Abstract
Objective
Burnout is a global work-related phenomenon. Intensive care unit (ICU) nurses are at risk of burnout and the COVID-19 pandemic may increase this risk. The objectives of this study were to assess the prevalence of burnout risk and identify risk factors among ICU nurses during the COVID-19 pandemic.
Research methodology
Web-based survey performed during the first wave of the COVID-19 pandemic in French speaking Belgium.
Main outcome measures
Risk of burnout was assessed with the Maslach Burnout Inventory scale.
Results
A total of 1135 ICU nurses responded to the questionnaire. The overall prevalence of burnout risk was 68%. A total of 29% of ICU nurses were at risk of depersonalisation (DP), 31% of reduced personal accomplishment (PA), and 38% of emotional exhaustion (EE). A 1:3 nurse-to-patient ratio increased the risk of EE (OR = 1.77, 95% CI: 1.07–2.95) and DP (OR = 1.38, 95% CI: 1.09–2.40). Those who reported having a higher perceived workload during the COVID-19 pandemic were at higher risk for all dimensions of burnout. Shortage of personal protective equipment increased the risk of EE (OR = 1.78, 95% CI: 1.35–3.34) and nurses who reported having symptoms of COVID-19 without being tested were at higher risk of EE (OR = 1.40, 95% CI: 1.68–1.87).
Conclusions
Two-thirds of ICU nurses were at risk of burnout and this risk was associated with their working conditions during the first wave of the COVID-19 pandemic. We recommend monitoring the risk of burnout and implementing interventions to prevent and manage it, taking into account the factors identified in this study.
Keywords: Coronavirus, Burnout, Intensive care unit, Nurses, Workload
Implications for clinical practice.
-
•
Overall, 68% of intensive care nurses were at risk of burnout during the first wave of the COVID-19 outbreak.
-
•
The most negatively affected dimension of burnout was emotional exhaustion, followed by reduced personal accomplishment and depersonalisation.
-
•
The main risk factors for burnout during the COVID-19 pandemic were a high ratio of patients per nurse, a perceived increase in workload, having symptoms of COVID-19 without being tested, and shortage of COVID-19 protective equipment.
-
•
We recommend monitoring the risk of burnout and implementing interventions to prevent and manage it, taking into account the factors identified in this study.
Introduction
Burnout is a global work-related phenomenon that is associated with the quality of working conditions, interpersonal relationships, role conflict, and workload (Maslach et al., 2001). Burnout is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed and leading to emotional exhaustion (EE), depersonalization (DP), and a lack of personal accomplishment (PA) (Maslach et al., 1996, World Health Organisation, 2019).
Nurses are particularly prone to burnout due to various professional practice circumstances and working conditions that can lead to physical and emotional exhaustion (Aiken et al., 2012, Estryn-Béhar et al., 2007, Woo et al., 2020). Nurses must provide patient care with patience and empathy, all in a very stressful environment, often with few resources and an excessive workload, and balance these factors that can harm their professional life (de Oliveira et al., 2019, Khamisa et al., 2015). Burnout among nurses has been shown to be associated with adverse health effects, increased turnover, and decreased patient satisfaction with care (Aiken et al., 2002, Dall’Ora et al., 2020, Van Bogaert et al., 2014).
Some studies have reported a high prevalence of burnout among nurses in Belgium compared to other European countries (Aiken et al., 2012, Estryn-Béhar et al., 2007). One study reported a burnout prevalence of 17% in 2012 (Vandenbroeck et al., 2017) while another reported a prevalence of 36% in 2019 (Van den Heede et al., 2019). One possible explanation for this high prevalence of burnout is the high nurse-patient ratio in Belgium in relation to the guideline recommendations from the government on this subject (Bruyneel et al., 2019, Van den Heede et al., 2019). Some studies have shown that intensive care unit (ICU) nurses have a higher prevalence of burnout compared to nurses in other units (Chuang et al., 2016, Vermeir et al., 2018, Woo et al., 2020). Indeed, a growing body of evidence suggests that burnout among ICU nurses is the direct consequence of this demanding and inexorably high-stress work environment (Fischer et al., 2020, Papazian et al., 2018, Poncet et al., 2007). Moreover, ICU nurses often have to deal with end-of-life matters, continuous suffering of patients, demands and distress of relatives, and, sometimes, ethical issues (Curtis et al., 2014, De Villers and DeVon, 2013).
Since March 2020, following in the footsteps of China, Europe has been facing the COVID-19 pandemic, caused by the SARS-CoV-2 virus. In Belgium, the Hospital Emergency Plan was launched on March 13, 2020. The peak of the pandemic occurred around April 10, 2020, with the country having more than 1500 patients hospitalised in intensive care units, an increased capacity to 2000 ICU beds (Sciensano, 2020) without sufficient redeployment of nurses trained in intensive care, and a significant excess of mortality compared to other European countries (Molenberghs et al., 2020). During the peak of the initial COVID-19 outbreak, frontline nurses working with COVID-19 patients, such as ICU nurses, were exposed to higher levels of stressful events (Chen et al., 2020, Guixia and Hui, 2020, Hu et al., 2020, Jalili et al., 2020, Shechter et al., 2020) and a high workload (Bruyneel et al., 2021) that could increase the risk of burnout.
The objectives of this study were (1) to assess the prevalence of burnout risk and (2) to identify risk factors among ICU nurses during the first wave of the COVID-19 pandemic in French-speaking Belgium.
Methods
Study design
Data were collected on nurses in the French-speaking part of Belgium between April 21 and May 04, 2020, using a web-based survey. The data collection period corresponds to the first peak period of COVID-19 daily hospitalisations in Belgium. The online questionnaire was disseminated via Belgian professional nursing associations, inpatient and outpatient health care services (e.g., hospitals, nursing homes, home care services, etc.), and social media. The questionnaire was also translated into Dutch, but we had a low response rate (50 respondents), these were therefore excluded from the analyzes. A total of 4,216 respondents completed the questionnaire, including 1,135 (27%) ICU nurses and there are around 5,000 (23%) active French-speaking ICU nurses in Belgium. In this study, only ICU nurses were analyzed. This is the first study on this questionnaire that will be published.
There is no guidance in Belgium on the nurses-patient ratio in ICU according to the patient profile and the severity of their illness. The nurse-patient ratio in ICU is regulated by a national law setting a maximum of 3 patients per nurse. Moreover, there is little middle care in the country and the patients in ICU are therefore very heterogeneous (Bruyneel et al., 2019).
Measures
The outcome variable was the risk of burnout. The risk of burnout was assessed using the French-version of the validated Maslach Burnout Inventory (MBI) scale (Dion and Tessier, 1994, Maslach et al., 1986). The MBI is a 22-item self-report inventory designed to assess symptoms of burnout among various care professional groups. It captures 3 dimensions of burnout: emotional exhaustion (EE), depersonalization (DP), and reduced personal achievement (PA). The cut-off points for low, moderate and high risk were respectively 0–18, 19–26, and >26 for emotional exhaustion, 0–5, 6–9, >9 for depersonalization, and >39, 34–39, 0–33 for reduced personal accomplishment (Maslach et al., 1986). To estimate the overall prevalence of burnout, we considered that an individual with a high risk in at least one of the three dimensions can be considered to be at risk of burnout, as in other studies (Boutou et al., 2019, Rotenstein et al., 2018).
Sociodemographic data were collected (age, gender, marital status, number of children, seniority in years, etc.) through the questionnaire. Concerning the training level of the nurses in the study, in Belgium, we have two levels of training (bachelor’s degree and no bachelor’s degree) as well as a specialization which takes place after the bachelor with an additional year that includes training in intensive and emergency care. ICU nurses were asked for the nurse-to-patient ratio during their last work shift. In addition, data were collected on their working conditions during the COVID-19 outbreak (e.g. perception of workload, number of COVID-19 patients in the ward, number of patient deaths from COVID-19, amount of personal protective equipment [PPE]) and exposure to the SARS CoV-2 virus (e.g. tested positive, symptomatic without testing because Belgium experienced a shortage of tests at the start of the pandemic). Through the questionnaire we asked the nurses to estimate these different variables, so they represent their perception.
Statistical analyses
Statistical analyses were performed with Software for Statistics and Data Science (14.0, Texas). A p-value < 0.05 was considered statistically significant. Means ± standard deviations (SD) were used to describe symmetric variables and median (Mdn) variables and InterQuartile Range (IQR) was used to describe asymmetric variables.
Univariate and multivariate logistic linear regression models were performed in order to test the association between the different independent variables and each of the three dimensions of the MBI. For these dimensions, we dichotomized them between low and moderate risk on the one hand and high risk on the other. There is no specific guideline for the use of the instrument in statistical models. However, since our target groups are nurses at high risk of burnout in the three dimensions, it seems relevant to identify the factors specifically associated with the high risk of burnout in the three dimensions, as in other studies (Embriaco et al., 2007, Shah et al., 2019) Odds ratios (OR) and 95% confidence intervals (95% CI) and p-values are used to describe the results.
Ethical considerations
Participation was voluntary, anonymous, and did not involve any compensation. Informed consent was obtained from all participants. Belgian Law does not require approval from an Ethical Board for an online survey with the general population and among health professionals. However, the study is covered by privacy regulations. Participants were provided with legal information relating to consent. All information related to respondents’ consent and the GDPR is available upon request. This is in accordance with the law that is applicable, including regulation 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC — General Data Protection Regulation. All methods were performed in accordance with the relevant Belgian guidelines and regulations.
Results
Sociodemographic characteristics
The study included 1135 ICU nurses with an average (±standard deviation) age of 36.9 years (±10.3), the proportion of women was 78%, and participants had an average of 13.9 ± 10.5 years of seniority (Table 1 ). The proportion of specialized nurses was 70% and 54% of respondents had children. A total of 62% of respondents reported a nurse-to-patient ratio of 1:2 and 89% agreed that they have had an increased workload due to the COVID-19 pandemic. Regarding COVID-19, 20% reported having COVID-19 symptoms but not having been tested, 51% said they did not have enough PPE, and 59% said that more than 25% of COVID-19 patients in their ward died (Table 1).
Table 1.
Sociodemographic characteristics (n = 1135).
| Age, year, mean ± SD | 36.9 ± 10.3 |
| Gender, female, n (%) | 892 (78) |
| Seniority, year, mean ± SD | 13.9 ± 10.5 |
| Diploma, n (%) | |
| Bachelor’s degree | 167 (15) |
| Specialized nurses | 789 (70) |
| University diploma | 73 (6) |
| Specialized nurses and University diploma | 63 (6) |
| Nurses no bachelor | 39 (3) |
| Children, n (%) | |
| Yes | 626 (54) |
| No | 521 (46) |
| COVID-19 transmission to nurses, n (%) | |
| Diagnosed test | 58 (5) |
| Suspect, no test but symptoms | 226 (20) |
| Perceived workload during the COVID-19 pandemic, n (%) | |
| Lower | 24 (2) |
| The same | 88 (9) |
| Higher | 920 (89) |
| Having adequate and sufficient protective equipment for COVID-19, n (%) | |
| Yes | 527 (49) |
| No | 550 (51) |
| Number of COVID-19 patients in the unit over the last week, n (%) | |
| None | 41 (4) |
| <25% of patients | 103 (10) |
| 25%-49% of patients | 123 (11) |
| 50%-75% of patients | 180 (17) |
| More than 75% of patients | 629 (58) |
| Working time in recent weeks, n (%) | |
| 25% | 7 (1) |
| 50% (half time) | 69 (6) |
| 75% | 234 (21) |
| 100% (full time) | 579 (51) |
| More than 100% | 244 (22) |
| Nurse-to-patient ratio, mean ± SD | 1.75 ± 0.67 |
| Nurse-to-patient ratio, n (%) | |
| 1:1 | 133 (13) |
| 1:2 | 615 (62) |
| 1:3 | 219 (22) |
| >1:3 | 28 (3) |
| Proportion of patient deaths due to COVID-19 in unit, n (%) | |
| None (ref) | 131 (12) |
| Only one death | 285 (27) |
| About 25% | 346 (32) |
| About 50% | 199 (19) |
| About 75% | 102 (10) |
| 100% | 6 (1) |
Descriptive statistics were performed after exclusion of missing data.
Prevalence of burnout risk
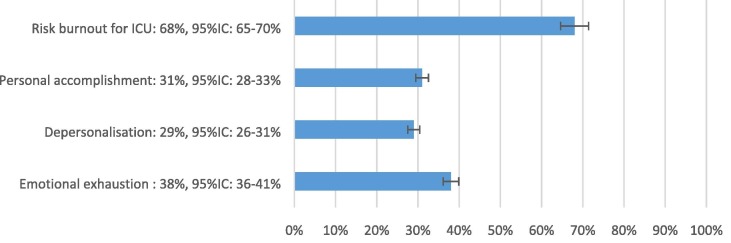
Based on the overall prevalence of burnout risk, 68% of ICU nurses who responded were at risk of burnout. Considering each dimension of the MBI separately, 29% of ICU nurses were at risk of depersonalisation (DP), 31% of reduced personal accomplishment (PA), and 38% of emotional exhaustion (EE) (Fig. 1 ).
Fig. 1.
Prevalence of burnout risk and high-risk dimensions of MBI for ICU nurses MBI, Maslach burnout inventory.
Factors associated with burnout risk
In univariate analysis, men were significantly more at risk of DP compared to women (OR = 2.34, 95% CI: 2.00–3.14) (Table 2 ). For the same dimension, seniority was a protective factor, i.e. nurses with more seniority were less at risk of DP. A high nurse-to-patient ratio (>1:2) was significantly associated with the risk for EE and DP. Not having children increased the risk for DP (OR = 1.51, 95% CI: 1.17–1.95). Regarding factors related to the COVID-19 outbreak, a perceived increased workload during the COVID-19 pandemic was associated with an increased risk in the three dimensions of burnout. Shortage of PPE also increased the risk for EE (OR = 1.97, 95% CI: 1.53–1.87) and DP (OR = 1.41, 95% CI: 1.08–1.83). The proportion of COVID-19 patients in the ward was not associated with burnout. A high number of patient deaths from COVID-19 was significantly associated with the DP dimension (Table 2).
Table 2.
Univariate analysis of risk factors by dimensions of the MBI.
| Variables | Emotional exhaustionOR (95%CI) | DepersonalizationOR (95%CI) | Reduced personal accomplishmentOR (95%CI) |
|---|---|---|---|
| Age, years | 1.01 (1.00–1.02) * | 0.97 (0.96–0.98) *** | 0.99 (0.98–1.00) |
| Gender, ref = female | |||
| Male | 0.92 (0.70–1.23) | 2.34 (2.00–3.14) *** | 1.08 (0.80–1.47) |
| Seniority, year | 1.00 (0.99–1.02) | 0.95 (0.94–0.98) *** | 1.00 (0.99–1.02) |
| Children, ref = yes | |||
| No | 0.81 (0.64–1.04) | 1.51 (1.17–1.95) ** | 1.03 (0.81–1.30) |
| Diploma, ref = Bachelor's degree | |||
| Specialized nurses | 1.09 (0.74–1.48) | 1.16 (0.83–1.61) | 0.77 (0.55–1.09) |
| University diploma | 0.89 (0.51–1.57) | 0.92 (0.53–1.59) | 0.71 (0.41–1.24) |
| Specialized nurses and University diploma | 1.18 (0.42–3.30) | 0.73 (0.36–1.47) | 0.59 (0.29–1.19) |
| Nurses no bachelor | 1.27 (0.68–2.35) | 1.34 (0.74–2.41) | 1.02 (0.52–1.71) |
| Nurse-to-patient ratio, ref = 1:1 | |||
| 1:2 | 1.24 (0.81–1.75) | 1.02 (0.70–1.48) | 0.93 (0.57–1.42) |
| 1:3 | 1.86 (1.19–2.91) ** | 1.61 (1.00–2.58) * | 1.09 (0.67–1.76) |
| >1:3 | 2.18 (1.94–5.03) * | 2.90 (1.24–6.76) * | 1.30 (0.53–3.14) |
| Perceived workload during the COVID-19 pandemic, ref = same | |||
| Lower | 1.39 (0.48–4.03) | 0.90 (0.33–2.99) | 0.82 (0.21–3.16 |
| Higher | 3.27 (1.89–5.63) *** | 2.17 (1.24–3.80) ** | 1.95 (1.06–3.60) * |
| COVID-19 transmission to nurses, ref: None diagnosed and none suspected | |||
| Diagnosed test | 1.08 (0.48–1.49) | 1.09 (0.64–1.85) | 1.09 (0.35–1.03) |
| Suspect, no test but symptoms | 1.39 (1.03–1.87) * | 1.25 (0.91–1.71) | 1.21 (0.89–1.66) |
| Having adequate and sufficient PPE for COVID-19, ref = yes | |||
| No | 1.97 (1.53–2.25) *** | 1.41 (1.08–1.83) ** | 1.14 (0.87–1.50) |
| Number of COVID-19 patients in the unit over the last week, ref = none | |||
| <25% of patients | 0.97 (0.46–2.02) | 0.99 (0.42–2.31) | 0.62 (0.28–1.38) |
| 25%-49% of patients | 0.70 (0.34–1.45) | 0.92 (0.40–2.09) | 0.92 (0.43–1.98) |
| 50%-75% of patients | 0.85 (0.42–1.72) | 1.51 (0.69–3.30) | 0.50 (0.23–1.06) |
| More than 75% of patients | 1.09 (0.57–2.07) | 1.50 (0.72–3.13) | 0.80 (0.40–1.58) |
| Proportion of patient deaths due to COVID-19 in unit, ref = none | |||
| Only one death | 0.77 (0.41–1.45) | 0.45 (0.18–1.11) | 1.00 (0.49–2.04) |
| About 25% | 1.01 (0.61–1.47) | 1.84 (1.15–2.94) ** | 1.31 (0.69–1.86) |
| About 50% | 1.09 (0.70–1.52) | 1.90 (1.15–3.16) * | 0.99 (0.62–1.58) |
| About 75% | 1.41 (0.84–2.38) | 1.76 (1.08–3.14) * | 1.30 (0.75–2.43) |
| 100% | 1.29 (0.30–2.63) | 7.03 (1.23–40.3) * | 3.09 (0.59–16.09) |
* p-value < 0.05, ** p-value < 0.01, *** p-value < 0.001; ref = reference, value in bold: significant, PPE: Personal Protection Equipment; MBI, Maslach burnout inventory
Multivariate analyses confirmed that men were at greater risk of DP (OR = 2.73, 95% IC: 1.88–3.99). A high nurse-to-patient ratio increased the risk of EE (ratio 1:3, OR = 1.77, 95% IC: 1.07–2.95) and DP (ratio 1:3, OR = 1.38, 95% IC:1.09–2.40) (ratio >1:3, OR = 2.72, 95% IC: 1.07–7.54). In addition, those who reported having a higher perceived workload during the COVID-19 pandemic were at higher risk for all dimensions of burnout. Shortage of PPE increased the risk of EE (OR = 1.78, 95% CI: 1.35–3.34) and ICU nurses who reported having symptoms of COVID-19 but not being tested were at greater risk of EE compared to asymptomatic ones (OR = 1.40, 95% CI:1.68–1.87) (Table 3 ).
Table 3.
Multivariate analysis of risk factors by dimensions of the MBI.
| Variables | Emotional exhaustion OR (95%CI) | Depersonalization OR (95%CI) | Reduced personal accomplishment OR (95%CI) |
|---|---|---|---|
| Age, year | 1.01 (0.99–1.03) | 0.96 (0.89–1.02) | 0.97 (0.91–1.04) |
| Gender, ref = female | |||
| Male | 0.93 (0.66–1.32) | 2.73 (1.88–3.99)*** | 0.87 (0.57–1.32) |
| Seniority, year | 0.97 (0.92–1.02) | 1.01 (0.95–1.08) | 1.02 (0.96–1.09) |
| Children, ref = yes | |||
| No | 1.20 (0.62–2.31) | 2.14 (0.92–5.00) | 0.99 (0.49–2.17) |
| Diploma, ref = Bachelor's degree | |||
| Specialized nurses | 1.15 (0.77–1.71) | 1.14 (0.70–1.85) | 1.11 (0.67–1.83) |
| University diploma | 1.09 (0.56–2.14) | 1.44 (0.66–3.08) | 0.68 (0.28–1.69) |
| Specialized nurses and University diploma | 1.10 (0.50–2.48) | 1.86 (0.55–6.31) | 1.40 (0.39–5.07) |
| Nurses no bachelor | 1.21 (0.62–2.38) | 0.91 (0.42–1.99) | 1.96 (0.91–4.23) |
| Nurse-to-patient ratio, ref = 1:1 | |||
| 1:2 | 1.07 (0.68–1.68) | 0.84 (0.52–1.37) | 1.05 (0.59–1.69) |
| 1:3 | 1.77 (1.07–2.95) * | 1.38 (1.09–2.40)* | 1.20 (0.67–2.16) |
| >1:3 | 1.23 (0.48–3.16) | 2.72 (1.07–7.54)* | 2.02 (0.74–5.50) |
| Perceived workload during the COVID-19 pandemic, ref = same | |||
| Lower | – | – | – |
| Higher | 3.23 (1.77–5.93)*** | 2.22 (1.14–4.33)** | 3.07 (1.39–6.76)** |
| COVID-19 transmission to nurses, ref = none diagnosed and none suspected | |||
| Diagnosed test | 1.08 (0.53–2.20) | 1.01 (0.46–2.23) | 0.54 (0.25–1.15) |
| Suspect, no test but symptoms | 1.40 (1.68–1.87)** | 0.93 (0.63–1.39) | 0.69 (0.46–1.05) |
| Having adequate and sufficient PPE for COVID-19, ref = yes | |||
| No | 1.78 (1.35–2.34)*** | 1.27 (0.89–1.71) | 1.19 (0.85–1.68) |
| Number of COVID-19 patients in the unit over the last week, ref = none | |||
| <25% of patients | 0.86 (0.37–2.03) | 0.87 (0.28–2.70) | 0.42 (0.15–1.20) |
| 25%-49% of patients | 0.70 (0.27–1.80) | 0.68 (1.19–2.37) | 0.69 (0.22–2.17) |
| 50%-75% of patients | 0.74 (0.28–1.93) | 0.66 (0.19–2.36) | 0.25 (0.17–1.17) |
| More than 75% of patients | 0.95 (0.38–2.38) | 0.77 (0.22–2.60 | 0.42 (0.13–1.31) |
| Proportion of patient deaths due to COVID-19 in unit, ref = none | |||
| Only one death | 0.84 (0.33–2.13) | 0.53 (0.16–1.71) | 0.72 (0.26–2.04) |
| About 25% | 0.99 (0.45–2.21) | 1.19 (0.49–2.88) | 1.06 (0.45–2.49) |
| About 50% | 1.12 (0.52–2.44) | 2.06 (0.49–4.82) | 1.13 (0.49–2.59) |
| About 75% | 1.17 (0.52–2.65) | 2.29 (1.04–5.57)* | 0.96 (0.40–2.31) |
| 100% | 1.53 (0.65–3.63) | 1.68 (0.65–4.34) | 1.20 (0.47–3.05) |
* p-value < 0.05, ** p-value < 0.01, *** p-value < 0.001; ref = reference, value in bold: significant, PPE: Personal Protection Equipment; MBI, Maslach burnout inventory.
Discussion
In this study, the socio-demographic characteristics of ICU nurses (e.g. age, seniority, proportion of women) were similar to those observed in a recent study in Belgium (Van den Heede et al., 2019).
Regarding the prevalence of risk of burnout (68%), this was higher in this study than in previous studies carried out in Belgium in a general nursing population that reported a prevalence ranging from 17% to 38% (Vandenbroeck et al., 2017, Van den Heede et al., 2019). Compared with other studies carried out only among ICU nurses, we also observed a higher prevalence in our study in comparison to others that reported prevalence rates ranging from 3% to 27% (Friganović and Selič, 2020, Vermeir et al., 2018, Woo et al., 2020). Overall, the other studies were not carried out during the COVID-19 pandemic, the context of the pandemic may, therefore, explain the higher prevalence, especially since Belgium has been strongly affected by the pandemic. Indeed, Belgium has experienced 837 deaths per million inhabitants and a historic excess mortality of 65% due to COVID-19 during the first wave (Bustos Sierra et al., 2020, Molenberghs et al., 2020).
Regarding the three dimensions of burnout, the risk of EE (38%), DP (29%), and reduced PA (31%) was high in this study compared to other studies (Chuang et al., 2016, Friganović and Selič, 2020, Guntupalli et al., 2014, Vermeir et al., 2018). Maslach et al. highlighted three dimensions to the burnout syndrome: emotional exhaustion, depersonalisation and personal accomplishment (Maslach et al. 1986). Emotional exhaustion is the core component of burnout syndrome and is a state of generalised fatigue that can be expressed through emotional, physical and low performance symptoms. Depersonalisation is the development of a detached attitude towards work and patient care. Finally, reduced personal accomplishment can be revealed when nurses repeatedly evaluate negatively their work and have an overall poor professional self-esteem.
The high risk of EE and DP may be explained by different work characteristics, environment, and patient population in the ICU compared to other units. The ICU is known to be highly stressful, demanding, and work intensive, with a much higher degree of difficulty with regard to patient disease status and imposition of higher emotional stress from both family members and patients (Chuang et al., 2016, Curtis et al., 2014). Moreover, ICU nurses often face end-of-life matters and continuous patient suffering, along with ethical issues and the need to deal with demanding and distressed relatives (Curtis et al., 2014, De Villers and DeVon, 2013). For the risk of reduced personal accomplishment, one explanation may be the high death rate and long length of stay for COVID-19 patients in the ICU (Bruyneel et al., 2021, Taccone et al., 2021). Indeed, our study showed an association between the high number of deaths of COVID-19 patients and a high risk of reduced personal accomplishment.
Regarding the factors associated with the risk of burnout, our results confirm other studies that have reported on the impact of the COVID-19 pandemic on the working conditions and mental health of ICU nurses (Hu et al., 2020, Kisely et al., 2020, Shechter et al., 2020). A nurse-to-patient ratio greater than 1:2 and a perceived increased workload significantly increased the risk of EE and DP. The workload among ICU nurses in Belgium is known to be high according to a study which compared the ratio of nurses to real patients and calculated according to the Nursing Activities Score scale (Bruyneel et al., 2019) and COVID-19 has increased nursing time in the ICU (Bruyneel et al., 2021). This association between workload and risk of burnout confirms observations already made in previous studies (Pérez-Francisco et al., 2020, Van Bogaert et al., 2014, Welp et al., 2019). It is, therefore, important to adapt nursing staff workloads to prevent burnout and, at the same time, improve the quality of patient care (Aiken et al., 2012, Pérez-Francisco et al., 2020, Van Bogaert et al., 2017).
The shortage of personal protective equipment (PPE) increased the risk of EE for ICU nurses in this study. Indeed, in Belgium, a shortage of PPE (e.g. masks, gloves, hydroalcoholic liquid) was observed at the start of the COVID-19 pandemic (Thornton, 2020, World Health Organisation, 2020). This lack of PPE was reported by 51% of ICU nurses. Obviously, the lack of PPE leads to a fear of contracting the virus and transmitting it to patients and to their loved ones (World Health Organisation, 2020). Moreover, nurses who reported having symptoms of COVID-19 but were not tested were at higher risk for EE. These results confirm that having enough PPE and testing for COVID-19 can prevent and reduce the risk of EE among ICU nurses (Kisely et al., 2020).
Regarding other risk factors, men were more at risk of DP. This finding has already been observed in other reports in the literature (Chuang et al., 2016, Friganović and Selič, 2020, Merlani et al., 2011). In contrast, there was no association between the level of training and the different dimensions of burnout.
During previous disease outbreaks (e.g. severe acute respiratory syndrome SARS), effective interventions were identified to mitigate the psychological distress of healthcare workers that should be applicable to the current COVID-19 pandemic (Kisely et al., 2020). In addition, preventive measures against burnout can be taken based on individual factors (e.g. rest periods, family, personality, and interpersonal behaviour) (Geuens et al., 2017) and organizational factors (e.g. communication and training, type of management) (de Oliveira et al., 2019).
In the context of a pandemic, this study identified additional preventive measures, such as the provision of sufficient protective equipment and testing and the adaptation of the workload by increasing the number of nurses per patient in ICU. We also recommend monitoring the risk of burnout and implementing interventions to prevent and manage it among ICU nurses.
Limitations
It is important to note that this study has some limitations. Despite its large sample size, the main limitation of this study is a potential selection bias. All nurses in the French-speaking part of Belgium were invited to participate in the survey, and those who responded were those who wanted to have a voice. It is, therefore, possible that the prevalence of nurses at risk of burnout during the COVID-19 crisis was overestimated in this study. Another limitation is that due to a lack of longitudinal information, we cannot prove a causal relationship between the increased prevalence of burnout risk and the COVID-19 pandemic. Despite these limitations, this study highlighted risk groups and risk factors for burnout which are important to identify in order to better target potential interventions. Concerning the factors associated with the risk of burnout, the workload and the nursing ratio per patient are elements that have not been evaluated objectively but self-declared by the respondents during the survey. In addition, in response to the increased workload, ICU nurses had to work with inexperienced nurses in the ICU. Although we have not collected any data on this topic, it is likely to increase the risk of burnout. Finally, other psychological factors (e.g. depression, anxiety) that were not analyzed in this study can also influence the risk of burnout (Fischer et al., 2020).
Conclusions
This study found a high prevalence of burnout risk among ICU nurses (68%) during the first wave of the COVID-19 pandemic in Belgium. The most negatively affected dimension of burnout was emotional exhaustion, followed by reduced personal accomplishment, and depersonalisation. In addition, various risk factors increased the risk of burnout, such as a nurse-to-patient ratio greater than 1:2, a high perceived workload, numerous deaths of COVID-19 patients, and the shortage of COVID-19 personal protective equipment. This study highlighted the importance of monitoring the risk of burnout among ICU nurses during the COVID-19 pandemic and of implementing interventions to prevent and manage it, considering the risk groups and risk factors identified in the scientific literature and in this study.
Funding source
None
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors acknowledge the contribution of a medical writer, Sandy Field, PhD, for English language editing and formatting of the manuscript.
References
- Aiken L.H., Clarke S.P., Douglas S.M., Sochalski J., Silber J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken, L.H., Sermeus, W., Van den Heede, K., Sloane, D.M., Busse, R., McKee, M., Bruyneel, L., Rafferty, A.M., Griffiths, P., Moreno-Casbas, M.T., Tishelman, C., Scott, A., Brzostek, T., Kinnunen, J., Schwendimann, R., Heinen, M., Zikos, D., Sjetne, I.S., Smith, H.L., Kutney-Lee, A., 2012. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. Brit. Med. J. 344, e1717–e1717. https://doi.org/10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed]
- Boutou A., Pitsiou G., Sourla E., Kioumis I. Burnout syndrome among emergency medicine physicians: an update on its prevalence and risk factors. Eur. Rev. Med. Pharmacol. Sci. 2019;23:9058–9065. doi: 10.26355/eurrev_201910_19308. [DOI] [PubMed] [Google Scholar]
- Bruyneel A., Gallani M.-C., Tack J., d'Hondt A., Canipel S., Franck S., Reper P., Pirson M. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit. Care Nurs. 2021;62:102967. doi: 10.1016/j.iccn.2020.102967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Tack J., Droguet M., Maes J., Wittebole X., Miranda D.R., Pierdomenico L.D. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): a prospective study in 16 hospitals in Belgium. J. Crit. Care. 2019;54:205–211. doi: 10.1016/j.jcrc.2019.08.032. [DOI] [PubMed] [Google Scholar]
- Bustos Sierra N., Bossuyt N., Braeye T., Leroy M., Moyersoen I., Peeters I., Scohy A., Van Der Heyden J., Van Oyen H., Renard F. All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. Arch Public Health. 2020;78:117. doi: 10.1186/s13690-020-00496-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Sun C., Chen J.-J., Jen H.-J., Kang X.L., Kao C.-C., Chou K.-R. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int. J. Mental Health Nurs. 2020;30(1):102–116. doi: 10.1111/inm.v30.110.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang C.-H., Tseng P.-C., Lin C.-Y., Lin K.-H., Chen Y.-Y. Burnout in the intensive care unit professionals: a systematic review. Medicine. 2016;95 doi: 10.1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis J.R., Sprung C.L., Azoulay E. The importance of word choice in the care of critically ill patients and their families. Intensive Care Med. 2014;40(4):606–608. doi: 10.1007/s00134-013-3201-8. [DOI] [PubMed] [Google Scholar]
- Dall’Ora C., Ball J., Reinius M., Griffiths P. Burnout in nursing: a theoretical review. Hum. Resour. Health. 2020;18(1) doi: 10.1186/s12960-020-00469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira, S.M., de Alcantara Sousa, L.V., Vieira Gadelha, M. do S., do Nascimento, V.B., 2019. Prevention Actions of Burnout Syndrome in Nurses: An Integrating Literature Review. Clin. Pract. Epidemiol. Ment. Health. 15, 64–73. https://doi.org/10.2174/1745017901915010064 [DOI] [PMC free article] [PubMed]
- De Villers Mary Jo, DeVon Holli A. Moral distress and avoidance behavior in nurses working in critical care and noncritical care units. Nurs. Ethics. 2013;20(5):589–603. doi: 10.1177/0969733012452882. [DOI] [PubMed] [Google Scholar]
- Dion G., Tessier R. Validation de la traduction de l’Inventaire d’épuisement professionnel de Maslach et Jackson. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement. 1994;26:210–227. doi: 10.1037/0008-400X.26.2.210. [DOI] [Google Scholar]
- Embriaco Nathalie, Azoulay Elie, Barrau Karine, Kentish Nancy, Pochard Frédéric, Loundou Anderson, Papazian Laurent. High level of burnout in intensivists: prevalence and associated factors. Am. J Respir. Crit. Care Med. 2007;175(7):686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- Estryn-Béhar M., Van der Heijden B.I.J.M., Ogińska H., Camerino D., Le Nézet O., Conway P.M., Fry C., Hasselhorn H.-M. The impact of social work environment, teamwork characteristics, burnout, and personal factors upon intent to leave among european nurses. Medical Care. 2007;45:939–950. doi: 10.1097/MLR.0b013e31806728d8. [DOI] [PubMed] [Google Scholar]
- Fischer Ronald, Mattos Paulo, Teixeira Cassiano, Ganzerla Daniel S., Rosa Regis Goulart, Bozza Fernando A. Association of burnout with depression and anxiety in critical care clinicians in Brazil. JAMA Netw. Open. 2020;3(12):e2030898. doi: 10.1001/jamanetworkopen.2020.30898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friganović, A., Selič, P., 2020. LEVELS OF BURNOUT SYNDROME IN CROATIAN CRITICAL CARE NURSES: A CROSS-SECTIONAL STUDY (preprint). Open Science Framework. https://doi.org/10.31219/osf.io/xdeyh [PubMed]
- Geuens Nina, Van Bogaert Peter, Franck Erik. Vulnerability to burnout within the nursing workforce-The role of personality and interpersonal behaviour. J. Clin. Nurs. 2017;26(23-24):4622–4633. doi: 10.1111/jocn.13808. [DOI] [PubMed] [Google Scholar]
- Guixia L., Hui Z. A study on burnout of nurses in the period of COVID-19. Psych. Behav. Sci. 2020;9:31. doi: 10.11648/j.pbs.20200903.12. [DOI] [Google Scholar]
- Guntupalli K.K., Wachtel S., Mallampalli A., Surani S. Burnout in the intensive care unit professionals. Indian J. Crit. Care Med. 2014;18:139–143. doi: 10.4103/0972-5229.128703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Deying, Kong Yue, Li Wengang, Han Qiuying, Zhang Xin, Zhu Li Xia, Wan Su Wei, Liu Zuofeng, Shen Qu, Yang Jingqiu, He Hong-Gu, Zhu Jiemin. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424. doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalili M., Niroomand M., Hadavand F., Zeinali K., Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study (preprint) Occup. Environ. Health. 2020 doi: 10.1101/2020.06.12.20129650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khamisa N., Oldenburg B., Peltzer K., Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int. J. Environ. Res. Public Health. 2015;12:652–666. doi: 10.3390/ijerph120100652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. Brit. Med. J. 2020;m1642 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C., Jackson, S.E., Leiter, M.P., 1996. Maslach Burnout Inventory Consulting Psychologists Press.
- Maslach C., Jackson S.E., Leiter M.P., Schaufeli W., Schwab R. Menlo Park; CA Mind Garden: 1986. Maslach Burnout Inventory manual, general survey, human services survey, educators survey ad scoring guides. [Google Scholar]
- Maslach, C., Schaufeli, W.B., Leiter, M.P., 2001. Job Burnout. Annu. Rev. Psychol. 52, 397–422. https://doi.org/10.1146/annurev.psych.52.1.397. [DOI] [PubMed]
- Merlani Paolo, Verdon Mélanie, Businger Adrian, Domenighetti Guido, Pargger Hans, Ricou Bara. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am. J. Respir. Crit. Care Med. 2011;184(10):1140–1146. doi: 10.1164/rccm.201101-0068OC. [DOI] [PubMed] [Google Scholar]
- Molenberghs G., Faes C., Verbeeck J., Deboosere P., Abrams S., Willem L., Aerts J., Theeten H., Devleesschauwer B., Sierra N.B., Renard F., Herzog S., Lusyne P., Van der Heyden J., Van Oyen H., Van Damme P., Hens N. Belgian COVID-19 Mortality, Excess Deaths, Number of Deaths per Million, and Infection Fatality Rates (9 March — 28 June 2020) (preprint) Epidemiology. 2020 doi: 10.1101/2020.06.20.20136234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papazian Laurent, Sylvestre Aude, Herridge Margaret. Should all ICU clinicians regularly be tested for burnout? Yes. Intensive Care Med. 2018;44(5):681–683. doi: 10.1007/s00134-018-5094-z. [DOI] [PubMed] [Google Scholar]
- Pérez-Francisco D.H., Duarte-Clíments G., del Rosario-Melián J.M., Gómez-Salgado J., Romero-Martín M., Sánchez-Gómez M.B. Influence of Workload on Primary Care Nurses’ Health and Burnout, Patients’ Safety, and Quality of Care: Integrative Review. Healthcare. 2020;8:12. doi: 10.3390/healthcare8010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poncet Marie Cécile, Toullic Philippe, Papazian Laurent, Kentish-Barnes Nancy, Timsit Jean-Francçois, Pochard Frédéric, Chevret Sylvie, Schlemmer Benoît, Azoulay Élie. Burnout syndrome in critical care nursing staff. Am. J. Respir. Crit. Care Med. 2007;175(7):698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- Rotenstein Lisa S., Torre Matthew, Ramos Marco A., Rosales Rachael C., Guille Constance, Sen Srijan, Mata Douglas A. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciensano, 2020. COVID-19 Belgium - Daily report. Sciensano. URL https://covid-19.sciensano.be/nl/covid-19-epidemiologische-situatie. (accessed 12.21.20).
- Shah A., Wyatt M., Gourneau B., Shih G., De Ruyter M. Emotional exhaustion among anesthesia providers at a tertiary care center assessed using the MBI burnout survey. Psychol. Health Med. 2019;24(5):620–624. doi: 10.1080/13548506.2018.1546019. [DOI] [PubMed] [Google Scholar]
- Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., Claassen J., Cornelius T., Derby L., Dong M., Givens R.C., Hochman B., Homma S., Kronish I.M., Lee S.A.J., Manzano W., Mayer L.E.S., McMurry C.L., Moitra V., Pham P., Rabbani L., Rivera R.R., Schwartz A., Schwartz J.E., Shapiro P.A., Shaw K., Sullivan A.M., Vose C., Wasson L., Edmondson D., Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taccone Fabio Silvio, Van Goethem Nina, De Pauw Robby, Wittebole Xavier, Blot Koen, Van Oyen Herman, Lernout Tinne, Montourcy Marion, Meyfroidt Geert, Van Beckhoven Dominique. The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium. The Lancet Regional Health - Europe. 2021;2:100019. doi: 10.1016/j.lanepe.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton J. Covid-19: Care homes in Belgium and Spain had “alarming living conditions”, says MSF report. Brit. Med. J. 2020;m3271 doi: 10.1136/bmj.m3271. [DOI] [PubMed] [Google Scholar]
- Van Bogaert P., Peremans L., Van Heusden D., Verspuy M., Kureckova V., Van de Cruys Z., Franck E. Predictors of burnout, work engagement and nurse reported job outcomes and quality of care: a mixed method study. BMC Nurs. 2017;16:5. doi: 10.1186/s12912-016-0200-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bogaert Peter, Timmermans Olaf, Weeks Susan Mace, van Heusden Danny, Wouters Kristien, Franck Erik. Nursing unit teams matter: Impact of unit-level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events—a cross-sectional survey. Int. J. Nurs. Stud. 2014;51(8):1123–1134. doi: 10.1016/j.ijnurstu.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Van den Heede, K., Bruyneel, L., Beeckmans, D., Boon, N., Bouckaert, N., Cornelis, J., Dossche, D., Van de Voorde, C., Sermeus, W., 2019. Safe nurse staffing levels in acute hospitals. Health Services Research (HSR) Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 325, D/2019/10.273/75.
- Vandenbroeck S., Van Gerven E., De Witte H., Vanhaecht K., Godderis L. Burnout in Belgian physicians and nurses. Occup. Med. 2017;67:546–554. doi: 10.1093/occmed/kqx126. [DOI] [PubMed] [Google Scholar]
- Vermeir P., Blot S., Degroote S., Vandijck D., Mariman A., Vanacker T., Peleman R., Verhaeghe R., Vogelaers D. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: a questionnaire study. Intensive. Crit. Care Nurs. 2018;48:21–27. doi: 10.1016/j.iccn.2018.07.001. [DOI] [PubMed] [Google Scholar]
- Welp, A., Rothen, H.U., Massarotto, P., Manser, T., 2019. Teamwork and clinician burnout in Swiss intensive care: the predictive role of workload, and demographic and unit characteristics. Swiss Med. Wkly. https://doi.org/10.4414/smw.2019.20033. [DOI] [PubMed]
- Woo T., Ho R., Tang A., Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J. Psych. Res. 2020;123:9–20. doi: 10.1016/j.jpsychires.2019.12.015. [DOI] [PubMed] [Google Scholar]
- World Health Organisation. 2020 [Google Scholar]
- World Health Organisation, 2019. Burn-out an “occupational phenomenon”: International Classification of Diseases.