Abstract
The COVID-19 pandemic has brought questions about the desirability of compact urban development to the fore. There are some concerns that high density may be a risk factor that makes it challenging to contain the pandemic. This study aims to investigate the link between density and pandemic spread through a case study of Tehran that has been the epicenter of the pandemic in Iran. Based on data obtained from an online platform and analyzed using structural equation modeling, we found that density alone cannot be considered a risk factor for the spread of COVID-19. In fact, density alone did not explain the geographic distribution pattern of confirmed COVID-19 cases and deaths across the 22 municipal districts of Tehran. We, therefore, argue that efforts should be made to minimize concerns about living in dense urban environments. Indeed, residents of high-density districts can live safely when an outbreak occurs, provided they make some changes in lifestyle and follow public health instructions. Based on the findings, and considering other benefits of compact cities (e.g., climate change mitigation) planners and policy makers are encouraged to continue promoting compact urban forms. They can also use the results of this study in their efforts towards developing appropriate mechanisms and guidelines for effective management of future pandemics in cities.
Keywords: COVID-19, Density, Risk factors, Compact city, Tehran
1. Introduction
COVID-19 was not the first infectious disease affecting cities, and it may not be the last. The pandemic affected cities in many ways. The rapid spread of pandemic convinced many central and local governments to adopt various combative strategies to limit its transmission through measures such as social distancing, partial and total lockdowns, and travel control (Sharifi & Khavarian-Garmsir, 2020; Wilder-Smith & Freedman, 2020). In the meanwhile, high-density cities and urban areas that have long been praised for providing efficiency improvements and fostering innovation and productivity, are now concerned to contribute to the spread of COVID-19 (Boterman, 2020; Hamidi, Sabouri, & Ewing, 2020; Hua et al., 2021; Megahed & Ghoneim, 2020).
Generally, the outbreak of the Coronavirus has resulted in renewed discussions regarding the desirability of compact urban areas. In the past few decades, there have been various efforts aimed at increasing urban density to enhance efficiency and contribute to climate change mitigation (Burton et al., 2003; Stevenson et al., 2016). However, the recent pandemic has raised concerns about the desirability of such efforts on the grounds that density may function as a risk factor by contributing to the spread of viruses such as the COVID-19 (Cordes & Castro, 2020).
Some earlier studies have sought to explain the relationship between urban density and the prevalence of contagious diseases. In this regard, comparing more than 600 U.S. cities, Dalziel et al. (2018) found that influenza transmission is more widespread in densely populated urban areas, probably due to higher rates of social contact between infected and uninfected people. Similarly, in an attempt to explore the origins of epidemics over the past decades, Carter (2017) and Shah (2016) identified a number of political and practical factors affecting global diseases. They argue that crowding could provide a fertile ground for the rapid transmission of pathogens such as Ebola, thereby making it more challenging to control it and leading to more economic and human losses. In contrast, Kissler et al. (2019) identified four hubs of the 2009 influenza pandemic in the United States, and demonstrated that all of them are in medium-sized cities. This contradicts the common view of infection transmission centers being more densely-populated and well-connected.
Mixed evidence has also been reported regarding the role of cities’ characteristics in the spread of COVID-19. Several studies did not find an association between density and the COVID-19 transmission rate (Bhadra, Mukherjee, & Sarkar, 2020; Federgruen & Naha, 2021; Hamidi et al., 2020; Perone, 2021; Sun et al., 2020). For instance, Boterman (2020) did not find compelling evidence that county density plays a critical role in explaining the prevalence of the COVID-19 epidemic in the highly urbanized and densely populated country of the Netherlands. Similar results have been reported by Hamidi et al. (2020) in their analysis of US metropolitan counties. Surprisingly, they observed slightly lower COVID-19 mortality rates in higher density counties. Based on the primary finding of a study by Lin et al. (2020), the percentage of the population migrated from Wuhan and population density are two key variables that can explain the COVID-19 infection rate. However, the linear association between population density and transmission rate was disappeared after controlling for the former variable. They further controlled for population density and found no high infection rates in the densely populated metropolitan regions, except the high-latitude regions. Therefore, they pointed out that factors other than migration from Wuhan and population density play a role in the high transmission rates of COVID-19 in high-latitude regions of China.
In contrast, some studies have reported associations between density and spread of the virus (Coşkun et al., 2021; Imdad et al., 2021; Jamshidi, Baniasad, & Niyogi, 2020; Kodera, Rashed, & Hirata, 2020; Mansour et al., 2021). For instance, in an analysis of demographic and geographic factors in 182 countries, Nguimkeu and Tadadjeu (2021) found that population density along with factors such as urbanization rate and the proportion of people aged 65 and over are decisive factors that can explain why the number of cases COVID-19 is different across countries. Ren et al. (2020) observed that larger population densities form the very high-risk zones of COVID-19 infection in Beijing and Guangzhou. However, this was not the case for Shenzhen, and higher risk zones for infection were characterized by the higher road length and the number of bus stops. There is also evidence from the US indicating that in the aftermath of the COVID-19 outbreak some individuals have migrated to the suburbs due to concerns over the high risks of living in high-density and overcrowded urban areas. This trend has reduced housing demand in high-density neighborhoods (Liu & Su, 2020).
Overall, what we know about the link between urban density and the prevalence of epidemic diseases, such as COVID-19, is largely based upon empirical studies that compare cities and towns across regions. There is still a paucity of research investigating the relationship between urban density and the COVID-19 outbreak at the sub-city level. A better understanding of the influence of urban density on the outbreak of COVID-19 necessitates examining the issue by choosing sub-city subdivisions as geographical units of analysis. This allows understanding the extent to which different areas within a city are affected by the disease.
To fill this gap, this study aims to shed more light on the linkages between urban density and the COVID-19 infection and death rates through analyzing data from Tehran, the capital city of Iran. Iran was among the first countries to report cases of COVID-19 disease and is one of the global epicenters of the pandemic, reporting 61,330 deaths and more than 1,755,000 cases as of March 16, 2021. Having the highest number of confirmed cases and deaths in Iran, Tehran is designated as a COVID-19 red-zone (Arab-Mazar, Sah, Rabaan, Dhama, & Rodriguez-Morales, 2020). Based on the Statistical Center of Iran (2016), Tehran has a population of about 8,600,000 million people. The city represents an excellent case study for the following reasons. First, it has been grappling with COVID-19 since mid-February 2020 and has gone through the early stages of the disease. Over the past few months, a large number of infections have been reported, making it possible to conduct statistical analysis. Secondly, as a big city, Tehran has a heterogeneous urban pattern, making it possible to examine possible associations between density and the intensity of the virus transmission. Thirdly, selecting a developing country city as a case study can extend current knowledge about COVID-19 because developing country cities are currently understudied in the literature.
The results of the study may have a number of implications for policy makers, researchers and the public. As mentioned earlier, COVID-19 pandemic is not the first worldwide epidemic disease and may not be the last. Therefore, the study attempts to add knowledge to existing anti-pandemic policies by providing information on the sub-city scale. It informs planners and policymakers of the type of strategies that are needed in dense areas to cope with pandemics, and discusses the extent to with which urban form characteristics, such as density, should be incorporated in public health policies. In addition, the need for social distancing caused by COVID-19 has left many questioning whether high-density neighborhoods are more susceptible to pandemics; thus casting doubts on the conventional wisdom that compact urban areas are more desirable (Pafka, 2020; Su et al., 2021). This means that exploring connections between density and COVID-19 spread patterns is pertinent to the current literature, and it may assist planners and the public in their future decision making towards sustainable urban development.
The results of the study may have a number of implications for policy makers, researchers and the public. As mentioned earlier, COVID-19 pandemic is not the first worldwide epidemic disease and may not be the last. Therefore, the study attempts to add knowledge to existing anti-pandemic policies by providing information on the sub-city scale. It informs planners and policymakers of the type of strategies that are needed in dense areas to cope with pandemics, and discusses the extent to with which urban form characteristics, such as density, should be incorporated in public health policies. In addition, the need for social distancing caused by COVID-19 has left many questioning whether high-density neighborhoods are more susceptible to pandemics; thus casting doubts on the conventional wisdom that compact urban areas are more desirable (Pafka, 2020). This means that exploring connections between density and COVID-19 spread patterns is pertinent to the current literature, and it may assist planners and the public in their future decision making towards sustainable urban development.
2. Urban density and socio-economic variables affecting the COVID-19 transmission patterns
Previous studies have shown two conflicting effects of density on virus transmission. A line of studies have noted that since more people live per unit area in high-density residentional settlements, there are more close social contacts that, in turn, can accelerate the spread of the virus (Ren et al., 2020; You, Wu, & Guo, 2020). In contrast, some others have pointed out that residents of densely populated places make shorter distance trips and have better access to health facilities. As a result, they are more likely to follow social distancing and stay home measures (Almagro & Orane-Hutchinson, 2020; Hamidi et al., 2020; Liu, 2020). However, previous studies have often only measured population density and overlooked other types of urban density.
Besides, some studies highlighted that age is an important risk factor for COVID-19 (Bialek et al., 2020; Guan et al., 2020; You et al., 2020). According to the results of a study by Liu et al. (2020), elderly COVID-19 patients are more likely to be hospitalized and progress to severe stages of the disease. As a result, a higher number of confirmed COVID-19 cases and death may be recorded in districts with higher proportions of aged people. transport system and infrastructure that increase inter- and intra- urban connectivity, are also regarded as key factors contributing to the spread of contagious diseases, and their role in previous outbreaks (e.g., Ebola) has already been demonstrated (Kutela et al., 2021). In this study, road density, trip generation rate, and car ownership are the variables used to investigate population mobility and connectivity of municipal districts.
In addition to the above-mentioned variables, socio-economic variables may also affect the transmission patterns of the disease. In connection with poverty, Maiti et al. (2021) and Finch and Hernández Finch (2020) argued that individuals with lower levels of education and those living in lower income communities are more susceptible to COVID-19. This is because these groups depend more on public transportation, are less able to work remotely, are less aware of the virus transmission patterns, and are also less likely to take social distancing measures seriously (Das et al., 2021). Therefore, an analysis of the literacy rate, the percentage of college-educated people, and the employment rate can test the above hypothesis. Finally, Wenham, Smith and Morgan (2020) and Jin et al. (2020) suggest that while COVID-19 affects both men and women, gender is a risk factor that may increase vulnerability to COVID-19, and is independent of age susceptibility.
3. Materials and methods
3.1. Data collection and analysis
Independent academics have difficulties in obtaining data from public agencies and healthcare centers that deal with COVID-19 patients. Even if they manage to get access to data, the geographical resolution is not always high. This issue is more profound in developing countries with much lower data transparency (Moghadasi, 2020).
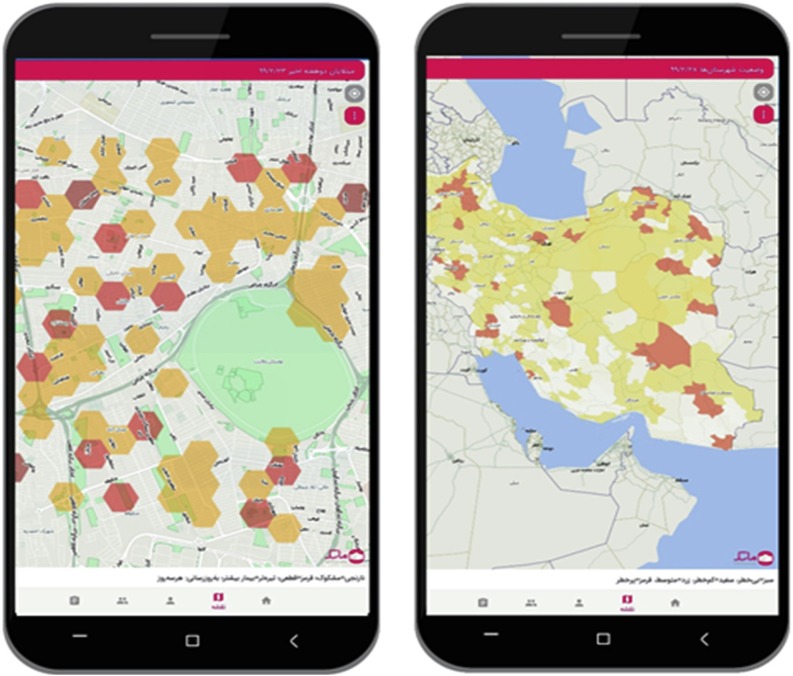
We obtained COVID-19 data from the AC-19 app. It is a coronavirus app released by the Iranian government as part of measures designed to restrain the spread of COVID-19 in the country. Over four million Iranians have installed the application on their smartphones. The app is regularly updated by its developers based on the data provided by the Ministry of Health and Medical Education of Iran. It visualizes the approximate geographical location of infected people at the local, regional, and national levels, and informs people about the latest situation of COVID-19 in each neighborhood and the distance from the high risk locations (see Fig. 1 ). Data was obtained in several stages: First, we zoomed in the city as much as the app allowed and took screenshots. Second, we carefully fitted together images of the zoomed areas to create a photomosaic. Third, we overlaid images obtained from the second stage on the Google Earth platform. Fourth, we tagged the points identified by the AC-19 application, saved the places as a KML file, and converted them into a shapefile.
Fig. 1.
Screenshots from the AC-19 Mobile app. The right figure shows the state of pandemic spread at the city level and the left one depicts the status at the national level. Source: authors.
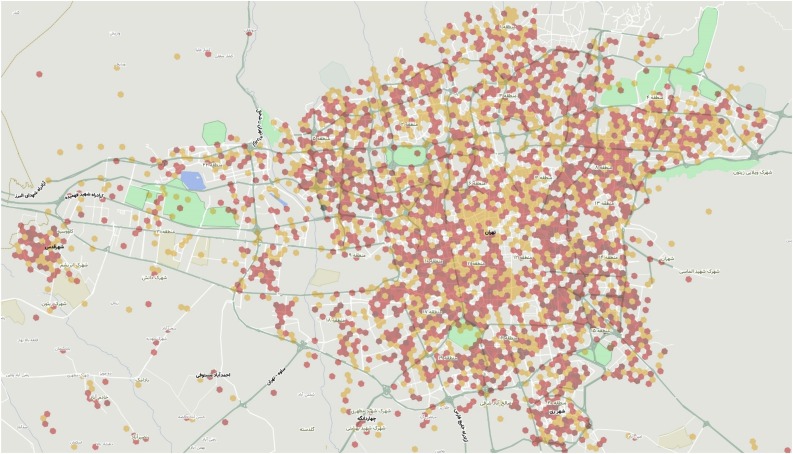
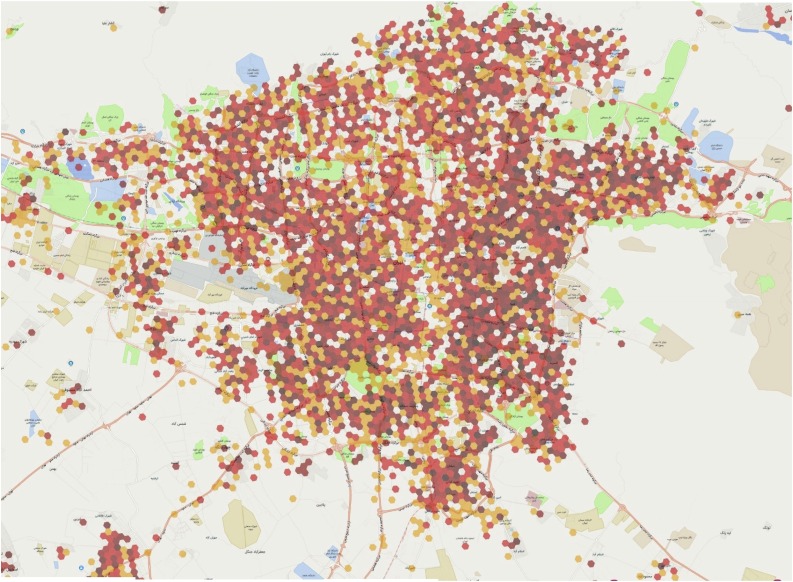
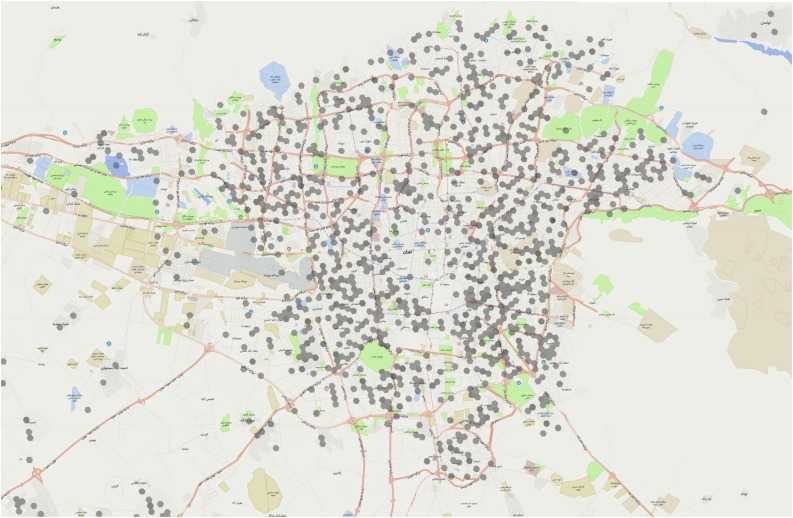
The dataset used in this study consisted of the number of confirmed cases until 4 April 2020 and 27 June 2020, and death cases until 27 June 2020 (see Fig. A1, Fig. A2, Fig. A3 in Appendix A). According to health experts, two waves of COVID-19 have hit Iran during the first six months of the pandemic. The first wave coincided with the Persian New Year holidays in late March and early April. However, the country adopted strict restrictions and controlled this wave in May 2020. The second wave began after relaxing lockdown measures in early April 2020 and led to a surge similar to the one observed in March (Pourghasemi et al., 2020). We selected April 4 and June 27 as the representative dates for the first and second waves, respectively. Moreover, the AC-19 application released the COVID-19 mortality data in June 2020, thus making it possible to analyze the COVID-19 mortality rate risk factors. It seems that examining the geographical distribution of patients with COVID-19 on 4 April can provide insights into how density and the socio-economic characteristics of urban districts can contribute to the spread of the virus in the early stages of the pandemic. Repeating such an analysis on June 27 (84 days later) could indicate the impact of urban density and other socio-economic factors on the persistence and severity of the COVID-19 pandemic and the subsequent mortality. Furthermore, analyzing this relationship over time can demonstrate the success or failure of measures designed to cope with the pandemic, because if COVID-19 policies were properly designed and implemented, the impacts of some risk factors would be reduced over time.
Fig. A1.
location of COVID-19 infected cases on April 4 in Tehran.
Source: Elaborated by authors from the AC-19 Mobile app.
Fig. A2.
location of COVID-19 infected cases on June 27 in Tehran.
Source: Elaborated by authors from the AC-19 Mobile app.
Fig. A3.
location of COVID-19 death cases on June 27 in Tehran.
Source: Elaborated by authors from the AC-19 Mobile app.
To examine the relationship between the explanatory variables of the study and the risk of COVID-19 infection and death, the Structural Equation Modeling (SEM) was used. The SEM has been widely recognized as a mature analysis method in advanced theoretical models for the past 30 years (Tarka, 2018). In addition to ease of use, this approach offers more flexibility to model and evaluate complex theoretical relations (Grace, 2008). The SEM is also widely recognized for the quality and reliability of the scores obtained from its measuring instruments1 (Schumacker & Lomax, 2010).
3.2. Research variables
We followed the modelling approach of Hamidi et al. (2020) who argued that density and socioeconomic factors, while having a direct path to the COVID-19 death and infection, can indirectly affect the COVID-19 death rate through increasing confirmed cases (Li et al., 2021). Accordingly, we examined associations between the COVID-19 morbidity and mortality rates (the dependent variables) and nine factors (independent variables), including various types of urban density (see Table 1 ).
Table 1.
Descriptive statistics of variables.
| Variables | Definitions | Units | Min. | Max. | Mean | Std.dev |
|---|---|---|---|---|---|---|
| population density | The ratio of the resident population to land area | person/km2 | 4.10 | 56.79 | 28.13 | 14.57 |
| aged people density | The ratio of the aged people population to land area | person/km2 | 0.15 | 3.05 | 1.42 | 0.79 |
| built-up density | The ratio of total built-up area to the land area | % | 39 | 100 | 66 | 16 |
| Road density | The ratio of total roads area to the land area | % | 0.003 | 0.73 | 0.21 | 0.21 |
| Trip generation rate | the number of trips that are generated by the residents of districts | Trip/person | 0.68 | 1.81 | 1.08 | 0.28 |
| Car ownership | The number of cars per 1000 inhabitants | Cars/1000 people | 37.54 | 75.79 | 55.15 | 13.09 |
| Distance to metro station | The average distance of neighborhoods to metro station | m2 | 243/16 | 2665/94 | 999/17 | 680/06 |
| Distance to bus station | The average distance of neighborhoods to metro station | m2 | 243/16 | 542/16 | 254/42 | 89/58 |
| Literacy rate | The ratio of literate persons to total population | % | 90.00 | 98.00 | 94.45 | 2.91 |
| Percentage of college-educated | The ratio of college-educated persons to total population | % | 7.9 | 45.19 | 21.7 | 11.5 |
| employment rate | The ratio of the number of employed persons to the active persons | % | 86.00 | 92.00 | 88.55 | 1.68 |
| Sex ratio | The ratio of males to females in the population of a district | Males/100 females | 91.91 | 103.88 | 99.38 | 3.39 |
| Average income | The average income earned per person in a given district | Tomana/person | 1.6 | 2.2 | 1.9 | 0.17 |
Toman is the official currency of Iran.
Previous studies have mostly focused on population density to show how urban density can affect the spread of the virus. However, we took four types of density, including road, population, built-up, and aged-people density into consideration. Road density refers to the ratio of the road network length to its area in a district. It includes all ground networks and is calculated separately for the 22 municipal districts of Tehran. It should, however, be noted that the variable does not include underground network. Population density refers to the ratio of the number of people living in a district to its area. We extracted population data from the population and housing census yearbook (2016). The area of each district was also calculated in the ArcGIS. The built environment density refers to the ratio of total built-up area of a municipal district to its land area. It comprises the total area of entire land uses that exist within a district, including residential, green space, health, education, and leisure land uses. We also included aged population density in this study. It is defined as the number of aged people living per km2of a municipal district. The number of aged people in each district was obtained from the National Census of Iran (2016).
We also investigated the influence of several socioeconomic variables along with urban density. The variables demonstrate the demographic, socioeconomic, and mobility status of residents. Trip generation rate and car ownership are used to examine the effects of mobility on the virus transmission patterns. Trip generation data were obtained from Tehran’s Statistical Yearbook (2016), and population data from Iran’s Population and Housing Census (2016). We divided the number of trips generated in each district by its population. Car ownership rate was also evaluated by dividing the number of cars in a district to its population. As owning and maintaining a car in Iran is costly and poor households cannot afford it, this variable indicates people’s mobility and is used to assess residents’ economic status. Distance to metro and bus stations are other urban transportation related variables. These two variables can predict the possible impact the public transportation may have on the spread of the pandemic. We calculated distance data using ArcGIS, based on the geographic data provided by the Statistical Center of Iran (2016). Each area was divided into several neighborhoods, and the distance of each neighborhood to the nearest metro and bus station was calculated. Finally, the distances were averaged for each of the municipal districts.
Literacy rate and the percentage of college-educated people are two variables that attempt to demonstrate the district’s social status. We downloaded literacy and education level data from Iran’s Population and Housing Census (2016). We also considered the role of sex ratio in the virus dynamic. The variable refers to the proportion of males to females in a district. Moreover, the employment rate and average income were considered in the model. Employment rate refers to the share of employed persons to the active population living within a district. By active population, we mean those between the age of 15 65. We also considered average income as an economic variable. It refers to the average income earned per person in a district. Income data was obtained from the Atlas of Tehran Metropolis (2016).
4. Results
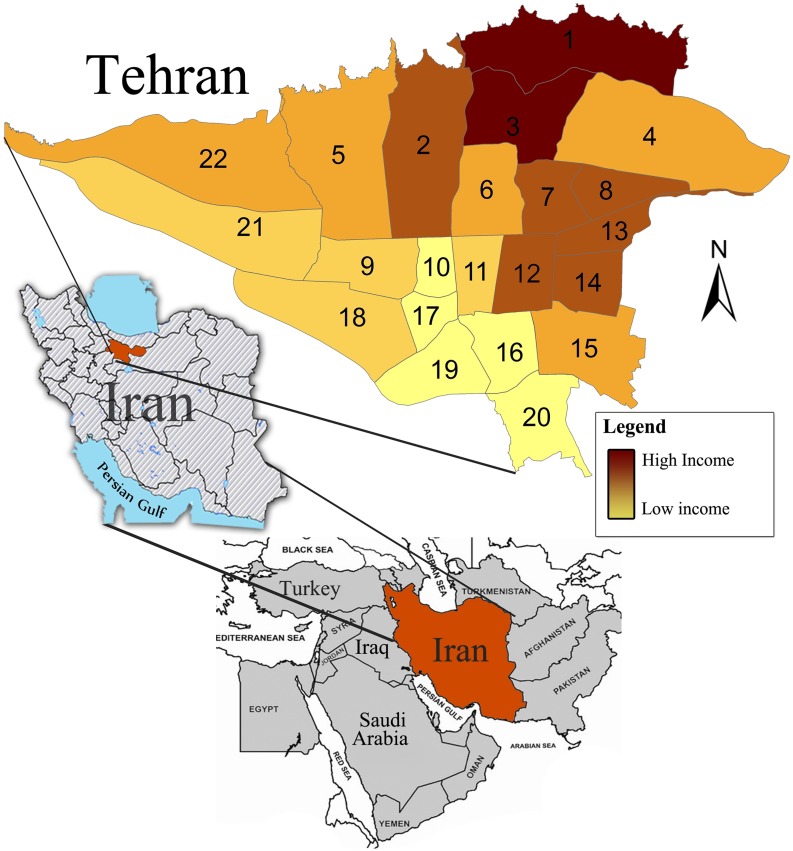
Tehran, the capital of Iran, has a population of 8.6 million people (Statistics Center of Iran, 2016). The city is divided into 22 municipal districts. Districts usually consist of several neighborhoods with similar characteristics. The geographic location of Tehran’s 22 municipal districts is depicted in Fig. 3. The districts that with higher average per capita income are marked with red color. On the other hand, the lower-income districts are shown by a yellow color. The figure shows that high income households mainly live in the northern part of the city while those with lower incomes live mainly in the southern districts. The figure also indicates that the people living in the eastern districts have higher incomes than those living in the western part.
Fig. 3.
The geographic location of Tehran and Iran and income levels in the 22 municipal districts of Tehran. Source: prepared by authors from Statistical Centre of Iran (2016) and Google Satellite images.
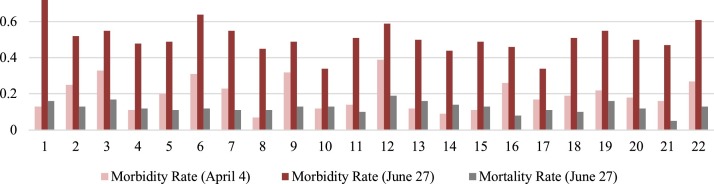
We selected the twenty-two municipal districts of Tehran as the units of analysis (see Fig. 3). Table 2 provides details on the population, area, and the confirmed COVID-19 cases across different districts, for April 4 and June 27, 2020. As can be seen, the municipal districts No. 4, 5, and 2 are the most populated districts, while the least populated ones are those located in the eastern parts of the city (district No.9, 22, 21) (see Fig. 3). Regarding the surface area, the districts No. 4, 22, and 5 are the largest, while the smallest ones are located in the center of the city (districts No. 11, 10, 17). We estimated the morbidity and mortality rates per thousand people based on the number of cases up to April 4 and June 27 and the number of deaths up to June 27. On April 4, the morbidity rate was the highest in districts No. 12, 3, and 9 (see Fig. 2 and Table 2). The lowest, on the other hand, was in districts No. 8, 14, 4 and 15. On June 27, the highest rate was recorded in districts 1, 6 and 22. At the same time, Districts No. 16, 10, and 14 had the lowest morbidity rates. Mortality rate data indicate that the highest mortality rate was in districts No. 3 and 12, while the lowest mortality was in districts No. 21, 16, 18 and 11 (see Fig. 2 and Table 2).
Table 2.
Population, area and information on the confirmed cases of Coronavirus in the 22 municipal districts of Tehran.
| District | Population (2016) | Area (hectare) | Confirmed Case -April 4 (Person) | Confirmed Case -June 27 (Person) | Death Case - June 27 (Person) | Morbidity Rate (%0) on April 4 | Morbidity Rate (%0) on June 27 | Mortality Rate (%0) on June 27 | Population density (Person/Km) | Built-up density (m) | Road density (m) | Average income | Distance to metro station | Distance to bus station |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 493,889 | 4573.9 | 66 | 356 | 81 | 0.13 | 0.72 | 0/16 | 106 | 6375/9 | 131/7 | 2/19 | 1531/5 | 378/26 |
| 2 | 692,579 | 4761.1 | 172 | 363 | 94 | 0.25 | 0.52 | 0/13 | 147 | 4171/0 | 208/9 | 2/05 | 611/98 | 282/71 |
| 3 | 330,004 | 2938.0 | 108 | 182 | 57 | 0.33 | 0.55 | 0/17 | 161 | 4280/7 | 179/1 | 2/21 | 965/42 | 295/70 |
| 4 | 917,261 | 6123.9 | 102 | 440 | 117 | 0.11 | 0.48 | 0/12 | 113 | 6106/4 | 187/7 | 1/98 | 1466/3 | 293/18 |
| 5 | 856,565 | 5318.2 | 172 | 422 | 100 | 0.20 | 0.49 | 0/11 | 149 | 5908/9 | 160/4 | 1/9 | 1228/8 | 337/36 |
| 6 | 250,753 | 2144.3 | 77 | 160 | 32 | 0.31 | 0.64 | 0/12 | 30 | 3847/7 | 93/2 | 1/94 | 340/44 | 175/24 |
| 7 | 312,002 | 1536.8 | 73 | 171 | 36 | 0.23 | 0.55 | 0/11 | 117 | 6399/5 | 234/7 | 2/08 | 358/44 | 206/75 |
| 8 | 425,044 | 1323.9 | 29 | 190 | 48 | 0.07 | 0.45 | 0/11 | 36 | 5902/8 | 97/9 | 2/03 | 412/56 | 171/43 |
| 9 | 174,115 | 1955.4 | 56 | 86 | 24 | 0.32 | 0.49 | 0/13 | 203 | 7329/1 | 242/5 | 1/79 | 863/75 | 251/49 |
| 10 | 326,885 | 805.9 | 40 | 111 | 45 | 0.12 | 0.34 | 0/13 | 323 | 6487/2 | 280/2 | 1/70 | 757/01 | 203/17 |
| 11 | 308,176 | 1223.9 | 43 | 157 | 31 | 0.14 | 0.51 | 0/10 | 197 | 6767/4 | 248/7 | 1/85 | 243/16 | 147/23 |
| 12 | 240,909 | 1602.4 | 94 | 143 | 48 | 0.39 | 0.59 | 0/19 | 151 | 7082/2 | 265 | 2/20 | 313/42 | 180/58 |
| 13 | 253,054 | 1232.5 | 31 | 127 | 41 | 0.12 | 0.50 | 0/16 | 256 | 7330/8 | 255/4 | 2/04 | 548/81 | 270/97 |
| 14 | 489,101 | 1455.9 | 42 | 214 | 71 | 0.09 | 0.44 | 0/14 | 88 | 8453/3 | 128/4 | 2/01 | 491/27 | 193/35 |
| 15 | 659,468 | 2855.2 | 73 | 322 | 88 | 0.11 | 0.49 | 0/13 | 399 | 7213/3 | 350/1 | 1/96 | 752/16 | 198/67 |
| 16 | 267,678 | 1644.9 | 70 | 123 | 24 | 0.26 | 0.46 | 0/08 | 336 | 5915/3 | 317/8 | 1/7 | 488/45 | 182/74 |
| 17 | 278,354 | 790 | 46 | 95 | 32 | 0.17 | 0.34 | 0/11 | 111 | 4499/5 | 103/5 | 1/61 | 507/55 | 175/54 |
| 18 | 419,249 | 3720.7 | 81 | 214 | 45 | 0.19 | 0.51 | 0/10 | 337 | 6382/4 | 309/5 | 1/84 | 2380/ | 289/56 |
| 19 | 255,533 | 2038.5 | 55 | 140 | 42 | 0.22 | 0.55 | 0/16 | 238 | 4916/6 | 201/6 | 1/72 | 1599/ | 284/89 |
| 20 | 367,600 | 2156.7 | 67 | 184 | 45 | 0.18 | 0.50 | 0/12 | 162 | 6329/8 | 155/2 | 1/7 | 1851/ | 192/19 |
| 21 | 186,319 | 5121.1 | 29 | 87 | 10 | 0.16 | 0.47 | 0/05 | 126 | 5649/7 | 142/5 | 1/85 | 1602/ | 344/11 |
| 22 | 175,398 | 6028.7 | 47 | 107 | 23 | 0.27 | 0.61 | 0/13 | 156 | 5052/5 | 142/4 | 1/97 | 2665/ | 542/16 |
Source: The demographic and area data was obtained from the Statistical Yearbook of Tehran (2016), the confirmed cases data was obtained from the AC-19 app.
Fig. 2.
COVID-19 morbidity and mortality rates on April 4 and June 27 in the 22 municipal districts of Tehran.
Besides, based on Table 2, districts No. 8, 10, 15, and 14 are the most densely populated, while districts No. 9, 21, and 22 have the lowest levels of population density. Districts No. 9, 17, and 21 have the highest level of built-up density, while districts No. 2, 5, 15, 18, 20, and 22 have the lowest levels. Regarding road density, districts No.10, 14, and 17 have the highest level of road density, while the eastern districts of 18, 21, and 22 have the lowest levels. We calculated the overall density by summing the three indexes of density mentioned above. Those districts that are located in the center of Tehran have the highest density. By contrast, eastern and western districts have relatively lower levels of urban density.
4.1. The link between the research explanatory variables and COVID-19 morbidity rate on 4 April and 27 June
The model illustrated in Fig. 3 was estimated using SPSS Amos software. The results of the analysis are shown in Table 3 . The rows in the table illustrate the dependent variables affecting the morbidity rates of COVID-19 on April 4 and June 27. The statistical summary shown at the bottom of the table shows the fitness of the model. The model is fitted because it has an appropriatly small chi-square relative to the degrees of freedom and the significant p value (>.05).
Table 3.
Direct effects of density, socioeconomic, and activity characteristics on COVID-19 morbidity rate in 4 April and 27 June.
| Estimate | S.E. | C.R. | P | |||
|---|---|---|---|---|---|---|
| Road density | → | COV4April | .719 | .031 | 23.274 | .000 |
| Road density | → | COV27June | .186 | .167 | 1.114 | .265 |
| Road density | → | Mortality rate | .151 | .011 | 13.922 | .000 |
| Built-up density | → | COV4April | −.007 | .002 | −2.678 | .007 |
| Built-up density | → | COV27June | −.007 | .003 | −2.207 | .027 |
| Built-up density | → | Mortality rate | .002 | .001 | 2.752 | .006 |
| Population Density | → | COV4April | −.003 | .001 | −2.951 | .003 |
| Population Density | → | COV27June | −.004 | .001 | −3.703 | .000 |
| Population Density | → | Mortality rate | .00 | .000 | 1.321 | .186 |
| Aged people density | → | COV4April | 45.707 | 11.202 | 4.080 | .000 |
| Aged people density | → | COV27June | 115.669 | 15.644 | 7.394 | .000 |
| Aged people density | → | Mortality rate | 29.531 | 7.444 | 3.967 | .000 |
| Sex ratio | → | COV4April | .156 | .026 | 5.885 | .000 |
| Sex ratio | → | COV27June | −.094 | .050 | −1.877 | .061 |
| Sex ratio | → | Mortality rate | .043 | .009 | 4.626 | .000 |
| Car ownership rate | → | COV4April | −.020 | .003 | −7.710 | .000 |
| Car ownership rate | → | COV27June | −.016 | .005 | −3.148 | .002 |
| Car ownership rate | → | Mortality rate | −.002 | .001 | −1.481 | .139 |
| Distance to metro station | → | COV4April | /000 | /000 | 1/937 | /053 |
| Distance to metro station | → | COV27June | /000 | /000 | −/681 | /496 |
| Distance to metro station | → | Mortality rate | /000 | /000 | −1/059 | /290 |
| Distance to bus station | → | COV4April | −/001 | /000 | −5/431 | .000 |
| Distance to bus station | → | COV27June | /000 | /000 | −6/715 | .000 |
| Distance to bus station | → | Mortality rate | /000 | /000 | /238 | /812 |
| Trip generation rate | → | COV4April | .001 | .001 | 1.366 | .172 |
| Trip generation rate | → | COV27June | .003 | .001 | 3.078 | .002 |
| Trip generation rate | → | Mortality rate | −.001 | .000 | −3.256 | .001 |
| % of college educated | → | COV4April | .001 | .001 | 1.013 | .311 |
| % of college educated | → | COV27June | .002 | .001 | 1.610 | .107 |
| % of college educated | → | Mortality rate | −.001 | .000 | −3.209 | .001 |
| Literacy rate | → | COV4April | .079 | .017 | 4.544 | .000 |
| Literacy rate | → | COV27June | −.011 | .026 | −.438 | .661 |
| Literacy rate | → | Mortality rate | .012 | .005 | 2.310 | .021 |
| Employment rate | → | COV4April | .018 | .031 | .602 | .547 |
| Employment rate | → | COV27June | −.087 | .032 | −2.697 | .007 |
| Employment rate | → | Mortality rate | .011 | .010 | 1.033 | .301 |
| Average income | → | COV4April | −/014 | /038 | -/376 | /707 |
| Average income | → | COV27June | /076 | /057 | 1/324 | /186 |
| Average income | → | Mortality rate | /101 | /026 | 3/862 | .130 |
Note: Chi-square 236; p value 0.0; comparative fit index: 0.96; normed fit index: 0.96; nonnormed fit index: 0.94; root mean square error of approximation: 0.10.
According to the results, a significant relationship was observed between road congestion and the incidence of COVID-19 on April 4 in Tehran. Areas with a higher density of roads had a higher infection rate. However, 84 days later, this relationship was not observed and shifted to a non-significant positive relationship. On June 27, areas with higher levels of road density did not necessarily have higher rates of COVID-19 morbidity. We also examined the built-up density. The results show a small but significant negative relationship between this type of density and the infection rate on April 4 (p-value: 0.007) and June 27 (p-value: 0.027). A similar relationship was observed between population density and the COVID-19 morbidity rate.
Aged people density was the explanatory variable that had the most significant impact on the COVID-19 morbidity rate across Tehran’s municipal districts. On April 4, there was a robust relationship between aged people density and the COVID-19 infection rate. This relationship was further strengthened on June 27. We also analyzed sex ratio and observed that it was initially an explanatory variable, and districts with a higher proportion of males had a higher COVID-19 morbidity rate. However, on June 27, this relationship became a non-significant negative predictor in the model.
An interesting variable in this study was the car ownership rate. Findings showed that car ownership has a significant inverse association with the infection rate of COVID-19. In other words, the higher the car ownership in a district, the lower the infection rate. However, car ownership was a more prominent explanatory variable on April 4 compared with June 27, although the relationship was at a high level of significance. Besides, on April 4, there was a significant negative but very weak relationship between the COVID-19 morbidity rate and the distance to bus station, indicating that people in areas with a smaller distance to bus stations appear to be slightly affected. However, this relationship disappeared on June 27. This study also showed that the distance to metro stations cannot explain the infection rate. The trip generation rate was another variable evaluated in the present study. The results showed that while there was no significant relationship between trip generation rate and COVID-19 morbidity rate on April 4, this variable later became a significant predictor. However, its effect was negligible (0.003).
In addition, the research findings showed that the literacy rate was a predictor of COVID-19 morbidity rate on April 4, while this was not the case for June 27. This means that the COVID-19 infection risk was higher in areas with higher literacy rates in the early stages of the pandemic, but over time this relationship has become insignificant. We also considered the role of education level. The results showed that there was no significant relationship between the percentage of college educated people and the infection rate of COVID-19. Unlike the literacy rate, the employment rate was primarily unrelated to the COVID-19 morbidity rate, but it had a significant negative impact on June 27. In other words, areas with higher employed populations had lower COVID-19 morbidity rate. Finally, the results indicated that the average income was not linked to the COVID-19 morbidity rate on both April 4 and June 27.
4.2. The link between the explanatory variables and COVID-19 mortality rate on June
The mortality rate in areas with higher road densities was higher, according to Table 4 . Furthermore, a significant but very poor association between mortality rate and built-up density was observed. We found no significant link between population density and mortality rate. This result means that municipal districts with higher population densities did not necessarily experience higher death rates. As expected, the COVID-19 mortality rate was higher in districts with a greater proportion of older people. By analyzing the sex ratio, we found a strong association between sex ratio and COVID-19 mortality rate, indicating that the mortality rate was higher in areas with a higher proportion of men.
Table 4.
Direct, indirect, and total effects of dependent variables on the COVID-19 mortality rate.
| Direct effect | Indirect effect | Total effect | |
|---|---|---|---|
| Road density | .151 | .008 | .159 |
| Built-up density | .002 | .000 | .002 |
| Population Density | .000 | .000 | .000 |
| Aged people density | 29.531 | 8.638 | 38.169 |
| Car ownership rate | −.002 | −.001 | −.003 |
| Distance to metro station | /000 | /000 | /000 |
| Distance to bus station | /000 | /000 | /000 |
| Trip generation rate | −.001 | .000 | −.001 |
| Literacy rate | .012 | −.002 | 010 |
| Employment rate | .011 | −.007 | .004 |
| Average income | .101 | .000 | .101 |
While the previous section showed that the car ownership rate was an influential factor in the prevalence of COVID-19, it did not affect the mortality rate significantly. Similarly, there was no connection between COVID-19 mortality and distance to metro and bus stations. The trip generation had a positive relationship with the COVID-19 mortality rate, but its significance was negligible and close to zero. Similarly, we found a very weak but significant negative association between the COVID-19 mortality rate, and the literacy rate and the percentage of college-educated people. This finding indicates that mortality rates were marginally lower in areas with more literate and highly educated individuals. Besides, while the rates of employment and COVID-19 mortality were associated on June 27, this indicator did not explain the mortality rate. As a result, mortality in areas with higher-employed populations was not necessarily lower. The results also indicated that the average income cannot explain the mortality rate.
5. Discussion
In this study, after accounting for some economic and social variables, we examined the association between urban density and the COVID-19 morbidity and mortality rates. The findings showed that road density has a significant impact on the COVID-19 morbidity rate on April 4, 45 days after the first COVID-19 case was recorded in Tehran. Nevertheless, 84 days later, the relationship became insignificant. This result may suggest that an increase in road density in the early days was followed by an increase in social interactions and congestion regardless of health protocols, because of a low level of public awareness about COVID-19 and lack of proper risk perception in the community. However, it seems that the risk perception and public awareness about the virus were increased over time. Besides, the Iranian government’s policies to control COVID-19 may have contributed to the disappearance of the effect of this form of density on the spread of COVID-19 in Tehran.
This study also showed that the built-up and population densities have a slight relationship with the incidence of COVID-19. This is consistent with some previous research that show density can have a double-edged impact on COVID-19 transmission: on the one hand, it can lead to increased human communication (Ren et al., 2020; You et al., 2020), and on the other hand, it may reduce travel distances and improve access to health services for residents, resulting in greater compliance with social distancing orders (Almagro & Orane-Hutchinson, 2020; Hamidi et al., 2020; Liu, 2020). What appears to be the case is that while many people adopted social distancing in order to avoid being infected by overcrowding, others failed to take safety precautions and interacted with citizens at crowded sites. These two variables were also not strongly related to the mortality rate, which suggests that COVID-19 mortality is more dependent on factors other than urban density.
The aged-people density was the most influential variable of the study. Consistent with Yu et al. (2020), we found that the older people density is strongly related to the COVID-19 morbidity and mortality rates. This shows that there is a link between age and hospitalization, ICU admission, and death (Abate et al., 2020). We also found that while a positive relationship existed between sex ratio and the COVID-19 morbidity rate on April 4, this relationship did not exist on June 27. However, the impact of gender differences on males’ vulnerability is significant. Wenham et al. (2020) suggests that while COVID-19 infection patterns among men and women are similar, death rates are higher among the male population due to variations in the sex-based immunological system, or gender-based differences such as patterns and prevalence of smoking. In investigating the gender difference in severity and mortality in COVID-19 patients, Jin et al. (2020) indicated that gender is a risk factor for COVID-19’s higher severity and mortality, and is independent of age susceptibility.
De Haas et al. (2020) suggest that people are increasingly opting for private cars following the pandemic, resulting in declines in public transport ridership. The study findings showed that the COVID-19 morbidity rate is higher in areas with lower levels of car ownership, and there is a significant but negative relationship between car ownership and the COVID-19 infection rate in Tehran. It may show that public transport users have not complied with health protocols, and the Tehran municipality has failed to maintain public health safety of the transit system. The findings indicated that the average distance to metro and bus stations cannot explain the geographical distribution pattern of the virus. This may be due to the fact that the proximity of public transport stations cannot affect people’s decision to use public transport system during the pandemic. This could indicate people’s concerns over the safety of the system. As a result, those who live or work near the metro and bus stations prefer other modes of transportation for their daily mobility.
Our findings showed that the literacy rate had a positive effect on the COVID-19 morbidity rate on April 4. At the same time, there was no significant relationship between the percentage of college-educated people and the infection rate. However, on June 27, the relationship became insignificant. Besides, there was a significant and positive relationship between the literacy rate and the mortality rate. The percentage of college-educated people had a significant negative but very weak relationship with the mortality rate. Some of these results are contrary to the findings of Hamidi et al. (2020) who found lower COVID-19 infection rates among the US counties with a higher percentage of educated people. It appears that, as a result of media awareness and society’s improved risk perception, the population without college education has also become aware of the threats of this virus and, like others, has complied with health measures. A part of the results mentioned above may be due to the type of work performed by literate and college-educated people who require more human communication. Moreover, distance working does not seem to be as prevalent in Iran as in some other countries, such as the United States. As a result, a significant proportion of educated people still commute to work on a daily basis. Moreover, it appears that the health protocols were not fully implemented in the office environments until 27 June. However, we need more evidence to judge in this regard, and explaining such a relationship could be a subject for future research.
While there was no significant relationship between the employment rate and the COVID-19 morbidity rate on April 4, this relationship became significant and negative on June 27. This means the higher the employment rate in the districts, the lower the infection ratio. However, it should be noted that the prevalence of COVID-19 has intensified economic recession and increased unemployment. Therefore, the employment data may have undergone notable changes, and one should be careful when analyzing the relationship between employment and the COVID-19 infection rate. Therefore, we can only analyze the consequences of previous differences in employment rates in the current crisis. It seems that in districts with a higher employment rate in the past, people saved more money and are now far more likely to stay entirely at home and comply with social distancing rules. In contrast, unemployed individuals, many of whom work in the informal economy in Tehran, do not have income stability and job security. They are deprived of many public benefits, such as unemployment and health insurance (International Labour Organization, 2019). As a result, this group has no choice but to continue working despite the health risks. Taxis and other modes of transportation that have a lower transmission risk are not also affordable options for this group and they are forced to use subways and public buses that are usually crowded and may increase the risk of transmission (Finch & Hernández Finch, 2020; Ruiz Estrada, 2020).
Generally, higher COVID-19 mortality rates have been reported among the urban poor (Sharifi & Khavarian-Garmsir, 2020). However, the results of this analysis revealed no significant connection between average income and COVID-19 morbidity and mortality rates. This could be explained by the fact that the districts vary significantly in terms of age composition. Northern districts with a higher average income have a higher average age, while southern districts with a lower average income have a younger age structure in Tehran. As a result, even though low-income people are more vulnerable to this pandemic, the difference in age composition has made high-income people living in the northern districts also vulnerable. While more people may be infected in the low-income districts, fewer ones go to the hospital or take tests due to their younger age. Besides, due to various factors such as the economic difficulties that the country has experienced recently, there has been a shortage of COVID-19 testing resources. Thus, only people over the age of 65 and those who are pregnant or have pre-existing medical conditions are tested for free. Consequently, a significant portion of the low-income population under the age of 65 cannot take tests and are not included in the statistics.
6. Conclusion
6.1. Concluding remarks
Based on public opinion, low density places seem to be safer against the pandemic since high density increases the number of persons per unit area, contributes to closer human encounters, and may raise the number of COVID-19 patients and the resulting mortality. There is also some evidence suggesting a renewed interest in suburbanization. For instance, Liu and Su (2020) suggest that, in the US, there are households who respond to the potential risk of living in a high-density neighborhood during the pandemic by moving to suburbs. The potential impacts of urban density on the COVID-19 transmission patterns can be considered from regional and local scales. The former compares cities and villages across a territory and investigates the link between the COVID-19 prevalence and urban density. However, on a smaller scale, as in the present study, it is attempted to determine whether density is a risk factor within a city, and whether densely populated districts are the COVID-19 risk zones.
Contrary to initial assumptions, the findings of this study showed that density does not play a major role in the COVID-19 morbidity and mortality rates. Accordingly, while a higher density can contribute to an increase in close social contacts under normal circumstance, this may not always be the case in times of crisis. As a result, residents of densely populated districts, while having better and more efficient access to urban infrastructure and services, can also live safely when an outbreak occurs, provided they make some lifestyle changes. What drives the spread of infectious disease during a pandemic is overcrowding that operates differently from density and can also occur in districts with a low density. As a result, metropolitan areas and densely populated zones can also be safe during the pandemic, as density alone cannot be considered a risk factor for COVID-19.
This research, in line with Nguimkeu and Tadadjeu (2021) and Federgruen and Naha (2021), emphasized that the demographic structure of the populations is much more influential than density. Age is a very important risk factor for the COVID-19 infection and death rates, playing a major role in the geographical distribution patterns of COVID-19. As we indicated, age can play a significant role. In fact, our results showed that the morbidity and mortality rates are not significantly different in the urban districts that have lower average income and a younger age composition. Therefore, a special attention should be paid to districts with a higher proportion of older people.
The presence or absence of a relationship between the spread of COVID-19 and some variables such as car ownership, literacy, higher education, and employment, rather than indicating a cause-and-effect relationship, reflects the success or failure of previous urban policies and the current strategies to cope with the COVID-19 outbreak. As a result, the next section provides key tips for policymakers dealing with COVID-19.
6.2. Research limitations
This study has some limitations, which provide some directions for future research. First, obtaining the official data of COVID-19 at the local level is difficult, if not impossible, in Iran. We extracted the required data based on an innovative method from the AC-19 app. Although the application is supported by the Ministry of Health and Medical Education of Iran, there will remain concerns about the accuracy of the data. Second, as Hamidi et al. (2020) pointed out, the COVID-19 pandemic is a rapidly evolving crisis and the number of confirmed cases is steadily rising. Therefore, it is perhaps too early to draw definitive conclusions. Future research is, therefore, needed to fully understand the relationship between urban density and the transmission patterns of COVID-19. Besides, there are highly populated cities in the global south, such as Cairo, Riyadh, Mumbai, Delhi, Lagos, Karachi, Jakarta, Istanbul, São Paulo, and Mexico City that can be interesting to compare to Tehran. Third, while there is a nationwide shortage of testing capacity, the number of confirmed cases highly depends on the number of individuals being tested. Moreover, relatively few children and young adults with COVID-19 are hospitalized and, therefore, they are not considered in statistics. Accordingly, it is possible that some positive cases have not been accounted for. Future research should pay special attention to the age structure when comparing societies. Forth, considering the lack of access to data on smaller sub-city divisions, the study only focuses on the 22-municipal district of Tehran. However, prospective studies should rely on a more granular scale (i.e., neighborhood) to obtain more accurate findings.
6.3. Key take away points for policymakers
This study revealed that the geographical distribution of COVID-19 infection and mortality is not uniform across Tehran. Therefore, policymakers should intelligently determine the type and severity of policy measures for each district based on demographic, environmental, economic, and social characteristics (Valizadeh et al., 2021). Districts with a higher number of older adults and people who are more reliant on public transit need more tailored policies. Specific testing services should be dedicated to these targeted districts, and further training for these socio-economic classes should be carried out. In many countries, such as Iran, testing for COVID-19 is costly, and this group of the population is less able to perform the test. As a result, testing for the elderly and households without a personal vehicle should be carried out at a lower cost (Cordes & Castro, 2020).
This study also showed an association between the COVID-19 infection rate and the proportion of college-educated people in the municipal districts of Tehran. While college-educated people may be better able to work remotely, it seems that this capacity has been so far unexploited. As a result, all available smart strategies for managing the outbreak need to be exploited. For the post-COVID era, policymakers and public agencies should create the necessary technological infrastructure to manage such a complex crisis. Such pre-crisis arrangements help keep societies from being overwhelmed when pandemics happen, as COVID-19 was not the first and would probably not be the last pandemic hitting cities.
This study indicated that a decrease in car ownership is associated with a rise in the number of COVID-19 patients in Tehran. This city has so far been expanded based on an auto-oriented pattern of development. The future development of the city needs to be adjusted based on a neighborhood-oriented plan that seeks to mix services within walking distance of homes, encourage residents to walk more, and allow them to accomplish more in one trip. This is expected to contribute to an overall reduction in the number of trips. Besides, this finding may also indicate that the transit system in Tehran has not yet been successful in providing a safe environment. As a result, public transportation providers should enhance public health safety of the public transportation system based on COVID-19 prevention considerations. Finally, this study showed that districts with lower levels of employment, literacy, and car-ownership are more vulnerable. Therefore, more efforts are needed to reduce socio-economic disparities and enhance social justice in Tehran.
6.4. Key take away points for planners
Major events such as war, natural disasters, and pandemics have always prompted a rethink about density. For example, throughout the 19th century, urban planners, such as Howard, sought to relocate their communities to suburbs and decentralize large industrial cities that were very polluted and hotspots of infectious diseases (Howard, 2013). Another example occurred during World War II when the severe damage caused by bombing large and densely populated cities prompted policymakers to decentralize activities away from big cities (Batty, 2020).
The outbreak of the COVID-19 pandemic has once again brought discussions regarding the desirability of high-density residential settlements to the fore. Since the beginning of this pandemic, doubts have arisen among urban planners about some concepts such as compact cities, smart growth, transportation-oriented development, and brownfield development (Batty, 2020). However, the findings of this study indicated that urban density could not be considered as inherently a risk factor for COVID-19, and post-COVID urban planning can take advantage of urban density while paying more emphasis on avoiding crowding.
Besides, the COVID-19 pandemic showed that living in a compact and transport-oriented city requires responsible citizens who pay attention to public health rules and regulations, because individual behaviors have a significant impact on community health and well-being (Budd & Ison, 2020). Indeed, what can turn densely populated cities into vulnerable areas is irresponsible behaviors. Furthermore, the post-COVID cities should be developed based on a neighborhood-oriented development pattern that can make cities more resilient against future pandemics. Such a compact and neighborhood-oriented pattern can also provide other socio-economic and environmental co-benefits. For instance, it can contribute to addressing issues related to climate change that is believed to be another major threat looming over cities (Sharifi, 2021).
Declaration of Competing Interest
The authors report no declarations of interest.
Footnotes
Interested readers are referred to Hoyle (2012) for more details about SEM.
Appendix A. High-resolution maps of infected and death cases
References
- Abate S.M., Ahmed Ali S., Mantfardo B., Basu B. Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: A systematic review and Meta-analysis. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0235653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almagro M., Orane-Hutchinson A. Covid economics: Vetted and real-time papers. 2020. The determinants of the differential exposure to COVID-19 in New York City and their evolution over time. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arab-Mazar Z., Sah R., Rabaan A.A., Dhama K., Rodriguez-Morales A.J. Mapping the incidence of the COVID-19 hotspot in Iran – Implications for Travellers. Travel Medicine and Infectious Disease. 2020;34:101630. doi: 10.1016/j.tmaid.2020.101630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty M. The Coronavirus crisis: What will the post-pandemic city look like? Environment and Planning B: Urban Analytics and City Science. 2020;47(4):547–552. doi: 10.1177/2399808320926912. [DOI] [Google Scholar]
- Bhadra A., Mukherjee A., Sarkar K. Impact of population density on Covid-19 infected and mortality rate in India. Modeling Earth Systems and Environment. 2020;7:623–629. doi: 10.1007/s40808-020-00984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bialek S., Boundy E., Bowen V., Chow N., Cohn A., Dowling N.…Sauber-Schatz E. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boterman W.R. Urban‐rural polarisation in times of the corona outbreak? The early demographic and geographic patterns of the SARS‐CoV‐2 epidemic in the Netherlands. Tijdschrift Voor Economische En Sociale Geografie. 2020;111(3):513–529. doi: 10.1111/tesg.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budd L., Ison S. Responsible Transport: A post-COVID agenda for transport policy and practice. Transportation Research Interdisciplinary Perspectives. 2020;6 doi: 10.1016/j.trip.2020.100151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton E., Jenks M., Williams K. Routledge; 2003. The compact city: A sustainable urban form? [Google Scholar]
- Carter E.D. Pandemic: Tracking Contagions, from Cholera to Ebola and Beyond; 2017. The AAG review of books. [DOI] [Google Scholar]
- Cordes J., Castro M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spatial and Spatio-Temporal Epidemiology. 2020;34 doi: 10.1016/j.sste.2020.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coşkun H., Yıldırım N., Gündüz S. The spread of COVID-19 virus through population density and wind in Turkey cities. Science of the Total Environment. 2021;751 doi: 10.1016/j.scitotenv.2020.141663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalziel B.D., Kissler S., Gog J.R., Viboud C., Bjørnstad O.N., Metcalf C.J.E., Grenfell B.T. Urbanization and humidity shape the intensity of influenza epidemics in U.S. cities. Science. 2018;362(6410):75–79. doi: 10.1126/science.aat6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das A., Ghosh S., Das K., Basu T., Dutta I., Das M. Living environment matters: Unravelling the spatial clustering of COVID-19 hotspots in Kolkata megacity, India. Sustainable Cities and Society. 2021;65 doi: 10.1016/j.scs.2020.102577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Haas M., Faber R., Hamersma M. How COVID-19 and the Dutch ‘intelligent lockdown’ change activities, work and travel behaviour: Evidence from longitudinal data in the Netherlands. Transportation Research Interdisciplinary Perspectives. 2020;6 doi: 10.1016/j.trip.2020.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federgruen A., Naha S. Crowding effects dominate demographic attributes in COVID-19 cases. International Journal of Infectious Diseases. 2021;102:509–516. doi: 10.1016/j.ijid.2020.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch W.H., Hernández Finch M.E. Poverty and Covid-19: Rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Frontiers in Sociology. 2020;15:1–10. doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace J.B. Structural equation modeling for observational studies. Journal of Wildlife Management. 2008;72(1):14–22. doi: 10.2193/2007-307. [DOI] [Google Scholar]
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J.…Zhong N. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020;58(4):711–712. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? Journal of the American Planning Association. 2020;86(4):495–509. doi: 10.1080/01944363.2020.1777891. [DOI] [Google Scholar]
- Howard E. Garden cities of to-morrow. 2013. Garden cities of To-morrow. [DOI] [Google Scholar]
- Hoyle R.H. Guilford press; 2012. Handbook of structural equation modeling. [Google Scholar]
- Hua J., Zhang X., Ren C., Shi Y., Lee T.-C. Spatiotemporal assessment of extreme heat risk for high-density cities: A case study of Hong Kong from 2006 to 2016. Sustainable Cities and Society. 2021;64 doi: 10.1016/j.scs.2020.102507. [DOI] [Google Scholar]
- Imdad K., Sahana M., Rana M.J., Haque I., Patel P.P., Pramanik M. A district-level susceptibility and vulnerability assessment of the COVID-19 pandemic’s footprint in India. Spatial and Spatio-Temporal Epidemiology. 2021;36 doi: 10.1016/j.sste.2020.100390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labour Organization . Tackling vulnerability in the informal economy. OECD Publishing; 2019. Protecting informal economy workers and their dependents. [Google Scholar]
- Jamshidi S., Baniasad M., Niyogi D. Global to USA county scale analysis of weather, urban density, mobility, homestay, and mask use on COVID-19. International Journal of Environmental Research and Public Health. 2020;17(21):7847. doi: 10.3390/ijerph17217847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin J.M., Bai P., He W., Wu F., Liu X.F., Han D.M.…Yang J.K. Gender differences in patients with COVID-19: Focus on severity and mortality. Frontiers in Public Health. 2020;8:1–6. doi: 10.3389/fpubh.2020.00152. 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissler S.M., Gog J.R., Viboud C., Charu V., Bjørnstad O.N., Simonsen L., Grenfell B.T. Geographic transmission hubs of the 2009 influenza pandemic in the United States. Epidemics. 2019;26:86–94. doi: 10.1016/j.epidem.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Kodera S., Rashed E.A., Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. International Journal of Environmental Research and Public Health. 2020;17(15):5477. doi: 10.3390/ijerph17155477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutela B., Novat N., Langa N. Exploring geographical distribution of transportation research themes related to COVID-19 using text network approach. Sustainable Cities and Society. 2021;67 doi: 10.1016/j.scs.2021.102729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Peng Y., He H., Wang M., Feng T. Built environment and early infection of COVID-19 in urban districts: A case study of Huangzhou. Sustainable Cities and Society. 2021;66 doi: 10.1016/j.scs.2020.102685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C., Lau A.K.H., Fung J.C.H., Guo C., Chan J.W.M., Yeung D.W., Zhang Y., Bo Y., Hossain M.S., Zeng Y., Lao X.Q. A mechanism-based parameterisation scheme to investigate the association between transmission rate of COVID-19 and meteorological factors on plains in China. Science of the Total Environment. 2020;737 doi: 10.1016/j.scitotenv.2020.140348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: Evidence from China. Cities. 2020;103:102759. doi: 10.1016/j.cities.2020.102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Su Y. Federal Reserve Bank of Dallas; 2020. The impact of the COVID-19 pandemic on the demand for density: Evidence from the U.S. Housing market. https://www.dallasfed.org/-/media/documents/research/papers/2020/wp2024r1.pdf Working Papers. [Google Scholar]
- Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. Journal of Infection. 2020 doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiti A., Zhang Q., Sannigrahi S., Pramanik S., Chakraborti S., Cerda A., Pilla F. Exploring spatiotemporal effects of the driving factors on COVID-19 incidences in the contiguous United States. Sustainable Cities and Society. 2021;68 doi: 10.1016/j.scs.2021.102784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansour S., Al Kindi A., Al-Said A., Al-Said A., Atkinson P. Sociodemographic determinants of COVID-19 incidence rates in Oman: Geospatial modelling using multiscale geographically weighted regression (MGWR) Sustainable Cities and Society. 2021;65 doi: 10.1016/j.scs.2020.102627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustainable Cities and Society. 2020;61:102350. doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghadasi A.N. Opportunities and threats: The necessity of research in dealing with the rapid spread of coronavirus disease 2019 (COVID-19) in Iran. Archives of Clinical Infectious Diseases. 2020;15(COVID-19) doi: 10.5812/archcid.102809. [DOI] [Google Scholar]
- Nguimkeu P., Tadadjeu S. Why is the number of COVID-19 cases lower than expected in Sub-Saharan Africa? A cross-sectional analysis of the role of demographic and geographic factors. World Development. 2021;138 doi: 10.1016/j.worlddev.2020.105251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pafka E. The Conversation; 2020. As coronavirus forces us to keep our distance, city density matters less than internal density.https://theconversation.com/as-coronavirus-forces-us-to-keep-our-distance-city-density-matters-less-than-internal-density-137790 [Google Scholar]
- Perone G. The determinants of COVID-19 case fatality rate (CFR) in the Italian regions and provinces: An analysis of environmental, demographic, and healthcare factors. Science of the Total Environment. 2021;755 doi: 10.1016/j.scitotenv.2020.142523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourghasemi H.R., Pouyan S., Heidari B., Farajzadeh Z., Fallah Shamsi S.R., Babaei S., Khosravi R., Etemadi M., Ghanbarian G., Farhadi A., Safaeian R., Heidari Z., Tarazkar M.H., Tiefenbacher J.P., Azmi A., Sadeghian F. Spatial modeling, risk mapping, change detection, and outbreak trend analysis of coronavirus (COVID-19) in Iran (days between February 19 and June 14, 2020) International Journal of Infectious Diseases. 2020;98:90–108. doi: 10.1016/j.ijid.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren H., Zhao L., Zhang A., Song L., Liao Y., Lu W., Cui C. Early forecasting of the potential risk zones of COVID-19 in China’s megacities. Science of the Total Environment. 2020;729(January) doi: 10.1016/j.scitotenv.2020.138995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz Estrada M.A. How COVID-19 Quarantine(s) Can Generate Poverty? SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3580703. [DOI] [Google Scholar]
- Schumacker R.E., Lomax R.G. Routledge; New York: 2010. A beginner’s guide to structural equation modelling. [Google Scholar]
- Shah S. The Atlantic; 2016. How cities shape epidemics like Zika and Ebola. [Google Scholar]
- Sharifi A. Co-benefits and synergies between urban climate change mitigation and adaptation measures: A literature review. Science of the Total Environment. 2021;750 doi: 10.1016/j.scitotenv.2020.141642. [DOI] [PubMed] [Google Scholar]
- Sharifi A., Khavarian-Garmsir A.R. Vol. 749. Elsevier B.V.; 2020. The COVID-19 pandemic: Impacts on cities and major lessons for urban planning, design, and management. (Science of the total environment). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistical Center of Iran . Statistical center of iran. Strategic Planning and Supervision, Statistical Centre of Iran; 2016. National population and housing census 2016. [Google Scholar]
- Statistics Center of Iran . Statistics Center of Iran; 2016. Statistical yearbook of Tehran. [Google Scholar]
- Stevenson M., Thompson J., de Sá T.H., Ewing R., Mohan D., McClure R.…Sun X. Land use, transport, and population health: Estimating the health benefits of compact cities. The Lancet. 2016;388(10062):2925–2935. doi: 10.1016/S0140-6736(16)30067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J., He X., Qing L., Niu T., Cheng Y., Peng Y. A novel social distancing analysis in urban public space: A new online spatio-temporal trajectory approach. Sustainable Cities and Society. 2021;68 doi: 10.1016/j.scs.2021.102765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Z., Zhang H., Yang Y., Wan H., Wang Y. Impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China. Science of the Total Environment. 2020;746 doi: 10.1016/j.scitotenv.2020.141347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarka P. An overview of structural equation modeling: Its beginnings, historical development, usefulness and controversies in the social sciences. Quality & Quantity. 2018;52(1):313–354. doi: 10.1007/s11135-017-0469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tehran municipality . Tehran Municipality Publications; 2016. Atlas of Tehran Metropolis. [Google Scholar]
- Valizadeh J., Hafezalkotob A., Seyed Alizadeh S.M., Mozafari P. Hazardous infectious waste collection and government aid distribution during COVID-19: A robust mathematical leader-follower model approach. Sustainable Cities and Society. 2021;69 doi: 10.1016/j.scs.2021.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. COVID-19: The gendered impacts of the outbreak. Lancet. 2020;395:846–847. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine. 2020;27(2) doi: 10.1093/jtm/taaa020. taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You H., Wu X., Guo X. Distribution of covid-19 morbidity rate in association with social and economic factors in Wuhan, China: Implications for urban development. International Journal of Environmental Research and Public Health. 2020;17(10):3417. doi: 10.3390/ijerph17103417. [DOI] [PMC free article] [PubMed] [Google Scholar]