Abstract
Objective
In the wake of the COVID-19 pandemic, telemedicine has become rapidly adopted by the neurosurgical community; however, few studies have examined predictors of telemedicine utilization. Here, we analyze patient variables associated with the acceptance of a telemedicine encounter by a pediatric neurosurgical population during the early phases of the COVID-19 pandemic.
Methods
All patients seen in a single institution's outpatient pediatric neurosurgery clinic between April 1, 2020 and July 31, 2020 were retrospectively reviewed. Demographic variables were collected for each patient's first completed encounter. Patients participating in telemedicine were compared with those seen in person. Univariate analysis was performed using the Wilcoxon rank sum test for continuous variables and Fischer exact test for categorical variables. A logistic regression multivariable analysis was then performed.
Results
We included 682 patients (374 telemedicine and 308 in person). Univariate analysis demonstrated that telemedicine visits were more likely to occur at earlier study dates (P < 0.001) and that patients participating in telemedicine visits were more likely to be established rather than new patients (P < 0.001), White or Caucasian (P < 0.001), not Hispanic or Latino (P < 0.001), English-speaking (P < 0.001), non-Medicare/Medicaid recipients (P < 0.001), have lower no-show rates (P = 0.006), and live farther from the hospital (P = 0.005). Multivariable analysis demonstrated older age (P = 0.031), earlier appointment date (P < 0.01), established patient status (P < 0.001), English-speaking (P < 0.02), and non-Medicare/Medicaid insurance (P < 0.05) were significant predictors of telemedicine utilization.
Conclusions
Significant demographic differences exist among pediatric patients who participated in telemedicine versus those who requested an in-person visit at our institution. Addressing barriers to access will be crucial for promoting health equity in continued utilization of telemedicine.
Key words: COVID-19, Pediatric neurosurgery, Telehealth, Telemedicine
Abbreviations and Acronyms: AOR, Adjusted odd's ratio; AUC, Area under the curve; CI, Confidence interval; COVID-19, Coronavirus disease 2019; IQR, Interquartile range
Introduction
Telemedicine is a rapidly evolving tool that uses technology to deliver health care from a distance.1 Within neurosurgery, telemedicine was initially incorporated into clinical practice in the 1990s, when “telepathology” was proposed for the remote analysis of intraoperative frozen sections.2 With technological advances over the past 3 decades, telemedicine has become increasingly integrated into modern neurosurgical practice. Current applications include interhospital consultations to triage patients and determine the need for transfer,3, 4, 5, 6 acute stroke trial enrollment,7 increasing access to care for underserved and rural communities,8, 9, 10, 11 care coordination in the postoperative period,12, 13, 14, 15 and remote programming of neuromodulator devices.16 , 17
More recently, telemedicine has taken on new urgency in the context of the coronavirus disease 2019 (COVID-19) pandemic. With the goals of optimizing patient and provider safety and facilitating social distancing, telemedicine has been rapidly adopted by the neurosurgical community. Since the onset of the pandemic, neurosurgeons have revisited the subject of telemedicine, reviewing practice recommendations and discussing the barriers, limitations, advantages, and efficacy of telemedicine in neurosurgical practice.18, 19, 20, 21, 22, 23, 24 Within pediatric neurosurgery specifically, recent studies have focused on the experience of brain tumor patients and their caregivers25 and have reported procedural, consult, and clinic volume trends during different stages of the pandemic.26 However, few studies have examined the impact of patient demographics on telemedicine utilization. Understanding this relationship is important to address barriers to the adoption of telemedicine as it is further integrated into models of health care delivery.
Here, we review the characteristics of pediatric neurosurgery patients who were seen via telemedicine versus in-person visits during the initial phases of the COVID-19 pandemic. Our objective was to identify patient-specific variables that are associated with the utilization of telemedicine in order to optimize and guide the expansion of telemedicine efforts in the future.
Methods
Data Collection
This study was approved by the institutional review board at Connecticut Children's (Institutional Review Board 20–108). All pediatric neurosurgical outpatient encounters scheduled at our institution between April 1, 2020 and July 31, 2020 were retrospectively reviewed. For patients with multiple encounters during the study period, only the patient's first completed encounter was included in the subsequent statistical analysis.
Patient demographics and encounter characteristics were collected using an automated report generated by the electronic medical record. These variables included medical record number; patient name; appointment date; appointment type (established or new, telemedicine or in-person); appointment status (cancelled, complete); appointment comments; age; race; ethnicity; sex; language; ZIP code; no-show rate; primary insurance payer; medical history; problem list; and encounter diagnosis. Patient charts were then individually reviewed for history of neurosurgical operation and, if so, date of last operation. To ensure the accuracy of the automated reports, 1 author (WAL) confirmed at least 4 randomly selected variables during manual chart review. No discrepancies were found.
The principal diagnosis associated with each encounter was consolidated into 1 of the following categories: 1) head shape and skull abnormalities; 2) tumors and intracranial cysts; 3) hydrocephalus; 4) congenital; 5) trauma; and 6) other. Assignments were made by 2 independent reviewers (WAL and NKL), and no discrepancies were identified. Distance from the hospital was determined based on patient ZIP code using Google Maps to calculate the minimum driving distance to the hospital address. All COVID-19−related data were collected from data.ct.gov.
Encounters were classified as 1) telemedicine or 2) in-person visits. During the study period, all patients were offered a telemedicine appointment unless an in-person physical examination was felt to be critical by the provider. Patients for whom the provider requested an in-person encounter, as documented by the office staff in the appointment comments, were excluded from further statistical analyses.
Statistical Analysis
Descriptive statistics were performed using median and interquartile range (IQR) for continuous variables and frequency and percentage for categorical variables. Univariate analysis was performed using an unpaired Wilcoxon rank sum test for continuous variables and Fischer exact test for categorical variables. For categorical variables that had more than 5 outcomes, a Fisher exact test with a Monte Carlo adjustment was used. Variables with a P value < 0.2 were then selected for the multivariable analysis. Wald tests were used to generate P values for the logistic model. All univariate analyses were performed using base functions in R, and the multivariable logistic regression was performed in SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Outpatient Encounters
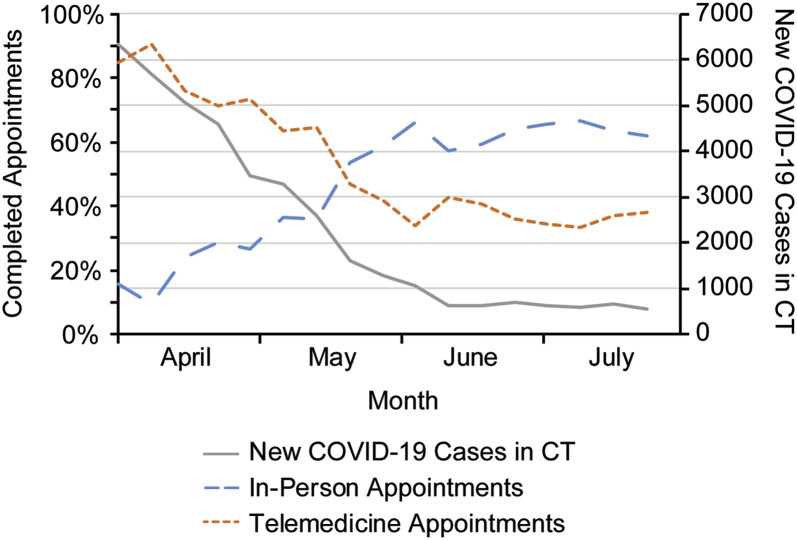
A total of 1833 outpatient encounters involving 986 unique patients were scheduled by the Connecticut Children's Division of Neurosurgery between April 1, 2020 and July 31, 2020. Of these scheduled visits, there were 125 (7%) no-shows, 782 (43%) cancellations or postponed visits, and 926 (50%) completed encounters. Clinic volume was lowest in April and May, with 138 and 167 completed appointments, respectively, but progressively increased in June and July, with 297 and 324 completed encounters, respectively. Conversely, appointment cancellation rates were highest in April and lowest in July (53% and 34%, respectively). Overall, slightly more patients completed their appointments in person than via telemedicine (52% and 48% respectively). There were higher rates of telemedicine utilization in April and May (80% and 63% of visits, respectively) compared with June and July (40% and 35% of visits, respectively). Over that time period, there was a decrease in the number of new COVID-19 cases in Connecticut (Figure 1 ).
Figure 1.
Trends in completed in-person encounters, telemedicine encounters, and new COVID-19 cases over time. The proportion of encounters that were completed via telemedicine decreased and those that were completed in-person increased from April through July 2020, as local COVID-19 rates decreased. Color is available online only.
Patient Characteristics
The 926 completed encounters involved 741 unique patients, 689 (93%) of whom were offered a telemedicine visit. Seven patients with incomplete demographic data were excluded, culminating in 682 patients whose first encounter was included in the analysis. The baseline characteristics of this cohort are reported in Table 1 . The median age at the time of the visit was 4 years (IQR 1–14), with males constituting 55% of the population. The majority of patients were White or Caucasian (60%), not Hispanic or Latino (75%), and English speaking (91%). Medicare/Medicaid recipients made up 48% of the population. The median driving distance to the hospital was 20.75 miles (IQR 11.2–37.0). Only 41% of the population had a history of a neurosurgical operation. Head shape and skull abnormalities were the most common encounter diagnoses seen (34%), followed by congenital abnormalities (20%), hydrocephalus (16%), tumors and intracranial cysts (15%), other (9%), and trauma (6%) (Table 1).
Table 1.
Patient and Encounter Characteristics (n = 682)
| Variable | All Patients (n = 682) | In Person (n = 308) | Telemedicine (n = 374) | P Value |
|---|---|---|---|---|
| Age, median years (IQR) | 4 (1–14) | 3 (0.9–14) | 4.5 (1–13) | 0.176 |
| Sex (%) | 0.105 | |||
| Male | 372 (55) | 179 (58) | 193 (52) | |
| Female | 310 (45) | 129 (42) | 181 (48) | |
| Race (%) | <0.001 | |||
| White or Caucasian | 412 (60) | 161 (52) | 251 (67) | |
| Black or African American | 67 (10) | 36 (12) | 31 (8) | |
| Other | 203 (30) | 111 (36) | 92 (25) | |
| Ethnicity (%) | <0.001 | |||
| Not Hispanic or Latino | 512 (75) | 212 (69) | 300 (80) | |
| Hispanic or Latino | 170 (25) | 96 (31) | 74 (20) | |
| Preferred language (%) | <0.001 | |||
| English | 619 (91) | 257 (83) | 362 (97) | |
| Spanish | 43 (6) | 35 (11) | 8 (2) | |
| Other | 20 (3) | 16 (5) | 4 (1) | |
| Primary payer (%) | <0.001 | |||
| Non-Medicare/Medicaid | 357 (52) | 136 (44) | 221 (59) | |
| Medicare/Medicaid | 325 (48) | 172 (56) | 153 (41) | |
| Patient status (%) | <0.001 | |||
| Established | 500 (73) | 180 (58) | 320 (86) | |
| New | 182 (27) | 128 (42) | 54 (14) | |
| Month of appointment (%) | <0.001 | |||
| April | 120 (18) | 12 (4) | 108 (29) | |
| May | 132 (19) | 37 (12) | 95 (25) | |
| June | 215 (32) | 119 (39) | 96 (26) | |
| July | 215 (32) | 140 (45) | 75 (20) | |
| No show rate, median (IQR) | 0% (0%–6%) | 1% (0%–7%) | 0% (0%–5%) | 0.006 |
| Distance to hospital, median miles (IQR) | 20.75 (11.2–37) | 17 (7.3–33.3) | 22 (12.4–39.2) | 0.005 |
| History of neurosurgical operation (%) | 282 (41) | 125 (41) | 157 (42) | 0.755 |
| Days since last neurosurgical operation (median [IQR]) | 859 (246–1916) | 793 (240–1850) | 940 (251–1905) | 0.649 |
| Diagnostic category (%) | 0.900 | |||
| Head shape and skull abnormalities | 230 (34) | 98 (32) | 132 (35) | |
| Tumors and intracranial cysts | 102 (15) | 50 (16) | 52 (14) | |
| Hydrocephalus | 110 (16) | 50 (16) | 60 (16) | |
| Congenital | 133 (20) | 62 (20) | 71 (19) | |
| Trauma | 44 (6) | 21 (7) | 23 (6) | |
| Other | 63 (9) | 27 (9) | 36 (10) |
Variables Associated with Telemedicine Utilization
In the univariate analysis, compared with patients seen in person, patients completing their visit via telemedicine were more likely to be seen at earlier dates during the study period (P < 0.001), be established patients rather than new patients (86% vs. 58%, P < 0.001), White or Caucasian (67% vs. 52%, P < 0.001), not Hispanic or Latino (80% vs. 69%, P < 0.001), English-speaking (97% vs. 83%, P < 0.001), a non-Medicare/Medicaid recipient (59% vs. 44%, P < 0.001), have lower no show rates (0% vs. 1%, P = 0.006), and live farther from the hospital (22 vs. 17 miles, P = 0.005) (Table 1). Patient age, sex, history of a neurosurgical operation, time since last operation, and diagnostic category did not differ significantly between the two groups.
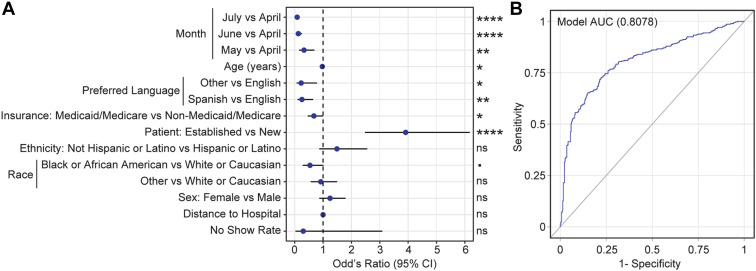
A multivariable logistic regression model identified 5 variables that were significantly associated with telemedicine utilization, with an area under the receiver operating characteristic curve of 0.8078 (95% CI 0.78–0.84) (Figure 2 ). Appointments completed in May, June, and July were all associated with lower telemedicine usage compared with appointments in April during the first peak of COVID-19 cases in Connecticut (adjusted odds ratio [AOR]May 0.33 [95% CI 0.16–0.69], P = 0.004; AORJune 0.13 [95% CI 0.06–0.25], P < 0.001; AORJuly = 0.09 [95% CI 0.04–0.17], P < 0.001). Established patients were more likely to use telemedicine compared with new patients (AOR = 3.91 [95% CI 2.48–6.17]; P < 0.001). Non−English-speaking patients were less likely to use telemedicine (AORSpanish = 0.25 [95% CI 0.10–0.65], P = 0.004; AOROther = 0.23 [95% CI 0.07–0.78], P = 0.019), as were Medicare/Medicaid insurance recipients (AOR = 0.68 [95% CI 0.46–1.00]; P = 0.047) and younger patients (AOR = 0.97 [95% CI 0.95–1.00]; P = 0.031). Finally, though Black or African American patients were less likely to use telemedicine (AOR = 0.54 [95% CI 0.29–1.01]; P = 0.053) compared with White or Caucasian patients, that association only trended toward significance (Table 2 ).
Figure 2.
Logistic regression analysis of variables associated with telemedicine use. (A) Forest plot of adjusted odds ratios and 95% confidence intervals corresponding to a multivariable logistic regression model comparing telemedicine with in-person visits (Wald test, P < 0.1, ∗ P < 0.05, ∗∗ P < 0.01, ∗∗∗∗ P < 0.001). (B) Receiver operating curve (ROC) for the multivariable logistic model. AUC, area under curve; Hosmer and Lemeshow Goodness-of-Fit, P < 0.01; Chi-square of model compared with chance, P < 0.0001).
Table 2.
Multivariable Analysis of Odds of Telemedicine Utilization
| Variable | Adjusted Odds Ratio | 95% CI | P Value |
|---|---|---|---|
| Age (years) | 0.97 | 0.95–1.00 | 0.031 |
| Female | 1.25 | 0.87–1.79 | 0.233 |
| Race | |||
| Black or African American versus White or Caucasian | 0.54 | 0.29–1.01 | 0.053 |
| Other versus White or Caucasian | 0.92 | 0.57–1.50 | 0.733 |
| Not Hispanic or Latino | 1.49 | 0.87–2.56 | 0.150 |
| Preferred language | |||
| Spanish versus English | 0.25 | 0.10–0.65 | 0.004 |
| Other versus English | 0.23 | 0.07–0.78 | 0.019 |
| Medicare/Medicaid insurance status | 0.68 | 0.46–1.00 | 0.047 |
| Established patient status | 3.91 | 2.48–6.17 | <0.001 |
| Month | |||
| May versus April | 0.33 | 0.16–0.69 | 0.004 |
| June versus April | 0.13 | 0.06–0.25 | <0.001 |
| July versus April | 0.09 | 0.04–0.17 | <0.001 |
| Distance to hospital | 1.00 | 0.99–1.01 | 0.719 |
Discussion
The use of telemedicine has rapidly expanded and has become an integral part of health care delivery since the onset of the COVID-19 pandemic. Here, we review our experience with adopting telemedicine during the early stages of the pandemic and demonstrate that specific demographic variables are associated with telemedicine utilization by patients and their families. Although these variables are nonmodifiable, our findings set the foundation for better understanding how to successfully integrate telemedicine into our future practice.
Changes in Volume Related to COVID-19
The neurosurgical community was quick to adapt to the COVID-19 pandemic. Early recommendations included conducting outpatient appointments by telemedicine when possible, stepwise reduction/postponement of elective surgery based on the COVID-inpatient census, personal protective equipment guidelines, and alterations to operative techniques to minimize aerosol production.18
Several groups have described their experience with shifts in clinical volume during the pandemic, with 1 reporting a 31% reduction in pediatric neurosurgical procedural volume during the first phase of the pandemic.26 Concomitantly, in-person adult and pediatric outpatient neurosurgical clinic encounters were reduced by 91%, while weekly neurosurgical telehealth encounters increased from 0 to 151. At our institution, we experienced similar trends in clinic volume, but notably, we found a reversal of these trends as local COVID-19 rates began to improve—completed encounters were at their lowest in April and May and primarily consisted of telemedicine visits, whereas overall volume and particularly in-person visits increased in June and July.
Despite these early trends, telemedicine is unlikely to represent a transient phenomenon, as both patients and providers have reported substantial satisfaction with the telemedicine experience. One study reported that 85% of providers wanted to incorporate telemedicine into their future practice, and 36% of patients reported they would like to conduct future visits via telemedicine.27 In another report, telemedicine utilization for spine patients was associated with an improvement in physician Press Ganey survey rankings from the 29th to the 93rd percentile.24 These studies support an ongoing role for telemedicine in future practice and highlight the importance of understanding how telemedicine is used by our patient population.
Predictors of Telemedicine Utilization
Prior studies have explored the benefits of and barriers to wide-scale implementation of telemedicine in adult populations.15 , 19 , 20 , 22 , 28 , 29 Though telemedicine has the potential to eliminate travel time and cost, improve wait times, enhance flexibility in scheduling, and increase geographic access to care, there are concerns that technological limitations and lack of education may limit access to telemedicine by specific subsets of patients. In addition, some providers argue that further expansion of telemedicine may result in increased no-show rates, more time spent per encounter, and an overwhelming number of second opinion consults, ultimately decreasing surgical yield.22
A recent systematic review of 52 studies involving 45,801 neurosurgical patients undergoing telemedicine consultation concluded that telemedicine is an effective tool for expanding neurosurgical care to populations that previously lacked adequate access.17 Notably, the studies included in the review primarily involved situations in which telemedicine was being used to supplement a gap in care, such as for remote stroke trial enrollment, triage before transfer, consultation for remote community hospitals without dedicated neurosurgical staff, and postoperative care for geographically remote patients. In the context of the COVID-19 pandemic, however, telemedicine instead serves as an alternative to established care systems to accommodate social distancing in a public health emergency. In this new context, subsets of patients, particularly those with a lower socioeconomic status, are at risk of being marginalized.30 Consequently, we undertook the current study in order to identify variables that are associated with the utilization of telemedicine within a pediatric neurosurgical population and identify those patients who require increased outreach.
Our multivariable analysis identified 5 variables that were significantly associated with the utilization of telemedicine by our patients: an appointment in April, status as a previously established patient, older age, English as primary language, and non-Medicare/Medicaid insurance status. The association between telemedicine utilization and an appointment date in April may reflect the widespread desire to avoid potential exposures to the virus when rates were at their peak during the initial wave of the pandemic. This variable, therefore, may not be generalizable to future telemedicine utilization. The other 4 variables, however, are not unique to a particular phase of the pandemic. While the particular reasons for choosing telemedicine versus in-person visits could not be determined through this retrospective review, we hypothesize that established patients may have been more likely to use telemedicine due to a preexisting relationship with the provider, whereas new patients may have had increased anxiety related to their diagnosis and therefore requested what they perceived to be a “more thorough” in-person visit. Parents of younger children may have been more likely to request an in-person visit for similar reasons.
English as the primary language and non-Medicare/Medicaid insurance status were also significantly associated with telemedicine utilization, raising concerns that socioeconomic status may impact patients' access to telemedicine. Others have also highlighted the potential for incorporation of telemedicine to exacerbate health disparities on the basis of race or socioeconomic status. In a retrospective analysis of the Mount Sinai Data Warehouse of >50,000 patients who sought care for COVID-19-related concerns, Black or African American patients were significantly more likely to use the emergency department or present to the office rather than use telemedicine.31 Others have shown that the impact of socioeconomic status on clinic attendance is not limited to telemedicine. Higher no-show rates and a lack of parent/caregiver compliance have been documented more frequently in patients of lower socioeconomic status.32 , 33 Further studies are needed in order to identify effective strategies for expanding access to these at-risk patient populations as well.
Study Limitations and Future Directions
This study has several limitations, in particular due to its retrospective and single-institution nature. Included variables were limited to those that were recorded in the electronic medical record. As a result, while socioeconomic status or level of education are important variables to consider, insurance status was used as a proxy instead. In addition, although the results of this study may be specific to our own patient population and geographic variations may limit its generalizability, our findings raise awareness that specific subpopulations of patients will require additional assistance and attention in order to effectively use telemedicine—a conclusion that is broadly applicable.
Notably, the decision-making process to access care via telemedicine versus an in-person visit during a global pandemic is complex and individualized to each unique patient and their family. In the present study, therefore, we do not attempt to describe this decision-making process but rather use a statistical model to identify variables that are significantly associated with the utilization of telemedicine.
In addition, this study relied on accurate charting by the office staff. The policy during the study period was to offer a telemedicine appointment to all patients, unless an in-person physical examination was felt to be critical by the provider. When an in-person visit was deemed necessary, or when the patient declined a telemedicine visit, a note was documented in the “appointment comments” attached to the encounter. Patients not offered a telemedicine appointment were subsequently excluded from the statistical analysis, but some instances may have been inconsistently documented.
In order to counter these limitations, future studies will use a prospective structure including a standardized survey to assess factors that affect patients' and families' decisions to use telemedicine versus in-person visits. These analyses will help structure future efforts to expand telemedicine options to all pediatric neurosurgical patients.
Conclusion
The COVID-19 pandemic has prompted the rapid expansion of telemedicine within pediatric neurosurgery, but not all patients use telemedicine equally. In this retrospective study, established, older patients who spoke English and had non-Medicaid/Medicare insurance were more likely to use telemedicine. A further understanding of the patient characteristics associated with telemedicine utilization will help optimize and guide the expansion of telemedicine within pediatric neurosurgery.
CRediT authorship contribution statement
William A. Lambert: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. Nathan K. Leclair: Data curation, Formal analysis, Methodology, Visualization, Validation, Writing – review & editing. Joshua Knopf: Data curation, Methodology, Writing – review & editing. Maua H. Mosha: Formal analysis, Methodology, Writing – review & editing. Markus J. Bookland: Conceptualization, Supervision, Resources, Writing – review & editing. Jonathan E. Martin: Conceptualization, Supervision, Resources, Writing – review & editing. David S. Hersh: Conceptualization, Methodology, Supervision, Resources, Project administration, Writing – review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Institute of Medicine Committee on Evaluating Clinical Applications of T . In: Telemedicine: A Guide to Assessing Telecommunications in Health Care. Field M.J., editor. National Academies Press; Washington, DC: 1996. The National Academies collection: reports funded by National Institutes of Health. [PubMed] [Google Scholar]
- 2.Becker R.L., Jr., Specht C.S., Jones R., Rueda-Pedraza M.E., O'Leary T.J. Use of remote video microscopy (telepathology) as an adjunct to neurosurgical frozen section consultation. Hum Pathol. 1993;24:909–911. doi: 10.1016/0046-8177(93)90142-4. [DOI] [PubMed] [Google Scholar]
- 3.Olldashi F., Latifi R., Parsikia A., et al. Telemedicine for neurotrauma prevents unnecessary transfers: an update from a nationwide program in Albania and analysis of 590 patients. World Neurosurg. 2019;128:e340–e346. doi: 10.1016/j.wneu.2019.04.150. [DOI] [PubMed] [Google Scholar]
- 4.Jackson E.M., Costabile P.M., Tekes A., et al. Use of telemedicine during interhospital transport of children with operative intracranial hemorrhage. Pediatr Crit Care Med. 2018;19:1033–1038. doi: 10.1097/PCC.0000000000001706. [DOI] [PubMed] [Google Scholar]
- 5.Alan N., Kim S., Agarwal N., et al. Inter-facility transfer of patients with traumatic intracranial hemorrhage and GCS 14-15: The pilot study of a screening protocol by neurosurgeon to avoid unnecessary transfers. J Clin Neurosci. 2020;81:246–251. doi: 10.1016/j.jocn.2020.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor M.A., Knochel M.L., Proctor S.J., et al. Pediatric trauma telemedicine in a rural state: Lessons learned from a 1-year experience. J Pediatr Surg. 2021;56:385–389. doi: 10.1016/j.jpedsurg.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Shoirah H., Wechsler L.R., Jovin T.G., Jadhav A.P. Acute stroke trial enrollment through a telemedicine network: a 12-year experience. J Stroke Cerebrovasc Dis. 2019;28:1926–1929. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.046. [DOI] [PubMed] [Google Scholar]
- 8.Hayward K., Han S.H., Simko A., James H.E., Aldana P.R. Socioeconomic patient benefits of a pediatric neurosurgery telemedicine clinic. J Neurosurg Pediatr. 2019:1–5. doi: 10.3171/2019.8.PEDS1925. [DOI] [PubMed] [Google Scholar]
- 9.Ellis M.J., Russell K. The potential of telemedicine to improve pediatric concussion care in rural and remote communities in Canada. Front Neurol. 2019;10:840. doi: 10.3389/fneur.2019.00840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simko A., Han S.H., Aldana P.R. Telemedicine: providing access to care in pediatric neurosurgery to underserved communities. World Neurosurg. 2020;138:556–557. doi: 10.1016/j.wneu.2020.03.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James H.E. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr. 2016;25:753–757. doi: 10.3171/2016.6.PEDS16202. [DOI] [PubMed] [Google Scholar]
- 12.Reider-Demer M., Raja P., Martin N., Schwinger M., Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41:497–501. doi: 10.1007/s10143-017-0878-0. [DOI] [PubMed] [Google Scholar]
- 13.Ponce B.A., Brabston E.W., Shin Z., et al. Telemedicine with mobile devices and augmented reality for early postoperative care. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:4411–4414. doi: 10.1109/EMBC.2016.7591705. [DOI] [PubMed] [Google Scholar]
- 14.Thakar S., Rajagopal N., Mani S., et al. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus. 2018;44:E17. doi: 10.3171/2018.2.FOCUS17543. [DOI] [PubMed] [Google Scholar]
- 15.Demaerschalk B.M., Cassivi S.D., Blegen R.N., et al. Health economic analysis of postoperative video telemedicine visits to patients’ homes. Telemed J E Health. 2021;27:635–640. doi: 10.1089/tmj.2020.0257. [DOI] [PubMed] [Google Scholar]
- 16.Mendez I., Song M., Chiasson P., Bustamante L. Point-of-care programming for neuromodulation: a feasibility study using remote presence. Neurosurgery. 2013;72:99–108. doi: 10.1227/NEU.0b013e318276b5b2. [DOI] [PubMed] [Google Scholar]
- 17.Eichberg D.G., Basil G.W., Di L., et al. Telemedicine in neurosurgery: lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 2020;88:E1–E12. doi: 10.1093/neuros/nyaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozoner B., Gungor A., Hasanov T., Toktas Z.O., Kilic T. Neurosurgical practice during coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;140:198–207. doi: 10.1016/j.wneu.2020.05.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mouchtouris N., Lavergne P., Montenegro T.S., et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daggubati L.C., Eichberg D.G., Ivan M.E., et al. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–e863. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blue R., Yang A.I., Zhou C., et al. Telemedicine in the era of coronavirus disease 2019 (COVID-19): a neurosurgical perspective. World Neurosurg. 2020;139:549–557. doi: 10.1016/j.wneu.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright C.H., Wright J., Shammassian B. COVID-19: Launching neurosurgery into the era of telehealth in the United States. World Neurosurg. 2020;140:54–55. doi: 10.1016/j.wneu.2020.05.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mazzatenta D., Zoli M., Cavallo M.A., et al. Remodulation of neurosurgical activities in an Italian region (Emilia-Romagna) under COVID- 19 emergency: maintaining the standard of care during the crisis [e-pub ahead of print] J Neurosurg Sci. 2020 doi: 10.23736/S0390-5616.20.05018-3. [DOI] [PubMed] [Google Scholar]
- 24.Basil G.W., Eichberg D.G., Perez-Dickens M., et al. Differences between neurosurgical subspecialties in telehealth adoption. World Neurosurg. 2021;146:e323–e327. doi: 10.1016/j.wneu.2020.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Voisin M.R., Oliver K., Farrimond S., et al. Brain tumors and COVID-19: the patient and caregiver experience. Neurooncol Adv. 2020;2:vdaa104. doi: 10.1093/noajnl/vdaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel P.D., Kelly K.A., Reynolds R.A., et al. Tracking the volume of neurosurgical care during the coronavirus disease 2019 pandemic. World Neurosurg. 2020;142:e183–e194. doi: 10.1016/j.wneu.2020.06.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohanty A., Srinivasan V.M., Burkhardt J.K., et al. Ambulatory neurosurgery in the COVID-19 era: patient and provider satisfaction with telemedicine. Neurosurg Focus. 2020;49:E13. doi: 10.3171/2020.9.FOCUS20596. [DOI] [PubMed] [Google Scholar]
- 28.Basil G.W., Eichberg D.G., Perez-Dickens M., et al. Letter: implementation of a neurosurgery telehealth program amid the COVID-19 crisis-challenges, lessons learned, and a way forward. Neurosurgery. 2020;87:E260–E262. doi: 10.1093/neuros/nyaa215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.LoPresti M.A., McDeavitt J.T., Wade K., et al. Letter: telemedicine in neurosurgery—a timely review. Neurosurgery. 2020;87:E208–E210. doi: 10.1093/neuros/nyaa175. [DOI] [PubMed] [Google Scholar]
- 30.Veinot T.C., Mitchell H., Ancker J.S. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc. 2018;25:1080–1088. doi: 10.1093/jamia/ocy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weber E., Miller S.J., Astha V., Janevic T., Benn E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27:1949–1954. doi: 10.1093/jamia/ocaa216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drewek R., Mirea L., Adelson P.D. Lead time to appointment and no-show rates for new and follow-up patients in an ambulatory clinic. Health Care Manag (Frederick) 2017;36:4–9. doi: 10.1097/HCM.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 33.MacGregor T.L., James H.E., Everett L., Childers D.O., Jr. Pediatric neurosurgery patients need more than a pediatric neurosurgeon. Part II. A clinical report: in the USA lack of parent/caregiver compliance interferes with the patient care sequence. Pediatr Neurosurg. 2016;51:229–235. doi: 10.1159/000445897. [DOI] [PubMed] [Google Scholar]