Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has changed health care delivery across the United States. Few analyses have specifically looked at quantifying the financial impact of the pandemic on practicing neurosurgeons. A survey analysis was performed to address this need.
Methods
A 19-question survey was distributed to practicing neurosurgeons in the United States and its territories. The questions evaluated respondents’ assessments of changes in patient and procedural volume, salary and benefits, practice expenses, staffing, applications for government assistance, and stroke management. Responses were stratified by geographic region.
Results
The response rate was 5.1% (267/5224). Most respondents from each region noted a >50% decrease in clinic volume. Respondents from the Northeast observed a 76% decrease in procedure volume, which was significantly greater than that of other regions (P = 0.003). Northeast respondents were also significantly more likely to have been reassigned to nonneurosurgical clinical duties during the pandemic (P < 0.001). Most respondents also noted decreased salary and benefits but experienced no changes in overall practice expenses. Most respondents did not experience significant reductions in nursing or midlevel staffing. These trends were not significantly different between regions.
Conclusions
The COVID-19 pandemic has led to decreases in patient and procedural volume and physician compensation despite stable practice expenses. Significantly more respondents in the Northeast region noted decreases in procedural volume and reassignment to nonneurosurgical COVID-related medical duties. Future analysis is necessary as the pandemic evolves and the long-term clinical and economic implications become clear.
Key words: COVID-19, Finance, Pandemic, Socioeconomic
Abbreviations and Acronyms: AANS, American Association of Neurological Surgeons; COVID-19, Coronavirus disease 2019; CSNS, Council of State Neurosurgical Societies
Introduction
In December 2019, multiple cases of pneumonia with unknown origin were reported in Wuhan, Hubei, China, and genetic sequencing analyses implicated a novel coronavirus, termed 2019-nCoV.1 Rapid spread of coronavirus disease 2019 (COVID-19) led to rising case rates and death counts in the United States.2, 3, 4 Cardiopulmonary and neurological complications contribute to the condition’s morbidity and mortality.5, 6, 7, 8
To curb the spread of the pathogen, individual states instituted social distancing measures, limited public and business gatherings, limited elective health care procedures, and issued shelter-in-place orders. While these strategies decreased community spread of the virus,9 , 10 they also resulted in myriad socioeconomic repercussions. Shelter-in-place orders substantially reduced outpatient medical care volume, and >60,000 health care jobs were lost in the initial months of the pandemic.11 Expanded availability of telehealth services and government assistance programs ameliorated some of these losses11; however, the emerging economic consequences of the COVID-19 pandemic are largely undefined. Specifically, minimal data exist to evaluate the financial effects of the COVID-19 pandemic on neurosurgery practice in the United States. To this end, the authors present the results of an electronic survey designed and distributed by the American Association of Neurological Surgeons (AANS) and the Council of State Neurosurgical Societies (CSNS) to assess the perspectives of practicing U.S. neurosurgeons on the financial impact of the COVID-19 pandemic. The results are stratified by geographic region and provide insights into changes in procedural volume, compensation, practice expenses, and staffing during the pandemic.
Materials and Methods
Survey Conception and Distribution
A 19-question electronic survey (Supplementary Figure 1) was designed by the AANS and the CSNS to assess respondents’ perception of the effect of the COVID-19 pandemic on patient and procedural volume, revenue and expenses, and administrative and staff compensation. The survey was created using Qualtrics online survey software (Qualtrics, Provo, Utah, USA) and sent to members on the AANS and CSNS mailing lists with the assistance of the CSNS Workforce Committee. After initial distribution of the survey, a reminder was sent to the same members approximately 1 week later. The survey was designed to exclude duplicate entries, participation was voluntary, and all survey responses were recorded anonymously. The survey was distributed to 5224 practicing neurosurgeons in the United States and associated U.S. territories, and 267 neurosurgeons responded between April 30, 2020, and June 7, 2020.
Statistical Analysis
A descriptive analysis was performed to characterize trends in survey responses from the study cohort for each question. Responses were stratified according to geographic region (Northeast, Midwest, South, and West) based on U.S. Census Bureau classifications. The question responses were represented as categorical variables, and standard descriptive statistics were calculated for each question. Given the nonparametric distribution of response values, 2-sided Pearson χ2 tests were applied for comparison of categorical variables to assess significant trends in responses to select questions of interest according to geographic region. A P value of < 0.05 was statistically significant. Statistical analysis was performed using SAS Version 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Respondent Demographic Information
The response rate was 5.1% (267 of 5224). The anonymous nature of the survey precludes analysis of how responses to these questions differed according to number of years in practice, subspecialty practice interests, or other demographic factors. However, data were available regarding geographic location of respondents: 17.6% (47/267) were in the Northeast, 23% (62/267) were in the Midwest, 30% (81/267) were in the South, and 24% (64/267) were in the West. There was a balanced representation of responses across geographic regions. The Northeast had the fewest number of responses among the 4 primary geographic regions, and it was the first region affected by the COVID-19 pandemic. Approximately 5% of respondents were in other U.S. territories.
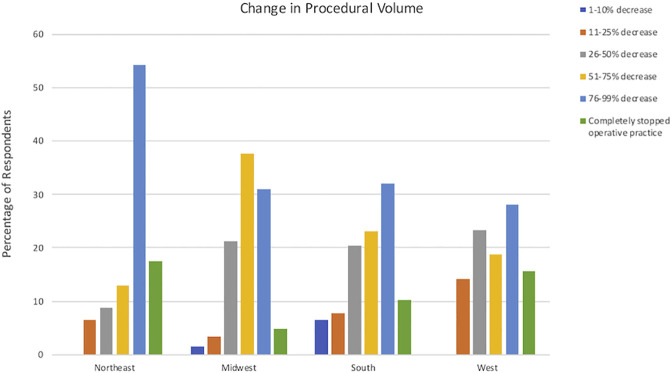
Patient/Procedural Volume and Applications for Government Funding
Of respondents, 59% noted a >50% decrease in neurosurgery clinic or emergency department visits and 56% noted a >50% decrease in procedural volume since the beginning of the COVID-19 epidemic. Additionally, 12% of respondents completely stopped their operative practice, and no respondents noted increases in operative volume. Most respondents noted a >50% decrease in clinic and emergency department visits, with no statistically significant difference present between regions (P = 0.056). However, the Northeast experienced a significantly larger decrease in procedure volume: 72% of Northeast respondents observed a >75% decrease in procedural volume compared with 36%–44% of respondents in other regions (P = 0.003). Figure 1 shows changes in procedural volume according to geographic region.
Figure 1.
Graph showing change in procedural volume.
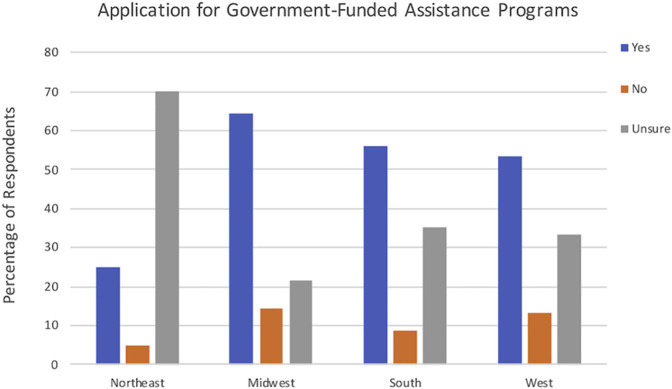
Of respondents, 56% noted that their institution had applied for government-funded assistance, and 15% of these respondents were aware of definitive plans or intent to pay back the government-funded assistance. Among regions, the Northeast had significantly fewer respondents who applied for government-funded assistance (25%) compared with other regions (>50%) (P = 0.038). Of respondents from the Northeast, 70% were unsure of whether their institution had applied for funding compared with 21%–35% in other regions. These results are shown in Figure 2 .
Figure 2.
Graph showing application for government-funded assistance programs.
Salary and Expenses
Approximately 63% of respondents noted reductions in their salary or benefits as a result of the COVID-19 pandemic compared with 37% of respondents who did not see a reduction. A complete loss of salary and benefits was noted by 4% of respondents, and a >50% reduction was reported by 25% of respondents. Among the respondents who reported no reduction in salary or benefits, 51% noted that they expect to see a reduction in the future, and an additional 33% considered this possibility. However, despite reports of reduced compensation, 74% of respondents noted unchanged practice expenses, and 8% of respondents noted increases in practice expenses. Additionally, 82% of respondents with reduced compensation have not been told when their previous salary and benefit levels will resume. Further, 89% of respondents were either moderately concerned or very concerned about the negative long-term effects of the COVID-19 pandemic on physician compensation. There were no significant differences between regions in reported salary and benefit reductions (P = 0.104), the expectation of future salary/benefit reductions (P = 0.205), or decreases in practice expenses (P = 0.275).
Involuntary Reassignment and Staffing Changes
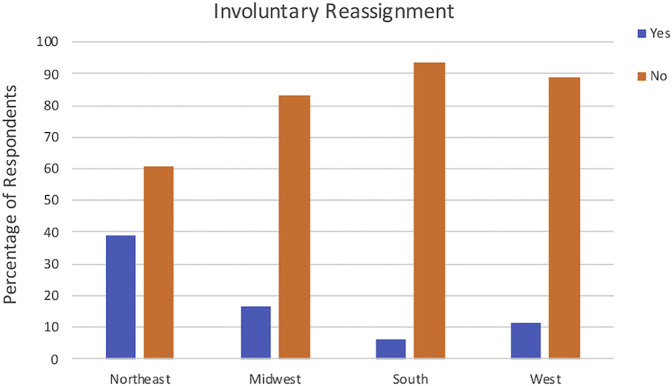
Figure 3 shows trends in involuntary reassignment. Of respondents, 17% confirmed that they or other neurosurgery providers were involuntarily reassigned to cover nonneurosurgical services during the COVID-19 pandemic compared with 83% who were not reassigned. Notably, 39% of respondents in the Northeast reported reassignment, which was significantly more than in other regions (6.4%–25%) (P < 0.001). Of respondents who were reassigned, 69% received no financial compensation for these work efforts, and 31% of respondents were compensated at a rate equal to or lower than their established salary rate. There were no significant differences between regions in financial compensation for reassignment (P = 0.356).
Figure 3.
Graph showing involuntary reassignment.
Additionally, 66% of respondents noted clerical staff changes during the COVID-19 pandemic, including decreased number, time, and availability. No respondents noted staff expansion, and only 33% of respondents noted no changes in clerical staffing. Similar trends were noted with nursing staff members (53% of respondents experienced a reduction and 47% did not). However, only 38% of respondents experienced a reduction in midlevel provider (nurse practitioner or physician assistant) support compared with 62% who did not. While only 16% of respondents experienced clinical or nursing staff layoffs, another 14% of respondents reported that they expect staff layoffs at a future time. Of respondents, 77% did not note reductions in surgical staff numbers, hours, or availability compared with 23% who did note reductions. There were no significant differences in staffing changes (clerical, nursing, midlevel, or surgeon) across different geographic regions.
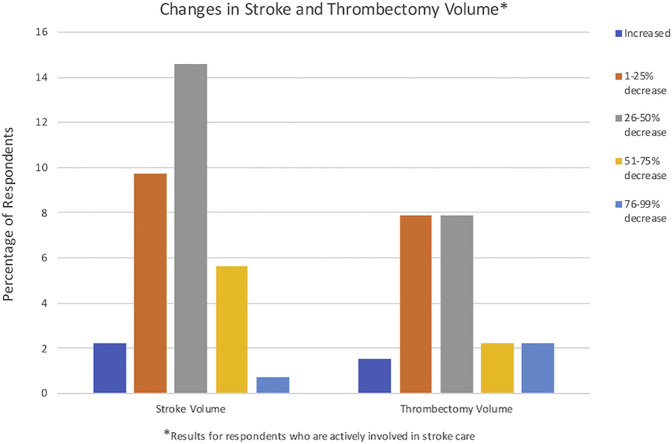
Interventional Stroke Treatment
Two survey questions assessed the effect of the pandemic on interventional stroke care in neurosurgery practices, and these results are shown in Figure 4 . Of respondents, 66% were not directly involved in interventional stroke care. However, 31% of respondents (94% of those who were involved in stroke care) noted decreases in stroke volume at their institutions. There were no significant differences between geographic regions in the decrease in stroke volume (P = 0.09). Of the respondents who performed endovascular thrombectomies (24% of respondents), 98% noted decreases in endovascular thrombectomy volume during the COVID-19 pandemic. There were no significant differences between regions in changes in thrombectomy volume (P = 0.192).
Figure 4.
Graph showing changes in stroke and thrombectomy volume. ∗Results for respondents actively involved in stroke care.
Discussion
The COVID-19 pandemic poses a unique challenge to neurosurgery practice in the United States. Patients requiring emergent or elective surgery are at great risk,12 and limitations on clinic visits, outpatient procedures, and personal protective equipment allocation will further compromise patient care. While the long-term consequences of the pandemic remain uncertain, the short-term economic impact on neurosurgery practice is unprecedented. Our survey was designed to clarify how practicing neurosurgeons in different regions have responded to the pandemic, how they perceive its effects, and how these changes might affect patient care and health care delivery.
Notably, the results of our survey are consistent with national trends. According to an American Medical Association survey on the financial impact of the COVID-19 pandemic, physician respondents confirmed an average of 32% loss of revenue, with 19% of physician respondents experiencing a >50% loss of revenue.13 Additionally, 81% of respondents were providing fewer in-person visits, and nearly 70% of respondents experienced a decrease in patient visits despite substantially increased telehealth visits compared with prepandemic levels.13 However, these responses were not stratified by geographic region or medical discipline. A majority of respondents from the American Medical Association survey also noted that federal financial relief was very helpful or extremely helpful, but increased personal protective equipment requirements and associated costs place an exceptional burden on physician-owned and smaller group practices.13 While our survey did not specify how personal protective equipment expenses have affected neurosurgeons’ practice costs, our data reflect a similar struggle for physicians to balance practice expenses with unanticipated downturns in patient volume and associated revenue.
Geographic Trends in the Pandemic’s Economic Impact
Decreased clinic volume, emergency department visits, compensation, and staffing resources were present across regions. However, Northeast respondents experienced significantly greater decreases in procedural volume and rates of clinical reassignment. The Northeast has a comparatively high population density, which may have exacerbated these trends. Despite being the smallest geographic region in area, 6 of the 9 states in the United States with the highest population density are located in the Northeast region. In April 2020, immediately preceding survey distribution, New York and New Jersey were among the worst-affected states in the country, and the rapidly rising case count and death rate in New York far outpaced the rest of the United States.14 Some literature suggests that high population density is associated with infection rates,15 and social distancing measures to prevent infection spread prove difficult in crowded spaces.14 However, despite greater declines in procedural volume and greater rates of reassignment, our survey revealed that respondents from the Northeast were less likely to report applying for government-funded financial assistance. Up to 70% of respondents from the Northeast were unsure whether their institution had applied for assistance; however, our survey did not enable respondents to explain this uncertainty. Respondents who expressed uncertainty regarding government funding applications may have comparatively less administrative responsibility. Alternatively, they may be junior members of larger practices who are not responsible for government funding applications. Follow-up analyses are warranted to account for variables such as respondents’ practice size and type.
Emerging Solutions
The intent of our analysis was to quantify the economic consequences of the COVID-19 pandemic on neurosurgical practice. However, the survey was not designed to assess how respondents planned to ameliorate these setbacks. Telemedicine protocols, including virtual clinic visits, remote imaging review, and telephone conferencing, may become an efficient alternative to in-person patient care. Prospective data show that new and established neurosurgery patients report high satisfaction with outpatient telemedicine clinic visits.16 Considering that some government assistance programs include funding for telehealth equipment,17 some respondents who applied for government funding may already be incorporating these technologies into their practice to offset financial losses.
Trends in Interventional Management of Stroke
Two questions in our survey focused on the effect of the pandemic on neurosurgeons’ involvement in stroke management. While most respondents were not involved in stroke management, a majority of those who were involved described decreased stroke and mechanical thrombectomy volume. These findings align with most existing data.18, 19, 20, 21 However, other analyses revealed stable proportions of patients with stroke requiring revascularization,22 elevated numbers of neurovascular emergencies,23 and nonsignificant increases in the number of thrombectomies performed during the pandemic.24 All of these observed variations in stroke care appear to contrast the principle that clinical care in neurovascular emergencies should remain consistently available, regardless of patient demographics, socioeconomic status, or changing community regulations. While our analysis cannot directly explain these variations, we propose that the COVID-19 pandemic has placed significant strain on existing imaging and transportation resources, which could perpetuate substantial delays in stroke care. Additionally, widespread public concern regarding the pandemic has motivated patients to delay medical care to avoid contracting COVID-19, which would diminish observed stroke volume and thrombectomy case numbers. It is clear that the pandemic will influence the future of neurosurgical stroke care, and neurosurgeons must continue to optimize inpatient stroke treatment pathways and encourage public awareness of stroke symptoms, as patients with COVID-19 can present with acute ischemic stroke.6 , 25 As we plan follow-up survey analyses, we will incorporate additional questions related to observed changes in stroke care pathways and mechanical thrombectomy volume.
Limitations and Future Directions
While we provide novel data regarding the financial impact of the COVID-19 pandemic on the neurosurgery community, our analysis is not without limitations. Given the uncertain duration and severity of the pandemic, we prioritized prompt distribution of the survey to capture responses, so the survey did not undergo psychometric validation before distribution. Additionally, a primary limitation of our analysis is the low survey response rate (5.1%). The low response rate may be attributable to several factors. Negatively affected respondents may be apt to respond to a survey dedicated to quantifying and understanding the pandemic’s consequences. Alternatively, respondents most affected by the pandemic may have the least amount of time and resources to dedicate to the survey. As the survey responses are anonymous, we cannot identify specific characteristics of nonrespondents versus respondents, but the low response rate predisposes our conclusions to sampling bias. This impacts whether our conclusions accurately represent the concerns and experiences of practicing neurosurgeons in the United States. As such, we attempt to present our results as a snapshot of trends in the field at a particular point in time.
Despite the myriad limitations associated with a low response rate, our overall volume of respondents (N = 267), with comparable distribution across geographic regions, lends credence to our findings. We attempted to encourage a robust response by including a reminder e-mail 1 week after distribution of the survey, the wide distribution of the survey allowed us to incorporate the experiences of 267 respondents, and we designed a comparatively short survey (19 questions) to assess specific indicators of financial stability. However, we did not include questions that further stratified respondent demographics, such as practice type, practice size, subspecialty, and surgeon experience level. We plan follow-up survey analyses, with specific questions designed to address these variables, using CSNS and AANS data to further characterize the financial impact of the COVID-19 pandemic. We will also account for the potential correlation between geographic location and clinical reassignment, given that changing state and federal regulations can influence the rate of COVID-19 infections in different locations. Additionally, we will plan our follow-up analyses to evaluate changes in the pandemic’s evolving effect on patient care and neurosurgery practice as COVID-19 vaccination becomes readily available and shelter-in-place and social distancing measures are lifted. For these follow-up surveys, we will use a similar methodology with more frequent reminder e-mails and a longer time period for response, which will supplement our overall response rate. Despite the above-mentioned limitations, this study confirms financial uncertainty within the neurosurgery community brought on by the pandemic. Most neurosurgeons experienced decreases in compensation, without accompanying decreases in practice expenses, and it is unclear when prepandemic levels of financial security will return. Many neurosurgeons are unsure of whether their institution applied for government-funded assistance, which exacerbates this uncertainty.
Conclusions
We present a preliminary analysis that clarifies the financial impact of the COVID-19 pandemic on neurosurgery practice. Survey respondents across the United States reported decreases in patient volume, procedural volume, and compensation despite stable practice expenses. Neurosurgeons in the Northeast experienced significantly greater decreases in procedural volume and rates of reassignment to nonneurosurgical care duties. Further study is necessary to follow the long-term economic impact of the pandemic, to clarify how different practice structures are affected, and to evaluate how regional differences in financial impact vary as case distributions fluctuate. The effect of the COVID-19 pandemic on health care delivery and economics continues to evolve, and it is imperative that the neurosurgery community continues to dedicate time, resources, and effort to protecting patients and health care providers during this time.
CRediT authorship contribution statement
James P. Caruso: Investigation, Formal analysis, Data curation, Writing - original draft, Writing - review and editing. Karin Swartz: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Catherine Mazzola: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Vin Shen Ban: Investigation, Formal analysis, Data curation, Writing - review and editing. Ravi Singh: Investigation, Formal analysis, Writing - review and editing. Cody Eldridge: Investigation, Formal analysis, Writing - review and editing. Clemens Schirmer: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Joseph Cheng: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Andrew M. Bauer: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Michael Steinmetz: Conceptualization, Methodology, Investigation, Formal analysis, Resources, Writing - review and editing, Supervision. Owoicho Adogwa: Conceptualization, Methodology, Investigation, Formal analysis, Data curation, Resources, Writing - review and editing, Supervision.
Acknowledgments
We acknowledge to the AANS and CSNS for the collaborative effort to design and distribute this survey. Additionally, we appreciate the respondents’ time and effort in answering the survey and providing valuable insight regarding neurosurgical practice during these unprecedented times. We look forward to future collaborative efforts to better define and address the unique socioeconomic consequences of the COVID-19 pandemic.
Footnotes
Conflict of interest statement: C. Schirmer reports research support from Penumbra and is a shareholder of NeuroTechnology Investors.
Supplementary Data
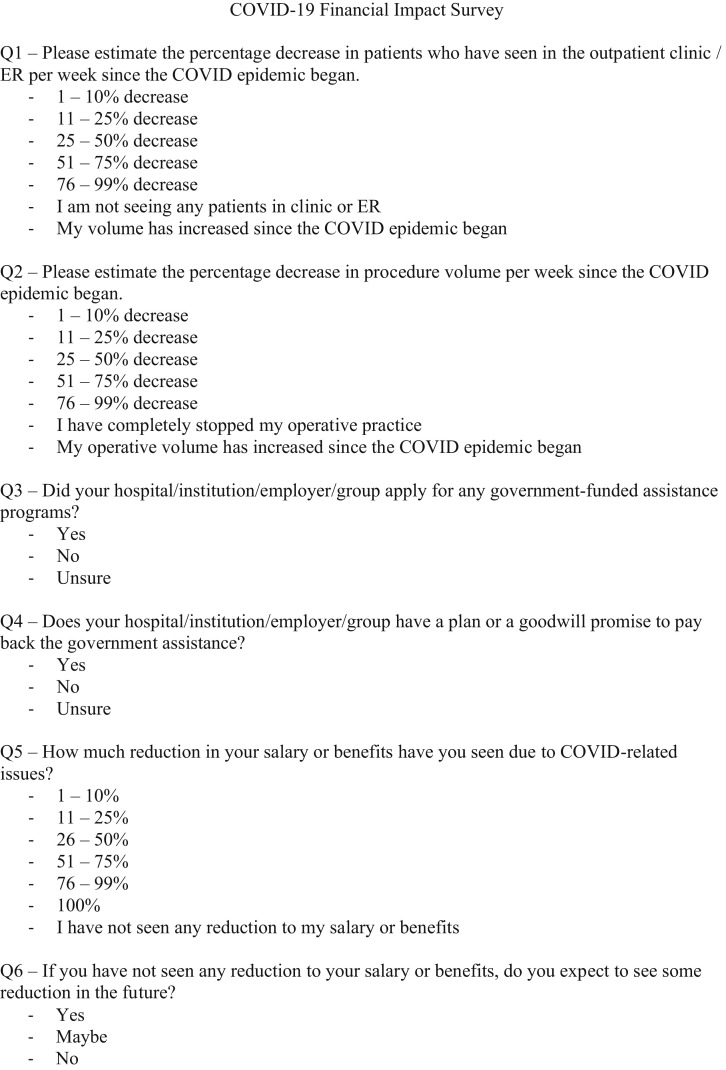
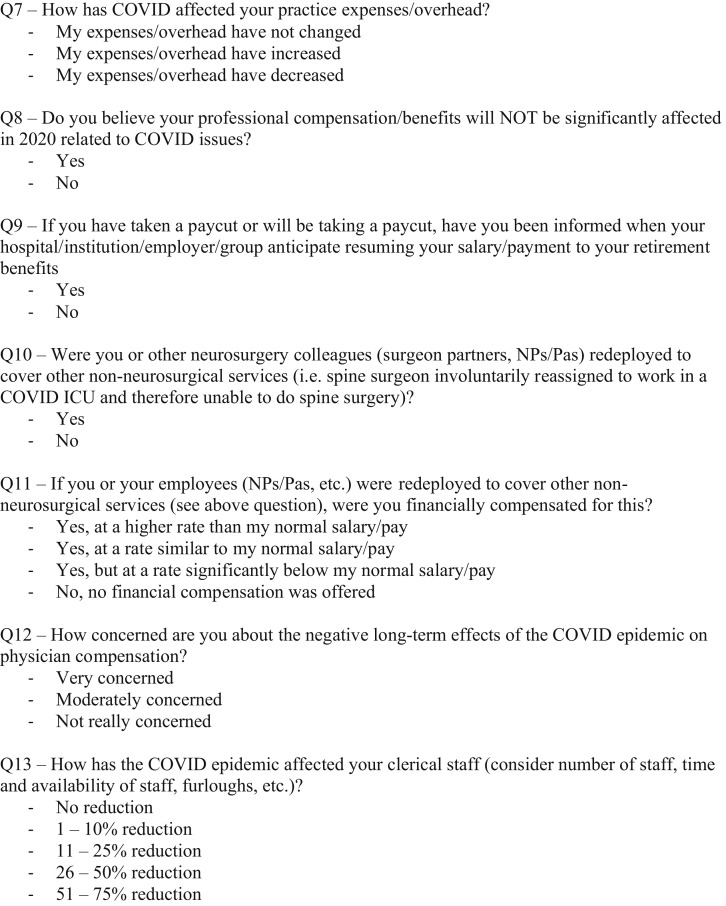
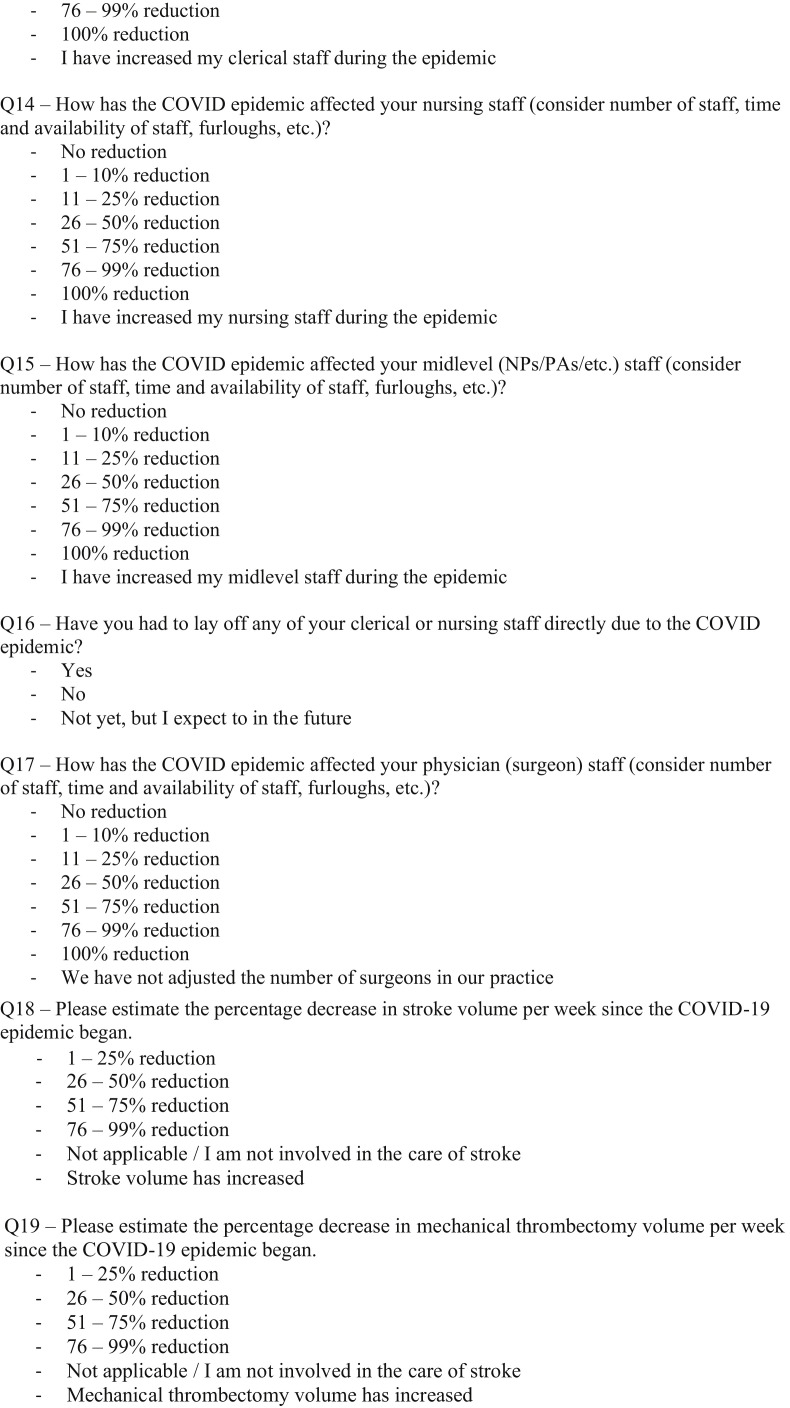
Supplementary Figure 1.
Electronic survey.
Supplementary Figure 1.
(Continued).
Supplementary Figure 1.
(Continued).
References
- 1.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Heath Organization Coronavirus disease (COVID-19) situation report 102. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200501-covid-19-sitrep.pdf?sfvrsn=742f4a18_4 Available at: Accessed June 30, 2021.
- 3.World Health Organization Coronavirus disease (COVID-19) situation report 105. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200504-covid-19-sitrep-105.pdf?sfvrsn=4cdda8af_2 Available at: Accessed June 30, 2021.
- 4.CDC cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/about-us-cases-deaths.html Available at: Accessed June 30, 2021.
- 5.Wu Y., Xu X., Chen Z., et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxley T.J., Mocco J., Majidi S., et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296:e119–e120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bridwell R., Long B., Gottlieb M. Neurologic complications of COVID-19. Am J Emerg Med. 2020;38:1549.e1543–1549.e1547. doi: 10.1016/j.ajem.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood) 2020;39:1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- 10.Pan A., Liu L., Wang C., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323:1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Provenzano D.A., Sitzman B.T., Florentino S.A., Buterbaugh G.A. Clinical and economic strategies in outpatient medical care during the COVID-19 pandemic. Reg Anesth Pain Med. 2020;45:579–585. doi: 10.1136/rapm-2020-101640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Medical Association COVID-19 physician practice financial impact survey results. https://www.ama-assn.org/practice-management/sustainability/covid-19-physician-practice-financial-impact-survey-results Available at: Accessed June 30, 2021.
- 14.Bashir M.F., Ma B., Bilal, et al. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cartenì A., Di Francesco L., Martino M. How mobility habits influenced the spread of the COVID-19 pandemic: results from the Italian case study. Sci Total Environ. 2020;741:140489. doi: 10.1016/j.scitotenv.2020.140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoon E.J., Tong D., Anton G.M., et al. Patient satisfaction with neurosurgery telemedicine visits during the coronavirus disease 2019 pandemic: a prospective cohort study. World Neurosurg. 2021;145:e184–e191. doi: 10.1016/j.wneu.2020.09.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Contreras C.M., Metzger G.A., Beane J.D., Dedhia P.H., Ejaz A., Pawlik T.M. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoyer C., Ebert A., Huttner H.B., et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 2020;51:2224–2227. doi: 10.1161/STROKEAHA.120.030395. [DOI] [PubMed] [Google Scholar]
- 19.Hsiao J., Sayles E., Antzoulatos E., et al. Effect of COVID-19 on emergent stroke care: a regional experience. Stroke. 2020;51:e2111–e2114. doi: 10.1161/STROKEAHA.120.030499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerleroux B., Fabacher T., Bricout N., et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke. 2020;51:2012–2017. doi: 10.1161/STROKEAHA.120.030373. [DOI] [PubMed] [Google Scholar]
- 21.Zhao J., Li H., Kung D., Fisher M., Shen Y., Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paliwal P.R., Tan B.Y.Q., Leow A.S.T., et al. Impact of the COVID-19 pandemic on hyperacute stroke treatment: experience from a comprehensive stroke centre in Singapore. J Thromb Thrombolysis. 2020;50:596–603. doi: 10.1007/s11239-020-02225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montagnon R., Rouffilange L., Agard G., Benner P., Cazes N., Renard A. Impact of the COVID-19 pandemic on emergency department use: focus on patients requiring urgent revascularization. J Emerg Med. 2021;60:229–236. doi: 10.1016/j.jemermed.2020.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frisullo G., Brunetti V., Di Iorio R., et al. Effect of lockdown on the management of ischemic stroke: an Italian experience from a COVID hospital. Neurol Sci. 2020;41:2309–2313. doi: 10.1007/s10072-020-04545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Immovilli P., Terracciano C., Zaino D., et al. Stroke in COVID-19 patients: a case series from Italy. Int J Stroke. 2020;15:701–702. doi: 10.1177/1747493020938294. [DOI] [PubMed] [Google Scholar]