Abstract
Purpose
To understand women’s perspectives, attitudes, and beliefs surrounding menopause transition and increase understanding of digital technology use for symptom management.
Patients and Methods
Information was obtained using three studies of women aged 40–65 years experiencing menopause transition symptoms. The HealthyWomen online cross-sectional survey was designed to reflect an inclusive sociodemographic sample representative of the US population. BECOME was a blinded, ethnographic, qualitative research study of women’s menopause transition experiences and comprised facilitator-led online asynchronous discussions, online homework entries, and audio-only teleconferences. The NODE.Health online, two-part, cross-sectional patient survey was designed to capture patient and healthcare provider (HCP) sentiment about the use of digital health technologies to address gaps in perimenopausal symptom knowledge and management.
Results
The HealthyWomen survey included 1045 participants, 37 were included in BECOME, and 100 completed the NODE.Health survey. Hot flashes, night sweats, and sleep problems were the most frequently experienced symptoms in the HealthyWomen survey, and over half of participants experiencing symptoms felt the need to seek relief. Whether menopause was considered a medical problem or natural process differed by self-identified race, culture, and ethnicity, as did the likelihood of consulting a HCP over symptoms. Participants preferred to discuss menopause transition with HCPs who did not rush them, were good listeners, and had expertise in the area. Most technology experience was with health websites, but nearly half were unsatisfied with online resources describing menopause-related symptoms. Convenience, ease of use, and accessibility were the most common reasons for pursuing digital health technology.
Conclusion
Factors such as cultural beliefs, values and attitudes towards menopause determine personal experiences. More open discussions with friends, family, and HCPs may raise awareness and reduce barriers to seeking help. To provide optimal care throughout the menopause transition, HCPs should consider patients’ psychosocial and cultural backgrounds, and personal and subjective perspectives.
Keywords: vasomotor symptoms, sleep disturbance, women’s health, weight gain, vaginal dryness, digital health
Introduction
Menopause is defined to have occurred after 12 consecutive months of amenorrhea.1 Most women (and people assigned female at birth) experience menopause between the ages of 45 and 54 years, with 51 years being the average age of the final menstrual period.2 Each individual experiences the menopause transition differently. Some experience this natural stage of life without symptoms, whereas others may have hot flashes, night sweats, sleep disturbances, fatigue, and/or vaginal or urinary changes, all of which can dramatically reduce the quality of life.2–4 In addition, these symptoms can have negative interpersonal and societal effects, disrupting relationships at home and in the workplace. Without adequate support, women at this stage of life may leave the workforce, resulting in a substantial impact on society owing to both direct and indirect financial costs and workplace inequality.5–11
Vasomotor symptoms (VMS), characterized by hot flashes (also called hot flushes) and/or night sweats, are the symptoms for which women most often seek treatment.12 In the United States (US), VMS are reported by about 60% to 80% of women during or after the menopausal transition.13–15 Furthermore, about 32% to 46% of peri- or postmenopausal women in the US report moderate-to-severe VMS.14,16 VMS associated with menopause persist for a median of 7.4 years.17 and can impact daily life, such that women with severe VMS report effects on sleep (94%), concentration (84%), mood (85%), energy (77%), and sexual activity (61%).6 Multiple factors, such as cultural norms, education, employment status, health status, stress, social status, and personal menopause knowledge, are likely to contribute to variability in the severity, duration, and perception of the importance of VMS.2
The multi-year Study of Women’s Health Across the Nation (SWAN) is an ongoing observational longitudinal study assessing differences in biological and psychosocial changes based on race and ethnicity in women who were enrolled prior to menopause.18 SWAN enrolled 3302 women in midlife across five racial and ethnic groups, with outcomes showing significant differences in the rate and magnitude of change in multiple health indicators.18,19 Black or African American women reported VMS more frequently than women who were White or of Hispanic/Latina descent, and Chinese and Japanese women were the least likely to report symptoms.19 In addition, the longest duration of VMS was reported by African American women (median 10.1 years).17 It is therefore vital that studies assessing impact of menopause consider the differences between racial and ethnic groups.
There is increasing recognition that the patient voice is integral to improving health. Patient experience surveys have been used to demonstrate a link between patient experience, knowledge of the condition, and clinical outcomes.20 Consequently, it is important to understand what information the patient has utilized when making healthcare decisions, and how new information is obtained.
We conducted three studies to understand women’s perspectives, attitudes, and beliefs surrounding menopause transition and assess how digital technology is being used to manage symptoms. The first study utilized data from HealthyWomen (HW), a not-for-profit organization which empowers women to take a proactive role in their health and that of their families. The second study, BECOME (Behaviors, Emotions and Concerns of women with perimenopause and Menopause and their real-life Experiences; conducted in partnership with Throughline Strategy), aimed to understand how symptomatology and access to healthcare and health technologies are shaped by race/ethnicity, socioeconomic status, and healthcare coverage. Finally, in partnership with NODE.Health (Network of Digital Evidence in Health) Foundation we conducted a cross-sectional survey that explored the attitudes, behaviors, and beliefs of perimenopausal women, as well as the drivers that encourage them to seek care. In addition, healthcare practitioners were asked about the challenges they face in addressing the needs of patients with menopause transition symptoms.
Materials and Methods
Study Designs
This paper reports results from three studies conducted by three different organizations that are separate from the authors’ affiliations. The studies were sponsored by Astellas Pharma Inc. (under contract) and the BECOME study was approved by the Astellas Ethics and Compliance committee. The studies were reviewed by the Advarra Institutional Review Board and qualified as IRB exempt. The e-consent process formed part of the protocols reviewed by the IRB. Data were collected anonymously and maintained confidentially. Participants in the BECOME study were provided with a pseudonym to protect privacy.
HealthyWomen
The HW study was an online cross-sectional survey of women with four objectives: 1) understand attitudes and beliefs related to menopause transition symptoms; 2) review beliefs related to specific treatment options for menopause transition and how these perceptions impact behaviors, including willingness to seek and initiate treatment; 3) gain information on how women with menopause transition symptoms utilize digital health and telehealth services; and 4) gain an understanding of how symptomatic women interact with their healthcare practitioners. All participants were required to provide informed e-consent before data collection. Participation in the study was voluntary and participants could withdraw their consent at any time.
The survey was available online for 5 weeks and designed to reflect an inclusive sociodemographic sample representative of the US population. Participants were recruited and verified by a market research agency (Dynata, Shelton, CT) using direct email and online marketing channels, including affiliate partners and targeted websites. The goal was to recruit 1000 participants assigned female at birth, aged 40–64 years, and experiencing hot flashes and night sweats. Individuals in the target age group not experiencing any menopause transition symptoms and those with amenorrhea for ≥7 years were excluded. The survey included 44 questions and was expected to take 15 minutes to complete (See Supplement for the HealthyWomen Survey Questions). All responses were reviewed and coded into themes; two designated team members then reviewed the coding.
BECOME
BECOME was a blinded, ethnographic, qualitative assessment of menopause transition experiences. It was conducted in four parts: A) facilitator-led online asynchronous discussions (with individual and group discussion questions); B) online homework entries; C) facilitator-led small-group discussions; and D) follow-up small group discussions; C and D took place through an audio-only teleconference platform over a 2-month study period. BECOME was developed and administered by Throughline Strategy (Toronto, Canada), an independent research company focused on improving health outcomes and experiences. Sessions were facilitated by an experienced moderator from Throughline Strategy and any quotes were derived from the discussions that aimed to gather additional context or encourage all participants to speak (See Supplement for BECOME Research Methods).
Participants were recruited through a global recruitment company (M3 Global Research, Fort Washington, PA, US). Study eligibility was determined based on responses to an email containing a screening questionnaire and those eligible were sent an invitation to the informed consent process (See Supplement for BECOME Study Details and BECOME Screening Questionnaire).
Eligible individuals self-identified as female, were aged 40–65 years, living in the US, and currently experiencing menopause transition symptoms defined as: irregularity of menses, hot flashes, and/or night sweats within the prior month, vaginal dryness, low sex drive, mood changes (including feelings of anxiety or depression), sleep disturbance (excluding insomnia), or weight gain. Women who had surgical menopause or worked in/had family working in advertising, marketing, public relations, the US Food and Drug Administration (FDA), or any media, healthcare, or pharmaceutical industries were excluded (See Supplement for BECOME Study Details).
Participants were categorized into six groups based on race/ethnicity (Black [n=9], Chinese American [n=5], Filipina American [n=5], Indian American [n=5], Latina [n=8], White [n=8]). Each group was required to include individuals from a range of socioeconomic backgrounds and mixed insurance coverage status. Each group had to meet requirements regarding the proportion of participants who A) were considered to be perimenopausal (60%) or postmenopausal (40%), B) had tried pharmacotherapy in the last 6 months (40%), C) had not tried pharmacotherapy but had used treatments not prescribed by a doctor (including home remedies, supplements, over the counter [OTC] therapies, alternative medicine, herbal remedies, or other activities) to manage symptoms (30%), and D) were defined as a “health technology super user” and had used more than one health technology more than once per week (20%) (See Supplement for full details of BECOME Group Requirements).
A qualitative analysis was conducted of notes and transcripts from the online asynchronous discussions, online homework, real-time small group meetings, and real-time small group follow-up meetings. Two coders reviewed the data, developed an initial set of codes, and identified emerging themes. The research team then discussed the emerging themes and the two coders developed an agreed codebook based on the emerging themes through negotiated consensus.21 One coder applied the codes to the data; the second coder reviewed the coded data. Any discrepancies were reviewed by the two coders; the codes were refined through further discussion and applied to the dataset. Codes were sorted into categories and themes that were refined and mapped to develop the broader theoretical framework.22
NODE.Health Survey
The NODE.Health survey was an online cross-sectional survey study that aimed to 1) explore the attitudes, behaviors, and beliefs of perimenopausal women and understand the drivers that encourage them to seek care; 2) understand how women with perimenopausal symptoms are using digital technology to manage their symptoms; and 3) understand the potential and current use of digital health technologies. Recruitment was done via online advertising on social media and posts in professional groups and societies, such as women’s health organizations, and potential participants completed a pre-screening tool (See Supplement for NODE.Health Screening Questionnaire). A small number of healthcare practitioners were recruited to discuss the challenges they face in addressing patients’ needs. Practitioners were recruited through NODE.Health’s extended physician researcher network.
The study was designed to recruit 100 participants who self-identified as female and were aged 40–64 years and experiencing perimenopausal symptoms. Perimenopausal symptoms were defined as: irregularity of menses, hot flashes (≥ 3 night sweats or hot flashes within the prior month), night sweats (≥ 2 night sweats within the prior month), vaginal dryness, low sex drive, mood changes (including feelings of anxiety or depression), sleep disturbance (excluding insomnia), and weight gain. Individuals without hot flashes or night sweats, and those who had not had a menstrual period in the past 12 months were excluded. The survey also requested responses from 15 healthcare practitioners.
An online verification identity platform was used to verify participant identity before participants submitted an online screener questionnaire and included their contact email addresses. Once submitted, a personal link to complete the 15-minute survey was sent to their email address. All participants provided informed e-consent. The patient survey was in two parts and available on a secure website for a period of 8 weeks (See Supplement for NODE.Health Part 1 and Part 2). A literature review did not identify any pre-existing, validated surveys covering the areas of interest. Therefore, three researchers with expertise in survey development iteratively developed the survey relating to perimenopausal experiences.23 No pretesting or cognitive interviews were conducted so respondents may have interpreted questions differently than intended.
Separately, 15 healthcare provider interviews were conducted to better understand diverse individual healthcare provider perspectives on treating women experiencing menopause (See NODE.Health Survey Healthcare Practitioners’ Experience Survey). Using an investigator-created interview guide, interviews with healthcare providers were led by a male physician with training in clinical research methods. Sessions were recorded and transcribed, and the interview findings synthesized according to common themes present.
Next, a focus group created by purposive sampling (broad range of healthcare provider types and geographies), consisting of 6 healthcare professionals (2 physicians from Obstetrics and Gynecology, 2 physicians from primary practice, and 2 physician assistants) was moderated by a male and female physician researcher to elicit themes related to symptom awareness, education, treatment, and the potential for technologies to assist women experiencing perimenopause.
Results
Participants
HealthyWomen
Overall, 1045 participants responded to the HW survey; 24% were aged 40–43 years, 54% 44–54 years, and 23% 55–64 years. Of the 900 participants who self-reported race, 7% responded Asian or Asian American, 14% Black or African American, and 74% White or Caucasian. When provided with definitions for perimenopause (menopause type symptoms but not lost menstrual period for 12 consecutive months) or menopause (not had menstrual period for 12 consecutive months), most (80%) classified themselves as meeting these criteria (43% perimenopausal; 37% menopausal), 7% responded neither, and 13% were unsure. Approximately 48% no longer experienced menses; 80% attributed this to natural menopause, 16% to surgery, and 4% responded that they did not know. Over half (55%) experienced a menstrual period < 12 months prior to completing the survey, 21% experienced their last menstrual period 12–36 months prior to the survey, and 23% 4–7 years previously. All 1045 participants reported having at least one episode of night sweats or hot flashes during the previous month.
BECOME
Thirty-seven participants were included in the BECOME study (Table 1), with 59% identifying as perimenopausal and 41% postmenopausal. A high proportion of participants (40%) had a bachelor’s degree, 33% had a graduate degree, 59% were married, 19% divorced, and 15% had never married. Participants were from a range of household income levels: < $50,000 (14%), $50,000–$74,999 (14%), $75,000–$99,999 (24%), $100,000–$149,999 (29%), and ≥ $150,000 (19%).
Table 1.
Group Characteristics in BECOME (n=37)
| Group | N | Perimenopausal, n (%) | Postmenopausal, n (%) | OTC Treatment Only, n (%) | Use Prescription Medication, n (%) | Health Technology Super Usera, n (%) |
|---|---|---|---|---|---|---|
| Black | 8 | 5 (62.5) | 3 (37.5) | 5 (62.5) | 1 (12.5) | 1 (12.5) |
| Chinese American | 5 | 3 (60.0) | 2 (40.0) | 3 (60.0) | 2 (40.0) | 1 (20.0) |
| Filipina American | 5 | 3 (60.0) | 2 (40.0) | 4 (80.0) | 1 (20.0) | 1 (20.0) |
| Indian American | 3 | 1 (33.3) | 2 (66.7) | 2 (66.7) | 1 (33.3) | 1 (33.3) |
| Latina or Hispanic | 9 | 6 (66.7) | 3 (33.3) | 7 (77.8) | 2 (22.2) | 2 (22.2) |
| White | 7 | 4 (57.1) | 3 (42.9) | 3 (42.9) | 4 (57.1) | 3 (42.9) |
| Overall | 37 | 22 (59.5) | 15 (40.5) | 24 (64.9) | 11 (29.7) | 9 (24.3) |
Note: aUsed more than one health technology more than once per week.
Abbreviation: OTC, over the counter.
NODE.Health Survey
One hundred participants were included in the NODE.Health study. Most were aged 45–54 years (72%), with 19% 40–44 years, 38% 45–49 years, 34% 50–54 years, and 9% aged 55–60 years. A majority self-identified as White (82%), 4% as Asian or Asian American, 10% as Black or African American, 2% as Hispanic, 2% as multi-racial, and 1% as “other”. Half the participants (51%) had perimenopausal symptom onset between 45–49 years of age, 24% between 40–44 years, and 18% between 50–54 years. Two-thirds (66%) had experienced perimenopausal symptoms for ≤ 2 years and 6% for > 5 years.
Fifteen healthcare practitioners completed virtual interviews. This cohort included physician assistants and nurse practitioners (n=5), physician specialists in obstetrics and gynecology (n=5), and primary care physicians (n=5). Seven worked in academic medical centers and eight in independent private practice and were located in the northeast (n=8), southeast (n=4), and west coast (n=3) of the US.
Awareness and Experience with Menopause Transition Symptoms
HealthyWomen
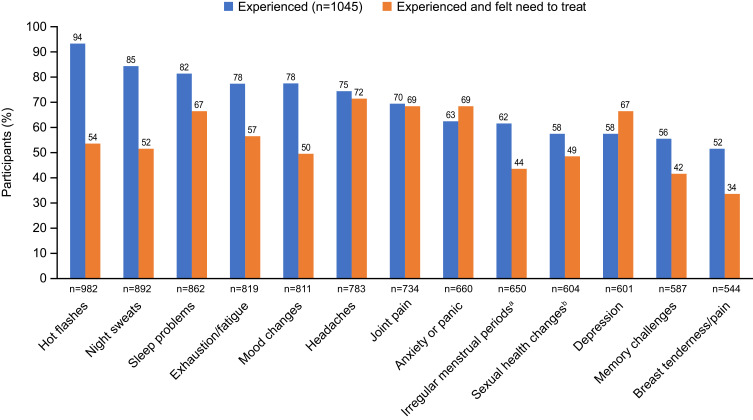
Hot flashes (94%), night sweats (85%), and sleep problems (83%) were the symptoms most frequently experienced by participants (Figure 1). While 19% reported < 1 hot flash or night sweat per day, 41% reported 1–3, 23% 4–6, 8% 7–9. and 7% ≥ 10 per day.
Figure 1.
Proportion of participants in the HealthyWomen survey who reported experiencing each symptom and the proportion experiencing each symptom who felt the need to get relief*.
Notes: *Note that the denominator is consistent for the initial question “Which of the following have you experienced?” (n=1045), but for the follow-up question, “For the ones you have experienced, from which have you felt you needed to try to get relief?”, the denominator varies accordingly. aMenstrual period different than it has been in terms of when it comes, how long it stays, or amount of bleeding; blow sex drive, dryness, pain during sex, or vaginal atrophy (thinning of tissue and muscle).
More than half the participants experiencing symptoms felt the need to seek relief (Figure 1). The time from symptom initiation to action to get relief (n=932) was < 1 year (34%), 1–2 years (25%), and > 5 years (1%), while 32% had never sought care. When asked what would have influenced them to seek care earlier, 32% responded knowing what are considered “normal” symptoms of menopause, 29% stated awareness that their symptoms were worse than what would be considered “normal”, 28% specified awareness of how long symptoms may last, and 25% responded more awareness of treatment options.
Participants who did not feel the need to get or actively seek symptom relief (n=1009) reported the following reasons: menopause is a natural part of life (34%), symptoms are not that bothersome (32%), uncomfortable going to get care (eg, staying away from medical offices due to COVID-19; 21%), non-medical methods for symptom relief in use (eg, yoga, prayer, home remedies, family traditions, or lifestyle remedies; 18%), concern about safety of available medications (17%), and insurance/cost challenges (13%). Changes initiated by women who did not seek symptom relief (n=487) included use of a fan (53%), exercise (37%), OTC treatments (35%), diet changes (32%), supplements including herbal remedies (30%), care from a healthcare provider (30%), self-care (eg, yoga or meditation; 24%), home remedies (18%), ice packs (18%), digital therapeutics (eg, cooling devices; 10%), and family tradition (6%). OTC medications or supplements that were used included products for pain relief (eg, acetaminophen, aspirin, naproxen, combinations of pain reliever, diuretic, and antihistamine; 17%), vitamins/minerals (eg, vitamin D, vitamin E, magnesium; 11%), black cohosh (8%), and melatonin (7%).
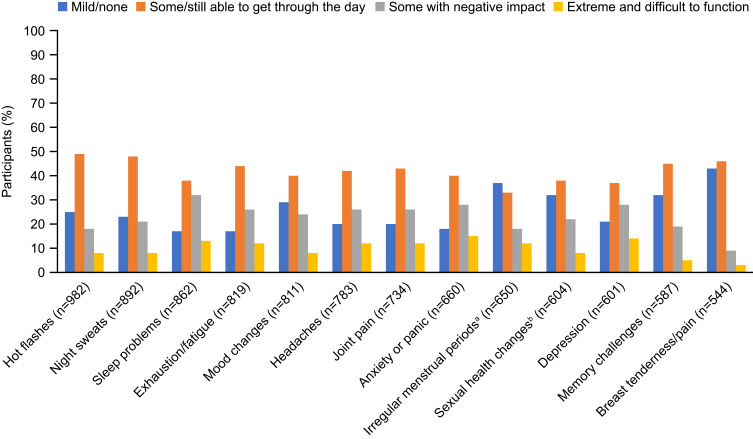
For most participants, symptoms had little to no impact on daily function, but approximately 10% described their symptoms as extremely uncomfortable, making it difficult to function (Figure 2). Approximately a quarter of participants reported some negative impact of symptoms on their life.
Figure 2.
Self-reported level of discomfort experienced for each symptom reported by participants in the HealthyWomen survey (n=1045).
Notes: aMenstrual period different than it has been in terms of when it comes, how long it stays, or amount of bleeding; blow sex drive, dryness, pain during sex, or vaginal atrophy (thinning of tissue and muscle).
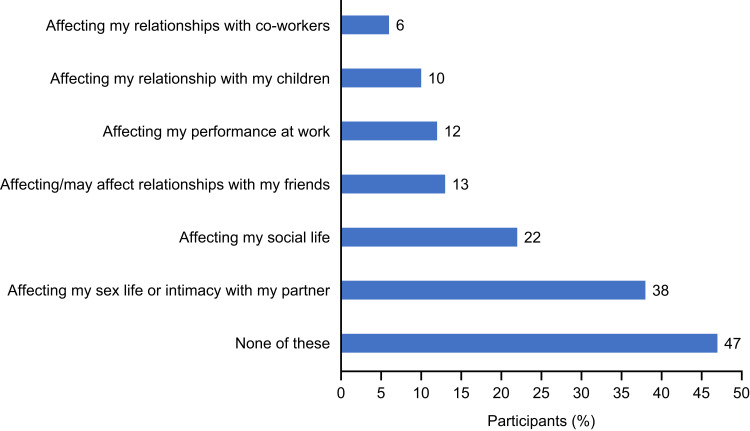
Half of participants (49%) felt that they had enough information to facilitate good decision-making, 20% did not, and 31% were unsure. Overall, 52% reported speaking about their menopause-related experiences with family, 44% with friends, and 42% with healthcare providers. There was substantial evidence of an impact of symptoms on participants’ lives, particularly on their sex lives and relationships with partners and friends and their social life (Figure 3). Many participants (58%) reported that they were happy they would no longer have their menstrual period, and 29% reported finding it liberating to no longer worry about getting pregnant. While 31% had no concerns about other people’s perceptions of their age, 29% reported not wanting to be considered as old.
Figure 3.
The impact of perimenopausal and menopausal symptoms on quality of life of women in the HealthyWomen study (n=1045).
Notes: Responses to the question: “Which of the following do you believe when it comes to menopause?”.
BECOME
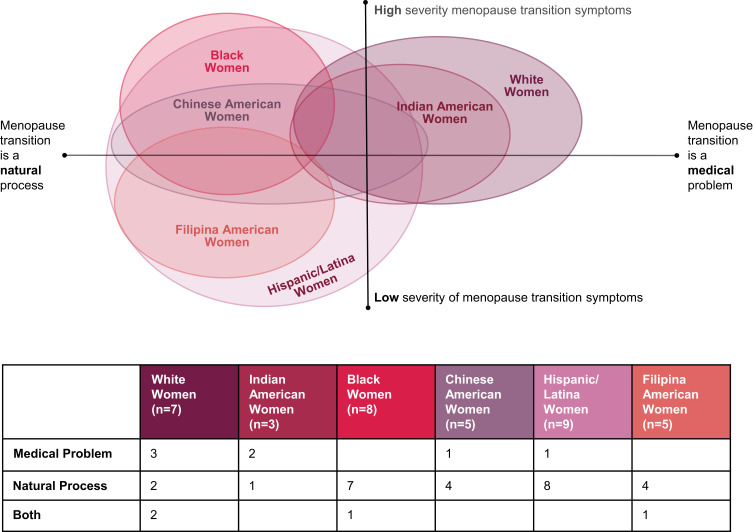
Participants (n=37) reported using a variety of behavioral, lifestyle, and traditional pharmacological strategies and prescription medications to address VMS, sleep difficulties, and fatigue (Table 2). Descriptions of menopause as a medical problem versus something more aligned with a natural process differed according to self-identified race, culture, and ethnicity (Figure 4). Participants who self-identified as White or Indian American were more likely to perceive menopause transition to be a medical problem, with symptoms described as severe. Participants who self-identified as Black, Hispanic, Chinese American, or Filipina American were more likely to perceive menopause transition to be a natural process; the perception of symptom severity varied between these groups. (See participant quotations on menopause transition experiences in Supplementary Table 1.)
Table 2.
Strategies for Symptom Management Reported by Participants in BECOME (n=37)
| Hot Flashes & Night Sweats | Difficulty Falling or Getting Back to Sleep | Fatigue |
|---|---|---|
| Placing ice packs and wet cloths by the bed | More exercise | Going outside for fresh air |
| Having fans by the bed and in purses | Doing word puzzles | Taking afternoon naps |
| Changing shirts, putting on new sheets | Reading before bed | Consuming more caffeine during the day |
| Taking a cold shower | Sleepy time tea | |
| Turning up the air conditioning | Going to bed extra early | |
| Wearables to track symptoms | Cutting back on sugar and caffeine | |
| Going online to look up treatments and remedies | Taking prescription sleep aids | |
| Prescription medication (HT, SSRIs) | Melatonin, CBD |
Abbreviations: CBD, cannabidiol; HT, hormone therapy; SSRIs, selective serotonin reuptake inhibitors.
Figure 4.
The influence of race, culture, and ethnicity on perceptions of and experiences with perimenopause and postmenopause on participants in the BECOME survey (n=37).
NODE.Health Survey
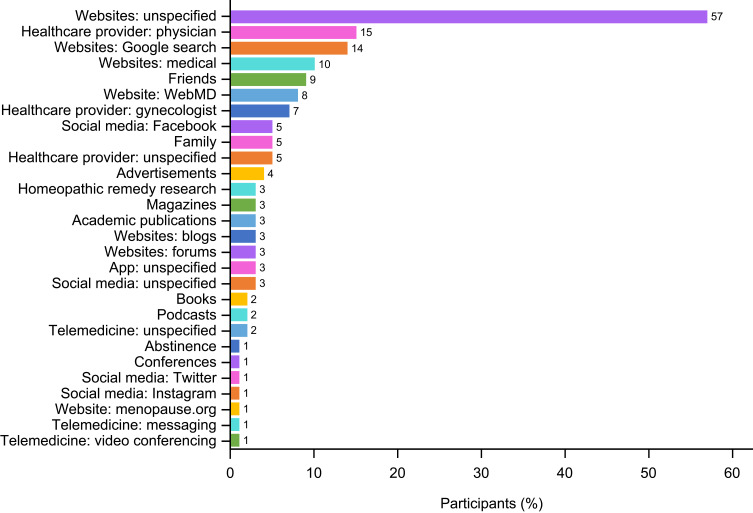
Over 80% of participants reported irregularity of menses, hot flashes, night sweats, sleep disturbances, and mood swings, although most participants (57%) were not tracking their symptoms. Only 27% cited the healthcare provider as a source for perimenopausal symptom management, with most citing use of a diverse array of technology-based information resources (Figure 5).
Figure 5.
Types of resources for perimenopause symptom management used by NODE.Health survey participants (n=100).
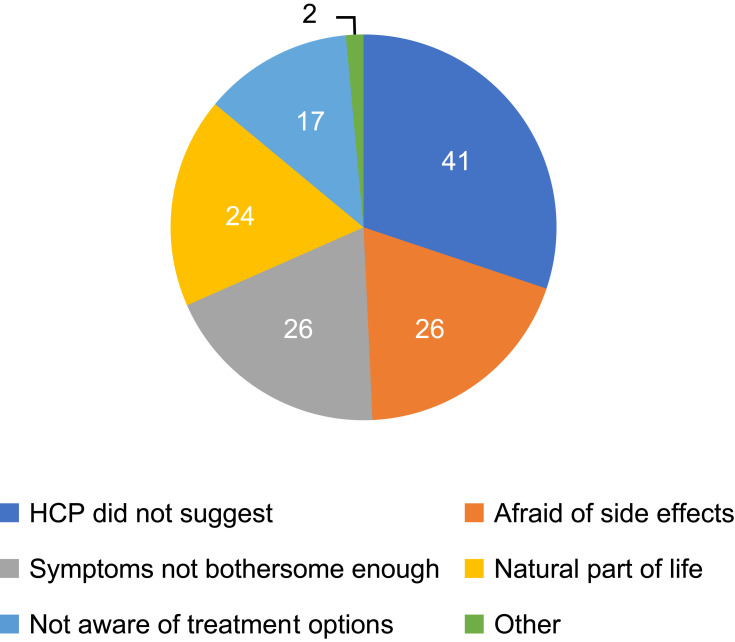
Interaction with the Healthcare Provider
Of the HW study participants who had a discussion with a healthcare provider (n=144), 66% received a prescription medication. Of these, 72% believed the medication reduced and/or improved their symptoms. Among participants who did not receive a prescription, different reasons were given (Figure 6). When asked for their preferences on who to receive care from for symptoms (n=1045), the most cited were an obstetrician/gynecologist (46%) or a primary care doctor (35%). Participants’ preferences on whether to receive care in-person or via telehealth/telemedicine changed with the COVID-19 pandemic, with 92% responding in-person prior to the COVID-19 pandemic compared with 71% after onset of the pandemic.
Figure 6.
Reasons why participants in the HealthyWomen survey who visited a healthcare practitioner for menopause symptoms did not take a prescription medication (n=42).
Abbreviation: HCP, healthcare practitioner.
In the BECOME study (Supplementary Table 2), consistent with views on menopause transition as a medical problem or a natural process, White participants were more likely to see a healthcare provider for their symptoms, while Filipina American participants were least likely. Participants described a preference to talk about menopause transition with healthcare providers who did not rush them, were good listeners, and had expertise in the area. Participants self-identifying as White were more likely to be taking a prescription medication for symptoms compared with those self-identifying as Black, Hispanic, or Filipina American. Overall, participants reported a preference for older female doctors, who could empathize with their experience. If participants felt that they were being pushed toward therapies that they did not want, they avoided discussing their experiences. If participants had had a negative experience in the past, they may switch provider or avoid seeing healthcare professionals.
Interviews with healthcare practitioners in the NODE.Health study (n=15) revealed that 67% (10/15) arrived at treatment decisions jointly with the patient. Treatment options discussed included hormonal therapy (HT; 100% [15/15]), non-HT (73% [11/15]), and natural supplements (40% [6/15]). Some healthcare providers (27% [4/15]) shared knowledge, treatments, or recommendations about complementary and alternative medicines in addition to FDA-approved treatments.
Use of Healthcare Technology
Data from the BECOME study suggest that a variety of technology is used to address menopause transition. The most experience was with health websites, followed by electronic medical record portals and online forums, and the least with digital health apps. Low awareness of digital health apps as well as app fatigue contributed to the low uptake of this technology. Many participants had experience with virtual visits, especially due to COVID-19, but usually for non-menopause-related health issues. Almost half, including all self-identifying as White, used electronic health record portals, not only to see their health information, but also often to communicate with their healthcare practitioners and manage their medical care. The most cited sources of information included WebMD and the Mayo Clinic and the most frequently used wearable devices were Fitbit and Apple Watch. Two-thirds of participants tracked symptoms or health experiences around menopause transition; a quarter used apps for tracking symptoms and a quarter used wearables, typically to track sleep and exercise. A third of participants tracked their symptoms using calendars or pen and paper.
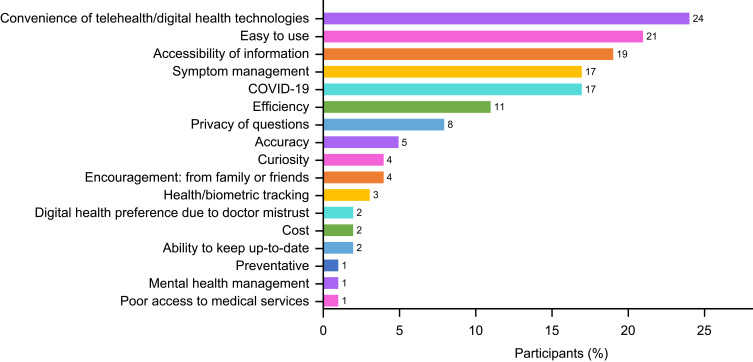
In the NODE.Health study most of the healthcare providers (87% [13/15]) offered remote visits during the COVID-19 pandemic via Zoom, telehealth platforms, Doximity Dialer, or telephone. The two practices not using remote visits cited age, computer literacy, and socioeconomic status as reasons. Most providers (53% [8/15]) preferred that women tracked symptoms digitally. Most participants (67% [67/100]) were interested in app-based technology to help with symptom management, with 64% (64/100) interested in an app-based service to receive treatment related to menopause symptoms. Over two-thirds (71% [71/100]) used Google searches or unspecified websites as a means of finding information pertaining to perimenopause, and 45% (45/100) were unsatisfied with the online resources that described menopause-related symptoms. For those interested in seeking digital health technology, convenience, ease of use, and accessibility were the most common reasons (Figure 7), while 16% (16/100) indicated no interest in technology.
Figure 7.
Factors influencing participant choice to pursue digital health technologies in the NODE.Health survey (n=100).
Discussion
It is well documented that some women are strongly affected by the physical and emotional changes of menopause transition.24 Consistent with previous studies, approximately half of participants in the HW survey felt the need to seek relief from symptoms. While for most participants symptoms had little to no impact on daily function, there were a number for whom symptoms made it difficult to function and had a negative impact on their life. Of the various symptoms, hot flashes were reported to have the most significant effect on daily life because of their association with additional psychological and physical symptoms such as irritability, fatigue, depression, memory problems, and aches and pains.25 In this study, there was evidence for a substantial or perceived impact of menopause transition symptoms on close relationships, social life, and work performance. Over a third of participants reported that symptoms will affect or are affecting sex life or intimacy with their partner, over a fifth of participants reported them affecting their social life, and there was also an impact reported on work performance and relationships with co-workers.
Once women recognize menopause transition symptoms, they are often reluctant to seek medical advice to help manage them.26 In this study the most commonly cited reasons for not seeking care earlier included lack of awareness on both what is considered “normal” in terms of type, severity, and longevity of symptoms and treatment options. In addition, reasons provided by women who had not tried to get care from a healthcare practitioner for their symptoms included feeling that menopause transition is a natural part of life, being uncomfortable with going to get care, or preferring to use alternative strategies, such as changes to lifestyle and diet, or alternative or complementary therapies or OTC therapies rather than prescribed medication. To add to the complexity regarding women’s reasons for not seeking care, it may be that social perceptions around femininity and aging affect women’s likelihood of seeking medical treatment. Indeed, responses from the HW survey showed that a third of participants had concerns about other people’s perceptions of their age or did not want to be considered old.
Among women who sought medical treatment and received a prescription, almost three-quarters believed the medication reduced and/or improved their symptoms. However, the most common reason for not providing a prescription was that the healthcare provider did not think it was needed.
Outcomes from the BECOME research appeared to be influenced by race, with women identifying as White or Indian American more frequently describing symptoms as severe and a medical problem compared with women in the other groups. This is supported by previous studies suggesting that Japanese and Chinese women report menopause transition symptoms less frequently than women from other ethnic groups, while African American and Hispanic women reported some symptoms more frequently than non-Hispanic Caucasian women. In addition, differences in attitudes towards menopause transition and symptoms have also been observed among Latin American and Asian women from different ethnic groups.27–31
Many women used online resources to find information on perimenopause, although many were dissatisfied with the available information. The healthcare needs of women experiencing menopause transition include easy access to data and sharing experiences with healthcare providers without a rigid and patronizing assessment of attitudes and behaviors. Results from the NODE.Health study suggest that the attitudes and perceptions that women hold about their healthcare providers may determine how comfortable they are with seeking support from healthcare practitioners throughout the menopausal transition.
To assist women experiencing menopause transition, healthcare providers may adopt strategies aimed at systematically identifying the physical and psychological changes they are undergoing, and accurately assess the severity and impact of symptoms.25 It is postulated that this may help to guide healthcare providers in making decisions regarding additional support needs, including appropriate treatment with drugs and complementary therapies. Furthermore, women experiencing menopause transition should be asked for their perspectives, have received adequate information to manage the transition, and be supported by family members, healthcare providers, and other social institutions to satisfy their care needs and preserve their quality of life.
It is important to note that this research is questionnaire-based and, as such, is directional in nature. In addition, online recruitment from the general population may have resulted in a biased sample with respect to sociodemographic and digital literacy factors. All three studies selected participants who experienced hot flashes or night sweats. However, there may be individuals who do not experience or recognize these symptoms but experience other menopause transition symptoms. While the BECOME study was designed to include a diverse group of women, it was not representative of the US population. In addition, the group sizes were small and the ability to draw definitive conclusions is limited.
Conclusion
Factors such as cultural beliefs, values, and attitudes towards menopause determine the personal experiences lived in this phase of life. In addition, lack of awareness regarding symptoms, their severity and treatment options, as well as concerns about the perceptions of others are often barriers to seeking help. More open discussions with friends, family, and medical professionals could raise awareness and further reduce any stigma associated with the menopause transition. In turn, to provide optimal care throughout the menopause transition, healthcare providers need to provide a comprehensive evaluation including assessment of medical history and current status, psychosocial and cultural background, and individual personal and subjective perspectives. Personal and tailored healthcare according to a woman’s needs, preferences, and expectations should be provided.
Acknowledgments
The authors would like to thank Kathryn Mossman PhD (Throughline Strategy), HealthyWomen, Throughline Strategy, and NODE.Health for help with conducting the studies, and everyone who participated in the surveys. Medical writing support was provided by Sam Coates of Envision Scientific Solutions, Horsham, UK, and funded by Astellas Pharma Inc. To mitigate any potential conflict of interest with the sponsor, Advarra (Columbia, MD) was selected as an independent Institutional Review Board and all three protocols were submitted for assessment. Advarra is fully accredited by the Association for the Accreditation of Human Research Protection Programs (AAHRPP).
Funding Statement
Funding was provided by Astellas Pharma Inc.
Data Sharing Statement
Researchers may request access to anonymized participant level data, trial level data and protocols from Astellas sponsored clinical trials at www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing see: https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Gloria Richard-Davis reports honoraria from Therapeutics MD and SCYNEXUS. Andrea Singer reports personal fees from Astellas, outside the submitted work. She also reports that conflicts relating to osteoporosis and bone health are research grants/quality improvement funding (paid to Georgetown University and MedStar Health) from Radius Health, UCB; consulting/advisory boards for AgNovos, Amgen, Radius Health, and UCB; speaking/teaching for Amgen and Radius Health. Deanna King and Lisa Mattle are employees for Astellas Pharma Inc. The authors report no other conflicts of interest in this work.
References
- 1.Dalal PK, Agarwal M. Postmenopausal syndrome. Indian J Psychiatry. 2015;57(Suppl 2):S222–232. doi: 10.4103/0019-5545.161483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Namazi M, Sadeghi R, Behboodi Moghadam Z. Social determinants of health in menopause: an integrative review. Int J Womens Health. 2019;11:637–647. doi: 10.2147/IJWH.S228594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whiteley J, DiBonaventura M, Wagner JS, Alvir J, Shah S. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health. 2013;22(11):983–990. doi: 10.1089/jwh.2012.3719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delamater L, Santoro N. Management of the Perimenopause. Clin Obstet Gynecol. 2018;61(3):419–432. doi: 10.1097/GRF.0000000000000389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whiteley J, Wagner JS, Bushmakin A, Kopenhafer L, Dibonaventura M, Racketa J. Impact of the severity of vasomotor symptoms on health status, resource use, and productivity. Menopause. 2013;20(5):518–524. doi: 10.1097/GME.0b013e31827d38a5 [DOI] [PubMed] [Google Scholar]
- 6.Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009;62(2):153–159. doi: 10.1016/j.maturitas.2008.12.006 [DOI] [PubMed] [Google Scholar]
- 7.Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015;22(3):260–266. doi: 10.1097/GME.0000000000000320 [DOI] [PubMed] [Google Scholar]
- 8.Garlick D. Menopause in the workplace: introducing good practice. The Endocrinologist; 2019. Available from: https://www.endocrinology.org/endocrinologist/131-spring19/features/menopause-in-The-workplace-introducing-good-practice/. Accessed September 20, 2021.
- 9.Burden L. Many women exit workforce for a little-talked about reason. Equality. Available from: https://www.bloomberg.com/news/articles/2021-06-18/women-are-leaving-the-workforce-for-a-little-talked-about-reason?leadSource=uverify%20wall. Accessed November 29, 2022.
- 10.CIPD. Majority of working women experiencing the menopause say it has a negative impact on them at work; 2019. Available from: https://www.cipd.co.uk/about/media/press/menopause-at-work. Accessed September 20, 2021.
- 11.Patterson J. It’s time to start talking about menopause at work. Harvard Business Review Health and Behavioral Science; 2020. Available from: https://hbr.org/2020/02/its-time-to-start-talking-about-menopause-at-work. Accessed September 20, 2021.
- 12.Williams RE, Kalilani L, DiBenedetti DB, Zhou X, Fehnel SE, Clark RV. Healthcare seeking and treatment for menopausal symptoms in the United States. Maturitas. 2007;58(4):348–358. doi: 10.1016/j.maturitas.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 13.Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health. 2006;96(7):1226–1235. doi: 10.2105/AJPH.2005.066936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014;21(9):924–932. doi: 10.1097/GME.0000000000000196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams RE, Kalilani L, DiBenedetti DB, et al. Frequency and severity of vasomotor symptoms among peri- and postmenopausal women in the United States. Climacteric. 2008;11(1):32–43. doi: 10.1080/13697130701744696 [DOI] [PubMed] [Google Scholar]
- 16.Nappi RE, Kroll R, Siddiqui E, et al. Global cross-sectional survey of women with vasomotor symptoms associated with menopause: prevalence and quality of life burden. Menopause. 2021;28(8):875–882. doi: 10.1097/GME.0000000000001793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531–539. doi: 10.1001/jamainternmed.2014.8063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Khoudary SR, Greendale G, Crawford SL, et al. The menopause transition and women’s health at midlife: a progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause. 2019;26(10):1213–1227. doi: 10.1097/GME.0000000000001424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thurston RC, Joffe H. Vasomotor symptoms and menopause: findings from the study of women’s health across the nation. Obstet Gynecol Clin North Am. 2011;38(3):489–501. doi: 10.1016/j.ogc.2011.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. doi: 10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 23.Gehlbach H, Artino AR Jr. The survey checklist (Manifesto). Acad Med. 2018;93(3):360–366. doi: 10.1097/ACM.0000000000002083 [DOI] [PubMed] [Google Scholar]
- 24.Monteleone P, Mascagni G, Giannini A, Genazzani AR, Simoncini T. Symptoms of menopause - global prevalence, physiology and implications. Nat Rev Endocrinol. 2018;14(4):199–215. doi: 10.1038/nrendo.2017.180 [DOI] [PubMed] [Google Scholar]
- 25.Hoga L, Rodolpho J, Gonçalves B, Quirino B. Women’s experience of menopause: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep. 2015;13(8):250–337. doi: 10.11124/jbisrir-2015-1948 [DOI] [PubMed] [Google Scholar]
- 26.Constantine GD, Graham S, Clerinx C, et al. Behaviours and attitudes influencing treatment decisions for menopausal symptoms in five European countries. Post Reprod Health. 2016;22(3):112–122. doi: 10.1177/2053369116632439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gold EB, Sternfeld B, Kelsey JL, et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152(5):463–473. doi: 10.1093/aje/152.5.463 [DOI] [PubMed] [Google Scholar]
- 28.Locklear TD, Doyle BJ, Perez AL, Wicks SM, Mahady GB. Menopause in Latin America: symptoms, attitudes, treatments and future directions in Costa Rica. Maturitas. 2017;104:84–89. doi: 10.1016/j.maturitas.2017.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monterrosa A, Blumel JE, Chedraui P. Increased menopausal symptoms among Afro-Colombian women as assessed with the menopause rating scale. Maturitas. 2008;59(2):182–190. doi: 10.1016/j.maturitas.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 30.Haines CJ, Xing SM, Park KH, Holinka CF, Ausmanas MK. Prevalence of menopausal symptoms in different ethnic groups of Asian women and responsiveness to therapy with three doses of conjugated estrogens/medroxyprogesterone acetate: the Pan-Asia Menopause (PAM) study. Maturitas. 2005;52(3–4):264–276. doi: 10.1016/j.maturitas.2005.03.012 [DOI] [PubMed] [Google Scholar]
- 31.Richard-Davis G, Wellons M. Racial and ethnic differences in the physiology and clinical symptoms of menopause. Semin Reprod Med. 2013;31(5):380–386. doi: 10.1055/s-0033-1348897 [DOI] [PubMed] [Google Scholar]