Abstract
Preliminary prospective research suggests emotion dysregulation may confer vulnerability to poor stress responses. The present prospective study extends this research by examining both specific emotion regulation strategies and global emotion regulation difficulties in the context of acute stress following onset of the COVID-19 global pandemic in 119 young adults. As part of a larger study, emotion regulation was assessed prior to pandemic onset (January 2019 – February 2020) using two standard measures (Emotion Regulation Questionnaire, ERQ, Gross & John, 2003; Difficulties in Emotion Regulation Scale, DERS, Gratz & Roemer, 2004). A self-report assessment of acute stress was conducted 2−3½ weeks after the COVID-19 pandemic declaration. Results demonstrated cognitive reappraisal and expressive suppression (i.e., ERQ) were not individually predictive of acute stress; however, there was a significant interaction of suppression by reappraisal. Simple effects indicated suppression was negatively associated with acute stress only when reappraisal levels were high. Greater global emotion regulation difficulties (i.e., DERS), particularly nonacceptance of emotions and limited access to emotion regulation strategies, significantly predicted greater acute stress. These results provide further evidence of the temporal relationship between emotion dysregulation and stress reactions, and also suggest the expected effects of emotion regulation strategies may differ across contexts.
Keywords: Emotion regulation, Acute stress, Coronavirus, COVID-19, Prospective research
1. Introduction
The experience of psychological stress is typically associated with heightened negative emotions, which over time, have been shown to be a risk factor for adverse mental and physical health outcomes (e.g., Cohen, Gianaros, & Manuck, 2016; Cohen, Janicki-Deverts, & Miller, 2007; Lupien, McEwen, Gunnar, & Heim, 2009). Individual differences in psychological responses to stress can determine the extent to which stress exposure contributes to negative consequences, such as greater negative emotionality, intrusive thoughts, memories, and avoidance (Bardeen, Fergus, & Wu, 2013; Bovin & Marx, 2011; Kumpula, Orcutt, Bardeen, & Varkovitzky, 2011).
One factor that appears to contribute to a poor stress response, both in the acute phase and long-term, is individual differences in emotion regulation (e.g., Frewen & Lanius, 2006; Litz, Orsillo, Kaloupek, & Weathers, 2000; Seligowski, Lee, Bardeen, & Orcutt, 2015; Wang & Saudino, 2011). Emotion regulation is often categorized into types of regulatory strategies, specifically antecedent or response-focused (i.e., either employed before or after an emotional response is fully generated; Gross, 1998). While many emotion regulation strategies have been identified (for review, see Webb, Miles, & Sheeran, 2012), cognitive reappraisal and expressive suppression are the most commonly examined (Gross & John, 2003). Cognitive reappraisal, an antecedent approach, requires the adaptive use of cognitive effort to modify the appraisal of a situation and subsequently alter the emotional response before it fully occurs. In contrast, expressive suppression is a response-focused approach involving a maladaptive behavioral attempt to inhibit the expression of an emotional response that is already in progress (Gross & John, 2003). Research has demonstrated that negative responses following potentially traumatic events are often associated with greater use of response-focused strategies such as expressive suppression, whereas antecedent-focused strategies such as cognitive reappraisal are typically under-utilized (Boden et al., 2013; Eftekhari, Zoellner, & Vigil, 2009; Ehlers & Clark, 2000; Ehring & Quack, 2010; Feeny & Foa, 2005; Marx & Sloan, 2005; Moore, Zoellner, & Mollenholt, 2008; Shepherd & Wild, 2014). The use of expressive suppression may prevent necessary emotional processing of a potentially traumatic event, thus perpetuating and maintaining symptom severity (Clohessy & Ehlers, 1999). Cognitive conceptual models suggest that an inability to effectively reappraise the potentially traumatic event and subsequent symptoms is critical to symptom severity maintenance (e.g., Ehlers, Maercker, & Boos, 2000; Ehlers, Mayou, & Bryant, 1998).
While previous research tends to examine these two strategies separately, and indeed factor analyses have shown that expressive suppression and cognitive reappraisal are independent constructs (Moore et al., 2008), the findings of other studies suggest the interaction between cognitive reappraisal and expressive suppression should be considered. For example, a recent study demonstrated that low levels of cognitive reappraisal moderated a positive relationship between expressive suppression and cortisol reactivity and recovery from an acute laboratory stress task (Raymond, Marin, Juster, & Lupien, 2019). In other words, expressive suppression was associated with greater cortisol reactivity and recovery only in individuals reporting low levels of habitual cognitive reappraisal. Another study examining women with/without trauma exposure, found that the combination of high cognitive reappraisal and low expressive suppression was protective, resulting in the lowest reports of anxiety, depression, and posttraumatic stress (Eftekhari et al., 2009). While greater use of expressive suppression is generally associated with negative outcomes (e.g., more negative affect, greater anxiety, depression), it appears from these previous studies that greater simultaneous use of cognitive reappraisal may buffer such effects.
Instead of focusing on the use of specific emotion regulation strategies, other conceptualizations emphasize that effective emotion regulation can be viewed in the context of global emotion regulation difficulties (Gratz & Roemer, 2004). Core difficulties include lack of awareness, understanding, and acceptance of emotions, inability to control behavioral impulses or engage in goal-related behavior, and lack of perceived access to effective emotion regulation strategies (Gratz & Tull, 2010). Global dimensions of emotion regulation difficulties have been associated with increased negative emotionality (Allan, Norr, Macatee, Gajewska, & Schmidt, 2015; Bardeen, Fergus, & Orcutt, 2012; Fowler et al., 2014; Pollock, McCabe, Southard, & Zeigler-Hill, 2016; Ritschel, Tone, Schoemann, & Lim, 2015; Roemer et al., 2009; Roy, Riley, & Sinha, 2018; Ruganci & Gençöz, 2010; Salsman & Linehan, 2012; Salters-Pedneault, Roemer, Tull, Rucker, & Mennin, 2006). With regards to reactions to potentially traumatic events, research suggests that a disruption in affect regulatory processes is a primary mechanism in the development and maintenance of sustained symptom severity (Brewin, Dalgleish, & Joseph, 1996; Ehlers & Clark, 2000; Foa & Kozak, 1986; Frewen & Lanius, 2006). Indeed, cross-sectional research has demonstrated that greater global emotion regulation difficulties are associated with greater stress reactions following a potentially traumatic event (e.g., Badour & Feldner, 2013; Barlow, Goldsmith Turow, & Gerhart, 2017; Ehring & Quack, 2010; Pugach, Campbell, & Wisco, 2020; Sundermann & DePrince, 2015; Tull, Barrett, McMillan, & Roemer, 2007; Viana et al., 2017; Woodward et al., 2020). Conceptually, individuals who are unable to effectively regulate their emotions may be more likely to appraise stressors as threatening and may also experience prolonged recovery from stress due to the inability to attenuate emotional distress and arousal (Bardeen, Kumpula, & Orcutt, 2013; Bouton, Mineka, & Barlow, 2001; Frewen & Lanius, 2006). The perceived inability to effectively regulate emotional experiences can then lead to fear and subsequent avoidance of further stress or trauma reminders, thus preventing habituation and recovery (Foa & Kozak, 1986).
Whereas individual differences in emotion regulation strategies and global emotion regulation difficulties putatively serve as a vulnerability to greater stress responses following a potentially traumatic event, the overwhelming majority of existing studies have used cross-sectional study designs. A lack of prospective research in this area limits the ability to draw conclusions (for a meta-analytic review, refer to Seligowski et al., 2015). However, one prospective study demonstrated that global emotion regulation difficulties, assessed using Gratz and Roemer’s (2004) conceptualization, prior to a mass-shooting on a college campus predicted subsequent stress reactions both in the acute aftermath of the shooting and in the longer-term (Bardeen, Kumpula et al., 2013). In another study, Bonanno, Papa, Lalande, Westphal, and Coifman (2004) recruited a sample of first year New York college students immediately after the 9/11 terrorist attacks, and experimentally examined whether the ability to enhance or suppress emotional responses to unpleasant imagery in the laboratory prospectively predicted psychological distress by the end of their second year. Interestingly, those who were able to both enhance or suppress negative emotional expression upon instruction demonstrated less psychological distress two years post the attacks. That said, no known study to date has directly examined the predictive value of the characteristic use of expressive suppression or cognitive reappraisal on the later development of stress reactions through a prospective study design.
The recent outbreak of the COVID-19 pandemic offered a unique way to prospectively examine the relationships between individual differences in emotion regulation strategies and global emotion regulation difficulties with later reported acute stress during the initial stages of the pandemic. The first COVID-19 case was reported in December 2019 in China and has since spread across the globe, resulting in 62,363,527 confirmed cases and 1,456,687 deaths reported to date worldwide (November 30, 2020; World Health Organization, 2020). The coronavirus COVID-19 was declared a global pandemic on March 11, 2020 (World Health Organization, 2020) and a U.S. national emergency on March 17, 2020 (Centers for Disease Control & Prevention, 2020). The negative psychological effects of COVID-19 have been well-documented, including increases in psychological distress, anxiety, depression, and stress (Brooks et al., 2020; Cao et al., 2020; Karatzias et al., 2020; Liu, Zhang, Wong, Hyun, & “Chris.” Hahm, 2020; Qiu et al., 2020; Rajkumar, 2020; Restubog, Ocampo, & Wang, 2020; Rossi et al., 2020; Wang, Pan, Wan, Tan, Xu, McIntyre et al., 2020). Stress responses are important to study in the context of life-threatening medical events, inclusive of the COVID-19 pandemic (Taylor & Asmundson, 2020), as individuals differ in their responses to those events (Galatzer-Levy, Huang, & Bonanno, 2018). Acute stress reactions following a potentially traumatic event (i.e., occurring within the first month) are one area of interest because those reactions can be useful for identifying individuals who may benefit from early intervention or subsequent monitoring (Bryant et al., 2014).
The present study aims to extend previous cross-sectional research by using a prospective design to assess whether individual differences in emotion regulation strategies, as well as difficulties, predict reported acute stress during a global pandemic. Measures of emotion regulation strategies and global emotion regulation difficulties were taken prior to the onset of the global pandemic (January 2019 – February 2020) and acute stress was assessed 2−3½ weeks after COVID-19 was declared a global pandemic. It was hypothesized that participants who report greater use of expressive suppression as an emotion regulation strategy would later report greater acute stress in response to the pandemic, whereas participants who report greater use of cognitive reappraisal as an emotion regulation strategy would later report less acute stress. Based on prior research suggesting that greater use of cognitive reappraisal can buffer against the negative effects of greater expressive suppression use (e.g., Eftekhari et al., 2009; Raymond et al., 2019), the interaction between cognitive reappraisal and expressive suppression was also examined. It was predicted that higher use of cognitive reappraisal would moderate (i.e., protect against) the proposed positive relationship between use of expressive suppression and later reported acute stress. Lastly, it was predicted that participants who report more global emotion regulation difficulties will later report greater acute stress (e.g., Bardeen, Kumpula et al., 2013).
2. Method
2.1. Participants and procedures
One hundred twenty-four young adults participated in the study. Participants were part of a larger study taking place between January 2019 and February 2020 (Phase 1). All participants from the larger study were contacted via email and phone (text messages) to participate in the present study (N = 457). One hundred and twenty-four participants opted to enroll in the present study. Five of the 124 participants who completed the present study were excluded from final data analyses due to missing data at either Phase 1 (n = 3) or Phase 2 (n = 2), resulting in a final total of 119 participants (M age = 19.40, SD = 0.95 years; 71.4 % female; 68.9 % Caucasian; 22.7 % Hispanic/Latino). Surveys at Phase 1 included measures of the following: demographics, adverse childhood experiences, personality (i.e., neuroticism), anxiety, depression, and emotion regulation. The present study (Phase 2) occurred between March 26, 2020 and April 5, 2020, approximately 2−3½ weeks after the COVID-19 pandemic declaration. Surveys at Phase 2 consisted of measures of COVID-19 related acute stress and perceived severity of infection. While Phase 1 took place in Central Texas, participants were located in 22 different states during the Phase 2 follow up and 89.1 % of the sample resided in a location with a “shelter in place” order. None of the participants had tested positive for COVID-19. Participants received course credit for completion of Phase 1 and were entered in a raffle to win a $25 gift card (15 cards available) for their completion of Phase 2. This study was approved by the university’s Institutional Review Board. All participants provided informed consent prior to both phases of the study and had the right to withdraw at any point.
2.2. Covariates
To assess the robustness of the proposed relationships, variables known to be risk factors for the development of stress reactions following potentially traumatic events, as well as associated with emotion dysregulation, were identified and controlled in the present study, including anxiety and depression (e.g., Amstadter, 2008; Campbell-Sills, Ellard, & Barlow, 2014; Christiansen & Elklit, 2008; Joormann & Stanton, 2016; O’toole, Marshall, Schureck, & Dobson, 1998), adverse childhood experiences (e.g., Burns, Jackson, & Harding, 2010; England-Mason et al., 2017; Lilly, London, & Bridgett, 2014; Weiss, Tull, Lavender, & Gratz, 2013), and neuroticism (e.g., Breslau & Schultz, 2013; Silverman et al., 2019). Demographic variables (sex, race, ethnicity, socioeconomic status) were also assessed and controlled based on the control procedures of previous, similar studies (e.g., Bardeen, Kumpula et al., 2013; Weiss et al., 2013). Lastly, perceived severity of potential COVID-19 infection was controlled to ensure that beliefs about COVID-19 did not influence stress outcomes in this study.
2.3. Measures
2.3.1. Emotion regulation
The Emotion Regulation Questionnaire (ERQ; Gross & John, 2003) is a 10-item self-report questionnaire that is divided into two subscales, which can be separately utilized to assess the use of two key emotion regulation strategies: cognitive reappraisal (six items) and expressive suppression (four items). The cognitive reappraisal subscale includes items such as, “I control my emotions by changing the way I think about the situation I’m in”, and the expressive suppression subscale includes items such as “When I am feeling negative emotions, I make sure not to express them”. Participants respond to each item using a 7-point ordered-category scale (1 = strongly disagree to 7 = strongly agree), with higher subscale scores indicating higher use of that strategy. In the present sample, internal consistency was acceptable for both ERQ subscales (Cronbach’s ⍺ for cognitive reappraisal = .79; expressive suppression = .74).
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report questionnaire that assesses general difficulties with regulating emotions (total score) as well as six domain-specific difficulties: (1) nonacceptance of emotional responses; (2) difficulties in engaging in goal-directed behavior; (3) impulse control difficulties; (4) lack of emotional awareness; (5) limited access to emotion regulation strategies; and (6) emotional clarity. Participants respond to each item utilizing a 5-point ordered-category scale (1 = almost never to 5 = almost always). Example items include, “When I am upset, I become irritated at myself for feeling that way” and “When I am upset, I believe that I will remain that way for a long time”. An overall total score and six subscale scores were obtained, with higher scores representing increased difficulty in regulation of emotions. In the present sample, the DERS had high overall internal consistency (⍺ = .93) as well as good internal consistency within each subscale (⍺ ≥ .80). Both the DERS and the ERQ were assessed during Phase 1 of the study.
2.3.2. COVID-19 related acute stress
The Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997) is a 22-item questionnaire that is used to assess subjective stress reactions in response to a specific event (in this case, the COVID-19 pandemic). Each individual item depicts a possible difficulty that one may encounter after experiencing the respective stressful event. Participants were requested to indicate on a 5-point ordered-category scale (0 = not at all to 4 = extremely) how much distress they experienced, with respect to each item, during the past seven days with regards to the ongoing COVID-19 pandemic. Example items include, “I thought about it when I didn’t mean to,” “I stayed away from reminders of it,” and “I felt watchful and on guard”. Items can be grouped into three subscales (intrusion, avoidance, and hyperarousal). However, the current study focused primarily on the total score, which can be obtained by summing all the items (0–88) and revealed high internal consistency in the current sample (⍺ = .92). Given that 1) the COVID-19 pandemic was in the initial stages during data collection, and therefore not “post” the traumatic event, and 2) the questionnaire asked people to rate their answers on the past seven days, rather than the past month as it states in the DSM-5 for posttraumatic stress disorder (PTSD) diagnosis, the IES-R should be conceptualized as an assessment of “acute stress” rather than PTSD in the present study (American Psychiatric Association, 2013; Asmundson & Taylor, 2021). The IES-R was given during Phase 2 of the current study.
2.3.3. Perceived severity of COVID-19 infection
Perceived severity of COVID-19 infection was assessed and controlled for using a single item, which was extracted from the 10-item Swine Flu inventory (item #7; Wheaton, Abramowitz, Berman, Fabricant, & Olatunji, 2012). The original item was adapted for the current study by replacing the wording “Swine” with “coronavirus COVID-19” (i.e., “If you did become infected with coronavirus COVID-19, to what extent are you concerned that you will be severely ill?”). Participants responded on a 5-point ordered-category scale (0 = very little to 4 = very much). This item was given during Phase 2 of the study.
2.3.4. Anxiety and depression
The Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) consists of 14 items, which are evenly separated into an anxiety subscale and a depression subscale. Using a four-point ordered-category scale (0–3), participants were asked to rate each item with regards to how they have been feeling in the past week. Higher scores indicate higher depression or anxiety. In the current sample, internal consistency was acceptable (⍺ for anxiety = 0.81; depression = 0.69). The HADS questionnaire was given at Phase 1 of the current study.
2.3.5. Adverse childhood experiences
The Adverse Childhood Experiences (ACEs; Felitti et al., 1998) questionnaire was used to assess and control for three domains of adverse childhood experiences before the age of 18 years (i.e., abuse, neglect, household dysfunction). The ACE questionnaire consists of 10-items which reflect 10 types of childhood adversity, to which participants respond yes or no (1 = yes, 0 = no). The responses are then summed to create a total ACE score (0–10); higher scores reflect a greater number of adverse experiences. The Cronbach’s ⍺ in the current sample was .67. The ACE questionnaire was administered during Phase 1.
2.3.6. Neuroticism
Trait neuroticism was measured and controlled for using the neuroticism subscale of the Big Five Inventory (John & Srivastava, 1999), a 44-item inventory used to measure the Big Five Factors of personality (Goldberg, 1993). The neuroticism subscale consists of 8 items and participants respond on a 5-point ordered-category scale (1 = disagree strongly to 5 = agree strongly). In the current study, the neuroticism subscale showed good internal consistency (⍺ = .87). This subscale was administered during Phase 1.
2.4. Statistical analyses
Pearson’s product-moment correlations were utilized to assess the associations between the main variables of interest. A hierarchal linear regression was conducted to examine if individual differences in emotion regulation (strategies and global difficulties) during Phase 1 significantly and independently predicted COVID-19 related acute stress (IES-R total) during Phase 2, while also adjusting for perceived severity of COVID-19 infection, sex, race, ethnicity, socioeconomic status (SES), adverse childhood experiences, anxiety, depression, and neuroticism. The emotion regulation variables of interest were together entered into Step 2 (ERQ expressive suppression, ERQ cognitive reappraisal, and DERS total score), while all covariates were entered into Step 1. A follow up model was conducted via PROCESS for SPSS (Version 3.5; Hayes, 2017) to examine the predictive value of a mean-centered interaction term between ERQ expressive suppression and ERQ cognitive reappraisal on IES-R total score (e.g., Eftekhari et al., 2009; Raymond et al., 2019), over and above all covariates, DERS global emotion regulation difficulties, ERQ expressive suppression, and ERQ cognitive reappraisal. If a significant interaction was found, simple slope tests were examined via PROCESS to further break down and understand the interaction effect (Hayes, 2017). Lastly, in order to assess whether different dimensions of global emotion regulation difficulties significantly predicted COVID-19 related acute stress, six supplemental hierarchal linear regression models were employed to separately examine the unique predictive value of each of the six DERS subscales (individually entered into Step 2) while also controlling for covariates, cognitive reappraisal, and expressive suppression in Step 1. All analyses were conducted using standardized predictors. Results were reported as statistically significant if p values were ≤ .05. SPSS version 27 (IBM Corp, USA) was used for analyses.
3. Results
3.1. Preliminary analyses
Means and standard deviations for the main variables of interest as well as covariates are presented in Table 1 . Pearson’s product-moment correlations indicated a statistically significant positive association between DERS total and IES-R total, as well as between four of the DERS subscales and IES-R total; DERS awareness and DERS goal-directed behavior were not statistically significantly associated with IES-R total. Neither ERQ cognitive reappraisal nor ERQ expressive suppression were statistically significantly associated with IES-R total; however, cognitive reappraisal was statistically significantly and negatively associated with DERS total, while expressive suppression was not. A statistically significant, yet small association was found between cognitive reappraisal and expressive suppression, demonstrating relative independence between the two subscales. Perceptions of COVID-19 infection severity were statistically significantly associated with IES-R total. While SES was not associated with IES-R total, it was negatively associated with the DERS total. Adverse childhood experiences, neuroticism, anxiety, and depression were all statistically significantly and positively associated with IES-R total. Table 2 presents a detailed correlation matrix.
Table 1.
Mean, standard deviation, minimum, and maximum of main study variables.
| Mean (SD) | Min - Max | |
|---|---|---|
| Main variables of interest | ||
| IES-R Total | 21.14 (14.25) | 0.00−63.00 |
| ERQ Reappraisal | 5.15 (0.88) | 2.00−7.00 |
| ERQ Suppression | 4.22 (1.24) | 1.25−6.75 |
| DERS Total | 86.18 (20.82) | 36.00−149.00 |
| DERS Nonacceptance | 14.60 (6.28) | 6.00−30.00 |
| DERS Strategies | 17.39 (6.49) | 8.00−35.00 |
| DERS Goal-Directed | 15.23 (4.44) | 5.00−25.00 |
| DERS Impulsive | 11.69 (4.70) | 6.00−27.00 |
| DERS Awareness | 15.11 (4.76) | 6.00−30.00 |
| DERS Clarity | 12.19 (3.79) | 5.00−22.00 |
| Covariates | ||
| COVID-19 severity | 2.74 (1.20) | 1.00−5.00 |
| SES | 5.93 (1.21) | 2.00−7.00 |
| ACE Total | 1.47 (1.71) | 0.00−6.00 |
| BFI Neuroticism | 2.95 (0.85) | 1.00−4.63 |
| HADS Anxiety | 8.44 (3.92) | 0.00−19.00 |
| HADS Depression | 4.29 (2.79) | 0.00−14.00 |
Note. COVID-19 severity = perceived severity of potential COVID-19 infection.
Table 2.
Correlations between emotion regulation variables with other study related variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. IES-R Total | __ | −.093 | −.020 | .329** | .292** | .312** | .156 | .244** | .068 | .218* | .246** | −.042 | .193* | .246** | .363** | .256** |
| 2. ERQ Reappraisal | __ | .190* | −.310** | −.117 | −.277** | −.252** | −.142 | −.262** | −.235** | .010 | −.073 | −.096 | −.317** | −.243** | −.279** | |
| 3. ERQ Suppression | __ | .134 | .159 | .004 | −.181* | .074 | .275** | .237** | −.014 | .078 | −.170 | −.154 | .003 | .071 | ||
| 4. DERS Total | __ | .761** | .852** | .648** | .719** | .389** | .634** | .141 | −.242** | .215* | .568** | .547** | .498** | |||
| 5. DERS Nonacceptance | __ | .552** | .394** | .422** | .237** | .294** | .105 | −.243** | .180 | .368** | .364** | .314** | ||||
| 6. DERS Strategies | __ | .611** | .659** | .076 | .424** | .214* | −.276** | .265** | .605** | .480** | .485** | |||||
| 7. DERS Goal-Directed | __ | .467** | −.062 | .189* | .118 | −.195* | .086 | .546** | .344** | .284** | ||||||
| 8. DERS Impulsive | __ | −.031 | .374** | .166 | −.155 | .089 | .379** | .380** | .406** | |||||||
| 9. DERS-Awareness | __ | .466** | −.107 | −.005 | .094 | .051 | .198* | .176 | ||||||||
| 10. DERS-Clarity | __ | .024 | −.027 | .097 | .297** | .454** | .324** | |||||||||
| 11. COVID-19 severity | __ | −.224* | .052 | .232* | .120 | .150 | ||||||||||
| 12. SES | __ | −.314** | −.271** | −.132 | −.188* | |||||||||||
| 13. ACE Total | __ | .229* | .280** | .332** | ||||||||||||
| 14. BFI Neuroticism | __ | .649** | .449** | |||||||||||||
| 15. HADS Anxiety | __ | .537** | ||||||||||||||
| 16. HADS Depression | __ |
Note. COVID-19 severity denotes perceived severity of a COVID-19 infection; *denotes p < .05, ** denotes p < .001.
3.2. Cognitive reappraisal, expressive suppression, global emotion regulation difficulties, and COVID-19 related acute stress
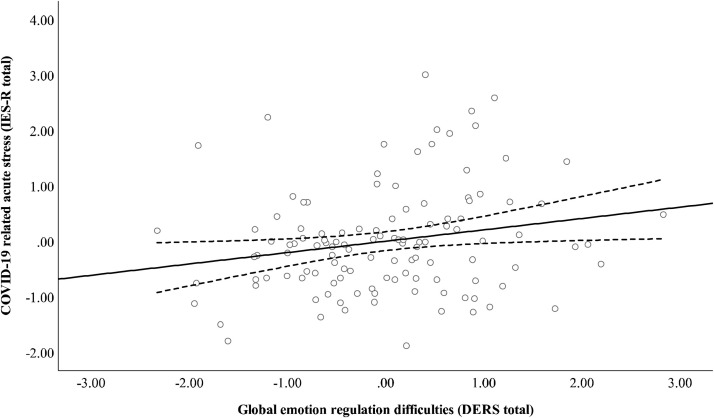
The covariates together explained 17.8 % of the variance in acute stress, F(9, 109) = 3.83, p < .001. The addition of ERQ cognitive reappraisal, ERQ expressive suppression, and global emotion regulation difficulties in Step 2 explained an additional 1.2 % of the variance in acute stress, F(12, 106) = 3.31, p < .001. However, only global emotion regulation difficulties (DERS total) was a statistically significant predictor of interest, such that greater global emotion regulation difficulties predicted greater acute stress, B = .17, p = .033, 95 % CI [0.01, 0.33]. Both ERQ cognitive reappraisal, B = .70, p = .650, 95 % CI [−2.34, 3.74] and ERQ expressive suppression, B = −.71, p = .507, 95 % CI [−2.81, 1.40] were not statistically significant unique predictors of acute stress. Table 3 reports the full regression analysis and Fig. 1 demonstrates the positive prospective relationship between global emotion regulation difficulties and acute stress.
Table 3.
Regression model for reappraisal, suppression, and global emotion regulation difficulties predicting acute stress (IES-R), N = 119.
| Acute Stress |
|||||
|---|---|---|---|---|---|
| Model | B | SE | β | t | p |
| Step 1 | |||||
| Sex | −0.60 | 3.00 | −0.02 | −0.20 | .841 |
| Race | −1.31 | 0.54 | −0.22 | −2.42 | .017 |
| Ethnicity | 5.22 | 3.10 | 0.15 | 1.68 | .095 |
| SES | 0.58 | 1.12 | 0.05 | 0.52 | .603 |
| COVID-19 severity | 3.21 | 1.07 | 0.27 | 3.00 | .003 |
| ACE Total | 0.89 | 0.78 | 0.11 | 1.14 | .257 |
| BFI Neuroticism | −0.44 | 2.03 | −0.03 | −0.22 | .830 |
| HADS Anxiety | 1.01 | 0.45 | 0.28 | 2.25 | .026 |
| HADS Depression | 0.48 | 0.54 | 0.09 | 0.88 | .380 |
| Step 2 | |||||
| ERQ Reappraisal | 0.70 | 1.53 | 0.04 | 0.46 | .650 |
| ERQ Suppression | −0.71 | 1.06 | −0.06 | −0.67 | .507 |
| DERS Total | 0.17* | 0.08 | 0.25 | 2.16 | .033 |
Note. COVID-19 severity = perceived severity of potential COVID-19 infection.
Fig. 1.
Scatterplot of the fully adjusted relationship between standardized residuals for global emotion regulation difficulties (DERS total) and COVID-19 related acute stress (IES-R total). Solid line represents line of best fit (linear); dotted lines represent upper and lower 95 % confidence intervals around the mean.
3.3. Cognitive reappraisal and expressive suppression interaction
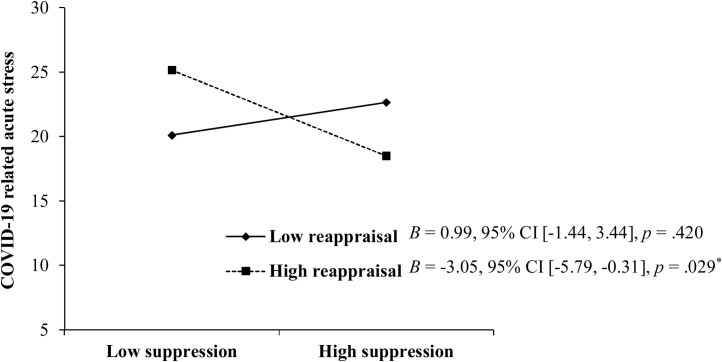
The interaction term between expressive suppression and cognitive reappraisal was a significant, unique predictor of IES-R scores, B = −2.30, p = .012, 95 % CI [−4.09, −0.52]. Follow-up simple slope analyses demonstrated that the effect of expressive suppression was significant when levels of cognitive reappraisal were high (above 1 SD), but not when they were low (below – 1 SD; see Fig. 2 ). A negative association was found between expressive suppression and COVID-19 related acute stress only when levels of cognitive reappraisal were high, suggesting that cognitive reappraisal moderates this relationship. Individuals who reported greater use of both cognitive reappraisal and expressive suppression reported the lowest levels of acute stress, whereas individuals who reported greater use of cognitive reappraisal, but less use of expressive suppression, reported the highest levels of acute stress.
Fig. 2.
Expressive suppression by cognitive reappraisal effects predicting COVID-19 related acute stress.
3.4. Specific dimensions of global emotion regulation difficulties
A supplementary series of hierarchical linear regressions examined which specific dimensions of emotion regulation difficulties (DERS subscales) predicted acute stress. To begin, all covariates, ERQ cognitive reappraisal, and ERQ expressive suppression together explained 16.2 % of the variance in reported acute stress, F(11, 107) = 3.08, p = .001. The separate inclusion of DERS subscales demonstrated that the significant outcome for DERS total was largely driven by 1) nonacceptance of emotional responses, F(12, 106) = 3.25, p = .001, which individually explained an additional 2.4 % of the variance in reported acute stress, and 2) limited perceived access to effective emotion regulation strategies, F(12, 106) = 3.28, p < .001, which individually explained an additional 2.6 % of the variance in symptoms. Greater nonacceptance predicted greater acute stress, B = .44, p = .044, [0.01, 0.87] and greater perceived lack of access to effective emotion regulation strategies predicted greater acute stress, B = .52, p = .038, [0.03, 1.01]. Difficulties in engaging in goal-directed behavior, lack of impulse control, lack of emotional awareness, and lack of emotional clarity did not independently offer any further significant predictive value of acute stress reactions than that offered by the covariates in Step 1 (refer to Supplementary Table S1 for a complete summary of these findings).
4. Discussion
Using a prospective design, the current study examined if emotion regulation strategies, as well as global emotion regulation difficulties, predicted acute stress in response to the COVID-19 pandemic. When examined separately, greater use of cognitive reappraisal and expressive suppression were not associated with acute stress. However, a significant interaction was found between the two strategies, such that expressive suppression was negatively associated with acute stress only when levels of cognitive reappraisal were high. This finding suggests that cognitive reappraisal moderates the relationship between expressive suppression and acute stress in response to the COVID-19 pandemic. Additionally, participants who reported greater global emotion regulation difficulties were also more likely to later report greater acute stress. Further examination of DERS subscales demonstrated that individuals who specifically reported greater emotional nonacceptance or greater perceptions of limited access to effective emotion regulation strategies were more likely to report later acute stress, whereas the other four dimensions of global emotion dysregulation were not found to be predictive (difficulties in engaging in goal-directed behavior, impulse control difficulties, lack of emotional awareness, and lack of emotional clarity). Notably, the observed results withstood controlling for factors known to be related to stress reactions and emotion regulation ability (e.g., anxiety, depression, adverse childhood experiences, neuroticism).
Cognitive reappraisal and expressive suppression, when examined separately, did not predict acute stress; this finding contradicts our initial hypotheses, as well as previous literature. Prior research has suggested that the development of stress reactions following traumatic events is associated with higher use of expressive suppression and lower use of cognitive reappraisal (e.g., Boden et al., 2013; Shepherd & Wild, 2014). However, our results indicate no independent relationships between expressive suppression or cognitive reappraisal and reported acute stress reactions following a potentially traumatic event. It should be noted that symptoms were examined during the initial stages of the pandemic (<30 days), and as such, it is possible there was insufficient time for symptom severity to develop, making these relationships difficult to detect at this assessment point. Rather, the observed results demonstrate an interaction between the two strategies, whereby greater habitual use of cognitive reappraisal moderates a negative relationship between expressive suppression and acute stress. Interestingly, these findings conflict with the findings of prior research (e.g., Eftekhari et al., 2009; Raymond et al., 2019), such that the combination of high cognitive reappraisal with low expressive suppression in the present study was related to the highest reports of stress symptoms, whereas high cognitive reappraisal with high expressive suppression was related to the lowest reports of symptoms.
It is important to note that emotion regulation strategies may have different outcomes in different contexts (Gross, 2014; Sheppes, 2014). For instance, research suggests that cognitive reappraisal is most effective when employed early (antecedent-focused), allowing time for the cognitive alternation of an event’s meaning before the emotional response is fully engaged (e.g., Gross & John, 2003). However, experimental studies reveal that the benefits of cognitive reappraisal are no longer evident if reappraisal is initiated after emotional intensity is already high (Sheppes & Meiran, 2007, 2008; Sheppes, Catran, & Meiran, 2009). Late reappraisal may result in greater physiological responding and cognitive resource expenditure in order to counteract the initial heightened emotional response. The unexpected and unpredictable nature of the COVID-19 pandemic may have prevented the opportunity for cognitive reappraisal prior to its onset, thus reducing the effectiveness of the strategy by forcing individuals to employ and maintain it after their initial emotional response (e.g., online emotion regulation; see Sheppes & Meiran, 2007). The measurement of acute stress in response to the global pandemic took place in the early stages of the pandemic, during one of the most unpredictable periods, with consistently changing guidelines and restrictions (e.g., Wang, Pan, Wan, Tan, Xu, Ho et al., 2020). This early phase assessment may explain why individuals in the current study who were high reappraisers, yet low suppressors reported greater COVID-19 related acute stress. The late initiation of cognitive reappraisal, combined with a lack of expressive suppression of negative emotions, may result in the heightened experience of stress as well as a greater likelihood of reporting stress symptoms.
Alternatively, the combination of high cognitive reappraisal and high expressive suppression predicted the lowest reports of acute stress. The effectiveness of late reappraisal may be dependent on the strength and intensity of the preceding initial emotional response (Sheppes & Meiran, 2007). The flexible and combined use of both strategies may provide a complimentary process for dealing with emotionally unpredictable situations (i.e., the COVID-19 pandemic), such that suppression dampens emotional expression just enough to allow for easier and less emotional cognitive reassessment of the situation. These findings support the somewhat similar findings of Bonanno et al. (2004), such that college students who were able to both flexibly enhance and suppress negative emotional expression in response to unpleasant images during a laboratory visit revealed less psychological distress two years after the 9/11 terrorist attacks. Healthy emotion regulation is not simply determined by the specific use of adaptive strategies over maladaptive strategies, but rather the ability to flexibly adapt and choose strategies that best address the demands of the situation at hand (Sheppes, 2014). A strategy that is considered adaptive in one context may very well be maladaptive in another context, and vice versa. For example, the use of expressive suppression, often considered maladaptive, may actually be beneficial in extremely emotional situations, such as during grief (Bonanno & Keltner, 1997). Future research is needed to replicate and extend these results. It should also be noted that this study only assessed reported stress reactions during the ongoing pandemic. If possible, future research should reexamine the relationships between use of cognitive reappraisal or expressive suppression with reported stress reactions after the COVID-19 pandemic, to see if these relationships remain stable or change over time.
The present results support our hypotheses and prior cross-sectional research regarding a positive association between global emotion regulation difficulties and stress symptoms (e.g., Badour & Feldner, 2013; Barlow et al., 2017). We also replicate and support the prospective findings of Bardeen, Kumpula et al. (2013), such that global emotion regulation difficulties were positively predictive of later stress symptoms following a traumatic event. This study adds to the premise that emotion regulation difficulties may offer insight into who may be at risk for developing negative responses following a stressful event. Prior research has identified all dimensions of emotion regulation difficulties to be related to stress responses, with the exception of emotional awareness (McDermott, Tull, Gratz, Daughters, & Lejuez, 2009; Tull et al., 2007) and in one study, emotional clarity (Weiss et al., 2012). In the current study, only two of the six measured dimensions of emotion regulation difficulties were found to be predictive of later acute stress; emotional nonacceptance and lack of access to emotion regulation strategies. Indeed, it is unsurprising that these two dimensions underlie the relationship between emotion regulation difficulties and acute stress. Emotional nonacceptance refers to an unwillingness to experience or accept negative emotions from a secondary emotional response, such as shame or guilt, on top of one’s initial response (Gratz & Roemer, 2004). This difficulty can compound the experience of emotional distress (Gratz & Tull, 2010) and may even result in situation avoidance or disengagement, thus preventing fear extinction (Foa & Kozak, 1986) and increasing the risk of developing sustained stress reactions in the form of posttraumatic stress symptoms (e.g., Viana et al., 2017; Woodward et al., 2020). The finding that perceived lack of access to effective emotion regulation strategies was also predictive of reported acute stress provides additional evidence for our results showing that a combination of greater cognitive reappraisal and greater expressive suppression was most protective in the development of future acute stress. This finding underscores the importance of having a flexible and wide repertoire of emotion regulation strategies to draw upon during times of distress (Aldao, Sheppes, & Gross, 2015).
While this study is strengthened by a prospective within-subjects design, some limitations offer directions for future research. First, this study consisted of only one wave, and the analyses are still correlational, such that the outcomes could have been influenced by another variable (Christenfeld, Sloan, Carroll, & Greenland, 2004). However, a number of potential confounding variables were identified and controlled (i.e., perceived severity of COVID-19 infection, sex, race, ethnicity, SES, adverse childhood experiences, anxiety, depression, and neuroticism). Second, participation for Phase 2 consisted of only 27 % of the original study sample that had participated in Phase 1, resulting in a relatively small subsample. While participants provided consent at Phase 1 to be contacted in the future about other potential study opportunities, we did not originally plan this follow-up study, and as such, no effort was made to maintain contact between Phase 1 and Phase 2. Additionally, a lack of participation may be the result of a lack of monetary or course credit incentive. However, there were no observed differences between those who participated in the follow-up and those who did not, in terms of age, race, ethnicity, SES, neuroticism, adverse childhood experiences, anxiety, depression, DERS total/subscale scores, or ERQ subscale scores. Females were more likely to participate than males, χ2 (1, 455) = 7.4, p = .006. Third, while this study utilized a relatively homogenous sample (undergraduate students at the same university), racial and ethnic diversity was still observed (31.1 % non-Caucasian and 22.7 % Hispanic/Latino). Future research may benefit from observing these relationships in other samples (e.g., older adults, diverse occupational status). Fourth, this study relied entirely upon self-report measurements, which may have been influenced by a participant’s willingness and ability to accurately report emotional experiences. That being said, the self-report measures of emotion regulation utilized in this study are strongly associated with behavioral measures as well as experimental manipulations of emotion regulation (Gratz & Tull, 2010; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Jentsch & Wolf, 2020). Still, future research may benefit from examining emotion regulation using other types of assessment (e.g., behavioral or physiological measurements, interviews, or experimental manipulation). Fifth, it is common for the IES-R to be utilized to quantify posttraumatic stress symptoms. However, the IES-R is not considered an official diagnostic instrument for PTSD, and as such, no clinical diagnoses can be made. In the present manuscript, we utilized the IES-R to quantify “acute stress,” given that the pandemic is still ongoing and not “post” the traumatic event (Asmundson & Taylor, 2021). Additionally, our sample likely did not have a consistent level of exposure to the distressing aspects of the COVID-19 pandemic (e.g., possible individual differences in loss of jobs, loved ones, state/city wide regulations), and as such, some exposures may not have met the DSM-5 definition of Criterion A regarding the experiencing, witnessing, or learning of the traumatic experience (American Psychiatric Association, 2013; Asmundson & Taylor, 2021).
Furthermore, it is worth noting that the IES-R was measured during the initial stages of the pandemic (<30 days) rather than after the pandemic; thus, the current findings are more representative of acute stress reactions than actual PTSD symptoms (Asmundson & Taylor, 2021). However, the findings of this study still have important clinical implications. Given the pandemic is ongoing, it is critical to determine if individuals are currently experiencing distress-like symptoms related to the pandemic, and whether individual differences may make some more susceptible than others. Acute stress reactions occurring within the first month of potential trauma exposure are a necessary area of research; those reactions have been found to be indicative of individuals who are at risk for subsequent, more serious psychological disorders (Bryant et al., 2014). As such, it is useful to understand what factors (e.g., emotion dysregulation) contribute to greater acute stress severity to identify individuals who may benefit from early intervention or monitoring (Bryant et al., 2014). In particular, interventions focused on improving regulation of emotions may be beneficial (e.g., Dialectical Behavior Therapy, Linehan et al., 1999; Skills Training in Affect and Interpersonal Regulation, Cloitre, Koenen, Cohen, & Han, 2002). Based on these findings, a more narrowed intervention approach that specifically targets improved flexibility of strategy use as well as greater acceptance of one’s emotional experience may be worth exploring.
In conclusion, the combined habitual use of high cognitive reappraisal with low expressive suppression, along with greater reported global difficulties in emotion regulation were predictive of later acute stress surrounding the initial onset of a stressful event (i.e., global pandemic). We offer further evidence of the temporal relationship between emotion regulation and future stress reactions while controlling for factors known to influence the likelihood of developing such symptoms. This prospective investigation makes a significant contribution to a literature that is heavily reliant upon cross-sectional designs. Additionally, these findings highlight a need to further examine the context surrounding different stress experiences, as the expected protective or harmful effects of certain emotion regulation strategies or abilities may differ from one experience to another. This may be informative for the development of interventions that take context into account when addressing emotion regulation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors report no declarations of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.janxdis.2021.102411.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Aldao A., Sheppes G., Gross J.J. Emotion regulation flexibility. Cognitive Therapy and Research. 2015;39:263–278. doi: 10.1007/s10608-014-9662-4. [DOI] [Google Scholar]
- Allan N.P., Norr A.M., Macatee R.J., Gajewska A., Schmidt N.B. Interactive effects of anxiety sensitivity and emotion regulation on anxiety symptoms. Journal of Psychopathology and Behavioral Assessment. 2015;37:663–672. doi: 10.1007/s10862-015-9484-z. [DOI] [Google Scholar]
- American Psychiatric Association . Author; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders (5th text revision) [Google Scholar]
- Amstadter A. Emotion regulation and anxiety disorders. Journal of Anxiety Disorders. 2008;22:211–221. doi: 10.1016/j.janxdis.2007.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G., Taylor S. Garbage in, garbage out: The tenuous state of research on PTSD in the context of the COVID-19 pandemic and infodemic. Journal of Anxiety Disorders. 2021;78 doi: 10.1016/j.janxdis.2021.102368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badour C.L., Feldner M.T. Trauma-related reactivity and regulation of emotion: Associations with posttraumatic stress symptoms. Journal of Behavior Therapy and Experimental Psychiatry. 2013;44:69–76. doi: 10.1016/j.jbtep.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen J.R., Fergus T.A., Orcutt H.K. An examination of the latent structure of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2012;34:382–392. doi: 10.1007/s10862-012-9280-y. [DOI] [Google Scholar]
- Bardeen J.R., Fergus T.A., Wu K.D. The interactive effect of worry and intolerance of uncertainty on posttraumatic stress symptoms. Cognitive Therapy and Research. 2013;37:742–751. doi: 10.1007/s10608-012-9512-1. [DOI] [Google Scholar]
- Bardeen J.R., Kumpula M.J., Orcutt H.K. Emotion regulation difficulties as a prospective predictor of posttraumatic stress symptoms following a mass shooting. Journal of Anxiety Disorders. 2013;27:188–196. doi: 10.1016/j.janxdis.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow M.R., Goldsmith Turow R.E., Gerhart J. Trauma appraisals, emotion regulation difficulties, and self-compassion predict posttraumatic stress symptoms following childhood abuse. Child Abuse & Neglect. 2017;65:37–47. doi: 10.1016/j.chiabu.2017.01.006. [DOI] [PubMed] [Google Scholar]
- Boden M.T., Westermann S., McRae K., Kuo J., Alvarez J., Kulkarni M.R.…Bonn-Miller M.O. Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social and Clinical Psychology. 2013;32:296–314. doi: 10.1521/jscp.2013.32.3.296. [DOI] [Google Scholar]
- Bonanno G.A., Keltner D. Facial expressions of emotion and the course of conjugal bereavement. Journal of Abnormal Psychology. 1997;106:126–137. doi: 10.1037/0021-843x.106.1.126. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Papa A., Lalande K., Westphal M., Coifman K. The importance of being flexible: The ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science. 2004;15:482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- Bouton M.E., Mineka S., Barlow D.H. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037/0033-295x.108.1.4. [DOI] [PubMed] [Google Scholar]
- Bovin M.J., Marx B.P. The importance of the peritraumatic experience in defining traumatic stress. Psychological Bulletin. 2011;137:47–67. doi: 10.1037/a0021353. [DOI] [PubMed] [Google Scholar]
- Breslau N., Schultz L. Neuroticism and post-traumatic stress disorder: A prospective investigation. Psychological Medicine. 2013;43:1697–1702. doi: 10.1017/s0033291712002632. [DOI] [PubMed] [Google Scholar]
- Brewin C.R., Dalgleish T., Joseph S. A dual-representation theory of posttraumatic stress disorder. Psychological Review. 1996;103:670–686. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant R.A., Creamer M., O’Donnell M., Silove D., McFarlane A.C., Forbes D. A comparison of the capacity of DSM-IV and DSM-5 acute stress disorder definitions to predict posttraumatic stress disorder and related disorders. The Journal of Clinical Psychiatry. 2014;76:391–397. doi: 10.4088/jcp.13m08731. [DOI] [PubMed] [Google Scholar]
- Burns E.E., Jackson J.L., Harding H.G. Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma. 2010;19:801–819. doi: 10.1080/10926771.2010.522947. [DOI] [Google Scholar]
- Campbell-Sills L., Ellard K.K., Barlow D.H. In: Handbook of emotion regulation. Gross J.J., editor. Guilford Press; New York, NY: 2014. Emotion regulation in anxiety disorders; pp. 393–412. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Coronavirus disease 2019: Cases in the US.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html (Accessed 25 September 2020) [Google Scholar]
- Christenfeld N.J.S., Sloan R.P., Carroll D., Greenland S. Risk factors, confounding, and the illusion of statistical control. Psychosomatic Medicine. 2004;66:868–875. doi: 10.1097/01.psy.0000140008.70959.41. [DOI] [PubMed] [Google Scholar]
- Christiansen D.M., Elklit A. Risk factors predict post-traumatic stress disorder differently in men and women. Annals of General Psychiatry. 2008;7:24. doi: 10.1186/1744-859x-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clohessy S., Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology. 1999;38:251–265. doi: 10.1348/014466599162836. [DOI] [PubMed] [Google Scholar]
- Cloitre M., Koenen K.C., Cohen L.R., Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology. 2002;70:1067–1074. doi: 10.1037/0022-006x.70.5.1067. [DOI] [PubMed] [Google Scholar]
- Cohen S., Gianaros P.J., Manuck S.B. A stage model of stress and disease. Perspectives on Psychological Science. 2016;11:456–463. doi: 10.1177/1745691616646305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Janicki-Deverts D., Miller G.E. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.168. [DOI] [PubMed] [Google Scholar]
- Eftekhari A., Zoellner L.A., Vigil S.A. Patterns of emotion regulation and psychopathology. Anxiety, Stress & Coping. 2009;22:571–586. doi: 10.1080/10615800802179860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A., Clark D.M. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Maercker A., Boos A. Posttraumatic stress disorder following political imprisonment: The role of mental defeat, alienation, and perceived permanent change. Journal of Abnormal Psychology. 2000;109:45–55. doi: 10.1037/0021-843x.109.1.45. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Mayou R.A., Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology. 1998;107:508–519. doi: 10.1037/0021-843x.107.3.508. [DOI] [PubMed] [Google Scholar]
- Ehring T., Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- England-Mason G., Kimber M., Khoury J., Atkinson L., MacMillan H., Gonzalez A. Difficulties with emotion regulation moderate the association between childhood history of maltreatment and cortisol reactivity to psychosocial challenge in postpartum women. Hormones and Behavior. 2017;95:44–56. doi: 10.1016/j.yhbeh.2017.07.007. [DOI] [PubMed] [Google Scholar]
- Feeny N.C., Foa E.B. In: Cognitive vulnerability to emotional disorders. Alloy L.B., Riskind J.H., editors. Lawrence Erlbaum Associates Publishers; Mahweh, NJ: 2005. Cognitive vulnerability to PTSD; pp. 285–301. [Google Scholar]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V.…Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Kozak M.J. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [DOI] [PubMed] [Google Scholar]
- Fowler J.C., Charak R., Elhai J.D., Allen J.G., Frueh B.C., Oldham J.M. Construct validity and factor structure of the difficulties in Emotion Regulation Scale among adults with severe mental illness. Journal of Psychiatric Research. 2014;58:175–180. doi: 10.1016/j.jpsychires.2014.07.029. [DOI] [PubMed] [Google Scholar]
- Frewen P.A., Lanius R.A. Toward a psychobiology of posttraumatic self-dysregulation: Reexperiencing, hyperarousal, dissociation, and emotional numbing. Annals of the New York Academy of Sciences. 2006;1071:110–124. doi: 10.1196/annals.1364.010. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy I.R., Huang S.H., Bonanno G.A. Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review. 2018;63:41–55. doi: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed] [Google Scholar]
- Goldberg L.R. The structure of phenotypic personality traits. American Psychologist. 1993;48:26–34. doi: 10.1037/0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- Gratz K.L., Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gratz K.L., Tull M.T. In: Assessing mindfulness and acceptance: Illuminating the processes of change. Baer R.A., editor. Harbinger Publications; 2010. Emotion regulation as a mechanism of change in acceptance- and mindfulness-based treatments; pp. 107–133. [Google Scholar]
- Gratz K.L., Rosenthal M.Z., Tull M.T., Lejuez C.W., Gunderson J.G. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115:850–855. doi: 10.1037/0021-843x.115.4.850. [DOI] [PubMed] [Google Scholar]
- Gross J.J. Antecedent-and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology. 1998;74:224–237. doi: 10.1037/0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross J.J. In: Handbook of emotion regulation. Gross J.J., editor. Guilford Press; New York, NY: 2014. Emotion regulation: Conceptual and empirical foundations; pp. 3–20. [Google Scholar]
- Gross J.J., John O.P. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Press; New York, NY: 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Jentsch V.L., Wolf O.T. The impact of emotion regulation on cardiovascular, neuroendocrine and psychological stress responses. Biological Psychology. 2020;154 doi: 10.1016/j.biopsycho.2020.107893. [DOI] [PubMed] [Google Scholar]
- John O.P., Srivastava S. In: Handbook of personality: Theory and research. Pervin L.A., John O.P., editors. Guilford Press; New York: 1999. The Big Five trait taxonomy: History, measurement, and theoretical perspectives; pp. 102–138. [Google Scholar]
- Joormann J., Stanton C.H. Examining emotion regulation in depression: A review and future directions. Behaviour Research and Therapy. 2016;86:35–49. doi: 10.1016/j.brat.2016.07.007. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Murphy J., McBride O., Ben‐Ezra M., Bentall R.P.…Hyland P. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: A population-based study. Journal of Traumatic Stress. 2020;33:365–370. doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpula M.J., Orcutt H.K., Bardeen J.R., Varkovitzky R.L. Peritraumatic dissociation and experiential avoidance as prospective predictors of posttraumatic stress symptoms. Journal of Abnormal Psychology. 2011;120:617–627. doi: 10.1037/a0023927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly M.M., London M.J., Bridgett D.J. Using SEM to examine emotion regulation and revictimization in predicting PTSD symptoms among childhood abuse survivors. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6:644–651. doi: 10.1037/a0036460. [DOI] [Google Scholar]
- Linehan M.M., Schmidt H., Dimeff L.A., Craft J.C., Kanter J., Comtois K.A. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. American Journal on Addictions. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Litz B.T., Orsillo S.M., Kaloupek D., Weathers F. Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology. 2000;109:26–39. doi: 10.1037/0021-843x.109.1.26. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., “Chris.” Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien S.J., McEwen B.S., Gunnar M.R., Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Marx B.P., Sloan D.M. Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy. 2005;43:569–583. doi: 10.1016/j.brat.2004.04.004. [DOI] [PubMed] [Google Scholar]
- McDermott M.J., Tull M.T., Gratz K.L., Daughters S.B., Lejuez C.W. The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. Journal of Anxiety Disorders. 2009;23:591–599. doi: 10.1016/j.janxdis.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore S.A., Zoellner L.A., Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behaviour Research and Therapy. 2008;46:993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’toole B.I., Marshall R.P., Schureck R.J., Dobson M. Posttraumatic stress disorder and comorbidity in Australian Vietnam veterans: Risk factors, chronicity and combat. Australian & New Zealand Journal of Psychiatry. 1998;32:32–42. doi: 10.3109/00048679809062703. [DOI] [PubMed] [Google Scholar]
- Pollock N.C., McCabe G.A., Southard A.C., Zeigler-Hill V. Pathological personality traits and emotion regulation difficulties. Personality and Individual Differences. 2016;95:168–177. doi: 10.1016/j.paid.2016.02.049. [DOI] [Google Scholar]
- Pugach C.P., Campbell A.A., Wisco B.E. Emotion regulation in posttraumatic stress disorder (PTSD): Rumination accounts for the association between emotion regulation difficulties and PTSD severity. Journal of Clinical Psychology. 2020;76:508–525. doi: 10.1002/jclp.22879. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond C., Marin M.-F., Juster R.-P., Lupien S.J. Should we suppress or reappraise our stress?: The moderating role of reappraisal on cortisol reactivity and recovery in healthy adults. Anxiety, Stress, & Coping. 2019;32:286–297. doi: 10.1080/10615806.2019.1596676. [DOI] [PubMed] [Google Scholar]
- Restubog S.L.D., Ocampo A.C.G., Wang L. Taking control amidst the chaos: Emotion regulation during the COVID-19 pandemic. Journal of Vocational Behavior. 2020;119 doi: 10.1016/j.jvb.2020.103440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritschel L.A., Tone E.B., Schoemann A.M., Lim N.E. Psychometric properties of the Difficulties in Emotion Regulation Scale across demographic groups. Psychological Assessment. 2015;27:944–954. doi: 10.1037/pas0000099. [DOI] [PubMed] [Google Scholar]
- Roemer L., Lee J.K., Salters-Pedneault K., Erisman S.M., Orsillo S.M., Mennin D.S. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy. 2009;40:142–154. doi: 10.1016/j.beth.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F.…Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy B., Riley C., Sinha R. Emotion regulation moderates the association between chronic stress and cardiovascular disease risk in humans: A cross-sectional study. Stress. 2018;21:548–555. doi: 10.1080/10253890.2018.1490724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruganci R.N., Gençöz T. Psychometric properties of a Turkish version of the difficulties in emotion regulation scale. Journal of Clinical Psychology. 2010;66:442–455. doi: 10.1002/jclp.20665. [DOI] [PubMed] [Google Scholar]
- Salsman N.L., Linehan M.M. An investigation of the relationships among negative affect, difficulties in emotion regulation, and features of borderline personality disorder. Journal of Psychopathology and Behavioral Assessment. 2012;34:260–267. doi: 10.1007/s10862-012-9275-8. [DOI] [Google Scholar]
- Salters-Pedneault K., Roemer L., Tull M.T., Rucker L., Mennin D.S. Evidence of broad deficits in emotion regulation associated with chronic worry and generalized anxiety disorder. Cognitive Therapy and Research. 2006;30:469–480. doi: 10.1007/s10608-006-9055-4. [DOI] [Google Scholar]
- Seligowski A.V., Lee D.J., Bardeen J.R., Orcutt H.K. Emotion regulation and posttraumatic stress symptoms: A meta-analysis. Cognitive Behaviour Therapy. 2015;44:87–102. doi: 10.1080/16506073.2014.980753. [DOI] [PubMed] [Google Scholar]
- Shepherd L., Wild J. Emotion regulation, physiological arousal and PTSD symptoms in trauma-exposed individuals. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45:360–367. doi: 10.1016/j.jbtep.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G. In: Handbook of emotion regulation. Gross J.J., editor. Guilford Press; New York, NY: 2014. Emotion regulation choice: Theory and findings; pp. 126–139. [Google Scholar]
- Sheppes G., Meiran N. Better late than never? On the dynamics of online regulation of sadness using distraction and cognitive reappraisal. Personality and Social Psychology Bulletin. 2007;33:1518–1532. doi: 10.1177/0146167207305537. [DOI] [PubMed] [Google Scholar]
- Sheppes G., Meiran N. Divergent cognitive costs for online forms of reappraisal and distraction. Emotion. 2008;8:870–874. doi: 10.1037/a0013711. [DOI] [PubMed] [Google Scholar]
- Sheppes G., Catran E., Meiran N. Reappraisal (but not distraction) is going to make you sweat: Physiological evidence for self-control effort. International Journal of Psychophysiology. 2009;71:91–96. doi: 10.1016/j.ijpsycho.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Silverman M.H., Wilson S., Ramsay I.S., Hunt R.H., Thomas K.M., Krueger R.F., Iacono W.G. Trait neuroticism and emotion neurocircuitry: Functional magnetic resonance imaging evidence for a failure in emotion regulation. Development and Psychopathology. 2019;31:1085–1099. doi: 10.1017/s0954579419000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundermann J.M., DePrince A.P. Maltreatment characteristics and emotion regulation (ER) difficulties as predictors of mental health symptoms: Results from a community-recruited sample of female adolescents. Journal of Family Violence. 2015;30:329–338. doi: 10.1007/s10896-014-9656-8. [DOI] [Google Scholar]
- Taylor S., Asmundson G. Life in a post-pandemic world: What to expect of anxiety-related conditions and their treatment. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull M.T., Barrett H.M., McMillan E.S., Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Viana A.G., Paulus D.J., Bakhshaie J., Garza M., Valdivieso J., Ochoa-Perez M.…Zvolensky M.J. Emotional nonacceptance within the context of traumatic event exposure: The explanatory role of anxiety sensitivity for traumatic stress symptoms and disability among Latinos in a primary care setting. General Hospital Psychiatry. 2017;44:30–37. doi: 10.1016/j.genhosppsych.2016.10.007. [DOI] [PubMed] [Google Scholar]
- Wang M., Saudino K.J. Emotion regulation and stress. Journal of Adult Development. 2011;18:95–103. doi: 10.1007/s10804-010-9114-7. [DOI] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S.…Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb T.L., Miles E., Sheeran P. Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin. 2012;138:775–808. doi: 10.1037/a0027600. [DOI] [PubMed] [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing psychological trauma and PTSD. Wilson J.P., Keane T.M., editors. Guilford Press; New York: 1997. The impact of event scale- revised; pp. 339–441. [Google Scholar]
- Weiss N.H., Tull M.T., Davis L.T., Dehon E.E., Fulton J.J., Gratz K.L. Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cognitive Behaviour Therapy. 2012;41:5–14. doi: 10.1080/16506073.2011.621970. [DOI] [PubMed] [Google Scholar]
- Weiss N.H., Tull M.T., Lavender J., Gratz K.L. Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect. 2013;37:944–954. doi: 10.1016/j.chiabu.2013.03.014. [DOI] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Woodward E.C., Viana A.G., Trent E.S., Raines E.M., Zvolensky M.J., Storch E.A. Emotional nonacceptance, distraction coping and PTSD symptoms in a trauma-exposed adolescent inpatient sample. Cognitive Therapy and Research. 2020;44:412–419. doi: 10.1007/s10608-019-10065-4. [DOI] [Google Scholar]
- World Health Organization . 2020. Coronavirus disease (COVID-2019) situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed 30 November 2020) [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.