Abstract
Objective
In March 2020, the world experienced a global pandemic, which involved the shutdown of schools or a transposition to remote teaching in most countries. The objective of the present study was to investigate the impact of the COVID-19 pandemic related lockdown on sleep patterns and sleep quality in adolescents and young adults.
Methods
An online survey was conducted in June 2020 with adolescents and young adults (n = 498) aged 12–25 years. Participants had to answer questions on sleep, first retrospectively, referring to the time prior to the pandemic, and then referring to the time during the pandemic.
Results
A pronounced shift towards later sleep combined with an increase in sleep duration was found during the pandemic. However, these changes in sleep habits were more pronounced in adolescents than in young adults and seem to occur mostly during weekdays compared to weekends. During the pandemic, teens also reported an improvement in daytime sleepiness and subjective sleep quality, while young adults reported an increase in sleep difficulties associated with sleep onset difficulties, nocturnal and early morning awakenings, and nightmares.
Conclusions
The COVID-19 related lockdown seems to have had a beneficial effect on sleep in adolescents. In young adults, benefits are not as obvious. These results support that later school start times would be beneficial for adolescents. However, in young adults it could be important to investigate the effects of other situational or interindividual factors (stress, lifestyle habits, employment, etc.).
Keywords: Youth, Coronavirus, Phase delay, Age differences
1. Introduction
In the spring of 2020, the world experienced a global pandemic, which involved strict social distancing rules along with the shutdown of schools and universities or a transposition to remote teaching in most countries [1,2]. Consequently, a large proportion of adolescents and young adults found themselves with greater flexibility in their sleep schedules, whether it was from later school start times, a reduction in commute time and extracurricular activities, or other factors caused by the imposed restrictions related to the pandemic [[3], [4], [5], [6], [7]]. In this regard, studies have shown that delaying school start times have benefits such as an increase in sleep duration and sleep satisfaction, a decrease in daytime sleepiness, attention difficulties and depressive symptoms, as well as an improvement in motivation and academic performance in adolescents [[8], [9], [10], [11]]. However, despite these evidences, a vast majority of high schools are still maintaining early school start times [12,13]. The unique context caused by the lockdown associated with the pandemic is therefore an opportunity to study the impact of a more flexible schedule on sleep in adolescents and young adults during the school year.
Recent studies measuring the impact of the pandemic on sleep in adults showed mixed results during the pandemic. Adults went to bed later, woke up later, took more naps, but slept less at night, increased their sleeping pill consumption, reported poorer sleep quality as well as being less satisfied with their sleep during the pandemic [14,15]. This was accompanied by higher levels of psychological distress, such as anxiety and depressive symptoms [14,[16], [17], [18]]. Other studies in adults have shown that feelings of loneliness and a perception of low social support during the pandemic were associated with poor sleep quality and increased sleep difficulties [19,20]. In young adults, results are similar with later bedtimes, later wake times, but with longer sleep duration during the pandemic [7,21]. Studies also showed significant changes in lifestyle habits in young adults during the pandemic, such as spending less time engaging in physical activity and increasing their screen time, which significantly impacts their sleep [7]. On the other hand, longer sleep onset latencies, poorer sleep quality, increased insomnia symptoms and high prevalence of sleep problems were found in young adults during the pandemic [7,21,22]. Moreover, a recent study has showed a relationship between psychological factors and sleep during the pandemic, depressive and anxiety symptoms predicting sleep quality in young adults without any pre-existing diagnostic [23].
The shifts in sleep patterns and decreases in sleep quality have also been shown in children, although the impact of the COVID-19 pandemic on sleep duration varies across studies in this population [[24], [25], [26]]. To date, a few studies have been conducted specifically on the impact of the pandemic on sleep in adolescents. Researches show that during the pandemic, teens slept more, went to bed later, got up later, improved their sleep quality and felt more refreshed after sleep [[27], [28], [29], [30]]. Other studies report on the other hand a high prevalence of sleep problems and disrupted sleep quality during the pandemic among this population [22,[31], [32], [33]]. Moreover, there is an association between COVID-19 related worries and sleep onset difficulties, difficulties maintaining sleep, and delayed sleep/wake behaviors [34], yet teenagers report increased levels of anxiety and depressive symptoms since the beginning of the pandemic [[35], [36], [37]].
Adolescents are particularly vulnerable when it comes to sleep. During puberty, their sleep patterns change and this impacts their daytime functioning [38,39]. A recent study conducted on 35,821 adolescents showed that 55% of them did not get 8 h of sleep per night [40]. However, experts recommend at least 8–10 h of sleep in adolescents to maintain optimal daytime functioning [[41], [42], [43], [44]]. Also, teens between the age of 11 and 17 show a natural tendency to go to bed later and wake up later as they grow older [[45], [46], [47]]. In this regard, since it interferes with their natural rhythm, early school start times have been associated with shorter sleep duration and levels of daytime sleepiness similar to the ones observed in narcoleptics [48,49]. Moreover, social jetlag occurs when adolescents tend to sleep more and delay their sleep on weekends, which leads to the adoption of different sleep patterns during school days and weekends [48,50]. Delayed sleep patterns and insufficient sleep observed in adolescents often persist among young adults [51]. A study showed that college students report important sleep delays in their bedtimes and wake times and have short sleep duration because of school hours [51,52]. Freshmen students are getting less sleep than their older peers, and senior students report longer sleep onset latencies on weekdays than younger students [52]. It's around the ages of 20–22 years old that the chronotype reaches its peak and then, in the following years, tends to reverse to an earlier type [53]. Studies show that sleep difficulties, daytime sleepiness and dissatisfaction with sleep are still present in early adulthood [54,55].
The COVID-19 pandemic restriction measures and shutdown of schools or remote teaching has freed a vast majority of youth from the constraints of getting up early in the morning to attend school and has given them more flexibility in their daily schedules. The objective of this study was to assess the impact of the pandemic related lockdown on sleep in adolescents and young adults. We hypothesized that sleep habits would shift to a later time and sleep quality would improve during the lockdown as teenagers and young adults would be able to adopt a schedule closer to their natural sleep rhythm. We expected changes to be more important in teenagers than in young adults, since sleep disturbances and the sleep debt are more predominant in this age group [56,57]. We also expected changes in sleep habits to be more pronounced during weekdays than weekends, since school start times have been known to be a major determinant of sleep schedule during weekdays, and sleep habits are usually already more aligned with personal preferences on weekends under normal circumstances [48,58,59].
2. Methods
2.1. Participants
A total of 583 adolescents and young adults completed an anonymous online survey made available in the Province of Québec, Canada. They were recruited by email and through social media (eg Facebook, university website) and informed consent was obtained before entering the survey. Participants with missing data on items analyzed in the current study were excluded. A final sample of 498 adolescents and young adults aged between 12 and 25 years old (22.6% boys and 76.3% girls; mean age = 18.17 ± 3.72 years old) was obtained. This study was approved by the ethics committee of the Université du Québec en Outaouais.
2.2. Procedure and measures
In the province of Quebec, Canada, the state of emergency and the lockdown were declared on March 13th, 2020 [60]. The government of Québec rapidly implemented severe restrictions in the first month of the pandemic, imposing a closure of public places (casinos, gyms, bars, public pools, arenas, ski centers, theaters, etc.), of restaurants, daycare, shopping centers, hair salon and other business that were not essential. Also, any inside or outside gatherings of people and traveling between different geographic regions was prohibited. All elementary, middle and high schools, as well as colleges and universities were closed during the first month of the pandemic. The mid-point of the first wave was reached around the end of April 2020 [60]. At the beginning of May 2020, many restrictions measures persisted, but they were more flexible. Schools, colleges and universities were allowed to reopen under special conditions. Daycare, specific businesses, public librairies and parks were also reopened. In June, more restrictions were lifted on business, sports activities, and social distancing rules allowed for small gathering of a maximum of 10 people from 3 families. The end of the first wave was reached in July 2020 [60]. Once the government decreed that schools could reopen in May, most colleges and universities resumed their activities by switching to online teaching in either synchronous or asynchronous mode. Middle and high schools had to adapt to their younger population, some institutions choosing to alternate between in-class (with severe distancing rules and only a few hours per week) and remote teaching, but the majority adopting online class, either in asynchronous or in synchronous mode. For the majority of teens and young adults in school during May and June 2020 attending school in Québec involved mostly remote teaching and personal work at home.
The survey was administered in French, using Lime Survey, from June 3rd to July 3rd, 2020. Participants were asked to answer questions on sleep, lifestyle habits (home-made questions), and emotions (Differential Emotions Scale IV, [61]), retrospectively, referring to the time prior to the COVID-19 pandemic and lockdown situation and then, a second time referring to the time during the pandemic and lockdown situation. Specific instructions were given to participants to give answers that best estimate the majority of nights and days during the past month. They also had to complete a resilience questionnaire (Connor-Davidson Resilience Scale-10, [62]) and the reduced Morningness and Eveningness Questionnaire (rMEQ, [63]). Sleep was assessed using questions derived from the Pittsburgh Sleep Quality Index (PSQI) [64]. In order to verify the changes in sleep patterns during weekdays and weekends separately, questions were adapted accordingly. In order to shorten the survey, only specific questions on sleep habits, sleep quality and sleep difficulties were integrated in the survey. It took about 20 min to complete all questions.
Only data regarding sleep habits, sleep quality and sleep difficulties are reported in the present study. Dependant variables for sleep habits were the self-reported bedtimes and wake times hours, and the self-reported subjective sleep onset latencies and subjective sleep durations in minutes for both weekdays and weekends. Dependant variables for subjective sleep quality, excessive daytime sleepiness, and sleep difficulties associated with sleep onset difficulties, awakenings and nightmares were scores obtained on individual questions that were evaluated on a Likert scale.
2.3. Statistical analyses
Participants were divided into four age groups according to grade levels in Canada: 1) 12–14 years old (beginning of secondary school, which is the equivalent of middle school in the US, n = 108; 23% boys and 74.6% girls), 2) 15–17 years old (end of secondary school, which is the equivalent of high school in the US, n = 141; 19.6% boys and 79.8% girls), 3) 18–21 years old (college and undergraduate university students, n = 130; 22.8% boys and 76.6% girls), and 4) 22–25 years old (undergraduate, graduate university students and employed young adults, n = 118; 25.7% boys and 73.5% girls). There were more female participants in the sample, but there were no significant differences in the distribution of boys and girls between the four age groups (χ 2 (3) = 1.642, p = 0.650). Three-way repeated measures ANOVAs COVID-19 (Pre vs During the pandemic) X Week (Weekdays vs Weekends) X Age Groups (12–14; 15 to 17; 18 to 21; 22–25 years old) were calculated for bedtimes, wake times, sleep onset latency, and sleep duration. Two-way repeated measures ANOVAs COVID-19 (Pre vs During the pandemic) X Age Groups (12–14; 15 to 17; 18 to 21; 22–25 years old) were calculated for subjective sleep quality, excessive daytime sleepiness, and sleep difficulties associated with sleep onset difficulties, with nocturnal and early morning awakenings, and with nightmares. Post-hoc paired t-tests with Bonferroni's correction were used to identify the significant differences. All statistical analyses were performed using SPSS Statistics (version 27.0).
3. Results
3.1. Sleep habits variables
Normality and sphericity assumptions were met for all sleep habits variables. For the post-hoc analyses, a Bonferroni correction was applied, and statistical significance was considered at p < 0.00625.
Results for bedtimes show significant main effects of COVID-19, Week and Age Groups, but also significant interactions COVID-19 X Week and COVID-19 X Age Groups (see Table 1, Table 2 ). Post-hoc t-tests revealed that participants went to bed, on average, 1 h 13 min later during the pandemic on weekdays (t (496) = 19.15, p < 0.001, d = 0.82) and 31 min later on weekends (t (490) = 9.46, p < 0.001, d = 0.33). Therefore, the pandemic had a greater impact on weekdays bedtimes in all participants (see Table 2). Moreover, results show that during the pandemic, participants aged 12–14 years old (t (105) = 9.85, p < 0.001, d = 0.78), 15–17 years old (t (138) = 10.08, p < 0.001, d = 0.78), 18–21 years old (t (128) = 8.81, p < 0.001, d = 0.51), and 22–25 years old (t (116) = 4.76, p < 0.001, d = 0.38) went to bed later during the pandemic. However, the younger the participants were, the greater the difference was between before and during the pandemic (see Table 2).
Table 1.
Results for the tree-way repeated measures ANOVAs COVID-19 (Pre vs During the pandemic) X Week (Weekdays vs Weekends) X Age Groups (12–14; 15 to 17; 18 to 21; 22–25 years old) on sleep habits.
| Bedtimes |
Waketimes |
Sleep onset latency |
Subjective sleep duration |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| df | F | p | np2 | df | F | p | np2 | df | F | p | np2 | df | F | p | np2 | |
| COVID-19 | 1, 487 | 276.95 | <0.001 | 0.36 | 1, 490 | 350.11 | <0.001 | 0.42 | 1, 490 | 3.67 | 0.056 | 0.01 | 1, 489 | 97.57 | <0.001 | 0.17 |
| Week | 1, 487 | 423.85 | <0.001 | 0.47 | 1, 490 | 822.95 | <0.001 | 0.63 | 1, 490 | 51.75 | <0.001 | 0.10 | 1, 489 | 279.81 | <0.001 | 0.36 |
| Age Groups | 3, 487 | 7.51 | <0.001 | 0.04 | 3, 490 | 0.50 | 0.685 | 0.00 | 3, 490 | 4.23 | 0.006 | 0.03 | 3, 489 | 6.93 | <0.001 | 0.04 |
| Week X Age Groups | 3, 487 | 0.38 | 0.766 | 0.00 | 3, 490 | 2.78 | 0.041 | 0.02 | 3, 490 | 0.31 | 0.820 | 0.00 | 3, 489 | 2.79 | 0.04 | 0.02 |
| COVID-19 X Week | 1, 487 | 145.34 | <0.001 | 0.23 | 1, 490 | 472.43 | <0.001 | 0.49 | 1, 490 | 8.78 | 0.003 | 0.02 | 1, 489 | 185.56 | <0.001 | 0.28 |
| COVID-19 X Age Groups | 3, 487 | 6.59 | <0.001 | 0.04 | 3, 490 | 7.01 | <0.001 | 0.04 | 3, 490 | 6.65 | <0.001 | 0.04 | 3, 489 | 1.70 | 0.167 | 0.01 |
| COVID-19 X Week X Age Groups | 3, 487 | 1.38 | 0.247 | 0.01 | 3, 490 | 7.05 | <0.001 | 0.04 | 3, 490 | 1.86 | 0.136 | 0.01 | 3, 489 | 0.22 | 0.883 | 0.00 |
Table 2.
Means and standard deviation (SD) of sleep variables before and during the COVID-19 pandemic.
| Bedtimes |
Waketimes |
Sleep onset latency |
Subjective sleep duration |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weekdays |
Weekends |
Weekdays |
Weekends |
Weekdays |
Weekends |
Weekdays |
Weekends |
|||||||||
| Hours | SD | Hours | SD | Hours | SD | Hours | SD | Hours | SD | Hours | SD | Hours | SD | Hours | SD | |
| All participants | ||||||||||||||||
| Before | 10:24 | 1:12 | 11:30 | 1:31 | 7:03 | 1:09 | 9:22 | 1:35 | 0:37 | 0:40 | 0:30 | 0:36 | 7:42 | 1:25 | 9:06 | 1:41 |
| During | 11:37 | 1:43 | 00:02 | 1:44 | 9:02 | 1:46 | 9:36 | 1:41 | 0:37 | 0:41 | 0:33 | 0:39 | 8:44 | 1:32 | 9:10 | 1:40 |
| 12–14 years old | ||||||||||||||||
| Before | 9:44 | 1:05 | 10:49 | 1:31 | 6:37 | 0:47 | 9:12 | 1:43 | 0:48 | 0:44 | 0:40 | 0:45 | 8:01 | 1:32 | 9:29 | 1:43 |
| During | 11:14 | 1:53 | 11:41 | 1:54 | 9:10 | 1:43 | 9:45 | 1:46 | 0:45 | 0:44 | 0:41 | 0:45 | 9:15 | 1:39 | 9:43 | 1:43 |
| 15–17 year old | ||||||||||||||||
| Before | 10:21 | 1:02 | 11:32 | 1:20 | 6:48 | 1:03 | 9:28 | 1:39 | 0:42 | 0:44 | 0:34 | 0:40 | 7:36 | 1:22 | 9:16 | 1:45 |
| During | 11:46 | 1:38 | 00:08 | 1:37 | 9:04 | 1:38 | 9:33 | 1:37 | 0:35 | 0:41 | 0:31 | 0:37 | 8:32 | 1:26 | 9:09 | 1:49 |
| 18–21 year old | ||||||||||||||||
| Before | 10:39 | 1:09 | 11:49 | 1:37 | 7:17 | 1:09 | 9:27 | 1:28 | 0:29 | 0:34 | 0:22 | 0:28 | 7:38 | 1:32 | 8:56 | 1:44 |
| During | 11:49 | 1:47 | 00:15 | 1:48 | 9:03 | 1:50 | 9:40 | 1:33 | 0:35 | 0:40 | 0:29 | 0:37 | 8:44 | 1:36 | 9:05 | 1:38 |
| 22–25 year old | ||||||||||||||||
| Before | 10:46 | 1:16 | 11:44 | 1:25 | 7:29 | 1:20 | 9:20 | 1:29 | 0:28 | 0:34 | 0:24 | 0:27 | 7:34 | 1:10 | 8:45 | 1:25 |
| During | 11:35 | 1:32 | 00:01 | 1:34 | 8:53 | 1:52 | 9:28 | 1:49 | 0:36 | 0:39 | 0:33 | 0:36 | 8:27 | 1:23 | 8:45 | 1:19 |
Results for wake times show significant main effects of COVID-19 and Week, significant Week X Age Groups, COVID-19 X Week, COVID-19 X Age Groups, and COVID-19 X Week X Age Groups interactions (see Table 1, Table 2). These results suggest that the effect of the pandemic was different between weekdays and weekends across age groups (see Table 2) during the pandemic. Post-hoc analyses revealed that adolescents aged 12–14 years old woke up later both on weekdays (t (107) = 15.10, p < 0.001, d = 1.92) and weekends (t (106) = 4.98, p < 0.001, d = 0.32) during the pandemic. On the other hand, changes in wake times were only noted during weekdays for the 15–17 years old (t (140) = 15.01, p < 0.001, d = 1.66), 18–21 years old (t (129) = 10.45, p < 0.001, d = 1.16) and 22–25 years old (t (117) = 9.21, p < 0.001, d = 0.87).
For sleep onset latency, significant main effects of Week and Age Groups, and significant COVID-19 X Week and COVID-19 X Age Groups interactions were found (see Table 1, Table 2). Post-hoc analyses revealed that on weekends, participants took on average 3 min longer to fall asleep during the pandemic (t (493) = 2.92, p = 0.004, d = 0.08), although the effect size of these changes is very small, while there were no changes during weekdays (t (496) = 0.51, p = 0.613). On the other hand, results showed that the pandemic had a different impact across age groups. Indeed, there was a significant increase in sleep onset latency during the pandemic in the 22–25 years old (t (116) = 3.22, p = 0.002, d = 0.27), but not in the 12–14 year olds (t (106) = −0.28, p = 0.781), the 15–17 year olds (t (140) = −2.09, p = 0.038) and the 18–21 year olds (t (128) = 2.68, p = 0.008).
Subjective sleep duration analyses showed significant main effects of COVID-19, Week and Age Groups, significant interactions Age Groups X Week and COVID-19 X Week (see Table 1, Table 2). Post-hoc comparisons showed that sleep duration was 1 h and 2 min longer on weekdays during the pandemic (t (495) = 14.63, p < 0.001, d = 0.70), but no significant changes were found during the weekend (t (493) = 0.95, p = 0.344). On the other hand, the analyses also showed that sleep duration was longer on weekends compared to weekdays in the 12–14 year olds (t (105) = 8.02, p < 0.001, d = 0.74), the 15–17 year olds (t (140) = 9.35, p < 0.001, d = 0.80), the 18–21 year olds (t (128) = 7.73, p < 0.001, d = 0.55), and the 22–25 year olds (t (116) = 9.55, p < 0.001, d = 0.68), but the difference between weekdays and weekends was greater in the younger participants (see Table 2).
3.2. Sleep quality, daytime sleepiness and sleep difficulties
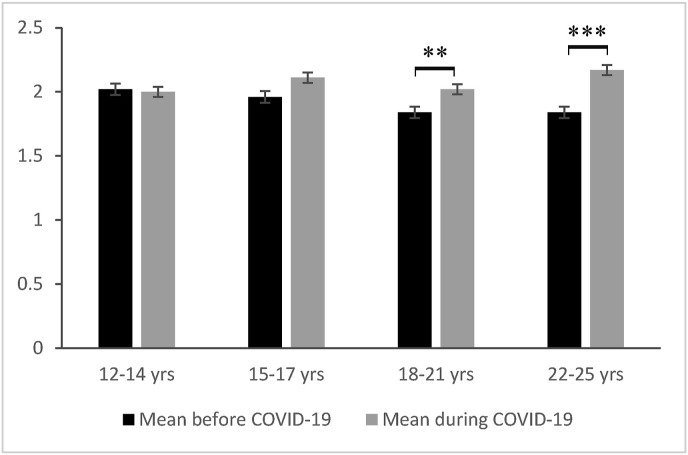
Sleep quality, daytime sleepiness and sleep difficulties results are presented in Table 3 and Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5 . Normality and sphericity assumptions were met for all variables. For the post-hoc analyses, a Bonferroni correction was applied, and statistical significance was considered at p < 0.01.
Table 3.
Results for the two-way repeated measures ANOVAs COVID-19 (Pre vs During the pandemic) X Age Groups (12–14; 15 to 17; 18 to 21; 22–25 years old) on subjective sleep quality, excessive daytime sleepiness and sleep difficulties variables.
| Subjective sleep quality |
Excessive daytime sleepiness |
Sleep onset difficulties |
Noctural and early morning awakenings |
Nightmares |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| df | F | p | np2 | df | F | p | np2 | df | F | p | np2 | df | F | p | np2 | df | F | p | np2 | |
| COVID-19 | 1, 493 | 30.82 | <0.001 | 0.06 | 1, 493 | 17.70 | <0.001 | 0.04 | 1, 495 | 2.02 | 0.156 | 0.00 | 1, 494 | 15.79 | <0.001 | 0.03 | 1, 494 | 21.09 | <0.001 | 0.04 |
| Age Groups | 3, 493 | 1.82 | 0.142 | 0.01 | 3, 493 | 0.90 | 0.443 | 0.01 | 3, 495 | 12.16 | <0.001 | 0.07 | 3, 494 | 0.47 | 0.702 | 0.00 | 3, 494 | 0.32 | 0.809 | 0.00 |
| COVID-19 X Age Groups | 3, 493 | 5.72 | 0.001 | 0.03 | 3, 493 | 2.70 | 0.045 | 0.02 | 3, 495 | 8.43 | <0.001 | 0.05 | 3, 494 | 2.29 | 0.078 | 0.01 | 3, 494 | 4.01 | 0.008 | 0.02 |
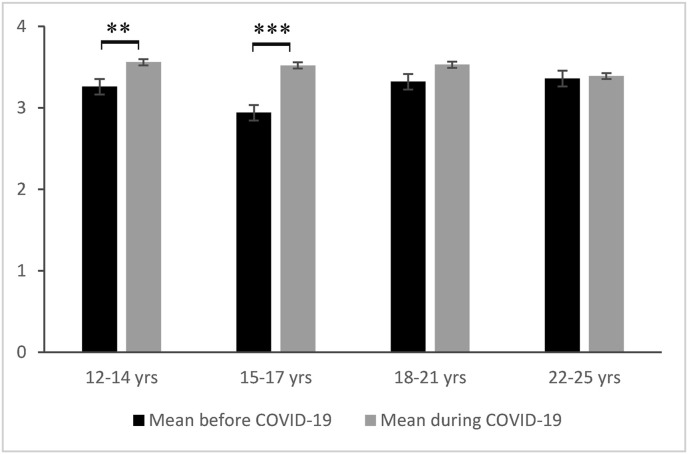
Fig. 1.
Post hoc paired t-tests for subjective sleep quality before and during the pandemic. ∗∗∗p < 0.001; ∗∗p < 0.01. Error bars represent standard errors of mean (SEM). Higher score means an improvement in subjective sleep quality.
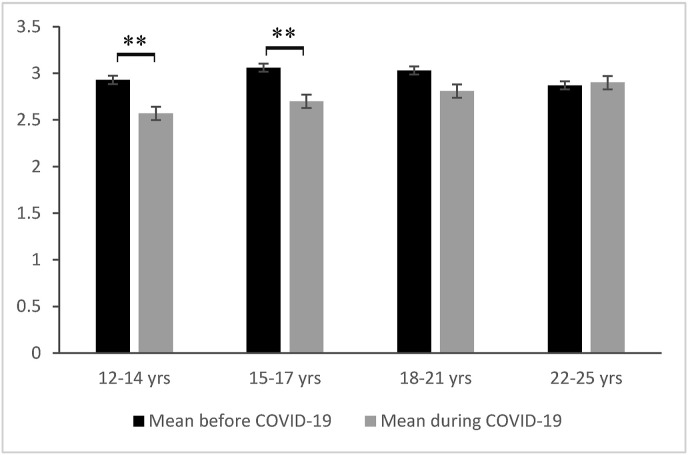
Fig. 2.
Post hoc paired t-tests for excessive daytime sleepiness before and during the pandemic. ∗∗p < 0.01. Error bars represent standard errors of mean (SEM). Higher score means more excessive daytime sleepiness.
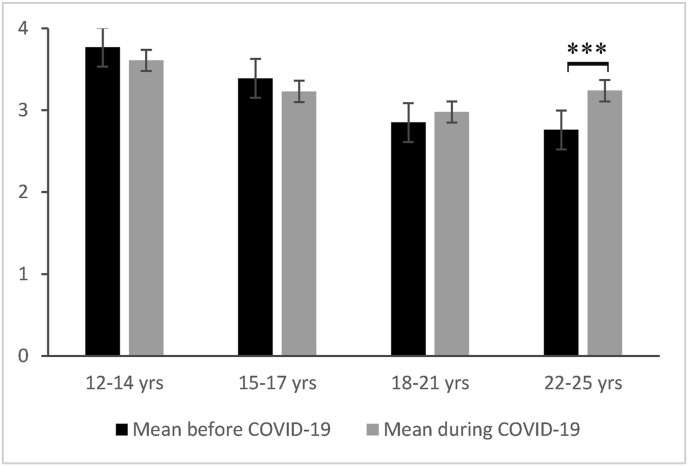
Fig. 3.
Post hoc paired t-tests for sleep difficulties associated with sleep onset difficulties before and during the pandemic. ∗∗∗p < 0.001, Error bars represent standard errors of mean (SEM), Higher score means more sleep onset difficulties.
Fig. 4.
Post hoc paired t-tests for sleep difficulties associated with nocturnal and early morning awakenings before and during the pandemic. ∗∗∗p < 0.001; ∗∗p < 0.01, Error bars represent standard errors of mean (SEM), Higher score means more nocturnal and early morning awakenings.
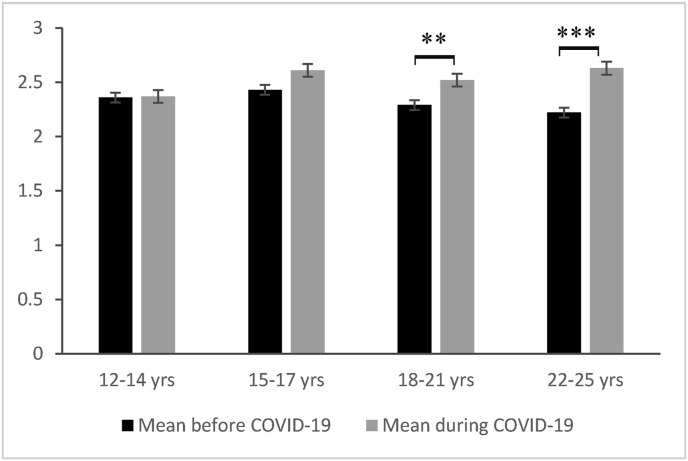
Fig. 5.
Post hoc paired t-tests for sleep difficulties associated with nightmares before and during the pandemic. ∗∗∗p < 0.001; ∗∗p < 0.01, Error bars represent standard errors of mean (SEM), Higher score means more nightmares.
Results for subjective sleep quality show a significant main effect of COVID-19 and a significant COVID-19 X Age Groups interaction (see Table 3 and Fig. 1). Post-hoc analyses showed an improved sleep quality during the pandemic, but this was only significant in the 12–14 year olds (t (107) = 2.61, p = 0.01, d = 0.28) and the 15–17 year olds (t (140) = 6.49, p < 0.001, d = 0.64). No significant changes in subjective sleep quality were reported in the 18–21 year olds (t (129) = 2.31, p = 0.022) and the 22–25 year olds (t (117) = 0.23, p = 0.816).
Excessive daytime sleepiness analyses show a significant main effect of COVID-19 and a significant COVID-19 X Age Groups interaction (see Table 3 and Fig. 2). Post hoc t-tests show that during the pandemic, there was an improvement in daytime sleepiness in the 12–14 year olds (t (107) = −3.21, p = 0.002, d = 0.34) and the 15–17 year olds (t (140) = −3.34, p = 0.001, d = 0.35) but not in the 18 to 21 (t (129) = −2.20, p = 0.03) and the 22–25 year olds (t (117) = 0.23, p = 0.818).
Results for sleep difficulties associated with sleep onset difficulties show a significant main effect of Age Groups and a significant COVID-19 X Age Groups interaction (see Table 3 and Fig. 3). Post hoc analyses revealed that there were no changes in sleep onset difficulties in the 12–14 year olds (t (107) = −1.60, p = 0.113), the 15–17 year olds (t (141) = −1.55, p = 0.124) and the 18–21 year olds (t (130) = 1.47, p = 0.145), while the 22–25 year olds reported a significant increase in sleep difficulties associated with sleep onset difficulties during the pandemic (t (117) = 4.31, p < 0.001, d = 0.37).
For sleep difficulties associated with nocturnal and early morning awakenings, a significant main effect of COVID-19 was found, post-hoc analyses showing an increase during the pandemic (t (497) = 4.04, p < 0.001, d = 0.18; see Table 3 and Fig. 4). In addition, exploratory analyses revealed that sleep difficulties associated with nocturnal and early morning awakenings significantly increased only for the 18–21 year olds (t (129) = 2.83, p = 0.005, d = 0.19) and the 22–25 year olds (t (117) = 3.66, p < 0.001, d = 0.35), and not for the 12–14 year olds (t (107) = 0.08, p = 0.935) and the 15–17 year olds (t (141) = 1.72, p = 0.088).
Analyses on sleep difficulties associated with nightmares show a significant main effect of COVID-19 and a significant COVID-19 X Age Group interaction (see Table 3 and Fig. 5). Post hoc t-tests revealed an increase in sleep difficulties associated with nightmares, but only in the 18–21 year olds (t (129) = 3.04, p = 0.003, d = 0.18) and 22–25 year olds (t (117) = 4.51, p < 0.001, d = 0.31), while there were no significant changes in reported by the 12–14 year olds (t (107) = −0.25, p = 0.801) and the 15–17 year olds (t (141) = 2.07, p = 0.041) during the pandemic.
4. Discussion
This study provides evidence of substantial changes in sleep in adolescents and young adults during the first wave of the COVID-19 pandemic. During weekdays, participants showed a delay in their bedtimes and wake times accompanied by an increase in sleep duration. On the other hand, during weekends, there were almost no changes in sleep patterns during the pandemic. Moreover, our results revealed significant differences in the impact of the pandemic on sleep across age. First, changes in sleep habits and sleep duration are more pronounced in teenagers than in young adults. Also, despite the presence of changes in sleep patterns and longer sleep duration in all participants, the adolescents were the only ones to report improvements in daytime sleepiness and subjective sleep quality, young adults reporting no changes during the pandemic on these aspects. Furthermore, young adults reported more sleep difficulties associated with longer sleep onset, nocturnal and early morning awakenings, and with nightmares during the pandemic, while there were no changes on these aspects in adolescents.
Our results suggest that the changes in sleep that occur with the COVID-19 pandemic seem to have beneficial effects on adolescents aged 12–17 years old. However, beyond the age of 18, these benefits are not as obvious. More interestingly, our results suggest that in teens, the biological drive combined with the sleep disturbances and omnipresent chronic sleep deprivation results in adolescents having, during the pandemic, a tremendous need to recuperate a long-acquired sleep debt. Thus, the benefits of a longer sleep, aligned with their circadian phase, outweigh the negative impacts that could be caused by additional stress related to the pandemic. Our results are also in accordance with other studies showing that adolescents experienced a delay in their sleep during the COVID-19 pandemic, resulting in longer sleep durations [27,65], improved subjective sleep quality and decreased daytime sleepiness [27]. Altogether, this suggests that when they are freed from environmental constraints such as school start times, adolescents tend to follow their natural rhythm, which leads to a delayed, more recuperative and longer sleep. This has also been reported by studies comparing sleep during the summer and sleep during the school year in teenagers [66,67]. Our results reinforce the importance of bringing forward the debate on school start times and how to adapt schedules to the needs of the adolescents. Delaying school start time in youth can increase sleep duration and lead to increased satisfaction with sleep, improved motivation and class attendance as well as reduced daytime sleepiness, fatigue, depressed mood and mental health concerns [10,68,69]. However, since the pandemic has brought tremendous changes in the lifestyle of teens and young adults, it is important to consider the fact that other factors could explain or may have exacerbated these changes in sleep habits in this population. In this regard, a significant reduction in physical activity levels, increases in sedentary behavior as well as in screen time have been reported in youth in various studies [31,65,70], factors that have been associated with sleep quality in teenagers [71,72]. This is consistent with the fact that despite an improvement in sleep on several levels, adolescents aged 12–17 years old still complain of high levels of sleep difficulties associated with long sleep onset latencies before and during the pandemic, reporting sleep latencies lasting around 40 min before as well as during the pandemic. It could therefore be important to address sleep hygiene in adolescents to properly frame personal time, especially evening time, in order to optimize the benefits of a good night's sleep.
The age differences that were found in this study could be modulated by interindividual or situational factors such as sex, chronotype, resilience, employment, or other external factors. This therefore implies that young adults’ sleep may possibly be more impacted than the younger teens by individual characteristics and by external stressors brought by the pandemic. For example, our results might be explained in part by the fact that young adults are already starting to experience more flexible schedules in college and universities, therefore the sleep debt in this population could be less pronounced. This is combined with a change towards an earlier chronotype at the beginning of their twenties [73,74]. Consequently, stress, changes in lifestyle habits, employment and other factors associated with the pandemic could be elements that have a greater impact on sleep in young adults and prevent them from fully benefiting from their new adopted sleep habits during the pandemic. As such, a study showed that high levels of post-traumatic stress disorder and COVID-19 related worry explained poorer sleep quality in young adults during the pandemic [23]. Other studies in adults and young adults have also found increases in nightmares during the pandemic [75,76]. Employment is another factor that can affect sleep in youth and is generally more prominent in young adults than in teenagers [[77], [78], [79], [80]]. In this regard, it is possible that young adults might have had to work more hours or experienced more stress towards work during the pandemic compared to young teenagers, and this could result in a decreased sleep quality and increased sleep onset latencies and awakenings [[79], [80], [81], [82]]. Moreover, a recent survey found elevated levels of substance use in adults and young adults during the first wave of COVID-19 [83], which is a lifestyle habit that has been associated with sleep difficulties in this population [[84], [85], [86], [87]].
It is important to note that this study focused on the impact of the COVID-19 lockdown on sleep during the first wave of the pandemic, in the spring of 2020. During this period, remote teaching and possible reduced school expectations lead to more flexible and less restrictive schedules in adolescents and young adults. However, strict social distancing rules and imposed isolation may have caused significant psychological distress in many people. In this regard, considering the benefits of sleep to mental health and well-being, improvements in sleep observed in adolescents at the beginning of the pandemic may have acted as a protective factor. However, schools, colleges and universities have resumed most of their activities in the Fall of 2020. Even though most of them chose remote teaching or an alternating mode (alternate between in-class and online class), the requirements and the restrictive school schedules are mostly in line with what was planned before the pandemic. Moreover, adolescents have now experienced the cumulating stress, anxiety and social isolation related to the pandemic for a year [88,89]. Consequently, without the opportunity to allocate more time to sleep and thus benefit from a good sleep, adolescents and young adults might be more at risk for mental health issues. This is even more concerning considering that young adults, despite an improvement in their sleep duration and a better alignment with their natural rhythm, were already reporting an increase in sleep difficulties at the beginning of the pandemic. This raises important issues regarding the identification of factors that may exacerbate sleep difficulties during the pandemic in this population and, in turn, increase vulnerability to mental health problems.
This study has several limitations. First, all data are subjective sleep measures that are self-reported. Secondly, the data in this research was collected through a cross-sectional design and part of it was collected retrospectively, since participants had to remember how they slept or felt before the pandemic. This could therefore lead to recall bias in participants. Third, other factors that could have been present before the pandemic were not assessed. Viral infection was also not measured in this study. However, specific instructions were given to participants to give answers that best estimate the majority of nights and days during the past month, thus hopefully minimizing the impact of any specific event in time. It is also important to point out that our results don't allow any causal relationship between the pandemic and sleep in youth, nor can it explain entirely the differences between the adolescents and young adults. Indeed, further research is needed to assess the contribution of many other factors to changes in sleep in this population. For example, the effect of chronotype, resilience, virus infection, employment, lifestyle habits, psychological factors, etc. could be investigated. The current study focuses on a general picture of the data, but does not exclude the presence of particular profiles within the sample. For example, the presence of sleep disturbances in youth is omnipresent and the pandemic has brought its own set of challenges. Thus, it would be important to investigate whether adolescents or young adults with particular profiles, such as pre-existing sleep problems or otherwise, were similarly affected by the pandemic. Also, we had equal distribution of sex across our age groups. However, it could be interesting to investigate if both boys and girls reported similar changes in their sleep during the pandemic and if they benefit from these changes in the same extent. Since the sample was comprised of only French Canadians from the province of Québec, this could also limit the generalizability of the results. Another important limitation is the fact that sleep was measured using only specific and adapted questions derived from the PSQI instead of the full original validated questionnaire. This was a choice the authors made in order to minimize the risk of the teens and young adults dropping out of the survey due to its length, but also because it allowed them to better estimate changes in sleep separately during weekdays and weekends, which was not possible with the original version. Aside from these limitations, this research provides valuable information about sleep in adolescents and young adults during the pandemic and helps us better understand how external factors may contribute to sleep habits and sleep disturbances in youth.
5. Conclusions
The first wave of the COVID-19 pandemic in March 2020 has caused many changes in sleep habits and sleep quality in adolescents and young adults. Further research is needed to assess the contribution of different modulating factors to these changes. However, it is important to note that a vast majority of schools have started again in the fall of 2020, with regular schedules. Therefore, today's young people find themselves in a situation where they have experienced the cumulating stress of the pandemic and extreme social isolation for almost a year but are unable to benefit from a good night of sleep as they did at the beginning of the pandemic. This highlights the necessity of bringing forward the debate of later school start times in adolescents in order to better adapt schedules to their needs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit authors statement
Laura Ramos Socarras, Jérémie Potvin and Geneviève Forest formulated the research question and designed the study. Laura Ramos Socarras and Jérémie Potvin carried out the data collection. Laura Ramos Socarras analyzed the data. Laura Ramos Socarras and Geneviève Forest were involved in writing the manuscript. All authors have approved the final draft for the submission and take responsibility for the entire manuscript.
Acknowledgments
The authors would like to thank everyone who participated in the study.
Footnotes
The authors have no conflicts of interest to declare.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.04.010.
Conflict of interest
The following is the supplementary data to this article:
Multimedia component 1
References
- 1.Wang G., Zhang Y., Zhao J., et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020 doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esposito S., Principi N. School closure during the coronavirus disease 2019 (COVID-19) pandemic: an effective intervention at the global level? JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1892. [DOI] [PubMed] [Google Scholar]
- 3.Meltzer L.J., Shaheed K., Ambler D. Start later, sleep later: school start times and adolescent sleep in homeschool versus public/private school students. Behav Sleep Med. 2016 doi: 10.1080/15402002.2014.963584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas J. Learning from homeschooling routines. J Res Christ Educ. 2016 doi: 10.1080/10656219.2016.1237910. [DOI] [Google Scholar]
- 5.Isumi A., Doi S., Yamaoka Y., et al. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abus Negl. 2020 doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Courtney D., Watson P., Battaglia M., et al. COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can J Psychiatr. 2020 doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sañudo B., Fennell C., Sánchez-Oliver A.J. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns preand during-COVID-19 quarantine in young adults from Spain. Sustain. 2020 doi: 10.3390/SU12155890. [DOI] [Google Scholar]
- 8.Dexter D., Bijwadia J., Schilling D., et al. Sleep, sleepiness and school start times: a preliminary study. Wis Med J. 2003 [PubMed] [Google Scholar]
- 9.Epstein R., Chillag N., Lavie P. Starting times of school: effects on daytime functioning of fifth-grade children in Israel. Sleep. 1998 doi: 10.1093/sleep/21.3.250. [DOI] [PubMed] [Google Scholar]
- 10.Owens J.A., Belon K., Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010 doi: 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 11.Wolfson A.R., Spaulding N.L., Dandrow C., et al. Middle school start times: the importance of a good night's sleep for young adolescents. Behav Sleep Med. 2007 doi: 10.1080/15402000701263809. [DOI] [PubMed] [Google Scholar]
- 12.Wheaton A.G., Ferro G.A., Croft J.B. School start times for middle school and high school students — United States, 2011–12 school year. MMWR Morb Mortal Wkly Rep. 2015 doi: 10.15585/mmwr.mm6430a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gariépy G., Janssen I., Sentenac M., et al. School start time and sleep in Canadian adolescents. J Sleep Res. 2017 doi: 10.1111/jsr.12475. [DOI] [PubMed] [Google Scholar]
- 14.Gupta R., Grover S., Basu A., et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatr. 2020 doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mandelkorn U., Genzer S., Choshen-Hillel S., et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. 2020 doi: 10.5664/jcsm.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duran S., Erkin Ö. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021 doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casagrande M., Favieri F., Tambelli R., et al. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stanton R., To Q.G., Khalesi S., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Publ Health. 2020 doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grossman E.S., Hoffman Y.S.G., Palgi Y., et al. COVID-19 related loneliness and sleep problems in older adults: worries and resilience as potential moderators. Pers Indiv Differ. 2021 doi: 10.1016/j.paid.2020.110371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grey I., Arora T., Thomas J., et al. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatr Res. 2020 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marelli S., Castelnuovo A., Somma A., et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2020 doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou S.J., Wang L.L., Yang R., et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hyun S., Hahm H.C., Wong G.T.F., et al. Psychological correlates of poor sleep quality among U.S. young adults during the COVID-19 pandemic. Sleep Med. 2021 doi: 10.1016/j.sleep.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dellagiulia A., Lionetti F., Fasolo M., et al. Early impact of COVID-19 lockdown on children's sleep: a 4-week longitudinal study. J Clin Sleep Med. 2020 doi: 10.5664/jcsm.8648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Z., Tang H., Jin Q., et al. Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J Sleep Res. 2020 doi: 10.1111/jsr.13142. [DOI] [PubMed] [Google Scholar]
- 26.Zreik G., Asraf K., Haimov I., et al. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. 2020 doi: 10.1111/jsr.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gruber R., Saha S., Somerville G., et al. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.López-Bueno R., López-Sánchez G.F., Casajús J.A., et al. Health-related behaviors among school-aged children and adolescents during the Spanish covid-19 confinement. Front Pediatr. 2020 doi: 10.3389/fped.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.López-Gil J.F., Tremblay M.S., Brazo-Sayavera J. Changes in healthy behaviors and meeting 24-h movement guidelines in Spanish and Brazilian preschoolers, children and adolescents during the COVID-19 lockdown. Children. 2021 doi: 10.3390/children8020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dragun R., Veček N.N., Marendić M., et al. Have lifestyle habits and psychological well-being changed among adolescents and medical students due to COVID-19 lockdown in Croatia? Nutrients. 2021 doi: 10.3390/nu13010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bates L.C., Zieff G., Stanford K., et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children. 2020 doi: 10.3390/children7090138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lavigne-Cerván R., Costa-López B., Juárez-Ruiz de Mier R., et al. Consequences of COVID-19 confinement on anxiety, sleep and executive functions of children and adolescents in Spain. Front Psychol. 2021 doi: 10.3389/fpsyg.2021.565516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murata S., Rezeppa T., Thoma B., et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021 doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Becker S.P., Dvorsky M.R., Breaux R., et al. Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep. 2021:1–25. doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duan L., Shao X., Wang Y., et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020 doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Racine N., Cooke J.E., Eirich R., et al. Child and adolescent mental illness during COVID-19: a rapid review. Psychiatr Res. 2020 doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tardif-Grenier K., Archambault I., Dupéré V., et al. Canadian adolescents' internalized symptoms in pandemic times: sex differences and association with sociodemographic characteristics, confinement habits, and support. Res Sq. 2020 doi: 10.21203/rs.3.rs-93849/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Owens J., Au R., Carskadon M., et al. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014 doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolfson A.R., Carskadon M.A. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998 doi: 10.1111/j.1467-8624.1998.tb06149.x. [DOI] [PubMed] [Google Scholar]
- 40.Patte K.A., Qian W., Leatherdale S.T. Sleep duration trends and trajectories among youth in the COMPASS study. Sleep Heal. 2017 doi: 10.1016/j.sleh.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 41.Fuligni A.J., Bai S., Krull J.L., et al. Individual differences in optimum sleep for daily mood during adolescence. J Clin Child Adolesc Psychol. 2019 doi: 10.1080/15374416.2017.1357126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hirshkowitz M., Whiton K., Albert S.M., et al. National sleep foundation's sleep time duration recommendations: methodology and results summary. Sleep Heal. 2015 doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 43.Paruthi S., Brooks L.J., D'Ambrosio C., et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016 doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Short M.A., Weber N., Reynolds C., et al. Estimating adolescent sleep need using dose-response modeling. Sleep. 2018 doi: 10.1093/sleep/zsy011. [DOI] [PubMed] [Google Scholar]
- 45.Andrade M., Menna-Barreto L. Sleep patterns of high school students living in são paulo, Brazil. Adolesc. Sleep Patterns. 2009 doi: 10.1017/cbo9780511499999.010. [DOI] [Google Scholar]
- 46.Crowley S.J., Acebo C., Carskadon M.A. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007 doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 47.Yang C.K., Kim J.K., Patel S.R., et al. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005 doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- 48.Hansen M., Janssen I., Schiff A., et al. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005 doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 49.Owens J.A., Dearth-Wesley T., Herman A.N., et al. A quasi-experimental study of the impact of school start time changes on adolescent sleep. Sleep Heal. 2017 doi: 10.1016/j.sleh.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Wittmann M., Dinich J., Merrow M., et al. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006 doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 51.Lund H.G., Reider B.D., Whiting A.B., et al. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010 doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 52.Tsai L.L., Li S.P. Sleep patterns in college students: gender and grade differences. J Psychosom Res. 2004 doi: 10.1016/S0022-3999(03)00507-5. [DOI] [PubMed] [Google Scholar]
- 53.Roenneberg T., Kuehnle T., Pramstaller P.P., et al. A marker for the end of adolescence. Curr Biol. 2004 doi: 10.1016/j.cub.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 54.Ohayon M.M., Roberts R.E. Comparability of sleep disorders diagnoses using DSM-IV and ICSD classifications with adolescents. Sleep. 2001 doi: 10.1093/sleep/24.8.920. [DOI] [PubMed] [Google Scholar]
- 55.Ohayon M.M., Roberts R.E., Zulley J., et al. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000 doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 56.Fukuda K., Ishihara K. Age-related changes of sleeping pattern during adolescence. Psychiatr Clin Neurosci. 2001 doi: 10.1046/j.1440-1819.2001.00837.x. [DOI] [PubMed] [Google Scholar]
- 57.Park Y.M., Matsumoto K., Shinkoda H., et al. Age and gender difference in habitual sleep-wake rhythm. Psychiatr Clin Neurosci. 2001 doi: 10.1046/j.1440-1819.2001.00825.x. [DOI] [PubMed] [Google Scholar]
- 58.Szymczak J.T., Jasinska M., Pawlak E., et al. Annual and weekly changes in the sleep-wake rhythm of school children. Sleep. 1993 doi: 10.1093/sleep/16.5.433. [DOI] [PubMed] [Google Scholar]
- 59.Andrade M.M.M., Benedito-Silva A.A., Domenice S., et al. Sleep characteristics of adolescents: a longitudinal study. J Adolesc Health. 1993 doi: 10.1016/S1054-139X(08)80016-X. [DOI] [PubMed] [Google Scholar]
- 60.Ligne du temps COVID-19 au Québec. Inst Natl Santé Publique Du Québec. 2021 [Google Scholar]
- 61.Ricard-St-Aubin J.S., Philippe F.L., Beaulieu-Pelletier G., et al. Validation francophone de l’Échelle des émotions différentielles IV (EED-IV) Rev Eur Psychol Appl. 2010 doi: 10.1016/j.erap.2009.05.001. [DOI] [Google Scholar]
- 62.Hébert M., Parent N., Simard C., et al. Validation of the French Canadian version of the brief Connor-Davidson resilience scale (CD-RISC 10) Can J Behav Sci. 2018 doi: 10.1037/cbs0000092. [DOI] [Google Scholar]
- 63.Adan A., Almirall H. Horne & Östberg morningness-eveningness questionnaire: a reduced scale. Pers Indiv Differ. 1991 doi: 10.1016/0191-8869(91)90110-W. [DOI] [Google Scholar]
- 64.Buysse D.J., Reynolds C.F., Monk T.H., et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989 doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 65.Oliviero B., Emanuela M., Mattia D., et al. Changes in sleep patterns and disturbances in children and adolescents in Italy during the covid-19 outbreak. Sleep Med. 2021 doi: 10.1016/j.sleep.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Crowley S.J., Acebo C., Fallone G., et al. Estimating dim light melatonin onset (DLMO) phase in adolescents using summer or school-year sleep/wake schedules. Sleep. 2006 doi: 10.1093/sleep/29.12.1632. [DOI] [PubMed] [Google Scholar]
- 67.De Sousa I.C., Louzada F.M., De Azevedo C.V.M. Sleep-wake cycle irregularity and daytime sleepiness in adolescents on schooldays and on vacation days. Sleep Sci. 2009 [Google Scholar]
- 68.Wahistrom K. Changing times: findings from the first longitudinal study of later high school start times. NASSP Bull. 2002 doi: 10.1177/019263650208663302. [DOI] [Google Scholar]
- 69.Wahlstrom K.L., Berger A.T., Widome R. Relationships between school start time, sleep duration, and adolescent behaviors. Sleep Heal. 2017 doi: 10.1016/j.sleh.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moore S.A., Faulkner G., Rhodes R.E., et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020 doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lang C., Kalak N., Brand S., et al. The relationship between physical activity and sleep from mid adolescence to early adulthood. A systematic review of methodological approaches and meta-analysis. Sleep Med Rev. 2016 doi: 10.1016/j.smrv.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 72.Woods H.C., Scott H. #Sleepyteens: social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J Adolesc. 2016 doi: 10.1016/j.adolescence.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 73.Randler C. Chronotype in children and adolescents. Somnologie. 2016 doi: 10.1007/s11818-016-0073-5. [DOI] [Google Scholar]
- 74.BaHammam A.S., Almestehi W., Albatli A., et al. Distribution of chronotypes in a large sample of young adult Saudis. Ann Saudi Med. 2011 doi: 10.4103/0256-4947.78207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kilius E., Abbas N.H., McKinnon L., et al. Pandemic nightmares: COVID-19 lockdown associated with increased aggression in female university students' dreams. Front Psychol. 2021 doi: 10.3389/fpsyg.2021.644636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schredl M., Bulkeley K. Dreaming and the COVID-19 pandemic: a survey in a U.S. Sample. Dreaming. 2020 doi: 10.1037/drm0000146. [DOI] [Google Scholar]
- 77.Sum A., Khatiwada I., Trubskyy M., et al. vol. 28. 2014. (The plummeting labor market fortunes of teens and young adults). [Google Scholar]
- 78.Knutson K.L., Lauderdale D.S. Sociodemographic and behavioral predictors of bed time and wake time among US adolescents aged 15 to 17 years. J Pediatr. 2009 doi: 10.1016/j.jpeds.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fischer F.M., Nagai R., Teixeira L.R. Explaining sleep duration in adolescents: the impact of socio-demographic and lifestyle factors and working status. Chronobiol Int. 2008 doi: 10.1080/07420520802110639. [DOI] [PubMed] [Google Scholar]
- 80.Hoefelmann L.P., Lopes A. da S., da Silva K.S., et al. Sociodemographic factors associated with sleep quality and sleep duration in adolescents from santa catarina, Brazil: what changed between 2001 and 2011? Sleep Med. 2013 doi: 10.1016/j.sleep.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 81.Kubota K., Shimazu A., Kawakami N., et al. Workaholism and sleep quality among Japanese employees: a prospective cohort study. Int J Behav Med. 2014 doi: 10.1007/s12529-012-9286-6. [DOI] [PubMed] [Google Scholar]
- 82.Loft M., Cameron L. The importance of sleep: relationships between sleep quality and work demands, the prioritization of sleep and pre-sleep arousal in day-time employees. Work Stress. 2014 doi: 10.1080/02678373.2014.935523. [DOI] [Google Scholar]
- 83.Czeisler M.É., Lane R.I., Petrosky E., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020 doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pollak C.P., Bright D. Caffeine consumption and weekly sleep patterns in us seventh-, eighth-, and ninth-graders. Pediatrics. 2003 doi: 10.1542/peds.111.1.42. [DOI] [PubMed] [Google Scholar]
- 85.Jaehne A., Loessl B., Bárkai Z., et al. Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev. 2009 doi: 10.1016/j.smrv.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 86.Ogeil R.P., Phillips J.G. Commonly used stimulants: sleep problems, dependence and psychological distress. Drug Alcohol Depend. 2015 doi: 10.1016/j.drugalcdep.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 87.Schierenbeck T., Riemann D., Berger M., et al. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Med Rev. 2008 doi: 10.1016/j.smrv.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 88.Ravens-Sieberer U., Kaman A., Erhart M., et al. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatr. 2021 doi: 10.1007/s00787-021-01726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Faisal R.A., Jobe M.C., Ahmed O., et al. Mental health status, anxiety, and depression levels of Bangladeshi university students during the COVID-19 pandemic. Int J Ment Health Addict. 2021 doi: 10.1007/s11469-020-00458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1