drowning, Outcome 1 Never leaving child alone in the bath.
Five studies reporting never leaving a child alone in the bath (Babul 2007; Kendrick 1999; Nansel 2002; Nansel 2008; Posner 2004) were included in the meta‐analysis. The study by Kendrick was adjusted for clustering using an ICC of 0.0082, calculated from the IPD from that study, and adjusted numerators and denominators were rounded to the nearest integer.
There was a lack of evidence that home safety interventions were effective in preventing children being left alone in the bath (OR 1.21, 95% CI 0.85 to 1.72), with no significant heterogeneity amongst effect sizes. Repeating the analyses using non‐integers for the numerators and denominators for cluster randomised studies produced a similar effect size (OR 1.22, 95% CI 0.85 to 1.75). Sensitivity analyses excluding each study in turn indicated that findings became significant when the study by Kendrick was excluded (OR 1.89, 95% CI 1.08 to 3.32).
Effect of covariates on never leaving child alone in the bath
Table 8 shows the effect of the interventions by child age, gender and social group. The effect of interventions did not differ by child age, gender or any of the social variables.
8. Odds ratios for never leaving a child alone in the bath (95% credible interval) by social variables.
| Social variables | Bath Alone |
| GENDER | |
| Boys | 1.17 (0.51, 3.12) |
| Girls | 1.73 (0.75, 4.97) |
| Interaction term (ratio of odds ratios) | 0.67 (0.29, 1.53) |
| ETHNIC GROUP | |
| Black and minority ethnic groups | 0.89 (0.23, 5.04) |
| White | 1.0 (0.25, 5.46) |
| Interaction term (ratio of odds ratios) | 0.89 (0.33, 2.45) |
| FAMILY TYPE | |
| Single parent family | 0.53 (0.14, 1.93)* |
| Two parent family | 1.13 (0.71, 1.83) |
| Interaction term (ratio of odds ratios) | 0.47 (0.11, 1.82) |
| HOUSING TENURE | |
| Non‐owner occupied | 1.80 (0.76, 4.34) |
| Owner occupied | 1.05 (0.45, 2.86) |
| Interaction term (ratio of odds ratios) | 1.68 (0.68, 4.09) |
| PARENTAL UNEMPLOYMENT | |
| 1 or more parent not in paid employment | N/A |
| Both parents in paid employment | N/A |
| Interaction term (ratio of odds ratios) | N/A |
| AGE | |
| Odds ratio at age 0 | 0.62 (0.17, 2.14) |
| Odds ratio at age 4 | 3.02 (0.66, 18.18) |
| Interaction term (ratio of odds ratios) | 1.50 (0.96, 2.43) |
* Fixed effect model used
Data not included in the meta‐analysis
Six studies reported a range of outcomes not included in the meta‐analysis. Five studies reported domestic swimming pool fencing (Babul 2007; Coggan 2000; Girasek 2010; Nansel 2002; Paul 1994); one of which found the intervention group were significantly more likely to acquire pool fencing (Coggan 2000). One study reported never leaving a child alone in the area of a paddling or swimming pool and never leaving a paddling pool full of water after use (Nansel 2002), and did not find significant effects for either of these outcomes. Finally one study found no significant difference in drowning mortality rates (Zhang 2003).
Home hazard or safety scores
Nineteen studies reported a range of home hazard scores or safety scores with little consistency in the tools used to measure hazards or safety, which precluded meta‐analyses for these outcomes.
Data not included in the meta‐analysis
Nine of the studies reporting home hazard or home safety scores reported significantly safer scores amongst intervention group families (Kelly 1987; Llewellyn 2003; Nansel 2002; Odendaal 2008; Olds 1994; Phelan 2010; Posner 2004; Schwebel 2009; Swart 2008). Seven studies found no significant difference between scores for the intervention and control groups (Dershewitz 1977; Gielen 2002; Guyer 1989; Paul 1994; Petridou 1997; Vineis 1994; Wissow 1989). One study reported only pre‐post changes in the score in intervention and control arms separately, stratified by child age and deprivation, type (advice versus use of equipment) and location (household, recreation and transport) of preventive activity (Mock 2003). They found significant improvements in scores in the intervention group but not the control group within most strata. One study reported the number of families making safety changes to their homes and reported a significantly greater number of intervention group families making safety changes than control group families (Colver 1982). The final study did not report the results for the overall score (Chan 2004) but did report significant improvements for some components of the score.
Assessment of publication bias
Only three safety practices outcomes had 10 or more studies and publication bias assessment was restricted to these. Specifically, the following P values for tests of asymmetry were obtained: ownership of a functioning smoke alarm (P = 0.063), ownership of syrup of ipecac (P = 0.761), and safe hot water temperature (P = 0.251). Hence, while no test attained a significant result at the 5% level, the P value for ownership of a functioning smoke alarm was low, indicating some concern publication biases may be present. A contour enhanced funnel plot for functioning smoke alarms is presented in Figure 2. Our interpretation of this is somewhat inconclusive, but the possibility of studies with non‐significant findings in the white region to the left of the data being missing is evident, and this would be consistent with publication bias mechanisms. Application of the regression bias adjustment method to this outcome resulted in a diminished OR of 1.44 (95% CI 1.07 to 1.92) compared to an OR of 1.79 (95% CI 1.28 to 2.50) without adjustment.
2.
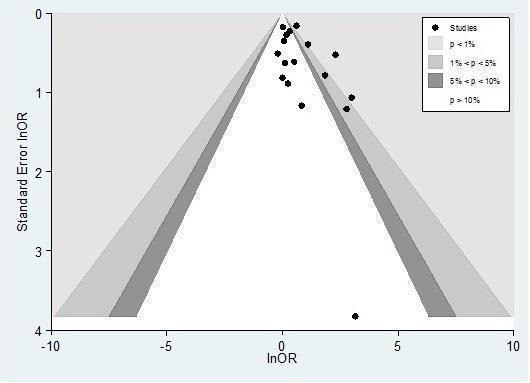
Contour enhanced funnel plot for possession of a functioning smoke alarm
Publication bias was also assessed for medically attended or self reported injuries, as more than 10 studies were included in these analyses. There was some evidence of asymmetry for the analyses adjusted for baseline injury rates (P = 0.082 for analysis including all injuries from Phelan 2010 and P = 0.06 for analysis including only preventable injuries from Phelan 2010). However, contour enhanced funnel plots do not show a pattern of studies consistent with publication bias based on statistical significance (Figure 3 and Figure 4). There was no evidence of publication bias in the analyses unadjusted for baseline injury rates (P = 0.495 for analysis including all injuries from Phelan 2010 and P = 0.366 for analyses including only preventable injuries from Phelan 2010).
3.
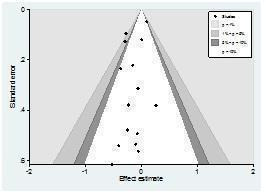
Contour enhanced funnel plot for medically attended or self reported injuries adjusted for baseline injury rates (including all injuries from Phelen 2010)
4.
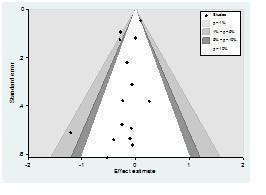
Contour enhanced funnel plot for medically attended or self reported injuries adjusted for baseline injury rates (including only preventable injuries from Phelen 2010)
Discussion
Summary of main results
There was a lack of evidence that home safety interventions were effective in reducing rates of thermal injuries or poisonings. There was some evidence that home safety interventions may be effective in reducing rates of all injuries combined, especially when follow‐up injury rates from CBA studies were adjusted for baseline injury rates.
Home safety interventions were effective in increasing a wide range of safety practices including having a safe hot tap water temperature, a functional smoke alarm, having or practising a fire escape plan, storing medicines and cleaning products out of reach, having syrup of ipecac and the poison control centre number accessible, having a fitted stair gate, not using a baby walker and using socket covers on unused sockets. There was some evidence that home safety interventions were effective in increasing use of fire guards. Effect sizes appeared to be larger for interventions that provided safety equipment than for those that provided education alone for having a functional smoke alarm, storing cleaning products out of reach, having syrup of ipecac, having the poison control number accessible, having a fitted stair gate and using socket covers on unused sockets. All of the studies reporting fire guard use included in the meta‐analyses provided fire guards. Effect sizes also appeared greater where interventions were delivered in the home as opposed to in clinical settings for having a safe hot water temperature, having a functional smoke alarm, storing cleaners out of reach, having syrup of ipecac and the poison control centre number accessible, having a fitted stair gate and socket covers. The effect of home safety interventions appeared to diminish with time, with greater effects demonstrated for having a functional smoke alarm, storing cleaning products out of reach, having window locks and socket covers over a shorter (three months or less) than a longer time period. However, significant effects were found for follow‐up periods of four months or more for having a safe hot tap water temperature, a functional smoke alarm, a fitted fire guard, syrup of ipecac, having the poison control centre number accessible, having a fitted stair gate, not using a baby walker and using socket covers on unused sockets.
Overall, there was a lack of evidence that home safety interventions were effective in increasing possession of non‐slip bath mats and decals or fire extinguishers, or in preventing children being left alone on high surfaces or in the bath, keeping hot food and drinks out of reach, checking smoke alarm batteries, or storing matches, sharp objects, small objects, poisons or plants out of reach. The number of studies and participants were small (≤ six studies and ≤ 1000 participants per arm) for eight of these outcomes. There was also a lack of evidence of the effect of home safety interventions on having window locks and screens or windows with limited opening, but subgroup analyses suggested that the interventions may be effective in the shorter, but not the longer term.
Overall, there was no consistent evidence that home safety interventions were less effective amongst children at greater risk of injury. There was evidence of differential effectiveness in only seven of 96 (7%) meta‐regression analyses. This is encouraging as it suggests that home safety interventions should not widen existing inequalities in child home injury rates.
Overall completeness and applicability of evidence
This is the largest and most comprehensive published systematic review and meta‐analysis assessing the effect of home safety education, with or without the provision of safety equipment, to date. It remains the only published review in the field of child home injury prevention to obtain individual participant data (IPD) and to use this in a series of meta‐analyses and meta‐regressions to quantify the effect of interventions by age, gender and social group.
More then 90% of our included studies were from higher income countries, predominantly from the USA, UK and Australia. This limits the generalisability of our findings to low and middle income countries, where housing conditions, family characteristics, living arrangements and cultural practices may be very different from those in the higher income countries.
It is likely that some outcome reporting bias has occurred in the studies included in our review. Almost half of the studies included in our review were not included in any of the meta‐analyses. They were excluded for a variety of reasons, most commonly because the reported outcomes were dissimilar from those reported in other studies. Studies were also excluded from the meta‐analyses where they failed to report numerators and denominators for outcomes in both treatment arms and we were unable to obtain these from contact with authors. Six of those not reporting numerators and denominators for outcomes in both treatment arms were conference abstracts without subsequent publication of the data (Blake 1993; Chan 2004; Gaffney 1996a; Garcia 1996; Mackay 2002; Moller 1996) and 12 were undertaken more than 10 years ago, so the likelihood of obtaining IPD or unpublished analyses from these studies was small. In general, the effects reported by studies not included in our meta‐analyses appeared to be consistent with the findings from the meta‐analyses. Our use of IPD has minimised outcome reporting bias in other ways because we were able to report outcomes (for example specific safety practices or use of items of safety equipment) and include data in meta‐analyses from studies that had previously only published composite outcome measures such as safety scores or hazard scores.
Despite the large number of studies included in our review, relatively few reported specific injury outcomes (for example thermal injuries and poisonings) and even fewer reported numerators and denominators for injury outcomes could be used in our meta‐analyses. Bearing in mind the low incidence of such injuries, it is likely that our analyses were underpowered to detect anything but very (and possibly implausibly) large treatment effects.
There was some evidence that home safety interventions may be effective in reducing rates of all injuries combined, especially when follow‐up injury rates from CBA studies were adjusted for baseline injury rates. Interventions provided at home as opposed to in clinical settings or in the community significantly reduced the risk of injury when analyses were adjusted for baseline injury rates and had a similar but non‐significant effect when analyses were not adjusted for baseline injury rates. Interventions which did not provide home safety equipment significantly reduced the risk of injury regardless of adjustment for baseline injury rates, whilst those that provided equipment did not. This finding is probably explained by two large studies, one school‐based study which did not provide equipment and which demonstrated a significant reduction in injury rates (Zhao 2005) and a second clinic‐based study which provided equipment and did not find a reduction in injury rates (Watson 2005). Sensitivity analyses indicated that exclusion of this latter study resulted in home safety interventions being associated with a significant reduction in injury risk, regardless of adjustment for baseline injury rates.
Most studies reported relatively short‐term outcomes (less than one year), few studies reported repeated measures of outcomes over time or long‐term outcomes. Overall, it appeared that effect sizes may diminish over time, hence we cannot assume that our findings would be maintained over longer time periods. Few studies for the less commonly reported outcomes also reported child age, gender or social variables. This will have limited the power of our meta‐regression analyses to detect differential treatment effects for some demographic and social variables for some outcomes.
Our findings in relation to a safe hot tap water temperature must be considered in the context of current recommendations about the temperature that can be considered to be 'safe'. Few studies used 46 ºC as the definition of 'safe' hot water, but this is the temperature currently recommended by the Child Accident Prevention Trust (CAPT 2004). It is therefore possible that home safety interventions, although effective in reducing hot tap water temperatures, may not be effective in reducing temperatures sufficiently to reduce the incidence of scalding.
The size of the review and the number of outcomes for which we have undertaken meta‐analyses inevitably resulted in estimating many 95% confidence (and credible) intervals. It is therefore possible that a small number of the 'significant' effects may have arisen by chance, and our findings must be interpreted with this in mind. However, this cannot explain the consistency of our findings relating to the positive effect of home safety interventions on many safety practices or the lack of significant differences in treatment effect for most outcomes for child age, gender and social group.
Quality of the evidence
Unlike many meta‐analyses, we included non‐randomised and controlled before and after (CBA) studies. Although these comprised only one quarter of the studies included in the meta‐analyses, their inclusion increased the power of our analyses. For the majority of outcomes findings were robust to study design, with similar effect sizes found amongst RCTs and other designs (non‐RCTs and CBAs). For three outcomes effect sizes appeared to be larger in RCTs than other designs (having the poison control number accessible, having window locks and having socket covers), and for one study the effect size appeared to be smaller in RCTs (having syrup of ipecac). In addition, study design did not appear to be important in explaining heterogeneity in effect sizes for most analyses.
The quality of the included studies was mixed and varied by study design. Of the RCTs only one third had adequate randomisation, allocation concealment or blinded outcome assessment, and half had follow‐up on at least 80% of participants in each treatment arm. None of the non‐RCTs had blinded outcome assessment, just over half had follow‐up on at least 80% of participants in each treatment arm, and only one third were considered to be balanced in terms of confounders. None of the CBA studies had blinded outcome assessment, three fifths had follow‐up on at least 80% of participants in each treatment arm, and one quarter were considered to be balanced in terms of confounders. There was some evidence that effect sizes varied with study quality. Effect sizes appeared to be smaller for eight outcomes amongst studies with blinded outcome assessment (having functional smoke alarms, stair gates, window locks, socket covers and the poison control number accessible; not having a baby walker; storing sharp objects out of reach and injuries). For five studies effect sizes appeared larger amongst studies with follow‐up on at least 80% of participants in each arm (having the poison control centre number accessible and socket covers, storing poisons out of reach, keeping small objects and sharp objects out of reach). Effect sizes were larger for two outcomes in studies with adequate allocation concealment (storing poisons out of reach and keeping sharp objects out of reach) and smaller for two outcomes in studies without adequate allocation concealment (storing cleaning products out of reach and having the poison control centre number accessible). Significant heterogeneity remained in many of these subgroup analyses. Care should be taken in interpreting these findings due to small numbers of studies in many subgroup analyses and multiple significance testing. The majority of analyses were robust to excluding each study in turn, indicating that findings were not dependent on single highly influential studies.
Significant heterogeneity was found amongst effect sizes for many of our meta‐analyses. The most common potential explanations for this were the setting in which the intervention was delivered, the provision of safety equipment, and blinding of outcome assessment. Greater effect sizes tended to be found amongst interventions delivered at home or in the community as opposed to in clinical settings (with the exception of interventions to reduce baby walker use). In terms of safety equipment provision, greater effect sizes tended to be found when safety equipment was provided (with the exception of studies reporting injuries as an outcome). Studies with blinded assessment for some outcomes tended to have smaller effect sizes than those with non‐blinded outcome assessment. Other factors less commonly explaining heterogeneity included follow‐up period, study design and other aspects of study quality. However, significant heterogeneity of effect sizes often remained within subgroup analyses, suggesting other factors may also be important potential explanations for differences in effect sizes between studies. We also found a wide variation in study populations in terms of child age, ethnic group, family type, housing tenure and parental unemployment. Our meta‐regression analyses suggest that differential effectiveness of interventions by child gender, age or social variables may explain some of the heterogeneity in effect sizes for ipecac possession, safe storage of poisons, use of stair gates and window locks, and safe storage of small and sharp objects. The problems of multiple significance testing and inadequate power in subgroup analyses must be borne in mind when interpreting these subgroup analyses.
Potential biases in the review process
We undertook comprehensive searches of both the published and unpublished literature to identify studies, but it is possible that our searches may have failed to identify some potentially eligible studies. We found evidence of a possible publication bias for one outcome only, that of possession of a functional smoke alarm. However, when adjusted for possible bias, the effect size was diminished but still statistically significant. Our use of pairs of independent researchers to select studies for inclusion, extract data and assess study quality should have minimised the potential for bias in the review process.
Agreements and disagreements with other studies or reviews
Our findings build on those of the two reviews by DiGuiseppi and colleagues (DiGuiseppi 2000; DiGuiseppi 2001) and are more positive than either of these reviews, both in terms of the effect of home safety interventions on safety practices and on injuries. The first review and meta‐analysis (DiGuiseppi 2000) found that interventions in a clinical setting were effective in promoting a safe hot tap water temperature, in increasing smoke alarm ownership and in increasing safe storage of cleaning products. Only two studies reported injury outcomes and neither found a significant reduction in injury occurrence. The review concluded that clinical counselling had little effect on most home safety practices designed to child proof the home and that the evidence about the impact of counselling on childhood injuries was limited. The second review (DiGuiseppi 2001) found interventions were effective in increasing functional smoke alarm ownership only in clinical settings and with a smaller effect size than that found in our review. Our findings are likely to be more positive as we have examined a wider range of outcomes, included a larger number of studies and obtained and used IPD, which allowed for analysis of previously unpublished data. In addition, some RCTs (King 2001; Watson 2005; Zhao 2005) and CBAs (Bentzen 1997; Yorkston 2007) had large sample sizes and some studies demonstrated very positive effects for some outcomes (Johnston 2000; Hendrickson 2002; Posner 2004; Sznajder 2003), including for injury rates (King 2001; Phelan 2010; Zhao 2005). Our meta‐analyses also suggest there is some evidence to support the finding of a reduction in injury rates in these studies, particularly for home‐based interventions; although further studies are needed to clarify the role of safety equipment provision.
In terms of examining the effect of home safety interventions by child age, gender and social group, there is little work with which to compare our findings. Our findings appear to confirm subgroup analyses from individual studies that interventions are not less effective in higher risk groups. Several studies have reported some subgroup analyses examining whether the treatment effect varied by a range of factors, with most finding no evidence of differential effectiveness by child or family factors (Kendrick 2005; Mock 2003; Vineis 1994; Watson 2005). Clamp 1998 reported that the effect of general practitioner safety advice plus access to low cost safety equipment appeared to be at least as, if not more, effective in families receiving means tested benefits than in those not receiving benefits. However, this was based on comparing effect sizes amongst families receiving and not receiving benefits and not on testing for an interaction between treatment arm and receipt of benefits. Sznajder 2003 assessed whether the effect of home delivery of an injury prevention kit varied by family type, educational level and family size. They found that the intervention appeared to be more effective amongst single parent families and those with low levels of education, but less effective amongst families with two or more children. This appeared to be based on comparisons of effect sizes between subgroups of families as opposed to tests of the hypothesis that there was no interaction between treatment arm and the subgroup variables. Olds 1994 examined the effect of a home visiting programme on hazardous exposures within the home amongst a subgroup of low‐income unmarried teenage mothers. They found a significant effect of the intervention in reducing hazardous exposures in the whole sample at both 34 and 46 months follow‐up and a significant effect amongst low‐income unmarried teenage mothers at 46 months only.
Authors' conclusions
Implications for practice.
Our evidence that home safety education and the provision of safety equipment is effective in increasing a range of safety practices, and possibly also in reducing child injury rates, suggests that child health and social care providers should provide home safety interventions including education and access to free, low cost or discounted safety equipment as part of their child health and well‐being programmes. It is important that practitioners provide interventions that are as similar as possible to those we included in our meta‐analyses otherwise they may not achieve similar effects. For example, most of the studies included in our meta‐analyses were based on one‐to‐one, face‐to‐face education delivered either at home or in a clinical setting, so our findings cannot necessarily be extrapolated to different methods of delivery in different settings.
Home safety education and modifying the home environment by the provision of safety equipment can only ever be one part of a strategy to reduce home injuries in children. Other engineering approaches are also important components of such a strategy, for example the design of products or components of the structure of the house to increase safety, especially as these often provide passive protection (Pless 1993; Towner 2001). Strategies also need to encompass enforcement approaches such as the use of standards, regulations and legislation as these have also been found to be effective in reducing child injury rates (Erdmann 1991; Sibert 1977).
Implications for research.
Our findings suggest that home safety education, especially with the provision of safety equipment, is effective in increasing a range of safety practices and it may also reduce injury rates. Further evidence is needed in relation to this latter outcome, in particular to the role of the provision of safety equipment and the effects of home‐based interventions as opposed to those delivered in other settings. There are two possible options for addressing the question of whether home safety interventions are effective in reducing child injury rates. The first, and most preferable, is that further large trials or multiple smaller trials that are sufficiently clinically homogenous to combine in future meta‐analyses are undertaken measuring injury outcomes. The second, but less preferable option, is that a series of methodologically rigorous observational studies that measure and adjust appropriately for a wide range of potential confounding factors are undertaken. The first option would provide the strongest evidence but at a much greater cost over a longer time period. The second would provide evidence at a lesser cost over a shorter time period, but the quality of the evidence could be limited, especially by selection bias, recall bias and confounding.
Multi‐faceted home visiting programmes aimed at improving a range of maternal and child health outcomes have been found to be effective in reducing child injury rates (Elkan 2000; Roberts 1996b). Most of these programmes did not provide home safety interventions similar to that provided in the studies included in our review. It would therefore be useful to assess whether adding a home safety education and equipment component to a multi‐faceted home visiting programme further reduces child injury rates.
The importance of ensuring that interventions do not widen existing inequalities in child injuries suggests that future studies should consider this possibility in their design, analysis and in the reporting of their findings. As we were unable to demonstrate differential effects for many outcomes for most demographic and social variables, some of which may have been due to a lack of power, these relationships can be re‐examined if future studies measure and report these variables. Standardisation of methods of measuring social variables would be helpful as this would maximise the number of studies whose data could be included in such meta‐analyses.
In relation to outcome measurement, one recent RCT (Phelan 2010) demonstrating a significant reduction in injury rates, defined injury outcomes in terms of whether they were potentially preventable by safety equipment provided as part of the intervention, and future studies should consider using such outcomes. The studies included in our review used a wide range of tools, some of which were validated, to measure a wide range of safety practices. Use of existing validated tools in future studies would maximise the potential for future meta‐analyses. Furthermore, we found that standardising IPD datasets across studies required a large amount of time, and the use of standard measures would make this task considerably easier and less time consuming. As the power of meta‐regression analysis is considerably greater in analyses containing IPD than in those using only summary data for participant level covariates (Lambert 2002), it is also important that the community of injury researchers is willing to share their IPD for such future research.
The model we developed for examining the effect of interventions by demographic and social variables was restricted to binary and continuous outcome measures, which comprised most of the outcomes included in our review. Whilst our model is not immediately generalisable to rate outcomes, future work may develop such models which may be useful in fields other than injury prevention.
What's new
| Date | Event | Description |
|---|---|---|
| 31 October 2014 | Amended | The authors have made corrections to the results section paragraph 'storage of poisons out of reach' which relates to Analysis 5.5. |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 1, 2007
| Date | Event | Description |
|---|---|---|
| 19 March 2012 | New citation required and conclusions have changed | The review has been updated with the inclusion of 18 new studies. The authors of the review have changed. |
| 25 November 2011 | New search has been performed | The review has been updated with the inclusion of 18 new studies. |
Notes
This work was undertaken by The University of Nottingham, which received funding from the Department of Health and the National Institute for Health Research. This review presents independent research commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP‐PG‐0407‐10231). The views expressed in this review are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Acknowledgements
We would like to thank Jayne Simpson for selecting studies for inclusion, extracting data and contributing to drafting the report for the original review.
We would like to thank the following authors for providing the IPD (*) and unpublished data (§) which were used in the analyses presented in this report:
M Bulzachelli *§, P Dawson §, C DiGuiesppi *§, K Georgieff §, A Gielen *§, D Girasek §, S Hendrickson *§, D Kendrick *§ (plus provided IPD on behalf of M Clamp), D Kolko *§, R McClure § (on behalf of E Yorkston), E McDonald *, T Nansel *§, T Ohn §, E Petridou *§, K Phelen*§, J Posner *§, I Roberts *§ (on behalf of D Rowland), D Schwebel *§, L Swart *§, M Sznajder *, N Tan *§, E Wald § (on behalf of S Sangvai), M Watson*§, B Ytterstad §
Appendices
Appendix 1. Search strategy
MEDLINE (Ovid) 1950 to May Week 1 2009 1.randomized controlled trial.pt. 2.exp Randomized Controlled Trial/ 3.randomi?ed controlled trial*.mp. 4.exp Random Allocation/ 5.exp Double‐Blind Method/ 6.exp Single‐Blind Method/ 7.exp Clinical Trial/ 8.controlled clinical trial.pt. 9.comparative stud*.mp. 10.intervention stud*.mp. 11.control group*.mp. 12.placebo*.mp. 13.evaluation stud*.mp. 14.placebo*.mp. 15.exp Placebos/ 16.exp control groups/ 17.random allocation.mp. 18.or/1‐17 19.Humans/ 20.18 and 19 21.exp Child/ 22.exp Infant/ 23.exp Adolescent/ 24.exp Minors/ 25.(child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies).mp. 26.or/21‐25 27.exp "Early Intervention (Education)"/ 28.exp Education/ 29.exp Patient Education as Topic/ 30.exp Health Education/ 31.public health/ed 32.exp Parenting/ 33.exp Counseling/ 34.training.mp. 35.(educat* or train* or teach* or parent* or counsel*).mp. 36.or/27‐35 37.exp Accident Prevention/ 38.exp Safety/ 39.exp Safety Management/ 40.safety practice*.mp. 41.exp Drug Storage/ 42.exp Hazardous Substances/po, ae [Poisoning, Adverse Effects] 43.or/37‐42 44.exp Equipment Safety/ 45.(safety adj3 equipment).mp. 46.exp Infant Equipment/ 47.exp Protective Devices/ 48.(fireguard* or fire‐guard*).mp. 49.(stair* adj3 gate*).mp. 50.(bab* adj3 walk*).mp. 51.(protect* adj3 device*).mp. 52.(kettle* adj3 (flex* or cable* or wire*)).mp. 53.(cook* adj3 guard*).mp. 54.(smok* adj3 (alarm* or detect*)).mp. 55.or/44‐54 56.exp Accidents/ 57.exp Accidents, Home/ 58.exp Burns, Chemical/ 59.exp Eye Burns/ 60.exp Burns/ 61.exp Burns, Inhalation/ 62.exp Burns, Electric/ 63.exp Smoke/ 64.exp Smoke Inhalation Injury/ 65.exp Poisoning/ 66.exp Carbon Monoxide Poisoning/ 67.exp "Wounds and Injuries"/ 68.(accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur*).mp. 69.exp Fractures, Bone/ 70.exp Asphyxia/ 71.suffocat*.mp. 72.exp Ipecac/ 73.exp Drowning/ 74.exp Near Drowning/ 75.or/56‐74 76.20 and 26 77.36 or 43 or 55 78.75 and 76 and 77 79.(2004* or 2005* or 2006* or 2007* or 2008* or 2009*).ed. 80.78 and 79
EMBASE (Ovid) (1980 to May 2009, Week 18) 1.exp Randomized Controlled Trial/ 2.randomi?ed controlled trial*.mp. 3.exp Random Allocation/ 4.exp Double‐Blind Method/ 5.exp Single‐Blind Method/ 6.exp Clinical Trial/ 7.comparative stud*.mp. 8.intervention stud*.mp. 9.control group*.mp. 10.placebo*.mp. 11.evaluation stud*.mp. 12.placebo*.mp. 13.exp Placebos/ 14.exp control groups/ 15.random allocation.mp. 16.or/1‐15 17.Humans/ 18.16 and 17 19.exp Child/ 20.exp Infant/ 21.exp Adolescent/ 22.exp Minors/ 23.(child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies).mp. 24.or/19‐23 25.exp Early Intervention/ 26.exp Education/ 27.exp Patient Education/ 28.exp Health Education/ 29.exp Public Health/ 30.26 and 29 31.exp Parenting/ 32.exp Counseling/ 33.training.mp. 34.(educat* or train* or teach* or parent* or counsel*).mp. 35.25 or 26 or 27 or 28 or 30 or 31 or 32 or 33 or 34 36.exp Accident Prevention/ 37.exp Safety/ 38.exp Safety Management/ 39.safety practice*.mp. 40.exp Drug Storage/ 41.exp Hazardous Substances/ 42.or/36‐41 43.exp Equipment Safety/ 44.(safety adj3 equipment).mp. 45.exp Infant Equipment/ 46.exp Protective Devices/ 47.(fireguard* or fire‐guard*).mp. 48.(stair* adj3 gate*).mp. 49.(bab* adj3 walk*).mp. 50.(protect* adj3 device*).mp. 51.(kettle* adj3 (flex* or cable* or wire*)).mp. 52.(cook* adj3 guard*).mp. 53.(smok* adj3 (alarm* or detect*)).mp. 54.or/43‐53 55.exp Accidents/ 56.exp Accidents, Home/ 57.exp Burns, Chemical/ 58.exp Eye Burns/ 59.exp Burns/ 60.exp Burns, Inhalation/ 61.exp Burns, Electric/ 62.exp Smoke/ 63.exp Smoke Inhalation Injury/ 64.exp Poisoning/ 65.exp Carbon Monoxide Poisoning/ 66.exp injury/ 67.(accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur*).mp. 68.exp Fractures, Bone/ 69.exp Asphyxia/ 70.suffocat*.mp. 71.exp Ipecac/ 72.exp Drowning/ 73.exp Near Drowning/ 74.or/55‐73 75.18 and 24 76.35 or 42 or 54 77.74 and 75 and 76 78.(2004* or 2005* or 2006* or 2007* or 2008* or 2009*).em. 79.77 and 78
PsycINFO (Ovid) 1806 to May (week 3) 2009 1.randomi?ed controlled trial*.mp. 2.exp Clinical Trial/ 3.comparative stud*.mp. 4.intervention stud*.mp. 5.control group*.mp. 6.placebo*.mp. 7.evaluation stud*.mp. 8.placebo*.mp. 9.exp control groups/ 10.random allocation.mp. 11.or/1‐10 12.(child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies).mp. 13.exp Education/ 14.exp Health Education/ 15.exp Counseling/ 16.training.mp. 17.(educat* or train* or teach* or parent* or counsel*).mp. 18.or/12‐17 19.exp Accident Prevention/ 20.exp Safety/ 21.safety practice*.mp. 22.(safety adj3 equipment).mp. 23.(fireguard* or fire‐guard*).mp. 24.(stair* adj3 gate*).mp. 25.(bab* adj3 walk*).mp. 26.(protect* adj3 device*).mp. 27.(cook* adj3 guard*).mp. 28.(smok* adj3 (alarm* or detect*)).mp. 29.or/19‐28 30.exp Accidents/ 31.exp Burns/ 32.exp Smoke/ 33.exp Poisoning/ 34.exp Carbon Monoxide Poisoning/ 35.(accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur*).mp. 36.exp Asphyxia/ 37.suffocat*.mp. 38.or/19‐36 39.11 and 18 and 29 and 38 ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) 1970 to May 2009 ISI Web of Science: Social Sciences Citation Index (SSCI) 1970 to May 2009 ISI Web of Science: Conference Proceedings Citation Index‐ Science (CPCI‐S) 1990 to May 2009 1.Topic=(child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies) 2.Topic=(accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur* or drown* or Carbon Monoxide or Smoke Inhal* or Ipecac or Drug Storage or Hazardous Substance* or Infant Equipment or Protective Device* or fireguard* or fire‐guard* or stair gate* or baby walk* or kettle flex* or kettle cable* or kettle wire* or cooker guard* or smoke alarm* or smoke detect*) Topic=(educat* or train* or teach* or parent* or counsel* or early Intervention or public health or accident prevention or prevent* or safe or safety) 3.Topic=(Home*) 4.Topic=(randomized or randomised or controlled trial* or Random Allocation or Double‐Blind or Single‐Blind or Clinical Trial* or comparative stud* or intervention stud* or control group* or placebo* or evaluation stud* or placebo*)
CINAHL (EBSCO) 1982 to May 2009 (2004 to 2009) 1.TX ( child* or adolesc* or infan* or young* or minor* or toddl* or baby or babies ) and ( accident* or burn* or scald* or asphyx* or chok* or cut* or suffocat* or poison* or fracture* or wound* or injur* or drown* or Carbon Monoxide or Smoke Inhal* or Ipecac or Drug Storage or Hazardous Substance* or Infant Equipment or Protective Device* or fireguard* or fire‐guard* or stair gate* or baby walk* or kettle flex* or kettle cable* or kettle wire* or cooker guard* or smoke alarm* or smoke detect* ) and ( educat* or train* or teach* or parent* or counsel* or “early Intervention” or “public health” or “accident prevention” or prevent* or safe or safety ) 2.TX Home* 3.4 and 5 4.randomized or randomized or controlled trial* or Random Allocation or Double‐Blind or Single‐Blind or Clinical Trial* or comparative stud* or intervention stud* or control group* or placebo* or evaluation stud* or placebo*
Data and analyses
Comparison 1. Medically attended or self reported injury rates.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Comparing medically attended or self‐reported injury rates ‐ unadjusted for baseline rates | 15 | 24406 | IRR (Random, 95% CI) | 0.93 [0.83, 1.05] |
| 2 Comparing medically attended or self‐reported injury rates ‐ adjusted for baseline rates | 15 | 24406 | IRR (Random, 95% CI) | 0.89 [0.78, 1.01] |
Comparison 2. Thermal injury rates.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Comparing thermal injury rates | 4 | 22682 | IRR (Random, 95% CI) | 0.85 [0.51, 1.42] |
Comparison 3. Poisoning injury rates.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Comparing poisoning rates | 4 | 17997 | IRR (Random, 95% CI) | 0.93 [0.65, 1.32] |
Comparison 4. Thermal injuries.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Safe hot tap water temperature | 16 | 3727 | Odds Ratio (M‐H, Random, 95% CI) | 1.41 [1.07, 1.86] |
| 2 Possession of a functional smoke alarm | 17 | 5107 | Odds Ratio (M‐H, Random, 95% CI) | 1.81 [1.30, 2.52] |
| 3 Use of fire guards | 4 | 2945 | Odds Ratio (M‐H, Random, 95% CI) | 1.40 [1.00, 1.95] |
| 4 Keeping hot drinks or food out of reach of children | 6 | 1660 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.61, 1.48] |
| 5 Storage of matches or lighters out of reach of children | 6 | 2169 | Odds Ratio (M‐H, Random, 95% CI) | 1.03 [0.63, 1.68] |
| 6 Possession of a fire extinguisher | 5 | 1803 | Odds Ratio (M‐H, Random, 95% CI) | 0.90 [0.53, 1.51] |
| 7 Has a fire escape plan | 4 | Odds Ratio (Random, 95% CI) | 2.01 [1.45, 2.77] | |
| 8 Smoke alarm batteries checked or changed | 4 | 633 | Odds Ratio (M‐H, Random, 95% CI) | 1.15 [0.63, 2.08] |
Comparison 5. Poisoning outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Storage of medicines out of reach | 13 | 4338 | Odds Ratio (M‐H, Random, 95% CI) | 1.53 [1.27, 1.84] |
| 2 Storage of cleaning products out of reach | 15 | 4847 | Odds Ratio (M‐H, Random, 95% CI) | 1.55 [1.22, 1.96] |
| 3 Possession of syrup of ipecac | 10 | 2183 | Odds Ratio (M‐H, Random, 95% CI) | 3.34 [1.50, 7.44] |
| 4 Having a poison control centre sticker available | 9 | 1839 | Odds Ratio (M‐H, Random, 95% CI) | 3.30 [1.70, 6.39] |
| 5 Storage of poisons out of reach | 5 | 1252 | Odds Ratio (M‐H, Random, 95% CI) | 2.07 [0.92, 4.66] |
| 6 Storage of plants out of reach | 3 | 608 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.40, 3.48] |
Comparison 6. Falls outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Having a fitted stair gate | 12 | 4987 | Odds Ratio (M‐H, Random, 95% CI) | 1.61 [1.19, 2.17] |
| 2 Possession and use of a baby walker | 9 | 3273 | Odds Ratio (M‐H, Random, 95% CI) | 1.57 [1.18, 2.09] |
| 3 Possession of window locks, screens or mechanisms to limit opening on at least some windows | 6 | 3724 | Odds Ratio (M‐H, Random, 95% CI) | 1.17 [0.87, 1.57] |
| 4 Possession of non‐slip bath mats or decals | 4 | 690 | Odds Ratio (M‐H, Random, 95% CI) | 1.10 [0.68, 1.79] |
| 5 Does not leave child unattended on a high surface | 3 | 661 | Odds Ratio (M‐H, Random, 95% CI) | 0.84 [0.58, 1.20] |
Comparison 7. Electrical injuries.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of socket covers | 9 | 1917 | Odds Ratio (M‐H, Random, 95% CI) | 2.69 [1.46, 4.96] |
Comparison 8. Lacerations and bruising.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Storage of sharp objects out of reach | 7 | 2983 | Odds Ratio (M‐H, Random, 95% CI) | 1.54 [0.90, 2.64] |
Comparison 9. Suffocation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Keeping small objects out of reach | 6 | 2114 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.36, 1.77] |
Comparison 10. Drowning.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Never leaving child alone in the bath | 5 | 1685 | Odds Ratio (M‐H, Random, 95% CI) | 1.21 [0.85, 1.72] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adler 1994.
| Methods | RCT | |
| Participants | Children aged 5‐16 years with a history of firesetting/fireplay | |
| Interventions | I1 = educational material, 2 home visits by fire fighters to provide education, behaviour modification, parental instruction in use of negative consequences in the event of firesetting, plotting events leading up to an incident and discussing alternative ways of responding to incidents in future I2 = same as I1 plus offer of psychiatric referral C1 = fire safety educational material C2 = fire safety educational material plus offer of psychiatric referral | |
| Outcomes | Outcomes measured over 12 months: Rate of fire setting Number of children setting fires causing or threatening to cause property damage ‐ data not reported separately for treatment arms No significant difference between experimental and control groups in rate of fire setting or seriousness of fire setting No P values reported |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Babul 2007.
| Methods | RCT | |
| Participants | Parents of new born infants at a general hospital serving mainly urban or suburban communities | |
| Interventions | I 1= Home visit + home safety inspection + free safety kit (smoke alarm, coupon for 50% discounted stair gate, corner cushions, cabinet locks, blind cord windups, water temperature card, door stoppers, socket covers, poison control centre sticker + safety brochure + home safety checklist for parents) I2 = free safety kit (as above) C = usual care |
|
| Outcomes | Outcomes measured at 12 months of age: Medically attended injuries Safe hot water temperature (temperature not specified) Possession of fire extinguisher Hot drinks/food out of reach Safe storage of medicines Plants out of reach Use of baby walker Left child alone on high surface Hall and stairways adequately lit I1=169/171, I2=161/162, C=144/146; I1 vs C OR 1.17 (0.08 to 16.37), I2 vs C OR 2.24 (0.11 to 132.72) Hall and stairways not cluttered I1=160/169, I2=152/162, C=135/144; I1 vs C OR 1.19 (0.40 to 3.47), I2 vs C OR 1.01 (0.35 to 2.87) Small objects kept out of reach Blind cords not accessible to child I1=150/171, I2=145/161, C=125/146; I1 vs C OR 1.20 (0.59 to 2.43), I2 vs C OR 1.53 (0.72 to 3.26) Never left child alone in bath Pools fully fenced I1 =112/172, I2 = 105/161, C = 104/144; I1 vs C OR 0.72 (0.43 to 1.19); I2 vs C OR 0.72 (0.43 to 1.21) |
|
| Notes | I1 and I2 arms combined for meta‐analyses Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n/a |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Barone 1988.
| Methods | RCT (C) Allocation at level of parenting classes | |
| Participants | 5 parenting classes (108 parents of toddlers) | |
| Interventions | I = slides, handouts on burn prevention, bath water thermometer, hot water gauge, usual safety education C = usual safety education | |
| Outcomes | Outcomes measured over 6 months: Possession of smoke alarm Functional smoke alarm Safe hot water temperature |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Inadequate |
Baudier 1988.
| Methods | RCT (C) Allocation at level of groups of schools | |
| Participants | Infant school children | |
| Interventions | I = teaching kit for use by teachers of infant classes, take home booklet, stickers, exhibitions, parents meetings C = none of above | |
| Outcomes | Outcomes measured during subsequent school term: Safe storage of poisons |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not used |
Bentzen 1997.
| Methods | CBA (C) Allocation at level of municipality | |
| Participants | Population of children aged 0‐15 years in 2 municipalities, Odense (intervention) and Randers (control) | |
| Interventions | I = community injury prevention programme including advice in well child clinics and group based health programmes, pamphlets, puppet theatre, posters, exhibitions C = no community injury prevention programme | |
| Outcomes | Outcomes measured over 4 years: Medically attended injuries (ED attendances) Incidence of cut injuries ‐ I = 468/10000 boys; 343/10000 girls at baseline and 361/10000 boys; 280/10000 girls at follow‐up C = 7.7/10000 boys; 5.8/10000 girls at baseline and 54.9/10000 boys; 40.9/10000 girls at follow‐up No P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Blake 1993.
| Methods | Non‐RCT/CBA | |
| Participants | Parents in two inner city health clinics | |
| Interventions | I = educational video C = no video | |
| Outcomes | Period over which outcomes measured not reported. Functional smoke alarm. Significant increase in purchase and installation of smoke alarms in intervention group No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ u Allocation of participants not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Bulzachelli 2009.
| Methods | Non‐RCT Randomised to I1 or I2 arms on days when mobile child safety centre present (Monday, Wednesday, Friday) and allocated to control arm when mobile child safety centre not present (Tuesday, Thursday) |
|
| Participants | Parents of children aged 1 month to seven years attending a well‐child clinic in low‐income urban communities | |
| Interventions | I1= prescribed visit to mobile child safety centre I2 = optional visit to mobile child safety centre C = told about purpose of mobile safety centre & given more information on request but not referred to centre |
|
| Outcomes | Outcomes measured at 2 to 4 weeks: Functional smoke alarm Safe storage of poisons |
|
| Notes | I1 and I2 arms combined for meta‐analyses Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n Control arm participants had higher baseline educational and income levels than intervention arm participants. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Campbell 2001.
| Methods | RCT (C) Allocation at level of schools | |
| Participants | Hispanic migrant youths, aged 11‐16 years, low income | |
| Interventions | I = 8 sessions of multimedia first aid and home safety training presented by bilingual and bicultural college students C = 8 sessions of multimedia tobacco and alcohol prevention education presented by bilingual and bicultural college students | |
| Outcomes | Outcomes measured over 12 months: Possession of fire extinguisher (No figures or P value reported) Practiced fire escape plan Safe storage of medicines (No figures or P value reported) Safe storage of cleaning products (No figures or P value reported) Removal of small objects (No figures or P value reported) No significant difference in total number of home safety changes made (No figures or P value reported) |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Carman 2006.
| Methods | CBA (C) Allocation at level of electoral wards |
|
| Participants | Children under 5 years in deprived electoral wards | |
| Interventions | I = home visit by injury prevention project workers + safety education + free equipment (bath mat, harness and reins, cupboard locks, corner cushions, multi‐purpose lock, socket covers) + low cost fitted equipment (stair gates, fireguards, smoke alarm, kitchen cupboard locks, glass safety film) + population wide injury prevention talks to community groups and safety events across locality + follow‐up of families whose children had attended the Emergency Department C = Population wide injury prevention talks to community groups and safety events across locality + follow‐up of families whose children had attended the Emergency Department |
|
| Outcomes | Outcomes measured over 2 years: Medically attended injuries (ED attendance) |
|
| Notes | Blinding ‐ u
Outcomes 80% ‐ y
Balance ‐ no Intervention areas had higher baseline ED attendance rates than control areas |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Chan 2004.
| Methods | RCT | |
| Participants | Families in two districts of Hong Kong with children under 3 years admitted to hospital with an unintentional injury | |
| Interventions | I = 4 quarterly home visits and monthly telephone follow‐ups focusing on practical solutions to potential for injury, from lay home visitors and standard educational material on injury prevention C = standard educational material on injury prevention | |
| Outcomes | Period over which outcomes measured not reported. Tested temperature of microwaved food Child proofed boiler and rice cookers, window frames and electrical heating devices Household rearrangement to avoid staggering furniture layout Home hazards assessed on a 51 item household environment checklist Significantly more intervention group families tested temperature of microwaved food (P = 0.05) and child proofed boilers and rice cookers (P = 0.05), window frames (P < 0.01) and electrical heating devices (P = 0.05) and rearranged furniture to avoid staggering layout (P < 0.01) No figures reported for any of the above outcomes No figures or P value reported for overall hazard score |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Clamp 1998.
| Methods | RCT | |
| Participants | Families with children < 5 years registered at one GP surgery | |
| Interventions | I = general practitioner safety advice, leaflets & low cost safety equipment (smoke alarms, window locks, cupboard and drawer catches, socket covers, door slam devices, fire guards, stair gates) C = usual care | |
| Outcomes | Outcomes measured at 6 weeks: Functional smoke alarm Possession of smoke alarm Fitted fire guard Safe storage of medicines Safe storage of cleaning products Use of stair gate Use of window locks Use of socket covers Sharp objects stored out of reach Use of door slam devices I = 50/82 C = 14/82 OR 7.59 (3.67 to 15.69) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Coggan 2000.
| Methods | CBA (C) Allocation at level of communities | |
| Participants | Population of two communities, Waitakere (intervention) and a control community matched on demographic variables, new housing developments, road safety and safer community coordinator positions | |
| Interventions | I = community based injury prevention programme focusing on child safety including multi‐agency collaboration, education & training, advocacy and action for hazard reduction C = no community based injury prevention program | |
| Outcomes | Outcomes measured over 2 years: Injury outcomes ascertained from injury surveillance system. Hospital admission rates for injury ‐ Significant reduction in injury hospitalisation rates during intervention and post intervention phase in intervention as compared to control community P < 0.05. Figures not reported. Fitted fire guard ‐ Intervention community significantly more likely to have a fitted fire guard P = 0.0002. No figures reported. Acquisition of stair gate ‐ Intervention group significantly more likely to acquire a stair gate P < 0.0001. No figures reported. Acquisition of appropriate fencing for swimming pools ‐ Intervention group more likely to acquire pool fencing, P = 0.0001. No figures reported. |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Intervention community had higher child injury rates at baseline than control community | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Colver 1982.
| Methods | RCT (C) Allocation at level of clinics, day nurseries and nursery classes | |
| Participants | Families with children < 5 years attending child health clinics, day nurseries, nursery classes and a toddler group in deprived area | |
| Interventions | I = encouraged to watch TV safety campaign + home visit + advice on benefits to obtain safety equipment and local availability of safety equipment C = encouraged to watch TV safety campaign | |
| Outcomes | Outcomes measured at 3 months: Safety changes made to home including cooker guards, fire guards and keeping matches out of reach ‐ Intervention group were more likely to report making safety changes to the home I = 22/37 C = 4/43, OR 14.30 (4.22 to 48.46) A physical hazard score comprising nine hazards in the home ‐ No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Davis 1987.
| Methods | RCT (C) Allocation at level of school class | |
| Participants | 41 grade 4‐6 classes | |
| Interventions | I = six 1 hour fire safety lessons with workbook, demonstrations, teacher training, materials and take home materials for parents C = usual lessons | |
| Outcomes | Outcomes measured immediately after last fire safety lesson: Possession of smoke alarm |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Dawson 1989.
| Methods | RCT | |
| Participants | Women aged 16 years and under attending maternity clinic, 20‐26 weeks pregnant, English speaking | |
| Interventions | I1 = home visits to provide emotional support, advice on child care including safety advice, practical help e.g. with housing, finding legal advice, transport to clinics; encouragement and transportation to use community resources
I2 = I1 plus 2 weekly parent groups
C1 = usual care C2 = usual care (selected post randomised enrolment) |
|
| Outcomes | Outcomes measured at 12 months: Poison centre phone number accessible ‐ I1+ I2 = 37/54 C1+ C2 = 20/33 OR 1.41 (0.57 to 3.49) Possession of ipecac I1+ I2 = 28/54 C1+ C2 = 17/33 OR 1.01 (0.43 to 2.41) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Dershewitz 1977.
| Methods | RCT | |
| Participants | Mothers of children attending a medical clinic enrolled in pre paid medical plan | |
| Interventions | I = safety advice + safety booklet + free safety equipment provided by researcher C = free safety equipment provided by researcher | |
| Outcomes | Outcomes measured at 2 months: Safe storage of prescription medicines Safe storage of cleaning products Use of socket covers Sharp objects (knives) stored out of reach Small objects (coins) out of reach Safe storage of non‐prescription medicines I = 1/101 C = 3/104 OR 0.34 (0.03 to 3.29) Use of cupboard locks (not specified for cupboards containing poisonous substances) I = 34/101 C = 32/104 OR 1.14 (0.64 to 2.05) Removal of pins and needles I = 33/101 C = 31/104 OR 1.14 (0.63 to 2.06) Household hazard scale comprising eleven potential hazards ‐ Total hazard score I = 53.2, C = 52.99, P = NS, P value not given |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
DiGuiseppi 2002.
| Methods | RCT (C) Allocation at level of electoral wards | |
| Participants | Households in council rented accommodation | |
| Interventions | I = free smoke alarm, and offer of free fitting, reminder to change batteries C = no smoke alarm | |
| Outcomes | Outcomes measured at 18 months: Fire related injuries: Rate ratio (RR) 1.3 (0.9,1.8), adjusted for baseline rates RR 1.3 (0.9,1.9) Hospitalisations and deaths: RR 1.3 (0.7,2.4), adjusted for baseline rates RR 1.3 (0.7,2.3) Preventable injuries*: RR 1.1 (0.8,1.7), adjusted for baseline rates RR 1.2 (0.8,1.8) Preventable hospitalisations and deaths: RR 1.0 (0.5,1.9), adjusted for baseline rates RR 1.0 (0.5,2.0) Attended fires: RR 1.0 (0.9,1.2), adjusted for baseline rates RR 1.1 (0.96,1.3) *Preventable = independently judged by 2 researchers blinded to treatment arm to be potentially preventable had a working smoke alarm been present. Functional smoke alarms |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y(i) n(sp) Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Emond 2002.
| Methods | CBA (C) Allocation at level of health visitor base | |
| Participants | First time mothers from socio‐economically deprived areas | |
| Interventions | I = first parent health visitor scheme (a programme of regular home visits to help, support and advise mothers) C = conventional health visiting | |
| Outcomes | Outcomes measured at 2 years: Use of stair gate ‐ intervention group significantly more likely to use stair gates. No figures or p values reported Use of socket covers ‐ Intervention group more likely to use socket covers. No figures or p values reported |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ u Balance ‐ n Intervention area chosen because of deprivation level. At baseline the intervention arm had higher proportion of black and Asian mothers, lower maternal educational level and less advantaged in terms of housing status than control arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Fergusson 1982.
| Methods | Non‐randomised controlled trial (C) Allocation at level of 2 month time periods and within time periods sequentially by date of birth | |
| Participants | Families of children aged 2‐3 years participating in the Christchurch Child Development Study | |
| Interventions | I = "Mr Yuk" stickers for poisonous substances + list of substances to which sticker should be attached + educational leaflet provided by researcher C = none of the above | |
| Outcomes | Outcomes measured at 12 months: Medically attended poisonings Mean number of poisons within child's reach I = 14.80, C = 17.70, P > 0.05 Poisoning hazards score I = 79.96, C = 78.29, P > 0.05. |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Franklin 2002.
| Methods | CBA | |
| Participants | Children and young people, aged 4‐17 years, referred from the county court system, fire departments, schools and parents with fire setting incident | |
| Interventions | I = trauma burn outreach prevention program (TBOPP) ‐ a 1 day multidisciplinary program with interactive content focusing on the impact of fire setting behaviour including a peer counselling approach C = No TBOPP | |
| Outcomes | Outcomes measured between 8 months and 2.5 years: Firesetting behaviour Recidivism rate ‐ I = 1/132 C = 37/102, OR 0.01 (0.002 to 0.1) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ n Control arm were children who were not referred to the prevention programme Control arm were marginally younger and less likely to have a history of arson | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Gaffney 1996a.
| Methods | CBA (C) Allocation level not reported | |
| Participants | Populations of unspecified control and intervention areas | |
| Interventions | I = multi‐faceted campaign to reduce risk factors and the rate of hot water scalds in children aged 0‐4 years C = no campaign | |
| Outcomes | Outcomes measured at 3 months and 2.5 years: Awareness and use of scald limiting products ‐ no changes in awareness or use of scald limiting products. No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Garcia 1996.
| Methods | CBA (C) Allocation at level of schools | |
| Participants | 4th grade elementary school children and their parents | |
| Interventions | I = safety fair at schools which included interactive safety stations on poisons, fires and home injuries. C = no safety fairs | |
| Outcomes | Period over which outcomes measured not reported: Fire safety behaviours ‐ intervention school parents showed significant improvement in safety behaviour. No figures or P values reported Poison safety ‐ Intervention school students showed a significant improvement in poison safety. No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Georgieff 2004.
| Methods | CBA (C) Allocated at level of electoral ward. | |
| Participants | Children < 3 years from 5 deprived wards | |
| Interventions | I1= awareness raising campaign including leaflets, a logo, a radio advert campaign, a bus advertising campaign, burns and scalds road shows, free bath water thermometers and hot tap water temperature testing by researchers I2 = I1 + free thermostatic mixer valve for baths C = none of the above | |
| Outcomes | Period over which outcomes measured not reported: Safe hot tap water temperature < 49 degrees Celsius Mean temperature after intervention (degrees Celsius) I (1) = 52, I (2) = 55, C = 58 No p values reported |
|
| Notes | I2 and C arms used for meta‐analyses Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n Intervention group had higher percentage of single parents |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Gielen 2002.
| Methods | RCT (C) Allocation at level of paediatricians | |
| Participants | 1st and 2nd year paediatric residents and their patient‐parent dyads Low income population of parents of children aged 0‐6 months | |
| Interventions | I = safety counselling by paediatricians + referral to child safety centre + home visit C = safety counselling by paediatricians + referral to child safety centre | |
| Outcomes | Outcomes measured over 12 months: Safe hot water temperature Functional smoke alarm Possession of ipecac Safe storage of poisons No toxic plants in the home Use of stair gate Safety score comprising the number of observed safety practices within the home ‐ zero safety practices I = 4/45 C = 2/40 OR 1.85 (0.32 to 10.71), 1 safety practice I = 22/46 C = 22/43 OR 0.88 (0.38 to 2.01), 2 safety practices I = 14/46 C = 13/43 OR 1.01 (0.41 to 2.49), ≥3 safety practices I = 6/46 C = 6/43 OR 0.93 (0.27 to 3.12) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Gielen 2007.
| Methods | RCT | |
| Participants | Parents of children aged 4‐66 months attending an urban paediatric ED | |
| Interventions | I = personalised report containing tailored, stage‐based messages based on the precaution adoption process model C = report on other child health topics |
|
| Outcomes | Outcomes measured at 2‐4 weeks: Possession of smoke alarm Functional smoke alarm Safe storage of medicines Safe storage of cleaning products Safe storage of poisons |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Girasek 2010.
| Methods | RCT (C) Allocated at level of pre‐natal class |
|
| Participants | Pregnant pool owners | |
| Interventions | I1 = viewing a video tape describing toddler drowning risks and recommended pool precautions I2 = viewing a videotape as above but including a mother describing how she lost her son to drowning C = standard care ‐ no videotape | |
| Outcomes | Installation of isolation pool fencing I1 + I2 = 10/62 C=2/30 OR 2.69 (0.61 to 11.85) Had first aid training I1 + I2 = 33/69 C=9/32 OR 2.33 (1.01 to 5.56) |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Gittelman 2007.
| Methods | CBA (C) Allocation at level of communities |
|
| Participants | Children aged 0‐18 years in an intervention community and in 3 control communities | |
| Interventions | I = Injury Free Coalition for Kids community injury prevention programme including after‐school programmes, summer educational classes for children, education at school and community fairs, free home safety kits (contents not specified). C = no community injury prevention programme |
|
| Outcomes | Outcomes measured over 5 years: Medically attended injuries (deaths, hospital admissions and ED attendances) |
|
| Notes | Blinding ‐ n
Outcomes 80% ‐ y
Balance ‐ n Intervention communities had higher baseline injury rates than control communities |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Guyer 1989.
| Methods | CBA (C) Allocation at level of cities and towns | |
| Participants | Population of 14 cities and towns in Massachusetts | |
| Interventions | I = Community injury prevention programme including injury counselling by paediatricians to parents of young children, school and community burn prevention education, home safety inspections + community wide promotion of poison centre service C = no community injury prevention programme | |
| Outcomes | Outcomes measured over 22 months: Rate of medically attended poisonings ‐ poisoning rate I = 36.14/10,000 person years C = 92.71/10,000 person years, OR 0.95 (0.57 to 1.58) (adjusted for socio‐economic group) Rate of medically attended fall injuries ‐ I = 175.02/10,000 person years C = 262.44/10,000 person years OR 0.78 (0.61 to 1.00) (adjusted for socio‐economic group) Medically attended thermal injuries ‐ I = 59.68/10000 person years C = 106.03/10000 person years OR 1.26 (0.84 to 1.90) (adjusted for socio‐economic group) Possession of smoke alarm Preventive behaviour score comprising behaviours for preventing poisonings (14 items), burns (12 items), falls (6 items) ‐ Mean score: Burns: I = 49.2, C = 46.8 Falls I = 30.3, C = 30.7 Poisoning I =34.3, C = 30.5. P values not reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Control communities had higher baseline injury rates, a greater proportion of Hispanic residents and lower household income than intervention communities | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Harvey 2004.
| Methods | RCT (C) | |
| Participants | Households without smoke alarms in areas with a high prevalence of residential fire deaths, a low prevalence of functional smoke alarms, a composition of primarily low‐income residents, and/or high proportion of rented housing | |
| Interventions | I1 = smoke alarm installation I2 = vouchers for free smoke alarm |
|
| Outcomes | Outcomes measured at 6 to 12 months: Functional smoke alarm. I1=1421/1583, I2=997/1545; OR 4.82 (3.96 to 5.88) Analyses not adjusted for clustering |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Hendrickson 2002.
| Methods | RCT | |
| Participants | Mothers with children aged 1‐4 years, predominantly Mexican/Mexican American | |
| Interventions | I = safety counselling from researchers, plus identification of home hazards + safety education + provision of safety equipment (door knob covers, smoke detectors or new batteries if smoke alarm already in situ, fire extinguisher, cabinet latches and outlet covers) C = none of the above | |
| Outcomes | Outcomes measured at 6 weeks: Functional smoke alarm Possession of a fire extinguisher Matches stored out of reach Hot drinks out of reach Safe storage of cleaning products Poison control centre number accessible Use of window locks Use of socket covers Small objects kept out of reach Floors not in need of repair I = 31/38, C = 28/40, OR 1.90 (0.66 to 5.50) Stairs not in need of repair I = 5/38, C = 1/40, OR 5.91 (0.66 to 53.15) Hand rail on stairs I = 5/38, C = 2/40, OR 2.88 (0.52 to 15.84) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Inadequate |
Hwang 2006.
| Methods | CBA | |
| Participants | 3rd and 4th grade students in 2 elementary schools in an urban, poor community | |
| Interventions | I = visit during school hours from fire department personnel who installed a free 10 year lithium smoke alarm on each level of the residence. Provided a fire escape plan verbally and on a dry erase board placed on the refrigerator. C = usual care |
|
| Outcomes | Outcomes measured at 4 weeks: Has a fire escape plan Has identified a meeting place outside the home in case of fire. OR 1.9 (1.0 to 3.8) Possession of smoke alarm. No significant difference between groups. Lighting of matches or lighters. No significant difference between groups. Child cooking on stove. No significant difference between groups. Possession of fire extinguisher. No significant difference between groups. Figures and p values not reported for the latter four outcomes. |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ u Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Jenkins 1996.
| Methods | RCT | |
| Participants | Families with children aged 0‐17 years admitted to a pediatric burns unit | |
| Interventions | I = education about burn care and prevention using specially designed booklet pre discharge from nurses, physiotherapists or occupational therapists C = routine discharge teaching without booklet | |
| Outcomes | Outcomes measured at first out‐patient appointment post‐discharge: Possession of smoke alarm |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Johnston 2000.
| Methods | RCT (C) Allocation at level of pre school enrichment programme centres | |
| Participants | Families of children aged 4‐5 years enrolled in Head Start program provided to socio‐economically disadvantaged children | |
| Interventions | I = home safety inspections + educational material + provision of ipecac, smoke alarms and batteries provided by educational paraprofessionals C = home safety inspection + written information only | |
| Outcomes | Outcomes measured at 3 months: Functional smoke alarm Possession of ipecac Removed poisons from home I = 61/202 C = 20/135 OR 2.48 (1.42 to 4.36) Disposed of unused medicine I = 18/202 C = 16/134 OR 0.72 (0.35 to 1.47) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Inadequate |
Katcher 1989.
| Methods | RCT (C) Allocated at level of half day of clinic visit | |
| Participants | Consecutive paediatric clinic clients randomised to two groups | |
| Interventions | I = counselling by paediatrician plus tap water thermometer and tap water safety literature C = counselling and tap water safety literature | |
| Outcomes | Outcomes measured at 1 month: Safe hot water temperature < 54.4 degrees Celsius Tested hot water temperature I = 122/263, C = 55/239, OR 2.89 (1.97 to 4.26) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Kelly 1987.
| Methods | RCT | |
| Participants | Parents of 6 month old children attending primary care centre for well child care | |
| Interventions | I = 3 part safety course at well child care visits C = routine safety education | |
| Outcomes | Outcomes measured at 2 weeks; Medically attended injuries (ED attendance, physician attendance or admission to hospital) Safe hot water temperature < 52 degrees Celsius Possession of smoke alarm Matches stored out of reach Safe storage of medicines Safe storage of cleaning products Possession of ipecac Uncovered electrical outlets Sharp objects stored out of reach No sharp corners on furniture I = 46/55 C = 42/54 OR 1.46 (0.56 to 3.81) A hazard score comprising 9 possible hazards observed on home visit ‐ Mean hazard score I = 2.4, C = 3.0, P<0.02 |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Kelly 2003.
| Methods | RCT (C) Allocation at level of well child care class | |
| Participants | Parents of children aged 15 months to 6 years attending Women, Infant and Children clinics | |
| Interventions | I = videotape + poison control centre pamphlet + poison control centre stickers C = usual care | |
| Outcomes | Outcomes measured at 2 weeks: Possession of ipecac Poison centre number accessible |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Kendrick 1999.
| Methods | Non‐randomised controlled trial (C) Allocated at level of GP practice. Randomised practices to intervention group and matched control group practices on deprivation score | |
| Participants | Children aged 3 to 12 months registered at 36 GP practices | |
| Interventions | I = health visitor safety advice at child health surveillance, low cost equipment (stair gates, fire guards, cupboard and drawer locks, smoke alarms), home safety checks and first aid training C = usual care | |
| Outcomes | Outcomes measured at 25 months: Medically attended thermal injuries Medically attended poisonings Medically attended injuries (primary care attendance, ED attendance, hospital admission or death) Stores hot iron out of reach I = 353/364, C = 358/366, OR 0.72 (0.28 to 1.80) Functional smoke alarm Fitted fire guard Safe hot water temperature < 54 degrees Celsius Hot drinks out of reach Stores matches out of reach Safe storage of cleaning products Use of stair gates Use of window locks Use of socket covers Sharp objects stored out of reach Never left child alone in bath Rugs fixed to floor I = 88/187, C = 64/169, OR 1.46 (0.96 to 2.23) Does not have toys small enough to fit in child's mouth I = 201/358, C = 216/365, OR 0.88 (0.66 to 1.19) Always checks toys with removable small parts I = 179/363, C = 179/365, OR 1.01 (0.76 to 1.35) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y(i) n(sp) Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Kendrick 2005.
| Methods | RCT (C) Allocation at level of general practices | |
| Participants | Women of at least 28 weeks gestation registered at participating general practices | |
| Interventions | I = midwife and health visitor advice to discourage walker use, information cards, fridge magnets, checklists for use in child health surveillance visit at 3 to 4 months. Encouraging use of stair gates and fire guards amongst walker users C = usual care | |
| Outcomes | Outcomes measured when child 9 months of age: Fitted fire guard Use of baby walker Use of stair gate |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Kendrick 2007.
| Methods | RCT (C) Allocation at level of schools |
|
| Participants | Children aged 7‐10 years in state funded primary schools | |
| Interventions | I = teachers were trained by Fire Service Personnel to deliver teaching on falls; poisoning; and fire and burns. Fire Service personnel provided free teaching resources, including Risk Watch folders and “Risky Boxes” which included background information, lesson plans and activities for pupils C = usual care |
|
| Outcomes | Outcomes measured at 4 months: Possession of smoke alarm Child never cooks without adult present I=117/163 C=141/184, 0.90 (0.45 to 1.82) Child never uses matches I=137/165 C=139/186, 1.84 (1.06 to 3.20) Child never gets medicines without asking adult. I=107/123 C=164/187, 0.69 (0.30 to 1.59) Child never plays on stairs. I=41/76 C=106/186, 0.80 (0.43 to 1.48) |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Kendrick 2010.
| Methods | RCT | |
| Participants | Households with children < 5 years in social housing in disadvantaged communities | |
| Interventions | I = Thermostatic mixer valve fitted by qualified plumber and educational leaflets prior to and at the time of fitting. C = usual care |
|
| Outcomes | Outcomes measured at 3 and 12 months: Safe water temperature |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
King 2001.
| Methods | RCT | |
| Participants | Children < 8 years attending A&E for injury or medical complaint | |
| Interventions | I = home safety inspection + information on correcting any deficiencies, discount vouchers for safety equipment, demonstrations of use of safety devices + information on preventing specific injuries provided by researcher C = home safety inspection & safety pamphlet. | |
| Outcomes | Outcomes measured at 12 (safety practices) and 36 (medically attended injuries) months: Self reported medically attended injuries (injury requiring attention by doctor) Stores matches or lighters out of reach Safe hot tap water not exceeding 54 degrees Celsius Functional smoke alarm Possession of a fire extinguisher Safe storage of cleaning products Use of stair gate Use of baby walker Small objects kept out of reach CRCs on cleaning products in kitchen I = 238/482, C = 233/469, OR 0.98 (0.77 to 1.27) Safe storage of bathroom cleaning products I = 255/482 C = 261/469 OR 0.90 (0.69 to 1.16) CRC's on bathroom cleaning products I = 355/482, C = 347/469, OR 0.98 (0.74 to 1.31) No windows opened easily beyond 6 inches in the living room I = 254/482, C = 238/469, OR 1.08 (0.84 to 1.39) No windows opened easily beyond 6 inches in the bedroom I = 299/482, C = 285/469, OR 1.05 (0.81 to 1.37) |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Kolko 2001.
| Methods | Non‐randomised controlled trial Participants only randomised to I1 and I2 arms. C arm families were those scheduled to have a home visit from a fire fighter prior to the study, those living too far from the clinic where CBT and FSE were provided and 2 families who would not agree to randomisation. |
|
| Participants | Boys referred for services by the City of Pittsburgh bureau of fire | |
| Interventions | I1 = CBT (cognitive behavioural therapy) ‐ designed to encourage behaviours other than fire setting I2 = FSE (fire safety education) ‐ instruction in fire safety skills, prevention practices, fire protection and evacuation C = HVF (home visit by firefighter) providing information about the danger of fires, the function of firefighters and asking children to promise not to get involved in unsanctioned fire play | |
| Outcomes | Outcomes measured at 13 weeks and 1 year: Any fire setting incident: At 13 weeks I1 = 3/17 I2 = 2/14 C = 4/14 I1 vs C OR 0.54 (0.10 to 2.94) I2 vs C OR 0.42 (0.06 to 2.77) At 1 year I1 = 4/17 I2 = 2/13 C = 7/14 I1 vs C OR 0.31 (0.13 to 1.43) I2 vs C OR 0.18 (0.03 to 1.14) Any match play incident At 13 weeks I1 = 6/17 I2 = 3/14 C = 4/14 I1 vs C OR 1.36 (0.30 to 6.28) I2 vs C OR 0.68 (0.12 to 3.83) At 1 year I1 = 6/17 I2 = 1/14 C = 8/14 I1 vs C OR 0.41 (0.10 to 1.75) I2 vs C OR 0.06 (0.01 to 0.57) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n I1 arm had higher, and I2 arm had lower frequency of child reported fire setting and match play incidents at baseline than control arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Krug 1994.
| Methods | CBA (C) Allocated at level of district | |
| Participants | Populations of 2 districts, Gelukspan (intervention) and Lehurutshe (control), Western Transvaal, South Africa | |
| Interventions | I = provision of child resistant kerosene container to households with small children C = no child resistant kerosene container provided | |
| Outcomes | Outcomes measured at 14 months: Medically attended kerosene poisonings ‐ Mean (SD) incidence of kerosene poisoning after CRC distribution. I = 4.54 (3.46), C = 9.8 (5.63), P = 0.015 |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Lacoutre 1978.
| Methods | CBA (C) Allocation at level of towns | |
| Participants | School children aged 6‐14 years in Wilmington (intervention) and Scituate (control), Massachusetts | |
| Interventions | I = community poison prevention education programme, directed at school children C = no community poison prevention education programme | |
| Outcomes | Period over which outcomes measured not reported. Possession of ipecac ‐ reports change in percentage of families having ipecac but does not report baseline prevalence. Significantly more intervention group families had ipecac than control group families, P < 0.05. |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ u Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
LeBailly 1990.
| Methods | Non‐randomised controlled trial Sequential allocation to treatment group |
|
| Participants | Families attending 2 paediatric group practices, 1 in urban area, other in suburban area | |
| Interventions | I1 = well child visit + safety equipment I2 = well child visit + safety equipment + safety counselling by physician I3 = well child visit + safety counselling by physician C = well child visit | |
| Outcomes | Outcomes measured at 9 months: Possession of fire extinguishers Functional smoke alarm ‐ Intervention groups (counselling and equipment and equipment only) had significantly greater use of fire extinguishers and smoke alarms. No figures or P values reported. Possession of ipecac ‐ Significantly more intervention group families (counselling and equipment and equipment only) possessed ipecac. No figures or P values reported. Use of outlet covers ‐ Intervention groups (counselling and equipment and equipment only) had significantly greater use of socket covers. No figures or P values reported. |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Lindqvist 1998a.
| Methods | CBA (C) Allocated at level of municipalities. | |
| Participants | Populations of 2 communities, Motala (intervention), Mjolby (control) | |
| Interventions | I = community injury prevention programme including multi‐agency collaboration, mass media campaigns, nurses provided age specific safety information in compulsory annual health visits. Video on hazards distributed to all families with children < 6 years, safety products and environmental modifications displayed at public places C = no community injury prevention programme | |
| Outcomes | Outcomes measured over 5‐6 years: Medically attended injuries (health centre attendance, ED attendance, hospital admission and deaths) for home injuries. Medically attended poisonings ‐ I = 29/8566 pre intervention and 17/8315 post intervention. Not reported for control area. RR post intervention to pre intervention, in intervention area: 0.60 (0.33 to 1.10) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Llewellyn 2003.
| Methods | RCT | |
| Participants | Parents with intellectual disability who were the primary carers of children < 5 years | |
| Interventions | I1= weekly home visits covering a different topic each week e.g. fire, electrical safety. I2= lesson books received by mail covering the same topics as I1 but without face to face contact C1 = current community services C2 = current community services | |
| Outcomes | Outcomes measured over 3 months: Mean (SD) hazard score comprising precautions taken to deal with 114 possible dangers in and around the home 1st post programme assessment: I1 = 60.35 (21.94) versus I2 = 48.73 (10.77) versus C1 = 53.3 (12.88), P < 0.001 2nd post programme assessment: I2 = 88.09 (34.92) versus C1 = 57.5 (11.48), P < 0.001 |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a C2 initially randomly allocated but reallocated to C1 to ensure completed program in study period | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Mackay 2002.
| Methods | RCT (C) Allocation at level of schools | |
| Participants | Elementary school children attending 12 schools | |
| Interventions | I = Risk Watch safety curriculum delivered by teachers for one year C = usual curriculum | |
| Outcomes | Outcomes measured over 12 months: Parental reported medically attended injuries and near misses ‐ No significant difference in medically attended injuries or near misses. No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Mallonee 1996.
| Methods | CBA (C) Allocation at level of geographical areas of a city | |
| Participants | Population of a 24 square mile area of Oklahoma City (intervention) and population of the rest of Oklahoma (control) | |
| Interventions | I = distribution of smoke alarms door to door by volunteers and community agencies to homes without a smoke alarm C = no smoke alarm distribution | |
| Outcomes | Outcomes measured over 4 years: Fire‐related injury rates ‐ Injury rate decreased 81% in the intervention area but only 7% in the control area. Only 2 children under 5 years of age were injured in the intervention area in the 6 years post intervention (denominator not reported). Numerator and denominator for child injury rate not reported for control area. |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n Area with highest fire injury rate chosen for intervention and rest of city chosen as control area. Lower household income in intervention area, lower property values and more fires started by children in the intervention area | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Matthews 1988.
| Methods | Non‐randomised controlled trial 18 mothers allocated using random numbers, 8 by alternation |
|
| Participants | 26 mothers of toddlers recruited from clinics, day care centres | |
| Interventions | I = home safety inspection, video, handouts, modelling re: safety and managing dangerous child behaviour, hot water thermometers, choke tube C = home visit with video, handouts, modelling on language simulation | |
| Outcomes | Outcomes measured over 2 weeks: Possession of smoke alarm Functional smoke alarm |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Mayer 1998.
| Methods | RCT | |
| Participants | Parents of children attending an orthopaedic outpatient clinic, with at least one child aged 0‐9 years | |
| Interventions | I = 20 minute video about lawnmower injuries and safety shown in orthopaedic clinic & educational leaflet C = no video | |
| Outcomes | Outcomes measured over 7 weeks: Not leaving mower running I = 22/30, C = 17/35, OR 2.91 (1.02 to 8.29) Making children stay indoors I = 19/30, C = 12/32, OR 2.88 (1.03 to 8.07) Tell children to leave yard I = 25/29, C = 25/33, OR 2.00 (0.53 to 7.50) Never leave child in yard I = 19/29, C = 15/34, OR 2.41 (0.87 to 6.69) Removal of debris prior to mowing I = 29/30, C = 29/34, OR 5.00 (0.55 to 45.48) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
McDonald 2005.
| Methods | RCT | |
| Participants | Parents of children aged 6 weeks to 24 months, attending well child clinic | |
| Interventions | I = tailored safety advice in well child clinic + feedback report to paediatrician to encourage safety counselling + information on safety equipment savings at child safety centre C = usual care | |
| Outcomes | Outcomes measured over 1 month: Possession of smoke alarm Possession of ipecac Use of stair gate Safe storage of medicines Safe storage of cleaning products Has changed smoke alarm batteries in last 6 months |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
McLoughlin 1982.
| Methods | CBA (C) Allocation at level of communities. | |
| Participants | Populations of Lynn, Quincy and Salem and Saugus (Intervention) and Holyoke and South Hadley (control), Massachusetts. | |
| Interventions | I = mass media campaign and school and community intervention programs C = media campaign only | |
| Outcomes | Outcomes measured over 8 months: Medically attended thermal injuries ‐ no significant difference in thermal injury rates pre intervention to post intervention in children in the intervention community. No p values reported | |
| Notes | Blinding ‐ u
Outcomes 80% ‐ u
Balance ‐ u Injury outcomes ascertained from injury surveillance system, but hospitals involved did not cover all residents and did not include private practices |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Miller 1982.
| Methods | Non‐randomised controlled trial (C) Allocated at level of 2 week periods of clinic attendance and sequential allocation by date of attendance | |
| Participants | Children attending for routine paediatrician healthcare | |
| Interventions | I = pamphlet and a one minute educational message by paediatrician, plus low cost smoke detector C = usual care | |
| Outcomes | Outcomes measured at 6 weeks Functional smoke alarm |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Mock 2003.
| Methods | CBA (C) Allocated at level of clinics. | |
| Participants | Upper socioeconomic stratum (SES) ‐ two private clinics Middle stratum ‐ two clinics charging low fees Lower stratum ‐ subsidised clinics | |
| Interventions | I1 (upper) ‐ lectures and demonstrations lasting 6 hours. Use of audio visual material including The Injury Prevention Program (TIPP) I2 (middle) ‐ as above but some participants also received clinic‐based counselling I3 (lower) ‐ half hour household visits by nurses and some audio visual materials also used C = standard injury prevention counselling | |
| Outcomes | Outcomes measured at 6 months: Functional smoke alarm Tested hot water temperature I1 = 0/25, C1 = 2/29, I2 = 0/18, C2 = 0/36, I3 = 1/27, C3 = 0/15; ORs not calculable Score of preventive behaviours ‐ Mean (SD) percent safe response scores: Upper SES I = 64.7 (12.9) pre, 72.8 (9.9) post, P < 0.001; C = 66.3 (12.8) pre, 63.9 (13.4) post, P = 0.12 Middle SES I = 60.2 (13.7) pre, 68.0 (11.5) post, P < 0.001; C = 54.3 (14.8) pre, 56.0 (15.5) post, P = 0.28 Lower SES I = 54.2 (14.9) pre, 61.8 (13.3) post, P < 0.001; C = 55.6 (16.2) pre, 59.7 (19.7) post, P = 0.09. |
|
| Notes | I1, I2 and I3 arms combined for meta‐analyses Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n Intervention arm had higher percentage of safe responses at baseline than control arm |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Moller 1996.
| Methods | CBA (C) Allocation at level of communities. | |
| Participants | Populations of 5 municipalities (number of intervention and control municipalities not specified) | |
| Interventions | I = community injury prevention programme including multi‐agency collaboration and utilizing injury data to target injury interventions C = no community injury prevention programme | |
| Outcomes | Outcomes measured at 2 years: Medically attended injuries (not defined) ‐ Significantly lower risk of home and play accidents amongst children aged 0‐5 years in intervention group than control group. No figures or P values reported. | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Mueller 2008.
| Methods | RCT | |
| Participants | Households with low to mid‐level income | |
| Interventions | I1= Ionization smoke alarm installed + instructions given in maintenance + fire extinguisher provided I2 = Photoelectric smoke alarm installed + instructions given in maintenance + fire extinguisher provided |
|
| Outcomes | Outcomes measured at 9 and 15 months: At 9 months: Functional smoke alarm. I1=264/332, I2=322/340; OR 0.22 (0.12 to 0.38) At 15 months: Functional smoke alarm. I1=239/311, I2=287/314; OR 0.31 (0.19 to 0.51) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Nansel 2002.
| Methods | RCT | |
| Participants | Parents of children aged 6‐20 months attending well child check | |
| Interventions | I = computer generated tailored safety advice in well child clinic C = computer generated generic safety advice in well child clinic | |
| Outcomes | Outcomes measured at 3 weeks: Safe hot water temperature <= 48.9 degrees Celsius Possession of smoke alarm Hot drinks/food out of reach Safe storage of medicines Safe storage of cleaning products Possession of ipecac Poison centre number accessible Use of stair gate Use of baby walker Never left child alone in bath Smoke alarm batteries checked or changed Use of socket covers Never left child alone in area of paddling pool I = 10/11, C = 15/16, OR 0.67 (0.04 to 11.94) Never left paddling pool full of water after use I = 11/11, C = 14/16, OR Not calculable Swimming pool has fence with locked gate I = 1/1, C = 2/2, OR Not calculable Never left child alone in pool area I = 1/1, C = 2/2, OR Not calculable Risk scores comprising injury risk behaviours for burns/fire, falls, poisoning, drowning ‐ Decrease in mean (SD) risk score I = 4.68 (6.44), C = 1.54 (5.58), P = 0.003 |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Nansel 2008.
| Methods | Non‐RCT Participants randomly allocated to I1 and C arms and remainder allocated to I2 |
|
| Participants | Parents of children aged <= 4 years attending well child visits at 3 paediatric clinics with mainly low to middle income patients | |
| Interventions | I1 = tailored injury prevention education I2 = tailored injury prevention education and provider tailored information C = general education |
|
| Outcomes | Outcomes measured at 1 month: Possession of smoke alarm Safe hot water temperature Hot drinks/food out of reach Safe storage of medicines Safe storage of cleaning products Poison centre number accessible Use of stair gates Use of baby walker Never leaves child alone on high surface Never left child alone in bath Turns pan handles away from edge of stove I1=7/7, I2=11/12, C=12/14, OR combining both I arms: 3.00 (0.14 to 186.62) Almost always keeps child away from stove or oven I1=4/7, I2=10/12, C=11/13, OR combining both I arms: 0.51 (0.04 to 3.98) |
|
| Notes | I1 and I2 arms combined for meta‐analyses Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n Participants in I2 arm were older, more likely to be Caucasian and had lower educational level than those in C arm. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Odendaal 2008.
| Methods | RCT | |
| Participants | Households with children <10 years old living in low‐income communities | |
| Interventions | I = 4 home visits including safety education, home inspection and distribution of free safety devices with a demonstration of use (first aid kit, roll of insulation tape, safety nails, 2L plastic paraffin container and a bag and hook for safe storage. C = usual care |
|
| Outcomes | Outcomes measured at 1 week: Hazard scores for thermal injuries, poisoning and falls 88 item home safety checklist. Mean (SE) score, Mean difference: Total safety score. I=20.3 (0.89) C=23.9 (0.92), 3.6 (1.12 to 6.16) Electrical burns score. I=3.0 (2.70) C=3.9 (0.29), 0.9 (0.15 to 1.70) Paraffin burns score. I=2.6 (0.24) C=3.3 (0.23), 0.7 (0.04 to 1.37) Burns safety practices score. I=6.8 (0.19) C=7.1 (0.21), 0.3 (‐0.31 to 0.80) Poisoning score. I=2.9 (0.23) C=4.0 (0.25), 1.1 (0.44 to 1.77) Falls score. I=5.0 (0.29) C=5.6 (0.30), 0.6 (‐0.16 to 1.47) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Ohn 2005.
| Methods | CBA (C) Allocation at level of "Sure‐Start" areas | |
| Participants | Children aged 0‐4 years in 2 Sure Start areas, Foxhill & Parsons Cross (intervention) and Firth Park (control) | |
| Interventions | I = free installation of home safety equipment (smoke alarms, fire guards and stair gates) C = no free installation of home safety equipment | |
| Outcomes | Outcomes measured over 3 years: Medically attended injuries (ED attendances and hospital admissions) ‐ No significant difference in the odds of an injury attendance being from the intervention area as opposed to the control area. No P value reported, OR 0.91 (0.82 to 1.02) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n Control arm more deprived | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Olds 1994.
| Methods | RCT | |
| Participants | Primiparous women registering before the 26th week of pregnancy from upstate New York, <19 years of age, single parents, or low socio‐economic status | |
| Interventions | I1 = families were provided with a home nurse visitor during pregnancy in addition to screening and transportation services I2 = as I1 but the nurse continued to visit until the child was 2 years of age C1 = screening for sensory and developmental problems C2 = free transportation for regular prenatal and well child care clinics | |
| Outcomes | Outcomes measured at 34 and 46 months: Safe storage of poisonous substances ‐ no significant difference. No figures or P values reported Hazard score comprising exposure to hazards in the home At 34 months: log incidence of hazardous exposures I2 = ‐1.75, C1 + C2 = ‐1.04, P = 0.04 At 46 months: log incidence of hazardous exposures I2 = ‐1.94, C1 + C2 = ‐0.83, P = 0.003 |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Ozanne‐Smith 2002.
| Methods | CBA (C) Allocated at level of communities | |
| Participants | Population of 2 communities, Shire of Bulla (intervention) and Shire of Melton (control) | |
| Interventions | I = community injury prevention programme including multi‐agency collaboration, promotion of child safety equipment, safety education for parents from healthcare staff, child safety courses, distribution of home safety package, exhibitions, use of mass media C = no community injury prevention programme | |
| Outcomes | Outcomes measured over 4‐5 years: Medically attended injuries (ED attendance, hospital admission or death) ‐ No significant difference between the control and intervention community. Figures and P values not reported. | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Control community had higher injury rates at baseline | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Paul 1994.
| Methods | RCT | |
| Participants | Families with children aged 10 months to 2 years born at local rural hospital | |
| Interventions | I = home safety check + tailored education booklet + local safety equipment retail outlets identified, mail order addresses provided or equipment ordered through research team and made available at local hospital C = none of the above | |
| Outcomes | Outcomes measured between 5 and 9 months: Possession of a cooker guard Thermostatic mixer valves in kitchen/bathroom/laundry Spring loaded safety taps in kitchen/bathroom/laundry Fitted fireguard No significant difference in any thermal injury outcomes. No figures or P values reported Lockable cabinet for storage of poisons in kitchen/bathroom/laundry ‐ Intervention group more likely to have lockable cabinets post intervention than pre intervention, P < 0.05 Possession of ipecac ‐ Intervention group more likely to have ipecac than control group, P < 0.01. Figures not reported. Roof areas child can gain access to Outside steps with no railings and non‐climbable barrier Balcony without adequate non‐climbable barrier High windows which open more than 10 cm Climbable fencing Interior steps without railings Non‐climbable barriers High chair without harness Intervention group less likely to have accessible roof areas post intervention than pre intervention (P < 0.05). No significant difference in other falls injury outcomes. Figures and P values not reported. Use of earth leakage circuit breakers Safety shuttered power points ‐ no significant difference in any electrical injury outcomes. Figures and P values not reported. Protected sharp edges ‐ Intervention group less likely to have bench tops with sharp edges, P < 0.001. Figures and P values not reported. No toys with small parts ‐ No significant difference between intervention and control groups. Figures and P values not reported Adequate pool fencing ‐ no significant difference in any drowning injury outcomes. Figures and P values not reported Use of safety glass in glass doors ‐ no significant difference. Figures and P value not reported Hazard score calculated based on a 24 item home hazard checklist ‐ Mean (SD) hazard score: I = 9.39 (2.30), C = 9.91 (2.76), P = NS |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Petridou 1997.
| Methods | CBA (C) Allocation at level of islands | |
| Participants | Population of two Greek islands, Naxos (intervention) and Spetses (Control) | |
| Interventions | I = community intervention including safety seminars for parents, workshops with teachers promoting school safety, courses with primary and secondary school children on safety and resuscitation, leaflets; plus focused intense intervention: lay home visitors, weekly visits to discuss home safety in households with children ( <=18 years) or older people ( >=65 years) C = none of the above | |
| Outcomes | Outcomes measured over 20 months: Possession of a fire extinguisher Poison centre number accessible Possession of ipecac Slip resistant bathroom mat Has a fire escape plan Safe balconies I = 24/128, C = 36/131, OR 0.61 (0.34 to 1.10) Safe indoor stairs I = 104/128, C = 110/131, OR 0.83 (0.43 to 1.58) Safe outdoor stairs I = 32/128, C = 17/131, OR 2.24 (1.17 to 4.27) Has circuit breaker ‐ Significant increase in the use of circuit breakers in intervention group from baseline. No difference in circuit breakers between intervention and control group I = 115/128, C = 120/131, OR 0.81 (0.35 to 1.88). Score comprising 28 home safety practices ‐ Mean (SD) score I = 15.18 (2.62), C = 15.24 (2.17) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ y |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Phelan 2010.
| Methods | RCT | |
| Participants | Pregnant women, aged 18 years and over, < 19 weeks gestation, attending pre‐natal practices in Cincinnati, USA. | |
| Interventions | I = home safety inspection, provision and fitting of free safety equipment when child is aged 3‐6 months (stair gates, non‐slip matting under rugs, window guards, repair of stair handrails, cupboard/drawer locks, door knob covers, storage bins, socket covers, smoke detectors, CO detectors, stove guards, stove locks) and safety advice handout. C = prior to child's birth family given targeted home repairs to control lead hazards (e.g. paint stabilization, water filters) |
|
| Outcomes | Outcomes measured at 12 and 24 months: Medically attended injuries (phone consultations, clinic or ED attendances) Modifiable medically attended injuries (phone consultations, clinic or ED attendances) Functional smoke alarm Safe storage of poisons Poison centre number accessible Use of baby walker Use of window locks Use of stair gate Non‐slip bath mat Use of socket covers Sharp objects out of reach Small objects kept out of reach Possession of CO detector: At 12 months: I=118/139 C=64/138, OR 1.83 (1.22 to 2.74) At 24 months: I=89/120 C=56/119, OR 1.58 (1.01 to 2.45) Number and density of injury hazards. Not reported. Injury hazards were significantly reduced in intervention group but not in control group at 1 and 2 years (p<0.004). |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Pless 2007.
| Methods | RCT | |
| Participants | Parents attending 5 private paediatric practices | |
| Interventions | I = product related posters pertaining to the dangers of venetian blinds and one to the risk of strangulation from clothing drawstrings C = no product related posters |
|
| Outcomes | Outcomes measured at 2 weeks: Taken recommended safety measures for clothing drawstrings. I=48/439 C=47/369, OR 0.84 (0.54 to 1.32) Taken recommended safety measures for blind cords. I=276/439 C=238/369, OR 0.93 (0.69 to 1.26) Not adjusted for clustering |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Ponce De Leon 2007.
| Methods | CBA (C) | |
| Participants | Children aged 0‐14 years living in 5 WHO Safe Communities (Lidkoping, Skovde, Tidaholm, Mariestad and Falkoping) and the remaining 10 municipalities in the same district (C1) and the rest of Sweden (C2) | |
| Interventions | I = WHO Safe Communities injury prevention programme including multi‐agency collaboration, safety education for parents from healthcare staff, training parents in child safety and first aid, exhibitions, posters, use of mass media C1 = no community injury prevention programme C2 = no community injury prevention programme |
|
| Outcomes | Outcomes measured over 16 years Medically attended injuries (hospital admissions) Significant reduction in hospital admission rate in one of the 5 intervention areas (Lidkoping). Significant increase in hospital admission rate in one of the 5 intervention areas (Skovde). No significant difference in other 3 intervention areas. Lidkoping: place*time interaction regression coefficient ‐0.562 (SE 0.097) p<0.01. Skovde: place*time interaction regression coefficient ‐0.249 (SE 0.067) p<0.01. |
|
| Notes | Blinding ‐ u
Outcomes 80% ‐ y
Balance ‐ n Some intervention communities had higher injury rates at baseline than the rest of Sweden (C2). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Posner 2004.
| Methods | RCT | |
| Participants | Caregivers of children < 5 years attending ED for home injury | |
| Interventions | I = home safety counselling by trained lay personnel, home safety kit (cupboard and drawer locks, socket covers, bath tub spout covers, non‐slip bath decals, bath water thermometer, poison control centre number stickers, free small parts tester) + home safety literature C = home safety literature | |
| Outcomes | Outcomes measured over 10 weeks: Possession of smoke alarm Hot drinks/food out of reach Safe storage of medicines Safe storage of cleaning products Poison centre number accessible Plants not accessible Use of stair gate Use of baby walker Non‐slip bath decals Never leaves child alone on high surface Use of socket covers Sharp objects stored out of reach Never left child alone in bath Time since last tested battery < 6 months Has a fire escape plan Use of water thermometer I = 43/49, C = 13/47, OR 18.74 (6.45 to 54.47) Has spout covers for bath taps I = 39/49, C = 18/47, OR 6.28 (2.53 to 15.61) Always uses fire guard for electric or kerosene space heater while sleeping I = 4/8, C = 2/3, OR 0.50 (0.03 to 7.99) Cooks on back burners of cooker I = 25/49, C = 16/47, OR 2.02 (0.89 to 4.60) Turns pan handles towards back of cooker I = 29/49, C = 23/47, OR 1.59 (0.71 to 3.59) Often heats kitchen by leaving oven door open I = 0/49, C = 0/47, OR Not calculable Never leaving burning candles in empty room I = 11/15, C = 17/23, OR 0.97 (0.22 to 4.24) No overloaded electrical sockets (>=3 items plugged into a socket) I = 23/48, C = 15/47, OR 1.96 (0.85 to 4.52) Never smoking in bed and method of disposing of ashes I = 6/9, C = 10/11, OR 0.20 (0.02 to 2.39) Never stores chemicals in drinks bottle I = 49/49, C = 46/47 OR not calculable Child exposed to lead paint I = 8/49, C = 2/47, OR 4.39 (0.88 to 21.88) Possession of CO detector I = 14/49, C = 11/47, OR 1.31 (0.52 to 3.27) Tested CO detector within 6 months I = 6/11, C = 9/11, OR 0.27 (0.04 to 1.85) Never places a carrier on a high surface I = 6/49 C = 6/47, OR 0.95 (0.28 to 3.20) Does not let child eat: Hot dogs I = 15/49, C = 14/47, OR 1.04 (0.43 to 2.49) Candy I = 25/49, C = 25/47, OR 0.92 (0.41 to 2.04) Carrots I = 31/49, C = 24/47, OR 1.65 (0.73 to 3.73) Nuts I = 38/49, C = 28/47, OR 2.34 (0.96 to 5.70) Grapes I = 11/49, C = 10/47, OR 1.07 (0.41 to 2.82) Uses small parts tester I = 27/49, C = 5/47, OR 10.31 (3.48 to 30.50) Eight category safety scores were calculated from responses to questions about safety practices. Fires (14 items) I = 81.7, C = 80.6, P < 0.61 Burns (12 items) I = 76, C = 68.4, P < 0.03 Poisoning (6 items) I = 74.4, C = 64.9, P < 0.02 Submersion (4 items) I = 95.9, C = 92.9, P < 0.33 Aspiration (6 items) I = 59.7, C = 52.7, P < 0.12 Cuts (6 items) I = 81.0, C = 66.4, P < 0.001 Falls (7 items) I = 58.9, C = 57.4, P < 0.79 Safety device use (9 items) I = 65.4, C = 44.3, P < 0.001 |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Rey 1993.
| Methods | CBA (C) Allocation at level of towns | |
| Participants | Population of two towns, Chambery (intervention) and Annecy (control) | |
| Interventions | I = community injury prevention programme including safety education for children in schools, exhibitions, apartment demonstrating home hazards, school children presenting accident projects to members of the public, film show about safety and use of mass media C = no community injury prevention programme | |
| Outcomes | Outcomes measured at 6 months: Medically attended injuries (physician attendance, clinic attendance, hospital attendance or admission). Significant reduction in domestic accidents requiring a medical consultation in intervention compared to control group, P < 0.02. No figures reported. Significant increase in accidents requiring urgent medical attention for children aged 6‐10 years in intervention group comparing post to pre injury rates. No figures reported. No significant difference in hospitalisation rates between intervention and control groups. No figures or P value reported. | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Rowland 2002.
| Methods | RCT | |
| Participants | 2145 households from a local authority housing estate | |
| Interventions | I1 = ionisation sensor with a zinc battery I2 = ionisation sensor with a zinc battery and pause button I3 = ionisation sensor with a lithium battery and pause button I4 = optical sensor with a lithium battery I5 = optical sensor with a zinc battery | |
| Outcomes | Outcomes measured at 15 months: Functional smoke alarm ‐ I1 = 86/141, I2 = 56/116, I3 = 44/63, I4 = 24/79, I5 = 40/57 |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Sangvai 2007.
| Methods | RCT | |
| Participants | Parents of children aged 0‐5 years enrolled at 3 paediatric practices | |
| Interventions | I = safety counselling from physician and researcher, free safety equipment (smoke detectors, gun locks, cabinet locks, and water temperature cards) and brief educational handout for parents. C = usual care |
|
| Outcomes | Outcomes measured at 6 months: Functional smoke alarm Safe hot water temperature Safe storage of poisons |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y for injury outcomes, n for safety practices Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Schelp 1987.
| Methods | CBA (C) Allocated at level of municipality | |
| Participants | Population of two municipal districts, Falkoping (intervention) and Lidkoping (control) | |
| Interventions | I = community injury prevention programme including multi‐agency collaboration, use of mass media, exhibitions at child health centres, demonstrations of safety equipment, use of checklists in child health surveillance visits, increased local availability of child safety equipment, parent education C = no community injury prevention programme | |
| Outcomes | Outcomes measured at 12 months: Medically attended injuries (clinic attendance, hospital attendance) occurring at home ‐ incidence I = 48.6/1000 pre, 32.2/1000 post intervention, P < 0.001. Figures not presented for control area | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Control municipality had higher injury rates at baseline | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Scherz 1968.
| Methods | CBA (C) Allocation at level of geographic area covering Army Post Exchanges | |
| Participants | Families of army personnel | |
| Interventions | I = free child resistant container attached to boxes of children's aspirin, sold at Post Exchanges C = children's aspirin sold at other sites without CRC attached | |
| Outcomes | Outcomes measured over 6 months: Medically attended aspirin poisoning ‐ proportion of all poisonings due to aspirin in intervention area pre = 27/38, post = 5/22. No P value reported. |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Schlesinger 1966.
| Methods | CBA (C) Allocated at level of housing developments with 10 or more homes | |
| Participants | Population of children aged < 7 years, in housing developments | |
| Interventions | I = community injury prevention programme including neighbourhood discussion groups, monthly newsletter to families, speakers at group and club meetings, distribution of safety literature C = no community injury prevention | |
| Outcomes | Outcomes measured over 24 months: Medically attended injuries (physician attendance, dentist attendance, hospital attendance) ‐ No significant difference in the rate of accidents in the intervention and control groups. No figures or P values reported. | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Intervention areas had higher injury rates at baseline than control areas | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Schwarz 1993.
| Methods | CBA (C) Allocation at census tract level | |
| Participants | Population of 9 census tracts, predominantly low income, urban, African‐American | |
| Interventions | I = home inspection and modification + education in homes and at block and community meetings. Provision of ipecac, smoke alarms and batteries, bath water thermometers, night lights, emergency centre number sticker and fridge sticker with information on preventing injury C = none of above | |
| Outcomes | Outcomes measured over 12 months: Fire‐related injuries/1000 ‐ I ‐ Before: 1.83, During: 1.14, After: 0.86. Incidence change (after vs before): 0.5 (0.4 to 0.6) C ‐ Before: 1.34, During: 2.68, After: 1.11. Incidence change (after vs before): 0.8 (0.6 to 1.1) Functional smoke alarms ‐ I = 866/902, C = 816/1060, OR 7.19 (4.98 to 10.64) Possession of ipecac Safe storage of medicines Medicines not in CRCs ‐ I = 66/250, C = 41/250, OR 1.83 (1.81 to 2.83) analyses not adjusted for clustering |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ y | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Schwebel 2009.
| Methods | RCT | |
| Participants | Female heads of households in 2 low income housing districts | |
| Interventions | I=kerosene safety intervention using a “train the trainers” model where trainers train local paraprofessionals to deliver education to communities, plus educational materials for paraprofessionals to distribute in communities on safe use of kerosene and kerosene powered appliances and treatment of kerosene related injuries. C=usual care |
|
| Outcomes | Outcomes measured at 4 weeks: Paraffin appliances on flat surfaces. I=92/95 C=102/108; OR 1.80 (0.44 to 7.42) Paraffin appliances on steady surfaces. I=89/96 C=99/107; OR 1.03 (0.36 to 2.95) Paraffin appliances on surfaces without tablecloths. I=24/95 C=31/108; OR 0.84 (0.45 to 1.57) Paraffin appliances out of reach. I=28/96 C=33/108; OR 0.94 (0.51 to 1.71) Flammable materials at least 1 metre away from all paraffin appliances. I=2/96 C=7/108; OR 0.31 (0.06 to 1.52) Dry sand available to extinguish flames. I=0/98 C=0/109; OR not calculable. Paraffin stored out of reach. I=16/92 C=32/109; OR 0.51 (0.26 to 1.00) Paraffin stored away from food. I=85/92 C=89/109; OR 2.73 (1.10 to 6.78) Paraffin stored in vessel marked “paraffin”. I=2/92 C=2/109; OR 1.19 (0.16 to 8.61) Paraffin stored in beverage container. I=68/92 C=103/109; OR 0.17 (0.06 to 0.42) Paraffin stored in vessel with CRC. I=0/92 C=3/109; OR not calculable Paraffin stored in covered container. I=55/92 C=95/109; OR 1.80 (0.44 to 7.42) Mean kerosene safety practices score (SD) score Baseline I=0.38 (0.09) C=0.41 (0.10) Follow‐up I=0.49 (0.17) C=0.46 (0.13) Mean change from baseline I=0.10 (0.18) C=0.05 (0.16) p<0.05 Analyses not adjusted for clustering |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Shani 2003.
| Methods | RCT (C) Allocation at level of school classes | |
| Participants | Bedouin schoolchildren aged 12‐13 years | |
| Interventions | I1= school safety slide show on burn prevention I2= school safety video show on burn prevention I3= school safety slide and video show on burn prevention | |
| Outcomes | Outcomes measured over 2 months: Burn related safety behaviour mean (SD) scores: I1 = 3.56 (0.56), I2 = 3.58 (0.51), I3 = 3.45 (0.76) P > 0.05 |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ u Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Shapiro 1987.
| Methods | RCT | |
| Participants | Women admitted to the maternity ward of 3 hospitals | |
| Interventions | I = pamphlet about tap water scalds and thermometer for testing, plus a one minute educational message summarising pamphlet C = pamphlet and thermometer | |
| Outcomes | Outcomes measured between 2 and 9 months: Tested hot water temperature I = 155/302 C = 88/302, OR 2.56 (1.83 to 3.59) Lowered hot water temperature Figures and P value not reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Steele 1985a.
| Methods | CBA (C) Allocated at level of cities | |
| Participants | Populations of Escondido (intervention) and Chula Vista (control), California | |
| Interventions | I = community poison prevention programme including mass media, training of healthcare personnel to provide poison prevention education to clients, safety fairs C = no community poison prevention programme |
|
| Outcomes | Outcomes measured over 12 months: Medically attended poisonings ‐ no significant difference in post versus pre injury rates in intervention or control communities. Poison centre utilisation Possession of ipecac ‐ no significant difference in poison centre utilisation or in possession of ipecac. No figures or P value reported. |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ u Unclear how intervention city chosen | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Steele 1985b.
| Methods | RCT | |
| Participants | Parents of children aged 6 months to 4 years attending well baby clinics, aged >= 18 years, English speaking with a telephone available | |
| Interventions | I1 = one‐to‐one poisoning education, with reinforcement by physician I2 = I1 + burns education I3 = one‐to‐one burns education, with reinforcement by physician C = no education | |
| Outcomes | Outcomes measured at 3, 6 and 12 months: Self reported poisoning ‐ no significant differences for poison injury rates Poisoning prevention behaviours Poison centre utilisation ‐ Intervention groups exhibited significantly more hazard reducing behaviour. No figures or P values reported |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ u Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Svanstrom 1995.
| Methods | CBA (C) Allocated at level of municipalities | |
| Participants | Population of 5 municipalities; Lidkoping (intervention), 4 bordering municipalities (control) | |
| Interventions | I = community injury prevention programme including multi‐agency collaboration, safety education for parents from healthcare staff, training parents in child safety and first aid, exhibitions, posters, use of mass media C = no community injury prevention | |
| Outcomes | Outcomes measured over 7 years: Medically attended injuries (hospital admissions) | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Intervention municipality had higher injury rates at baseline than control municipalities. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Swart 2008.
| Methods | RCT (C) Allocation at level of blocks of households |
|
| Participants | Households with children <= 10 years old living in low‐income communities | |
| Interventions | I = 4 home visits focusing on child development and the prevention of burns, poisoning and falls and providing safety education + free safety devices (child proof locks and paraffin container safety caps). C = usual care |
|
| Outcomes | Outcomes measured at 2 weeks: Paraffin stove used as heater. I = 28/189 C = 21/188; OR 1.65 (0.46 to 5.84) Paraffin stove filled whilst warm. I = 19/189 C = 18/188; OR 1.13 (0.44 to 2.89) Paraffin heater < 30cm from flammable material. I = 8/189 C = 4/188; OR 2.02 (0.60 to 6.83) Paraffin heater on unstable surface. I = 0/189 C = 2/188; OR not calculable Paraffin cooker < 30cm from flammable material. I = 39/189 C = 22/188; OR 2.39 (0.53 to 10.82) Paraffin cooker on unstable surface. I = 7/189 C = 5/188; OR 1.40 (0.44 to 4.49) Paraffin lamp < 30cm from flammable material. I = 12/189 C = 17/188; OR 0.60 (0.13 to 2.82) Paraffin lamp on unstable surface. I = 31/189 C = 45/188; OR 0.53 (0.19 to 1.45) Paraffin appliances on when family sleeping. I = 79/189 C = 69/188; OR 2.03 (0.57 to 7.26) Candles placed on unstable surface. I = 18/189 C = 12/188; OR 1.68 (0.38 to 7.51) Candles used < 30cm from flammable material. I = 27/189 C = 45/188; OR 0.53 (0.08 to 3.50) Tablecloth under candle, paraffin heater, stove or lamp. I = 34/189 C = 49/188, OR 0.75 (0.17 to 3.20) Beauty products properly labelled in tightly closed non‐glass containers. I = 185/189 C = 185/188; OR 0.75 (0.17 to 3.42) Safe storage of beauty products. I = 172/189 C = 157/188; OR 2.13 (1.00 to 4.53) Medicines properly labelled in tightly closed non‐glass containers. I = 186/189 C = 187/188; OR 0.33 (0.03 to 3.23) Safe storage of medicines. Paraffin properly labelled in tightly closed non‐glass containers. I = 173/189 C = 146/188; OR 5.02 (1.26 to 19.98) Safe storage of paraffin. I = 123/189 C = 114/188; OR 1.47 (0.51 to 4.25) Paraffin stored in CRC. I = 162/189 C = 128/188; OR 3.39 (1.28 to 9.02) Cleaning products properly labelled in tightly closed non‐glass containers. I = 184/189 C = 176/188; OR 6.04 (0.44 to 83.02) Safe storage of cleaning products. Cleaners stored on same shelf as food. I = 5/189 C = 5/188; OR 0.84 (0.17 to 4.14) Alcohol properly labelled in tightly closed non‐glass containers. I = 186/189 C = 185/188; OR 1.01 (0.20 to 5.07) Safe storage of alcohol. I = 183/189 C = 178/188; OR 1.76 (0.48 to 6.50) Rat poison properly labelled in tightly closed non‐glass containers. I = 187/189 C = 186/188; OR 1.01 (0.14 to 7.25) Safe storage of rat poison. I = 189/189 C = 185/188; OR not calculable. 90 item home safety checklist: Mean (SE) score, Mean difference: Total safety score. I = 13.9 (0.53) C = 14.2 (0.54), ‐0.31 (‐1.8 to 1.2) Electrical burns score. I = 1.1 (0.14) C = 1.3 (0.14), ‐0.19 (‐0.54 to 0.16) Paraffin burns score. I = 3.2 (0.21) C = 3.2 (0.21), ‐0.03 (‐0.64 to 0.57) Burns safety practices score. I = 2.5 (0.12) C = 2.9 (0.12), ‐0.41 (‐0.76 to ‐0.07) Poisoning score. I = 1.9 (0.11) C = 2.4 (0.20), ‐0.45 (‐1.01 to 0.11) Falls score. I = 3.7 (0.24) C = 3.6 (0.24), 0.09 (‐0.60 to 0.78) |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Sznajder 2003.
| Methods | RCT | |
| Participants | Socio‐economically disadvantaged families, with medical or psychological difficulties which place them at high risk | |
| Interventions | I = home safety counselling by health professionals, safety leaflets, free home safety kit (cupboard and drawer locks, door handle covers, furniture corner protectors, socket covers, non‐slip bath mat, fitted smoke alarm, poison control centre number stickers) C = home safety counselling + safety leaflets | |
| Outcomes | Outcomes measured over 2 months: Functional smoke alarm Possession of a fire extinguisher Stores matches out of reach Safe storage of medicines Safe storage of cleaning products No toxic plants in the home Use of stair gate Use of a baby walker Use of non‐slip bath mats Use of socket covers Small objects kept out of reach Hot water system has adjustable thermostat I = 5/47, C = 5/50; OR 1.07 (0.29 to 3.97) High chair safe I = 28/47, C = 34/50; OR 0.69 (0.30 to 1.59) Risk of falling from a window or balcony I = 9/46, C = 17/49; OR 0.46 (0.18 to 1.17) Cables/leads lying around likely to cause falls I = 6/46 C = 12/48; OR 0.45 (0.15 to 1.32) Carpets fixed safely I = 7/48 C = 6/50; OR 1.25 (0.39 to 4.04) Use of furniture corner covers I = 30/35, C = 20/34; OR 4.20 (1.31 to 13.50) Food items that can cause choking out of reach I = 45/50; C = 45/50, OR 2.50 (0.46 to 13.56) Cords and chains for blinds out of reach I = 6/25, C = 11/31; OR 0.57 (0.18 to 1.86) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Tan 2004.
| Methods | Non‐randomised controlled trial (C) Allocation at level of week of clinic attendance and sequential allocation to treatment arm | |
| Participants | Caregivers and infants aged 4‐5 months attending three health clinics | |
| Interventions | I = structured nurse counselling + leaflets aimed at discouraging walker use C1 = no nurse counselling C2 = no nurse counselling and no baseline data collection | |
| Outcomes | Outcomes measured when child 9 months of age: Self reported walker injuries: Toppling over on flat ground I = 12/228, C1+ C2 = 19/480; OR 1.35 (0.64 to 2.83) From falling down steps I = 2/228, C1+ C2 = 6/480; OR 0.70 (0.14 to 3.49) Hospitalised due to walker injury I = 0/228; C1+ C2= 1/480, OR not calculable Use of baby walker |
|
| Notes | C1 and C2 arms combined for meta‐analyses Blinding ‐ u Outcomes 80% ‐ y Balance ‐ y |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Thomas 1984.
| Methods | RCT | |
| Participants | Parents attending well‐baby classes | |
| Interventions | I = standard information and literature plus a lecture on burn prevention provided by nurse practitioners, leaflets on protecting home against fire, adjusting hot water settings and cost of smoke alarms at local stores, plus $7 discount coupon for a smoke alarm. C = standard information and literature | |
| Outcomes | Outcomes measured at 6 weeks: Safe hot water temperature Functional smoke alarm I = 28/29 C = not reported P > 0.05 |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Inadequate |
Vineis 1994.
| Methods | Non‐randomised controlled trial (C) Allocation at level of 2‐3 week periods of clinic attendance and sequential allocation to treatment group | |
| Participants | Parents of newborn babies | |
| Interventions | I = 15 minutes counselling by nurse + distribution of 3 educational booklets ‐ 1 on prevention of home injuries in childhood, 1 on smoking and one on passive smoking C = none of the above | |
| Outcomes | Outcomes measured over 2 and 4 years: Risk of burns ‐ no significant difference in preventive behaviours. No P values reported. Scores of risk of poisoning by (a) cleaning products and (b) medicines ‐ no significant difference in preventive behaviours. No P values reported. Scores of risk of falls ‐ no significant difference in preventive behaviours. No P values reported. Scores of risk of electric shock ‐ no significant difference in preventive behaviours. No P values reported. Risk of home injury score comprising behaviours relating to burns, poisonings, falls and electrical injury ‐ reports change from baseline in risk scores, but baseline scores not presented. No significant difference in risk scores between groups. No P values reported. |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ u | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Waller 1993.
| Methods | RCT | |
| Participants | A random sample of Dunedin area children taken from birth records | |
| Interventions | I = free plumbing advice, home visit to measure tap water temperature, discuss dangers of hot water in the home and how to reduce tap water temperature provided by nurses C1 = no home visit C2 = no home visit and no baseline data collection | |
| Outcomes | Outcomes measured at 4 months: Safe hot water temperature < 60 degrees Celsius |
|
| Notes | C1 and C2 arms combined for meta‐analyses Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Watson 2005.
| Methods | RCT | |
| Participants | Families with children < 5 years on caseloads of health visitors in deprived areas | |
| Interventions | I = health visitor safety consultation, free fitted safety equipment (stair gates, fire guards, cupboard and drawer locks, smoke alarms, window locks) C = usual care | |
| Outcomes | Outcomes measured at 12 and 24 months: Medically attended thermal injuries Medically attended poisonings Medically attended injuries (primary care attendance, ED attendance, hospital admission or death) Functional smoke alarms Fitted fire guard Safe storage of medicines Safe storage of cleaning products Use of stair gate Use of window locks Sharp objects stored out of reach |
|
| Notes | Blinding ‐ y(injuries) n(safety practices) Outcomes 80% ‐ y(injuries) n(safety practices) Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Williams 1988.
| Methods | RCT (C) Allocation at level of prenatal classes | |
| Participants | Pregnant women attending prenatal classes | |
| Interventions | I = 1 hour lecture, handouts on burn prevention, usual safety education. C = usual safety education. | |
| Outcomes | Outcomes measured at 1 month: Safe hot water temperature (not defined) Possession of smoke alarm Functional smoke alarm ‐ no significant difference in alarm ownership between groups. Figures and P values not reported |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ u Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Wissow 1989.
| Methods | RCT | |
| Participants | Families with children < 6 years attending paediatric ED or clinic following injury | |
| Interventions | I = home hazard inspection + education + free safety equipment provided at home C = free safety equipment provided at hospital | |
| Outcomes | Period over which outcomes measured not reported. Possession of a fire extinguisher ‐ no figures or P value reported Fire escape plan ‐ no figures or P value reported Possession of ipecac ‐ significantly more control group families had ipecac, P = 0.009. Poison centre number accessible ‐ no figures or P value reported Testing for lead poisoning ‐ no figures or P values reported Peeling paint ‐ no figures or P values reported Possession of bathmat slip guard ‐ no figures or P value reported Use of stair gates ‐ no P values reported Use of socket covers ‐ no figures or P values reported Sharp objects stored out of reach ‐ no figures or P values reported Mean number of hazards present calculated based on a 50 item home hazard inventory ‐ No significant difference in the mean number of hazards, P >0.05 No figures reported |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Woolf 1987.
| Methods | RCT (C) Allocated at level of week of clinic visit | |
| Participants | Families attending medical ED with children < 5 years Urban poor population | |
| Interventions | I = counselling by medical staff on poisoning treatment methods, leaflet on poison prevention, poison control centre number sticker + ipecac C1 = none of the above C2 = none of the above and no baseline data collection | |
| Outcomes | Outcomes measured over 6 months: Possession of ipecac Poison centre number accessible Storage of cleaning products, medicines, perfume ‐ no figures or P values reported |
|
| Notes | C1 and C2 arms combined for meta‐analyses Blinding ‐ y Outcomes 80% ‐ n Balance ‐ n/a |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Woolf 1992.
| Methods | RCT (C) Allocated at level of day of recruitment | |
| Participants | Families of children less than or equal to 5 years with a poisoning who contacted the poison control centre and did not have ipecac | |
| Interventions | I = mailed $1 coupon for ipecac, one cupboard lock, checklist for poison proofing the home, leaflets C = none of the above | |
| Outcomes | Outcomes measured over 3 months: Self reported repeat poisoning ‐ no significant difference. No figures or P value reported Possession of ipecac Poison centre number accessible Safe storage of cleaning products |
|
| Notes | Blinding ‐ y Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Yang 2008.
| Methods | RCT | |
| Participants | Rural households participating in a cohort study examining multiple health outcomes | |
| Interventions | I1 = installation of photoelectric smoke alarm with lithium battery I2 = installation of photoelectric smoke alarm with carbon‐zinc battery I3 = installation of ionizing smoke alarm with lithium battery I4 = installation of ionizing smoke alarm with carbon‐zinc battery |
|
| Outcomes | Outcomes measured at 12 months: Number of photoelectric vs. ionising alarms: I1+ 12=952/1018 I3+ I4=889/973; OR 1.30 (0.88 to 1.92) Number of alarms with lithium vs. carbon‐zinc battery: I1+ I3=975/1030 I2+ I4=866/961; OR 1.91 (1.30 to 2.82) Number of false alarms photoelectric vs. ionising alarms: I1+ 12=55/1018 I3+ I4=120/973; OR 0.41 (0.29 to 0.56) Number of false alarms with lithium vs. carbon‐zinc battery: I1+ I3=91/1030 I2+ I4=84/961; OR 1.05 (0.78 to 1.42) |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Yorkston 2007.
| Methods | CBA (C) | |
| Participants | Children aged 0‐4 years living in 2 intervention and 16 control communities | |
| Interventions | I = WHO Safe Communities injury prevention programme C = no community injury prevention programme |
|
| Outcomes | Outcomes measured over 7 years which included 2 years post commencement of intervention: Medically attended injuries (hospital admissions) No significant reduction in logarithmically transformed injury rates. Reduction in logarithmically transformed injury rates of 0.09 per 10,000 children aged 0‐4 years associated with intervention (95% CI ‐0.29 to 0.11) p=0.36. Adjusted for remoteness of area, marital status, indigenous population. |
|
| Notes | Blinding ‐ u
Outcomes 80% ‐ y
Balance ‐ no Intervention communities had higher baseline injury rates than control communities |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Ytterstad 1998.
| Methods | CBA (C) Allocated at level of cities | |
| Participants | Children < 5 years in the city of Harstad (intervention) and Trondheim (control) | |
| Interventions | I = promotion of cooker guards in electrical stores, mass media campaign to lower tap water thermostat to 55 degrees Celsius, health education, parental counselling and home assessment. C = none of the above | |
| Outcomes | Outcomes measured over 10 years: Medically attended thermal injuries Thermal injury severity and mechanism ‐ severity of stove and tap water scalds reduced in intervention area but figures only reported for intervention area. No P values reported. | |
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n Control city had higher injury rates and educational level than intervention city at baseline | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Zhang 2003.
| Methods | CBA (C) Allocation at level of counties | |
| Participants | Children aged 0‐4 years from 12 townships from 6 counties; 6 intervention and 6 control townships | |
| Interventions | I = health education comprising booklet containing methods of preventing suffocation and drowning, education by paediatricians to prevent suffocation and teaching sessions on vaccination day C = usual care | |
| Outcomes | Outcomes measured over 12 months: Mortality from suffocation I = 1/1414, C = 4/1447, OR 0.26 (0.03 to 2.30) Parents not swaddling babies ‐ no figures or P values reported Mortality from drowning I = 3/8293 C = 5/7653, P > 0.05, OR 0.55 (0.13 to 2.32) Use of fencing round pools ‐ No figures or P values reported |
|
| Notes | Blinding ‐ n Outcomes 80% ‐ n Balance ‐ n Intervention areas had higher baseline injury rates than control areas | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study |
Zhao 2005.
| Methods | RCT | |
| Participants | Children aged 7‐13 years attending 4 primary schools | |
| Interventions | I = safety education provided to parents and children C = usual care |
|
| Outcomes | Outcomes measured at 1 and 2 years: Self reported injuries (unclear if children reported multiple injuries) Self reported all injuries combined 1 year after intervention I=262/3172 C=234/2699; not significant (p value not given) Self reported all injuries combined 2 years after intervention I=211/3226 C=229/2654, χ2 =9.26, p<0.01 Self reported falls 1 year after intervention I=90/3172 C=67/2699; not significant (p value not given) Self reported falls 2 years after intervention I=64/3226 C=75/2654, p<0.05 Self reported scalds/burns 1 year after intervention I=28/3172 C=25/2699; not significant (p value not given) Self reported scalds/burns 2 years after intervention I=10/3226 C=18/2654, p<0.05 Self reported poisoning 1 year after intervention I=6/3172 C=8/2669; not significant (p value not given) Self reported poisoning 2 years after intervention I=4/3226 C=11/2654, p<0.05 Self reported electrical injury 1 year after intervention I=11/3172 C=10/2699; not significant (p value not given) Self reported electrical injury 2 years after intervention I=2/3226 C=6/2654; not significant (p value not given) Self reported inhalation injury 1 year after intervention I=10/3172 C=9/2699; not significant (p value not given) Self reported inhalation injury 2 years after intervention I=8/3226 C=5/2654; not significant (p value not given) Self reported cuts 1 year after intervention I=12/3172 C=11/2699; not significant (p value not given) Self reported cuts 2 years after intervention I=20/3226 C=9/2654; not significant (p value not given) Self reported other injuries 1 year after intervention I=1/3172 C=6/2699; not significant (p value not given) Self reported other injuries 2 years after intervention I=5/3226 C=6/2654; not significant (p value not given) |
|
| Notes | Blinding ‐ u Outcomes 80% ‐ y Balance ‐ n/a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
(C) = clustered allocation Numerators and denominators only presented for outcomes not included in meta analyses. Blinding: y = yes, n = no, u = unclear Outcomes measured on 80% (Outcomes 80%) of participants in each arm: y = yes, n = no, u = unclear Treatment arms balanced for confounding (Balance): y = yes, n = no, u = unclear, n/a = not applicable
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdelilah 1991 | Does not report study design of interest |
| Adesso 1974 | Does not report outcome of interest |
| Adler‐Grinberg 1985 | Does not report outcome of interest |
| Alaii 2003 | Does not report outcome of interest |
| Alpert 1966 | Does not report study design of interest |
| Altundag 2007 | Does not report study design of interest |
| Anonymous 1994 | Does not report study design of interest |
| Armstrong 2000 | Does not report intervention of interest |
| Aronson 1980 | Does not report study design of interest |
| Asher 1995 | Does not report outcome of interest |
| Atkins 2004 | Does not report outcome of interest |
| Bablouzian 1997 | Does not report study design of interest |
| Barnes‐Boyd 1995 | Does not report study design of interest |
| Barone 1986 | Does not report study design of interest |
| Bass 1985 | Does not report study design of interest |
| Baudier 1996 | Does not report study design of interest |
| Beirens 2008 | Does not report study design of interest |
| Belanger‐Bonneau 2002 | Does not report study design of interest |
| Bernard‐Bonnin 2003 | Does not report study design of interest |
| Bjerre 1997 | Does not report participants of interest |
| Bjerre 1998a | Does not report participants of interest |
| Bjerre 1998b | Does not report participants of interest |
| Bjerre 2000 | Does not report participants of interest |
| Bouter 1989 | Trial did not take place |
| Braden 1979 | Does not report outcome of interest |
| Cagle 2006 | Does not report study design of interest |
| Cardenas 1993 | Does not report outcome of interest |
| Carmel 1991 | Does not report outcome of interest |
| Chapman 2000 | Does not report outcome of interest |
| Charney 1983 | Does not report intervention of interest |
| Chen 2003 | Does not report study design of interest |
| Chevallier 1999 | Does not report study design of interest |
| Chung 2004 | Does not report outcome of interest |
| Cooper 1988 | Does not report study design of interest |
| CPSC (USA) 2004 | Does not report study design of interest |
| Davidson 1994 | Does not report outcome of interest |
| Day 2001 | Does not report study design of interest |
| Dershewitz 1984 | Does not report study design of interest |
| Dickson 1964 | Does not report study design of interest |
| DiGuiseppi 1999 | Does not report study design of interest |
| DiLillo 2001 | Does not report outcome of interest |
| Duckart 1998 | Does not report study design of interest |
| Duff 2002 | Does not report study design of interest |
| Dugdill 1991 | Does not report study design of interest |
| Duggan 1999 | Does not report intervention of interest |
| Duncan 1996 | Does not report outcome of interest |
| Duperrex 1999 | Does not report study design of interest |
| Eaton‐Jones 2000 | Does not report study design of interest |
| Eckelt 1985 | Does not report study design of interest |
| Ekman 1996 | Does not report study design of interest |
| Facchin 2004 | Does not report study design of interest |
| Fallat 1993 | Does not report study design of interest |
| Farmakakis 2004 | Does not report study design of interest |
| Fergusson 2005 | Does not report outcome of interest |
| Fisher 1985 | Does not report study design of interest |
| Frank 1992 | Does not report outcome of interest |
| Frankenfield 1991 | Does not report study design of interest |
| Frederick 2000 | Does not report outcome of interest |
| Gaffney 1996b | Does not report outcome of interest |
| Gallagher 1984 | Does not report study design of interest |
| Gallagher 1985 | Does not report study design of interest |
| Gatheridge 2004 | Does not report outcome of interest |
| Geddis 1989 | Does not report study design of interest |
| Gielen 1996 | Does not report outcome of interest |
| Gielen 2001 | Does not report participants of interest |
| Ginnelly 2005 | Does not report study design of interest |
| Glotzer 1997 | Does not report study design of interest |
| Grant 1992 | Does not report outcome of interest |
| Grant 2004 | Does not report study design of interest |
| Gray 1979 | Does not report intervention of interest |
| Gresham 2001 | Does not report outcome of interest |
| Gross 1990 | Does not report intervention of interest |
| Grossman 2000 | Does not report outcome of interest |
| Guldvog 1993 | Trial did not take place |
| Gutelius 1977 | Does not report intervention of interest |
| Guyer 2000 | Does not report intervention of interest |
| Hall 1985 | Does not report study design of interest |
| Hall 1994 | Does not report study design of interest |
| Hardy 1989 | Does not report intervention of interest |
| Hardy 1996 | Does not report outcome of interest |
| Hardy 2002 | Does not report outcome of interest |
| Harre 1998a | Does not report study design of interest |
| Harre 1998b | Does not report study design of interest |
| Harre 2000 | Does not report study design of interest |
| Hemmo‐Lotem 2005a | Does not report study design of interest |
| Hemmo‐Lotem 2005b | Does not report study design of interest |
| Himle 2004 | Does not report outcome of interest |
| HIPRC 2004 | Does not report study design of interest |
| Huxley 1993 | Does not report intervention of interest |
| Jackson 1980 | Does not report study design of interest |
| Jackson 1983 | Does not report study design of interest |
| Johnson 1993 | Does not report intervention of interest |
| Johnson 2000 | Does not report intervention of interest |
| Johnston 2002 | Does not report outcome of interest |
| Jones 2001 | Does not report study design of interest |
| Jordan 1993 | Does not report study design of interest |
| Jordan 2003 | Does not report intervention of interest |
| Kaplan 1999 | Does not report study design of interest |
| Katcher 1987 | Does not report study design of interest |
| Kendrick 2009 | Does not report study design of interest |
| Ketvertis 2003 | Does not report study design of interest |
| King 1999 | Does not report study design of interest |
| Kitzman 1997 | Does not report intervention of interest |
| Klassen 1995 | Does not report study design of interest |
| Koniak‐Griffin 2003 | Does not report intervention of interest |
| Korn 2009 | Does not report study design of interest |
| Kravitz 1973 | Does not report study design of interest |
| Krenzelok 1981 | Does not report study design of interest |
| Kuhn 1994 | Does not report study design of interest |
| Lagerberg 2000 | Does not report study design of interest |
| Lamb 2006 | Does not report outcome of interest |
| Lane 1971 | Does not report participants of interest |
| Lanphear 1999 | Does not report intervention of interest |
| Larcher 1987 | Does not report study design of interest |
| Larson 1980 | Does not report intervention of interest |
| Lealman 1983 | Does not report study design of interest |
| Lechman 1991 | Does not report outcome of interest |
| Leduc 1999 | Does not report study design of interest |
| Lee 2002 | Could not obtain reference |
| Lenton | Does not report study design of interest |
| Lenton 2000 | Trial did not take place |
| Liller 1998 | Does not report study design of interest |
| Liller 2003 | Does not report outcome of interest |
| Linares 1979 | Does not report study design of interest |
| Lindqvist 1998b | Does not report study design of interest |
| Loescher 1995 | Does not report outcome of interest |
| Lowe 1999 | Does not report outcome of interest |
| Luria 2000 | Does not report outcome of interest |
| Mackenzie 2004 | Does not report study design of interest |
| Malouin 2003 | Does not report outcome of interest |
| Margolis 2001 | Does not report study design of interest |
| Marion 2004 | Does not report outcome of interest |
| McConnell 1996a | Does not report study design of interest |
| McConnell 1996b | Does not report outcome of interest |
| McWhirter 2000 | Does not report outcome of interest |
| Melhuish 2008 | Does not report outcome of interest |
| MET 1986 | Does not report outcome of interest |
| Milliner 1980 | Does not report study design of interest |
| Milne 1999 | Does not report outcome of interest |
| Milne 2000 | Does not report outcome of interest |
| Milne 2002 | Does not report outcome of interest |
| Minchom 1984 | Does not report study design of interest |
| Minkovitz 2001 | Does not report intervention of interest |
| Minkovitz 2003 | Does not report intervention of interest |
| Mondozzi 2001 | Does not report outcome of interest |
| Moore 2004 | Does not report study design of interest |
| Mori 1986 | Does not report outcome of interest |
| Morrison 1988 | Does not report study design of interest |
| Morrongiello 1998 | Does not report outcome of interest |
| Naidoo 1984 | Could not obtain reference |
| Nicholson 2002 | Does not report study design of interest |
| Nossar 2001 | Does not report study design of interest |
| Novick 1997 | Does not report outcome of interest |
| O'Connor 1982 | Does not report study design of interest |
| O'Connor 1990 | Does not report outcome of interest |
| O'Donnell 1996 | Does not report study design of interest |
| Oakley 1998 | Does not report intervention of interest |
| Olds 1986 | Does not report intervention of interest |
| Olds 1999 | Does not report intervention of interest |
| Olds 2002 | Does not report study design of interest |
| Palmisano 1981 | Does not report study design of interest |
| Parcel 1983 | Does not report study design of interest |
| Paulson 1981 | Does not report study design of interest |
| Pena 1994 | Does not report outcome of interest |
| Peterson 1984a | Does not report outcome of interest |
| Peterson 1984b | Does not report outcome of interest |
| Petridou 1994 | Does not report study design of interest |
| Petridou 1995 | Does not report study design of interest |
| Petridou 2002 | Does not report study design of interest |
| Phillips 1980 | Does not report study design of interest |
| Phillips 1986 | Does not report study design of interest |
| Pocknall 1993 | Does not report study design of interest |
| Polivka 1999 | Does not report study design of interest |
| Potts 1998 | Does not report study design of interest |
| Powell 2000 | Does not report study design of interest |
| Quan 1990 | Does not report outcome of interest |
| Rahman 2002 | Could not obtain reference |
| Reichelderfer 1976 | Does not report study design of interest |
| Rhoads 1999 | Does not report intervention of interest |
| Rutstein 1977 | Does not report study design of interest |
| Sadan 1995 | Does not report study design of interest |
| Sahlin 1990 | Does not report study design of interest |
| San Agustin 1973 | Does not report study design of interest |
| Schnell 1993 | Does not report study design of interest |
| Schwebel 2002 | Does not report study design of interest |
| Sell 1977 | Does not report study design of interest |
| Sherman 1980 | Does not report study design of interest |
| Sibert 1977 | Does not report study design of interest |
| Sibert 1999 | Does not report study design of interest |
| Sibert 2002 | Trial did not take place |
| Smith 1984 | Does not report outcome of interest |
| Smith 2002 | Does not report study design of interest |
| Smith 2006 | Does not report outcome of interest |
| Smithson 1998 | Does not report study design of interest |
| Smithson 2000 | Does not report study design of interest |
| Solis 1991 | Does not report study design of interest |
| Sorensen 1976 | Does not report study design of interest |
| Spallek 2004a | Does not report study design of interest |
| Spallek 2004b | Does not report study design of interest |
| Speigel 1995 | Does not report study design of interest |
| Spiller 2004 | Does not report outcome of interest |
| St Pierre 1999 | Does not report intervention of interest |
| Stanley 1979 | Does not report study design of interest |
| Stennies 1999 | Does not report outcome of interest |
| Stephen 1993 | Does not report study design of interest |
| Stevens 2002 | Does not report outcome of interest |
| Sullivan 1990 | Does not report study design of interest |
| Sundelin 1996 | Does not report outcome of interest |
| Svanstrom 1996 | Does not report study design of interest |
| Swaine 2000 | Does not report study design of interest |
| Taha 1999 | Does not report study design of interest |
| Temple 1978 | Does not report study design of interest |
| Tenn 1996 | Does not report outcome of interest |
| Terzidis 2007 | Does not report study design of interest |
| Thompson 1998 | Does not report study design of interest |
| Thomson 1999 | Does not report intervention of interest |
| Thuen 1994 | Does not report study design of interest |
| Timpka 1999 | Does not report outcome of interest |
| Towner 1996 | Does not report outcome of interest |
| Towner 1998 | Does not report outcome of interest |
| Velsog 1996 | Does not report outcome of interest |
| Vernberg 1984 | Does not report outcome of interest |
| Vogel 1968 | Does not report outcome of interest |
| Webne 1989 | Does not report study design of interest |
| Wester 1985 | Does not report study design of interest |
| Whitfield 2000 | Does not report study design of interest |
| Whitt 1982 | Does not report outcome of interest |
| Wiggins 2004 | Does not report intervention of interest |
| Wortel 1991 | Does not report study design of interest |
| Wurtele 1989 | Does not report outcome of interest |
| Young 2000 | Does not report outcome of interest |
| Ytterstad 2000 | Does not report study design of interest |
| Zwi 2004 | Does not report study design of interest |
Characteristics of ongoing studies [ordered by study ID]
Cusimano (Canada).
| Trial name or title | The long term persistence of the "Think First for Kids" injury prevention programme at six and eighteen months |
| Methods | |
| Participants | Elementary school children |
| Interventions | I = 8 week implementation of "Think First for Kids" programme C = no "Think First for Kids" programme |
| Outcomes | Reduction in risky behaviour |
| Starting date | 2002 |
| Contact information | cusimanom@smh.toronto.on.ca |
| Notes |
Grossman (USA).
| Trial name or title | Raise the Alarms (A trial of smoke detector types) |
| Methods | |
| Participants | 784 owner occupied dwellings in King County |
| Interventions | I1 = installation of ionisation smoke detector I2 = installation of photoelectric smoke detector |
| Outcomes | Functional smoke alarm at 9 and 15 months follow‐up |
| Starting date | not reported |
| Contact information | bmueller@fhcrc.org |
| Notes |
Contributions of authors
DK had the idea for the review, drafted the protocol and the funding application, contributed to study selection, data extraction, developing the statistical models for assessing the effect of the covariates and the analyses, and drafted the final report. CC contributed to study selection, developing the statistical models for assessing the effect of the covariates and to drafting the protocol, the funding application and the final report. CM contributed to study selection, quality assessment and drafting the protocol, the funding application and the final report. SS contributed to the searches, quality assessment and drafting the protocol and the final report. AJS developed the statistical models for assessing the effect of the covariates and contributed to drafting the protocol, the funding application and the final report. MW contributed to study selection and drafting the protocol, the funding application and the final report. AM‐J (nee AW) contributed to study selection, quality assessment, the analyses and drafting the protocol, the funding application and the final report. BY contributed to the analysis and drafting the final report. PW and NI contributed to study selection, data extraction, quality assessment and drafting of the final report. NJC contributed to the funding application, drafting the protocol, the analysis and drafting the final report. FAA and SJH contributed to drafting the protocol, the analysis and drafting of the final report.
Sources of support
Internal sources
University of Nottingham, UK.
University of Leicester, UK.
External sources
Department of Health, UK.
-
National Institute for Health Research, UK.
This study was funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP‐PG‐0407‐10231).The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Declarations of interest
Denise Kendrick, Carol Coupland, Michael Watson, Caroline Mulvaney and Amanda Mason‐Jones are authors of some of the studies included in this review.
Edited (no change to conclusions)
References
References to studies included in this review
Adler 1994 {published data only}
- Adler R, Nunn R, Northam E, Lebnan V, Ross R. Secondary prevention of childhood firesetting. Journal of the American Academy of Child and Adolescent Psychiatry 1994;33(8):1194‐202. [DOI] [PubMed] [Google Scholar]
Babul 2007 {published data only (unpublished sought but not used)}
- Babul S, Olsen L, Janssen P, McIntee P, Raina P. A randomized trial to assess the effectiveness of an infant home safety programme. International Journal of Injury Control & Safety Promotion 2007;14(2):109‐17. [DOI] [PubMed] [Google Scholar]
Barone 1988 {published data only}
- Barone VJ. An analysis of well‐child parenting classes: the extent of parenting compliance with health‐care recommendations to decrease potential injury of their toddlers. University of Kansas 1988.
Baudier 1988 {published data only}
- Baudier F, Marchais M, Ferry B, Bouderont D, Pinochet C, Blum D. The cooperative program for the prevention of domestic accidents in children in the department of the Doubs.II Training aspects and evaluations [French]. Archives Francaises de Pediatrie 1988;45(7):499‐503. [PubMed] [Google Scholar]
Bentzen 1997 {published data only}
- Bentzen I. Does intervention prevent injuries in children? An evaluation of the "Safety for Active Children" programme in Odense, Denmark 1989‐1993. University of Tromso 1997.
Blake 1993 {published data only}
- Blake KD, Griffioen A, Taylor BW. Impact of a child accident prevention video on parents of preschool children. 2nd World Conference on Injury Control. Atlanta, USA, 1993.
Bulzachelli 2009 {published and unpublished data}
- Bulzachelli MT, Gielen AC, Shields WC, McDonald EM, Frattaroli S. Parental safety‐related knowledge and practices associated with visiting a mobile safety center in a low‐income urban population. Family and Community Health 2009;32(2):147‐58. [DOI] [PubMed] [Google Scholar]
Campbell 2001 {published data only}
- Campbell NR, Ayala GX, Litrownick AJ, Slyman DJ, Zavala F, Elder JP. Evaluation of a first aid and home safety program for Hispanic migrant adolescents. American Journal of Preventive Medicine 2001;20(4):258‐65. [DOI] [PubMed] [Google Scholar]
Carman 2006 {published data only}
- Carman J, Friedman E, Lamb D, Lennon K. Evaluating the impact of a child injury prevention project. Community Practitioner 2006;79(6):188‐92. [PubMed] [Google Scholar]
Chan 2004 {published data only}
- Chan CC. Promoting a safer household environment: a volunteer based home visit program. 7th World Conference on Injury prevention and Safety promotion. Vienna, Austria, 2004.
Clamp 1998 {published and unpublished data}
- Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ 1998;316(7144):1576‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coggan 2000 {published data only}
- Coggan C, Patterson P, Brewin M, Hooper R, Robinson E. Evaluation of Waitekere Community Injury Prevention Project. Injury Prevention 2000;6(1):130‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Colver 1982 {published data only}
- Colver A, Hutchinson P, Judson E. Promoting children's home safety. BMJ 1982;285:1177‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 1987 {published data only}
- Davis JW. Get fired up: a model for developing inschool Four‐H programs (safety). Clemson University 1987.
Dawson 1989 {published and unpublished data}
- Dawson P, Doorninck WJ, Robinson JL. Effects of home‐based informal social support on child health. Journal of Developmental Behavioral Pediatrics 1989;10(2):63‐7. [PubMed] [Google Scholar]
Dershewitz 1977 {published data only}
- Dershewitz RA. Will mothers use free household safety devices?. American Journal of Diseases of Children 1979;133(1):61‐4. [DOI] [PubMed] [Google Scholar]
- Dershewitz RA, Williamson JW. Prevention of childhood household injuries: a controlled clinical trial. American Journal of Public Health 1977;67(12):1148‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiGuiseppi 2002 {published and unpublished data}
- DiGuiseppi C, Roberts I, Wade A, Sculpher M, Edwards P, Godward C, et al. Incidence of fires and related injuries after giving out free smoke alarms: Cluster randomised controlled trial. BMJ 2002;325(7371):995‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Emond 2002 {published data only}
- Emond A, Pollock J, Deave T, Bonnell S, Peters TJ, Harvey I. An evaluation of the first parent health visitor scheme. Archives of Disease in Childhood 2002;86(1):150‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fergusson 1982 {published data only}
- Fergusson DM, Horwood LJ, Beautrais AL, Shannon FT. A controlled field trial of a poisoning prevention method. Pediatrics 1982;69(5):515‐20. [PubMed] [Google Scholar]
Franklin 2002 {published data only}
- Franklin GA, Pucci PS. Decreased juvenile arson and firesetting recidivism after implementation of a multidisciplinary prevention program. Journal of Trauma, Injury Infection and Critical Care 2002;53(2):260‐6. [DOI] [PubMed] [Google Scholar]
Gaffney 1996a {published data only}
- Gaffney D. Preventing hot water scalds among young children in New South Wales. 3rd International Conference on Injury Prevention and Control. Melbourne, Australia, 1996.
Garcia 1996 {published data only}
- Garcia VF. Safety Fairs: evaluation of a school‐based injury prevention program. 3rd International Conference on Injury Prevention and Control. Melbourne, Australia, 1996.
Georgieff 2004 {unpublished data only}
- Georgieff K, Maw C. The Wakefield District Burns and Scalds Prevention Project: Health Development Unit. Wakefield Metropolitan District Council 2004.
Gielen 2002 {published data only}
- Gielen AC, McDonald EM, Wilson MEH, Hwang WT, Serwint JR, Andrews JS, et al. Effects of improved access to safety counseling products and home visits on parents' safety practices: results of a randomized trial. Archives of Pediatrics and Adolescent Medicine 2002;156(1):33‐40. [DOI] [PubMed] [Google Scholar]
Gielen 2007 {published and unpublished data}
- Gielen AC, McKenzie LB, McDonald EM, Shields WC, Wang M‐C, Cheng Y‐J, et al. Using a computer kiosk to promote child safety: results of a randomized controlled trial in an urban pediatric emergency department. Pediatrics 2007;120(2):330‐9. [DOI] [PubMed] [Google Scholar]
Girasek 2010 {unpublished data only}
- Girasek, DC. Valid measurement of isolation pool fencing: A methodologic challenge. Injury Prevention 2010;16, Suppl 1:A249. [Google Scholar]
Gittelman 2007 {published data only}
- Gittelman MA, Pomerantz WJ, McNealy T. Reducing injury rates using a community based approach. The Journal of Trauma, Injury, Infection and Critical Care 2007;63(3):S45‐9. [DOI] [PubMed] [Google Scholar]
Guyer 1989 {published data only}
- Guyer B, Gallacher SS, Chang B, Azzara CV, Cupples LA, Colton T. Prevention of childhood injuries: evaluation of the statewide childhood injury prevention program (SCIPP). American Journal of Public Health 1989;79(1):1521‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harvey 2004 {published data only}
- Harvey PA, Aitken M, Ryan GW, Demeter LA, Givens J, Sundararamen R, Goulette S. Strategies to increase smoke alarm use in high‐risk households. Journal of Community Health 2004;29(5):375‐85. [DOI] [PubMed] [Google Scholar]
Hendrickson 2002 {published and unpublished data}
- Hendrickson S. Reaching an underserved population with a randomly assigned home safety intervention. Injury Prevention 2005;11(5):313‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hwang 2006 {published data only}
- Hwang V, Duchossois GP, Garcia‐Espana JF, Durbin DR. Impact of a community based fire prevention intervention on fire safety knowledge and behaviour in elementary school children. Injury Prevention 2006;12:344‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jenkins 1996 {published data only}
- Jenkins HM, Blank V, Miller K, Turner J, Stanwick RS. A randomized single‐blind evaluation of a discharge teaching book for pediatric patients with burns. Journal of Burn Care & Rehabilitation 1996;17(1):49‐61. [PubMed] [Google Scholar]
Johnston 2000 {published data only}
- Johnston BD, Britt J, D'Ambrosio L, Mueller BA, Rivara FP. A preschool program for safety and injury prevention delivered by home visitors. Injury Prevention 2000;6(11):305‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Katcher 1989 {published data only}
- Katcher ML, Landry GL, Shapiro MM. Liquid‐crystal thermometer use in pediatric office counseling about tap water burn prevention. Pediatrics 1989;83(5):766‐71. [PubMed] [Google Scholar]
Kelly 1987 {published data only}
- Kelly B, Sein C, McCarthy PL. Safety education in a pediatric primary care setting. Pediatrics 1987;79(5):818‐24. [PubMed] [Google Scholar]
Kelly 2003 {published data only}
- Kelly NR, Huffman LC, Mendoza FS, Robinson TN. Effects of a videotape to increase use of poison control centres by low‐income and Spanish‐speaking families: a randomized controlled trial. Pediatrics 2003;111(1):21‐6. [DOI] [PubMed] [Google Scholar]
Kendrick 1999 {published and unpublished data}
- Kendrick D, Marsh P, Fielding K, Miller P. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318(7189):980‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kendrick 2005 {published and unpublished data}
- Kendrick D, Illingworth R, Woods A, Watts K, Collier J, Dewey M, et al. Promoting child safety in primary care: a cluster randomised controlled trial to reduce baby walker use. British Journal of General Practice 2005;55(517):582‐8. [PMC free article] [PubMed] [Google Scholar]
Kendrick 2007 {published and unpublished data}
- Kendrick D, Groom L, Stewart J, Watson M, Mulvaney C, Casterton R. "Risk Watch": cluster randomised controlled trial evaluating an injury prevention program. Injury Prevention 2007;13:93‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kendrick 2010 {published and unpublished data}
- Kendrick D, Stewart J, Smith S, Coupland C, Hopkins N, Groom L, et al. Randomised controlled trial of thermostatic mixer valves in reducing bath hot tap water temperature in families with young children in social housing. Archives of Disease in Childhood 2011;96:232‐9. [DOI] [PubMed] [Google Scholar]
King 2001 {published data only}
- King WJ, Klassen TP, LeBlanc J, Bernard‐Bonnin A, Robitaille Y, Coyle D, et al. The effectiveness of a home visit to prevent childhood injury. Pediatrics 2001;108(2):382‐8. [DOI] [PubMed] [Google Scholar]
Kolko 2001 {published and unpublished data}
- Kolko DJ. Efficacy of cognitive‐behavioural treatment and fire safety education for children who set fires: initial and follow up outcomes. Journal of Child Psychology and Psychiatry and Allied Disciplines 2001;42(3):359‐69. [PubMed] [Google Scholar]
Krug 1994 {published data only}
- Krug A, Ellis JB, Hay IT, Mokgabudi NF, Robertson J. The impact of child‐resistant containers on the incidence of paraffin (kerosene) ingestion in children. South African Medical Journal 1994;84(11):730‐4. [PubMed] [Google Scholar]
Lacoutre 1978 {published data only}
- Lacoutre P, Minisci M, Gouveia MS, Lovejoy FH. Evaluation of a community‐based poison education program. Clinical Toxicology 1978;13(5):623‐9. [DOI] [PubMed] [Google Scholar]
LeBailly 1990 {published data only}
- LeBailly SA, Freel K, Hicks‐Bartlett S, Kirschenman J, Ritts‐Benally K, Sasicki J. The children's safety research project. Elk Grove Village, Illinois. American Academy of Pediatrics 1990. [Google Scholar]
Lindqvist 1998a {published data only}
- Lindqvist K, Timpka T, Schlep L, Risto O. Evaluation of a child safety program based on the WHO safe community model. Injury Prevention 2002;8(1):23‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Llewellyn 2003 {published data only}
- Llewellyn G, McConnell D, Honey A, Mayes R, Russo D. Promoting health and home safety for children of parents with intellectual disability: a randomized controlled trial. Research in Developmental Disabilities 2003;24(6):405‐31. [DOI] [PubMed] [Google Scholar]
Mackay 2002 {published data only}
- MacKay AM, Rothman KJ. The incidence and severity of burn injuries following Project Burn Prevention. American Journal of Public Health 1982;72(3):248‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mallonee 1996 {published data only}
- Mallonee S. Evaluating Injury prevention Programs: The Oklahoma City Smoke Alarm Project. The Future of Children 2000;10(1):164‐74. [PubMed] [Google Scholar]
Matthews 1988 {published data only}
- Matthews JR. An analysis of dangerous behaviour in toddlers. University of Kansas 1988.
Mayer 1998 {published data only}
- Mayer JP, Anderson C, Gabriel K, Soweid R. A randomized trial of an intervention to prevent lawnmower injuries in children. Patient Education and Counseling 1998;34(3):239‐46. [DOI] [PubMed] [Google Scholar]
McDonald 2005 {published and unpublished data}
- McDonald EM, Solomon B, Shields W, Serwint JR, Jacobsen H, Weaver NL, et al. Evaluation of a kiosk‐based tailoring to promote household safety behaviors in an urban pediatric primary care practice. Patient Education and Counseling 2005;58(2):168‐81. [DOI] [PubMed] [Google Scholar]
McLoughlin 1982 {published data only}
- McLoughlin E, Vince CJ, Lee AM, Crawford JD. Project burn prevention: outcomes and implications. American Journal of Public Health 1982;72(3):241‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 1982 {published data only}
- Miller RE, Reisinger KS, Blatter MM, Wucher F. Pediatric counseling and subsequent use of smoke detectors. American Journal of Public Health 1982;72(4):392‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mock 2003 {published data only}
- Mock C, Arreola‐Risa C, Trevino‐Perez R, Almazan‐Saavedra V, Zozaya‐Paz JE, Gonzalez‐Solis R, et al. Injury prevention counselling to improve safety practices by parents in Mexico. Bulletin of the World Health Organization 2003;81(8):591‐8. [PMC free article] [PubMed] [Google Scholar]
Moller 1996 {published data only}
- Moller B. Community based injury prevention ‐ success or failure? Results from the 5‐community‐project in Denmark. 3rd International Conference on Injury Prevention and Control. Melbourne, Australia, 1996.
Mueller 2008 {published data only}
- Mueller BA, Sidman EA, Alter H, Perkins R, Grossman DC. Randomised controlled trial of ionization and photoelectric smoke alarm functionality. Injury Prevention 2008;14:80‐6. [DOI] [PubMed] [Google Scholar]
Nansel 2002 {published and unpublished data}
- Nansel TR, Weaver N, Donlin M, Jacobsen H, Kreuter MW, Simons‐Morton BG. Baby, Be Safe: the effect of tailored communications for pediatric injury prevention provided in a primary care setting. Patient Education and Counseling 2002;46(1):175‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nansel 2008 {published and unpublished data}
- Nansel TR, Weaver NL, Jacobsen HA, Glasheen C, Kreuter MW. Preventing unintentional pediatric injuries: a tailored intervention for parents and providers. Health Education Research 2008;23(4):656‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Odendaal 2008 {published data only}
- Odendaal W, Niekerk A, Jordaan E, Seedat M. The impact of a home visitation programme on household hazards associated with unintentional childhood injuries: A randomised controlled trial. Accident Analysis and Prevention 2009;41:183‐90. [DOI] [PubMed] [Google Scholar]
Ohn 2005 {unpublished data only}
- Ohn TT. Sure Start and Safety: controlled intervention study of children's safety scheme in Sheffield. University of Sheffield 2005.
Olds 1994 {published data only}
- Olds DL, Henderson CR, Jr, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93(1):89‐98. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Kitzman H. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78(1):65‐78. [PubMed] [Google Scholar]
Ozanne‐Smith 2002 {published data only}
- Ozanne‐Smith J, Day LM, Stathakis V, Sherrard J. Controlled evaluation of a community based injury prevention program in Australia. Injury Prevention 2002;8(1):18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paul 1994 {published data only}
- Paul CL, Redman S, Evans D. Preventing accidental injury to young children in the home using volunteers. Health Promotion International 1994;9(4):241‐9. [Google Scholar]
Petridou 1997 {published and unpublished data}
- Petridou E, Tolma E, Dessypris N, Trichopoulos D. A controlled evaluation of a community injury prevention project in two Greek Islands. International Journal of Epidemiology 1997;26(1):173‐9. [DOI] [PubMed] [Google Scholar]
Phelan 2010 {published and unpublished data}
- Phelan KJ, Khoury J, Xu Y, Liddy S, Hornung R, Lanphear BP. A randomised controlled trial of home injury hazard reduction: the HOME injury study. Injury Prevention 2010;16 Suppl:A171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pless 2007 {published data only}
- Pless IB, Hagel B, Patel H, Leduc D, Magdalinos H. Preventing product related injuries. A randomized controlled trial of poster alerts. Canadian Journal of Public Health 2007;98(4):271‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ponce De Leon 2007 {published data only}
- Ponce De Leon A, Svanstrom L, Welander G, Schelp L, Santesson P, Ekman R. Differences in child injury hospitalizations in Sweden: The use of time‐trend analysis to compare various community injury prevention approaches. Scandinavian Journal of Public Health 2007;35:623‐30. [DOI] [PubMed] [Google Scholar]
Posner 2004 {published and unpublished data}
- Posner J, Hawkins L, Garcia‐Espana F, Durbin D. A randomized clinical trial of a home safety intervention based in an emergency department setting. Pediatrics 2004;113(6):1603‐8. [DOI] [PubMed] [Google Scholar]
Rey 1993 {published data only}
- Rey S, Courtois X, Zmirou D, Francois M, Oberle D, Navet J. Evaluation of a health educative program against childhood injuries. Pediatrie 1993;48(10):727‐33. [PubMed] [Google Scholar]
Rowland 2002 {published and unpublished data}
- Rowland D, DiGuiseppi C, Roberts I, Curtis K, Roberts H, Ginnelly L, et al. Prevalence of working smoke alarms in local authority inner city housing: randomised controlled trial. BMJ 2002;325:998‐1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sangvai 2007 {published and unpublished data}
- Sangvai S, Cipriani L, Colborn DK, Wald ER. Studying injury prevention: practices, problems and pitfalls in implementation. Clinical Pediatrics 2007;46(3):228‐35. [DOI] [PubMed] [Google Scholar]
Schelp 1987 {published data only}
- Schelp L. Community intervention and changes in accident pattern in a rural Swedish municipality. Health Promotion 1987;2(2):109‐25. [Google Scholar]
- Schelp L. The role of organisations in community participation ‐ prevention of accidental injuries in a rural Swedish municipality. Social Science and Medicine 1988;26(11):1087‐93. [DOI] [PubMed] [Google Scholar]
Scherz 1968 {published data only}
- Scherz RG. Childhood poisonings from medications: three prevention programs that worked. Military Medicine 1968;133(11):911‐3. [PubMed] [Google Scholar]
Schlesinger 1966 {published data only}
- Schlesinger ER, Dickson DG, Westaby JR, Lowen L, Logrillo VM, Maiwald AA. A controlled study of health education in accident prevention: the Rockland County Child Injury Project. Injury Prevention 1997;3(3):218‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwarz 1993 {published data only}
- Schwarz DF, Grisso JA, Miles C, Holmes JH, Sutton RL. An injury prevention programme in an urban African‐American Community. American Journal of Public Health 1993;83(5):675‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwebel 2009 {published and unpublished data}
- Schwebel DC, Swart D, Simpson J, Hobe P, Hui SK. An intervention to reduce kerosene‐related burns and poisonings in low‐income Soth African communities. Health Psychology 2009;28(4):493‐500. [DOI] [PubMed] [Google Scholar]
Shani 2003 {published data only}
- Shani E, Ayalon A, Abu Hammad I, Sikron F. What picture is worth a thousand words? A comparative evaluation of a burn prevention programme by type of medium in Israel. Health Promotion International 2003;18(4):361‐71. [DOI] [PubMed] [Google Scholar]
Shapiro 1987 {published data only}
- Shapiro MM, Katcher ML. Injury‐prevention education during postpartum hospitalization. American Journal of Diseases of Children 1987;141:382. [Google Scholar]
Steele 1985a {published data only}
- Steele P, Spyker DA. Poisonings. Pediatric Clinics of North America 1985;32(1):77‐86 ((a) 83‐4). [DOI] [PubMed] [Google Scholar]
Steele 1985b {published data only}
- Steele P, Spyker DA. Poisonings. Pediatric Clinics of North America 1985;32(1):77‐86 ((b) 82). [DOI] [PubMed] [Google Scholar]
Svanstrom 1995 {published data only}
- Svanstrom L, Ekman R, Schlep L, Lindstom A. The Lidkoping Accident Prevention Programme ‐ a community approach to preventing childhood injuries in Sweden. Injury Prevention 1995;1(3):169‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swart 2008 {published and unpublished data}
- Swart L, Niekerk A, Seedat M, Jordaan E. Paraprofessional home visitation program to prevent childhood unintentional injuries in low‐income communities: a cluster randomised controlled trial. Injury Prevention 2008;14:164‐9. [DOI] [PubMed] [Google Scholar]
Sznajder 2003 {published and unpublished data}
- Sznajder M, Leduc S, Janvrin MP, Bonnin MH, Aegerter P, Baudier F, et al. Home delivery of an injury prevention kit for children in four French cities: a controlled randomized trial. Injury Prevention 2003;9(1):261‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2004 {published and unpublished data}
- Tan NC, Lim NMLH, Gu K. Effectiveness of nurse counselling in discouraging the use of infant walkers. Asia‐Pacific Journal of Public Health 2004;16(2):104‐8. [DOI] [PubMed] [Google Scholar]
Thomas 1984 {published data only}
- Thomas KA, Hassanein RS, Christophersen ER. Evaluation of group well‐child care for improving burn prevention practices in the home. Pediatrics 1984;74(5):879‐82. [PubMed] [Google Scholar]
Vineis 1994 {published data only}
- Vineis P, Ronco G, Ciccone G, Gogliani F. Home injuries in children: a population‐based intervention trial. Epidemiology 1994;5(3):349‐51. [PubMed] [Google Scholar]
Waller 1993 {published data only}
- Waller AE, Clarke JA, Langley JD. An evaluation of a program to reduce home hot tap water temperatures. Australian Journal of Public Health 1993;17(2):116‐23. [PubMed] [Google Scholar]
Watson 2005 {published and unpublished data}
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson JL. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1988 {published data only}
- Williams GE. An analysis of parental education classes: an early start to injury prevention. University of Kansas 1988.
Wissow 1989 {published data only}
- Wissow L. Home injury hazards in the inner city. First World Conference on Accident and Injury Prevention. Stockholm, Sweden, 1989.
Woolf 1987 {published data only}
- Woolf A, Lewander W, Filippone G, Lovejoy FH. Prevention of childhood poisoning: efficacy of an educational program carried out in an emergency clinic. Pediatrics 1987;80(3):359‐63. [PubMed] [Google Scholar]
Woolf 1992 {published data only}
- Woolf AD, Saperstein A, Forjuoh S. Poisoning prevention knowledge and practices of parents after a childhood poisoning incident. Pediatrics 1992;90(6):867‐70. [PubMed] [Google Scholar]
Yang 2008 {published data only}
- Yang J, Peek‐Asa C, Jones MP, Nordstrom DL, Taylor C, Young TL, Zwerling C. Smoke alarms by type and battery life in rural households. A randomized controlled trial. American Journal of Preventive Medicine 2008;35(1):20‐4. [DOI] [PubMed] [Google Scholar]
Yorkston 2007 {published and unpublished data}
- Yorkston E, Turner C, Schuler PJ, McClure R. Quantifying the effect of a community‐based injury prevention program in Queensland using a generalized estimating equation approach. Injury Prevention 2007;13:191‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ytterstad 1998 {published and unpublished data}
- Ytterstad B, Sogaard AJ. The Harstad Injury Prevention Study: prevention of burns in small children by a community‐based intervention. Burns 1995;21(4):259‐66. [DOI] [PubMed] [Google Scholar]
Zhang 2003 {published data only}
- Zhang PB, Chen RH, Deng JY, Xu BR, Hu YF. Evaluation of the efficacy of health education interventions on unintentional suffocation and drowning to children aged 0‐4 years in China. [Chinese]. Zhonghua Er Ke Za Zhi 2003;41(7):497‐500. [PubMed] [Google Scholar]
Zhao 2005 {published data only}
- Zhao C‐H, Qui H‐S, Qui H‐K. Interventions to prevent accidental injuries in children between 7 and 13 years of age. Chinese Journal of Contemporary Pediatrics 2006;8(4):331‐3. [PubMed] [Google Scholar]
References to studies excluded from this review
Abdelilah 1991 {published data only}
- Abdelilah M, Mabe B. Prevention des accidents domestiques aupres des populations immigrees. In : Les accidents domestiques de l'enfant: un probleme majeur de sante publique, IDEF/CIE/Syros, Paris 1991:217‐25. [Google Scholar]
Adesso 1974 {published data only}
- Adesso NA. An evaluation of the Champaign‐Urbana Safety Town Program. http://www.mrw.interscience.wiley.com/cochrane/clcentral/articles/449/CN‐00241449/frame.html 1974. [Google Scholar]
Adler‐Grinberg 1985 {published data only}
- Adler‐Grinberg D, Lovato C, Nussenblatt H, Davis‐Poirier R. Evaluation of the NSPB elementary school teaching units on eye health and safety. Journal of the American Optometric Association 1985;56(11):882‐6. [PubMed] [Google Scholar]
Alaii 2003 {published data only}
- Alaii JA, Borne HW, Kachur SP, Mwenesi H, Vulule JM, Hawley WA, et al. Perceptions of bed nets and malaria prevention before an after a randomised controlled trial of permethrin‐treated bed nets in western Kenya. American Journal of Tropical Medicine and Hygiene 2003;68 Suppl 4:142‐8. [PubMed] [Google Scholar]
Alpert 1966 {published data only}
- Alpert JJ, Heagarty MC. Evaluation of a program for distribution of ipecac syrup for the emergency home management of poison ingestions. Journal of Pediatrics 1966;69(1):142‐6. [DOI] [PubMed] [Google Scholar]
Altundag 2007 {published data only}
- Altundag S, Ozturk MC. The Effects of Home Safety Education on Taking Precautions and Reducing the Frequency of Home Accidents. Turkish Journal of Trauma & Emergency Surgery ‐ Ulusal Travma Ve Acil Cerrahi Dergisi 2007;13(3):180‐5. [PubMed] [Google Scholar]
Anonymous 1994 {published data only}
- Anonymous. Proposed safety measures aimed at protecting children from iron poisoning. American Journal of Hospital Pharmacy 1994;51(23):2887. [PubMed] [Google Scholar]
Armstrong 2000 {published data only}
- Armstrong KL, Fraser JA, Dadds MR, Morris J. Promoting a secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. Journal of Paediatrics & Child Health 2000;36(6):555‐62. [DOI] [PubMed] [Google Scholar]
Aronson 1980 {published data only}
- Aronson SS, Aiken LS. Compliance of child care programs with health and safety standards: impact of program evaluation and advocate training. Pediatrics 1980;65(2):318‐25. [PubMed] [Google Scholar]
Asher 1995 {published data only}
- Asher KN, Rivara FP, Felix D, Vance L, Dunne R. Water safety training as a potential means of reducing risk of young children's drowning. Injury Prevention 1996;1(4):228‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atkins 2004 {published data only}
- Atkins S. Home visitation programme for childhood injury reduction in South Africa: injury and injury risk outcomes. 7th World Conference on Injury Prevention and Safety Promotion, Vienna, Austria 2004. [Google Scholar]
Bablouzian 1997 {published data only}
- Bablouzian L, Freedman ES, Wolski KE, Fried LE. Evaluation of a community based childhood injury prevention program. Injury Prevention 1997;3(1):14‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnes‐Boyd 1995 {published data only}
- Barnes‐Boyd C. Effects of sustained nurse/mother contact on infant outcomes among low‐income African‐American families. Public Health Nursing 1995;12(6):378‐85. [DOI] [PubMed] [Google Scholar]
Barone 1986 {published data only}
- Barone V, Greene B, Lutzker J. Home safety with families being treated for child abuse and neglect. Behaviour Modification 1986;10(1):93‐114. [DOI] [PubMed] [Google Scholar]
Bass 1985 {published data only}
- Bass JL, Mehta KA, Ostrovsky M, Halperin SF. Educating parents about injury prevention. Pediatric Clinics of North America 1985;32(1):233‐42. [DOI] [PubMed] [Google Scholar]
Baudier 1996 {published data only}
- Baudier F, Janvrin M. Preventing childhood home injuries in France: 12 years experience in national campaign and field work. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Beirens 2008 {published data only}
- Beirens TMJ, Brug J, Beeck EF, Dekker R, Hertog P, Raat H. Assessing psychosocial correlates of parental safety behaviour using Protection Motivation Theory: stair gate presence and use among parents of toddlers. Health Education Research 2008;23(4):723‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Belanger‐Bonneau 2002 {published data only}
- Belanger‐Bonneau M. Prevenons les Blessures chez nos enfants: guide a l'intention des intervenants ‐ evaluation du guide. 6th World Conference on Injury Prevention and Control, Montreal, Canada 2002. [Google Scholar]
Bernard‐Bonnin 2003 {published data only}
- Bernard‐Bonnin AC, Pless IB, Robitaille Y, LeBlanc J, King WJ, Tenenbein M, et al. Home injury patterns in children: a comparison by hospital sites. Paediatrics and Child Health 2003;8(7):433‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjerre 1997 {published data only}
- Bjerre B, Jonell A. The community safety approach in Falun, Sweden. What makes it work?. International Journal for Consumer and Product Safety 1997;5(3):139‐53. [Google Scholar]
Bjerre 1998a {published data only}
- Bjerre B. A community based injury prevention study in Falun, Sweden. Evaluation of the effects and considerations regarding the efficiency of the different parts of the injury prevention programme. 4th World Conference on Injury Prevention and Control, Amsterdam, Holland 1998. [Google Scholar]
Bjerre 1998b {published data only}
- Bjerre B, Sandberg BM. The effects of a community‐based injury prevention study in Falun, Sweden ‐ outpatient and hospital‐based injury records. International Journal for Consumer and Product Safety 1998;5(3):129‐38. [Google Scholar]
Bjerre 2000 {published data only}
- Bjerre B, Schlep L. The community safety approach in Falun, Sweden‐ is it possible to characterise the most effective prevention endeavours and how long‐lasting are the results?. Accident Analysis and Prevention 2000;32(3):461‐70. [DOI] [PubMed] [Google Scholar]
Bouter 1989 {published data only}
- Bouter L. The importance of planning health education for injury prevention. First World Conference on Accident and Injury Prevention, Stockholm, Sweden 1989. [Google Scholar]
Braden 1979 {published data only}
- Braden BT. Validation of a poison prevention program. American Journal of Public Health 1979;69(9):942‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cagle 2006 {published data only}
- Cagle KM, Davis JW, Dominic W, Gonzales W. Results of a focused scald‐prevention program. Journal of Burn Care & Research 2006;27(6):859‐63. [DOI] [PubMed] [Google Scholar]
Cardenas 1993 {published data only}
- Cardenas MP, Simons‐Morton BG. The effect of anticipatory Guidance on mothers' self‐efficacy and behavioural intentions to prevent burns caused by hot tap water. Patient Education and Counseling 1993;21(3):117‐23. [Google Scholar]
Carmel 1991 {published data only}
- Carmel S, Shani E, Rosenberg L. Evaluation of a burn prevention program in Israeli schools. Health Promotion International 1991;6(2):87‐92. [Google Scholar]
Chapman 2000 {published data only}
- Chapman S Cornwall J, Righetti J, Sung L. Preventing dog bites in children: randomised controlled trial of an educational intervention. BMJ 2000;320(7248):1512‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Charney 1983 {published data only}
- Charney E, Kessler B, Fargel M, Jackson D. Childhood Lead Poisoning: a controlled trial of the effect of dust‐control measures on blood lead levels. New England Journal of Medicine 1983;309(18):1089‐93. [DOI] [PubMed] [Google Scholar]
Chen 2003 {published data only}
- Chen LH, Gielen AC, McDonald EM. Validity of self reported home safety practices. Injury Prevention 2003;9(1):73‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chevallier 1999 {published data only}
- Chevallier B, Bruneau C, Leroux G, Sznajder M, Auvert B. Approche communautaire de la prevention des accidents de l‐enfant. Concept et application pratique; le programme de la ville de Boulogne‐Billancourt 1998‐2002. Annales de Pediatrie 1999;46(5):330‐6. [Google Scholar]
Chung 2004 {published data only}
- Chung ES, Jeong IS, Song MG. Development and effect analysis of web‐based instruction program to prevent elementary school students from safety accidents. Taehan Kanho Hakhoe Chi 2004;34(3):485‐94. [DOI] [PubMed] [Google Scholar]
Cooper 1988 {published data only}
- Cooper JM, Widness JA, O'Shea JS. Pilot evaluation of instructing parents of newborns about poison prevention programs. American Journal of Disease in Childhood 1988;142(6):627‐9. [DOI] [PubMed] [Google Scholar]
CPSC (USA) 2004 {published data only}
- US Consumer Product Safety Commission. Preventing child drownings. Consumer Product Safety Review 2004;9(1):1‐5. [Google Scholar]
Davidson 1994 {published data only}
- Davidson LL, Durkin MS, Kuhn L, O'Connor P, Barlow B, Heagarty MC, et al. The impact of the safe kids/healthy neighborhoods injury prevention program in Harlem, 1988 through 1991. American Journal of Public Health 1994;84(4):580‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Day 2001 {published data only}
- Day LM, Ozanne‐Smith J, Cassell E, Li L. Evaluation of the Latrobe Valley Better Health Injury prevention Program. Injury Prevention 2001;7(1):66‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dershewitz 1984 {published data only}
- Dershewitz RA, Paichel W. Effectiveness of a health education program in a lower socioeconomic population. Replication of an ipecac guidance study. Clinical Pediatrics 1984;23(12):686‐8. [DOI] [PubMed] [Google Scholar]
Dickson 1964 {published data only}
- Dickson DG, Schlesinger ER, Westaby JR, Lowen L. Medically attended injuries among young children: observations in a suburban area. American Journal of Disease in Childhood 1964;107(6):618‐23. [DOI] [PubMed] [Google Scholar]
DiGuiseppi 1999 {published data only}
- DiGuiseppi C, Slater S, Roberts I, Adams L, Sculpher M, Wade A, et al. The "lets get alarmed!" initiative: a smoke alarm giveaway programme. Injury Prevention 1999;5(3):177‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiLillo 2001 {published data only}
- DiLillo D, Tremblay G. Maternal and Child Reports of Behavioural Compensation in Response to safety equipment usage. Journal of Pediatric Psychology 2001;26(3):175‐84. [DOI] [PubMed] [Google Scholar]
Duckart 1998 {published data only}
- Duckart JP. An evaluation of the Baltimore Community Lead Education and Reduction Corps (CLEAR Corps) program. Evaluation Review 1998;22(3):373‐402. [DOI] [PubMed] [Google Scholar]
Duff 2002 {published data only}
- Duff S, Ryan M, Mullan C, O'Keefe B, Nicholson AJ. The use of local accident and emergency injury surveillance to monitor the impact of a lay safety community programme. Irish Medical Journal 2002;95(5):143‐5. [PubMed] [Google Scholar]
Dugdill 1991 {published data only}
- Dugdill L, Ashton J. Evaluation of the 'YUK' Accidental Poisoning Prevention Campaign in Liverpool. Dept of Public Health University of Liverpool 1991. [Google Scholar]
Duggan 1999 {published data only}
- Duggan AK, McFarlane EC, Windham AM, Rohde CA, Salkever DS, Fuddy L, et al. Evaluation of Hawaii's Health Start Program. Future of Children 1999;9(1):66‐90. [PubMed] [Google Scholar]
Duncan 1996 {published data only}
- Duncan T, Cross D, Davies M. Evaluation of a child safety demonstration house. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Duperrex 1999 {published data only}
- Duperrex O. Preventing injuries in children: cluster randomised controlled trial in primary care. Journal of Pediatrics 1999;135(5):648‐9. [PubMed] [Google Scholar]
Eaton‐Jones 2000 {published data only}
- Eaton‐Jones SE, Fields KB, Rasco T, Akintemi OK. Preventing Childhood Poisoning. An intervention in a family medicine residency program. North Carolina Medical Journal 2000;61(6):333‐5. [PubMed] [Google Scholar]
Eckelt 1985 {published data only}
- Eckelt K, Fannon M, Blades B, Munster AM. A successful burn prevention program in elementary schools. Journal of Burn Care and Rehabilitation 1985;6(6):509‐10. [DOI] [PubMed] [Google Scholar]
Ekman 1996 {published data only}
- Ekman R. Falkoping ‐ still a safe community?. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Facchin 2004 {published data only}
- Facchin P. Child safety promotion through parents' information: risk patterns, timing and efficacy. 7th World Conference on Injury Prevention and Safety Promotion, Vienna, Austria 2004. [Google Scholar]
Fallat 1993 {published data only}
- Fallat ME, Rengers SJ. The effect of safety education and safety devices on scald burn prevention. Journal of Trauma 1993;34:560‐3. [DOI] [PubMed] [Google Scholar]
Farmakakis 2004 {published data only}
- Farmakakis T, Alexe DM, Nicolaidou P, Dessypris N, Petridou E. Baby bouncer related injuries; an under‐appreciated risk. European Journal of Pediatrics 2004;163(1):42‐3. [DOI] [PubMed] [Google Scholar]
Fergusson 2005 {published data only}
- Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the Early Start program of home visitation. Pediatrics 2005;116(6):e803‐9. [DOI] [PubMed] [Google Scholar]
Fisher 1985 {published data only}
- Fisher L, Lawrence R, Nitzkin J, Sinacore J, Ennis A. Generee Region Poison Prevention Project: Phase II. Veterinary and Human Toxicology 1985;28(2):123‐6. [PubMed] [Google Scholar]
Frank 1992 {published data only}
- Frank RG, Bouman DE, Cain K, Watts C. A Preliminary Study of a Traumatic Injury Prevention Program. Psychology and Health 1992;6(1‐2):129‐40. [Google Scholar]
Frankenfield 1991 {published data only}
- Frankenfield DL, Reynolds DR, Regina DA. Pharmacist‐initiated poison prevention campaign in a rural county. American Journal of Hospital Pharmacy 1991;48(12):2657‐8. [PubMed] [Google Scholar]
Frederick 2000 {published data only}
- Frederick K Bixby E, Orzel MN, Stewart‐Brown S, Willett K. An evaluation of the effectiveness of the Injury Minimisation Programme for Schools (IMPS). Injury Prevention 2000;6(2):92‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaffney 1996b {published data only}
- Gaffney DT, Elkington JM, Stoker L. Reducing the opportunity for water scalds risks in domestic bathrooms. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Gallagher 1984 {published data only}
- Gallagher SS, Finison K, Guyer B, Goodenough S. The incidence of injuries among 87,000 Massachusetts children and adolescents; results of the 1980‐81 Statewide Childhood Injury Prevention Program surveillance system. American Journal of Public Health 1984;74:1340‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gallagher 1985 {published data only}
- Gallagher SS, Hunter P, Guyer B. A home injury prevention program for children. Pediatric Clinics of North America 1985;32(1):95‐112. [DOI] [PubMed] [Google Scholar]
Gatheridge 2004 {published data only}
- Gatheridge BJ, Miltenberger RG, Huneke DF, Satterlund MJ, Mattern AR, Johnson BM, et al. Comparison of two programs to teach firearm injury prevention skills to 6 and 7 year old children. Pediatrics 2004;114(3):294‐9. [DOI] [PubMed] [Google Scholar]
Geddis 1989 {published data only}
- Geddis D. Child Accident Prevention in New Zealand ‐ an overview. First World Conference on Accident and Injury Prevention, Stockholm, Sweden 1989. [Google Scholar]
Gielen 1996 {published data only}
- Gielen AC, Dannenberg AL, Ashburn N, Kou J. Teaching safety: evaluation of a children's village in Maryland. Injury Prevention 1996;2(1):26‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gielen 2001 {published data only}
- Gielen AC, Wilson ME, McDonald EM, Serwint JR, Andrews JS, Hwang WT, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Archives of Pediatrics & Adolescent Medicine 2001;1551(1):42‐9. [DOI] [PubMed] [Google Scholar]
Ginnelly 2005 {published data only}
- Ginnelly L, Sculpher M, Bojke C, Roberts I, Wade A, Diguiseppi C. Determining the cost effectiveness of a smoke alarm give‐away program using data from a randomized controlled trial. European Journal of Public Health 2005;15(5):448‐53. [DOI] [PubMed] [Google Scholar]
Glotzer 1997 {published data only}
- Glotzer DE, Weitzman M, Ascengrau A, Freedberg K. Economic evaluation of environmental interventions of low‐level childhood lead poisoning. Ambulatory Child Health 1997;3(3):255‐67. [Google Scholar]
Grant 1992 {published data only}
- Grant E, Turney E, Bartlett M, Winbon C, Peterson HD. Evaluation of a burn prevention program in a public school system. Journal of Burn Care and Rehabilitation 1992;13(6):703‐7. [PubMed] [Google Scholar]
Grant 2004 {published data only}
- Grant EJ. Burn prevention. Critical Care Nursing Clinics of North America 2004;16(1):127‐38. [DOI] [PubMed] [Google Scholar]
Gray 1979 {published data only}
- Gray JD, Cutler CA, Dean JG, Kempe CH. Prediction and prevention of child abuse and neglect. Journal of Social Issues 1979;35(2):127‐39. [PubMed] [Google Scholar]
Gresham 2001 {published data only}
- Gresham LS, Zirkle DL, Tolchin S, Jones C, Maroufi A, Miranda J. Partnering for injury prevention: evaluation of a curriculum‐based intervention program among elementary school children. Journal of Pediatric Nursing 2001;16(2):79‐87. [DOI] [PubMed] [Google Scholar]
Gross 1990 {published data only}
- Gross RT. Enhancing the outcomes of low‐birth‐weight, premature infants. A multisite, randomized trial. The Infant Health and Development Program. Journal of the American Medical Association 1990;263(22):3035‐42. [DOI] [PubMed] [Google Scholar]
Grossman 2000 {published data only}
- Grossman DC, Cummings P, Koepsell TD, Marshall J, D'Ambrosio L, Thompson RS, Mack C. Firearm safety counselling in primary care pediatrics: a randomized controlled trial. Pediatrics 2000;106(1 pt 1):22‐6. [DOI] [PubMed] [Google Scholar]
Guldvog 1993 {published data only}
- Guldvog G, Kopjar B. Community based injury control and evaluation in Norway‐ The Sogn & Fjordane injury prevention project. 2nd World Conference on Injury Control, Atlanta, USA 1993. [Google Scholar]
Gutelius 1977 {published data only}
- Gutelius MF, Kirsch AD, McDonald s, Riddick Brooks M, McErlan T. Controlled study of child health supervision: behaviour results. Pediatrics 1977;60(3):294‐304. [PubMed] [Google Scholar]
Guyer 2000 {published data only}
- Guyer B, Hughart N, Strobino D, Jones A, Scharfstein D. Assessing the impact of pediatric‐based development services on infants, families and clinicians: challenges to evaluating the Healthy Steps program. Pediatrics 2000;105(3):E33. [DOI] [PubMed] [Google Scholar]
Hall 1985 {published data only}
- Hall J. A decade of detectors: measuring the effect. Fire Journal 1985;78:37‐43. [Google Scholar]
Hall 1994 {published data only}
- Hall JR. The U.S. experience with smoke detectors: who has them? How well do they work? When don't they work?. National Fire Protection Association Journal 1994;88(5):36‐9, 41‐6. [PubMed] [Google Scholar]
Hardy 1989 {published data only}
- Hardy JB, Streett R. Family support and parenting education in the home: an effective extension of clinic‐based preventive health care services for poor children. Journal of Pediatrics 1989;115(6):927‐31. [DOI] [PubMed] [Google Scholar]
Hardy 1996 {published data only}
- Hardy MS, Armstrong FD, Martin BL, Strawn KN. A firearm safety program for children: they just can't say no. Journal of Developmental and Behavioural Pediatrics 1996;17(4):216‐21. [PubMed] [Google Scholar]
Hardy 2002 {published data only}
- Hardy MS. Teaching firearm safety to children: failure of a program. Journal of Behavioral Pediatrics 2002;23(2):71‐6. [DOI] [PubMed] [Google Scholar]
Harre 1998a {published data only}
- Harre N, Field J, Polzer‐Debruyne A. New Zealand children's involvement in home activities that carry a burn or scald risk. Injury Prevention 1998;4(4):266‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harre 1998b {published data only}
- Harre N, Polzer‐Debruyne A. A community based program for the prevention of burns and scalds to pre‐school children. Early Child Development and Care 1998;142(1):9‐22. [Google Scholar]
Harre 2000 {published data only}
- Harre N, Coveney A. School‐based scalds prevention: reaching children and their families. Health Education Research 2000;15(2):191‐202. [DOI] [PubMed] [Google Scholar]
Hemmo‐Lotem 2005a {published data only}
- Hemmo‐Lotem M, Jinich‐Aronowitz C, Endy‐Findling L, Molcho M, Klein M, Waisman Y, Danon YL, Merrick J. Child injury in Israel: emergency room visits to a children's medical centre. TheScientificWorldJOURNAL 2005;5:253‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hemmo‐Lotem 2005b {published data only}
- Hemmo‐Lotem M, Merrick E, Endy‐Findling L, Freh AA, Aziza A, Jinich‐Aronowitz C, Korn L, Merrick J. Childhood Injury Prevention: Intervention in the Bedouin city of Rahat. TheScientificWorldJOURNAL 2005;5:596‐608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Himle 2004 {published data only}
- Himle MB, Miltenberger RG, Gatheridge BJ, Flessner CA. An evaluation of two procedures for training skills to prevent gun play in children. Pediatrics 2004;113(1):70‐7. [DOI] [PubMed] [Google Scholar]
HIPRC 2004 {published data only}
- Harborview Injury Prevention Research Center. Gun lockbox intervention project. www.cdc.gov/ncipc Access date 25.08.04. [Google Scholar]
Huxley 1993 {published data only}
- Huxley P, Warner R. Primary prevention of parenting dysfunction in high‐risk cases. American Journal of Orthopsychiatry 1993;63(4):582‐8. [DOI] [PubMed] [Google Scholar]
Jackson 1980 {published data only}
- Jackson RH, Craft AW. Child resistant containers. Lancet 1980;1(8159):97. [PubMed] [Google Scholar]
Jackson 1983 {published data only}
- Jackson RH. Play It Safe: a campaign for the prevention of children's accidents. Community Development Journal 1983;18(2):172‐6. [Google Scholar]
Johnson 1993 {published data only}
- Johnson Z, Howell F, Molloy B. Community mothers' programme: randomised controlled trial of non‐professional intervention in parenting. British Medical Journal 1993;306(6890):1449‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2000 {published data only}
- Johnson Z, Molloy B, Scallan E, Fitzpatrick P, Rooney B, Keegan T, et al. Community Mothers Programme ‐ seven year follow up of a randomised controlled trial of non‐professional intervention in parenting. Journal of Public Health Medicine 2000;22(3):337‐42. [DOI] [PubMed] [Google Scholar]
Johnston 2002 {published data only}
- Johnston BD, Rivara F, Droesch R, Dunn C, Copass M. Behaviour change counselling in the emergency department to reduce injury risk: a randomised, controlled trial. Pediatrics 2002;110(2):267‐74. [DOI] [PubMed] [Google Scholar]
Jones 2001 {published data only}
- Jones AR, Thompson CJ, Davis MK. Smoke alarm ownership and installation: a comparison of a rural and a suburban community in Georgia. Journal of Community Health 2001;26(5):307‐29. [DOI] [PubMed] [Google Scholar]
Jordan 1993 {published data only}
- Jordan EA, Duggan AK, Hardy JB. Injuries in children of adolescent mothers: home safety education associated with decreased injury risk. Pediatrics 1993;91(2):481‐7. [PubMed] [Google Scholar]
Jordan 2003 {published data only}
- Jordan CM, Yust BL, et al. A randomised trial of education to prevent lead burden in children at high risk for lead exposure: efficacy as measured by blood lead poisoning. Environmental Health Perspectives 2003;111(16):1947‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaplan 1999 {published data only}
- Kaplan DW, Grindis CD. A comparison study of an elementary school‐based health centre: effects on health care access and use. Archives of Pediatrics and Adolescent Medicine 1999;153(3):235‐43. [DOI] [PubMed] [Google Scholar]
Katcher 1987 {published data only}
- Katcher ML. Prevention of Tap Water Scald Burns: evaluation of a multi‐media injury control program. American Journal of Public Health 1987;77(9):1195‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kendrick 2009 {published data only}
- Kendrick D, Mulvaney C, Watson M. Does targeting injury prevention towards families in disadvantaged areas reduce inequalities in safety practices?. Health Education Research 2009;24(1):32‐41. [DOI] [PubMed] [Google Scholar]
Ketvertis 2003 {published data only}
- Ketvertis KM. Behavior change counselling in the emergency department to reduce injury risk: a randomized controlled trial [4] (multiple letters). Pediatrics 2003;111(5):1125. [DOI] [PubMed] [Google Scholar]
King 1999 {published data only}
- King L, Thomas M, Gatenby K, Georgiou A, Hua M. "First aid for scalds" campaign: reaching Sydney's Chinese, Vietnamese and Arabic speaking communities. Injury Prevention 1999;5(2):104‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kitzman 1997 {published data only}
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomised controlled trial. JAMA 1997;278(8):644. [PubMed] [Google Scholar]
Klassen 1995 {published data only}
- Klassen TP. Primary care counselling for injury prevention: where is the evidence?. Injury Prevention 1995;1(3):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koniak‐Griffin 2003 {published data only}
- Koniak‐Griffin D, Verzemnieks IL, Anderson NL, Brecht ML, Lesser J, Kim S, et al. Nurse visitation for adolescent mothers: two‐year infant health and maternal outcomes. Nursing Research 2003;52(2):127‐36. [DOI] [PubMed] [Google Scholar]
Korn 2009 {published data only}
- Korn L, Hemmo‐Lotem M, Endy‐Findling L. Safe communities for children: insight from a pilot program for preventing unintentional injuries. International Journal of Adolescent Medicine and Health 2009;21(2):187‐95. [DOI] [PubMed] [Google Scholar]
Kravitz 1973 {published data only}
- Kravitz H. Prevention of accidental falls in infancy by counselling mothers. Illinois Medical Journal 1973;144(6):570‐3. [PubMed] [Google Scholar]
Krenzelok 1981 {published data only}
- Krenzelok EP, Garber RJ. Teaching poison prevention to preschool children, their parents, and professional educators through child care centers. American Journal of Public Health 1981;71(7):750‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuhn 1994 {published data only}
- Kuhn L, Davidson LL, Durkin MS. Use of Poisson regression and time series analysis for detecting changes over time in rates of child injury following a prevention program. American Journal of Epidemiology 1994;140(10):943‐55. [DOI] [PubMed] [Google Scholar]
Lagerberg 2000 {published data only}
- Lagerberg D. Secondary Prevention in child health: effects of psychological intervention, particularly home visitation, on children's development and other outcome variables. Acta Paediatrica supplement 2000;89(434):43‐52. [DOI] [PubMed] [Google Scholar]
Lamb 2006 {published data only}
- Lamb R, Joshi MS, Carter W, Cowburn G, Matthews A. Children's acquisition and retention of safety skills: the Lifeskills program. Injury Prevention 2006;12(3):161‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lane 1971 {published data only}
- Lane MF, Barbarite RV, Bergner L, Harris D. Child‐resistant medicine containers: experience in the home. American Journal of Public Health 1971;61(9):1861‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lanphear 1999 {published data only}
- Lanphear BP, Howard C, Eberley S, Auinger P, Kolassa J, Weitzman M, et al. Primary Prevention of Childhood Lead Exposure: a randomised trial of dust control. Pediatrics 1999;103(4 pt 1):772‐7. [DOI] [PubMed] [Google Scholar]
Larcher 1987 {published data only}
- Larcher P. Childhood accidents: comparison of televised prevention campaigns. Annals de Pediatrie 1987;34(3):239‐41. [PubMed] [Google Scholar]
Larson 1980 {published data only}
- Larson CP. Efficacy of prenatal and postpartum home visits on child health and development. Pediatrics 1980;66(2):191‐7. [PubMed] [Google Scholar]
Lealman 1983 {published data only}
- Lealman GT, Haigh D, Phillips JM, Stone J, Ord‐Smith C. Prediction and prevention of child abuse‐‐an empty hope?. Lancet 1983;1(8339):1423‐4. [DOI] [PubMed] [Google Scholar]
Lechman 1991 {published data only}
- Lechman BC, Bronwich EB. Evaluation of an Education Program for Spinal Cord Injury Prevention: Some preliminary findings. Spinal Cord Injury Digest (Model Systems) 1991;3:27‐34. [Google Scholar]
Leduc 1999 {published data only}
- Leduc C. Evaluation d'une trousse de prevention des traumatismes a domicile surveyant a de jeunes enfants. Direction de la sante publique, de la planification at de l'evaluation. Quebec: regie regionale de la sante et des services sociaux du Bas‐Saint‐Laurent 1999. [Google Scholar]
Lee 2002 {published data only}
- Lee L‐L, Pai L, Shen P‐C. Community home injury prevention for children under 5. Chinese Journal of Public Health 2002;21(1):61‐72. [Google Scholar]
Lenton {published data only}
- Lenton S. Defining the health service contribution to reducing injuries to preschool children in Wiltshire. Unpublished report. [Google Scholar]
Lenton 2000 {published data only}
- Lenton S. Randomised controlled community intervention trial to reduce injuries to pre‐school children in "high risk" communities. Unpublished report. [Google Scholar]
Liller 1998 {published data only}
- Liller KD, Craig J, Crane N, McDermott RJ. [Evaluation of a poison prevention lesson for kindergarten and third grade students]. Injury Prevention 1998;4(3):218‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liller 2003 {published data only}
- Liller KD, Perrin K, Nearns J, Pesce K, Crane NB, Gonzalez RR. Evaluation of the "respect not risk" firearm safety lesson for 3rd graders. Journal of School Nursing 2003;19(6):142‐8. [DOI] [PubMed] [Google Scholar]
Linares 1979 {published data only}
- Linares AZ, Linares HA. Burn prevention programmes for children: are they effective?. Burns 1979;6(2):73‐9. [Google Scholar]
Lindqvist 1998b {published data only}
- Lindqvist K, Timpka T, Scelp L, Ahlgren M. The WHO safe community program for injury prevention: evaluation of the impact on injury severity. Public Health 1998;112(6):385‐91. [DOI] [PubMed] [Google Scholar]
Loescher 1995 {published data only}
- Loescher LJ, Emerson J, Taylor A, Christensen DH, McKinney M. Educating preschoolers about sun safety. American Journal of Public Health 1995;85(7):939‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 1999 {published data only}
- Lowe JB, Balanda KP, Stanton WR, Gillespie A. Evaluation of a three‐year school‐based intervention to increase adolescent sun protection. Health Education and Behaviour 1999;26(3):396‐408. [DOI] [PubMed] [Google Scholar]
Luria 2000 {published data only}
- Luria JW, Smith GA, Chapman JI. An evaluation of a safety education program for kindergarten and elementary school children. Archives of Pediatrics and Adolescent Medicine 2000;154(3):227‐31. [DOI] [PubMed] [Google Scholar]
Mackenzie 2004 {published data only}
- Mackenzie E. Managed care and child safety. www.cdc.gov/ncipc Access date 25.08.04. [Google Scholar]
Malouin 2003 {published data only}
- Malouin R, Winch P, Leontsini E, Glass G, Simon D, Hayes EB, Schwartz BS. Longitudinal evaluation of an educational intervention for preventing tick bites in an area with endemic lyme disease in Baltimore county, Maryland. American Journal of Epidemiology 2003;157(11):1039‐51. [DOI] [PubMed] [Google Scholar]
Margolis 2001 {published data only}
- Margolis PA, Stevens R, Bordley WC, Stuart J, Harlan C, Keyes‐Elstein L, et al. From concept to application: the impact of a community‐wide intervention to improve the delivery of preventive services to children. Pediatrics 2001;108(3):E42. [DOI] [PubMed] [Google Scholar]
Marion 2004 {published data only}
- Marion DW. Implementation and Evaluation of "Think first for kids" in the City of Pittsburgh Elementary Schools. www.cdc.gov/ncipc Access date 25.08.04. [Google Scholar]
McConnell 1996a {published data only}
- McConnell CF, Dwyer WO, Leeming FC. A behavioural approach to reducing fires in public housing. Journal of Community Psychology 1996;24:201‐12. [Google Scholar]
McConnell 1996b {published data only}
- McConnell C, Leeming F, Dwyer W. Evaluation of a fire safety training program for preschool children. Journal of Community Psychology 1996;24:213‐27. [Google Scholar]
McWhirter 2000 {published data only}
- McWhirter JM, Collins M, Bryant I, Wetton NM, Newton Bishop J. [Evaluating 'safe in the sun', a curriculum programme for primary schools]. Health Education Research 2000;15(2):203‐7. [DOI] [PubMed] [Google Scholar]
Melhuish 2008 {published data only}
- Melhuish E, Belsky J, Leyland AH, Barnes J. Effects of fully‐established Sure Start Local Programmes on 3‐year‐old children and their families living in England: a quasi‐experimental observational study. Lancet 2008;372(9650):1641‐7. [DOI] [PubMed] [Google Scholar]
MET 1986 {published data only}
- MET Electrical Testing Company. Evaluation of presently available swimming pool/alarm detection systems. US Consumer Product Safety Commission, Washington 1986. [Google Scholar]
Milliner 1980 {published data only}
Milne 1999 {published data only}
- Milne E, English DR, Cross D, Corti B, Costa C, Johnston R. Evaluation of an intervention to reduce sun exposure in children: design and baseline results. American Journal of Epidemiology 1999;150(2):164‐73. [DOI] [PubMed] [Google Scholar]
Milne 2000 {published data only}
- Milne E, English DR, Johnston R, Cross D, Borland R, Costa C, et al. Improved sun protection behaviour in children after two years of the Kidskin intervention. Australian and New Zealand Journal of Public Health 2000;24(5):481‐7. [DOI] [PubMed] [Google Scholar]
Milne 2002 {published data only}
- Milne E, Johnston R, Cross D, Giles‐Corti B, English DR. Effect of a school based sun‐protection intervention on the development of melanocytic nevi in children. American Journal of Epidemiology 2002;155(8):739‐45. [DOI] [PubMed] [Google Scholar]
Minchom 1984 {published data only}
- Minchom PE, Sibert JR, Newcombe RG, Bowley MA. Does health education prevent childhood accidents?. Postgraduate Medical Journal 1984;60(702):260‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Minkovitz 2001 {published data only}
- Minkovitz C, Strobino D, Hughart N, Scharfstein D, Guyer B. Early effects of the healthy steps for young children program. Archives of Pediatric Adolescent Medicine 2001;155(4):470‐9. [DOI] [PubMed] [Google Scholar]
Minkovitz 2003 {published data only}
- Minkovitz CS, Hughart N, Strobino D, Scharfstein D, Grason H, Miller T, et al. A practice‐based intervention to enhance quality of care in the first 3 years of life: the Healthy Steps for Young Children Program. JAMA 2003;290(23):3136‐8. [DOI] [PubMed] [Google Scholar]
Mondozzi 2001 {published data only}
- Mondozzi MA, Harper MA. In search of effective education in burn and fire prevention. Journal of Burn Care and Rehabilitation 2001;22(4):277‐81. [DOI] [PubMed] [Google Scholar]
Moore 2004 {published data only}
- Moore J, Morath K, Harre N. Follow up study of a school based scalds prevention programme. Health Education Research 2004;19(4):430‐9. [DOI] [PubMed] [Google Scholar]
Mori 1986 {published data only}
- Mori L, Peterson L. Training preschoolers in home safety skills to prevent inadvertent injury. Journal of Clinical Child Psychology 1986;15(2):106‐14. [Google Scholar]
Morrison 1988 {published data only}
- Morrison MI, Herath K, Chase C. Puppets for prevention: 'playing safe is playing smart'. Journal of Burn Care and Rehabilitation 1988;9(6):650‐1. [DOI] [PubMed] [Google Scholar]
Morrongiello 1998 {published data only}
- Morrongiello BA, Miron J, Reutz R. Prevention of paediatric acquired brain injury: an interactive, elementary‐school program. Canadian Journal of Public Health 1998;89(6):391‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Naidoo 1984 {published data only}
- Naidoo J. Evaluation of the Play it Safe campaign in Bristol. Child Accident Prevention Trust 1984. [Google Scholar]
Nicholson 2002 {published data only}
- Nicholson AJ, Duff S, Mullan C, O'Keefe B, Ryan M. The use of local accident emergency injury surveillance to monitor the impact of a lay safety community programme. Irish Medical Journal 2002;95(5):1‐7. [PubMed] [Google Scholar]
Nossar 2001 {published data only}
- Nossar V, Hudson D. Improving health outcomes for children by home visiting. Medicine Today 2001;2(8):135‐6. [Google Scholar]
Novick 1997 {published data only}
- Novick M. To burn or not to burn: use of computer‐enhanced stimuli to encourage application of sunscreens. Cutis 1997;60(2):105‐8. [PubMed] [Google Scholar]
O'Connor 1982 {published data only}
- O'Connor PJ. Poisoning prevention: results of a public media campaign. Australian Pediatric Journal 1982;18(4):250‐2. [PubMed] [Google Scholar]
O'Connor 1990 {published data only}
- O'Connor PJ, Innes JM. Audio‐visual information on child illness prevention in hospital waiting rooms: an experimental evaluation. Health Promotion International 1990;5(1):3‐8. [Google Scholar]
O'Donnell 1996 {published data only}
- O'Donnell G. The S.A.F.E programme: working towards a safe accident free environment. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Oakley 1998 {published data only}
- Oakley A. Randomised controlled trial and economic evaluation of two alternative strategies of providing support for socially disadvantaged inner city families with infants. www.nrr.nhs.uk 1998. [Google Scholar]
Olds 1986 {published data only}
- Olds DL, Henderson CR Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78(1):65‐78. [PubMed] [Google Scholar]
Olds 1999 {published data only}
- Olds DL, Henderson CR Jr, Kitzman HJ, Eckenrode JJ, Cole RE, Tatelbaum RC. Prenatal and infancy home visitation by nurses: recent findings. Future Child 1999;9(1):44‐65, 190‐1. [PubMed] [Google Scholar]
Olds 2002 {published data only}
- Olds, DL. Prenatal and infancy home visiting by nurses: from randomised trials to community replication. Prevention Science 2002;3(3):153‐72. [DOI] [PubMed] [Google Scholar]
Palmisano 1981 {published data only}
- Palmisano PA. Targeted intervention in the control of accidental drug overdoses by children. Public Health Reports 1981;96(2):150‐6. [PMC free article] [PubMed] [Google Scholar]
Parcel 1983 {published data only}
- Parcel GS, Bruhn JG, Murray JL. Preschool health education program (PHEP): analysis of educational and behavioral outcome. Health Education Quarterly 1983;10(3‐4):149‐72. [DOI] [PubMed] [Google Scholar]
Paulson 1981 {published data only}
- Paulson JA. Injury prevention in children. Journal of Family Practice 1981;13(1):123‐4. [PubMed] [Google Scholar]
Pena 1994 {published data only}
- Pena R, Thorn A. Results from a community intervention project in the Nicaraguan mining community El Limon. An overview. Social Science and Medicine 1994;38(4):623‐9. [DOI] [PubMed] [Google Scholar]
Peterson 1984a {published data only}
- Peterson L. The "safe at home" game. Training comprehensive prevention skills in latchkey children. Behaviour Modification 1984;8(4):474‐94. [DOI] [PubMed] [Google Scholar]
Peterson 1984b {published data only}
- Peterson L. Teaching home safety and survival skills to latch‐key children: a comparison of two manuals and methods. Journal of Applied Behaviour Analysis 1984;17(3):279‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petridou 1994 {published data only}
- Petridou E, Kouri N. School injuries in Athens: Socioeconomic and family risk factors. Journal of Epidemiology and Community 1994;48(5):490‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petridou 1995 {published data only}
- Petridou E, Polychronopoulou A, Kouri N, Karpathios T, Trichopoulos D. Childhood poisonings from ingestion of cigarettes. Lancet 1995;346:8985. [DOI] [PubMed] [Google Scholar]
Petridou 2002 {published data only}
- Petridou E, Alexe D, Trichopoulos D. Central heating devices cause childhood injuries but rarely burns; a study in Greece. European Journal of Pediatrics 2002;161(6):347‐8. [DOI] [PubMed] [Google Scholar]
Phillips 1980 {published data only}
- Phillips WR, Little TL. Continuity of care and poisoning prevention and education. Patient Counselling and Health Education 1980;2(4):170‐3. [DOI] [PubMed] [Google Scholar]
Phillips 1986 {published data only}
- Phillips W, Mahairas E, Hunt D, Pegg SP. The epidemiology of childhood scalds in Brisbane. Burns 1986;12(5):343‐50. [DOI] [PubMed] [Google Scholar]
Pocknall 1993 {published data only}
- Pocknall H. Preventing childhood accidents. Nursing New Zealand 1993;1(6):22‐3. [PubMed] [Google Scholar]
Polivka 1999 {published data only}
- Polivka BJ. Rural residents knowledge of lead poisoning prevention. Journal of Community Health 1999;24(5):393‐408. [DOI] [PubMed] [Google Scholar]
Potts 1998 {published data only}
- Potts R, Swisher L. Effects of televised safety models on children's risk taking and hazard identification. Journal of Pediatric Psychology 1998;23(3):157‐63. [DOI] [PubMed] [Google Scholar]
Powell 2000 {published data only}
- Powell E, Tanz R, Uyeda A, Gaffney M, Sheehan K. Injury prevention education using pictorial information. Pediatrics 2000;105(1):1‐5. [DOI] [PubMed] [Google Scholar]
Quan 1990 {published data only}
- Quan L, Gomez A. Swimming pool safety: an effective submersion prevention program. Journal of Environmental Health 1990;52(6):344‐6. [Google Scholar]
Rahman 2002 {published data only}
- Rahman AF. Safe communities: the experience from introducing Safe Communities into Bangladesh. In: Cho JP, Svanstrom L editor(s). Developing Safe Communities—Two Decades of Experiences. Suwon, Korea: Department of Emergency Medicine, Ajou University School of Medicine, 2002. [Google Scholar]
Reichelderfer 1976 {published data only}
- Reichelderfer TE. Preventing accidents from power lawnmowers. Pediatric Annals 1976;6(11):39‐40. [PubMed] [Google Scholar]
Rhoads 1999 {published data only}
- Rhoads GG, Ettinger AS, Weisel CP, Buckley TJ, Goldman KD, Adgate J, Lioy PJ. The effect of dust lead control on blood lead in toddlers: a randomised trial. Pediatrics 1999;103(3):551‐5. [DOI] [PubMed] [Google Scholar]
Rutstein 1977 {published data only}
- Rutstein R, Butler AJ. Cost Effectiveness of Fire Prevention Publicity ‐ Final Report on the 1976/77 Fat Pan Fire Publicity Campaign. Home Office Scientific Advisory Branch Report 1977;Report No 9/77. [Google Scholar]
Sadan 1995 {published data only}
- Sadan N, Raz A, Wolach B. Impact of community educational programmes on foreign body aspiration. European Journal of Pediatrics 1995;154(10):859‐62. [DOI] [PubMed] [Google Scholar]
Sahlin 1990 {published data only}
- Sahlin Y, Lereim I. Accidents among children below school age. Changes of incidence after intervention. Acta Paediatrica Scandinavica 1990;79:691‐7. [DOI] [PubMed] [Google Scholar]
San Agustin 1973 {published data only}
- San Agustin M, Stevens E, Hicks D. An evaluation of the effectiveness of a Children and Youth project. Health Services Reports 1973;88(10):942‐6. [PMC free article] [PubMed] [Google Scholar]
Schnell 1993 {published data only}
- Schnell LR, Tanz RR. The effect of providing ipecac to families seeking poison related services. Pediatric Emergency Care 1993;9(1):36‐9. [DOI] [PubMed] [Google Scholar]
Schwebel 2002 {published data only}
- Schwebel DC, Speltz ML, Jones K, Bardina P. Unintentional injury in preschool boys with and without early onset of disruptive behaviour. Journal of Pediatric Psychology 2002;27(8):727‐37. [DOI] [PubMed] [Google Scholar]
Sell 1977 {published data only}
- Sell RG. What Does Safety Propoganda do for Safety? A Review. Applied Ergonomics 1977;8(4):203‐14. [DOI] [PubMed] [Google Scholar]
Sherman 1980 {published data only}
- Sherman FT. Child resistant containers. Lancet 1980;1(8159):97‐8. [PubMed] [Google Scholar]
Sibert 1977 {published data only}
- Sibert JR, Craft AW, Jackson RH. Child resistant packaging and accidental child poisoning. Lancet 1977;2(8032):289‐90. [DOI] [PubMed] [Google Scholar]
Sibert 1999 {published data only}
- Sibert J. Evaluating a community safety project for families with babies ‐ a randomised controlled trial. Child Care Health and Development 1999;28(6):439. [Google Scholar]
Sibert 2002 {published data only}
- Sibert JR, Kemp AM. Safe communities for children: only models of good practice or ways through practical difficulties in injury prevention?. Child Care Health and Development 2002;28(6):439‐42. [DOI] [PubMed] [Google Scholar]
Smith 1984 {published data only}
- Smith JE, Rachman SJ. Non accidental injury to children‐II. A controlled evaluation of a behavioural management programme. Behaviour Research and Therapy 1984;22(4):349‐66. [DOI] [PubMed] [Google Scholar]
Smith 2002 {published data only}
- Smith LE, Greene MA. Study of the effectiveness of the USsafety standard for child resistant cigarette lighters. Injury Prevention 2002;8(3):192‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2006 {published data only}
- Smith GA, Splaingard M, Hayes JR, Xiang H. Comparison of a personalized parent voice smoke alarm with a conventional residential tone smoke alarm for awakening children. Pediatrics 2006;118(4):1623‐32. [DOI] [PubMed] [Google Scholar]
Smithson 1998 {published data only}
- Smithson RD. Community childhood accident prevention project. 4th World Conference on Injury Prevention and Control, Amsterdam, Holland 1998. [Google Scholar]
Smithson 2000 {published data only}
- Smithson RD, Mullan C. Community Childhood Accident Prevention. 5th World Conference on Injury Prevention and Control, Delhi, India 2000. [Google Scholar]
Solis 1991 {published data only}
- Solis GR. Evaluation of a children's safety fair. Pediatric Nursing 1991;17(3):255‐8. [PubMed] [Google Scholar]
Sorensen 1976 {published data only}
- Sorensen B. Prevention of burns and scalds in a developed country. Journal of Trauma 1976;16(4):249‐58. [PubMed] [Google Scholar]
Spallek 2004a {published data only}
- Spallek M, Bain C, McClure R, Najman J, Nixon J, Purdie D, et al. The effectiveness of a community wide hot water scalds prevention campaign. 7th World Conference on Injury Prevention and Safety Promotion, Vienna, Austria 2004. [Google Scholar]
Spallek 2004b {published data only}
Speigel 1995 {published data only}
- Speigel C, Lindaman F. Children can't fly; a program to prevent childhood morbidity and mortality from window falls. Injury Prevention 1995;1(3):194‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spiller 2004 {published data only}
- Spiller HA, Mowry JB. Evaluation of the effect of a public educator on calls and poisonings reported to a regional poison center. Veterinary and Human Toxicology 2004;46(4):206‐98. [PubMed] [Google Scholar]
Stanley 1979 {published data only}
- Stanley TV. [Childproof containers]. Lancet 1979;2(8152):1132‐3. [DOI] [PubMed] [Google Scholar]
Stennies 1999 {published data only}
- Stennies G, Ikeda R, Leadbetter S, Houston B, Sacks J. Firearm storage practices and children in the home, United States, 1994. Archives of Pediatrics and Adolescent Medicine 1999;153(6):586‐90. [DOI] [PubMed] [Google Scholar]
Stephen 1993 {published data only}
- Stephen FR, Murray JP. Prevention of hot tap water burns ‐ a comparative study of three types of automatic mixing valve. Burns 1993;19(1):56‐62. [DOI] [PubMed] [Google Scholar]
Stevens 2002 {published data only}
- Stevens M, Olson A, Gaffney C, Tosteson T, Mott L, Starr P. A pediatric, practice based, randomised trial of drinking and smoking prevention and bicycle helmet, gun and seatbelt safety promotion. Pediatrics 2002;109(3):490‐7. [DOI] [PubMed] [Google Scholar]
St Pierre 1999 {published data only}
- Pierre RG, Layzer JI. Using home visits for multiple purposes: the Comprehensive Child Development Programme. Future Child 1999;9(1):134‐51. [PubMed] [Google Scholar]
Sullivan 1990 {published data only}
- Sullivan M. Reducing child hazards in the home. A joint venture in injury control. Journal of Burn care and Rehabilitation 1990;1:175‐9. [DOI] [PubMed] [Google Scholar]
Sundelin 1996 {published data only}
- Sundelin C, Rasmussen F, Berfenstam R, Troedsson K. Information through television: does it promote child safety?. Injury Prevention 1996;2(1):36‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Svanstrom 1996 {published data only}
- Svanstrom L, Schelp L, Ekman R, Lindstrom A. Falkoping, Sweden, ten years after: still a safe community?. International Journal of Consumer Safety 1996;3(1):1‐7. [Google Scholar]
Swaine 2000 {published data only}
- Swaine BR, Pless IB, Friedman DS, Montes JL. Effectiveness of a head injury program for children: a preliminary investigation. American Journal of Physical Medicine and Rehabilitation 2000;79(5):412‐20. [DOI] [PubMed] [Google Scholar]
Taha 1999 {published data only}
- Taha T, Kanarek MS, Schultz BD, Murphy A. Low‐cost household paint abatement to reduce children's blood lead levels. Environmental Research 1999;81(4):334‐8. [DOI] [PubMed] [Google Scholar]
Temple 1978 {published data only}
- Temple AR. Testing of child‐resistant containers. Clinical Toxicology 1978;12(3):357‐65. [DOI] [PubMed] [Google Scholar]
Tenn 1996 {published data only}
- Tenn L, Dewis ME. An evaluation of a Canadian peer‐driven injury prevention programme for high‐risk adolescents. Journal of Advanced Nursing 1996;23(2):329‐37. [DOI] [PubMed] [Google Scholar]
Terzidis 2007 {published data only}
- Terzidis A, Koutroumpa A, Skalkidis I, Matzavakis I, Mallori M, Frangakis CE, DiScala C, Petridou ET. Water safety: age specific changes in knowledge and attitudes following a school based intervention. Injury Prevention 2007;13(2):120‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 1998 {published data only}
- Thompson R, Edwards P, Jarvis S, Avery A, Towner E, Walsh S. Childhood accidents: is it time to prescribe safety equipment?. Community Practitioner 1998;71:138‐40. [Google Scholar]
Thomson 1999 {published data only}
- Thomson H, Ross S, Wilson P, McConnachie A, Watson R. Randomised controlled trial of effect of Baby Check on use of health services in first 6 months of life. British Medical Journal 1999;318(7200):1740‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thuen 1994 {published data only}
- Thuen F, Sam DL. Use of safety equipment among immigrant children in Norway. A comparison with Norwegian children. Tidsskrift for Den Norske Lageforening 1994;114(2):195‐8. [PubMed] [Google Scholar]
Timpka 1999 {published data only}
- Timpka T, Lindqvist K, Schelp L, Ahlgren M. Community‐based injury prevention: effects on health care utilization. International Journal of Epidemiology 1999;28(3):502‐8. [DOI] [PubMed] [Google Scholar]
Towner 1996 {published data only}
- Towner E. A randomised controlled trial of an injury prevention programme in primary schools. http://www.controlled‐trials.com/mrct/trial/TOWNER%7CE/1054/43303.html 1996. [Google Scholar]
Towner 1998 {published data only}
- Towner EML, Young A, Errington G, Jarvis S. Documenting the process of an injury prevention programme in primary schools. 4th World Conference on Injury Prevention and Control, Amsterdam, Holland 1998. [Google Scholar]
Velsog 1996 {published data only}
- Velsog G. Educational model evaluation for prevention and first aids accidents in home. 3rd International Conference on Injury Prevention and Control, Melbourne, Australia 1996. [Google Scholar]
Vernberg 1984 {published data only}
- Vernberg K, Culver‐Dickinson P, Spyker DA. The deterrent effect of poison‐warning stickers. American Journal of Diseases of Children 1984;138(11):1018‐20. [DOI] [PubMed] [Google Scholar]
Vogel 1968 {published data only}
- Vogel RE, Charles D. The effectiveness of a handgun education safety program. Journal of Police Science and Administration 1968;14(3):248. [Google Scholar]
Webne 1989 {published data only}
- Webne S. Pediatric Burn Prevention: an evaluation of the efficacy of a strategy to reduce tap water temperature in a population at risk for scalds. Journal of Developmental and Behavioural Pediatrics 1989;10:187‐91. [PubMed] [Google Scholar]
Wester 1985 {published data only}
- Wester TB. Project ipecac: an accident prevention program of the Robeson County Department of Health. North Carolina Medical Journal 1985;46(7):425‐6. [PubMed] [Google Scholar]
Whitfield 2000 {published data only}
- Whitfield T. An evaluation of swimming pool alarms. Consumer Product Safety Commission, USA 2000.
Whitt 1982 {published data only}
- Whitt JK, Casey P. The mother‐infant relationship and infant development: the effect of pediatric intervention. Child Development 1982;53(4):948‐56. [PubMed] [Google Scholar]
Wiggins 2004 {published data only}
- Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al. The social support and family health study; a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner‐city areas. Health Technology Assessment 2004;8(32):1‐134. [DOI] [PubMed] [Google Scholar]
Wortel 1991 {published data only}
- Wortel E, Ooijendijk WTM, Geus GH de, Stompedissel I. Volunteers as safety educators in a community campaign on child safety. Health Promotion International 1991;6(3):173‐80. [Google Scholar]
Wurtele 1989 {published data only}
- Wurtele SK, Kast LC, Miller‐Perrin CL, Kondrick PA. Comparison of programs for teaching personal safety skills to preschoolers. Journal of Consulting and Clinical Psychology 1989;57(4):505‐11. [DOI] [PubMed] [Google Scholar]
Young 2000 {published data only}
- Young A, Errington G, Sparks G, Towner E, Jarvis S, Carr G. Measuring and influencing the safety culture of primary schools. 5th World Conference on Injury Prevention and Control, Delhi, India 2000. [Google Scholar]
Ytterstad 2000 {published data only}
- Ytterstad B, Lund J. Prevention of childhood accidents in Norway. Tidsskrift for Den Norske Leogeforening 2000;120(28):3375. [PubMed] [Google Scholar]
Zwi 2004 {published data only}
- Zwi K, Williamson A. Injury prevention in the clinical setting. Book Chapter ‐ Evidence‐based Pediatrics and Child Health. 2. Vol. 1, 2004:211‐21. [Google Scholar]
References to ongoing studies
Cusimano (Canada) {published data only}
- Cusimano M. The long term persistence of the think first for kids injury prevention program at six and eighteen months. 6th World Conference on Injury Prevention and Control, Montreal, Canada 2002. [Google Scholar]
Grossman (USA) {published data only}
- Grossman D. Raise the Alarms (a trial of smoke detector types). www.cdc.gov/ncipc Access date 25.08.04. [Google Scholar]
Additional references
Adams 2004
- Adams G, Gulliford MC, Ukoumunne OC, Eldridge S, Chinn S, Campbell MJ. Patterns of intra‐cluster correlation from primary care research to inform study design and analysis. Journal of Clinical Epidemiology 2004;57:785‐94. [DOI] [PubMed] [Google Scholar]
Alwash 1998
- Alwash R, McCarthy M. Accidents in the home among children under 5: ethnic differences or social disadvantage?. BMJ 1988;296(6634):1450‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Azizi 1994
- Azizi BH, Zulkifli HI, Kassim MS. Circumstances surrounding accidental poisoning in children. Medical Journal of Malaysia 1994;49(2):132‐7. [PubMed] [Google Scholar]
Bennett 2008
- Bennett C, Macdonald G, Dennis JA, Coren E, Patterson J, Astin M, Abbott J. Home‐based support for disadvantaged adult mothers. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD003759.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bijur 1988a
- Bijur PE, Golding J, Haslum M. Persistence of occurrence of injury: can injuries of preschool children predict injuries of school‐aged children?. Pediatrics 1988;82(5):707‐12. [PubMed] [Google Scholar]
Bijur 1988b
- Bijur PE, Golding J, Kurzon M. Childhood accidents, family size and birth order. Social Science & Medicine 1988;26(8):839‐43. [DOI] [PubMed] [Google Scholar]
CAPT 2004
- Child Accident Prevention Trust. Preventing bath water scalds using thermostatic mixer valves. Preventing bath water scalds using thermostatic mixer valves. London: Child Accident Prevention Trust, 2004. [Google Scholar]
Cubbin 2000a
- Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. American Journal of Public Health 2000;90(1):70‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cubbin 2000b
- Cubbin C, LeClare FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood dominants. Journal of Epidemiology and Community Health 2000;54:517‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
DETR 2001
- Department of the Environment Transport and the Regions. Road accident involvement of children from ethnic minorities: a literature review. Road Safety Research Report No.19. Department of the Environment, Transport and the Regions 2001;London. [Google Scholar]
DiGuiseppi 1998
- DiGuiseppi C, Roberts I, Li L. Smoke alarm ownership and house fire death rates in children. Journal of Epidemiology and Community Health 1998;52(11):760‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiGuiseppi 2000
- DiGuiseppi C, Roberts I. Individual‐level injury prevention strategies in the clinical setting. The Future of Children 2000;10(1):53‐82. [PubMed] [Google Scholar]
DiGuiseppi 2001
- DiGuiseppi C, Goss CW, Higgins JPT. Interventions for promoting smoke alarm ownership and function. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD002246] [DOI] [PMC free article] [PubMed] [Google Scholar]
Donner 2000
- Donner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold, 2000. [Google Scholar]
Dowswell 1996
- Dowswell T, Towner EM, Simpson G, Jarvis SN. Preventing childhood unintentional injuries ‐ what works? A literature review. Injury Prevention 1996;2(2):140‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dowswell 2002
- Dowswell T, Towner E. Social deprivation and the prevention of unintentional injury in childhood: a systematic review. Health Education Research 2002;17(2):221‐37. [DOI] [PubMed] [Google Scholar]
Edwards 2006
- Edwards P, Roberts I, Green J, Lutchmun S. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333:119‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elkan 2000
- Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al. The effectiveness of domiciliary health visiting: A systematic review of international studies and a selective review of the British literature. Health Technology Assessment 2000;4(13):1‐339. [PubMed] [Google Scholar]
Elkington 1999
- Elkington J, Blogg S, Kelly J, Carey V. Head injuries in infants: A closer look at baby‐walkers, stairs and nursery furniture. New South Wales Public Health Bulletin 1999;10(7):82‐3. [Google Scholar]
Erdmann 1991
- Erdmann TC, Feldman KW, Rivara FP, Heimbach DM, Wall HA. Tap water burn prevention: the effect of legislation. Pediatrics 1991;88(3):572‐7. [PubMed] [Google Scholar]
Erens 2001
- Erens B, Primatesta P, Prior G, editors. Health survey for England ‐ the health of ethnic minority groups '99. London: The Stationery Office 2001. [Google Scholar]
Hayes 1999
- Hayes R, Bennett S. Simple sample size calculation for cluster‐randomized trials. International Journal of Epidemiology 1999;28(2):319‐26. [DOI] [PubMed] [Google Scholar]
Haynes 2003
- Haynes R, Reading R, Gale S. Household and neighbourhood risks for injury to 5‐14 year old children. Social Science & Medicine 2003;57(4):625‐36. [DOI] [PubMed] [Google Scholar]
Hippisley‐Cox 2002
- Hippisley‐Cox J, Groom L, Kendrick D, Coupland C, Webber E, Savelyich B. Cross sectional survey of socioeconomic variations in severity and mechanism of childhood injuries in Trent 1992‐7. BMJ 2002;324:1132‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
HIPRC 2005b
- Harborview Injury Prevention and Research Center. Best Practices ‐ Poisoning. Harborview Injury Prevention and Research Center Access date 8/11/05. [http://depts.washington.edu/hiprc/practices/topic/poisoning]
HIPRC 2005c
- Harborview Injury Prevention and Research Center. Best Practices ‐ Falls. Harborview Injury Prevention and Research Center Access date 8/11/05. [http://depts.washington.edu/hiprc/practices/topic/falls]
HIPRC 2005d
- Harborview Injury Prevention and Research Center. Best Practices ‐ Choking, Aspiration and Suffocation. Harborview Injury Prevention and Research Center Access date 8/11/05. [http://depts.washington.edu/hiprc/practices/topic/suffocation]
HIPRC 2005e
- Harborview Injury Prevention and Research Center. Best Practices ‐ Drowning. Harborview Injury Prevention and Research Center Access date 8/11/05. [http://depts.washington.edu/hiprc/practices/topic/drowning]
HIPRC 2005f
- Harborview Injury Prevention and Research Center. Best Practices ‐ Fire & Burns. Harborview Injury Prevention and Research Center Access date 8/11/05. [http://depts.washington.edu/hiprc/practices/topic/fireburns]
Kendrick 1994
- Kendrick D, Marsh P. The effectiveness of intervention programmes in reducing accidental injuries to children and young people. Report to Trent Regional Health Authority. Nottingham. University of Nottingham, 1994.
Kendrick 2000
- Kendrick D, Marsh P. Inequalities in receipt of injury prevention in primary care. Health Education Journal 2000;59:150‐6. [Google Scholar]
Kendrick 2005b
- Kendrick D, Mulvaney C, Burton P, Watson M. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Social Science & Medicine 2005;61(9):1905‐15. [DOI] [PubMed] [Google Scholar]
Kendrick 2006
- Kendrick D, Sutton A, Smith S, Mulvaney C, Woods A, Watson M, et al. Does the effect of home safety education, with or without the provision of safety equipment, differ by social group? Systematic review and meta‐analysis. Report to the Department of Health.
Klassen 2000
- Klassen TP, Mackay JM, Moher D, Walker A, Jones AL. Community‐based injury prevention interventions. The Future of Children 2000;10(1):83‐110. [PubMed] [Google Scholar]
Lambert 2002
- Lambert PC, Sutton AJ, Abrams KR, Jones DR. A comparison of summary patient‐level covariates in meta‐regression with individual patient data meta‐analysis. Journal of Clinical Epidemiology 2002;55(1):86‐94. [DOI] [PubMed] [Google Scholar]
Lyons 2003
- Lyons RA, Jones SJ, Deacon T, Heaven M. Socioeconomic variation in injury in children and older people: a population based study. Injury Prevention 2003;9(1):33‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mackay 1999
- Mackay M, Reid DC, Moher D, Klassen TP. A systematic review of the relationship between childhood injury and socio‐economic status. Health Canada and the CHEO Research Institute 1999.
Marshall 1998
- Marshall SW, Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts JD. Fatal residential fires: who dies and who survives?. Journal of the American Medical Association 1998;279(20):1633‐7. [DOI] [PubMed] [Google Scholar]
Moreno 2009
- Moreno S, Sutton AJ, Stanley T, Ades A, Abrams KR, Peters J, Cooper NJ. Comparison of methods to adjust for publication bias in meta‐analysis. BMC Medical Research Methodology 2009;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison 1999
- Morrison A, Stone DH, Doraiswamy N, Ramsay L. Injury surveillance in an accident and emergency department: a year in the life of CHIRPP. Archives of Disease in Childhood 1999;80(6):533‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nilsen 2004
- Nilsen P. What makes community‐based injury prevention work? In search of evidence of effectiveness. Injury Prevention 2004;10(5):268‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connor 2000
- O'Connor TG, Davies L, Dunn J, Golding J. Distribution of accidents, injuries, and illnesses by family type ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Pediatrics 2000;106(5):E68. [DOI] [PubMed] [Google Scholar]
ONS 2009
- Office for National Statistics. Child Mortality Statistics 2009: England and Wales. http://www.statistics.gov.uk/downloads/theme_health/child‐mortality/child_mort_stats_2009.pdf 2009. [Poisoning ‐ Series DH4 No. 28, London]
Overpeck 1997
- Overpeck MD, Jones DH, Trumble AC, Scheidt PC, Bijur PE. Socioeconomic and racial/ethnic factors affecting non‐fatal medically attended injury rates in US children. Injury Prevention 1997;3(4):272‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearson 2009
- Pearson M, Garside R, Moxham T, Anderson R. Accessed 14/05/2010. Preventing Unintentional Injuries Among Under ‐15s in the Home Report 1: Systematic reviews of effectiveness and cost‐effectiveness of home safety equipment and risk assessment schemes. http://www.nice.org.uk/nicemedia/live/11974/46010/46010.pdf 2009.
Peters 2008
- Peters J, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour enhanced meta‐analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61:991‐6. [DOI] [PubMed] [Google Scholar]
Petridou 1998
- Petridou E, Trichopoulos D, Mera E, Papadatos Y, Papazoglou K, Marantos A, et al. Risk factors for childhood burn injuries: a case‐control study from Greece. Burns 1998;24(2):123‐8. [DOI] [PubMed] [Google Scholar]
Pless 1993
- Pless B. The scientific basis of childhood injury prevention : A review of the medical literature. Child Accident Prevention Trust. London, 1993.
Pomerantz 2001
- Pomerantz WJ, Dowd MD, Buncher CR. Relationship between socioeconomic factors and severe childhood injuries. Journal of Urban Health 2001;78(1):141‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Popay 1993
- Popay J, Young A. Reducing accidental death and injury in children. North West Regional Health Authority. A report produced for North West Regional Health Authority Public Health Working Group on Child Accidents 1993.
Reading 1999
- Reading R, Langford IH, Haynes R, Lovett A. Accidents to preschool children: comparing family and neighbourhood risk factors. Social Science & Medicine 1999;48(3):321‐30. [DOI] [PubMed] [Google Scholar]
Reimers 2005
- Reimers A, Laflamme L. Neighbourhood social and socio‐economic composition and injury risks. Acta Paediatrica 2005;94(10):1488‐94. [DOI] [PubMed] [Google Scholar]
Riley 2008
- Riley RD, Lambert PC, Staessen JA, Wang J, Gueyffier F, Boutitie F. Meta‐analysis of continuous outcomes combining individual patient data and aggregate data. Statistics in Medicine 2008;27:1870‐93. [DOI] [PubMed] [Google Scholar]
Roberts 1996a
- Roberts I, Power C. Does the decline in child injury mortality vary by social class? A comparison of class specific mortality in 1981 and 1991. BMJ 1996;313:784‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberts 1996b
- Roberts I, Kramer M, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ 1996;312:29‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberts 1997
- Roberts I. Cause specific social class mortality differentials for child injury and poisoning in England and Wales. Journal of Epidemiology and Community Health 1997;51:334‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberts 1998
- Roberts I, DiGuiseppi C, Ward H. Childhood injuries: extent of the problem, epidemiological trends, and costs. Injury Prevention 1998;4 Suppl(4):10‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rucker 2008
- Rücker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta‐analyses with binary outcomes. Statistics in Medicine 2008;27:746‐63. [DOI] [PubMed] [Google Scholar]
Runyan 1992
- Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts J. Risk factors for fatal residential fires. New England Journal of Medicine 1992;327(12):859‐63. [DOI] [PubMed] [Google Scholar]
Scholer 1999
- Scholer SJ, Hickson GB, Ray WA. Sociodemographic factors identify US infants at high risk of injury mortality. Pediatrics 1999;103(6 pt 1):1183‐8. [DOI] [PubMed] [Google Scholar]
Sibert 1977
- Sibert JR. Child‐resistant packaging and accidental child poisoning. Lancet 1977;2(8032):189‐90. [DOI] [PubMed] [Google Scholar]
Smith 1995
- Smith T, Spiegelhalter D, Thomas A. Bayesian approaches to random‐effects meta‐analysis: A comparative study. Statistics in Medicine 1995;14:2685‐99. [DOI] [PubMed] [Google Scholar]
Speller 1995
- Speller V, Mulligan J, Law C, Foot B. Preventing injury in children and young people: a review of the literature and current practice. Wessex Institute of Public Health Medicine 1995.
Spinks 2004
- Spinks A, Turner C, McClure R, Nixon J. Systematic review of community based prevention programs targeting all injuries for children. Injury Prevention 2004;10(3):180‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spinks 2005
- Spinks A, McClure R, Turner C, Nixon J. The "WHO Safe Communities" model for the prevention of injury in whole populations. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD004445.pub2] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Sutton A, Ioannidis J, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta‐analysis of randomised controlled trials. BMJ 2011;1912(1):1345‐50. [DOI] [PubMed] [Google Scholar]
Sutton 2008
- Sutton AJ, Kendrick D, Coupland CAC. Meta‐analysis of individual‐ and aggregate‐level data. Statistics in Medicine 2008;27:651‐69. [DOI] [PubMed] [Google Scholar]
Ta 2006
- Ta VM, Frattaroli S, Bergen G, Gielen AC. Evaluated community fire safety interventions in the United States: a review of current literature. Journal of Community Health 2006;31(3):176‐97. [DOI] [PubMed] [Google Scholar]
Thompson 1998
- Thompson DC, Rivara F. Pool fencing for preventing drowning of children. Cochrane Database of Systematic Reviews 1998, Issue 1. [DOI: 10.1002/14651858.CD001047] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tobin 2002
- Tobin MD, Milligan J, Shukla R, Crump B, Burton PR. South Asian ethnicity and risk of childhood accidents: an ecological study at enumeration district level in Leicester. Journal of Public Health Medicine 2002;24(4):313‐8. [DOI] [PubMed] [Google Scholar]
Towner 1993
- Towner E, Dowswell T, Jarvis S. Reducing childhood accidents. The effectiveness of health promotion interventions: a literature review. Health Education Authority. London, 1993.
Towner 1996
- Towner E, Dowswell T, Simpson G, Jarvis S. Health promotion in childhood and young adolescence for the prevention of unintentional injuries. Health Education Authority. London, 1996.
Towner 2001
- Towner E, Dowswell T, Mackereth C, Jarvis S. What works in preventing unintentional injuries in children and young adolescents? An updated systematic review. London: Health Development Agency, 2001. [Google Scholar]
Towner 2002
- Towner E, Dowswell T. Community‐based childhood injury prevention interventions: what works?. Health Promotion International 2002;17(3):273‐84. [DOI] [PubMed] [Google Scholar]
Towner 2005
- Towner E, Dowswell T, Errington G, Burkes M, Towner J. Injuries in children aged 0‐14 years and inequalities. Health Development Agency. London, 2005.
Turner 2000
- Turner RM, Omar RZ, Yang M, Goldstein H, Thompson SG. A multilevel model framework for meta‐analysis of clinical trials with binary outcomes. Statistics in Medicine 2000;19(24):3417‐32. [DOI] [PubMed] [Google Scholar]
Turner 2004
- Turner C, Spinks A, McClure R, Nixon J. Community‐based interventions for the prevention of burns and scald in children. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD004335.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2011
- Turner S, Arthur G, Lyons RA, Weightman AL, Mann MK, Jones SJ, John A, Lannon S. Modification of the home environment for the reduction of injuries. Cochrane Database of Systematic Reviews 2011, Issue 2. [DOI: 10.1002/14651858.CD003600.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JA, Burney PG. Methods for evaluating area‐wide and organisation‐based interventions in health and health care: a systematic review. Health Technology Assessment 1999;3(5):92. [PubMed] [Google Scholar]
Unicef 2001
- Unicef. A league table of child deaths by injury in rich nations. Innocenti report card. Innocenti Research Centre, Florence February 2001, issue No 2.
van Weeghal 1997
- Weeghel I, Kendrick D, Marsh P. Accidental injury: risk and preventative interventions. Archives of Disease in Childhood 1997;77(1):28‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wadsworth 1983
- Wadsworth J, Burnell I, Taylor B, Butler N. Family type and accidents in preschool children. Journal of Epidemiology & Community Health 1983;37:100‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warda 1999
- Warda L, Tenenbein M, Moffatt ME. House fire injury prevention update. Part II. A review of the effectiveness of preventive interventions. Injury Prevention 1999;5(3):217‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2008
- World Health Organization and Unicef. World Report on Child Injury Prevention. http://whqlibdoc.who.int/publications/2008/9789241563574_eng.pdf 2008. [PubMed] [Google Scholar]
Wicklund 1984
- Wicklund K, Moss S, Frost F. Effects of Maternal Education, Age, and Parity of Fatal Infant Accidents. American Journal of Public Health 1984;74(10):1150‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeoh 2008
- Yeoh B, Woolfenden S, Wheeler DM, Alperstein G, Lanphear B. Household interventions for prevention of domestic lead exposure in children. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD006047.pub2] [DOI] [PubMed] [Google Scholar]


