Abstract
The COVID-19 pandemic has created unique challenges for family caregivers of children with developmental disabilities (DD). The purpose of this study was to conduct a 6-month follow-up on the experiences of caregiver burden and psychological distress among caregivers of children with autism (ASD) and/or attention deficit hyperactivity disorder (ADHD) during COVID-19 pandemic, compare their experiences to caregivers of children without DD, and test the interaction between opportunities for self-care and caregiver burden and psychological distress. Results indicated caregivers of children with ASD/ADHD continued to report significantly higher levels of psychological distress and caregiver burden compared to caregivers of children without DD. Counter to study hypotheses decreased opportunities to engage in self-care as a result of the pandemic predicted higher levels of psychological distress and caregiver burden for caregivers of children without DD, whereas only caregiver burden was moderated by self-care for caregivers of children with ASD/ADHD. Overall, the COVID-19 pandemic is continuing to negatively impact the psychological health of family caregivers of school-age children. In general, greater challenges are presented for caregivers of children with ASD/ADHD, but they seem to be more resilient to some COVID-19 challenges than caregivers of children without DD.
Keywords: COVID-19, Family caregivers, Children, Autism, ADHD, Developmental disabilities
What this paper adds?
As the COVID-19 pandemic persists, family caregivers of children with DD continue to experience higher anxiety, depression, stress, and caregiver burden than family caregivers of children without DD. Results support the need for focus on the psychological health of family caregivers, particularly those caring for children with Autism and/or Attention Deficit Hyperactivity Disorder given their additional psychological distress and burden, to ultimately support their self-care.
1. Introduction
The COVID-19 pandemic has had, and continues to have, substantial impact on the lives of individuals across the U.S. and globally. In addition to physical health and safety issues resulting from the novel coronavirus, increased psychological concerns are prevalent. Compared to reports from 2018 and 2019, adults from across the U.S. have reported a 17.4 % increase in symptoms of anxiety disorder, a 17.8 % increase in depression, and a 6.4 % increase in suicidal thoughts or ideation (Czeisler et al., 2020). These increases in negative psychological health indicators are troubling given the millions of children, particularly those with developmental disabilities (DD), who rely on these adults for assistance with health, education, and activities of daily living. Data from 2009 suggested almost 17 million adults serving as family caregivers for children under 18 with DD (National Alliance for Caregiving & AARP, 2009); estimates are likely higher today given increasing rates of children with DD (Zablotsky, Black, & Maenner, 2019) and new data suggesting an increase of over 4 million family caregivers of children under 18 since 2015 (AARP & National Alliance for Caregiving, 2020). Further, recent figures indicate that 61 % of all family caregivers are female (AARP & National Alliance for Caregiving, 2020), with previous data indicating even greater percentages (72 %) of family caregivers of children under the age of 18 with DD who identified as female (National Alliance for Caregiving & AARP, 2009). Given studies linking caregiver well-being to outcomes for children with DD (Clauser et al., 2020; Pinquart, 2018), the challenges resulting from the COVID-19 pandemic are particularly concerning for both the family caregiver as well as the child.
Demands associated with caregiving for any child, both expected and unexpected, have increased dramatically during the COVID-19 pandemic. For example, although a majority of parents supported closing schools in spring of 2020, caregivers also indicated challenges with balancing work, childcare, and remote learning; they also noted concern about their child falling behind academically and lack of motivation to actively participate in remote learning (Garbe, Ogurlu, Logan, & Cook, 2020). Mothers caring for school-age children have experienced a significantly greater reduction in work time than fathers as a result of the demands of caregiving and remote learning (Collins, Landivar, Ruppanner, & Scarborough, 2020). As recently noted by Adams and Todd (2020), the immediate and long-term success of children and families, along with the “health and economic recovery of businesses and employers, communities, states, and the country” (p. 1), depends in large part on helping family caregivers balance work and caregiving responsibilities.
Although there is critical need to support all family caregivers, particular attention should be directed to caregivers of children who have special needs. Children with DD may be at increased risk for regression in academic, social, emotional, and behavioral skills when typical services are altered, reduced, or removed (Frederick, Raabe, Rogers, & Pizzica, 2020). The individualized and specialized school-based supports provided to children with DD have been altered, reduced, or removed as a result of COVID-19, leaving family caregivers to fill service gaps.
During the first wave of COVID-19-related school closures in spring of 2020, family caregivers of children with DD were thrust into the role of the primary person responsible for facilitating their child’s education, including specialized support services (e.g., academic and behavioral interventions, speech/physical/occupational therapy services; Frederick et al., 2020). Family caregivers have experienced implementation challenges, noting issues such as accessibility of education and instructional materials as a result of school/teacher-related difficulties, internet access, and capacity to deliver support services (Garbe et al., 2020). Given these challenges, it might be expected that parenting stress has increased, particularly for those who are presented with substantial caregiving duties such as supporting moderate to severe child behavior challenges. Parenting stress, which has been defined as “distress or discomfort that results from demands associated with the role of parenting,” (p. 629, Hayes & Watson, 2013), is akin to caregiver burden, or “the extent to which caregivers perceive the adverse effect that caregiving has on their emotional, social, financial, and physical functioning” (Zarit et al., 1986). This is troublesome, as caregiver burden can lead to psychological distress, defined as “a state of emotional suffering typically characterized by symptoms of depression and anxiety,” (p. 687, Arvidsdotter et al., 2016).
Findings from an April 2020 survey of 407 family caregivers of school-aged children suggested that although all indicated challenges as a result of the pandemic, challenges were significantly greater among caregivers of children with DD, specifically autism (ASD) and attention-deficit/hyperactivity disorder (ADHD) with caregiver-reported moderate-to-severe behavior challenges, particularly with regard to psychological distress and caregiver burden (Chafouleas & Iovino, in press). In order to combat these negative psychological health effects, family caregivers need to engage in self-care, which includes activities aimed at promoting well-being such as exercise, getting enough sleep, eating a balanced diet, and leisure activities (Iovino, Chafouleas, Sanetti, & Gelbar, 2020). Unfortunately, self-care opportunities were a challenge for family caregivers of children with DD, such as ASD and ADHD, prior to the global pandemic (Chafouleas, Iovino, & Koriakin, 2020; Iovino et al., 2020). These pre-existing challenges with engaging in self-care present concerns for family caregivers’ ability to engage in self-care during the pandemic, and ultimately the personal well-being of family caregivers and their children. As such, understanding challenges among family caregivers is critical, particularly within the context of the COVID-19 pandemic, to inform strategies that can support caregiver psychological well-being.
The ongoing pandemic coupled with early findings of negative impact particularly for family caregivers of children with ASD and ADHD necessitate continued evaluation of the implications of COVID-19 for caregivers. Therefore, the purpose of this study was to (a) conduct a 6-month follow-up on the experience of caregiver burden and psychological distress among caregivers of children with ASD and ADHD during the COVID-19 pandemic, (b) compare their experiences to caregivers of children without DD, and (c) explore the interaction between self-reported opportunities for self-care and caregiver group on their caregiver burden and psychological distress. It was hypothesized that caregivers of children with ASD/ADHD would continue to experience more substantial negative impact on caregiver burden and psychological distress than caregivers of children without DD.
2. Methods
2.1. Participants and procedures
A total of 407 family caregivers completed a survey in April 2020 to better understand the impact of the COVID-19 pandemic on their psychological distress and caregiver burden, and differences between caregivers of children with ASD/ADHD with moderate-to-severe behavioral challenges and without DD were explored (see Chafouleas & Iovino, in press for more details). Between mid-September and mid-October 2020, a total of 352 caregivers completed the six-month follow-up survey sent via Qualtrics. Identical questions were included at both time points, with the exception that demographic questions were only asked at time one.
Item-level response checks were conducted to ensure the validity of participant responses given the survey was conducted online and direct identity checks were not possible. Participants were assigned unique identification numbers and responses to key items were checked for consistency over time. Two key validity check items were the number of children under their care and if participants indicated they lost a loved one as a result of COVID-19 at time one but not time two. Inconsistent responses across the two time points resulted in the exclusion of 15 participants from the final sample (n = 337).
Eligible participants were required to (a) be at least 18 years of age and (b) be a primary caregiver of a school-aged child (i.e., between the ages of 6 and 18). Two groups of caregivers were surveyed based on the time one inclusionary criteria. Caregivers in group one reported their child was diagnosed with ASD and/or ADHD and rated the child’s behavioral challenges as moderate or severe (referred to as caregivers of children with ASD/ADHD). Caregivers in group two indicated their child was not diagnosed with a developmental disability (referred to as caregivers of children without DD). The time two follow-up sample included 189 caregivers of a child with ASD/ADHD and 148 caregivers of a child without DD. Participants resided in 40 US states, 23 % lived in Connecticut, 15 % in California, 10 % in Florida, and between 4% and 0.3 % in the other 37 states. The majority of participants were female White/non-Hispanic parents who were married or in a domestic partnership and were between 35−44 years old with a college degree or higher (see Table 1 for demographics by group). Most were employed full-time, were the sole provider of care for their child, and lived in homes with an average of two adults. Among caregivers of a child with ASD/ADHD, most of their children were diagnosed with ASD, exhibited moderate behavioral challenges, identified as male, and their mean age was 11.07. See Table 1 for children’s demographics by group. Among caregivers of children without DD, the mean age of their children was 10.69 and 53 % identified as female. The majority of children without DD received hybrid school instruction in October (76 %), whereas the dominant instruction modality for children with ASD/ADHD was split between hybrid (36 %) and remote (43 %). Across both groups, more than 90 % of caregivers were primarily responsible for facilitation of remote and hybrid school instruction.
Table 1.
Participant and Child Characteristics by Group.
| Variable | Child With ASD/ADHD (N = 189) |
Child Without Disabilities (N = 148) |
||
|---|---|---|---|---|
| N | % | N | % | |
| Caregivers’ Characteristics | ||||
| Age | ||||
| 18−24 | 1 | .5 % | 0 | 0 % |
| 25−34 | 12 | 6.3 % | 18 | 12.9 % |
| 35−44 | 136 | 72.0 % | 85 | 57.4 % |
| 45−54 | 36 | 19.0 % | 36 | 24.3 % |
| 65−74 | 2 | 1.1 % | 1 | 0.7 % |
| Gender | ||||
| Male | 83 | 43.9 % | 40 | 27.0 % |
| Female | 105 | 55.6 % | 108 | 73.0 % |
| Race | ||||
| American Indian/Alaska Native | 4 | 2.1 % | 1 | 0.7 % |
| Asian | 8 | 4.2 % | 4 | 2.7 % |
| Black/African American | 23 | 12.2 % | 35 | 23.6 % |
| Pacific Islander/Native Hawaiian | 3 | 1.6 % | 0 | 0 % |
| White | 150 | 79.4 % | 105 | 70.9 % |
| Prefer not to say | 1 | 0.5 % | 0 | 0 % |
| Bi/Multi-Racial | 0 | 0 % | 3 | 2.0 % |
| Ethnicity | ||||
| Hispanic | 59 | 31.2 % | 37 | 25.0 % |
| Not Hispanic | 124 | 65.6 % | 111 | 75.0 % |
| Prefer not to say | 6 | 3.2 % | 0 | 0 % |
| Level of Education | ||||
| Less than high school | 1 | 0.5 % | 1 | 0.7 % |
| High school | 16 | 8.5 % | 13 | 8.2 % |
| Some college | 34 | 18.0 % | 25 | 16.5 % |
| 2-year degree | 26 | 13.8 % | 12 | 8.2 % |
| 4-year degree | 94 | 49.7 % | 32 | 22.0 % |
| Masters or greater | 18 | 9.5 % | 65 | 43.9 % |
| Income | ||||
| Less than $20,000 | 1 | 0.5 % | 2 | 1.4 % |
| $20,000−39,999 | 8 | 4.2 % | 9 | 6.1 % |
| $40,000−59,999 | 52 | 32.3 % | 31 | 20.9 % |
| $60,000-$79,999 | 58 | 30.7 % | 15 | 10.2 % |
| $80,000-$99,999 | 44 | 23.3 % | 23 | 15.5 % |
| $100,000 or greater | 25 | 13.2 % | 68 | 45.9 % |
| Marital Status | ||||
| Married/Domestic Partnership | 161 | 85.2 % | 31 | 88.5 % |
| Widowed | 15 | 7.9 % | 2 | 1.4 % |
| Divorced | 6 | 3.2 % | 9 | 6.1 % |
| Separated | 2 | 1.1 % | 1 | 0.7 % |
| Never Married | 3 | 1.6 % | 4 | 2.7 % |
| Other | 1 | 0.5 % | 1 | 0.7 % |
| Employment Status | ||||
| Full Time | 120 | 63.5 % | 77 | 52.0 % |
| Part Time | 25 | 13.2 % | 32 | 21.6 % |
| Retired | 2 | 1.1 % | 0 | 0 % |
| Student | 1 | 0.5 % | 1 | 0.7 % |
| Homemaker | 22 | 11.6 % | 12 | 8.1 % |
| Self-employed | 3 | 1.6 % | 7 | 4.7 % |
| Unemployed* | 15 | 7.9 % | 18 | 12.6 % |
| Unable to Work | 1 | 0.5 | 1 | 0.7 % |
| Sole Provider of Care for Child | ||||
| Yes | 151 | 79.9 % | 84 | 56.8 % |
| No | 38 | 20.1 % | 64 | 43.2 % |
| Who Shares Caregiving Responsibilities | ||||
| Spouse/Partner | 34 | 89.5 % | 59 | 92.2 % |
| Caregiver’s parent | 4 | 10.5 % | 4 | 6.3 % |
| Ex-Spouse/Co-Parent | 0 | 0 % | 1 | 1.6 % |
| Relationship to Child | ||||
| Parent | 177 | 93.7 % | 142 | 95.9 % |
| Grandparent | 5 | 2.6 % | 0 | 0 % |
| Guardian | 6 | 3.2 % | 6 | 4.1 % |
| Other | 1 | 0.5 % | 0 | 0 % |
| Child’s School Instruction Modality | ||||
| In-person | 40 | 21.2 % | 7 | 4.7 % |
| Hybrid | 68 | 36.0 % | 113 | 76.4 % |
| Remote | 81 | 42.9 % | 28 | 18.9 % |
| Primarily Responsible for Child’s Hybrid or Remote School Instruction** | ||||
| Yes | 146 | 98.0% | 131 | 92.9% |
| No | 3 | 2.0% | 10 | 7.1% |
| Children’s Characteristics | ||||
| Child Gender | ||||
| Male | 133 | 70.4 % | 68 | 45.9 % |
| Female | 55 | 29.1 % | 79 | 53.4 % |
| Non-Binary | 0 | 0 % | 1 | 0.7 % |
| Child Disability Diagnosis*** | ||||
| Autism Spectrum Disorder | 124 | 65.6% | N/A | – |
| Attention Deficit/Hyperactivity Disorder | 47 | 24.9% | N/A | – |
| Both | 18 | 9.5 % | N/A | – |
| Child Behavioral Challenges** | ||||
| Moderate | 161 | 85.2% | N/A | – |
| Severe | 28 | 14.8% | N/A | – |
| Child and Home Characteristics | M | SD | M | SD |
| Child Age | 11.07 | 2.31 | 10.69 | 2.30 |
| Number of children in care | 1.47 | 0.65 | 1.85 | 0.984 |
| Adults living in home | 2.33 | 0.77 | 1.95 | 0.49 |
Notes: *The ‘unemployed’ income category included unemployed not looking for work and unemployed looking for work. **If participants indicated their child received in-person school instruction they skipped the item about facilitation of remote and hybrid school instruction. ***Participants were asked if they were the primary caregiver of a child with a developmental disability and if they selected yes, they were asked to specify the diagnosis.
Participants read a study information sheet, agreed to voluntarily participate, and were informed they could skip items and discontinue the survey at any time. Participants’ completion of the follow-up survey was incentivized with a $15 gift card. Survey completion time was less than 30 min. Institutional review board approval was granted by the [University IRB blinded for review].
2.2. Measures
2.2.1. Demographic and COVID-19 impact survey
Demographic and COVID-19 exposure and impact survey items were created by the researchers. Participants completed 20 demographic items about themselves and one child between the ages of 6–18 and provided information about their family composition (see Table 1). Participants whose child was diagnosed with ASD/ADHD also identified their child’s diagnosis and their severity of behavioral challenges.
Participants responded to dichotomous items about the extent of their exposure to COVID-19. Five items were the focus of this study, which included whether the caregiver/family members inside or outside the home were infected, if they lost a loved one as a result of COVID-19, if the caregiver or an adult in the home was an essential worker, and if there was an outbreak in their community (coded 1 if present). Participants also rated the degree the pandemic impacted them and/or their families on five-point Likert scale (1 = not at all, 2 = slightly, 3 = somewhat, 4 = moderately, 5 = extremely). Six COVID-19 impact items were analyzed in this study, which included items about childcare resource availability, reduced or eliminated supports for their child’s specialized educational goals, loss of or reduced employment, increased financial strain, decreased opportunities for self-care, and inability to see friends and family as usual.
2.2.2. Depression anxiety and stress scales
Caregivers completed the short-version of the 21-item Depression Anxiety and Stress Scales which served as a measure of their psychological distress (DASS-21; Lovibond & Lovibond, 1995). The DASS-21 is a self-report measure comprised of three seven-item scales which measure depression, anxiety, and stress symptoms. Examples of depression items include dysphoria, hopelessness, lack of interest; anxiety items include physiological symptoms and feelings of panic and worry; and stress items include agitation, the tendency to overreact, and difficulty relaxing. Respondents rate their symptoms over the past week on a four-point frequency scale from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). Ratings are summed and then doubled to obtain total scores that range from 0 to 42, higher scores indicate greater symptom severity (Lovibond & Lovibond, 1995). The DASS-21 is a free measure that has been used to assess adult psychological distress following a traumatic event (e.g., Kerns et al., 2014). In our sample, scores on the three scales had adequate internal consistency at both time points (Cronbach’s alpha for stress = 0.79 and 0.78, depression = 0.86 and 0.82, and anxiety = 0.88 and 0.84 at times 1 and 2 respectively).
2.2.3. Burden scale for family caregivers
Caregivers completed a self-report scale of subjective caregiver burden, the 10-item short version of the Burden Scale for Family Caregivers (BSFC-s; Graessel, Berth, Lichte, & Grau, 2014). BSFC-s items measure stressful aspects of caregiving such as physical exhaustion, financial stress, relational stress, competing demands, loss of self, and life satisfaction. BSFC-s items are rated on a four-point scale from 0 (strongly disagree) to 3 (strongly agree), and total scores range from 0 to 30, with higher scores indicating higher levels of subjective burden (Graessel et al., 2014). The BSFC-s is free, available in 20 languages, and scores are related to caregivers’ self-reported strain, quality of life, depressive symptoms, and physical complaints (Pendergrass, Malnis, Graf, Engel, & Graessel, 2018). BSFC-s scores in this sample had adequate internal consistency at both time points (Cronbach’s alpha = 0.85 and 0.79 at times 1 and 2 respectively).
2.3. Data analysis
First, caregivers’ psychological distress and burden scores in April and October were compared to determine if there was a significant change between the two time points. Paired samples t-tests were conducted for each caregiver group. Second, caregivers’ October (time two) depression, anxiety, stress, and caregiver burden scores were separately analyzed in four multiple regressions to test the influence and relative importance of 16 variables on each outcome. Four demographic predictors included if the caregiver was the sole care provider for the children (coded 1 = yes), if the child was diagnosed with ASD or ADHD (coded 1 = yes), the caregiver’s educational level, and annual household income. Caregivers’ time one score on the outcome variable, measured in April, was controlled in each model (e.g., time one depression scores were controlled in the depression time two model, and time one caregiver burden scores were controlled in the caregiver time two model). Five COVID-19 exposure categorical predictors (all coded 1 = yes) included an outbreak in their community, if the caregiver or family member in the home was an essential worker, if a family member living outside their home was infected, if the caregiver or a family member in the home was infected, and if a loved one died due to COVID-19. Six COVID-19 impact predictors included decreased access to childcare resources, reduced or eliminated supports for the child’s specialized educational goals, loss of employment or reduction in hours, increased financial strain, decreased opportunities for self-care, and decreased ability to see friends and/or family as usual.
Third, one interaction term was tested to determine if the influence of decreased opportunities for self-care on each outcome was moderated by a child’s disability diagnosis. To test the interaction, the Likert-scale self-care variable was mean centered and multiplied by the dichotomous disability diagnosis variable to create a cross-product. Hierarchical (sequential) regressions were conducted, 16 predictors were entered in the first block and the interaction term was entered in the second step. The change in R 2 was examined to determine if the addition of the interaction term resulted in a statistically significant increase in variance explained. IBM SPSS version 26 was used to conduct all analyses and the small amount of missing data was handled with pairwise deletion.
3. Results
Descriptive statistics and sample sizes for all variables are presented by group in Table 2 . Scores on continuous and Likert-scale variables were approximately normally distributed (absolute skew ≤ 1 and kurtosis ≤ 2; Curran, West, & Finch, 1996). There were no concerns with multicollinearity (variance inflation factor < 3). Graphs of the standardized residuals verified the assumptions of linearity, homoscedasticity, and normally distributed errors. All regressions included 332 out of 337 participants.
Table 2.
Descriptive Statistics for Total Sample.
| Continuous Outcomes, T1 Measures, COVID-19 Impact Predictors | M (SD) | Skew | Kurtosis | n |
|---|---|---|---|---|
| Time 1 Anxiety Total Score | 14.34 (8.88) | −0.19 | −1.15 | 337 |
| Time 2 Anxiety Total Score | 14.62 (8.95) | −0.20 | −0.95 | 337 |
| Time 1 Depression Total Score | 15.95 (8.36) | −0.01 | −0.45 | 337 |
| Time 2 Depression Total Score | 15.84 (8.13) | −0.18 | −0.33 | 337 |
| Time 1 Stress Total Score | 18.80 (6.94) | 0.09 | 0.61 | 337 |
| Time 2 Stress Total Score | 18.71 (7.54) | −0.09 | 0.62 | 337 |
| Time 1 Caregiver Burden Total Score | 18.02 (5.06) | −0.69 | 0.63 | 337 |
| Time 2 Caregiver Burden Total Score | 18.34 (4.78) | −1.02 | 2.06 | 337 |
| Reduced Childcare Resources | 3.01 (1.19) | −0.13 | −0.75 | 337 |
| Reduced supports for child’s specialized educational goals | 2.91 (1.31) | −0.21 | −1.19 | 337 |
| Employment Loss or Reduction | 2.92 (1.39) | −0.06 | −1.22 | 335 |
| Increased Financial Strain | 3.16 (1.33) | −0.26 | −1.08 | 336 |
| Decreased Self-Care Opportunities | 3.41 (1.14) | −0.40 | −0.56 | 337 |
| Less Ability to See Friends/Family | 3.79 (0.92) | −0.38 | −0.45 | 334 |
| Dichotomous COVID-19 Exposure Predictors |
Present, coded 1 n (% of sample) |
|||
| Community-Wide Outbreak | 81 (24.0 %) | – | – | 337 |
| Essential Worker | 140 (41.5 %) | – | – | 337 |
| Family living outside the home infected | 86 (25.5 %) | – | – | 337 |
| Caregiver/family in home infected | 32 (9.5 %) | – | – | 337 |
| Loss of loved one from COVID-19 | 49 (14.5 %) | – | – | 337 |
Within the caregivers of children with ASD/ADHD group the paired sample t-tests were not statistically significantly different for April and October depression, anxiety, stress, and caregiver burden scores (see Table 3 for further details). Within the caregivers of children without DD group there was a statistically significant decrease between April and October depression scores (on average 1.82 points lower); the effect size was below the cut-off for a small effect (Cohen’s d = 0.184). Anxiety, stress, and caregiver burden scores were not statistically significantly different in April and October for those caring for children without DD. On average caregivers’ psychological distress and caregiver burden did not significantly change six months into the COVID-19 pandemic regardless of group membership.
Table 3.
Independent Samples t-tests.
| April Scores |
October Scores |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variables | M | SD | M | SD | t | df | p | Cohen’s d |
| ASD/ADHD group (n = 189) | ||||||||
| Caregiver Burden | 19.32 | 4.49 | 19.24 | 3.40 | 0.25 | 188 | 0.80 | 0.02 |
| Depression | 17.29 | 7.95 | 18.52 | 7.14 | −1.89 | 188 | 0.06 | −0.14 |
| Anxiety | 17.10 | 7.66 | 17.83 | 7.74 | −1.20 | 188 | 0.23 | −0.09 |
| Stress | 19.82 | 6.30 | 20.10 | 7.01 | −0.44 | 188 | 0.66 | −0.03 |
| No disabilities group (n = 148) | ||||||||
| Caregiver Burden | 16.35 | 5.26 | 17.18 | 5.91 | −1.37 | 147 | 0.17 | −0.11 |
| Depression | 14.24 | 8.58 | 12.42 | 8.06 | 2.25 | 147 | 0.03 | 0.19 |
| Anxiety | 10.81 | 9.11 | 10.51 | 8.74 | 0.36 | 147 | 0.72 | 0.03 |
| Stress | 17.50 | 7.49 | 16.95 | 7.85 | 0.65 | 147 | 0.52 | 0.05 |
The overall regression equations and the addition of the interaction term were statistically significant in all four models. Table 4, Table 5, Table 6, Table 7 display the full regression results including the unstandardized coefficients, unstandardized coefficients’ confidence intervals, standardized coefficients, and model summaries. The adjusted R 2 ranged from 18 % of the variance in stress to 49 % of the variance in anxiety explained by the set of predictors. Family caregivers of a child with ASD/ADHD had statistically significantly higher depression, anxiety, stress, and caregiver burden scores than those whose child did not have DD (ranging from 1.15 (caregiver burden) to 2.69 (depression) points higher; see Table 4, Table 5, Table 6, Table 7), even after controlling for the other 16 variables in the models. Caregivers who were the sole providers of care had significantly higher anxiety, depression, and caregiver burden scores; the effect size was moderate (Keith, 2019). Caregivers with lower education levels had significantly higher anxiety scores and those with lower household incomes had significantly higher depression scores (both were moderate effect sizes). Higher depression and anxiety scores in April predicted significantly higher depression and anxiety scores, respectively, in October (moderate effect sizes). For example, on average a one point higher anxiety or depression score in April predicted a 0.19−0.20 point higher anxiety or depression score in October, respectively, controlling for other variables in the model.
Table 4.
Anxiety regression results: Unstandardized coefficients and confidence intervals for unstandardized coefficients, standardized coefficients, p-values, model summaries.
| Predictors | b (S.E). | b 95% CI | β | p |
|---|---|---|---|---|
| Intercept | 5.89 (3.07) | −0.15, 11.93 | – | – |
| Child has ASD/ADHD* | 2.10 (0.86) | 0.41, 3.80 | 0.12 | .02 |
| Sole Provider* | 3.57 (1.02) | 1.57, 5.58 | 0.18 | .001 |
| Caregiver Education Level | −0.94 (0.31) | −1.56, -0.32 | −0.17 | <.01 |
| Household Income | 0.02 (0.18) | −0.34, 0.38 | 0.01 | .91 |
| Time 1 Anxiety Total Score | 0.19 (0.05) | 0.10, 0.28 | 0.19 | <.001 |
| Community-Wide Outbreak | 2.46 (0.96) | 0.58, 4.34 | 0.12 | .01 |
| Essential Worker | 1.30 (0.78) | −0.23, 2.83 | 0.07 | .10 |
| Family not in home infected | 1.33 (0.88) | −0.41, 3.07 | 0.07 | .13 |
| Caregiver/family in home infected | 2.52 (1.27) | 0.01, 5.03 | 0.08 | .05 |
| Loss of loved one from COVID-19 | 0.91 (1.13) | −1.31, 3.13 | 0.04 | .42 |
| Reduced Childcare Resources | 0.15 (0.35) | −0.54, 0.85 | 0.02 | .67 |
| Reduced supports for child’s specialized educational goals | 0.40 (0.34) | −0.27, 1.06 | 0.06 | .24 |
| Employment Loss or Reduction | 0.74 (0.35) | 0.05, 1.43 | 0.12 | .04 |
| Increased Financial Strain | 0.24 (0.36) | −0.48, 0.95 | 0.04 | .52 |
| Less Ability to See Friends/Family | −1.05 (0.44) | −1.92, -0.19 | −0.11 | .02 |
| Decreased Self-Care Opportunities | 1.23 (0.51) | 0.22, 2.24 | 0.16 | .02 |
| Interaction: Child has ASD/ADHD x Decreased Self-Care | −1.78 (0.64) | −3.05, -0.52 | −0.17 | <.01 |
Model Summary 1: F(16, 315) = 20.00, p < .001, Adj. R2 = 0.48.
Model Summary 2 (interaction added): F(17, 314) = 19.67, p < .001, Adj. R2 = 0.49.
Note: Statistically significant coefficients are bolded.
Table 5.
Depression Regression Results Unstandardized coefficients and confidence intervals for unstandardized coefficients, standardized coefficients, p-values, model summaries.
| Predictors | b (S.E). | b 95% CI | β | p |
|---|---|---|---|---|
| Intercept | 9.13 (3.05) | 3.12, 15.14 | – | – |
| Child has ASD/ADHD | 2.69 (0.83) | 1.05, 4.33 | 0.17 | .001 |
| Sole Provider | 2.73 (0.99) | 0.78, 4.68 | 0.15 | <.01 |
| Caregiver Education Level | −0.45 (0.31) | −1.06, 0.16 | −0.09 | .15 |
| Household Income | −0.49 (0.18) | −0.84, -0.13 | −0.16 | <.01 |
| Time 1 Depression Total Score | 0.20 (0.05) | 0.12, 0.29 | 0.21 | <.001 |
| Community-Wide Outbreak | −0.21 (0.94) | −2.05, 1.64 | −.01 | .83 |
| Essential Worker | 0.38 (0.76) | −1.12, 1.88 | 0.02 | .62 |
| Family not in home infected | 0.90 (0.87) | −0.81, 2.62 | 0.05 | .30 |
| Caregiver/family in home infected | 3.09 (1.25) | 0.62, 5.56 | 0.11 | .01 |
| Loss of loved one from COVID-19 | 0.37 (1.12) | −1.82, 2.57 | 0.02 | .74 |
| Reduced Childcare Resources | 0.05 (0.35) | −0.64, 0.73 | 0.01 | .90 |
| Reduced supports for child’s specialized educational goals | 0.15 (0.33) | −0.51, 0.80 | 0.02 | .66 |
| Employment Loss or Reduction | 0.53 (0.34) | −0.14, 1.21 | 0.09 | .12 |
| Increased Financial Strain | −0.04 (0.36) | −0.74, 0.66 | −0.01 | .91 |
| Less Ability to See Friends/Family | −1.06 (0.43) | −1.92, -0.21 | −0.12 | .02 |
| Decreased Self-Care Opportunities | 2.19 (0.51) | 1.20, 3.19 | 0.31 | <.001 |
| Interaction: Child has ASD/ADHD x Decreased Self-Care | −1.90 (0.63) | −3.14, -0.66 | −0.20 | <.01 |
Model Summary 1: F(16, 315) = 14.00, p < .001, Adj. R2 = 0.39.
Model Summary 2 (interaction added): F(17, 314) = 14.04, p < .001, Adj. R2 = 0.40.
Note: Statistically significant coefficients are bolded.
Table 6.
Stress Regression Results Unstandardized coefficients and confidence intervals for unstandardized coefficients, standardized coefficients, p-values, model summaries.
| Predictors | b (S.E). | b 95% CI | β | p |
|---|---|---|---|---|
| Intercept | 5.88 (3.37) | −0.75, 12.51 | – | – |
| Child has ASD/ADHD | 1.95 (0.90) | 0.17, 3.72 | 0.13 | .03 |
| Sole Provider | 1.03 (1.07) | −1.08, 3.14 | 0.06 | .34 |
| Caregiver Education Level | −0.62 (0.33) | −1.27, 0.04 | −0.13 | .07 |
| Household Income | −0.20 (0.19) | −0.59, 0.18 | −0.07 | .29 |
| Time 1 Stress Total Score | 0.10 (0.06) | −0.01, 0.21 | 0.09 | .08 |
| Community-Wide Outbreak | 0.58 (1.02) | −1.41, 2.58 | 0.03 | .57 |
| Essential Worker | 0.17 (0.83) | −1.46, 1.79 | 0.11 | .84 |
| Family not in home infected | −1.01 (0.94) | −2.86, 0.85 | −0.06 | .29 |
| Caregiver/family in home infected | 2.31 (1.36) | −0.36, 4.98 | 0.09 | .09 |
| Loss of loved one from COVID-19 | −1.69 (1.20) | −4.06, 0.67 | −0.08 | .16 |
| Reduced Childcare Resources | 0.19 (0.38) | −0.56, 0.93 | 0.03 | .62 |
| Reduced supports for child’s specialized educational goals | −0.48 (0.36) | −1.19, 0.23 | −0.08 | .19 |
| Employment Loss or Reduction | 0.26 (0.37) | −0.48, 1.00 | 0.05 | .49 |
| Increased Financial Strain | 0.39 (0.39) | −0.37, 1.16 | 0.07 | .32 |
| Less Ability to See Friends/Family | 0.55 (0.47) | −0.38, 1.47 | 0.07 | 0.24 |
| Decreased Self-Care Opportunities | 3.06 (0.55) | 1.98, 4.13 | 0.46 | <.001 |
| Interaction: Child has ASD/ADHD x Decreased Self-Care | −3.24 (0.69) | −4.59, -1.89 | −0.37 | <.001 |
Model Summary 1: F(16, 315) = 4.02, p < .001, Adj. R2 = 0.13.
Model Summary 2 (interaction added): F(17, 314) = 5.35, p < .001, Adj. R2 = 0.18.
Note: Statistically significant coefficients are bolded.
Table 7.
Caregiver Burden Regression Results Unstandardized coefficients and confidence intervals for unstandardized coefficients, standardized coefficients, p-values, model summaries.
| Predictors | b (S.E). | b 95% CI | β | p |
|---|---|---|---|---|
| Intercept | 3.12 (1.77) | −0.35, 6.60 | – | – |
| Child has ASD/ADHD | 1.15 (0.48) | 0.22, 2.09 | 0.12 | .02 |
| Sole Provider | 1.42 (0.55) | 0.33, 2.51 | 0.14 | .01 |
| Caregiver Education Level | −0.29 (0.17) | −0.63, 0.5 | −0.10 | .10 |
| Household Income | 0.00 (0.10) | −0.20, 0.20 | 0.00 | .98 |
| Time 1 Burden Total Score | 0.08 (0.04) | −0.01, 0.16 | 0.08 | .08 |
| Community-Wide Outbreak | −1.18 (0.53) | −2.21, -0.14 | −0.11 | .03 |
| Essential Worker | 0.32 (0.43) | −0.52, 1.16 | 0.03 | .45 |
| Family not in home infected | −0.54 (0.49) | −1.51, 0.41 | −0.05 | .26 |
| Caregiver/family in home infected | −1.45 (0.70) | −2.84, -0.07 | −0.09 | .04 |
| Loss of loved one from COVID-19 | −0.17 (0.62) | −1.40, 1.05 | −0.01 | .78 |
| Reduced Childcare Resources | 0.64 (0.20) | 0.25, 1.02 | 0.16 | <.01 |
| Reduced supports for child’s specialized educational goals | 0.61 (0.19) | 0.24, 0.99 | 0.17 | <.01 |
| Employment Loss or Reduction | 0.17 (0.19) | −0.21, 0.55 | 0.05 | .39 |
| Increased Financial Strain | 0.62 (0.20) | 0.22, 1.01 | 0.17 | <.01 |
| Less Ability to See Friends/Family | 0.50 (0.24) | 0.02, 0.98 | 0.10 | .04 |
| Decreased Self-Care Opportunities | 1.74 (0.28) | 1.18, 2.29 | 0.41 | <.001 |
| Interaction: Child has ASD/ADHD x Decreased Self-Care | −1.31(0.36) | −2.01, -0.61 | −0.23 | <.001 |
Model Summary 1: F(16, 315) = 16.85, p < .001, Adj. R2 = 0.43.
Model Summary 2 (interaction added): F(17, 314) = 17.30, p < .001, Adj. R2 = 0.46.
Note: Statistically significant coefficients are bolded.
In terms of COVID-19 exposure, a COVID-19 infection among caregivers or another family member in their homes predicted significantly higher depression scores, but significantly lower caregiver burden (small effect sizes). Caregivers living in communities with COVID-19 outbreaks had significantly higher anxiety, but lower caregiver burden (moderate effect sizes, see Table 4, Table 5, Table 6, Table 7).
A stronger impact of COVID-19 on families’ inability to see friends and family as usual predicted significantly higher caregiver burden, but lower anxiety and depression scores; effect sizes were moderate. A stronger impact of COVID-19 on the availability of childcare resources and supports for children’s specialized educational goals predicted significantly higher caregiver burden scores (moderate effect sizes). A stronger impact of COVID-19 on loss of employment or reduced work hours predicted significantly higher anxiety scores (moderate effect, see Table 4, Table 5, Table 6, Table 7).
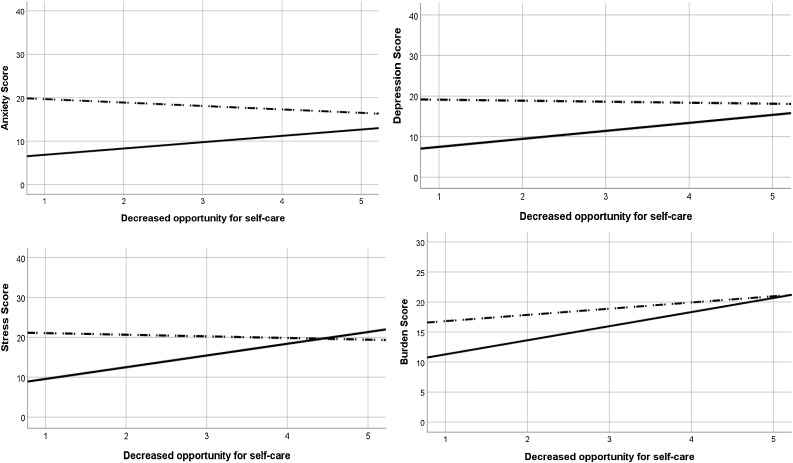
The relation of decreased opportunities for self-care impacted by COVID-19 on anxiety, depression, stress, and caregiver burden was significantly moderated by whether caregivers had a child with ASD/ADHD (Δ Adj. R 2 = 0.01 (anxiety and depression), 0.03 (burden), 0.05 (stress)), after controlling for all variables in the models. The four statistically significant interactions are graphed in Fig. 1 and separate regressions were run for each group to test the statistical significance of self-care on each outcome. Counter to study hypotheses, stronger impacts of COVID-19 on decreased opportunities for self-care significantly increased anxiety, depression, and stress scores for those whose children were not diagnosed with DD, but the influence was not significant for caregivers whose children had ASD/ADHD (without DD ranges: (F(1, 146) = 5.40–32.22, p < .001–.02, Adj. R 2 = 0.03 – 0.18; with ASD/ADHD ranges: F(1, 187) = 0.30–2.58, p = .11–.59, Adj. R 2 = -0.00 – 0.01). The influence on caregiver burden was significant for both groups but appeared stronger for caregivers of children without DD (see Fig. 1; without DD: F(1, 146) = 37.22, p < .001, Adj. R 2 = 0.20; with ASD/ADHD: F(1, 187) = 25.63, p < .001, Adj. R 2 = 0.12).
Fig. 1.
Interaction graphs. The dashed lines represent caregivers of children with ADHD/ASD and the solid lines represent caregivers of children without a developmental disability.
4. Discussion
Results of this follow-up study contribute to our understanding of the ongoing impact of the COVID-19 pandemic on caregivers of school-age children in the U.S. This study expands upon findings from early in the pandemic by offering a 6-month follow-up on the psychological health of family caregivers of children with ASD/ADHD and without DD. Six months into the pandemic, caregivers of children with ASD/ADHD who exhibit moderate to severe behavioral challenges scored higher than those of children without DD on measures of anxiety, depression, stress, and caregiver burden. These findings are consistent with pre-pandemic reports that parents of children with ASD report higher levels of psychological distress and caregiver burden (e.g., Hayes & Watson, 2013; Keenan, Newman, Gray, & Rinehart, 2016), along with findings from earlier in the pandemic (e.g., Chafouleas & Iovino, in press).
In terms of psychological distress and caregiver burden, for all caregivers, being the sole provider of care for their child(ren) significantly predicted higher levels of depression, anxiety, and burden. This is consistent with findings from before the pandemic suggesting that single parents experience greater challenges as a result of caregiving (Berryhill & Durtschi, 2017). Lower education levels and loss of employment as a result of the pandemic significantly influenced level of anxiety for all caregivers, whereas annual household income significantly influenced level of depression. Results are also consistent with results from before the COVID-19 pandemic which indicate that parenting stress, which relates to psychological distress, is highest among family caregivers of low socioeconomic status (Parkes, Sweeting, & Wight, 2015).
With respect to self-care, indication of a greater negative impact of decreased opportunities for self-care due to COVID-19 predicted significantly higher depression, anxiety, stress, and caregiver burden for caregivers whose children were not diagnosed with ASD/ADHD. Inconsistent with our hypothesis, decreased opportunities to engage in self-care did not significantly predict depression, anxiety, or stress for caregivers of children with ASD/ADHD. Decreased opportunities for self-care, however, did predict higher caregiver burden. Caregiver appraisals of their ability to engage in self-care have varied, with some findings indicating that caregiving restricts the perceived ability to engage in self-care and thus leading to higher levels of reported symptoms of anxiety and depression, and others indicating that caregiving responsibilities have not correlated with reduced time for aspects of self-care (Pope, Giger, Lee, & Ely, 2017). It is possible that similar variations in caregiver appraisal of ability to engage in self-care occurred in the current study. That is, caregivers of children with ASD/ADHD already struggled to engage in self-care prior to COVID-19 (Chafouleas et al., 2020; Iovino et al., 2020). As such, it is possible that the pandemic has not impacted perceived ability to engage in self-care over and above typical circumstances, or has been relatively less compared to other factors.
For all caregivers, a greater inability to see friends and family as typical predicted lower levels of depression and anxiety. This is inconsistent with other findings, as prior work has indicated that lower levels of perceived social support are associated with higher levels of psychological distress (George, Kecmanovic, Meade, & Kolt, 2020). As such, it is possible that although caregivers reported an impact on their ability to see friends and family as typical, their perception of social support was not impacted. Regarding COVID-19 exposure, the impact of a community-wide outbreak and the caregiver themselves or a family member living in the home becoming infected with the virus resulted in higher levels of anxiety and depression and lower levels of caregiver burden. Level of stress was significantly influenced by caregiver group (i.e., caring for a child with or without ASD/ADHD) and by an interaction with decreased opportunities to engage in self-care, but was least influenced by predictors compared to other indicators of psychological distress and caregiver burden.
There are limitations to consider when interpreting the current findings. For one, our sample of caregivers identified as mostly White, highly educated, and having income levels well above the U.S. poverty line. This lack of socioeconomic and racial diversity is of particular concern given the COVID-19 pandemic has had a disproportionately negative impact on minoritized individuals, particularly Black Americans (Cyrus et al., 2020). Further, outside of the context of COVID-19, Black and Latinx families of children with ASD have indicated greater barriers to accessing self-care outlets (Iadarola, Perez-Ramos, Smith, & Dozier, 2019). Thus, our findings should not be generalized across all family caregiver populations. In addition, as with all research studies based on self-report measures, participant responses may have been subject to response distortion such as social desirability bias or survey comprehension difficulties, thus potentially impacting the validity of study findings. Finally, caregivers’ reports were relied on for children’s diagnoses and the severity of their behavioral challenges, thus, validity was not verified. Future research may incorporate additional measures or reporters. Given the ongoing nature of the COVID-19 pandemic, future research could continue to explore the impact of COVID-19 on various outcomes (e.g., personal well-being, self-care, academic/occupational) on the child, family, and caregiver levels. The influence of the COVID-19 pandemic will likely continue well beyond the pandemic’s resolution, and follow-up studies at various intervals may reveal a host of long-term consequences.
4.1. Conclusions
Six months into the COVID-19 pandemic, family caregivers of children with ASD/ADHD reported continuing to experience higher anxiety, depression, stress, and caregiver burden than those without DD. Fewer opportunities for self-care during COVID-19 were related to higher psychological distress among caregivers of children without DD, but no significant relation was found for caregivers of children with ASD/ADHD, which is inconsistent with study hypotheses. Decreased opportunities for self-care predicted higher caregiver burden for all caregivers, especially for those caring for children without DD. Overall, our results highlight the importance of supporting caregivers’ psychological health, particularly those caring for children with ASD/ADHD given the additional psychological distress and burden they reported.
Funding
This study was approved by the University of Connecticut HS-IRB and is funded by a seed grant from the University of Connecticut’s Institute for Collaboration on Health, Intervention, and Policy (InCHIP).
CRediT authorship contribution statement
Emily A. Iovino: Conceptualization, Funding acquisition, Investigation, Writing - original draft, Writing - review & editing. Jacqueline Caemmerer: Formal analysis, Writing - original draft, Writing - review & editing. Sandra M. Chafouleas: Conceptualization, Funding acquisition, Investigation, Supervision, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
No. of reviews completed is 2
References
- AARP, National Alliance for Caregiving . AARP; Washington, DC: 2020. Caregiving in the United States 2020. (May) [DOI] [Google Scholar]
- Adams G., Todd M. Meeting the School-Age Child Care Needs of Working Parents Facing COVID-19 Distance Learning: Policy Options to Consider. Urban Institute; 2020. https://bettercarenetwork.org/sites/default/files/2020-07/meeting-the-school-age-child-care-needs-of-working-parents-facing-covid-19-distance-learning.pdf (July) Retrieved from: [Google Scholar]
- Arvidsdotter T., Marklund B., Kylén S., Taft C., Ekman I. Understanding persons with psychological distress in primary health care. Scandinavian Journal of Caring Sciences. 2016;30:687–694. doi: 10.1111/scs.12289. [DOI] [PubMed] [Google Scholar]
- Berryhill M.B., Durtschi J.A. Understanding single mothers’ parenting stress trajectories. Marriage & Family Review. 2017;53:227–245. doi: 10.1080/01494929.2016.1204406. [DOI] [Google Scholar]
- Chafouleas S.M., Iovino E.A., Koriakin T.A. Caregivers of children with developmental disabilities: Exploring perceptions of health-promoting self-care. Journal of Developmental and Physical Disabilities. 2020 doi: 10.1007/s10882-019-09724-x. [DOI] [Google Scholar]
- Chafouleas, S.M., & Iovino, E.A. (in press). Comparing the initial impact of COVID-19 on burden and psychological distress among family caregivers of children with and without developmental disabilities. School Psychology Quarterly. [DOI] [PubMed]
- Clauser P., Ding Y., Chen E.C., Cho S., Wang C., Hwang J. Parenting styles, parenting stress, and behavioral outcomes in children with autism. School Psychology International. 2020 doi: 10.1177/0143034320971675. [DOI] [Google Scholar]
- Collins C., Landivar L.C., Ruppanner L., Scarborough W.J. COVID-19 and the gender gap in work hours. Gender, Work & Organization. 2020 doi: 10.1111/gwao.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran P.J., West S.G., Finch J.F. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1996;1:16–29. doi: 10.1037/1082-989X.1.1.16. [DOI] [Google Scholar]
- Cyrus E., Clarke R., Hadley D., Bursac Z., Trepka M.J., Devieux J.G., et al. The impact of COVID-19 on African American communities in the United States. Health Equity. 2020;4 doi: 10.1089/heq.2020.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. Center for Disease Control and Prevention Morbidity and Mortality Weekly Report. 2020;69(August (32)):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederick J.K., Raabe G.R., Rogers V.R., Pizzica J. Advocacy, collaboration, and intervention: A model of distance special education support services amid COVID-19. Behavior Analysis in Practice. 2020;13:748–756. doi: 10.1007/s40617-020-00476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbe A., Ogurlu U., Logan N., Cook P. COVID-19 and remote learning: Experiences of parents with children during the pandemic. American Journal of Qualitative Research. 2020;4:45–65. doi: 10.29333/ajqr/8471. [DOI] [Google Scholar]
- George E.S., Kecmanovic M., Meade T., Kolt G.S. Psychological distress among carers and the moderating effects of social support. BMC Psychiatry. 2020;20(154) doi: 10.1186/s12888-020-02571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graessel E., Berth H., Lichte T., Grau H. Subjective caregiver burden: Validity of the 10-item short version of the Burden Scale for Family Caregivers BSFC-s. BMC Geriatrics. 2014;14 doi: 10.1186/1471-2318-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S.A., Watson S.L. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(3):629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Iadarola S., Perez-Ramos J., Smith T., Dozier A. Understanding stress in parents of children with autism spectrum disorder: A focus on under-represented families. International Journal of Developmental Disabilities. 2019;65:20–30. doi: 10.1080/20473869.2017.1347228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iovino E.A., Chafouleas S.M., Sanetti L.M.H., Gelbar N. 2020. Mixed methods pilot evaluation of a Facebook group self-care intervention for primary caregivers of children with developmental disabilities. Manuscript submitted for publication. [Google Scholar]
- Keenan B.M., Newman L.K., Gray K.M., Rinehart N.J. Parents of children with ASD experience more psychological distress, parenting stress, and attachment-related anxiety. Journal of Autism and Developmental Disorders. 2016;46(9):2979–2991. doi: 10.1007/s10803-016-2836-z. [DOI] [PubMed] [Google Scholar]
- Keith T.Z. Multiple regression and beyond: An introduction to multiple regression and structural equation modeling (3rd ed.) Routledge. 2019 [Google Scholar]
- Lovibond S.H., Lovibond P.F. Psychology Foundation.; Sydney: 1995. Manual for the depression anxiety stress scales. [Google Scholar]
- National Alliance for Caregiving, AARP . National Alliance for Caregiving; Washington, DC: 2009. Caregivers of children: A focused look at those caring for a child with special needs under the age of 18.https://www.caregiving.org/wp-content/uploads/2020/05/Report_Caregivers_of_Children_11-12-09.pdf (November) Retrieved from. [Google Scholar]
- Parkes A., Sweeting H., Wight D. Parenting stress and parent support among mothers with high and low education. Journal of Family Psychology. 2015;29:907–918. doi: 10.1037/fam0000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendergrass A., Malnis C., Graf U., Engel S., Graessel E. Screening for caregivers at risk: Extended validation of the short version of the Burden Scale for Family Caregivers (BSFC-S) with a valid classification system for caregivers caring for an older person at home. BMC Health Services Research. 2018;18:229. doi: 10.1186/s12913-018-3047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M. Parenting stress in caregivers of children with chronic physical condition: A meta-analysis. Stress and Health. 2018;34:197–207. doi: 10.1002/smi.2780. [DOI] [PubMed] [Google Scholar]
- Pope N., Giger J., Lee J., Ely G. Predicting personal self-care in informal caregivers. Social Work in Health Care. 2017;56:822–839. doi: 10.1080/00981389.2017.1344755. [DOI] [PubMed] [Google Scholar]
- Zablotsky B., Black L., Maenner M., et al. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics. 2019;144(4) doi: 10.1542/peds.2019-0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit S.H., Todd P.A., Zarit J.M. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26:260–266. doi: 10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]