Abstract
This study adopts a public value perspective to examine the eHealth services deployed by national and regional governments to contain the coronavirus (Covid-19) pandemic, including symptoms checkers, information portals and contact-tracing applications. We analyse 50 cases of eHealth applications adopted in 25 European Economic Area (EEA) and outline how these systems and technologies map against four dimensions of public value: user orientation, participation, legality and equity. Our findings reveal that the public value of the eHealth applications adopted in the context of the current pandemic is affected by both endogenous and exogenous factors that undermine their ability to improve the quality of healthcare services and social wellbeing. We conclude by suggesting areas for further research to address such factors and the trade-offs emerging between different dimensions of public value.
Keywords: eHealth applications, European Economic Area, Contact-tracing, Covid-19, Pandemic, Public value
1. Introduction
The coronavirus (Covid-19) pandemic has spread across the globe with over 100 million confirmed cases and over 2.4 million deaths (at the time of writing). Covid-19 pandemic has put a huge strain on national health services and the global economy. To better control Covid-19 contagion and improve the delivery of healthcare services, the use of eHealth applications has been advocated by researchers and policymakers (UCLG, 2020; WHO, 2020; Ye, Zhou, & Wu, 2020).
eHealth here refers to a wide range of e-government applications that use information and communication technologies (ICT) in the context of healthcare services (Oh, Rizo, & Enkin, 2005; WHO, 2020). Contact-tracing apps (CTAs), symptoms checkers and information portals are some examples of how eHealth can be deployed during a pandemic (Kretzschmar et al., 2020; Kristensen & Ruckenstein, 2018; Savona, 2020; Storeng & de Bengy Puyvallée, 2021). Many of these applications have been adopted worldwide by local and national governments (eHealth Network, 2020, Hakmeh, Taylor, Peters, & Ignatidou, 2021; Kummitha, 2020), in collaboration with public healthcare and private technology providers. For example, in the UK, NHS Covid-19 app has been downloaded over 1.7 million times and prevented 600,000 infections (Bradshaw & Venkataramakrishnan, 2021; Kelion, 2021).
Despite their potential contribution to curtailing Covid-19 contagion, these eHealth applications have attracted numerous criticisms. For example, the deployment of CTAs has been opposed by those fearing that such short-term strategy could lead to a permanent state surveillance using personal data (Ferguson et al., 2020; Gasser, Ienca, Scheibner, Sleigh, & Vayena, 2020; Hakmeh et al., 2021; Kristensen & Ruckenstein, 2018). In addition, scholars have also highlighted the lack of accessibility of these applications by vulnerable members of the society (McDonald, 2020; Savona, 2020). Overall, the debate and implementation of eHealth applications has been dominated by two opposing views. According to a techno-driven approach, the advantages of smart technologies justify their top-down imposition onto citizens. Conversely, the human-driven approach to smart technologies values the engagement of citizens in the development and implementation of eHealth applications (Kummitha, 2020). These opposing views reflect different conceptions of technology as well as the ongoing trade-off between individual rights and public interest that has become evident after the imposition of restrictive measures to mitigate the impact of Covid-19 pandemic (van Kolfschooten & de Ruijter, 2020).
This paper aims to contribute to the ongoing debate on the implementation of eHealth applications in the context of a pandemic, by adopting a public value perspective (Moore, 1995). Public value theory has been widely employed to assess e-Government services, of which eHealth applications represent a specific variant (Scott, DeLone, & Golden, 2016; Twizeyimana & Andersson, 2019). Drawing upon public value theory, we developed a conceptual framework that encompasses both utilitarian and social benefits expected from the use of ICT in healthcare sector. This framework is applied to analyse the eHealth applications adopted within the European Economic Area (EEA) to provide a comprehensive overview of the human-driven approaches to eHealth adopted in Western countries in tackling Covid-19 pandemic.
Our qualitative comparison explores the features and functions of these applications to map the different strategies adopted so far and assess whether they are effectively designed to deliver and maximise public value. By focusing on both utilitarian and social benefits of eHealth applications, our analysis also sheds light on the potential trade-offs between individual rights and public interest emerging from the use of smart technologies in the context of reimagining healthcare strategies in a society that is increasingly becoming digitalised.
Our paper is structured as follows: the concept of public value and the analytical framework used in this paper are discussed in Section 3 after a brief review of the debate on eHealth services in the context of Covid-19 pandemic (Section 2). Section 4 briefly details the methodology employed for the case study. Our analysis and findings are outlined in Section 5 followed by the discussion in Section 6. Section 7 then concludes with a set of recommendations for policymakers and future research.
2. eHealth applications in the context of a pandemic
eHealth is a type of e-government application, encompassing a wide range of devices and services that employ ICT to assist and enhance the provision of healthcare (Oh et al., 2005). ICT has long been used in the healthcare sector to facilitate access to medical information and patients' data through, for example, online portals and smartcards. More recently, new digital technologies such as wearables and artificial intelligence have emerged as a potential gamechanger in the delivery of healthcare services (Firouzi et al., 2018).
The extant literature has long emphasised the scope for using ICT to tackle health crises. For example, Li et al. (2012) stressed the importance of organisational preparedness in the development and adoption of eHealth services to deal with an influenza pandemic, while Timpka et al. (2014) explored the potential of eHealth systems to improve the surveillance of infectious diseases. More recently, CTAs, using location data from smartphones to trace people who may have been in contact with infected patients, have been presented as a powerful tool to mitigate the inefficiency of traditional contact-tracing and minimise the spread of Covid-19 (Arakpogun, Elsahn, Prime, Gerli, & Olan, 2020; Kretzschmar et al., 2020). Furthermore, since Covid-19 was declared a pandemic, many governments in East Asian and European countries have invested in eHealth applications to manage various aspects of Covid-19. For example, alongside CTAs, symptoms checkers have been developed to help citizens to monitor their health conditions and early detection of Covid-19 cases. Various portals and apps have also been launched to disseminate information on the pandemic (eHealth Network, 2020; Storeng & de Bengy Puyvallée, 2021), while some governments in East Asia have used smartphone apps and wearables to monitor the location of patients and enforce lockdown measures (Hernández-Orallo, Manzoni, Calafate, & Cano, 2020; WHO, 2020).
Whereas East Asia countries have followed a top-down and techno-driven approach that resulted into the adoption of eHealth applications to curtail the spread of Covid-19, their use in western democracies has been at the centre of public debate for several months (Kummitha, 2020; Ye et al., 2020). Concerns have been raised over the implications of eHealth applications for data protection as these technologies record, transmit and store a wide range of personal data, including patient medical information and the movement of users and non-users (Savona, 2020; van Kolfschooten & de Ruijter, 2020). Furthermore, it has been highlighted how inequalities in the access to connectivity and the lack of digital literacy may hamper the ability of certain social groups to take advantage of these applications (Arakpogun et al., 2020; McDonald, 2020; Savona, 2020). Thereby, exacerbating stigma against marginalised groups (such as migrants), and disproportionally affecting certain individuals that are already disadvantaged, including those unable to work from home (Davis, 2020; Klenk & Duijf, 2020).
In their review of the current debate on the use of digital technologies to contain the spread of Covid-19, Savona (2020) highlighted the need for a more articulated and comprehensive reflection on the use of eHealth in the context of a pandemic. Indeed, previous studies have explored the implications of eHealth applications from a purely theoretical and conceptual standpoint, highlighting potential drawbacks and shortcoming in the design and implementation of eHealth strategies in response to the outbreak of Covid-19 (Arakpogun et al., 2020).
While an empirical evaluation of the effects of eHealth applications in the current pandemic is not yet feasible given the fluidity of events, this paper aims to expand the research on this topic by mapping the strategies adopted across the EEA and assessing whether they are effectively designed to create public value. The latter provides a comprehensive sample of the eHealth initiatives adopted by Western democracies, thereby shedding light on the implications of the human-driven approach followed by these countries in the context of the current pandemic (Kummitha, 2020).
As explained in the following section, these case studies are assessed against several dimensions of public value, that reflect both the utilitarian and social benefits of eHealth applications. This approach is expected to produce a comprehensive understanding of the actual design and implementation of eHealth strategies, thereby overcoming some of the limitations identified in the extant research (Savona, 2020). Furthermore, the theory of public value provides a solid framework to explore the potential trade-off emerging between individual rights and public interest when smart technologies are used to contain the spread of a pandemic (Kummitha, 2020; van Kolfschooten & de Ruijter, 2020).
3. Public values, ICT and healthcare
The evaluation of ICT use in organisations is a central topic in the information systems (IS) literature (Rose, Persson, Heeager, & Irani, 2015), but most of the frameworks that evaluate IS are underpinned by market logic, thereby emphasising values such as profitability and efficiency (Grimsley & Meehan, 2007). These models are less applicable to study the implementation of IS within the public sector (Frisk, Bannister, & Lindgren, 2015), where the use of ICT goes beyond the narrow focus of profitability to include the achievement of social and political goals (Rose et al., 2015).
Consistently, the analysis of e-government services, which are designed to achieve public interest rather than commercial purposes, has often been based on the theory of public value (Twizeyimana & Andersson, 2019). As Moore (2000, p.186) argues, value, as understood in the public domain, is about “the achievement of the political mandated mission of the organization and the fulfilment of the citizen aspiration that was more or less reliably reflected in that mandate”. Accordingly, from a public value perspective, the evaluation of public services goes beyond the focus on efficiency and effectiveness to encompass a wider range of values, which also reflect the contribution of the public sector to society and democracy (Bryson, Crosby, & Bloomberg, 2014; Jørgensen & Bozeman, 2007). By creating public value, e-government services are expected to both generate net benefits for the end-users and enhance the relationship between citizens and governments (Grimsley & Meehan, 2007; Seltsikas & O'Keefe, 2010). Consequently, e-government has been assessed against its ability to generate both tangible (e.g., cost savings) and intangible outcomes (e.g., social inclusion) (Scott et al., 2016).
The perspective of public value has also been applied to analyse eHealth services, which are e-government services employing ICT for the delivery of healthcare information and services to citizens. Bend (2004) measured the public value of eHealth applications against the achievement of desired outcomes and the level of trust between citizens and healthcare providers. Svejvig, Schlichter, and Andersen (2012) adopted a broader perspective and considered how eHealth also affects the perceived quality of healthcare services among patients and employees. Other scholars have also argued that the evaluation of eHealth services should integrate the view of public value with that of social justice and include dimensions such as privacy, security, and accountability (Atherley, 2005; Hakmeh et al., 2021; Storeng & de Bengy Puyvallée, 2021).
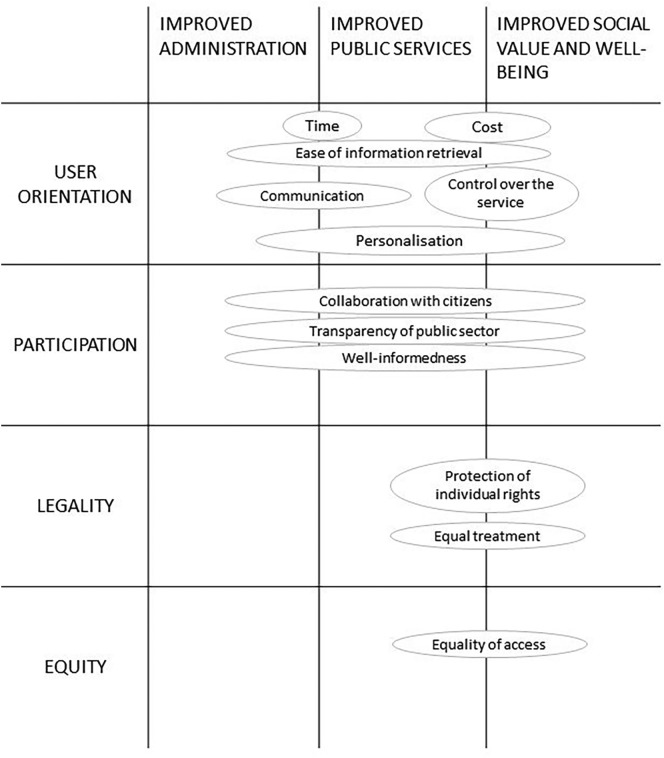
The evaluation of eHealth remains particularly challenging, due to the complex nature of healthcare services and the variety of stakeholders involved (Alalwany & Alshawi, 2008). However, the literature on the public value of e-government provides a solid theoretical foundation and a well-defined set of concepts that can be used to explore to what extent eHealth applications contribute to achieving the political mandates of public organisations and the aspirations of citizens. Accordingly, the evaluation of eHealth applications in this paper is based on a novel framework (see Fig. 1 ) that combines concepts and dimensions of public value from three existing taxonomies.
Fig. 1.
Analytical framework for analysing the public value of eHealth applications.
Source: Developd by authors based on Jørgensen and Bozeman (2007), Scott et al. (2016) and Twizeyimana and Andersson (2019).
Firstly, the values associated by Jørgensen and Bozeman (2007) with the relationship between public administration and citizens (user orientation, participation, legality and equity) were integrated with the three overarching and overlapping dimensions (improved public services, improved administration and improved social value) identified by Twizeyimana and Andersson (2019) in their review of the literature on public value and e-government. Secondly, the outcomes adopted by Scott et al. (2016) and the indicators listed by Twizeyimana and Andersson (2019) to specifically assess e-government services were mapped against these dimensions. As a result, our framework (Fig. 1) shows how different indicators, reflecting specific dimensions of public value, contribute to enhance public value by either improving administration, improving public services, or improving social value and wellbeing.
User orientation is linked to the direct outcomes and services that eHealth services can provide to their end-users (Scott et al., 2016). According to Scott et al. (2016) and Twizeyimana and Andersson (2019), these outcomes can be assessed in terms of cost and time savings as well as higher degree of personalisation and control over the delivery of public services, better communication with public administration, and easier retrieval of information. Echoing the dimension of dialogue included in Jørgensen and Bozeman (2007), participation refers to the potential of ICT to enhance the involvement of citizens in policymaking (Scott et al., 2016). This can be evaluated against the degree of collaboration between governments and citizens, the level of transparency of the public sector, and the informedness of citizens (Twizeyimana & Andersson, 2019). Speaking of transparency, Alessandro, Lagomarsino, Scartascini, Streb, and Torrealday (2021) further highlights that transparency in the public sector also increases the trustworthiness of governments.
Furthermore, legality and equity reflect to what extent eHealth services are compliant with individual rights, ensure an equal treatment of citizens and reduce inequalities in the access to healthcare services. These dimensions have not been thoroughly examined in the context of e-government (Scott et al., 2016; Twizeyimana & Andersson, 2019). Yet they recur as crucial issues in the literature on eHealth services (Atherley, 2005; Bend, 2004; Cashen, Dykes, & Gerber, 2004; Choi & DiNitto, 2013; Kearns, 2004) and in the public debate about eHealth applications developed in response to the pandemic, particularly the violation of individual rights and the exclusion of vulnerable social groups as indicated in Section 2.
As observed by Twizeyimana and Andersson (2019) and represented in Fig. 1, there is an overlap between dimensions and indicators of public value. Some values are expected to enhance both the quality of public services, the efficiency of public administration and social well-being: for example, easier access to information improves the experience of single end-users but also benefits the society as a whole. This is in addition to reducing the time and cost of administrative processes. The values associated to legality and equity, instead, only concern the quality of public services and social well-being. The framework developed in Fig. 1 will be used to map how different eHealth services contribute to creating public value, considering both the social and the utilitarian benefits associated with the use of ICT to deliver public services. By highlighting the potential overlap among different dimensions of public values, this framework is also expected to clarify the potential trade-offs between individual rights and public interest in the implementation of eHealth applications (de Lecuona & Villalobos-Quesada, 2018; van Kolfschooten & de Ruijter, 2020).
4. Methodology
The analysis in this paper draws from the secondary data of 50 cases of eHealth applications adopted in 25 EEA countries1 (See Appendix 2). These EEA countries are developed economies and established democracies subject to the same regulations such as the General Data Protection Regulation (GDPR). However, they also display significant differences in terms of size, culture, and political environment. Consequently, they provide a comparable yet heterogeneous sample to study the design and implementation of eHealth applications in Western countries during Covid-19 pandemic.
Our analysis is also limited to government-to-citizen (G2C) applications, developed under the supervision or with the endorsement of public organisations. Although public values can also be fostered by non-public organisations (Bryson et al., 2014), limiting the scope of the analysis to the applications developed under the supervision of public organisation makes this comparison more systematic and consistent with the framework in Section 3, which considers eHealth as a form of e-government service. The case studies were identified through the consultation of multiple repositories, listing the eHealth applications put in place since the outbreak of Covid-19 (Bischoff, 2020; eHealth Network, 2020; Open government partnership, 2020). Data on the single cases were retrieved from the websites of the organisations offering these applications and from the app marketplaces where these applications can be downloaded, including Apple and Play Stores. Further information on the case studies was sourced from online news platforms (such as BBC News, Deutsche Welle, Financial Times) and online repositories (such as GitHub). Systematic analyses of press releases, FAQ sections and privacy statements were conducted to collect detailed information on the design and governance of these eHealth services.
The analysis focused on several technical and organisational features that reflected the dimensions of public value described in Fig. 1. As detailed in Appendix 1, each dimension was explored through a set of questions, derived from the literature. As detailed in Appendix 2, these questions were then used to guide the analysis of the applications and to map them against the different dimensions included in the conceptual framework to assess whether their design is likely to create public value.
5. Analysis and findings
Consistent with Grimsley and Meehan (2007), the first step of the analysis was to map the outcomes expected and the services offered by these applications. As summarised in Table 1 (see Appendix 1 for details), two major outcomes were identified. Most of the eHealth applications developed within the EEA in response to Covid-19 aim to provide citizens with better access to medical information and care. Alternatively, smartphone-based apps have been adopted to prevent the spread of the virus through tracing the movements and contacts of their users or by monitoring the location of individuals.
Table 1.
Classification of the eHealth applications developed in EEA in response to Covid-19.
| eHealth applications for better access to healthcare information and care | eHealth applications designed to contain the spreads of the virus |
|---|---|
| 22 apps and websites providing updated information on the disease and the healthcare services available | 20 apps that track the movements and record the contacts of their users |
| 26 apps and websites for checking symptoms | 3 smartphone-apps monitoring the location and behaviour of their users |
| 5 applications monitoring the health conditions of patients in self-isolation through multiple channels | 1 application monitoring the health conditions of voluntary citizens through wearables |
Source: Developed by authors using data from Appendix 2.
Twenty-two apps and websites have been developed to provide citizens with updated information on the virus and the healthcare services locally available. In 16 cases, this functionality is combined with symptoms checkers that enable end-users to obtain a preliminary assessment of their health conditions and personal recommendations on the behaviours or medication to take. In five cases, eHealth applications have been developed to provide better treatments to those patients who tested positive but were not hospitalised. This outcome is pursued by equipping the patients with wearables that monitor their health conditions (e.g., the case of HSE Covid-19 in Ireland and H-Casa in Italy) or by asking them to regularly record their symptoms on an app or a website (e.g., the case of TreCovid19 in Italy and Covidom in France). The data collected through these applications are shared with health professionals that can take tailored actions or suggest specific medications. Wearables are also being used in Germany to collect data and monitor the health of those citizens voluntarily joining the Corona-datenspende (literally, Corona data donation) programme. A similar initiative is under pilot in Liechtenstein, where 2000 biometric bracelets have been distributed to the local population. The data collected through these devices are expected to help health authorities to monitor and better predict the future spread of Covid-19.
CTAs have been launched in 20 countries, but their implementation was under discussion in additional five EEA countries. In only three cases digital technologies have been used to monitor the behaviours of specific groups of citizens. In Poland and Lithuania individuals in quarantine are requested to prove evidence of their location through an app, which reports to the police those not complying with self-isolation. The government of Sardinia (a region in Italy), instead, requests those visiting the island to download (voluntarily) an app to record their arrival.
Matching our case analysis with the proposed framework in Fig. 1, we identified several findings in relation to the user orientation of these applications. The comparison revealed that all the eHealth applications adopted across the EEA are available for free to end-users (Q1 in Appendix 1). The gratuitousness of these services is frequently emphasised, but it is not necessarily an advantage of eHealth applications. In fact, the offline services that they replace or complement (e.g., phone helplines and human contact tracing) are also available for free. Conversely, these applications may entail hidden costs for the end-users that are required to upgrade their digital devices or use their internet connection to access online services.
In terms of time-savings, websites or apps providing medical information, symptoms checkers and CTAs speed up the exchange of information between citizens and health authorities (Q2a) by providing instant updates on the healthcare services available and the potential risk of contagion. Conversely, only health monitoring apps ensure timely access to healthcare services by triggering medical interventions as soon as the conditions of patients worsen (Q2b). In six cases, symptom checkers also speed up access to healthcare by enabling users to arrange an online consultation with their doctors. In two cases (ViruSafe in Bulgaria and Lazio Doctor in Italy), doctors can also contact their patients if the data collected through symptom checkers suggest the need for a medical intervention.
Similarly, the analysis revealed that information retrieval is enhanced when the applications include a section with details on the contagion, its treatment, and the services available to citizens (Q3a). These functions are naturally embedded in symptoms checkers and apps/websites providing medical information, although in two cases (Covid19check in Malta and Corona-datenspende in Germany) symptom checkers do not provide users with personalised recommendations based on their responses to the questionnaire. Furthermore, the comparison revealed that only three CTAs integrate symptom checkers or medical information. Our analysis rather emphasised how eHealth applications facilitate the collection of data on the disease to the benefit of healthcare institutions (Q3b). This is evident for CTAs and health monitoring applications, purposely designed to trace the spread of the virus and track the conditions of infected individuals. However, symptom checkers also allow to collect geo-localised data and to monitor the diffusion of the disease within the territory.
In terms of enhanced communications, only four applications allow citizens to directly interact with health professionals (Q4a): these are symptom checkers that give their users the option to call a doctor or arrange an appointment with their general practitioners (GPs). Conversely, 26 applications enabled health authorities to communicate with end-users (Q4b), either through automatic notifications (in the case of CTAs) or phone calls (triggered by health professionals monitoring the health conditions of patients).
In terms of control over the service, the comparison highlighted that just one application is mandatory (Kwarantanna domowa in Polonia), limited to users who tested positive and are self-isolating (Q5a). This and Karantinas in Lithuania are also the only applications that do not allow any control from their users (Q5b), consistent with their monitoring function. In the other cases, citizens can exert some form of control over the application: for example, users of CTAs can interrupt the app by switching off their Bluetooth signal and symptom checkers are only compiled on the initiative of their users.
Similarly, most of these applications enhance the personalisation of personalised healthcare services (Q6). In fact, symptom checkers, CTAs and health monitoring apps provide recommendations and treatments that reflect the personal information collected by or inputted in these applications. Likewise, movement monitoring apps only target those individuals who tested positive. However, neither the symptom checker developed in Malta nor the health monitoring app adopted in Germany delivers personalised recommendations. Likewise, information portals generally provide generic information, even though the use of AI-enabled chatbots can help to personalise this service (e.g., the case of Suvi in Estonia).
As summarised in Fig. 1, e-government services are also expected to enhance the participation of citizens to democracy by favouring their inclusion in the decision-making processes, their access to updated information and the transparency of the public sector. Within the EEA, 2/3 of the applications were developed by public institutions in partnership with private companies (Q7a). The latter included either small application developers or large corporations in the ICT industry. Given their role as gatekeepers of apps marketplaces and mobile operating systems, Apple and Google inevitably influenced the design of smartphone applications and contributed to the design of certain CTAs such as the NHS Covid-19 app in the UK. In only two cases, communities of citizens (with tech expertise) were directly involved in the design of the applications.
However, 23 smartphone apps (out of 44) have been identified as designed according to the principle of open-source software (Q7b). The latter implies that the source code of the app is made publicly available so that third parties can detect and fix technical issues or develop enhancements. This is expected to facilitate the engagement of citizens in policymaking by favouring their involvement in the design of e-government services (Linders, 2012). Furthermore, the adoption of open-source principles increases the transparency of the public sector.
The latter dimension has been also assessed in relation to the storage of personal data and the design of algorithms. Out of 24 applications storing the data centrally, only two do not disclose who oversees this (Q8a). As to the transparency over the algorithms embedded in eHealth applications, CTAs do not publish their algorithm but disclose the criteria applied to filter the contacts. Conversely, no monitoring applications and only two symptom checkers (MaladieCoronavirus in France and Andrija in Croatia) specified who designed the algorithms used to elaborate the responses of users and provide personal recommendations.
From the perspective of well-informedness, it is reasonable to assume that eHealth applications improve the quality and quantity of information available to citizens on the pandemic and the public responses put in place. This naturally applies to those apps and websites providing updates on the evolution of the disease and the measures adopted at the national and local levels to contain the contagion. However, some symptoms checkers and all CTAs (apart from the Icelandic one) do not include this functionality (Q9).
As to the other two dimensions identified by Jørgensen and Bozeman (2007), legality and equity, the case study analysis explored the protection of individual rights, the equality of treatment across different social groups and the fairness of access to these eHealth services. Consistent with extant literature on eHealth applications, we focused on privacy rights and potential barriers to eHealth adoption that could compromise equal access to health services (Murray et al., 2016, Mizera-Pietraszko & Świątek, 2015, Choi & DiNitto, 2013).
As mentioned in Section 1 and 2, privacy has been widely debated in relation to CTAs. Across the sample, all the apps (except Smittestopp in Norway and StopCovid in France) have opted for the decentralised model (Q10a), which is considered more compliant with data protection law as data on potential contacts are solely stored on the phones of the users for a limited amount of time (Savona, 2020). However, our analysis revealed that the protection of personal data is not at risk only within CTAs. Monitoring apps and symptoms checkers also collect personal data, generally stored for a long period well beyond Covid-19 pandemic (Q10b). For example, the data collected by HSE Covid-19 Patient Management in Ireland are to be stored for eight years, while the responses input in The Corona Check (the symptom checker developed by Dutch hospitals) are to be kept for 20 years.
A further issue emerging from this comparison is the risk of discriminating against different groups of users or creating inequalities in the access to healthcare services. Whereas CTAs are deployed at a national level, the sample also includes symptom checkers and monitoring apps developed by regional authorities and only integrated with the regional healthcare system (Q11a). As a result, citizens from the same country receive different services based on the regions where they reside. The analysis also highlighted that 22 applications are solely available in the official language(s): this has been recognised as a major barrier to access eHealth for patients that are non-native speakers (Q11b).
Likewise, in 20 cases the users of these applications are requested to register with the IDs provided by national or regional authorities (12a). This automatically excludes from the use of the applications those individuals who are not officially registered as they may be temporarily or illegally residing in a country. Another major impediment to equitable access to these services is linked to the technology used to deliver them (12b). Thirty-one of these eHealth services are only available via smartphone apps and often only work on the most recent versions of mobile operating systems: for example, while over 1.7 million people have downloaded the NHS Covid app in the UK (Kelion, 2021), the app cannot be downloaded on smartphones with operating systems older than iOS 13.5 or Android 6. As a result, users without smartphones or with older models are unable to benefit from these critical applications.
6. Discussion
The analysis in Section 5 highlighted how several eHealth applications have been adopted across the EEA since the outbreak of Covid-19. The case studies suggested that they can improve the administration of public healthcare by facilitating the dissemination and collection of information on the spread of Covid-19. However, the overall public value of these applications is sometimes affected by endogenous or exogenous factors (summarised in Table 2 ) that undermine the ability of eHealth applications to improve the quality of healthcare services and social wellbeing.
Table 2.
Factors affecting the public value of eHealth applications.
| Endogenous Factors | Exogenous Factors | |
|---|---|---|
| User orientation |
|
|
| Participation |
|
|
| Legality |
|
|
| Equity |
|
|
Source: Developed by authors based on the analysis of the case studies in Appendix 2.
The former reflects shortcomings in the design of eHealth applications that affect their user orientation and ability to maximise participation, legality, and equity. For example, the analysis revealed that only two symptom checkers allow their users to directly communicate with healthcare professionals (Q4a) and one does not even provide personalised recommendations (Q6). This undermines the potential of these applications to provide faster access to personal medical services. Likewise, the participation of citizens could be further enhanced by adopting open-source software principles (Q7b), currently limited to 23 apps, or disclosing the criteria used by the algorithms embedded in symptom checkers and chatbots (Q8b). The developers of eHealth applications should also pay more attention to those factors that may lead to the exclusion of some users: within the sample, only 16 applications were available in a non-official language (Q11b) and 20 requested national or regional IDs to login (Q12b), thereby discriminating against non-native speakers and unregistered residents.
Alongside these endogenous issues, our comparison highlighted that the public value of eHealth applications in the context of Covid-19 is also undermined by exogenous factors, reflecting market failures in the digital ecosystem and the potential trade-off existing between individual rights and public interest. The latter affects the ‘legality’ of eHealth applications, while the former impact on both the ‘participation of citizens’ and the ‘equity’ of these services.
The analysis confirmed that the design of eHealth applications has been primarily led by public agencies in partnership with technology providers, while the involvement of citizens has been negligible (Q7a). The adoption of open-source software principles may mitigate this, but there is little that health authorities can do to counterbalance the power of big players like Apple and Google in the digital ecosystem. Given their control over app marketplaces and operating systems for smartphones, these two companies have exerted significant influence over the design and interoperability of CTAs. The involvement of corporations in the development of eHealth applications raise more general concerns on the interference of private interests in the management of public healthcare, as previously noted by Hellberg and Johansson (2017).
Furthermore, the public value of eHealth services is undermined by structural inequalities in the access and usage of digital technologies (the so-called digital divide). This implies that many are not equipped with the devices and/or skills needed to benefit from eHealth applications (Q12a). Quite worryingly, these issues mostly affect those social groups (elderly people, deprived households, migrants) that are most exposed to Covid-19 (Davis, 2020). Therefore, despite providing most citizens with better access to medical information and tailored medical treatments, these technologies may exacerbate inequalities in the access to healthcare services and undermine the universality of public healthcare.
Finally, our analysis highlighted a potential trade-off between the individual right to privacy and the public value that can be derived from the collection of personal data. Whereas the risks of CTAs in this context have been largely discussed and generally minimised (by adopting a decentralised model and complying with GDPR), our comparison showed that symptoms checkers and health-monitoring apps also pose a threat to the privacy of their end-users as they collect a significant amount of sensitive information often stored for a long period (Q10b) and shared with third parties (Q10c). The latter is likely to create value for the public by enabling both healthcare providers to track the contagion and researchers to further study this disease. However, this may clash with the rights of individual users, especially if the latter are not fully aware of why their personal data are being collected and how these are going to be used.
Consequently, our analysis confirmed the concerns over the fairness and legality of the eHealth strategies developed in response to the current pandemic (McDonald, 2020; Savona, 2020). The comparison clarified that such limitations result from either shortcoming in the design of these applications or structural failures in the digital ecosystem. It must be emphasised that the issues of the legality and fairness of eHealth services are not only driven by ethical considerations: any factor that hampers the adoption of these applications is also likely to undermine their effectiveness. In fact, the latter is often affected by the number of individuals using these services. This is well evidenced by the CTA developed in Norway that was launched in April 2020 but suspended two months later since most of the population refused to download it due to privacy concerns.
Our findings also have several theoretical implications. As discussed in Section 3, the public value of eHealth applications can be assessed against a wide range of dimensions. Whereas the latter is often presented as complementary, this study suggests that tensions may exist among different dimensions of public value. Whereas the need to make public healthcare more efficient and more responsive pushes towards a broader usage of eHealth applications, the latter do not necessarily result in ‘improved social value and wellbeing’.
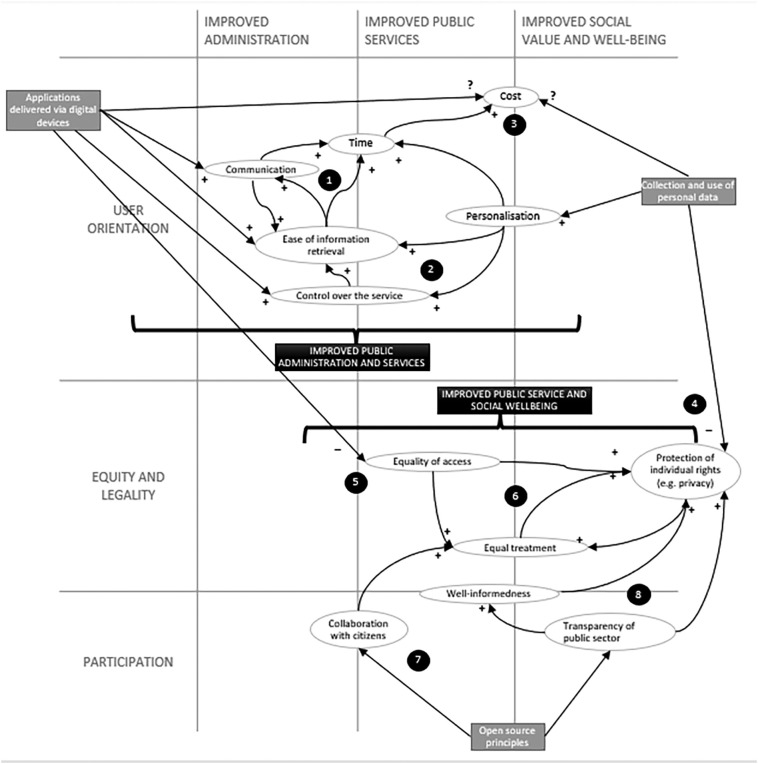
As noted above and visualised in Fig. 2 , the ability of eHealth applications to deliver timely healthcare services largely depend on what degree these applications facilitate the retrieval of information and enable direct communication between users and health professionals (as shown in Fig. 2, circle 1). The ease of information retrieval is enhanced by the personalisation of medical services (made possible by the collection of personal data) and the possibility for the users to control their health status without depending on the availability of health professionals (Fig. 2, circle 2).
Fig. 2.
A revised framework for the public value of eHealth applications.
Source: Developd by the authors, based on Jørgensen and Bozeman (2007), Scott et al. (2016), Twizeyimana and Andersson (2019) and the findings from the case study analysis.
The timeliness of eHealth services arguably reduces the travel and time costs to access healthcare: for example, individuals using symptom checkers no longer need to take time off work to visit a GP, as they can receive diagnosis and recommendations through an app (EXPH, 2019). However, the overall relationship between eHealth and cost remains ambiguous as noted above and highlighted in Fig. 2 (circle 3). In fact, the use of digital devices and online services may entail hidden costs for the end-users, as they need to use their own connectivity or buy a specific device to access these services. Furthermore, the value of personal data should also be considered when estimating the cost of e-health for the end-users (de Lecuona & Villalobos-Quesada, 2018).
The collection of personal data may also harm the right of citizens, with specific regard to privacy (Fig. 2, circle 4). More generally, the individual rights of citizens may be threatened by inequalities in the access to eHealth services, reflecting the fact that users without digital skills and digital devices are unable to use these services (Fig. 2, circle 5). The exclusion of those citizens compromises the equality of treatment in public healthcare and undermines the universal right to access medical services, thereby failing to improve social value and wellbeing (Fig. 2, circle 6).
Open-source principles can help mitigate these trade-offs. As shown in Fig. 2 (cicle 7), by enabling citizens to contribute to the design of public services, the open-source approach is expected to favour the development of eHealth applications that preventively address those obstacles leading to the unfair treatment of individuals (such as a language barriers). The open-source approach also increases the transparency of the public sector, which in turn augments the well-informedness of citizens and reinforces the protection of individual rights, as shown in Fig. 2 (circle 8). In fact, the transparency of data collection and storage are essential to safeguard privacy rights (Marelli et al., 2020). Furthermore, well-informedness contributes to ensuring the equal treatment of healthcare users, by enhancing the quality and quantity of information available to citizens on the pandemic and the public responses put in place. However, structural failures in the market of digital platforms remain an unsolved issue that affects the public value of eHealth applications but cannot be addressed solely by health authorities.
7. Conclusion
Given the ubiquity and the enabling role of ICT across industries and societies, Covid-19 would not be the last time CTAs and other eHealth applications would be used to combat a pandemic. This is consistent with Hakmeh et al. (2021), who argues that Covid-19 pandemic has underlined the need for businesses and governments to reinvent themselves through the integration of digital technology or risk falling behind the global landscape. This is exemplified in the UK where NHS GPs are using technology to contact people and schedule Covid-19 vaccination appointments. However, our analysis highlighted that some limitations exist that may hamper the public value of technological applications. Alongside shortcomings in their design, eHealth applications are affected by exogenous factors, reflecting structural inequalities in the usage of ICT (such as the digital divide), path dependencies in the digital economy (due to the market power of digital platforms) and trade-offs between individual rights and public interest in the use of personal data. Speaking of digital divide, Hernández-Orallo et al. (2020) and Kretzschmar et al. (2020) revealed that without the inclusion of a significant proportion of the population, contact-tracing with technology will be ineffective.
Going forward, policymakers should bear in mind that while the use of eHealth applications can mitigate the inefficiency of traditional contact-tracing and enhance the delivery of healthcare services, certain limitations exist that need to be tackled to maximise their impact in terms of social value and wellbeing. Consequently, eHealth applications should be designed to enhance their accessibility, for example by allowing multiple users to access them from the same device or making them available on older smartphones. eHealth services should also be provided in the languages most frequently spoken within the country by ethnic minorities or the largest communities of migrants to expand their adoption among these social groups. Making eHealth applications interoperable would also allow tourists and expatriates to access and use these services from different regions or countries. Furthermore, the open-source principle should be applied more consistently in the attempt to make these applications more inclusive and transparent. Higher transparency should be guaranteed on the usage of personal data and the paternity of algorithms. All eHealth applications, and not just CTAs, should comply with GDPR to make sure that their users are fully aware of how their data are used, stored, transferred, and shared.
From a theoretical perspective, this study confirms that the public value theory offers a solid framework to analyse e-government services, but also highlights the complexity of the relationships among the different dimensions of public value in the context of healthcare provision. This aspect needs to be further explored from both an empirical and theoretical perspective to clarify how eHealth applications can create value for the public without undermining the rights and benefits of individual users and marginalised groups. Further research is also needed to understand how failures in the digital ecosystem can be addressed to minimise their effects on the design and delivery of eHealth services.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Biographies
Paolo Gerli, PhD, is a Lecturer in Entrepreneurship and Innovation at Edinburgh Napier University, UK. His research explores both business models and public policies for an inclusive and fair digital transformation, with a focus on the digital divide and its implications for the economy and society. He obtained his PhD degree from Northumbria University and has industry experience in the regulation of telecommunications and digital markets.
Emmanuel Ogiemwonyi Arakpogun, PhD, is a Senior Lecturer in Digital Economy and International Business Management at Newcastle Business School. His research interests lie at the intersection of the liberalisation of the telecoms market, telco MNEs participation and universal access policies as a combined strategy for closing the digital divides in emerging economies. He is a reviewer for several journals including Information Technology and People, Technological Forecasting and Social Change, and Journal of Management Information Systems.
Ziad Elsahn, PhD, is a Senior Lecturer in International Business at the Entrepreneurship, innovation, and Strategy department at Northumbria University, Newcastle Business School. His research interests lie at the intersection of International Business, Organisation theory, and Strategy. Specifically, his research focuses on internationalisation, knowledge coordination and integration within and between firms, and strategy process in multinational enterprises (MNEs).
Femi Olan, PhD, is a Senior Lecturer in Business Information Management at Northumbria University, UK. He obtained his PhD degree from Plymouth University, UK. He has teaching and industry experience in the field of information systems. His research interests focus on knowledge sharing, organizational factors, and performance management in organizations. He has collaborated on numerous research projects for, among others, development agencies. He has authored numerous articles in peer-reviewed journals and books.
Karla Simone Prime, PhD, is a Senior Lecturer in Economics at Northumbria University, UK. She has published in areas of institutional economics, economic growth and development and poverty and inequality. At the centre of her research is the question of how and through which mechanisms national institutional infrastructure and development influences economic policy and reduction of poverty and inequality in low- and middle-income countries. She is co-author of What can be learned from China’s Success? Investigating institutional capacity, trade and investment in African economies and Institutions, economic growth and international competitiveness.
Footnotes
At the time of writing, a further 7 applications were being developed or trialled within the EEA, but these have been excluded from the analysis because they are yet to be completed and made available to citizens. Consequently, our sample does not include cases from five EEA countries (Liechtenstein, Luxembourg, Malta, Romania, Slovakia) where eHealth applications are still under development. Sweden has also been omitted from this analysis because, at the time of writing, there are no plans to adopt eHealth applications to fight Covid-19 in this country.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.giq.2021.101581.
Appendix A. Supplementary data
Supplementary material
References
- Alalwany H., Alshawi S. Evaluation of e-health services: user’s perspective criteria. Transforming Government: People, Process and Policy. 2008;2(4):243–255. [Google Scholar]
- Alessandro M., Lagomarsino B.C., Scartascini C., Streb J., Torrealday J. Transparency and trust in government evidence from a survey experiment. World Development. 2021;138:105223. [Google Scholar]
- Arakpogun E.O., Elsahn Z., Prime K.S., Gerli P., Olan F. Digital contact-tracing and pandemics: Institutional and technological preparedness in Africa. World Development. 2020;136 doi: 10.1016/j.worlddev.2020.105105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atherley G. Evidence of public value and public risk of electronic health records: An issue for social justice? Healthcare Quarterly. 2005;8(3):96–103. [PubMed] [Google Scholar]
- Bend J. Institute for Public Policy Research; 2004. Public value and eHealth. [Google Scholar]
- Bischoff P. Comparitech. 2020. COVID-19 app tracker: Is privacy being sacrificed in a bid to combat the virus?https://www.comparitech.com Retrieved from. [Google Scholar]
- Bradshaw T., Venkataramakrishnan S. Financial Times. 2021, February 09. NHS Covid app prevented 600,000 infections, claim researchers.https://www.ft.com/content/49427a5f-6404-44e5-b977-4a691316fefa Retrieved from. [Google Scholar]
- Bryson J., Crosby B., Bloomberg L. Public value governance: Moving beyond traditional public administration and the new public management. Public Administration Review. 2014;74 [Google Scholar]
- Cashen M.S., Dykes P., Gerber B. eHealth technology and internet resources: Barriers for vulnerable populations. Journal of Cardiovascular Nursing. 2004;19(3) doi: 10.1097/00005082-200405000-00010. [DOI] [PubMed] [Google Scholar]
- Choi N.G., DiNitto D.M. The digital divide among low-income homebound older adults: Internet use patterns, eHealth literacy, and attitudes toward computer/internet use. Journal of Medical Internet Research. 2013;15(5):e93. doi: 10.2196/jmir.2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis S.L.M. Contact tracing apps: Extra risks for women and marginalized groups. Health and Human Rights Journal. 2020;4 [Google Scholar]
- eHealth Network . Belgium. 2020. Mobile applications to support contact tracing in the EU’s fight against COVID-19. Brussels. [Google Scholar]
- EXPH . Brussels; Belgium: 2019. Expert panel on effective ways of investing in health (EXPH) Defining value in “value-based healthcare. [Google Scholar]
- Ferguson N.M., Laydon D., Nedjati-Gilani G., Imai H., Ainslie K., Baguelin M.…Ghani A.C. Imperial College London; 2020. Report 9. Impact of non-pharmaceutical interventions (NPIs) to reduce covid19 mortality and healthcare demand. [DOI] [Google Scholar]
- Firouzi F., Rahmani A.M., Mankodiva K., Badaroglu M., Merrett G.V., Wong P., Farahani B. Internet-of-things and big data for smarter healthcare: From device to architecture, applications and analytics. Future Generation Computer Systems. 2018;78(2):583–586. [Google Scholar]
- Frisk J.E., Bannister F., Lindgren R. Evaluation of information system investments: A value dials approach to closing the theory-practice gap. Journal of Information Technology. 2015;30(3):276–292. [Google Scholar]
- Gasser U., Ienca M., Scheibner J., Sleigh J., Vayena E. Digital tools against COVID-19: Framing the ethical challenges and how to address them. arXiv preprint. 2020 doi: 10.1016/S2589-7500(20)30137-0. arXiv:2004.10236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimsley M., Meehan A. E-government information systems: Evaluation-led design for public value and client trust. European Journal of Information Systems. 2007;16:134–148. [Google Scholar]
- Hakmeh J., Taylor E., Peters A., Ignatidou S. International Security Programme; Chatham House: 2021. The COVID-19 pandemic and trends in technology: Transformations in governance and society. [Google Scholar]
- Hellberg S., Johansson P. eHealth strategies and platforms – The issue of health equity in Sweden. Health Policy & Technology. 2017;6(1):26–32. [Google Scholar]
- Hernández-Orallo E., Manzoni P., Calafate C.T., Cano J.C. Evaluating how smartphone contact tracing technology can reduce the spread of infectious diseases: The case of COVID-19. IEEE Access. 2020;8:99083–99097. doi: 10.1109/ACCESS.2020.2998042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jørgensen T.B., Bozeman B. Public values: An inventory. Administration and Society. 2007;39(3):354–381. [Google Scholar]
- Kearns I. Institute for Public Policy Research; 2004. Public value and E-government. [Google Scholar]
- Kelion L. BBC; 2021, February 09. Covid-19: NHS app has told 1.7 million to self-isolate.https://www.bbc.co.uk/news/technology-55985562 Retrieved from. [Google Scholar]
- Klenk Michael, Duijf Hein. Ethics of Digital Contact Tracing and COVID-19: Who Is (Not) Free to Go? Ethics and Information Technology. 2020 doi: 10.1007/s10676-020-09544-0. May 28 Available at SSRN: https://ssrn.com/abstract=3595394 or http://dx.doi.org/10.2139/ssrn.3595394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kolfschooten H., de Ruijter A. COVID-19 and privacy in the European Union: A legal perspective on contact tracing. Contemporary Security Policy. 2020;41(3):478–491. [Google Scholar]
- Kretzschmar M.E., Rozhnova G., Bootsma M.C., van Boven M., van de Wijgert J.H., Bonten M.J. Impact of delays on effectiveness of contact tracing strategies for COVID-19: A modelling study. The Lancet Public Health. 2020;5(8):e452–e459. doi: 10.1016/S2468-2667(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen D.B., Ruckenstein M. Co-evolving with self-tracking technologies. New Media & Society. 2018;20(10):3624–3640. doi: 10.1177/1461444818755650. [DOI] [Google Scholar]
- Kummitha R.K.R. Smart technologies for fighting pandemics: The techno- and human- driven approaches in controlling the virus transmission. Government Information Quarterly. 2020 doi: 10.1016/j.giq.2020.101481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lecuona I., Villalobos-Quesada M. European perspectives on big data applied to health: The case of biobanks and human databases. Developing World Bioethics. 2018;18(3):291–298. doi: 10.1111/dewb.12208. [DOI] [PubMed] [Google Scholar]
- Li J., Seale H., Ray P., Rawlinson W., Lewis L., MacIntyre C.R. Issues regarding the implementation of eHealth: Preparing for future influenza pandemics. Interactive Journal of Medical Research. 2012;1(2):e20. doi: 10.2196/ijmr.2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linders D. From e-government to we-government: Defining a typology for citizen coproduction in the age of social media. Government Information Quarterly. 2012;29(4):446–454. [Google Scholar]
- McDonald S. Brookings Institute; 2020. Contact-tracing apps are political. [Google Scholar]
- Mizera-Pietraszko J., Świątek P. 2015. Access to eHealth language-based services for multinational patients, paper presented at 17th International Conference on E-health Networking, Application & Services (HealthCom), Boston (MA) [Google Scholar]
- Moore M. Harvard University Press; Cambridge (MA): 1995. Creating public value: Strategic management in government. [Google Scholar]
- Moore M. Managing for value: Organizational strategy in for-profit, nonprofit, and governmental organizations. Nonprofit and Voluntary Sector Quarterly. 2000;29(1_suppl):183–204. [Google Scholar]
- Murray E., Hekler E.B., Andersson G., Collins L.M., Doherty A., Hollis C.…Wyatt C.J. Evaluating digital health interventions: Key questions and approaches. American Journal of Preventive Medicine. 2016;51(5):843–851. doi: 10.1016/j.amepre.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh H., Rizo C., Enkin M. Jadad, Alejandro What is eHealth (3): A systematic review of published definitions. Journal of Medical Internet Research. 2005;7(1):e1. doi: 10.2196/jmir.7.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Open government partnership Collecting open government approaches to COVID-19. 2020. https://www.opengovpartnership.org/collecting-open-government-approaches-to-covid-19/ Retrieved May 20, 2020, from.
- Rose J., Persson J.S., Heeager L.T., Irani Z. Managing e-government: Value positions and relationships. Information Systems Journal. 2015;25(5):531–571. [Google Scholar]
- Savona M. 2020-10. SPRU Working Paper Series (SWPS); 2020. The Saga of the Covid-19 contact tracing apps: Lessons for data governance; pp. 1–12. [Google Scholar]
- Scott M., DeLone W., Golden W. Measuring eGovernment success: A public value approach. European Journal of Information Systems. 2016;25(3):187–208. [Google Scholar]
- Seltsikas P., O’Keefe R.M. Expectations and outcomes in electronic identity management: The role of trust and public value. European Journal of Information Systems. 2010;19(1):93–103. [Google Scholar]
- Storeng K.T., de Bengy Puyvallée A. The smartphone pandemic: How big tech and public health authorities partner in the digital response to Covid-19. Global Public Health. 2021:1–17. doi: 10.1080/17441692.2021.1882530. [DOI] [PubMed] [Google Scholar]
- Svejvig P., Schlichter B.R., Andersen P. MCIS 2012 Proceedings. 2012. From business IT value to public IT value–an action research study of healthcare in the Faroe Islands; p. 18. [Google Scholar]
- Timpka T., Spreco A., Dahlström Ö., Eriksson O., Gursky E., Ekberg J.…Holm E. Performance of eHealth data sources in local influenza surveillance:A 5-year open cohort study. Journal of Medical Internet Research. 2014;16(4):e116. doi: 10.2196/jmir.3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twizeyimana J.D., Andersson A. The public value of E-government – A literature review. Government Information Quarterly. 2019;36(2):167–178. [Google Scholar]
- UCLG . 2020. Digital technologies and the COVID19 pandemic. [Google Scholar]
- WHO . Available at who.Int. 2020. COVID-19 and digital health: What can digital health offer for COVID-19? [Google Scholar]
- Ye Q., Zhou J., Wu H. Using information technology to manage the COVID-19 pandemic: Development of a technical framework based on practical experience in China. JMIR Medical Informatics. 2020;8(6) doi: 10.2196/19515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material