Prolonged use of screens has previously been shown to increase symptoms of dry eye disease (DED) [1]. Although this relationship in adults has been well-studied, few studies have examined this relationship in pediatrics and none have assessed the effects of the COVID-19 pandemic—and its associated increase in screen time—on DED in children [2,3]. The purpose of this study was to determine the effect of the COVID-19 pandemic on screen time (ST) and its relationship with DED symptoms in children using a modified SPEED questionnaire (m-SPEED).
This was a cross-sectional study performed at pediatric ophthalmology clinics at two different institutes in Egypt (Benha University and Research Institute of Ophthalmology) between December 2020 and the end of March 2021. The study was approved by the ethics committees of Benha University Hospitals and Research Institute of Ophthalmology and adhered to the tenets of the Declaration of Helsinki.
Children aged 10–18 years old were eligible for the study. Children with developmental delay, corneal disease, or childhood glaucoma were excluded. M-SPEED questionnaires translated into Arabic were given to children and their parents. Informed consent was obtained from the legal guardian of each child included in the study. Questionnaires evaluated the frequency and severity of different DED symptom clusters and ST before and after March 2020 which represents the onset of the COVID-19 lockdowns (CL) in Egypt.
Data was analyzed using SPSS (version 26). A paired two-sample t-test was used to compare the total m-SPEED score, total ST, ST for education, and ST for leisure before and after the CL. Pearson's correlation was used to examine the associations between the post-lockdown m-SPEED score and different risk factors. Regression analyses were used to assess risk and protective factors underlying the post-CL m-SPEED score and the four dry eye symptom clusters of the m-SPEED questionnaire. P values less than 0.05 were considered statistically significant.
The study included 403 subjects with a mean age of 12.7 ± 1.9 years (range 10–18) who presented to the outpatient pediatric ophthalmology clinic. 50.4 % of patients were male. 89.6 % of the questionnaires were filled out by a parent and 10.4 % were filled out by the patient under parental supervision. 59.6 % of patients had an urban residence, while 40.4 % were living in rural areas. The most frequent current symptom was eye fatigue followed by dryness/grittiness/scratchiness, then burning/watering, and lastly, soreness/irritation. 16.6 % of the patients reported current use of artificial tears.
The total m-SPEED questionnaire score increased significantly after March 2020 (3.9 ± 4.53) compared to pre-COVID-19 scores (0.83 ± 2.04) (P < 0.001). Similarly, the ST for both education and leisure also increased significantly, with a mean difference of 1.06 ± 1.5 and 1.39 ± 2.04 h per day, respectively (P<0.001).
Mean total ST was not significantly different between those living in rural vs urban areas during both the pre- and post-CL (P = 0.6, and 0.17, respectively). When divided into leisure and educational, educational ST was significantly higher in those living in urban areas (P < 0.001) with a mean difference of 0.95 ± 0.2 h per day. The mean m-SPEED questionnaire score post-CL was significantly higher among those living in urban areas (4.68 ± 4.87) compared to those living in rural areas (2.97 ± 3.69) (P<0.001).
The m-SPEED score post-CL was significantly higher in males (4.54 ± 4.87) compared to females (3.44 ± 4.04, P = 0.019). Male sex was associated with greater ST with a mean difference of 0.6 ± 0.31 h per day (P=0.047).
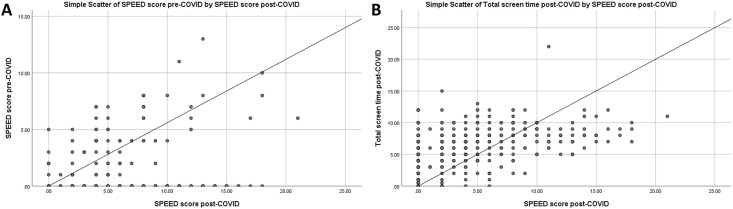
The post-CL m-SPEED score had moderate positive correlations with the pre-COVID-19 m-SPEED score and total ST (R = 0.3, P < 0.001; R = 0.473, P < 0.001, Fig. 1 ). There was no correlation between age and post-CL m-SPEED and total ST (P=0.8, and 0.07, respectively).
Fig. 1.
Scatter plots showing significant positive correlations between post-COVID lockdown SPEED score and A) Pre-COVID SPEED score (R = 0.3, P < 0.001), and B) the total screen time (R = 0.473, P < 0.001).
Multivariate linear regression analysis revealed that 25.3 % of the m-SPEED score after CL could be predicted by total ST and the pre-COVID-19 m-SPEED score (P < 0.001).
The purpose of this study was to determine the effect of increased ST on pediatric DED using m-SPEED questionnaire pre- and post-CL. In March 2020, many countries shut down their schools due to COVID-19, affecting approximately 862 million children with a subsequent increase in digital device usage [4]. A previous study demonstrated that students increased their ST by an average of approximately 5 h per day [5]. Our study further supports the finding of increased ST use post CL.
Increased ST has been associated with increased DED symptoms. Our study found that, compared to pre-CL, the total m-SPEED questionnaire score increased significantly. While no previous studies have evaluated this in children in the context of COVID-19, this finding supports the results of previous studies that have investigated the role of increased ST on DED [2,3].
Several factors have been proposed to explain the development of DED symptoms in association with prolonged ST [3]. One theory posits that increased ST reduces the blink rate which in turn leads to loss of tear film homeostasis. Additionally, increased ST has been associated with a higher incidence of meibomian gland dysfunction with meibomian gland dropout [3]. The Osaka Study previously demonstrated that excessive ST may induce goblet cell dysfunction and decreased mucin production [6].
We found a significant increase in both leisure and educational ST post-CL, consistent with previous reports [3]. We found that educational ST was significantly less in those living in rural areas compared to urban areas. Multivariate logistic regression also demonstrated that rural residence correlated with reduced rates of the DED symptoms, consistent with previous reports [2]. Multiple socioeconomic and behavioral variables likely account for differences in ST and DED symptoms in every symptom cluster between children living in urban vs. rural areas.
The post-CL m-SPEED score had positive correlations with the pre-COVID-19 m-SPEED score and total ST. It may be that increased ST during CL was the catalyst for the development or progression of DED in eyes already prone to developing it. Although DED has been shown to be more prevalent in females than males in adults, our pediatric study showed greater ST and increased rates DED symptoms in males [2]. Though screen time is only one variable in the risk of DED, in this population it is a significant one. It may be that screen time use equalizes between males and female as they age and, with the introduction of other variables, alters the male/female prevalence of DED. Alternatively, adolescent females may be less likely to subjectively report symptoms of DED, despite having more clinical signs of DED compared to males of a similar age [7].
Our study has limitations. Parents and participants may have recall bias as to what symptoms they were experiencing at various timepoints. Additionally, children may have difficulty expressing their symptoms to parents. Nevertheless, the large sample size allows for meaningful conclusions to be made that can be generalized to other populations. It is also the first study to assess the effects of the COVID-19 pandemic on DED in children. The long-term consequences need to be longitudinally studied once school systems transition back to full-time in-person learning.
In conclusion, this study suggests that increased ST in children during the COVID-19 pandemic can contribute to symptoms of DED with potential negative impact on their ocular health. Increased ST is likely to continue to some degree even after resumption of in-person school, and it behooves us to understand its effects on children.
Funding
None.
Declaration of competing interest
The authors AME, TKE. MSY, JG, RHE, AH, JTK, IAE, SMAS, OS, HNS declare no relevant disclosures or potential conflicts of interest.
References
- 1.Elhusseiny A.M., Khalil A.A., El Sheikh R.H., Bakr M.A., Eissa M.G., El Sayed Y.M. New approaches for diagnosis of dry eye disease. Int J Ophthalmol. 2019;12(10):1618–1628. doi: 10.18240/ijo.2019.10.15. [published Online First: Epub Date] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Golebiowski B., Long J., Harrison K., Lee A., Chidi-Egboka N., Asper L. Smartphone use and effects on tear film, blinking and binocular vision. Curr Eye Res. 2020;45(4):428–434. doi: 10.1080/02713683.2019.1663542. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 3.Mehra D., Galor A. Digital screen use and dry eye: a review. Asia Pac J Ophthalmol (Phila) 2020;9(6):491–497. doi: 10.1097/apo.0000000000000328. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 4.Viner R.M., Russell S.J., Croker H., et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. The Lancet Child & Adolescent Health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bahkir F.A., Grandee S.S. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68(11):2378–2383. doi: 10.4103/ijo.IJO_2306_20. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchino Y., Uchino M., Yokoi N., et al. Alteration of tear mucin 5AC in office workers using visual display terminals: the Osaka Study. JAMA Ophthalmol. 2014;132(8):985–992. doi: 10.1001/jamaophthalmol.2014.1008. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 7.Ayaki M., Kawashima M., Uchino M., et al. Gender differences in adolescent dry eye disease: a health problem in girls. Int J Ophthalmol. 2018;11(2):301–307. doi: 10.18240/ijo.2018.02.20. [DOI] [PMC free article] [PubMed] [Google Scholar]