Abstract
This case-control study aimed to assess pathologic alteration in the serum levels of the atherogenic index, cholesterol to high-density lipoprotein (HDL) ratio, HDL cholesterol, total cholesterol, triglyceride, HbA1c, and glucose in 158 COVID-19 patients who were hospitalized in Erbil international hospital, Erbil, Iraq, between January and May 2020, in the early stage of infection. The patients were confirmed for SARS-CoV-2 on admission. The laboratory test results were compared between this group and a group of healthy individuals (n=158). A statistically significant difference was found between the studied factors in healthy controls and COVID-19 patients, except for low-density lipoprotein (LDL) cholesterol (P=0.13). In the case of COVID-19 patients, total levels of cholesterol and HDL cholesterol were significantly lower than controls (P<0.003). Triglyceride, VLDL cholesterol, atherogenic index, and total cholesterol to HDL ratio were found to be significantly higher in COVID-19 patients, compared to controls (P<0.005). Atherogenic index were found to be positively correlated with triglyceride (r=0.88, P=0.00), HbA1C (r=0.6, P=0.05), and glucose index (r= 0.62, P= 0.05), and the ratio of cholesterol to HDL (r=0.64, P=0.04). In contrast, no correlation was found between atherogenic index and cholesterol to HDL ratio in controls. The results of the current study indicated that risk factors for the cardiovascular disease increased in patients with COVID-19 infection, which included atherogenic index, cholesterol to HDL ratio, as well as the association between atherogenic index, and all were organized in one cluster. Therefore, lipids can perform a vital physiological function in patients infected with COVID-19.
Keywords: COVID-19, Atherogenic index, Cholesterol to HDL ratio
1. Introduction
Viruses are known to be the cause of a large range of diseases. Coronavirus disease COVID-19 was discovered in Wuhan city of China in December 2019. Ever since various cases of interstitial pneumonia have been reported ( 1 ). Several severe systemic complications, such as acute respiratory distress
syndrome (ARDS) and acute respiratory failure, were developed very quickly in certain patients due to COVID-19 infection. As a result of a thorough analysis of lower respiratory tract samples, a new coronavirus was detected which was originally named SARS-CoV-2 in 2019 as a novel coronavirus (2019-nCoV) ( 2 ).
The disease quickly spread from Asia to the rest of the world and led to the death of thousands of people. Eventually, the World Health Organization declared COVID-19 a pandemic disease on March 11, 2020.
SARS-CoV-2 has four structural proteins, including spick protein (S), an envelope protein (E), membrane protein (M), and nucleocapsid protein (N). The virus contains a genome that codes for the four structural proteins: approximately 30,000 nucleotides ( 3 ). Most of these are dependent on the S protein, which plays a key role in viral attachment as well as fusion and entry into cells. As a host receptor, it binds the receptor-binding domain (RBD) in the subunit S1 to angiotensin-converting enzyme2 (ACE2) and then connects the viruses and host membranes via its subunit S2 ( 4 , 5 ).
High levels of lipid profile, such as triglycerides, and total cholesterol, as well as their association with high-density lipoprotein (HDL) lipoprotein, low-density lipoprotein (LDL), and VLDL lipoprotein, are referred to as dyslipidemia ( 6 ). In case of the absence of an unfavorable lipid profile, the possibility of attack with one of the cardiovascular diseases cannot be ruled out completely ( 7 ).
In terms of cardiac risk estimation, the atherogenic index of plasma (AIP) is a crucial index that can be used on its own ( 8 ). The risk of atherosclerotic complications increases after changes in one’s lipid profile ( 9 ). AIP is calculated as the logarithm of plasma TG to HDL-C ratio and is strongly correlated with the risk of cardiovascular disease ( 10 ). The total-cholesterol-to-HDL ratio is another test that helps to determine coronary heart disease and stroke. This test is used as part of regular medical checkups to determine risk factors for coronary heart disease, with a low level of HDL cholesterol ( 11 ).
To date, very few studies have been carried out on the lipid profile of patients with COVID-19. A recent preliminary study found that serum lipid concentrations were altered compared to those without COVID-19, indicating that levels of lipid can have an important role in both viral and internalized levels as well as in immune activation. Therefore, the current study aimed to determine how the lipid profiles of patients infected with COVID-19 changed during the initial phase of infection.
2. Materials and Methods
2.1. Study Design
This case-control study was carried out to investigate serum levels of the atherogenic index, cholesterol to HDL ratio, total cholesterol, triglycerides, HDL cholesterol, LDL cholesterol, glucose, and HbA1c in COVID-19 patients (n=158) hospitalized in Erbil International Hospital between January and May 2020. The patients were confirmed for SARS-CoV 2 disease at admission. The laboratory test results of this group and a group of healthy individuals (controls) were compared (n=158).
2.2. Laboratory Test
Biochemical parameters (i.e., glucose, LDL-cholesterol, HDL-cholesterol, total cholesterol, and triglycerides) were assessed using the spectrophotometry method, and the Randox kit was utilized for lipid profile and glucose. HbA1c was assayed using High-performance liquid chromatography (HPLC) ( 12 ). Atherogenic index, cholesterol to HDL ratio, and VLDL cholesterol were calculated using different equations.
2.3. Statistical Analysis
Statistical analysis was performed in SPSS software (version 25). All data are presented as mean+SE. Student independent t-test was used to identify the significant difference between the study groups. The bivariate analysis was used to find out the association among the various biochemical parameters based on the Pearson test. Cluster analysis was based on the word method. A P-value less than 0.05 (P<0.05) was considered statistically significant.
3. Results and Discussion
Participants in the study comprised 158 (78.6%) COVID-19-positive individuals with a mean±SD age of 53±14 years and 43 (21.4%) healthy individuals (controls) with a mean±SD age of 44±4 years, as presented in figure 1.
Figure 1.

Groups distribution in the current study
The mean±SD total cholesterol and HDL cholesterol in COVID-19 patients were lower in positive patients, compared to that in healthy controls in baseline (126±7.7 vs. 164.5±5.5 mg/dL, 34.2±2.7 vs. 65±3.0, respectively) with P<0.003 (Table 1). It was found that patients with COVID-19 had higher levels of serum triglyceride, glucose, VLDV cholesterol, atherogenic index, and a greater ratio of total cholesterol to HDL (179±28.8 vs. 110±3.5, 185±11.9 vs. 90±0.7, 7.6±0.8 vs. 5.2±0.08, 35.6±5.7 vs. 22±0.7 mg/dL) (0.72 vs. 0.20, 3.7/ 1 vs. 2.7/1), respectively (Table 1). In particular, LDL cholesterol level was not statistically significantly distinguished.
Table 1.
Comparison of biochemical parameters between COVID-19 patients and healthy controls
| Parameters | Patients | Control | P-value | ||||
|---|---|---|---|---|---|---|---|
| Mean±SE | Minimum | Maximum | Mean±SE | Minimum | Maximum | ||
| Glucose | 185±1.9 | 81 | 383 | 90±0.7 | 85 | 95 | 0.00 |
| HbA1C | 7.6±0.8 | 6 | 11 | 5.2±0.08 | 4.8 | 6.1 | 0.00 |
| Total Cholesterol | 126±7.7 | 76 | 179 | 164.5±5.5 | 111 | 199 | 0.00 |
| Triglyceride | 179±28.8 | 62 | 357 | 110±3.5 | 90 | 130 | 0.005 |
| HDL Cholesterol | 34.2±2.7 | 19 | 54 | 65±3.0 | 40 | 78 | 0.003 |
| LDL Cholesterol | 85.1±7.2 | 41 | 124 | 73.4±3.6 | 50 | 60 | 0.13 |
| VLDV Cholesterol | 35.6±5.7 | 12.4 | 75 | 22±0.7 | 10 | 12 | 0.00 |
| Atherogenic index | 0.72 | 0.50 | 0.81 | 0.20 | 0.4 | 0.2 | 0.00 |
| Total-Cholesterol-to-HDL ratio | 3.7/ 1 | 4 /1 | 3.3/1 | 2.5/1 | 2.7/1 | 2.5/1 | 0.00 |
Infection with the SARS-CoV-2 virus has the potential to have significant effects on lipid metabolism. Patients with SARS-CoV-2 infection had lower initial lipid levels, particularly total cholesterol, and HDL cholesterol, compared to healthy controls (P=0.003), while triglyceride levels were higher in these patients (Table 1). Patients with COVID-19 had similar alterations in lipid profile values in previous studies ( 13 - 16 ).
Physiologically, HDL is the most important lipid type involved in the inflammation and oxidation of cells, since it consists of several lipoproteins. Apo-A-I, apo A-II, phospholipids, transfer proteins, and enzymes are all found in HDL. This group of lipoproteins is crucial for vasodilatation as well as LDL oxidation-reduction, inflammation, infection, thrombosis, and apoptosis. HDLs are an anti-inflammatory lipoprotein that protects from oxidation of lipid, reduces the stimulation of T-cells and the expression of inflammatory intermediaries in dendritic cells and macrophages ( 17 - 19 ). Antioxidant functions allow for the elimination of oxidized fats and the neutralization of certain oxidative mediators. Moreover, the increase in HDL level may lead to a reduction of monocyte penetration into the artery wall ( 20 ). Oxidized HDL and LDL can be upregulated during the inflammatory period and immune activation were upregulated ( 15 , 21 ). In the present study, HDL levels in COVID-19 patients were significantly lower in the early stage of illness compared to controls. Therefore, the decrement may be due to the contribution of HDL in the adjustment of immune cells through illness. Lipid microdomains that contain a high concentration of cholesterol play an essential role in COVID-19 life cycle. The viral infection depends on how the plasma membrane elements of the host cell interact with the viral envelope. The compounds of the target cell surface, especially cholesterol, are important for enabling COVID-19 infections. Cholesterol-rich microdomains faciliat interaction between angiotensin-converting enzyme 2 and spike glycoprotein on COVID-19 ( 22 ). In the current study, cholesterol levels were low in the first stage of infection with COVID-19; therefore, the initial decline of cholesterol level may correlate with the viral infection. Other markers, such as AIP, that are defined as Triglyceride-to-HDL-C logarithmic transformation, and cholesterol to HDL ratio have been evaluated in the present study. Chronic diseases, such as cardiovascular disease and diabetes are associated with AIP. Our studies showed that patients in the initial phase of COVID-19 had higher levels of AIP, triglyceride, cholesterol to HDL level, and lower total cholesterol, compared to healthy controls. Lipid profile alteration, particularly high triglyceride, and low HDL-C levels are considered a cardiovascular disease risk factor. AIP was another risk factor, and previous studies showed that AIP was correlated with cardiovascular diseases and diabetes mellitus. Therefore, COVID-19 affected the cardiovascular system ( 23 ).
The virus’ status may be monitored through cholesterol and lipoproteins, while the lipid metabolic and membrane composition pathways may allow for selective inhibition of the virus cycle as a basis for antiviral treatment ( 24 ). Medical illnesses that contribute to the common metabolic changes for high glucose levels and dyslipidemia, such as cardiovascular comorbidity, hypertension, and type 2 diabetes mellitus, were observed in patients with serious consequences of coronavirus disease ( 25 ). In the current study, higher HbA1c, glucose levels sensitivity, metabolic syndrome, and adverse cardiovascular events were associated with an AIP and high cholesterol-to-high-density lipoprotein (Cholesterol/HDL), indicating that COVID-19 patients may develop cardiovascular disease or diabetes. Therefore, we can take those markers as the predictors of complications in COVID-19 patients.
The bivariate analysis of glucose, HbA1C, total cholesterol, triglyceride, HDL cholesterol, LDL cholesterol, VLDL cholesterol, atherogenic index, and total-cholesterol-to-HDL ratio in COVID-19 patients compared to controls are presented in tables 2 and 3, respectively. Atherogenic index was positively correlated with triglyceride (r=0.88, P=0.00), HbA1C (r=0.6, P=0.05), glucose (r=0.62, P=0.05), and cholesterol to HDL ratio (r=0.64, P=0.04) (Table 2). Moreover, total cholesterol was positively correlated with HDL cholesterol (r=0.6, P=0.02) and LDL- cholesterol (r=0.9, P=0.00). No significant association was observed between other parameters. HbA1C level was observed to be negatively correlated with the level of triglyceride, LDL cholesterol, HDL cholesterol, and total cholesterol.
Table 2.
Bivariate analysis of presented parameters in patients with COVID-19
| Parameters | Total Cholesterol | Triglyceride | HDL | Cholesterol | LDL Cholesterol | HbA1C | Glucose | AIP | Cholesterol to HDL |
|---|---|---|---|---|---|---|---|---|---|
| Total Cholesterol | r | 1 | 0.515 | 0.603* | 0.910** | -0.03 | -0.035 | 0.292 | 0.379 |
| P | 0.02 | 0.00 | |||||||
| Triglyceride | r | 1 | 0.036 | 0.319 | -0.04 | 0.339 | 0.880** | 0.416 | |
| P | 0.00 | ||||||||
| HDL-Cholesterol | r | 1 | 0.356 | -0.03 | -0.376 | -0.407 | -0.591 | ||
| P | |||||||||
| LDL- Cholesterol | r | 1 | -0.02 | 0.019 | 0.242 | 0.587 | |||
| P | |||||||||
| HbA1C | r | 1 | 0.994 | 0.6 | 0.51 | ||||
| P | 0.05 | ||||||||
| Glucose | r | 1 | 0.622 | 0.462 | |||||
| P | 0.05 | ||||||||
| AIP | r | 1 | 0.647* | ||||||
| P | 0.04 | ||||||||
| Cholesterol to HDL | r | 1 | |||||||
| P | |||||||||
There are significant differences between * and **
Table 3.
Bivariate analysis for presented parameters in healthy controls
| Parameters | Total Cholesterol | Triglyceride | HDL-Cholesterol | LDL- Cholesterol | HbA1C | Glucose | AIP | Cholesterol to HDL | |
|---|---|---|---|---|---|---|---|---|---|
| Total Cholesterol | r | 1 | -0.70** | 0.752** | 0.103 | 0.497* | 0.098 | -0.93** | -0.529 |
| P | 0.001 | 0.000 | .0026 | 0.001 | |||||
| Triglyceride | r | 1 | -0.79** | -0.008 | -0.597** | 0.177 | 0.905** | 0.409 | |
| P | 0.000 | 0.005 | 0.002 | ||||||
| HDL Cholesterol | r | 1 | -0.133 | 0.584** | 0.250 | -0.912** | -0.875** | ||
| P | 0.007 | 0.002 | 0.004 | ||||||
| LDL Cholesterol | r | 1 | -0.230 | -0.236 | -0.354 | 0.214 | |||
| P | |||||||||
| HbA1C | r | 1 | 0.212 | -0.643 | -0.659 | ||||
| P | |||||||||
| Glucose | r | 1 | 0.103 | -0.480 | |||||
| P | |||||||||
| AIP | r | 1 | 0.675 | ||||||
| P | |||||||||
| Cholesterol to HDL | r | 1 | |||||||
| P | |||||||||
There are significant differences between * and **
The cluster analysis using the words method of glucose, HbA1C, total cholesterol, triglyceride, HDL cholesterol, LDL cholesterol, VLDL cholesterol, atherogenic index, and total-cholesterol-to-HDL ratio in COVID-19 patients compared to controls are presented in figures 2 and 3, respectively. The study parameters were organized in five clusters in COVID-19 patients. First cluster included AIP, HDL-cholesterol, cholesterol to HDL ratio, and HbA1C. The second cluster included the combination of AIP, total cholesterol, triglyceride, and LDL-cholesterol. The rest of the clusters were ordered (i.e., total cholesterol, triglyceride, and LDL-cholesterol) in one group, and triglyceride and LDL-cholesterol were ordered in another group. Eventually, total cholesterol and glucose were ordered in one group.
Figure 2.
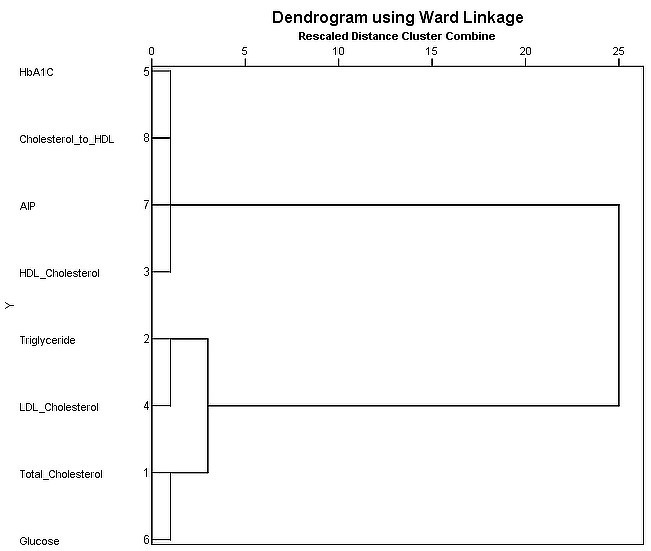
Cluster analysis for presented parameters in COVID-19 patients
Figure 3.
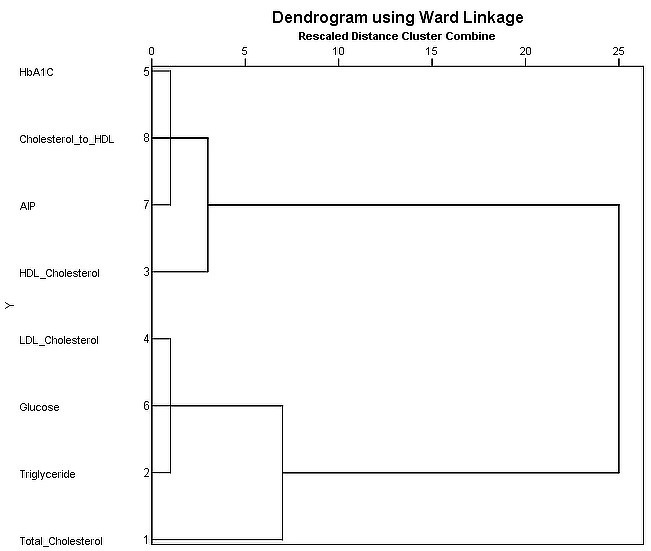
Cluster analysis of presented parameters in healthy controls
In the control group, atherogenic index was positively correlated with triglyceride (r=0.9, P=0.002), total cholesterol (r=-0.93, P=0.00), and HDL cholesterol (r=-0.9, P=0.002) (Table 3). In addition, total cholesterol was positively correlated with HDL cholesterol (r=0.7, P=0.00), triglyceride (r=0.7, P=0.00), and HbA1C (r=0.4, P=0.02). Significant correlations were identified in triglyceride to HDL-cholesterol (r=0.79, P=0.00), triglyceride to HbAIC (r=-0.5, P=0.005), HDL-cholesterol to HbAIC (r=0.58, P=0.007), HDL cholesterol to cholesterol to HDL ratio (r=-0.87, P=0.004). The other parameters had no significant association with each other. Whereas HbA1C levels was observed to be inversely associated with triglyceride, LDL cholesterol, HDL cholesterol, and total cholesterol levels.
The study parameters were organized into five clusters in healthy controls. The first cluster included AIP, cholesterol to HDL ratio, and HbA1C. The second cluster included the combination of cholesterol to HDL ratio and HDL cholesterol. The third cluster included cholesterol to HDL ratio, HDL cholesterol, total cholesterol, and glucose. The fourth cluster included triglyceride, glucose, and LDL cholesterol, and the last cluster included total cholesterol and glucose.
Bacterial or fungal infections caused a decrease in total cholesterol, low-density lipoprotein, high-density lipoprotein, and elevated triglyceride ( 26 ). This phenomenon appeared in viral infection as well, and the findings of several studies confirmed our results in the present study ( 27 - 30 ).
In conclusion, the results of this study indicated that the risk factor for the cardiovascular disease increased in patients with COVID-19 by an increase in the atherogenic index, cholesterol to HDL ratio, and the high association between atherogenic index, and their organization in one cluster. Therefore, lipids may play an important physiological role in patients with COVID-19 infection. We also speculate that the lipid abnormalities observed in COVID-19 patients and healthy controls can be used to assess indirect cardiac status.
Authors' Contribution
E. M. T., M. M. T., and S. M. R. conceived the present idea. E. M. T. and S. K. A. carried out the experiment. E. M. T., M. M. T., S. K. Al., S. M. R., and B. F.s contributed to the final version of the manuscript
Ethics
The study protocol was approved by the Ethical Committee of the College of Science for Women at the University of Baghdad, Baghdad, Iraq. The study was performed in accordance with the ethical standard as laid down in the 1964 declaration of Helsinki and its later amendments or comparable ethical standards, and the researchers followed the Iraqi ministry of health protocols. Informed consent was obtained from all individual participants.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgment
The authors would like to express gratitude to authorities at the University of Baghdad, College of Science for Women, and Erbil International Hospital in Erbil, Iraq.
References
- 1.Jeppesen S, Miklian J, editors. Introduction: Research in the Time of Covid-19. Forum for Development Studies; 2020: Taylor amp; Francis. [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng W, Liu G, Ma H, Zhao D, Yang Y, Liu M, et al. Biochemical characterization of SARS-CoV-2 nucleocapsid protein. Biochem Biophys Res Commun. 2020;527(3):618–23. doi: 10.1016/j.bbrc.2020.04.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang Y, Yang C, Xu X-f, Xu W, Liu S-w. Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharmacol Sin. 2020;41(9):1141–9. doi: 10.1038/s41401-020-0485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shang J, Wan Y, Luo C, Ye G, Geng Q, Auerbach A, et al. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci U S A. 2020;117(21):11727–34. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shattat GF. A review article on hyperlipidemia: types, treatments and new drug targets. Biomed Pharmacol J. 2015;7(1):399–409. [Google Scholar]
- 7.Orozco-Beltran D, Gil-Guillen VF, Redon J, Martin-Moreno JM, Pallares-Carratala V, Navarro-Perez J, et al. Lipid profile, cardiovascular disease and mortality in a Mediterranean high-risk population: The ESCARVAL-RISK study. PLoS One. 2017;12(10):e0186196. doi: 10.1371/journal.pone.0186196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sami Khaza M. Atherogenic index of plasma (AIP) as a parameter in predicting cardiovascular risk in males compared to the conventional dyslipidemic indices (cholesterol ratios) Kerbala J Med. 2013;6(1):1506–13. [Google Scholar]
- 9.Dayimu A, Wang C, Li J, Fan B, Ji X, Zhang T, et al. Trajectories of lipids profile and incident cardiovascular disease risk: a longitudinal cohort study. J Am Heart Assoc. 2019;8(21):013479. doi: 10.1161/JAHA.119.013479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niroumand S, Khajedaluee M, Khadem-Rezaiyan M, Abrishami M, Juya M, Khodaee G, et al. Atherogenic Index of Plasma (AIP): A marker of cardiovascular disease. Med J Islam Repub Iran. 2015;29:240. [PMC free article] [PubMed] [Google Scholar]
- 11.Quispe R, Elshazly MB, Zhao D, Toth PP, Puri R, Virani SS, et al. Total cholesterol/HDL-cholesterol ratio discordance with LDL-cholesterol and non-HDL-cholesterol and incidence of atherosclerotic cardiovascular disease in primary prevention: The ARIC study. Eur J Prev Cardiol. 2020;27(15):1597–605. doi: 10.1177/2047487319862401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dildar S, Imran S, Naz F. Method comparison of Particle Enhanced Immunoturbidimetry (PEIT) with High Performance Liquid Chromatography (HPLC) for glycated hemoglobin (HbA1c) analysis. Clin Diabetes Endocrinol. 2021;7(1):1–5. doi: 10.1186/s40842-021-00123-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu X, Chen D, Wu L, He G, Ye W. Declined serum high density lipoprotein cholesterol is associated with the severity of COVID-19 infection. Clinica Chimica Acta. 2020;510:105–10. doi: 10.1016/j.cca.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu X, Chen D, Wu L, He G, Ye W. Low serum cholesterol level among patients with COVID-19 infection in Wenzhou, China. China (February 21, 2020) 2020 [Google Scholar]
- 15.Roccaforte V, Daves M, Lippi G, Spreafico M, Bonato C. Altered lipid profile in patients with COVID-19 infection. J Lab Precis Med. 2020 [Google Scholar]
- 16.Wang G, Zhang Q, Zhao X, Dong H, Wu C, Wu F, et al. Low high-density lipoprotein level is correlated with the severity of COVID-19 patients: an observational study. Lipids Health Dis. 2020;19(1):1–7. doi: 10.1186/s12944-020-01382-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilser JR, Han Y, Biswas S, Gukasyan J, Cai Z, Zhu R, et al. Association of serum HDL-cholesterol and apolipoprotein A1 levels with risk of severe SARS-CoV-2 infection. J Lipid Res. 2021;62 doi: 10.1016/j.jlr.2021.100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thacker SG, Zarzour A, Chen Y, Alcicek MS, Freeman LA, Sviridov DO, et al. High‐density lipoprotein reduces inflammation from cholesterol crystals by inhibiting inflammasome activation. Immunology. 2016;149(3):306–19. doi: 10.1111/imm.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang G, Deng J, Li J, Wu C, Dong H, Wu S, et al. The Role of High-Density Lipoprotein in COVID-19. Front Pharmacol. :2021–1847. doi: 10.3389/fphar.2021.720283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeGoma EM, degoma RL, Rader DJ. Beyond high-density lipoprotein cholesterol levels: evaluating high-density lipoprotein function as influenced by novel therapeutic approaches. J Am Coll Cardiol. 2008;51(23):2199–211. doi: 10.1016/j.jacc.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Navab M, Reddy ST, Van Lenten BJ, Fogelman AM. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011;8(4):222–32. doi: 10.1038/nrcardio.2010.222. [DOI] [PubMed] [Google Scholar]
- 22.Baglivo M, Baronio M, Natalini G, Beccari T, Chiurazzi P, Fulcheri E, et al. Natural small molecules as inhibitors of coronavirus lipid-dependent attachment to host cells: a possible strategy for reducing SARS-COV-2 infectivity? . Acta Biomed. 2020;91(1):161. doi: 10.23750/abm.v91i1.9402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yıldırım ÖT, Kaya Ş. The atherogenic index of plasma as a predictor of mortality in patients with COVID-19. Heart & Lung. 2021;50(2):329–33. doi: 10.1016/j.hrtlng.2021.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kočar E, Režen T, Rozman D. Cholesterol, lipoproteins, and COVID-19: Basic concepts and clinical applications. Biochim Biophys Acta Mol Cell Biol Lipids Bba-Mol Cell Biol L. 2021;1866(2):158849. doi: 10.1016/j.bbalip.2020.158849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alcántara-Alonso E, Molinar-Ramos F, González-López JA, Alcántara-Alonso V, Muñoz-Pérez MA, Lozano-Nuevo JJ, et al. High triglyceride to HDL-cholesterol ratio as a biochemical marker of severe outcomes in COVID-19 patients. Clin Nutr ESPEN. 2021 doi: 10.1016/j.clnesp.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feingold KR. The bidirectional link between HDL and COVID-19 infections. J Lipid Res. 2021;62 doi: 10.1016/j.jlr.2021.100067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang S, Zhou C, Yuan Z, Xiao H, Wu X. The clinical value of high-density lipoprotein in the evaluation of new coronavirus pneumonia. Adv Clin Exp Med. 2021;30(2):153–6. doi: 10.17219/acem/130606. [DOI] [PubMed] [Google Scholar]
- 28.Tanaka S, De Tymowski C, Assadi M, Zappella N, Jean-Baptiste S, Robert T, et al. Lipoprotein concentrations over time in the intensive care unit COVID-19 patients: Results from the ApoCOVID study. PLoS One. 2020;15(9):e0239573. doi: 10.1371/journal.pone.0239573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wei X, Zeng W, Su J, Wan H, Yu X, Cao X, et al. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol. 2020;14(3):297–304. doi: 10.1016/j.jacl.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yue J, Xu H, Zhou Y, Liu W, Han X, Mao Q, et al. Dyslipidemia is related to mortality in critical patients with coronavirus disease 2019: a retrospective study. Front Endocrinol. 2021;12 doi: 10.3389/fendo.2021.611526. [DOI] [PMC free article] [PubMed] [Google Scholar]


