Abstract
The pandemic has affected children's behaviors and this fact has an effect on their healthy habits, such as sleep and diet. The aim of the current study was to determinate the prevalence of sleep-related problems and its relationship with eating habits in children from the south of Brazil during the pandemic.
Parents/legal guardians of 3–17 years old participants responded to a online survey distributed using the snowball sampling strategy in Brazil. The survey was conducted in April, 2020. Participants were asked for their sleep duration and sleep-related problems, as well as for their eating habits. Logistic regressions were performed to analyze the relationship between sleep-related problems and eating habits.
495 participants were included in the analysis. 48.8% of participants reported sleep-related problems with 12.3% not meeting the sleep guidelines. Moreover, participants reported eating fruits or vegetables and sweets over four and three per week, respectively. Different associations were found between varibles of sleep and eating habits.
Those participants with healthy eating habits showed a lower prevalence of sleep-related problems.
Keywords: Nutrition, Children, Adolescents, Brazil, Pandemic
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has originated a worldwide crisis, changing the daily routines and schedules of billions of people. Families are facing many pandemic-related changes, staying at home following government recommendations [1]. This fact has affected children's movement behaviours and probably other behaviours too [2], such as eating behaviors or sleeping patterns [3]. In this regard, the overall percentage of sleep complaints and sleep problems in both children and adolescents is very high, reaching around 80% in certain parts of the world [4]. The lack of sleep and unbalanced sleep habits increase the risk of health problems and mental disorders since adequate sleep is a critical determinant supporting healthy development in the young population [5,6]. Moreover, eating habits have been shown to affect sleep, by both the type of nutrients and the timing when they were ingested, concerning sleeping time [7]. Both sleep and eating habits are regulated by a complex interaction of neurotransmitter systems in the brain. While wakefulness is principally stimulated by neurons in the upper brainstem, posterior hypothalamus, and basal forebrain that release neurotransmitters (ie serotonin, dopamine); the inhibition and preservation of sleep are associated with neurotransmitters (ie acetylcholine, γ-aminobutyric acid (GABA)), for instance, from the anterior hypothalamus and the pons [8]. At the same time, neurotransmitters such as serotonin or dopamine, exert a crucial role in stimulating appetite, mood, motivation, reward, as well as food consumption [9], highlighting that regulating one system could affect the other systems.
Studies performed in children and adolescents have reported that insufficient sleep duration diminishes the quality of the diet. For instance, [10] in one systematic review found an inverse relationship between lower sleep duration in children and unhealthy dietary habits, especially with a higher intake of energy-dense food (eg, soda, snacks), and a lower intake of vegetables and fruits. Also, one study performed in Italian adolescents showed that participants with shorter sleep duration are more likely to eat fewer fruits and vegetables and eating out more frequently [11]. Similarly, scientific literature has pointed out that some eating habits such as eating in front of the TV, eating without the family, or eating fast-food have been linked to an inadequate quality diet as well as a higher stress level, a recognized factor of youths’ sleep quality [12,13]. Another important role in the relationship between sleep duration and eating habits is apparently attributed to certain adipokines. Thus, it has been pointed out the influence of sleep on the higher circulating levels of some adipokines (eg both leptin) [14]. Conversely, healthy eating habits have been linked to lower levels of adipokines (eg leptin) in children [15].
In this line, one study performed during COVID-19 lockdown has suggested that young adults experienced considerable adverse psychosocial changes during the COVID-19 lockdown, such as mental health problems [16] or, even, eating disorders [17]. These problems have been also reported in children (eg, insomnia) [18]. Notwithstanding, studies coping with this problem among the young population are scarce. To the best of our knowledge, this is the first study that assessed the relationship between sleep disorders and healthy eating habits during the COVID-19 lockdown. Thus, the aim of the present study was twofold: 1) to determine the prevalence of sleep-related problems during the COVID-19 lockdown, and 2) to explore the relationship with eating habits in the Brazilian young population.
2. Methods
2.1. Study design and population
This research was conducted following the Helsinki Declaration for Human Studies and approved by the Ethical Committee of the Universidade Tecnológica do Paraná (UTFPR) (CAAE: 32023220.8.0000.5547; approval number: 4.275.232). All participants were informed of the study's aims and a written informed consent was collected from participants and their parents/legal guardians.
Parents/legal guardians of pre-schoolers/children/adolescents aged 3–17 years were elegible to be enrolled through social networks. An online survey was generated and sent using a snowball sampling strategy. Around 15 min were needed to fulfill the online survey. Missing data were excluded in this study. Before starting, data about the study's aims were explained and informed consent was required. Data were collected between 14th and 28th April 2020, as the lockdown had begun in many parts of Brazil. In this phase, the epidemiological situation in Brazil presented 61,888 confirmed cases and 4205 deaths [19]. Of the first 544 south Brazilian respondents, 19 participants were excluded because they were <3 years old or >17 years old. Moreover, 30 participants were excluded because they presented missing values. Finally, data from 495 respondents were included in the final analysis.
2.2. Procedures
2.2.1. General information
Participants were asked to complete the survey in case they had been isolated during the previous week. The first part of the questionnaire presented general information on the COVID-19 lockdown scenario during the previous week. Also parents were asked for information about the sex and age of their children, educational level, and socioeconomic status (by the Family Affluence Scale – FAS-III [20]). Similarly, anthropometric information was reported by parents/legal guardians about their children. Weight was self-reported in kilograms and height in meters. Both the z-score for body mass index (BMI) and the classification of overweight/obesity were computed following the WHO criteria [21,22].
2.2.2. Sleep duration
The following question was used to ask parents/legal guardians for their children's sleep duration as the average of sleep time each night: “How long does your child sleep generally during the COVID-19 lockdown?” According to the guidelines of the National Sleep Foundation [23], young people who slept less/more than 8–10 h (14–17 years old) 9–11 h (5–13 years old) and 10–13h (3–4 years old), respectively [23], are considered to be in non-compliance with the sleep guidelines.
2.2.3. Sleep-related problems
The BEARS (Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, and Sleep-disordered breathing) sleep screening [24] was used in the present study. This screening tool was designed to screen the most common sleep problems in preschoolers (2–5 years) and children (6–12 years) and adolescents (13–18 years). Participants’ sleep-related problems were reported by parents/legal guardians. This tool could assist in the early detection of sleep-related problems since it is an easy-to-apply questionnaire which has presented good performance [25].
2.2.4. Eating habits
The eating habits were assessed by the Food Frequency Survey of the National System of Food and Nutrition Security (SISVAN, Sistema Nacional de Segurança Alimentar e Nutricional) [26], which aims to identify healthy (having breakfast, having lunch/dinner with parents, eating vegetables, foods, beans) and unhealthy dietary habits (having lunch/dinner watching TV, consumption of fried-food, sweets, fast-food, beverages) using indicators of food consumptions.
2.2.5. Covariates
Age, sex (females/males), educational level (incomplete primary education, complete primary education, incomplete secondary education, complete secondary education, incomplete higher education, or complete higher education), socioeconomic status (high, medium, or low) [20] and BMI (z-score) [21,22] were included as potential covariates. The choice of these covariates was made following the potential correlates indicated in the scientific literature [27].
2.3. Statistical analysis
Data were shown as means (standard deviation) for continuous variables and numbers (percentages) for categorical variables. The association between variables was determined by the point biserial correlation coefficient (rpb), which is a correlation coefficient applied when one variable (eg, sleep-related problems) is dichotomous. The rpb is equal to the Pearson's correlation from a mathematical point of view, that is, when we have one continuous variable “x” and a dichotomous variable “y”, rxy = rpb. Finally, both univariate and multivariate logistic regression analyses were performed to verify the association between healthy eating habits (predictors) and different sleep disorders (dependent variable). In the case of multivariate analyses, stepwise Ward's method was applied. Age, sex, educational level, socioeconomic status, and BMI z-score were included as potential covariates. All analyses were performed with SPSS statistical software. The level of statistical significance was set at p < 0.05.
3. Results
Table 1 shows the characteristic of the study with 495 participants, being 44.4% females. The mean age was 10.7 (4.3) and most of the analyzed sample were children (47.7%). Similarly, the prevalence of the sum of overweight and obesity was 43.6%. For sleep, 48.8% of participants reported certain sleep disorder and 12.3% did not meet the sleep guidelines. The average of days per week having lunch/dinner with parents and having breakfast was over 5. The average number of days eating fruits and vegetables was over four and participants reported an average of 3 days consuming sweets.
Table 1.
Characteristic of the study participants (n = 495).
| Variables | M (SD)/n (%) | 95% CI |
|---|---|---|
| Age | 10.7 (4.3) | 9.8–11.6 |
| Age group | ||
| Pre-schoolers | 71 (14.3) | 11.3–17.4 |
| Children | 236 (47.7) | 43.3–52.1 |
| Adolescents | 188 (38.0) | 33.7–42.3 |
| Sex (%) | ||
| Females | 220 (44.4) | 40.1 48.8 |
| Males | 275 (55.6) | 51.2 59.9 |
| Breadwinner's educational level (%) | ||
| Incomplete primary | 28 (5.7) | 3.6–7.7 |
| Complete primary education | 6 (1.2) | 0.2–2.2 |
| Incomplete secondary education | 43 (8.7) | 6.2–11.2 |
| Complete secondary education | 27 (5.5) | 3.5–7.5 |
| Incomplete higher education | 40 (8.1) | 7.3–12.5 |
| Complete higher education | 351 (70.9) | 66.9–74.9 |
| Socioeconomic statusa (%) | ||
| Low | 201 (40.6) | 36.3–44.9 |
| Medium | 221 (44.6) | 40.3–49.0 |
| High | 73 (14.7) | 11.6–17.9 |
| Anthropometric data | ||
| Height (cm) | 148.4 (25.1) | 135.3–161.5 |
| Weight (kg) | 46.18 (20.40) | 42.11–50.25 |
| BMI (z-score) | 0.91 (1.84) | 0.83–0.99 |
| Prevalence of Overweight/Obesityb (%) | 216 (43.6) | 39.3–48.0 |
| Sleep disorders (%) | ||
| Prevalence of bedtime problems | 88 (17.8) | 14.4–21.1 |
| Prevalence of excessive day sleepiness | 120 (24.2) | 20.5–28.0 |
| Prevalence of awakenings during the night | 42 (8.5) | 6.0–10.9 |
| Prevalence of nightmares | 45 (9.1) | 6.6–11.6 |
| Prevalence of problems related to regularity and duration of sleep | 116 (23.4) | 19.7–27.2 |
| Prevalence of sleep-disordered breathing | 72 (14.5) | 11.4–17.7 |
| Prevalence of reported at least one sleep-related problem | 241 (48.7) | 44.3–53.1 |
| Sleep duration | ||
| Daily sleep (hours) | 9.84 (1.34) | 9.24–10.44 |
| Prevalence of non-meeting of the sleep guidelines (%) | 61 (12.3) | 9.0–10.7 |
| Eating healthy habits (days/weekly) | ||
| Lunch/dinner with parents | 5.7 (2.3) | 5.2–6.2 |
| Breakfast | 5.3 (2.4) | 4.8–5.8 |
| Lunch/dinner watching TV | 2.6 (2.6) | 2.4–2.8 |
| Fast-food | 0.7 (0.9) | 0.6–0.8 |
| Fruits | 4.5 (2.5) | 4.1–4.9 |
| Beans | 4.1 (2.2) | 3.7–4.5 |
| Vegetables | 4.2 (2.6) | 3.8–4.6 |
| Fried-food | 1.6 (1.5) | 1.5–1.7 |
| Sweets | 3.0 (2.2) | 2.7–3.3 |
| Beverages | 1.2 (1.6) | 1.1–1.3 |
Data expressed as numbers (n) and percentage (%) for categorical variables and mean (M) and standard deviation (SD) for continuous variables. BMI: body mass index. SES: socioeconomic status.
Socioeconomic status based on the Family Affluence Scale (FAS-III) [20].
Table 2 depicts the partial correlations between eating habits and the different sleep disorders, adjusted by several covariates. It is remarkable the inverse relationship between having breakfast and score and presenting any sleep disorders (r = −0.153 and r = −0.092, respectively). However, all of these correlations were low.
Table 2.
Association between eating healthy habits according to the sleep duration and sleep-related problems during COVID-19 lockdown.
| Item | Bedtime problems | Excessive day sleepiness | Awakenings during the night | Nightmares | Regularity and duration of sleep | Sleep-disordered breathing | Any sleep-related problem | Non-meeting of the sleep guidelines |
|---|---|---|---|---|---|---|---|---|
| Lunch/dinner with parents (days/weekly) | −0.063 | −0.099∗ | −0.110∗ | −0.117∗ | −0.089∗ | −0.065 | −0.082 | 0.037 |
| Breakfast (days/weekly) | −0.122∗ | −0.116∗ | −0.089∗ | −0.085 | −0.095∗ | −0.054 | −0.153∗∗ | −0.036 |
| Lunch/dinner watching TV (days/weekly) | −0.068 | −0.025 | −0.020 | −0.064 | −0.023 | 0.107∗ | −0.028 | −0.036 |
| Fast-food (days/weekly) | 0.039 | 0.088∗ | −0.058∗ | −0.003∗ | −0.005∗ | 0.037 | 0.023 | −0.088 |
| Fruits (days/weekly) | −0.102∗ | −0.054 | −0.076 | −0.096∗ | −0.090∗ | −0.022 | −0.092∗ | −0.040 |
| Beans (days/weekly) | −0.049 | −0.023 | −0.069 | −0.132∗ | 0.021 | −0.073 | −0.032 | 0.023 |
| Vegetables (days/weekly) | −0.021 | −0.126∗ | −0.080 | −0.158∗∗ | −0.090∗ | −0.029 | −0.082 | 0.050 |
| Fried-food (days/weekly) | 0.034 | −0.006 | −0.054 | −0.010 | −0.002 | 0.049 | 0.009 | −0.043 |
| Sweets (days/weekly) | 0.078 | 0.056 | −0.011 | −0.034 | 0.019 | 0.098∗ | 0.048 | 0.006 |
| Beverages (days/weekly) | 0.017 | −0.023 | 0.036 | 0.028 | 0.006 | 0.061 | −0.022 | 0.001 |
Data expressed as a point biserial correlation coefficient. Adjusted by sex, age, body mass index (z-score), socioeconomic status and educational level. ∗p < 0.05; ∗∗p < 0.001.
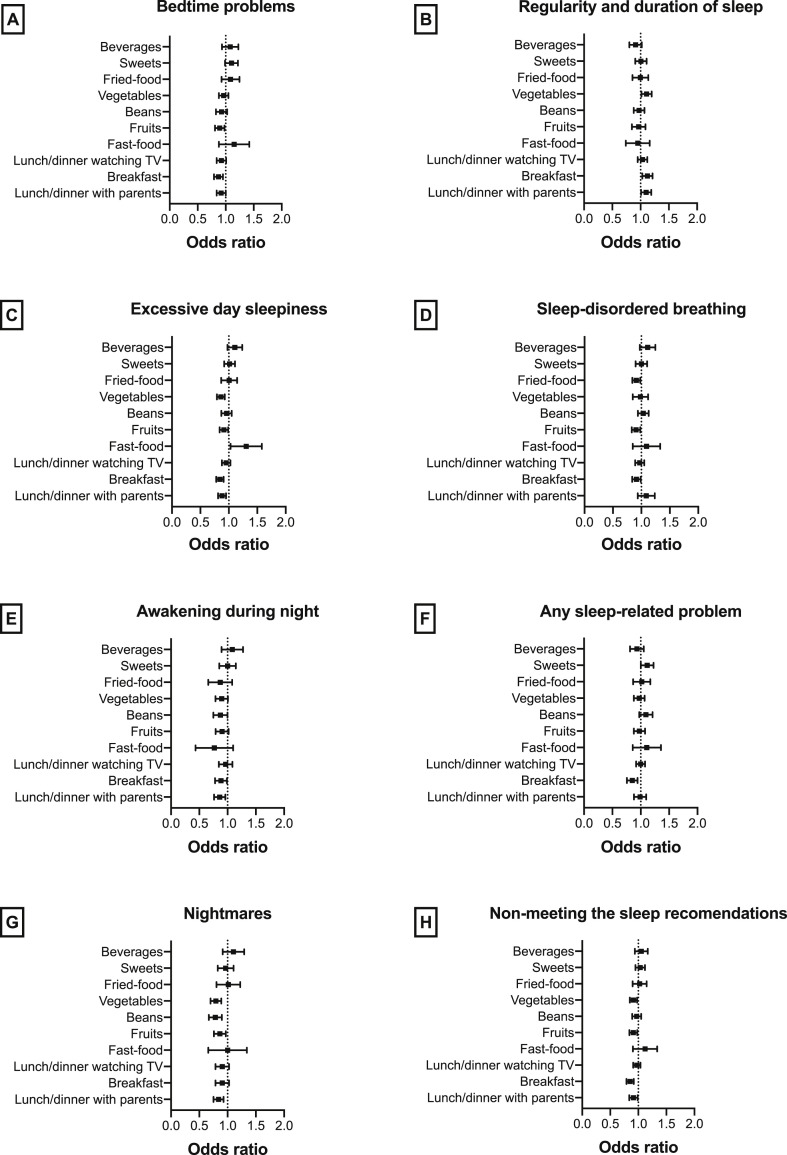
The associations between eating habits and the different sleep disorders in the univariate model are shown in Fig. 1 . Likewise, Table 3 indicates the final result of the multivariate model. Thus, eating less vegetables was associated with excessive daytime sleep (OR = 0.88; 95%CI = 0.79–0.98), nightmares (OR = 0.84; 95%CI = 0.73–0.97), regularity and duration of sleep (OR = 0.90; 95%CI = 0.82–1.00), as well as non-meeting the sleep guidelines (OR = 0.87; 95%CI = 0.77–0.99). Similarly, eat/lunch with parents was linked to awakenings during the night (OR = 0.87; 95%CI = 0.77–0.99). Moreover, less days of breakfast consumption was associated with bedtime problems (OR = 0.85; 95%CI = 0.77–0.94), excessive day sleepiness (0.88; 95%CI = 0.79–0.98), regularity and duration of sleep (OR = 0.89; 95%CI = 0.80–0.99) and any sleep-related problem (OR = 0.85; 95%CI = 0.78–0.92). Another finding was the association between eat beans less times and problems related to regularity and duration of sleep (OR = 0.88; 95%CI = 0.78–1.00). Conversely, eat/lunch watching TV was related to sleep-disordered breathing (OR = 1.15; 95%CI = 1.03–1.28). Finally, another eating habit that appeared inversely related to sleep disorders was sweet consumption; being so in the case of bedtime problems (OR = 1.16; 95%CI = 1.03–1.29) and any sleep-related problem (OR = 1.10; 95%CI = 1.00–1.20). This finding was also found between fast food intake times and excessive day sleepiness (OR = 1.30; 95%CI = 1.02–1.66).
Fig. 1.
Univariate single-level logistic regression analysis with eating healthy habits as independent variables and sleep-related problems as a dependent variable, among south Brazilian participants. A: Problems related to bedtime; B: Problems related to regularity and duration of sleep; C: Problems related to excessive day sleepiness; D: Problems related to sleep-disordered breathing; E: Problems related to awakening during night; F: Any problem related to sleep; G: Problems related to nightmares; H: Problems related to meeting the sleep recommendations.
Table 3.
Final result of the multilevel logistic regression analysis with potential eating healthy habits correlates as predictors and sleep-related problems as a dependent variable, among south Brazilian participants.
| Predictors | p | |
|---|---|---|
| Bedtime problems | ||
| Breakfast (days/weekly) | 0.85 (0.77–0.94) | 0.002 |
| Sweets (days/weekly) | 1.16 (1.03–1.29) | 0.011 |
| Excessive day sleepiness | ||
| Breakfast (days/weekly) | 0.88 (0.79–0.98) | 0.021 |
| Fast-food (days/weekly) | 1.30 (1.02–1.66) | 0.033 |
| Vegetables (days/weekly) | 0.88 (0.79–0.98) | 0.017 |
| Awakenings during the night | ||
| Lunch/dinner with parents (days/weekly) | 0.87 (0.77–0.99) | 0.032 |
| Nightmares | ||
| Vegetables (days/weekly) | 0.84 (0.73–0.97) | 0.019 |
| Regularity and duration of sleep | ||
| Breakfast (days/weekly) | 0.89 (0.80–0.99) | 0.036 |
| Beans (days/weekly) | 0.88 (0.78–1.00) | 0.044 |
| Vegetables (days/weekly) | 0.90 (0.82–1.00) | 0.050 |
| Sleep-disordered breathing | ||
| Lunch/dinner watching TV (days/weekly) | 1.15 (1.03–1.28) | 0.009 |
| Any sleep-related problem | ||
| Breakfast (days/weekly) | 0.85 (0.78–0.92) | <0.001 |
| Sweets (days/weekly) | 1.10 (1.00–1.20) | 0.044 |
| Non-meeting the sleep guidelinesa | ||
| Vegetables (days/weekly) | 0.87 (0.77–0.99) | 0.038 |
Data expressed as a odds ratio (95% confident intervals). Adjusted by sex, age, body mass index (z-score), socioeconomic status and educational level. Sleep-related problem selected as a reference group.
According to the guidelines of the National Sleep Foundation [23].
4. Discussion
This study aimed to determine the prevalence of sleep-related problems during the COVID-19 lockdown, as well as to explore the relationship with eating habits in young population from the South Region of Brazil. About half of the south Brazilian participants (48.8%) related suffering from sleep problems, especially excessive day sleepiness. Similarly, some of the eating behaviors analysed (higher vegetable and beans consumption, breakfast more often, eat/lunch more times with parents, and lower sweet consumption) were associated with a lower prevalence of sleep disorders during the COVID-19 lockdown in south Brazilian children and adolescents.
Scientific literature has pointed out that children and adolescents who sleep less are more likely to consume energy-rich foods, get higher proportions of calories from fats or refined carbohydrates, consume lower proportions of vegetables and fruits, and have more irregular meal patterns, and consume snacks more often than those sleeping more [28]. Our findings reveal that eating less times per week with parents or more times watching TV, having breakfast less frequently, lower weekly intakes of vegetables and beans, as well as greater consumption per week of sweets or fast-food were associated with some sleep-related problems during the COVID-19 lockdown. These results coincide with one study performed by Khan [29] who observed that Canadian children who frequently ate fast foods, ate in front of the TV or alone as opposed to around the table with family were more likely to have a sleep of poor quality. Also, skipping breakfast and eating irregularly has been strongly associated with poor sleep quality [30]. Some factors could explain, at least partially, these results. Firstly, due to the COVID-19 pandemic and the effects of atypical work schedules, it was recommended to keep a regular schedule for sleep, meals, work, and social contacts, since these activities are important time cues that help maintain the entrainment of one's biological clock [31]. Secondly, the scientific literature has suggested that food consumption (especially if it comes from energy-dense snacks and beverages) could increase during TV viewing which could extend the total energy intake and, consequently, in body weight gains; being known this hypothesis as a ‘mindless eating’ [32]. Likewise, sedentary behavior has been related to unhealthier dietary habits [33,34]. Thus, preliminary studies in adults indicate that the consumption of energy drinks can interfere with sleep and recent population-based studies suggest that consumption of energy drinks is increasing, especially in adolescents [35]. Another study performed by Sousa [36] among Brazilian adolescents showed that the fourth quartile of ultra-processed foods (eg sweets, beverages) was associated with a higher prevalence of poor sleep quality. Also, fast-food consumption (ie, energy-dense food) was associated with excessive day sleepiness. Similarly, high saturated fat and sugar intake are associated with lighter, less restorative sleep with more arousals [37].
Moreover, eating habits and sleep patterns are associated with mental well-being (eg depression) [38] and the COVID-19 pandemic has affected mental heatlh [39]. Therefore, the negative effects of the lockdown on emotional well-being could have affected eating behavior [40]. Nonetheless, mental health was not assessed in our study.
On the other hand, our results indicated that lower weekly consumption of beans had an unprotected effect on sleep disorders related to regularity and duration of sleep. Beans are tryptophan-rich foods which is an essential amino acid whereby its influence on sleep has been related to its role in the synthesis of the brain neurotransmitter serotonin (5-hydroxytryptamine) [5]. To exert this effect, this amino acid has to cross the blood–brain barrier where it is utilized to synthesize serotonin, which, in turn, gets converted into melatonin. Serotonin is the neurotransmitter that affects mood and appetite, as well as other processes in the body, while melatonin is the vital hormone to facilitating sleep [41].
In this line, our findings indicated the protective effect of higher intake of vegetables (rich in vitamins and fiber) in some sleep disorders, as well as in the non-meeting of the National Sleep Foundation guidelines during the COVID-19 lockdown. Supporting this notion, there is also substantial evidence concerning the influence of B-complex vitamins on sleep. For instance, vitamin B6 serves as a cofactor in the synthesis of serotonin from 5-hydroxytryptophan and thus indirectly affects the synthesis of melatonin [30]. Also, vitamin B9 (ie, folic acid) deficiency has been linked to insomnia and restless leg syndrome [42]. Similarly, low fiber intake is also associated with lighter, less restorative sleep with more arousals [37]. Moreover, a higher intake of fresh or minimally processed foods (eg vegetables) was a protective factor for poor sleep quality, whereas higher ultra-processed food consumption is a risk factor for poor sleep quality [36]. Also, certain micronutrient deficiencies have been linked to suboptimal hormonal regulation causing disrupted sleep, and also macronutrient imbalances have been reported, though not consistently, to affect sleep [28]. For the sleep guidelines, one study with data from NHANES (United States) showed that short sleepers, generally defined as those who sleep <7 h/night, consume a smaller variety of foods (including high-fiber foods such as vegetables) relative to normal sleepers who report 7–8 h of sleep/night [43].
The main limitation of the present study is represented by the self-reported questionnaire used, which may lead to the actual misreporting of data. However, our web-survey was similar to others that have been frequently employed [2,44]. Another limitation is that the use snowball sampling implies obtaining a non-probabilistic sample or possible correlations between network size and selection probabilities. Also, as mentioned previously, the pandemic has affected mental health and this could be responsible for changes in lifestyle habits but this was not assessed in the current study, therefore future studies with these variables are recommended. Conversely, a strength of our study was represented by the fact that the survey was conducted quickly in one of the most critical periods of the epidemic in Brazil, less than three weeks after the lockdown. Also, another strength is that, to the best of our knowledge, this is the first study in evaluating the eating habits among the young population during COVID-19 lockdown.
It has been hypoyhetized that during the lockdown scenario was likely to have had adverse consequences on many factors influencing sleep quality, as many people suffered major changes in their daily routines, lived with uncertainty and stress, insecurity about their health and concerns related to the situation and its duration [45]. Thus, our findings result meaningful from a public health perspective, since promoting healthy eating habits, could exert a protective effect in young populations against the development of sleep disorders; especially in future possible scenarios of lockdown. Supporting this notion, it seems to be necessary the development of intervention programs to prevent and/or treat the problems found in the analyzed sample with the aim of minimising the possible drawbacks that the lockdown has provoked, both in their quality of sleep and eating habits. In this sense, social and educational strategies focused on the most vulnerable population (pre-schoolers, children and adolescents) must be concentrated on not eating while spending time front screens, eating with parents/legal guardians, having breakfast (or trying to maintain a fixed routine with meals), increasing vegetables and beans intake, and diminishing fast-food and sweets consumption, to prevent the development of sleep disorders from an eating healthy perspective.
5. Conclusions
Almost half of the south Brazilian young population analyzed suffered from sleep disorders during the COVID-19 lockdown. The prevalence of sleep disorders was lower in those participants with some eating healthy habits. Further studies are required to elucidate the mechanism which could further explain the relationship between sleep disorders and eating healthy habits. Public health strategies are needed to advise the population about the importance of sleep, healthy sleep routines, and eating healthy habits to deal with the COVID-19 pandemic and prevent or diminish long-term adverse consequences.
Credit author statement
Formal analysis, J.F.L-G.; Investigation, J.F.L-G. and J.B–S.; Resources, J.F.L-G. and J.B–S.; Data curation, J.F.L-G.; Writing—original draft preparation, J.F.L-G., A.R.G., C.I.C., R.G.S., H.B.S.C. and J.B–S.; Writing—review and editing, J.F.L-G., A.R.G., C.P.R., C.I.C., R.G.S., H.B.S.C. and J.B–S.; Visualization, J.F.L-G., A.R.G., C.P.R. and J.B–S.; Supervision, A.R.G., and J.B–S.; Project administration, J.F.L-G. and J.B–S.; Funding acquisition, J.F.L-G. and J.B–S. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
None declared.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.07.003.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Riazi N.A., Wunderlich K., Gierc M., et al. “You can't go to the park, you can't go here, you can't go there”: exploring parental experiences of COVID-19 and its impact on their children's movement behaviours. Children. 2021;8:219. doi: 10.3390/children8030219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore S.A., Faulkner G., Rhodes R.E., et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Activ. 2020;17:85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodgers R.F., Lombardo C., Cerolini S., et al. The impact of the COVID -19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sadeh A., Mindell J., Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12:478–482. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Schneider N., Mutungi G., Cubero J. Diet and nutrients in the modulation of infant sleep: a review of the literature. Nutr Neurosci. 2018;21:151–161. doi: 10.1080/1028415X.2016.1258446. [DOI] [PubMed] [Google Scholar]
- 6.Owens J.A., Weiss M.R. Insufficient sleep in adolescents: causes and consequences. Minerva Pediatr. 2017;69:326–336. doi: 10.23736/S0026-4946.17.04914-3. [DOI] [PubMed] [Google Scholar]
- 7.Phillips F., Crisp A.H., Mcguinness B., et al. Isocaloric diet changes and electroencephalographic sleep. Lancet. 1975;306:723–725. doi: 10.1016/S0140-6736(75)90718-7. [DOI] [PubMed] [Google Scholar]
- 8.Preedy V.R., Patel V.B., Le L.-A., editors. Handbook of nutrition, diet and sleep. Human Health Handbooks No 3. Wageningen Academic Publishers; Netherlands: 2013. [Google Scholar]
- 9.Volkow N.D., Wang G.-J., Baler R.D. Reward, dopamine and the control of food intake: implications for obesity. Trends Cognit Sci. 2011;15:37–46. doi: 10.1016/j.tics.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Córdova F.V., Barja S., Brockmann P.E. Consequences of short sleep duration on the dietary intake in children: a systematic review and metanalysis. Sleep Med Rev. 2018;42:68–84. doi: 10.1016/j.smrv.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Ferranti R., Marventano S., Castellano S., et al. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci. 2016;9:117–122. doi: 10.1016/j.slsci.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale L., Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Börnhorst C., Wijnhoven T.M., Kunešová M., et al. WHO European Childhood Obesity Surveillance Initiative: associations between sleep duration, screen time and food consumption frequencies. BMC Publ Health. 2015;15:442. doi: 10.1186/s12889-015-1793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin J., Jiang Y., Wang G., et al. Associations of short sleep duration with appetite-regulating hormones and adipokines: a systematic review and meta-analysis. Obes Rev. 2020;21 doi: 10.1111/obr.13051. [DOI] [PubMed] [Google Scholar]
- 15.Duarte Junior Ma dos S., Gaya A.C.A., Lemes V.B., et al. Association between eating habits, body mass index, cardiorespiratory fitness, and cardiometabolic risk factors in children. Rev Nutr. 2021;34 doi: 10.1590/1678-9865202134e200116. [DOI] [Google Scholar]
- 16.Papandreou C., Arija V., Aretouli E., et al. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID -19 outbreak: cross-sectional analysis of two different confinement strategies. Eur Eat Disord Rev. 2020;28:836–846. doi: 10.1002/erv.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCombie C., Austin A., Dalton B., et al. “Now it's just old habits and misery”–understanding the impact of the covid-19 pandemic on people with current or life-time eating disorders: a qualitative study. Front Psychiatr. 2020;11:589225. doi: 10.3389/fpsyt.2020.589225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zreik G., Asraf K., Haimov I., et al. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. 2021;30 doi: 10.1111/jsr.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19): situation report - 99. Geneva, Switzerland. [Google Scholar]
- 20.Schnohr C.W., Makransky G., Kreiner S., et al. Item response drift in the family affluence Scale: a study on three consecutive surveys of the health behaviour in school-aged children (HBSC) survey. Measurement. 2013;46:3119–3126. doi: 10.1016/j.measurement.2013.06.016. [DOI] [Google Scholar]
- 21.Onis M., Onyango A.W., Borghi E., et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . WHO Press; Geneva: 2006. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age ; methods and development. [Google Scholar]
- 23.Hirshkowitz M., Whiton K., Albert S.M., et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Owens J.A., Dalzell V. Use of the ‘BEARS’ sleep screening tool in a pediatric residents' continuity clinic: a pilot study. Sleep Med. 2005;6:63–69. doi: 10.1016/j.sleep.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Nunes M.L., Bruni O. Insomnia in childhood and adolescence: clinical aspects, diagnosis, and therapeutic approach. J Pediatr. 2015;91:S26–S35. doi: 10.1016/j.jped.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Instituto Brasileiro de Geografia e Estatística . Instituto Brasileiro de Geografia e Estatística; Rio de Janeiro (Brazil): 2016. Pesquisa nacional de Saúde do escolar (PeNSE): 2015. [Google Scholar]
- 27.Rollo S., Antsygina O., Tremblay M.S. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. Journal of Sport and Health Science. 2020;9:493–510. doi: 10.1016/j.jshs.20220.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peuhkuri K., Sihvola N., Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32:309–319. doi: 10.1016/j.nutres.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Khan M.K.A., Faught E.L., Chu Y.L., et al. Is it nutrients, food items, diet quality or eating behaviours that are responsible for the association of children's diet with sleep? J Sleep Res. 2017;26:468–476. doi: 10.1111/jsr.12466. [DOI] [PubMed] [Google Scholar]
- 30.St-Onge M.-P., Mikic A., Pietrolungo C.E. Effects of diet on sleep quality. Advances in Nutrition. 2016;7:938–949. doi: 10.3945/an.116.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morin C.M., Carrier J., Bastien C., et al. Circadian Network Sleep and circadian rhythm in response to the COVID-19 pandemic. Can J Public Health. 2020;111:654–657. doi: 10.17269/s41997-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cleland V.J., Patterson K., Breslin M., et al. Longitudinal associations between TV viewing and BMI not explained by the ‘mindless eating’ or ‘physical activity displacement’ hypotheses among adults. BMC Publ Health. 2018;18:797. doi: 10.1186/s12889-018-5674-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carson V., Hunter S., Kuzik N., et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metabol. 2016;41:S240–S265. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- 34.García-Hermoso A., Ezzatvar Y., López-Gil J.F., et al. Is adherence to the Mediterranean Diet associated with healthy habits and physical fitness? A systematic review and meta-analysis including 565,421 youths. Br J Nutr. 2020:1–32. doi: 10.1017/S0007114520004894. [DOI] [PubMed] [Google Scholar]
- 35.Han E., Powell L.M. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet. 2013;113:43–53. doi: 10.1016/j.jand.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sousa da R.S., Bragança M.L.B.M., Oliveira de B.R., et al. Association between the degree of processing of consumed foods and sleep quality in adolescents. Nutrients. 2020;12:462. doi: 10.3390/nu12020462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.St-Onge M.-P., Roberts A., Shechter A., et al. Fiber and saturated fat are associated with sleep arousals and slow wave sleep. Journal of Clinical Sleep Medicine. 2016;12:19–24. doi: 10.5664/jcsm.5384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raboch J., Ptacek R., Vnukova M., et al. How does lifestyle affect depression? Eur Psychiatr. 2017;41:S539. doi: 10.1016/j.eurpsy.2017.01.745. S539. [DOI] [Google Scholar]
- 39.Osimo S.A., Aiello M., Gentili C., et al. The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front Psychol. 2021;12:630751. doi: 10.3389/fpsyg.2021.630751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cecchetto C., Aiello M., Gentili C., et al. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. 2021;160:105122. doi: 10.1016/j.appet.2021.105122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hartmann J.A., Wichers M., van Bemmel A.L., et al. The serotonin transporter 5-HTTLPR polymorphism in the association between sleep quality and affect. Eur Neuropsychopharmacol. 2014;24:1086–1090. doi: 10.1016/j.euroneuro.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 42.Kelly G.S. Folates: supplemental forms and therapeutic applications. Alternative Med Rev. 1998;3:208–220. [PubMed] [Google Scholar]
- 43.Grandner M.A., Jackson N., Gerstner J.R., et al. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 2013;64:71–80. doi: 10.1016/j.appet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guerrero M.D., Vanderloo L.M., Rhodes R.E., et al. Canadian children's and youth's adherence to the 24-h movement guidelines during the COVID-19 pandemic: a decision tree analysis. Journal of Sport and Health Science. 2020;9:313–321. doi: 10.1016/j.jshs.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Altena E., Baglioni C., Espie C.A., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1