Abstract
Background
Restricted access to hospitals due to the 2019 novel coronavirus disease (COVID-19) pandemic has significantly altered practice patterns for elective neurosurgical care. Particularly, telemedicine has become the primary modality of patient visits for nonemergent conditions. This study aimed to characterize user experiences of neurosurgeons and advanced practice providers focusing on perceived utility and barriers of telemedicine in management of elective neurosurgical patients during COVID-19.
Methods
An online survey was sent to clinicians involved in neurosurgical care using telemedicine with questions focusing on frequency of utilization, duration of patient encounters, benefits of telemedicine, and barriers to current forms of remote patient visits. Survey responses were stratified by clinical position (neurosurgeon vs. advanced practice provider) and subspecialty focus (cranial vs. spinal neurosurgery).
Results
The survey was completed by 14 of 17 eligible clinicians. Respondents included 10 neurosurgeons and 4 APPs with 57% specializing in cranial neurosurgery and 43% specializing in spinal neurosurgery. During the COVID-19 period, 78% of respondents used teleconference/video conference visits multiple times in a week, and 86% planned to continue using telemedicine after the pandemic. The most common barrier for telemedicine was the inability to perform a neurological examination, while the most common perceived benefit was increased convenience for patients.
Conclusions
During the COVID-19 period, telemedicine was heavily relied on to ensure the continuation of perioperative care for patients with elective neurosurgical pathologies. While clinicians identified numerous barriers for current telemedicine platforms, the use of telemedicine will likely continue, as it has provided unique benefits for patients, clinicians, and hospitals.
Key words: COVID-19, Neurosurgery, Telemedicine, User experience
Abbreviations and Acronyms: APP, Advanced practice provider; COVID-19, 2019 novel coronavirus disease
Introduction
The use of telemedicine has significantly increased in the last decade with nearly 76% of hospitals in the United States now implementing virtual health care by ways of videoconferencing, remote monitoring, electronic consultations, and wireless communications.1 In parallel with this trend, hundreds of clinical studies have examined the efficacy and utility of telemedicine.2 , 3 Global adoption of mobile technology has further supported the expansion of telemedicine and the development of novel telemedicine applications.4 The 2019 novel coronavirus disease (COVID-19) pandemic has significantly altered the access to health care as conventional in-person evaluations were restricted to emergencies only. This unforeseen crisis necessitated the implementation of telemedicine as the primary modality of patient care across various medical and surgical specialties, including neurosurgical care.
The dependence on telemedicine is new for many clinicians treating neurosurgical patients who would have otherwise been evaluated in an outpatient clinic setting. This likely stems from the fact that the management of neurosurgical pathologies often relies on subtle physical examination findings and involves in-depth discussion with patients. However, as the use of telemedicine becomes integrated into the standard of care, it is essential to understand the strengths and limitations of this technology by examining the end-user experience. The objective of this study was to characterize the experiences of neurosurgeons and advanced practice providers (APPs) with telemedicine, specifically focusing on the perceived utility and barriers of telemedicine in the management of patients receiving elective neurosurgical care.
Materials and Methods
Study Setting and Participants
This was a single-center, cross-sectional study. An online survey with a cover letter stating the study objective was sent to neurosurgeons and APPs at a tertiary care institution. Health care providers who provided neurosurgical care using telemedicine platforms during the COVID-19 period were eligible to participate in the survey. For this study, telemedicine platforms included any electronic communication tools that facilitated long-distance patient encounters, such as teleconference, video conference, e-mails, web-based communications, and direct messaging.5 Three neurosurgery APPs were deployed to other hospital services for COVID-19 response and thus were not actively involved in neurosurgical care during the study period. The Institutional Research Ethics Board approved this research study with the participants providing electronic consent before completing the survey.
Survey Design
The online survey included questions on clinical role, subspecialty focus, and types of telemedicine platform used (Table 1 ). Specific questions regarding teleconference/video conference were asked including the frequency of utilization, duration of patient encounters, and barriers to current forms of teleconference/video conference. The survey questions were derived from previously published studies on telemedicine along with discussion between the authors.6 , 7 The survey design was further modified to collect qualitative data by incorporating multiple comment sections if the categorical options did not include suitable answers. The responses were collected anonymously and stratified by clinical position (neurosurgeon vs. APP) and subspecialty focus (cranial neurosurgery vs. spinal neurosurgery).
Table 1.
User Experience of Telemedicine Survey
| Questions | Response |
|---|---|
| 1. What is your clinical position? |
|
| 2. What is your subspecialty focus? |
|
| 3. Which type(s) of eHealth platforms do you use? (Select all that apply.) |
|
| 4. What hardware devices do you use for video/telemedicine visits? (Select all that apply.) |
|
| 5. On average, how often did you do video/telemedicine visits before the current COVID-19 period? |
|
| 6. On average, how often are you doing video/telemedicine visits currently during the COVID-19 period? |
|
| 7. What is the purpose of the video/telemedicine visits? (Select all that apply.) |
|
| 8. On average, how long do your video/telephone visits usually take? |
|
| 9. How do you think the time for a video/telemedicine visit compares with an in-office visit? |
|
| 10. What is your perception of the quality of care with video/telemedicine visits? |
|
| 11. What do you perceive as challenges with video/telemedicine visits? (Select all that apply.) |
|
| 12. What do you perceive as benefits of video/telemedicine visits? (Select all that apply.) |
|
| 13. Do you plan to use video/telemedicine visits next year? |
|
| 14. What kind of video/telemedicine support is at your workplace? |
|
APP, advanced practice provider; EMR, electronic medical record; IT, information technology.
Statistical Analysis
Descriptive statistics were used to examine the respondents’ answers to the survey questions. The responses were grouped based on clinical position (neurosurgeon vs. APP). Comparative analysis was done using Fisher exact test for categorical variables. A P value <0.05 was set as statistically significant. Statistical analyses were performed using STATA 14.3 (StataCorp LLC, College Station, Texas, USA).
Results
Of 17 eligible clinicians, 14 completed the survey (74% response rate). This included 10 neurosurgeons and 4 APPs with 57% (8 of 14) specializing in cranial neurosurgery and 43% (6 of 14) specializing in spinal neurosurgery. There was no difference in the distribution of clinical roles (neurosurgeon vs. APP) and subspecialty focus of the respondents (P > 0.05). Before the COVID-19 period, 85% of participants did not use any form of teleconference or video conference. One participant noted using teleconference on a monthly basis, while another reported using teleconference in the context of a research project.
User Experience During COVID-19 Period
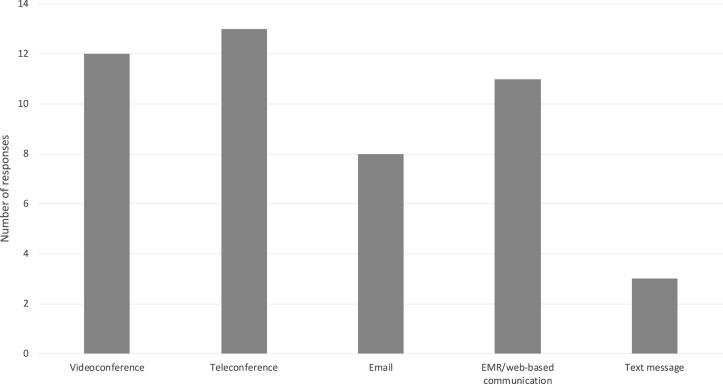
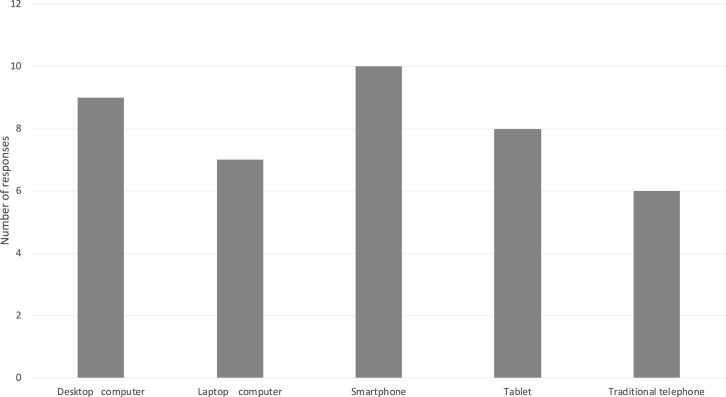
During the COVID-19 period, 78% of respondents used teleconference/video conference visits multiple times in a week, and 14% participated in daily teleconference/video conference visits. In terms of the telemedicine platforms used, the most commonly used forms of communication were teleconference followed by video conference (Figure 1 ). However, the majority of respondents used multiple telemedicine platforms, including e-mails, text messages, and electronic medical record/web-based communications. Multiple hardware devices were used to communicate with patients, with smartphones and desktop computers being the most frequently used devices (Figure 2 ).
Figure 1.
Types of telemedicine platforms used. EMR, electronic medical record.
Figure 2.
Types of devices used for telemedicine platforms.
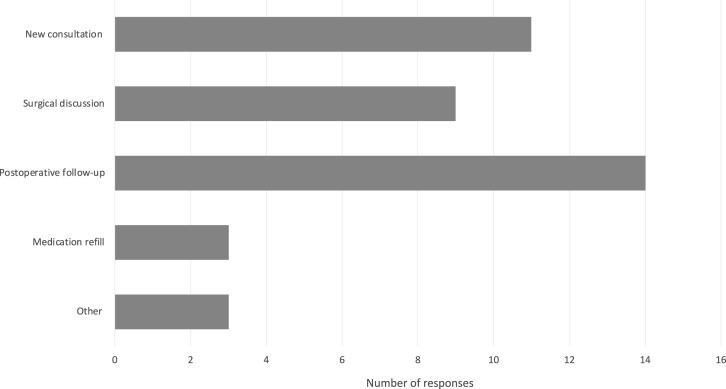
The teleconference/video conference visits were used most commonly for postoperative follow-up. New consultation and surgical discussion were also frequent reasons for teleconference or video conference visits (Figure 3 ). The duration of teleconference or video conference visits ranged from <15 minutes to approximately 30–60 minutes with 78% of participants reporting 15–30 minutes per visit. Compared with in-person visits, 71% thought that teleconference or video conference visits were shorter; only 1 respondent thought it took longer (Table 2 ). Of the 14 participants, 10 thought that teleconference/video conference visits were inferior to traditional in-person visits (Table 2). Even with the numerous limitations and barriers, 12 of 14 respondents planned to continue using teleconference/video conference visits after COVID-19 restrictions are lifted. The distribution of clinicians who planned to continue using teleconference/video conference visits versus clinicians who planned to stop did not differ based on subspecialty focus (cranial neurosurgery vs. spinal neurosurgery, P = 0.1648).
Figure 3.
Purpose of teleconference/video conference visits. Other reasons were routine follow-up visits and implanted device checks.
Table 2.
User Perception of Time Consumption and Quality of Care of Teleconference and Video Conference Compared with In-Person Visits
| Neurosurgeons (n = 10) | APPs (n = 4) | |
|---|---|---|
| Duration of teleconference/video conference visits? | <15 minutes: 2 | <15 minutes: 0 |
| 15–30 minutes: 8 | 15–30 minutes: 3 | |
| 30–60 minutes: 0 | 30–60 minutes: 1 | |
| >60 minutes: 0 | >60 minutes: 0 | |
| Perceived time consumption compared with in-person visit? | Shorter: 7 | Shorter: 3 |
| Equivalent: 3 | Equivalent: 0 | |
| Longer: 0 | Longer: 1 | |
| Quality of care compared with in-person visit? | Superior: 0 | Superior: 0 |
| Equivalent: 3 | Equivalent: 1 | |
| Inferior: 7 | Inferior: 3 |
Strengths and Limitations of Teleconference/Video Conference
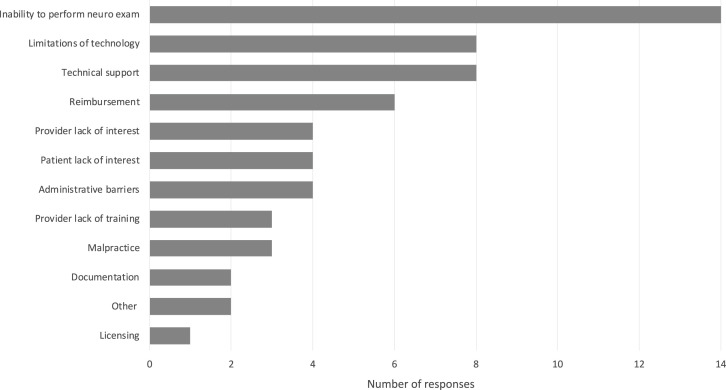
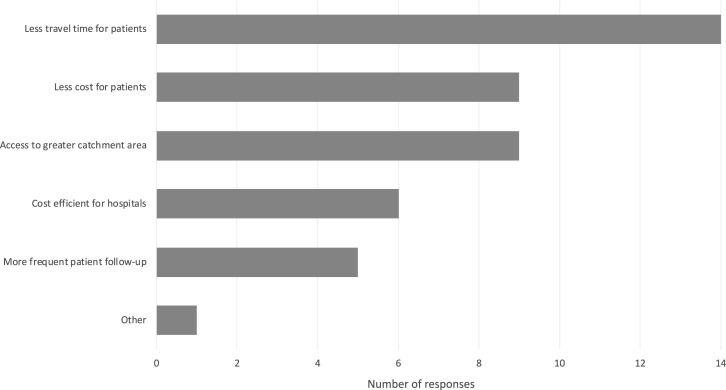
The clinicians perceived numerous challenges to current teleconference/video conference visits. Uniformly, all surgeons and APPs noted the inability to perform a neurological examination as a limitation compared with in-person visits. Furthermore, multiple neurosurgeons raised the concern of being able to establish a meaningful rapport with patients through telemedicine. In particular, discussing a potentially life-altering diagnosis and treatment plan with major risks requires a level of trust and sense of empathy that is challenging to achieve remotely. In such cases, surgeons felt the need to schedule an in-person clinic visit following the telemedicine encounter. Concerning the technical barriers, surgeons reported challenges in accessing patient imaging during the virtual encounters if the scans were performed in other institutions or the patients failed to mail the hard copy in time. Even with accessible imaging, some surgeons found reviewing them with the patients over video conference was challenging, especially ensuring that patients understood both the images and the didactic information. This challenge can be further amplified when dealing with inconsistent video and audio connections along with patients who are unfamiliar with digital communication technology. Other common barriers included the uncertainty of reimbursement and lack of technical support (Figure 4 ). The perceived strengths of teleconference/video conference visits included increased convenience for patients, less cost for patients, improved access for surgeons to a broader catchment area, and cost savings for hospitals (Figure 5 ). For the teleconference/video conference visits, 93% of respondents relied on clinical support staff as their technical support compared with 64% using the information technology help desk. One respondent reported not having sufficient technical support.
Figure 4.
Barriers to current teleconference/video conference visits. Other reasons included the inability to do implanted device programing and technical challenges for elderly patients. neuro exam, neurological examination.
Figure 5.
Perceived benefits of teleconference/video conference visits. Other reason was improved access for disabled patients.
Discussion
The sudden cessation of in-person clinic visits as a result of the COVID-19 pandemic has forced patients and health care providers to rapidly adopt telemedicine as the primary avenue to continue perioperative patient management. Although there was a growing interest in telemedicine before COVID-19, its routine use within the field of neurosurgery was previously limited.8 The results of this study highlight that telemedicine was heavily used during the COVID-19 restriction period, but there were numerous concerns and perceived barriers with the current implementation setup as noted by the clinicians. While most respondents plan to continue using telemedicine in the future, addressing these barriers will be crucial to realizing the benefits of this technology as an adjunct tool for enhancing the quality of care for neurosurgical patients.
As the health care system continues to expand digital and long-distance patient encounters, broader changes in personal communication technology may influence the user experience of telemedicine. For example, the increasing variety of communication devices and their technical capability are major drivers for changes in telemedicine setup and implementation. In 2019, an estimated 81% of people in the United States owned a smartphone, and tablet use increased from 3% in 2010 to 52%.9 The survey results presented here demonstrated a similar trend with a broad range of devices employed for telemedicine during the COVID-19 period (Figure 2). Smartphones were the most widely used devices; this likely can be attributed to the long battery life and mobility while providing access to all telemedicine platforms as shown in Figure 1. Although the advantages of smartphone use are easily acknowledged, handheld devices can be nausea provoking and are susceptible to connectivity issues with inconsistent cellular services.10 Furthermore, the use of personal communication devices poses potential risks related to data security and confidentiality.11 Desktop computers are widely available and provide reliable internet connectivity within the secure hospital network. However, hospital computers often require modifications for telemedicine, such as installing a camera and linking audio input to the telemedicine software. During the initial implementation phase, this required frequent information technology troubleshooting, which delayed start times with patient visits and became a major deterrent for video conferences (Figure 4). In fact, numerous clinicians either reverted to using traditional telephones or transitioned to tablets if video conference was required.
Benefits of Telemedicine
The ability to evaluate postoperative patients was noted to be the most frequent and most impactful use of telemedicine service in the survey. Several crucial elements are involved in the postoperative visit, including the ability to visualize the surgical wound and ensuring that the patient can sufficiently convey their concerns. A prospective study demonstrated the effectiveness of triaging and managing postoperative patients following a lumbar discectomy using a mobile app.12 Both the number of calls to the primary care physician and the number of emergency department visits decreased.12 Additionally, given the available mobile apps for patient-reported outcome surveys, pain severity, and medication consumption, patients can provide useful metrics of postoperative progress that can be easily tracked by clinicians.13 , 14 The combination of telemedicine platforms may mitigate the loss of follow-up for patients with disabilities, patients with lack of access to transportation, and patients who relocated after surgery. An important requirement in successfully implementing such a multimodal system of telemedicine is ensuring ease of use for patients with varying age, socioeconomic status, education, and computer literacy.11
All but one of the survey respondents reported teleconference/video conference duration to be either the same or shorter than in-person visits. This is a shared finding in telemedicine visits across other specialties.10 The use of teleconference/video conference offers an opportunity for a more focused conversation, such as triaging of surgical consultations, supplemental surgical discussion, or routine follow-up care. This, in turn, has the potential improvement in cost-efficiency for hospitals and patients with a reduction in the number of in-person visits to those deemed clinically necessary.8 , 15 Additionally, it provides the opportunity for the hospital to engage in a larger catchment area as noted by the survey results.
Newer telemedicine platforms allow visual assessment of wounds and review of radiology imaging via a share screen function not previously possible with traditional telephone conversations. These advances in telemedicine functionality along with the elimination of inconveniences associated with in-person visits may lead to greater patient satisfaction. In a pilot study, Reider-Demer et al.16 reported 85% of patients preferred telemedicine visits after elective neurosurgery compared with traditional clinic visits.
Barriers for Telemedicine
The most common limitation of telemedicine noted by the survey respondents was the inability to perform a full neurological examination. This likely was a major contributing factor to the perception that telemedicine decreased the quality of care as outlined in Table 2. The role of the physical examination in management decisions may be uniquely important in neurosurgery, as studies in other medical specialties most commonly report technical difficulties and resistance to change as key barriers for health care providers.11 Studies have reported that in patients with neurosurgical emergencies, such as ischemic stroke or intracranial hemorrhage, remote consultation with radiographic imaging and simple neurological examination can reduce unnecessary transfers and provide specialty access to surgical patients.17 , 18 However, no study in the literature has outlined how to overcome this challenge for patients with elective cranial or spine pathologies. Relatable, but not neurosurgical-specific, attempts at evaluating the musculoskeletal examination have been reported in a limited number of studies in the physiatry literature.19 , 20 Common barriers to the physical examination component include the ability to clearly communicate instructions and the potential safety concerns involved in a patient independently ambulating with a primary neurological or musculoskeletal pathology. Additionally, these studies reported interrater agreement of 68%–83% between telemedicine assessments and in-person examinations.
The survey identified other challenges to telemedicine that were not previously emphasized in the literature. For example, surgeons reported concerns about the potential detrimental impact of telemedicine on patient-physician rapport. In a surgical specialty such as neurosurgery where life-altering diagnoses are made and surgical treatments often involve major risks, communication is essential to building trust between the patient and surgeon. Moreover, patients must trust and feel confident in the recommendations of the physician. For cases involving difficult decisions or complications, relaying compassion and empathy is essential to maintain this rapport with the patient. In fact, major predictors of postoperative satisfaction were patients’ perceptions that their health care providers tried to address their pain and feeling like they are heard.21 Owing to these concerns, participating surgeons reported the need to arrange in-person visits following the virtual encounters in cases of surgical consent or challenging decisions. While telemedicine will not replace in-person visits entirely, one of the strengths of telemedicine is providing multiple avenues of communication for patients so that the patient-physician rapport can be augmented by improving patients’ perception of access to health care.
Before the COVID-19 pandemic, telemedicine services were reimbursed only if these visits occurred in designated health clinic locations or were approved in certain rural communities. While temporary adjustments in reimbursement were made to facilitate the rapid implementation of remote patient visits, insurance coverage for telemedicine after the pandemic remains uncertain. In the survey, concerns about reimbursement were one of the main concerns of health care providers even during the COVID-19 period. Another significant barrier to the broader use of telemedicine is the potential for abuse and increased health care utilization.4 For example, patients can potentially seek an evaluation from multiple surgeons in a short amount of time even with nonsurgical pathologies. While this may empower the patient with management options, it can also lead to an excessive number of consultations in an already overused and high-demand specialty. Furthermore, patients may use this method to gain access to high-risk medications, such as narcotic prescriptions.
Future Research
New technologic advancements may be able to address a few of these concerns. For example, sensors embedded in smartphones allow mobile apps to measure gait, joint position, and range of motion of the neck.22 , 23 The increased integration of Bluetooth technology (Bluetooth SIG, Inc., Kirkland, Washington, USA) could provide an opportunity to link external tools with smartphones and telemedicine platforms to provide an automated collection of objective patient data. One such example is the electronic handgrip strength dynamometer device, which has been used to assess and compare preoperative and postoperative strength.24 , 25 While barriers for clinical use of these tools exist, such as the device cost, internet access, and ease of use, these devices can provide greater granularity in patient outcome by enabling closer monitoring of patient progress from home. Advancements in the use of telemedicine will occur by correlating and validating supplemental tools to the traditional neurological examination. Lastly, future studies incorporating administrative data, such as telemedicine visit volume and insurance reimbursement during the COVID-19 period, may provide additional insights into how telemedicine can be better used in the future.
Study Limitations
This study has numerous limitations. First, this was a single-center survey of clinicians involved in neurosurgical care. The generalizability of this finding may be limited based on both regional and institutional practice patterns. Furthermore, the limited sample size of this study limited the statistical analysis with the risk of being underpowered. We focused instead on descriptive analysis and characterizing the feedback that clinicians provided. However, by focusing on a single institution, we were able to capture a high response rate of 74% with a comprehensive distribution of cranial and spinal neurosurgeons along with APPs. Furthermore, we were able to engage with the clinicians to provide in-depth insights that they may not otherwise feel comfortable sharing. Second, we did not survey the patients for their user experience on telemedicine. As the successful implementation of this technology relies on buy-in from all stakeholders, the barriers for patients with neurosurgical pathologies are important to assess. However, this assessment was beyond the scope of the study objective, which was focused on identifying barriers and strengths from the clinicians’ perspective. While previous publications in telemedicine have reported on patient satisfaction and feedback with telemedicine, there has not been a study focused on the user experience of clinicians.12 , 26 Therefore, this study characterizes multiple barriers of telemedicine from the perspective of the clinicians that are unique and important to the continuing adoption of this communication tool. Lastly, this was a cross-sectional study with the survey distributed approximately 6 weeks after COVID-19 restrictions. The perceived challenges of telemedicine may have changed depending on the timing of the survey based on the learning curve of clinicians and hospital information technology support staff. As telemedicine becomes more integrated into the daily practices of clinicians, it will provide an opportunity to address current limitations and inefficiencies associated with the early adoption of novel technology. Even with the noted limitations, the findings of this study may provide useful insights for ensuring the optimization of telemedicine as an adjunct tool for patient communication.
Conclusions
During the COVID-19 period, telemedicine was heavily relied on to ensure the continuation of perioperative care for patients with elective neurosurgical pathologies. While clinicians identified numerous barriers for current telemedicine platforms, the use of telemedicine will likely continue as an adjunct tool for patient care, as it has provided unique benefits for patients, clinicians, and hospitals.
CRediT authorship contribution statement
Won Hyung A. Ryu: Conceptualization, Data curation, Writing - original draft, Writing - review & editing. Mena G. Kerolus: Conceptualization, Data curation, Writing - original draft, Writing - review & editing. Vincent C. Traynelis: Writing - original draft, Writing - review & editing, Supervision.
Acknowledgments
We thank the Rush University Department of Neurological Science Research team for their help in this study.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.American Hospital Association Fact sheet: telehealth. https://www.aha.org/system/files/2019-02/fact-sheet-telehealth-2-4-19.pdf Available at:
- 2.Wootton R. Twenty years of telemedicine in chronic disease management—an evidence synthesis. J Telemed Telecare. 2012;18:211–220. doi: 10.1258/jtt.2012.120219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deldar K., Bahaadinbeigy K., Tara S.M. Teleconsultation and clinical decision making: a systematic review. Acta Inform Med. 2016;24:286–292. doi: 10.5455/aim.2016.24.286-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorsey E.R., Topol E.J. State of telehealth. N Engl J Med. 2016;375:154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 5.HealthIT.gov What is telehealth? How is telehealth different from telemedicine? www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine Available at:
- 6.Rogove H.J., McArthur D., Demaerschalk B.M., Vespa P.M. Barriers to telemedicine: survey of current users in acute care units. Telemed J E Health. 2012;18:48–53. doi: 10.1089/tmj.2011.0071. [DOI] [PubMed] [Google Scholar]
- 7.Hassan A., Dorsey E.R., Goetz C.G., et al. Telemedicine use for movement disorders: a global survey. Telemed J E Health. 2018;24:979–992. doi: 10.1089/tmj.2017.0295. [DOI] [PubMed] [Google Scholar]
- 8.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 9.Pew Research Center Mobile fact sheet. https://www.pewresearch.org/internet/fact-sheet/mobile/ Available at:
- 10.Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage. 2020;60:e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott Kruse C., Karem P., Shifflett K., et al. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Debono B., Bousquet P., Sabatier P., et al. Postoperative monitoring with a mobile application after ambulatory lumbar discectomy: an effective tool for spine surgeons. Eur Spine J. 2016;25:3536–3542. doi: 10.1007/s00586-016-4680-4. [DOI] [PubMed] [Google Scholar]
- 13.Kim C.H., Chung C.K., Choi Y., et al. The usefulness of a mobile device-based system for patient-reported outcomes in a spine outpatient clinic. Spine J. 2016;16:843–850. doi: 10.1016/j.spinee.2016.02.048. [DOI] [PubMed] [Google Scholar]
- 14.Hou J., Yang R., Yang Y., et al. The effectiveness and safety of utilizing mobile phone-based programs for rehabilitation after lumbar spinal surgery: multicenter, prospective randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:e10201. doi: 10.2196/10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de la Torre-Díez I., López-Coronado M., Vaca C., et al. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health. 2015;21:81–85. doi: 10.1089/tmj.2014.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reider-Demer M., Raja P., Martin N., Schwinger M., Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41:497–501. doi: 10.1007/s10143-017-0878-0. [DOI] [PubMed] [Google Scholar]
- 17.Esteves L.A., Ribeiro A.T., Silva E.G.D., et al. Evaluation of safety, effectiveness and reproducibility of telemedicine for neurosurgical screening. Einstein (Sao Paulo, Brazil) 2019;17:eAO4609. doi: 10.31744/einstein_journal/2019AO4609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angileri F.F., Cardali S., Conti A., et al. Telemedicine-assisted treatment of patients with intracerebral hemorrhage. Neurosurg Focus. 2012;32:E6. doi: 10.3171/2012.1.FOCUS11356. [DOI] [PubMed] [Google Scholar]
- 19.Cottrell M.A., O’Leary S.P., Swete-Kelly P., et al. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract. 2018;38:99–105. doi: 10.1016/j.msksp.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 20.Peterson S., Kuntz C., Roush J. Use of a modified treatment-based classification system for subgrouping patients with low back pain: agreement between telerehabilitation and face-to-face assessments. Physiother Theor Pract. 2019;35:1078–1086. doi: 10.1080/09593985.2018.1470210. [DOI] [PubMed] [Google Scholar]
- 21.Levin J.M., Winkelman R.D., Tanenbaum J.E., et al. Key drivers of patient satisfaction in lumbar spine surgery. J Neurosurg Spine. 2018;28:586–592. doi: 10.3171/2017.10.SPINE17732. [DOI] [PubMed] [Google Scholar]
- 22.Pourahmadi M.R., Bagheri R., Taghipour M., Takamjani I.E., Sarrafzadeh J., Mohseni-Bandpei M.A. A new iPhone application for measuring active craniocervical range of motion in patients with non-specific neck pain: a reliability and validity study. Spine J. 2018;18:447–457. doi: 10.1016/j.spinee.2017.08.229. [DOI] [PubMed] [Google Scholar]
- 23.Rye Hanton C., Kwon Y.J., Aung T., et al. Mobile phone-based measures of activity, step count, and gait speed: results from a study of older ambulatory adults in a naturalistic setting. JMIR Mhealth Uhealth. 2017;5:e104. doi: 10.2196/mhealth.5090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee S.C., Wu L.C., Chiang S.L., et al. Validating the capability for measuring age-related changes in grip-force strength using a digital hand-held dynamometer in healthy young and elderly adults. Biomed Res Int. 2020;2020:6936879. doi: 10.1155/2020/6936879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Persson L.C., Moritz U., Brandt L., Carlsson C.A. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997;6:256–266. doi: 10.1007/BF01322448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilkinson J.R., Spindler M., Wood S.M., et al. High patient satisfaction with telehealth in Parkinson disease: a randomized controlled study. Neurol Clin Pract. 2016;6:241–251. doi: 10.1212/CPJ.0000000000000252. [DOI] [PMC free article] [PubMed] [Google Scholar]