Abstract
Objective
Medical education experienced widespread disruption during the first peak of the COVID-19 pandemic. In response, members of the Society of Pediatric Cardiology Training Program Directors (SPCTPD) created a series of live, Zoom-based lectures for pediatric cardiology fellows. The goals were to support fellow didactic education and connect fellows and faculty during the pandemic. We sought to determine the impact of the lecture series on pediatric cardiology fellows around the country.
Methods
Pediatric cardiology experts from across the country volunteered to give lectures in the Pediatric Cardiology National Education Series (PC-NES). Lectures were held online once or twice weekly for 3 months during Spring 2020, while many fellows had modified clinical responsibilities. Fellows voluntarily completed an online survey before and after the lecture series.
Results
On the initial survey, a majority of fellows responded they would benefit from more didactic education while their training was impacted by COVID-19. After the series concluded, almost all (95%) fellows responded that PC-NES lectures were valuable supplements to their training during COVID-19. They included quality of lectures, board-relevance, and a way to connect to the pediatric cardiology community as key reasons for participating in PC-NES, and 100% responded they felt PC-NES should continue in some capacity.
Conclusion
The PC-NES was a low-cost, simple way to deliver high-quality supplemental education to pediatric cardiology fellows, help trainees build a network of peers and learn from experts outside their home institution. Similar models could connect other pediatric trainees at local, regional, or national levels, and provide valuable supplemental education opportunities.
Keywords: Medical education, COVID-19, Pediatric cardiology training
1. Introduction
The COVID-19 pandemic has presented many challenges to the medical community within and beyond the scope of patient care. Among these challenges, medical education has experienced widespread disruption including limiting trainee participation to adhere to physical distancing requirements, redeploying trainees to support patient care demands, canceling or postponing educational conferences and meetings, and restructuring program-specific didactic education. Nationwide, across all medical specialties, trainee education has had to adapt to this changing landscape. Additionally, these disruptions isolated many trainees from their peers and mentors during a time of personal and professional stress [1,2].
Providing high-quality educational opportunities for trainees during a global crisis required rapid collaboration among educators and a commitment to finding alternative educational methods. Little data exist to date that objectively describes the impact of the pandemic on trainee education, however, many commentaries acknowledge challenges for training physicians [[3], [4], [5], [6], [7], [8]]. In one survey of pediatric gastroenterology fellowship program directors, 90% reported that they were under a “stay-at-home” order for a median of 4 weeks at the time of the survey and fellows stopped participating in outpatient clinic in 43% of programs [3]. Changes to inpatient care included reduced fellow staffing, limiting who entered patient rooms, and rounding remotely [3,6,7]. Fellows in three New York programs were deployed to adult medicine units, and didactics were moved to virtual conferences in 94% of programs [3]. Clinical research and, disproportionately, bench research were restricted [3]. As a direct result of these changing responsibilities, medical educators across specialties sought alternative methods to support trainee education [[4], [5], [6], [7], [8]].
The Society of Pediatric Cardiology Training Program Directors (SPCTPD) comprises all fellowship directors for the 63 ACGME-accredited categorical pediatric cardiology training programs. Through this organization, several program directors created a series of live, web-based lectures for pediatric cardiology fellows and titled the series the Pediatric Cardiology – National Education Series (PC-NES). The goals of PC-NES were to support fellow didactic education and connect fellows and faculty during the pandemic. Across the country, pediatric cardiology faculty volunteered to share their expertise and hosted live one-hour lectures which were also recorded for trainees unable to participate in real-time. We sought to determine the impact of the PC-NES series on pediatric cardiology fellows around the country.
2. Methods
Once the idea for the PC-NES was established in mid-March 2020, faculty around the country were emailed and asked to contribute their expertise. Within days, pediatric cardiology experts from across the country volunteered to give lectures covering a diverse range of high-yield, board-relevant topics in pediatric cardiology. Before the first lecture, pediatric cardiology program directors were emailed a brief survey to distribute to their fellows, to better understand fellows' didactic education structure before COVID-19, personal feelings of connection to the pediatric cardiology community, and the impact COVID-19 had on fellow training and didactic education. The survey was also made available immediately before the first lecture to all active lecture participants and then closed 15 minutes after the first lecture began. An Institutional Review Board waiver was granted for this activity.
In April and May 2020, while many fellows had modified clinical responsibilities, PC-NES lectures were held twice weekly. Meetings were held via the web-based application Zoom, allowing participants to view the lecturer's slides, share their own video, and communicate with moderators via an online messaging application built into the program. Fellowship directors were encouraged to remind their fellows about the series, and the Zoom link was made available on the SPCTPD website. Faculty speakers were given guidance on optimizing the sessions for a virtual environment, including discrete learning objectives posted ahead of time and use of the “poll” function of Zoom, which allowed participants to answer multiple-choice questions in real-time and thereby promoted active participation during lectures. Most faculty opted to use this poll function to include board-style questions into their presentations, which encouraged active learning, participation, and reinforced key concepts. Fellows and faculty attending the lectures were encouraged to share their video to create a greater sense of community. A brief session evaluation was administered to participants after each lecture to provide feedback to the PC-NES organizers and lecturing faculty. After the first month, participating fellows were also asked for suggestions for lecture topics. Lectures covered general cardiology and physical examination, hemodynamics and interventional cardiology, echocardiography and advanced cardiac imaging, anatomy and physiology, electrophysiology, fetal cardiology, and adult congenital heart disease.
By June 2020, many fellows and faculty returned to clinical duties and PC-NES lecture frequency was decreased to once weekly to accommodate increasing clinical responsibility. The lecture series concluded on June 30, 2020, at the end of the academic year. A follow-up survey was distributed to pediatric cardiology program directors via email, and a survey link was shared following the final lectures of the series to assess fellows' satisfaction and the value of PC-NES. Fellows were asked about their satisfaction with the PC-NES lectures, their perceived impact of COVID-19 on their fellowship training, and their personal feelings of connection to the pediatric cardiology community. Demographic information including training year, region of training, and fellowship program size were also collected for both surveys.
3. Results
Twenty-two lectures occurred with faculty representation from seventeen pediatric cardiac centers with a broad geographical variety. Due to the overwhelming amount of faculty interest, some faculty could not be accommodated. Lectures were assigned according to area of expertise and interest. A total of 144 pediatric cardiology fellows completed the initial PC-NES survey. Participants were distributed evenly by training year and came from programs of varying sizes around the country (Table 1 ). Among respondents, 72% (103/144) reported their fellowship program was offering about the same or more dedicated teaching and 70% (101/144) responded the quality of their lectures at their home institutions was about the same as before the start of pandemic. Eighty-nine percent (128/144) responded that they agreed or strongly agreed that they would benefit from more didactic education while their training was impacted by COVID-19. Sixty-two percent (89/144) responded that they agreed or strongly agreed they felt personally connected to the pediatric cardiology community.
Table 1.
Demographics of survey respondents.
| Initial PC-NES survey (n = 144) | % | Follow-Up PC-NES survey n = 130 | % | |
|---|---|---|---|---|
| Training year | ||||
| PGY-4 | 40 | 27.78 | 52 | 40 |
| PGY-5 | 41 | 28.47 | 34 | 26.15 |
| PGY-6 | 41 | 28.47 | 38 | 29.23 |
| PGY-7 | 16 | 11.11 | 5 | 3.85 |
| Other | 6 | 4.17 | 1 | 0.77 |
| Geographic locationa | ||||
| Northeast | 31 | 23.85 | ||
| Mid-Atlantic | 8 | 6.15 | ||
| Southeast | 20 | 15.38 | ||
| Midwest | 40 | 30.77 | ||
| Rocky Mountain | 7 | 5.38 | ||
| Southwest | 7 | 5.38 | ||
| West Coast | 17 | 13.08 | ||
| Number of categorical fellows | ||||
| <5 | 29 | 20.14 | 23 | 17.83 |
| 6–11 | 86 | 59.72 | 65 | 50.39 |
| 12–17 | 12 | 8.33 | 18 | 13.95 |
| >18 | 17 | 11.81 | 23 | 17.83 |
Location of fellowship was not asked on the initial survey.
The follow-up PC-NES survey at the end of the series had 130 respondents. Demographics of fellows completing the follow-up survey were similar to those of respondents in the initial survey (Table 1). There were significantly more first year fellows who answered the second survey and fewer 4th year fellows.
Ninety-five percent (112/118) of fellows responded that PC-NES lectures are valuable supplements to their training during COVID-19. They listed quality of lectures, board-relevance, and a way to connect to the pediatric cardiology community as key reasons for participating in PC-NES (Fig. 1 ). Interestingly, while 69% of respondents chose “[PC-NES] makes me feel connected to the pediatric cardiology community” when asked about reasons for participating in the lecture series, the percentage of fellows who responded “Agree” or “Strongly Agree” to the question, “As a pediatric cardiology fellow, I feel personally connected to the pediatric cardiology community,” decreased from 62% to 52% from the initial to follow up surveys.
Fig. 1.
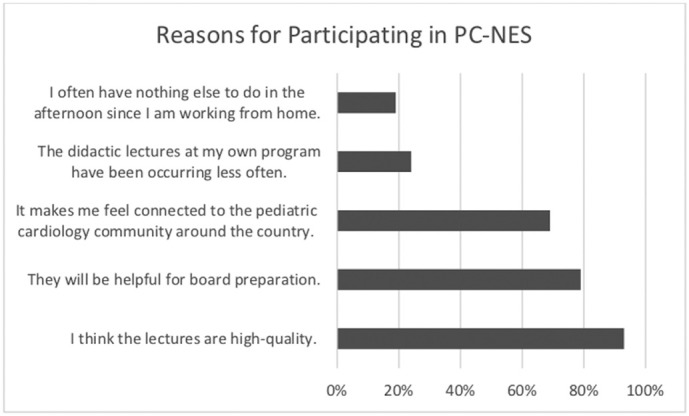
Fellow identified reasons for participating in PC-NES.
A majority of fellows (63%) responded that they continued to watch lectures live, even once lectures were recorded and available on the SPCTPD website. Almost 60% of respondents attended or accessed at least 5 PC-NES lectures and 18% responded that they attended 12 or more lectures. After the final PC-NES lecture, 100% of fellows responded that they felt PC-NES should continue in some capacity, with 92% expressing interest in continuing either once or twice per month.
4. Discussion
The PC-NES lecture series was a rapid and successful response to the impact that the COVID-19 pandemic had on pediatric cardiology fellow education in April–June 2020. As social-distancing recommendations became the norm at many medical institutions, the medical education community scrambled to find solutions to providing high-quality education to trainees whose clinical and didactic experiences were affected by the pandemic. Web-based teaching is accepted as a valuable supplement to traditional methods because it allows for asynchronous education at a distance and encourages self-directed learning [4]; and the PC-NES was a practical solution to supplement pediatric cardiology education at a national level.
Experts in their fields from across the country volunteered to provide high-quality lectures to fellows on a national scale, relieving some pressure for individual institutions to supplement trainee education if fellows were removed from clinical responsibilities and in-person education. This format also allowed fellows to interact with leaders in the pediatric cardiology community in a relatively intimate environment, dedicated to their education. The Zoom platform made lectures more interactive and flexible than what would have been possible through standard webinars or pre-recorded lectures. Additionally, fellows at some institutions received lectures on specific topics they may not have exposure to at their home institutions.
Through the network of the SPCTPD, PC-NES organizers were able to share information and scheduling details without extensive advertising or frequently emailing fellows, which also kept the lectures limited to the pediatric cardiology trainee community. This allowed for focused lectures tailored to board-relevant topics for fellows. Involving faculty from across the country ensured a wide geographical distribution of lecturers and participants and the commitment to connecting participants during an unprecedented time in medical education.
Determining dates and times for lectures that could accommodate schedules for as many trainees as possible was one of the most challenging barriers to developing the PC-NES. Navigating time zones, clinical duties, and predetermined didactic education schedules prohibited some trainees from participating in PC-NES in real time. These barriers likely explain the discrepancy between the lower number of West Coast and Southwest participants when compared to the East Coast and Midwest participants. Once the schedule was created, however, there was minimal administrative time necessary. The option to view recorded lectures allowed fellows the flexibility to participate in lectures as schedules allowed, however, the notable drop in live participation in later months, presumably due to fellows returning to clinical responsibilities, may be a barrier to faculty volunteering to participate in the future (Fig. 2 ). Additionally, survey respondents were likely participants in the PC-NES lectures, creating a selection bias for survey responses.
Fig. 2.
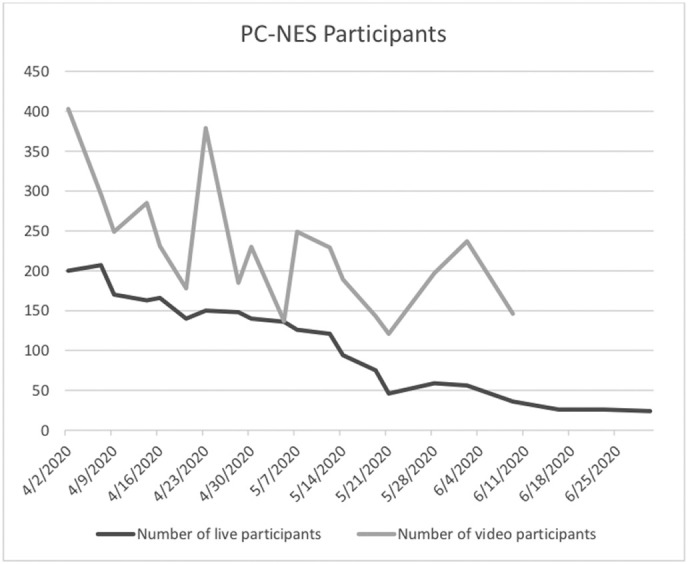
Number of viewers of live and recorded lectures for each presentation. June lectures were not available online at the time of this data collection.
The PC-NES lecture series had another benefit – bringing the community of pediatric cardiology fellows together during a time of uncertainty and stress in the medical community. On the follow up survey, fellows responded that their sense of connection to the pediatric cardiology community decreased from the start of the series to the end. This effect is likely multifactorial, including time away from clinical responsibilities, conferences moving to virtual platforms, missed networking opportunities, etc.; however, fellows' overwhelming approval of the lecture series and consistent participation, both live and through recorded videos, suggests their satisfaction with the program.
5. Conclusion
The COVID-19 pandemic is an unprecedented situation in the modern graduate medical education era, requiring adaptation to trainee education across all specialties. The PC-NES was a low-cost, relatively simple way to deliver high-quality supplemental education to pediatric cardiology fellows at a national level. While the schedule availability of fellows and faculty that occurred during the height of the pandemic may not be reproducible again, the concept of providing lectures on a larger scale could benefit other pediatric and pediatric subspecialty training programs. The feasibility of and fellow satisfaction with PC-NES also suggests that there is potential to build community among fellows through shared education. Currently, fellows have limited opportunities to interact with other trainees outside their home institutions. Regional sessions would have the additional benefits of encouraging more active fellow participation due to smaller group size, maximizing attendance as scheduling would not need to span several time zones, and promoting networking and community across fellowship programs whose hospitals may even be competitors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
This study was granted a waiver from the Institutional Review Board at Advocate Children's Hospital.
Informed consent
Consent was obtained from all individual participants included in the study.
CRediT authorship contribution statement
Drs Gandhi and Frank conceptualized and designed the study, coordinated and supervised data collection, and reviewed and revised the manuscript.
Dr. Weld drafted the data collection instruments, collected data, carried out the initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.ACGME Resident/Fellow Education and Training Considerations related to Coronavirus (COVID-19) Accreditation Council for Graduate Medical Education. 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10085/ACGME-Resident-Fellow-Education-and-Training-Considerations-related-to-Coronavirus-COVID-19 Published March 13.
- 2.American Board of Medical Specialties Statement Regarding Continuing Certification During COVID-19 American Board of Medical Specialties. 2020. https://www.abms.org/news-events/abms-statement-regarding-continuing-certification-during-covid-19/ Published March 26.
- 3.Mallon D., Pohl J.F., Phatak U.P., et al. Impact of COVID-19 on pediatric gastroenterology fellow training in North America. J Pediatr Gastroenterol Nutr. 2020;71(1):6–11. doi: 10.1097/MPG.0000000000002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiel L., Winthrop Z., Winn A.S. The COVID-19 pandemic and pediatric graduate medical education. Pediatrics. 2020;146(2) doi: 10.1542/peds.2020-1057. [DOI] [PubMed] [Google Scholar]
- 5.Rabinowitz D.G., Sundheim K.M. Trainee-directed educational pursuits and advocacy during the COVID-19 pandemic. Pediatrics. 2020;146(3):e20201564. doi: 10.1542/peds.2020-1564. [DOI] [PubMed] [Google Scholar]
- 6.Sabharwal S., Ficke J.R., LaPorte D.M. How we do it: modified residency programming and adoption of remote didactic curriculum during the COVID-19 pandemic. J Surg Educ. 2020 Sep-Oct;77(5):1033–1036. doi: 10.1016/j.jsurg.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bambakidis N.C., Tomei K.L. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020 Apr;17:1–2. doi: 10.3171/2020.3.JNS20965. [Epub ahead of print. PMID: 32302990; PMCID: PMC7164320] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bloom D.A., Reid J.R., Cassady C.I. Education in the time of COVID-19. Pediatr Radiol. 2020;50:1055–1058. doi: 10.1007/s00247-020-04728-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


