Abstract
As part of our ongoing interest in patient- and family-centered care in epilepsy, we began, before the onset of the CoVID-19 pandemic, to evaluate the concerns and preferences of those delivering and receiving care via telemedicine. CoVID-19 arrived and acted as an unexpected experiment in nature, catalyzing telemedicine’s widespread implementation across many disciplines of medicine. The arrival of CoVID-19 in Ireland gave us the opportunity to record these perceptions pre- and post-CoVID. Data were extracted from the National Epilepsy Electronic Patient Record (EEPR). Power BI Analytics collated data from two epilepsy centers in Dublin. Analysis of data on reasons for using the telephone support line was conducted. A subset of patients and clinicians who attended virtual encounters over both periods were asked for their perception of telemedicine care through a mixed methods survey. Between 23rd December 2019 and 23rd March 2020 (pre-CoVID era), a total of 1180 patients were seen in 1653 clinical encounters. As part of a telemedicine pilot study, 50 of these encounters were scheduled virtual telephone appointments. Twenty eight surveys were completed by clinicians and 18 by patients during that period. From 24th March 2020 to 24th June 2020, 1164 patients were seen in 1693 encounters of which 729 (63%) patients were seen in 748 scheduled virtual encounters. 118 clinician impressions were captured through an online survey and 75 patients or carers completed a telephone survey during the post-CoVID era. There was no backlog of appointments or loss of care continuity forced by the pandemic. Clinicians expressed strong levels of satisfaction, but some doubted the suitability of new patients to the service or candidates for surgery receiving care via telemedicine. Patients reported positive experiences surrounding telephone appointments comparing them favorably to face-to-face encounters. The availability of a shared EEPR demonstrated no loss of care contact for patients with epilepsy. The survey showed that telemedicine is seen as an effective and satisfactory method of delivering chronic outpatient care.
Keywords: Telemedicine, Electronic Patient Records, Digital Health, eHealth, Remote Care
1. Introduction
Epilepsy is a chronic, noncommunicable disease of the brain characterized by recurrent seizures [1]. In Ireland, it is believed that up to 37,000 people suffer from epilepsy, and this number may be increasing [2].
The traditional model of chronic disease management involves episodic, reactive, and hospital centric care being delivered to patients via face-to-face encounters [3]. The establishment of the Irish National Care Programme for Epilepsy (NCPE) in 2010 sought to drive clinical service improvements in Ireland through improved patient experience, access to care, and value [4], [5]. At the core of the NCPE was an emphasis of delivering truly person-centered care (PCC) to people with epilepsy (PWE) nationwide, which would be achieved through continuous meaningful engagements between the health system and PWE [6], [7]. In the past few years, extensive engagements with PWE have resulted in the rollout of nurse-led epilepsy services supported by a point of care, web-based national epilepsy electronic patient record (EEPR), and dedicated emergency department seizure care pathways across Ireland [8], [9], [10].
Telemedicine refers to the practice of medicine using technology when the clinician and patient are not in the same location [11]. It encompasses a range of information and communication technologies that support delivery of remote or long-distance clinical care such as telephone, video, or email consultations [11], store and forward systems [12], and mobile health (mHealth| applications [13]. There is a growing evidence base across several conditions indicating that telemedicine has benefits in reducing cost, improving health outcomes, and diagnostic accuracy [13], [14], [15], [16], [17], [18]. When deployed correctly telemedicine can lead to Low-cost high Value E-care (LoVE) and provides an opportunity to improve patient health service engagement choices, promote self-care and reduce face-to-face clinician contact where relevant and appropriate – all core objectives of the NCPE.
St. James’s Hospital (SJH) and Beaumont Hospital (BH) are large teaching hospitals in Dublin hosting two of the country’s largest epilepsy services. In December 2019, SJH began a pilot study to explore the provision of care through the creation of ‘virtual clinics’ and utilization of telemedicine for chronic epilepsy management. These virtual clinics were held monthly and consisted of preselected PWE receiving their care via a telephone call by an advanced nurse practitioner (ANP), a specialist registrar in neurology or a consultant epileptologist. The rest of the clinics were delivered in the form of face-to-face appointments in the outpatient department (OPD) clinic.
From the end of March 2020, the coronavirus (CoVID-19) pandemic forced a rapid-reorganization of chronic disease care delivery. Social distancing and self-isolation, introduced by governments to limit the spread of viral infection, dramatically reduced face-to-face encounters. Changes that typically would have encompassed months of planning, pilot testing, and education were compressed into days [19]. CoVID-19 reached the Republic of Ireland in the spring of 2020. On 12th March, the government shut all schools, childcare facilities, and cultural institutions, and advised canceling large gatherings. On 24th March, almost all businesses, venues, and amenities were shut. Three days later, the government banned all ‘nonessential’ travel outside one’s home (including visits to family and partners). Scheduled outpatient clinics were largely canceled across the health system [20].
Both SJH and BH made the decision to facilitate as many epilepsy OPD clinic appointments as possible through telephone calls. It was decided to continue the evaluation of telemedicine which began pre-CoVID in SJH and expand it across the two centers.
This project, therefore, began before the CoVID-19 era with a carefully planned implementation of a telehealth solution based on the use of a point of care electronic patient record and telephone contact in selected patients. As part of the implementation we sought to understand the perceptions of chronic epilepsy management via telephone consultations from a clinician and patient perspective.
In this manuscript, an audit of the following aspects of epilepsy patient care is reported:
-
(1)
The impact of the pandemic declaration on the mode of care for patients with epilepsy.
-
(2)
The experience of those delivering and receiving care via telemedicine-enabled epilepsy care.
2. Methods
2.1. EEPR data capture and analysis
A quantitative approach was taken to extract data from the Irish National Epilepsy Electronic Patient Record (EEPR) and assess the readiness of epilepsy clinical services to adopt a telemedicine model in the face of CoVID-19.
The EEPR is a custom-designed, web-based point of care clinical record that is shared across geographical and institutional boundaries [21]. The EEPR has approximately 9000 unique patient records from all over Ireland, over 100 clinician users with more than 700 encounters every month.
Power BI software (Microsoft) was used to extract quantitative data collected in the three months prior to CoVID-19 up to 23rd March 2020 and for the three months during and immediately after the society wide lockdown to June 24th, 2020. As part of the recording in the EEPR, the encounter type is recorded indicating how that encounter took place, such as in the outpatient clinic or as part of a scheduled virtual encounter. Quantitative data showing the overall numbers of encounters by encounter type were extracted and analyzed for both reporting periods pre and post-CoVID.
2.2. Clinical audit – data capture
2.2.1. Survey tools
Both quantitative and qualitative approaches were taken during this evaluation to understand the experience of clinicians and patients delivering and receiving epilepsy care via telemedicine.
Patients attending ‘pre-CoVID virtual clinics’ at SJH were identified by the EEPR and a subset were surveyed by a researcher (JB) from 23rd December 2019 to 23rd March 2020 in order to capture the experience of clinicians and patients receiving their care in this manner.
We sought to capture the experience of clinicians and patients in a short and effective manner through the use of semi-structured surveys. In order to minimize disruption to clinical appointments and ease the burden of clinicians and patients, we limited the survey to one page. As a tool specifically existing for epilepsy management via telemedicine does not exist, questions from the Telehealth Satisfaction Questionnaire [22] and Telemedicine Satisfaction Questionnaire [23] were adapted to create clinician and patient surveys for use in this study (Supporting Table 1 ). Uniquely, we also collected qualitative data from epilepsy patients receiving care through telemedicine, which had not been reported in the literature previously.
Table 1.
Questions common to the survey tools used to collect data from clinicians and patients both pre- and post-CoVID.
| Clinician Questionnaire | Patient Questionnaire | |
|---|---|---|
| 1. | With whom did you conduct this telephone appointment? | Do you typically have to take time off work, school, or college to attend a face-to-face appointment in the hospital? |
| 2. | Did you experience any technical difficulties during this encounter? | How do you typically travel to face-to-face appointments in the hospital? |
| 3. | Did you feel this patient was appropriate for a telephone appointment? | How was your experience interacting with the clinician during this appointment? |
| 4. | Are you happy for this patient to continue their routine care virtually? | How was your overall experience having this appointment over the phone? |
| 5. | Did you discharge this patient? | Do you have any other thoughts or opinions surrounding telephone appointments for epilepsy care? |
2.2.2. Pre-CoVID quantitative data capture
In the pre-CoVID audit the researcher (JB) placed paper questionnaires on the desks of the clinicians working at the virtual clinic. Following each appointment conducted over the phone they were requested to complete it. The researcher collected the completed questionnaires 1–2 days after the clinic from the administrative staff and manually inputted these data on Microsoft Excel. The researcher then contacted all patients who had an appointment via telephone. If the patient was busy and not in a position to speak on the phone, they were called at a later time. Telephone survey data were recorded on Microsoft Excel.
2.2.3. Post-CoVID quantitative data capture
In the post-CoVID era, the methodology of collecting data from clinicians and patients needed to be adapted to facilitate social distancing. The clinician feedback, therefore, would be collected through the Qualtrics online survey tool. Again, patient contact details were gathered from the National EEPR. These patients were contacted via telephone within 48 hours of the virtual encounter, and if they agreed they would complete a survey over the telephone. In the same manner as pre-CoVID, patients were called at a later time if the timing of the initial call did not suit them.
2.2.4. Pre and Post-CoVID qualitative data capture
At the end of each telephone survey with patient participants, we collected qualitative impressions from patients about the use of telemedicine for receiving epilepsy care. Participants were asked if they had any additional thoughts or impressions about telemedicine not expressed in the previous survey questions. These oral data were transcribed verbatim by the researcher.
2.3. Data analysis
Survey data collected from clinicians pre-CoVID were manually inputted and analyzed on Microsoft Excel. Post-CoVID, clinician data were exported from Qualtrics to Microsoft Excel to facilitate data analysis.
Patient data collected via telephone surveys were inputted and analyzed on Microsoft Excel. Qualitative impressions recorded by patients at the end of surveys were coded and common codes were organized into themes surrounding experience of telemedicine.
2.4. Ethics
This study was classified as a Clinical Audit by the SJH Research & Innovation Office and the BH Clinical Audit Department. Surveying clinicians and patients about their experience using telemedicine did not require referral to a full institutional ethical board review, but was subjected to the local governance rules and a Data Protection Impact Assessment (DPIA) was produced in advance of the audit.
3. Results
3.1. EEPR data analysis
Quantitative data for all encounters from 23rd December 2019 to 23rd March 2020 were compared to data from encounters from 24th March 2020 to 24th June 2020. Despite the abruptness of the deployment of telehealth, the numbers show that there was practically no loss of access to scheduled expert opinion and care between the pre and post-CoVID eras.
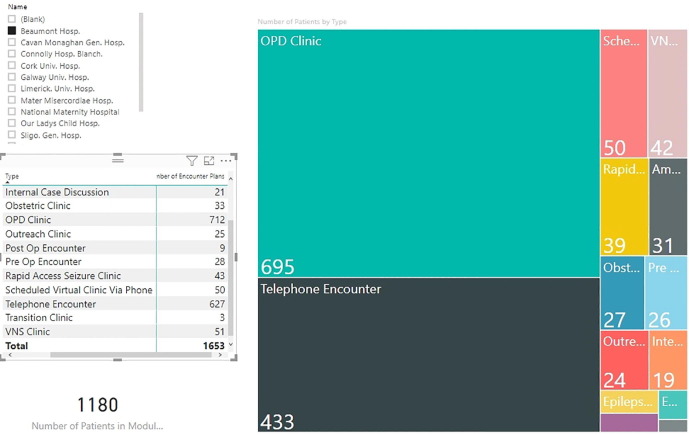
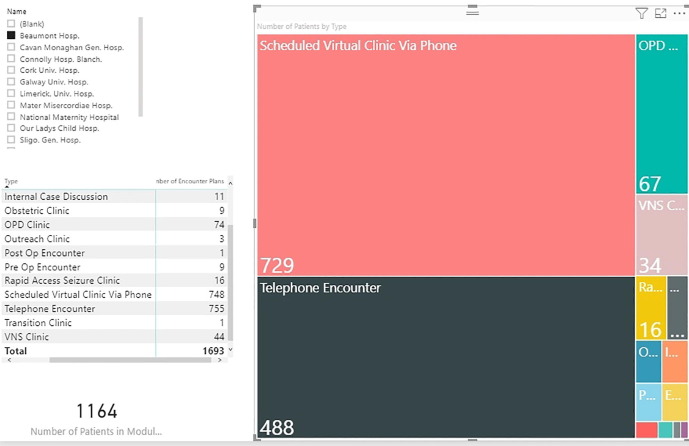
Pre-CoVID, 1180 patients were seen across 1653 encounters. Post-CoVID, 1164 patients were seen across 1693 encounters. In both instances, some patients had more than one encounter during these periods which explains the greater number of encounters relative to the number of patients.
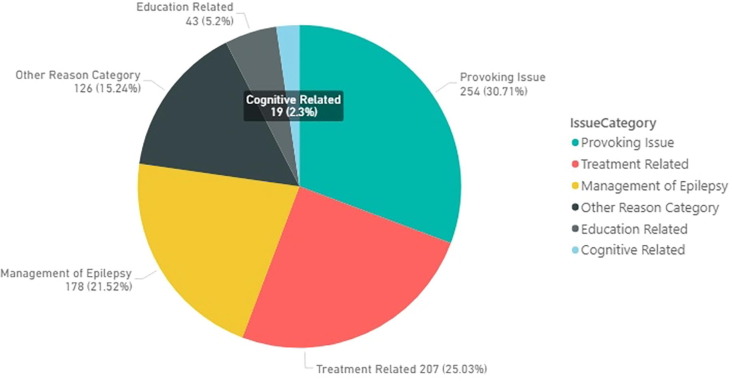
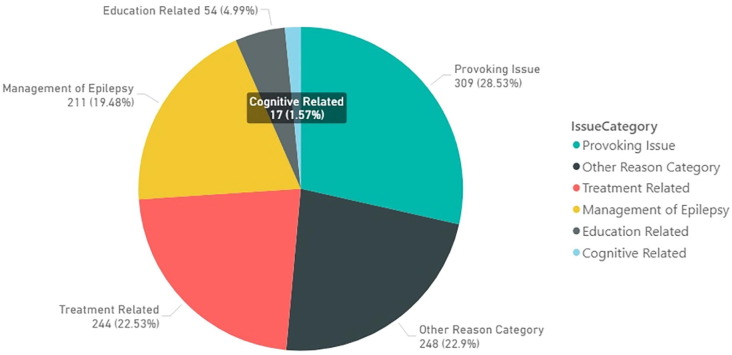
Fig. 1, Fig. 2 show the increase in virtual encounters between the two periods without the loss of care continuity. Furthermore, 433 patients had unscheduled telephone encounters using dedicated helpline numbers pre-CoVID compared to 488 patients post-COVID, indicating no loss of access to unscheduled care support. It should be noted that four clinicians in one of the centers (SJH) contracted the virus and four other clinicians were sent into self-isolation due to contact tracing for 14 days. For that period, none of the epilepsy staff were at work. Similarly, across the two centers four nurses who had intensive care unit (ICU) experience were also redeployed to manage the surge in admissions during that time. Despite this, there was no accrual of missed encounters as the staff were able to deliver care from their homes. Fig. 3, Fig. 4 show data pertaining to the reasons for the use of unscheduled telephone and email services between the pre and post-CoVID eras. The overall concerns of patients using the advice lines did not dramatically differ. This indicates that the CoVID pandemic did not substantially change the requirement for expert advice.
Fig. 1.
Breakdown of Encounters by Encounter Type in BH and SJH from 23rd December 2019 to 23rd March 2020.
Fig. 2.
Breakdown of Encounters by Encounter Type in BH and SJH from 24th March 2020 to 24th June 2020.
Fig. 3.
Breakdown of Telephone Encounters by Issue Category in BH and SJH from 23rd December 2019 to 23rd March 2020.
Fig. 4.
Breakdown of Telephone Encounters by Issue Category in BH and SJH from 24th March 2020 to 24th June 2020.
3.2. Survey of clinician and patient experience
3.2.1. Clinician experience
From 23rd December 2020 to 23rd March 2020, 50 scheduled telephone encounters took place. 28 questionnaires were completed by 8 clinicians following these telephone encounters. From 24th March 2020 to 24th June 2020, 729 scheduled telephone encounters took place. 118 questionnaires were completed by 13 clinicians following these telephone encounters during this period. Clinicians did not repeat the survey if they had previously completed a virtual telephone appointment with the same patient.
Pre-CoVID, in 52% of telephone encounters, clinicians spoke directly to patients. In the other 48% of telephone encounters, clinicians spoke to either a family member or a carer. Post-CoVID, 77% of telephone encounters were directly with patients and 23% were with family members or carers. Clinicians reported experiencing technical difficulties in 24% of encounters pre-CoVID and 8% of encounters post-CoVID. The most common difficulties cited were poor telephone signal and disconnections occurring during the appointments.
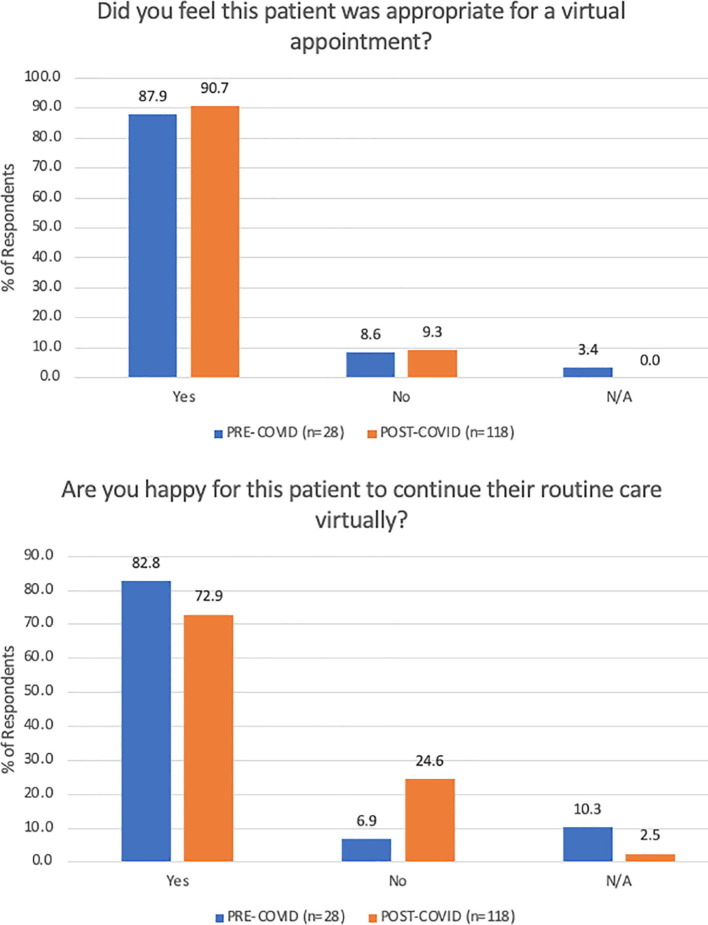
Clinicians largely felt that the patients they conducted telemedicine appointments with were appropriate for this type of care both pre- and post-CoVID. Results indicated that clinicians were happy for the majority of the patients to continue their care virtually. These results are illustrated in Fig. 5 .
Fig. 5.
Graphs outlining clinician response to questions surrounding patient appropriateness and future mode of care delivery.
3.2.2. Quantitative data surrounding patient experience
Pre-CoVID, 18 patients who had a virtual appointment were followed up and they or a family member or carer completed a survey via telephone to record their experience. Post-CoVID, 75 patients or their family members or carers completed a survey via telephone. In both the pre- and post-CoVID populations, no patient who answered the phone call from the researcher declined to take part in the survey. No patient completed the survey with the researcher more than once.
Pre-CoVID, 44% of respondents to the telephone survey stated that they needed to take time off work, school, or college to attend a face-to-face appointment. Post-CoVID, 55% of respondents stated they need to take time off to attend appointments.
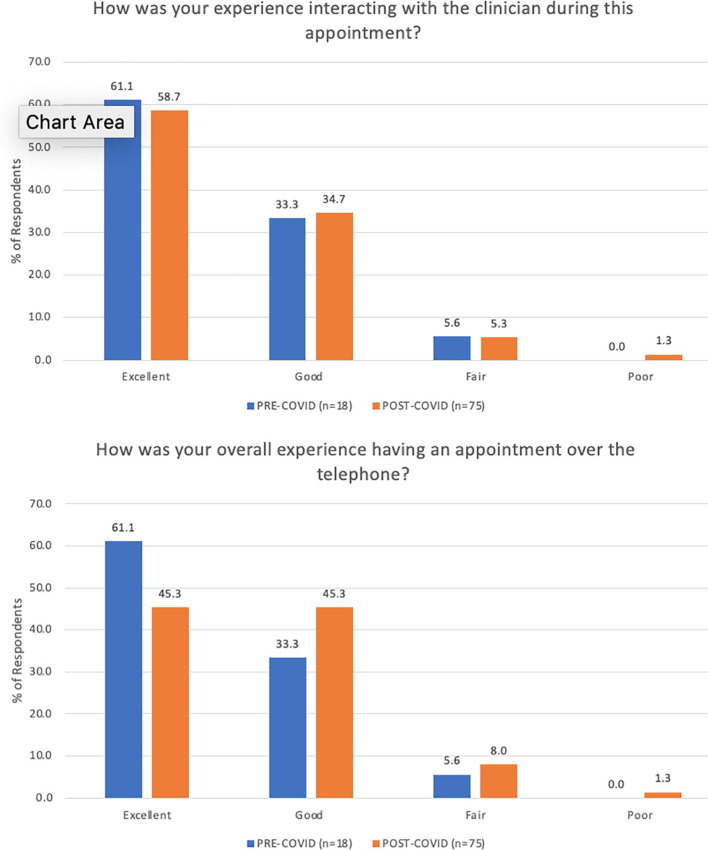
Patients and carers reported similarly positive responses pre- and -post-CoVID with regard to interaction with their clinician and overall experience receiving their care via telephone. These results are illustrated in Fig. 6 .
Fig. 6.
Graphs outlining patient response to questions surrounding interaction with clinician and overall experience using telemedicine.
3.2.3. Qualitative data surrounding patient experience
Patients expressed a range of responses, both positive and negative, in response to the question ‘Do you have any other thoughts or opinions surrounding telephone appointments for epilepsy care?’ both pre- and post-CoVID.
3.2.3.1. Similarities to face-to-face appointments
Many patients remarked at how similar the telephone call was to a face-to-face appointment. A number of patients stated that the nature and conversation of the virtual appointment was the same as previous face-to-face encounters.
P70 – ‘I got the exact same treatment as I would if I had gone in to BH’
P43 – ‘Unless you need a test done, it’s the same as sitting across from them really’
P48 – ‘There’s no physical contact on any of my appointments anyway so the phone is fine’
3.2.3.2. Convenience
Many patients highlighted the convenience of not having to travel to the hospital for an appointment that can often be quite brief.
P13 – ‘I was quite impressed by it. There was no waiting around for a ten-minute appointment’
The convenience of not having to travel to the hospital for an appointment was highlighted in particular by carers of patients who have intellectual or physical disabilities.
P69 – ‘Going to the hospital is usually horrendous. Waiting areas, toilet facilities and all that. This is so great’
3.2.3.3. Stability of condition
The large number of respondents stated that their willingness to engage with telemedicine in the future would depend on the stability of their condition. Many patients expressed that they would be happy to continue with telemedicine for a routine ‘check-up’ with clinicians if their seizure frequency remains the same or if epilepsy presents no new problems in their lives.
P47 – ‘If it’s a routine check-up, there’s no need for me to be in wasting the clinician or my time’
P42 – ‘When there’s nothing urgent this is a great way of doing things’
However, a number of respondents stated that if their seizure frequency increased or their epilepsy began to impact their lives in a new manner, they would rather be seen in person rather than virtually.
P36 – ‘If someone is having active seizures, a phone call might not be the best idea’
P75 – ‘If everything is going smoothly then phone is grand. If you’ve a problem you’d want to be seen face to face though’.
3.2.3.4. Video appointments
Many respondents reported that they would like to see the clinician’s face in future virtual appointments through the use of video-conferencing software.
P51 – ‘It would be great if you could see the clinician’s face, I’d love to do a video call’
P1 – ‘Facetime or Zoom would be better than the phone call’
3.2.3.5. Concentration and appointment flow
Some patients expressed that this new style of appointment required more concentration and preparation compared to face-to-face appointments.
P66 – ‘You’ve to think more on your feet…You’ve to do a bit more thinking than if you were there in person’
P8 – ‘Questions come up more easily (In face to face appointments). It’s easier to develop conversation…If you’re doing it on the phone have your questions written down beforehand’
3.2.3.6. Preference for face-to-face
Other patients stated that telemedicine was something they did not wish to utilize in the future, and they would prefer face-to-face.
P15 – ‘This was not very satisfactory to be honest. I’d prefer face to face’
P35 – ‘If I’d a choice, I’d prefer face to face. I feel more comfortable chatting in person’
P58 – ‘I’m not great at talking on the phone I don’t think. I can explain things more in depth in person. I like getting out of the house and going to the hospital for the appointments’
4. Discussion
The predominantly face-to-face model of outpatient follow-up for epilepsy care has existed since the 19th century [24]. In-person outpatient care often fails to reliably provide responsive care when patients need intervention [25]. Despite this, telemedicine has not been widely used to provide chronic epilepsy care for patients. Clinicians and patients persisted with onsite appointments in spite of the potential feasibility of remote visits, especially for stable chronic patients [26], [27].
The CoVID-19 pandemic has forced health administrators and clinicians to adopt and implement telemedicine in a short space of time to continue caring for patients during society-wide travel restrictions. It is already clear that patients are apprehensive about the risk of coronavirus exposure and a study on severe psychological distress conducted in China during the initial CoVID-19 outbreak revealed that PWE showed higher psychological distress scores than otherwise healthy individuals [28]. Furthermore, epilepsy tends to be more severe in patients with intellectual disability whose daily routines have been severely disrupted by the pandemic. A hastily or poorly implemented telehealth system could add to these difficulties.
In this study, quantitative data garnered from the National EEPR show that the switch to telehealth coincided with a nationwide social lockdown on the 24th of March 2020. The switch was comprehensive and the data reveal that the two large epilepsy services in large urban centers caring for more than 7000 epilepsy patients managed to avoid any backlog, seeing almost the same number of cases in the 3 months up to the end of March compared to the 3 months after. The agility of the services was in our view largely to do with the dynamic capability of the EEPR which was able to enable and facilitate the switch with its point of care capability and remote access.
The other finding from the quantitative data is that the use of telephone and email support services showed that in the number of enquiries increased slightly from 433 to 488, but, in general, the concerns of epilepsy patients were only marginally different comparing pre- and post-CoVID periods. This suggests that there may not have been a significant increase in care requirement for epilepsy patients during the pandemic, although this is being analyzed separately [29].
Studies which compare the experiences and outcomes of telemedicine vs face-to-face visits for neurological conditions have consistently displayed positive results for telemedicine [11], [30], [31]. This audit is unique in that not only does it provide quantitative data reporting positive experience, it provides qualitative insights into what aspects of telephone appointments patients did and did not enjoy. To our knowledge, this is the first time such qualitative data have been reported.
Survey data collected, both pre and post-CoVID, displayed high levels of satisfaction with telemedicine from both a clinician and patient perspective. Importantly, patients who received their care via telemedicine pre-CoVID were carefully selected for these types of appointments based on the impression clinicians had of their condition from previous appointment history. Post-CoVID, all patients, not just preselected ones, were subject to telemedicine care – which raises concerns about the suitability of unselected cohorts; however, the high levels of clinician and patient satisfaction seen in both cohorts indicate that telemedicine is a viable process for all, not just a select few who clinicians believe are suitable for it.
Interestingly, clinicians were more likely to express concerns about the suitability of certain patients for using telemedicine for their care going forward than the patients themselves (25% vs 9%). Clinicians described concerns that patients experiencing their first clinic visit; those with unclear seizure frequencies and those who were surgical candidates are not appropriate for receiving care via telemedicine. While patients in general were more predisposed to telehealth, some expressed more concern that if their condition were to worsen, they would prefer to receive care in person than over the phone.
It is important to implement the learnings of epilepsy care delivery during this pandemic in a post-CoVID world. A number of publications and policy documents have stated that we must maintain remote models of care for patients with chronic conditions and not return to ‘business as usual’ once this pandemic ends [9], [17], [19], [27], [32], [33]. Our results, in particular the qualitative data garnered from patients, indicate that a majority of patients with epilepsy are happy to continue their care virtually if their condition remains stable or no new issues arise between appointments. If structures were to be created which allow patients or their carers to submit their preference for a telemedicine or face-to-face visit in advance of an outpatient appointment, this would likely decrease the number of patients who are unnecessarily traveling to hospitals to receive their epilepsy care. Our group has recently reported the introduction of a patient portal which has the capability to indicate these preferences and even alter the notion of scheduled visits [9]. The use of video consultations has become quite common during CoVID across many disciplines of medicine [34]. The utilization of video as opposed to telephone could provide additional visual cues to clinicians and therapeutic presence to patients, which could allow more difficult consultations to take place remotely [34].
5. Limitations
The number of completed surveys by clinicians and patients in the pre-CoVID era is low. Data were collected following 50 clinical encounters from clinicians and 18 patients completed surveys via telephone over a 3-month period from December 2019 to March 2020. During this period of data collection, clinicians were inconsistent in completing surveys following each appointment, and patients proved difficult to reach in the days following the clinic. Nonetheless, we feel it is important to include the pre-CoVID data because they serves to illustrate the similarities in clinician and patient experience of telemedicine from an era when it was voluntarily being employed for selected patients to when it was employed out of necessity for continuing to provide care to all patients during a pandemic.
6. Conclusion
The switch to telemedicine during the CoVID pandemic in the Irish Epilepsy Service, as in many centers around the world, was rapid and comprehensive. The availability of a shared agile web-based EEPR allowed us to demonstrate no loss of care contact for this vulnerable group across two large urban epilepsy centers. A mixed methods survey allowed us to demonstrate that telemedicine is seen to be an effective and satisfactory method of delivering chronic outpatient care. This was true regardless of the CoVID-19 pandemic indicating the long-term potential of telemedicine as a method of care delivery.
Acknowledgments
Acknowledgements
The authors would like to thank the clinicians working in SJH and BH Epilepsy Departments for facilitating this audit of care delivery and experience. The authors would also like to thank the patients, family members, and carers who were contacted and completed the survey as part of this audit.
Funding
This publication has emanated from research supported in part by a research grant from Science Foundation Ireland (SFI) under Grant Number 16/RC/3948 and co-funded under the European Regional Development Fund and by FutureNeuro industry partners.
Declaration of competing interest
None of the authors of this paper have competing interests which could inappropriately bias this study.
References
- 1.Epilepsy n.d. https://www.who.int/health-topics/epilepsy#tab=tab_1 (accessed January 10, 2020).
- 2.Linehan C., Kerr M.P., Walsh P.N., Brady G., Kelleher C., Delanty N., et al. Examining the prevalence of epilepsy and delivery of epilepsy care in Ireland. Epilepsia. 2010;51:845–852. doi: 10.1111/j.1528-1167.2009.02417.x. [DOI] [PubMed] [Google Scholar]
- 3.Varley J., Kiersey R., Power R., Byrne J.P., Doherty C., Saris J., et al. Igniting intersectoral collaboration in chronic disease management: a participatory action research study on epilepsy care in Ireland. J Interprof Care. 2019;00:1–9. doi: 10.1080/13561820.2019.1697655. [DOI] [PubMed] [Google Scholar]
- 4.Royal College of Physicians of Ireland, National Clinical Programme for Epilepsy (NCPE). The National Clinical Programme for Epilepsy MODEL OF CARE Clinical Strategy and Programmes Division 2016.
- 5.Darker C.D., Nicolson G.H., Carroll A., Barry J.M. The barriers and facilitators to the implementation of National Clinical Programmes in Ireland: Using the MRC framework for process evaluations 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Health Serv Res. 2018;18:1–10. doi: 10.1186/s12913-018-3543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrne J.-P., Power R., Kiersey R., Varley J., Doherty C.P., Saris A.J., et al. The rhetoric and reality of integrated patient-centered care for healthcare providers: an ethnographic exploration of epilepsy care in Ireland. Epilepsy Behav. 2019;94:87–92. doi: 10.1016/J.YEBEH.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Power R., Byrne J.P., Kiersey R., Varley J., Doherty C.P., Lambert V., et al. Are patients ready for integrated person-centered care? A qualitative study of people with epilepsy in Ireland. Epilepsy Behav. 2020;102 doi: 10.1016/j.yebeh.2019.106668. [DOI] [PubMed] [Google Scholar]
- 8.Higgins A., Downes C., Varley J., Doherty C.P., Begley C., Elliott N. Supporting and empowering people with epilepsy: contribution of the Epilepsy Specialist Nurses (SENsE study) Seizure. 2019;71:42–49. doi: 10.1016/j.seizure.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Power K, McCrea Z, White M, Breen A, Dunleavy B, O’Donoghue S, et al. The development of an epilepsy electronic patient portal: Facilitating both patient empowerment and remote clinician‐patient interaction in a post‐COVID‐19 world. Epilepsia 2020:epi.16627. https://doi.org/10.1111/epi.16627. [DOI] [PMC free article] [PubMed]
- 10.Williams J., Doherty J., Di Blasi C., Mabarak D., Kennedy U., Doherty C.P. Seizure care in the emergency department. Identifying and bridging the gaps. A study of care and outcomes from 644 seizure presentations. Epilepsy Behav. 2018;78:226–231. doi: 10.1016/j.yebeh.2017.08.042. [DOI] [PubMed] [Google Scholar]
- 11.Bahrani K., Singh M.B., Bhatia R., Prasad K., Vibha D., Shukla G., et al. Telephonic review for outpatients with epilepsy—A prospective randomized, parallel group study. Seizure. 2017;53:55–61. doi: 10.1016/J.SEIZURE.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Breen P., Murphy K., Browne G., Molloy F., Reid V., Doherty C., et al. Formative evaluation of a telemedicine model for delivering clinical neurophysiology services part II: the referring clinician and patient perspective. BMC Med Inform Decis Mak. 2010;10:49. doi: 10.1186/1472-6947-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patterson V. Managing epilepsy by telemedicine in resource-poor settings. Front Public Heal. 2019;7:321. doi: 10.3389/fpubh.2019.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Promise and the Peril of Virtual Health Care | The New Yorker n.d. https://www.newyorker.com/magazine/2020/06/29/the-promise-and-the-peril-of-virtual-health-care?utm_source=nl&utm_brand=tny&utm_mailing=TNY_Daily_062320&utm_campaign=aud-dev&utm_medium=email&bxid=5be9d3693f92a40469e2a4e4&cndid=29146287&hasha=c9fd094af004e6f7b61f1e3a9af41e53&hashb=f990541eccb6cc147bcc63d4ef8ccf526241b196&hashc=007aded235eed36f8e92f401a73efdc18b81425f10ac9a00450f376499f81d3d&esrc=AUTO_OTHER&utm_term=TNY_Daily (accessed June 26, 2020).
- 15.Telemedicine & Epilepsy - Practical Neurology n.d. https://practicalneurology.com/articles/2019-oct/telemedicine-epilepsy (accessed April 7, 2020).
- 16.Teixeira-Poit S.M., Halpern M.T., Kane H.L., Keating M., Olmsted M. Factors influencing professional life satisfaction among neurologists. BMC Health Serv Res. 2017;17:409. doi: 10.1186/s12913-017-2343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guzik A.K., Switzer J.A. Teleneurology is neurology. Neurology. 2020;94:16–17. doi: 10.1212/WNL.0000000000008693. [DOI] [PubMed] [Google Scholar]
- 18.Mercy Opens World’s First Virtual Care Center - PR.com n.d. https://www.pr.com/press-release/640030 (accessed July 31, 2020).
- 19.Mehrotra A., Ray K., Brockmeyer D.M., Barnett M.L., Bender J.A. Rapidly converting to “Virtual Practices”: outpatient care in the era of Covid-19. NEJM Catal. 2020;1 doi: 10.1056/CAT.20.0091. [DOI] [Google Scholar]
- 20.Ban on visitors, appointments cancelled at hospitals n.d. https://www.rte.ie/news/coronavirus/2020/0306/1120709-hospital-restrictions-virus/ (accessed September 28, 2020).
- 21.Delanty N., White M., Benson K., McCormack M., Heavin S., Comerford E., et al. Development of a genomics module within an epilepsy-specific electronic health record: toward genomic medicine in epilepsy care. Epilepsia. 2019;60:1670–1677. doi: 10.1111/epi.16278. [DOI] [PubMed] [Google Scholar]
- 22.Telehealth Satisfaction Questionnaire: National First Nations Telehealth Research Project. n.d.
- 23.Yip M.P., Chang A.M., Chan J., MacKenzie A.E. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J Telemed Telecare. 2003;9:46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 24.Page R., Shankar R., McLean B.N., Hanna J., Newman C. Digital care in epilepsy: a conceptual framework for technological therapies. Front Neurol. 2018;9:99. doi: 10.3389/fneur.2018.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw S.E., Cameron D., Wherton J., Seuren L.M., Vijayaraghavan S., Bhattacharya S., et al. Technology-enhanced consultations in diabetes, cancer, and heart failure: protocol for the Qualitative Analysis of Remote Consultations (QuARC) project. JMIR Res Protoc. 2018;7 doi: 10.2196/10913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kissani N., Lengané Y.T.M., Patterson V., Mesraoua B., Dawn E., Ozkara C., et al. Telemedicine in epilepsy: How can we improve care, teaching, and awareness? Epilepsy Behav. 2020;103 doi: 10.1016/j.yebeh.2019.106854. [DOI] [PubMed] [Google Scholar]
- 27.Conde-Blanco E., Centeno M., Tio E., Muriana D., García-Peñas J.J., Serrano P., et al. Emergency implementation of telemedicine for epilepsy in Spain: results of a survey during SARS-CoV-2 pandemic. Epilepsy Behav. 2020;111 doi: 10.1016/j.yebeh.2020.107211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E., et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020:1–8. doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozuna J., Kelly P., Towne A., Hixson J. Self-management in epilepsy care: untapped opportunities. Fed Pract. 2018 [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmed S.N., Mann C., Sinclair D.B., Heino A., Iskiw B., Quigley D., et al. Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient’s perspective. Epilepsia. 2008;49:573–585. doi: 10.1111/j.1528-1167.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 31.Rasmusson K.A., Hartshorn J.C. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia. 2005;46:767–770. doi: 10.1111/j.1528-1167.2005.44804.x. [DOI] [PubMed] [Google Scholar]
- 32.Moynihan R., Johansson M., Maybee A., Lang E., Légaré F. Covid-19: an opportunity to reduce unnecessary healthcare. BMJ. 2020;370 doi: 10.1136/bmj.m2752. [DOI] [PubMed] [Google Scholar]
- 33.Bloem B.R., Dorsey E.R., Okun M.S. The coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1452. [DOI] [PubMed] [Google Scholar]
- 34.Greenhalgh T., Koh G.C.H., Car J. Covid-19: A remote assessment in primary care. BMJ. 2020;368 doi: 10.1136/bmj.m1182. [DOI] [PubMed] [Google Scholar]