Abstract
Background
People with disabilities and chronic health conditions rely on a range of services and supports to complete daily tasks, maintain health, and participate in the community. Preliminary research suggests the COVID-19 pandemic greatly disrupted these services and this population may be particularly susceptible to unemployment.
Objective
Describe employment and service disruptions for individuals with disabilities and chronic health conditions during the onset of community-based spread of COVID-19 in the United States.
Methods
Adults with disabilities and chronic health conditions completed online surveys to report employment and service changes via multiple choice and open-ended questions. Multiple choice questions were analyzed using descriptive statistics; open-ended responses were coded using content analysis.
Results
Participants (n = 109): 79.8% female, 88.1% white, 77.121% completed a 4-year college degree or greater, 61.4% had annual income ≥$45,000. Only 14.9% of survey respondents reported disruptions in employment. On average, 54.0% of service changes were due to discontinuation, including loss of physical therapy, job coaching, community organizations, transportation, and peer supports. Other changes included a shift to virtual service delivery and family members taking the role of service providers.
Conclusions
Individuals with chronic health conditions and disabilities experienced service disruptions, even in a sample with considerably more economic, social, and educational privilege than the general population of people with chronic health conditions and disabilities in the United States.
Keywords: COVID-19, Chronic disease, Disability, Health services, Employment
Introduction
People with disabilities and chronic health conditions experience higher risk of severe complications or mortality from COVID-19.1, 2, 3 There have been several calls to attend to the specific challenges of people with disabilities during the pandemic, many of whom experienced healthcare disparities prior to the pandemic.4, 5, 6, 7, 8, 9, 10 One area of concern is loss of access to supports and services that people with disabilities rely upon to engage in work, volunteering, education, recreation/leisure, and to meet their daily needs.6 , 11
Although some services have transitioned to telehealth, not all direct hands-on supports and services can be provided in a telehealth format (e.g., support with daily life activities such as dressing or making meals). Providers who deliver hands-on supports have reported that they are uncertain about the continuity of services and that they lack guidelines for maintaining the safety of their clients and themselves.12 Barriers to accessing telehealth can also create service disruptions. Researchers describe challenges with bandwidth, WiFi access, access to a device for the telehealth session, and caregiver support during telehealth services.13, 14, 15 These disparities may be further exacerbated by socioeconomic status and regional differences in resources.13 , 15 , 16 Additionally, people with disabilities may experience challenges hearing or seeing when on video calls.6 , 15
Preliminary research suggests outpatient supports and services became scarce in the early stages of the pandemic. A survey from April 2020 reported that 83% of European countries had completely stopped outpatient services.17 Additionally, a survey conducted by the American Association on Health and Disability in April 2020 reported 56% of respondents who regularly access healthcare treatment were not able to maintain access.6 Furthermore, 23% of respondents who require direct home-based services lost access to this care,11 likely leading to significant health consequences and/or reliance on family members.14
We sought to deepen our understanding of the extent to which individuals with disabilities and chronic health conditions experienced service disruptions in the context of daily needs, work, volunteering, education, and recreation/leisure during the initial onset of community-based COVID-19 spread in the United States. We also sought to describe employment for individuals with disabilities and chronic health conditions during the first months of the COVID-19 outbreak in the United States, as loss of services needed to maintain employment may amplify this population’s existing vulnerability to unemployment.18 , 19 Our research questions were: During the first several months of the COVID-19 outbreak in the United States:
-
1)
To what extent did individuals with disabilities and chronic health conditions experience service disruptions related to their daily activities and participation?
-
2)
Did individuals with disabilities and chronic health conditions experience loss of employment at similar or different rates than the general population?
-
3)
What is the relationship between service loss and employment?
Method
Recruitment
We recruited participants across the United States through professional contacts, organizations serving individuals with disabilities and chronic health conditions, and social media across. One hundred and eighteen individual, organizational (e.g., United Cerebral Palsy, Epilepsy Foundation of New England, Great Lakes Ehlers-Danlos Syndrome Support, The Arc, Self Advocates Becoming Empowered, etc.), or social media contacts were made during recruitment, with several contacts receiving reminders after 4–6 weeks of initial contact. Individuals self-reported personal characteristics to determine their eligibility. Inclusion criteria were: 1) self-report of a developmental disability, chronic health condition, and/or physical disability, 2) live in the United States, and 3) ages 18–65. This population typically requires a range of in-person services for daily living. We excluded individuals whose only disability was a learning disability, ADHD, or a mental health condition, as these individuals typically do not receive the same range of services. Individuals with a temporary health condition or injury (e.g., broken bone) or living in an institutional setting (e.g., nursing home, skilled rehabilitation facility) were also excluded. At the time the study was designed, we anticipated gathering a large, heterogenous sample (>400 participants); however the small, homogeneous nature of our sample prohibited subgroup analyses.
Survey
The survey was administered online from May 2020–August 2020 using QualtricsXM. The survey was developed by the authors, based on their expertise in participation-based research with individuals with a range of disabilities and chronic health conditions. Two authors are researchers with a chronic health condition, and their experiences contributed to survey development. Additionally, an autistic researcher (and author) contributed to refinements in survey wording after the survey was complete. The survey evaluated participants’ use of supports or services prior to the COVID-19 pandemic (e.g., nursing, occupational therapy, peer support, etc.) across five areas of participation: daily living, education, employment, volunteering, and recreation/leisure. Participants reported if each support or service changed due to the pandemic (see Appendix 1 for questions).
Data analysis
The data were downloaded from Qualtrics™ and analyzed using IBM SPSS, version 26.
Descriptive analyses of mean, median, range, or frequencies were calculated to describe participant characteristics and changes in employment status. Due to small cell counts, level of education was dichotomized (<4 year college degree or ≥4 year college degree), as was family income (<$45,000 or ≥$45,000). Fisher’s exact tests were used to examine the associations between job loss with level of education and income. Due to low counts of services used, services were collapsed across area of participation with the final dichotomized variable indicating if a participant received the service or support in any area of participation. We also collapsed data regarding the type of changes in services or supports across areas of participation. To examine the relationship between service loss and changes in employment, we created a summary variable for the total number of discontinued services (sum of services discontinued, participant can’t receive, and chose not to receive) and conducted independent samples Mann-Whitney U tests of number of services lost between the groups of those who reported maintained versus lost employment.
Participants’ zip codes and self-reports of local pandemic-related laws/precautions were collected. However, the small sample prevented analysis of service changes by locality and pandemic-related laws/precautions.
Data from open-ended questions were analyzed using content analysis20 to triangulate quantitative findings and identify additional experiences not captured by multiple-choice questions. First, two coders reviewed all open-ended responses to reach consensus on the data relevant to the research questions. Then, one coder reviewed all relevant open-ended data to identify recurrent patterns, which were then used to develop codes. After initial codes were assigned to the data, the second coder reviewed the coded data to identity alternative interpretations and potential additional codes. Last, coded data was organized by related multiple-choice questions, thereby adding depth to the interpretation of close-ended responses.21 , 22
Results
Participant characteristics
The online survey was opened 232 times and 119 participants completed the survey (response rate of 51.3%). Participants represented 34 states, with the most participants from Massachusetts (n = 30). Most respondents to the primary survey reported living in suburban areas. The majority of participants reported a white racial identity, female gender identity, and had very high levels of education and high incomes (Table 1 ).
Table 1.
Participant characteristics.
| Variable | Primary survey (n = 109) |
|---|---|
| Age (mean, sd) | 39.96 (12.93) |
| Gender identitya | |
| Male | 11.0% |
| Female | 79.8% |
| Non-binary, genderqueer, or another gender identity | 8.3% |
| Prefer not to say | 0.9% |
| White racial identity | 88.1% |
| Under guardianship | 1.8% |
| Self-reported Primary disabilitya | |
| Autism | 7.3% |
| Speech/language impairment | 0% |
| Blindness/visual impairment | 1.8% |
| Traumatic or acquired brain injury | 2.8% |
| Deaf/hearing impairment | 2.8% |
| Specific learning disability | 1.8% |
| Intellectual disability | 0% |
| Mental or emotional health condition | 3.7% |
| Orthopedic impairmentb | 18.3% |
| Other health impairmentc | 52.3% |
| Family’s annual income | |
| <$20,000 | 12.8% |
| $20,000-$44,999 | 19.3% |
| $45,000-$139,999 | 39.4% |
| $140,000-$199,999 | 11.0% |
| >$200,000 | 11.0% |
| I don’t know | 5.5% |
| I feel like I have enough money to do the things I need and want to do | 0% |
| I feel like I don’t have enough money to do the things I need and want to do | 1.8% |
| I’m not sure if I have enough money | 3.7% |
| Highest level of education completed | |
| Some high school, high school, or GED | 4.6% |
| Some college or two year college degree | 18.4% |
| Four year college degree | 39.5% |
| Master’s degree | 22.0% |
| Doctorate degree | 15.6% |
Some participants did not respond to this question so the sum percent is <100%.
Example orthopedic impairments include: cerebral palsy (n = 4), arthritis (n = 3), spinal cord injury (n = 4), and fibromyalgia (n = 2). Some examples of other orthopedic impairments reported by only one participant include: Congenital amputations, spinal cord atrophy, and adhesive arachnoiditis.
Example conditions include: Ehlers-Danlos Syndrome (n = 7), arthritis (n = 6), fibromyalgia (n = 7), autoimmune conditions (n = 4), postural orthostatic tachycardia syndrome (n = 3). Additionally, some participants reported having other chronic health conditions, such as cancer, chronic Lyme’s disease, and diabetes.
Effects of COVID-19 on service use and access
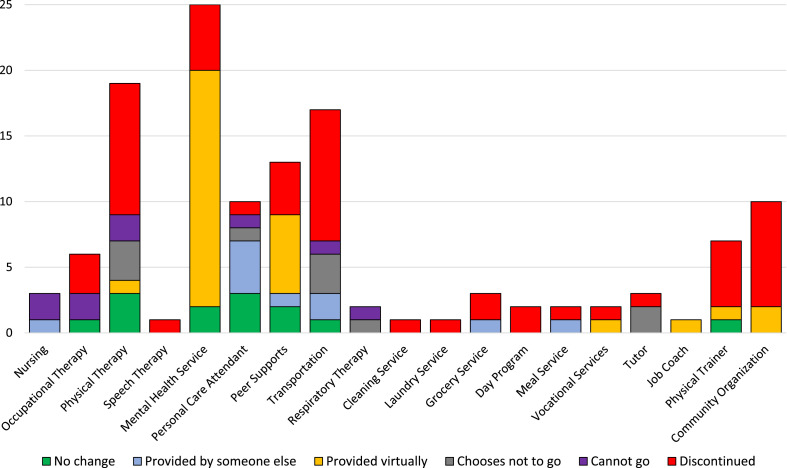
Participants received few supports and services prior to the pandemic (Fig. 1 ). The most common supports received were mental health services (23.9%, n = 26), physical therapy (16.5%, n = 18), transportation services (16.5%, n = 18), and peer support (12.8%, n = 14). On average, services received were impacted by the COVID-19 pandemic, with participants most commonly reporting services being discontinued. Across 16 service types, an average of 54% of service changes were due to the service being discontinued (range = 14–100%). Other changes to service provision were varied based on the type of service. For example, 72% of the changes in mental health services were due to the service taking place virtually, whereas 40% of the changes in personal care assistant (PCA) services were because someone new (primarily, family members) was now providing the service. For seven service types, some participants (range = 6–30%) reported no change in service provision (Fig. 1). Thirteen participants (11.9%) reported loss of at least 2 service types.
Fig. 1.
Service changes experienced during initial onset of community-based spread of COVID-19 in the United States.
In general, participants expressed a need for more skilled supports for completing daily tasks. For example, one person described experiencing a “lack of help with tasks I have difficulty with (laundry, cleaning, carrying grocery deliveries to my apartment).” Another shared that lack of PCA supports led them to “move back in with parents, thus eliminating my independence.” A different participant was able to maintain in-person supports, but reported that these supports were not ideal: “I have PCAs who I would never have hired before, however, because of COVID I am desperate.” Additionally, several participants described how service loss led to challenges with nutrition: “I am not eating as regularly as I would like because I cannot prepare enough food without help”; “Losing access to grocery delivery due to high demand and lack of availability impacted me greatly … it made me realize how much I rely on and need that service.”
Service loss not only impacted daily activities, but also was perceived to be associated with physical regression, increased medical complications, and pain. Some participants shared the sentiment that, “All my health problems are on hold because I can’t ask a doctor about them.” In one individual’s case, this led to hospitalization, “because I couldn’t get service from the urology team when I needed it [due to the COVID-19 outbreak].” Several participants specifically mentioned loss of physical therapy as contributing to “frequent dislocations,” “loss [of] muscle mass,” and “more pain with things like showering or attempting to cook for myself or do hobbies.” Therefore, several individuals were concerned about loss of function and/or physical regression during this time period.
Despite these challenges, some participants noted how the pandemic has led to increased accessibility of services, reporting it was “easier to attend medical appointments due to telemedicine options,” and hoped for “more virtual medical appointments” to continue when the pandemic concluded. Therefore, a subset of participants perceived transition of (some) services to telehealth as a benefit.
Loss of and changes in employment
Of the 67 participants who reported working prior to the pandemic, ten (14.9%) reported no longer working (Table 2 ). The average national unemployment rate during the time of data collection was 10.8%23; we observed a slightly higher unemployment rate among those previously working and a much higher employment rate compared to the general population of individuals with disabilities (29.4%).24 Exploratory analyses indicated that a higher proportion of participants who were no longer working had less than a 4-year college degree (Fisher’s exact test p = .026) and a family income less than $45,000 (Fisher’s exact test p = .007). Despite continuing to work, three participants reported that they have experienced challenges related to work, attributable to loss of health-related services. For example, one participant shared: “I can’t access [regular shots for migraine pain management] so I’ve needed to shift the way I do work—minimize time at the computer, taking breaks, cutting hours.” Another participant noted that increased stress during this time had led to an increased reliance on mental health services:
I get therapy to help me manage mental health issues so I can work effectively … I have needed my therapist more often and occasionally supplemented with a crisis line. I’ve also needed more medication to manage it … there are more days it’s hard to work because of … my mental health.
Table 2.
Employment status.
| Participants, n (%) | |
|---|---|
| Work status prior to the pandemic | |
| Not working | 42 (38.5%) |
| Receiving disability benefits | 11 |
| Looking for a job | 9 |
| Retired | 2 |
| Working | 67 (61.5%) |
| Work status at time of survey | |
| No longer working | 10 (14.9%a) |
| Lost job | 5 |
| Furloughed | 4 |
| Decided to stop working | 1 |
| Still working | 56 (83.6%a) |
| Working from homeb | 43 |
| Hours have increasedb | 11 |
| Working fewer hoursb | 7 |
Reported percent of those working prior to the pandemic (out of 67).
Participants could select all changes in work status that apply; 1 participant did not provide current work status.
Herein, some participants shared that even though they have maintained their jobs, they have experienced challenges at work related to their health.
Several participants noted that working from home led to improved wellbeing, and that they hoped employers would continue to be open to remote work in the future. For example, a participant who had not previously worked from home shared:
Now that I realize I can avoid those symptoms by working from home … All the time it takes me to get ready to go into an office can now be spent on acts of daily living. The pain and effort it takes to sit upright all day in an office designed for able bodied people is not worth it … I work from a hospital bed with an external monitor mounted on it. I can then use my energy and upright time for doing things instead of wasting it on work … In this respect my life has drastically improved.
Another participant reported: “I’m doing immeasurably better working from home. I had no idea how exhausting I was finding it to go [to work] before … My quality of life is so much better now.” These participants and others hoped to continue working from home in the future and anticipated that employers will be “more flexible about working from home. Maybe being more inclusive since we have the tech in place now [to ensure] that folks needing to be home can still engage.” Such comments suggest that within this subsample of individuals who retained employment, many perceived working from home as positively impacting their health.
Relationship between service loss and employment
Total number of discontinued services was not significantly different between participants who maintained employment (Mdn = 1.0) compared to those who lost employment (Mdn = 0.0) suggesting no association between service and employment loss, U(N employed = 56, N unemployed = 10) = 235.00, z = -.82, p = .412.
Discussion
This is one of the first studies to provide reports from individuals with disabilities and chronic health conditions about COVID-19’s impact on a range of services. We sought to describe the extent to which individuals with disabilities and chronic health conditions experienced service disruptions related to daily activities and participation (research question 1). In this sample, participants reported receiving few services and supports prior to the pandemic. However, most individuals who previously received services experienced some service loss. Mental health services were an exception to this finding, with these services often maintained through telehealth. These findings demonstrate that even those with financial, social, and educational privilege have experienced service losses that impact health and participation. As participants noted, service loss has the potential to lead to declines in health, potentially leading to greater health concerns and economic impacts. In many cases, individuals reported turning to family members to provide personal care services. If family members do not have proper training and are required to serve in several caregiving roles, this may increase family stress and/or result in improper care.25 , 26
As people with disabilities and chronic health conditions often receive care from multiple providers and agencies, they may benefit from service coordination and integrated care to ensure that essential services, or realistic alternatives, are available in the case of public health emergencies.27 , 28 Prospectively planning to draw upon community services may mitigate the impact of loss of professionally provided services and the need to rely on family members who do not have adequate training and may not have the flexibility in their workday to provide the level of care that is required. To ensure that individuals have consistent, high-level supports, policy should prioritize personal protective equipment and disease-surveillance (i.e., testing) for personal care attendants, and other providers who provide services that support individuals to maintain independence and health.
With regards to loss of employment, this study did not identify large differences between the general population and those with disabilities and chronic health conditions (research question 2). Within this sample, the relatively low rate of unemployment observed is likely attributable to high educational attainment, as individuals with higher educational attainment were more likely to maintain employment through remote work.29 Whereas a ten year average (2008–2018) suggests that approximately 22.7% of individuals with disabilities do not attain a high school diploma, and only 13.5% attained a bachelor’s degree or higher,30 almost all participants in this study had completed at least some college. This may have been attributable to the inclusion of people with chronic health conditions with onset later in life (e.g., arthritis, fibromyalgia), who may not have experienced health- or disability-related educational impacts. Further, analysis suggested no significant association between service loss and employment (research question 3). However, this may be due to the limited variability across measured variables within this sample.
Participants who continued to work remotely reported several health benefits of remote work. While limited, previous research suggests that employees may have heightened productivity working at home,31 , 32 and this perception has been maintained by workers during the pandemic.33 Policy makers could consider establishing remote work as a right for all workers, providing they are able to perform essential work functions in a remote-work context and employers should invest in the necessary technology to enact this universal accommodation.
Of note, this study documents the changes experienced primarily by individuals of white racial identity, female gender identity, with high incomes and educational attainment. Thus, our findings identify the impact of COVID-19 on supports and services for those who likely have fewer barriers to accessing supports compared to individuals with less financial, educational, and/or social privilege. Service losses and changes in employment reported by our sample have implications for practice and policy, and suggests the need for future research with a more heterogeneous sample.
Strengths, limitations and future research
Findings suggest that even those with financial and racial privilege still experienced health and disability-related barriers to receiving adequate support during the early COVID-19 outbreak. This study’s homogenous population helps to more confidently describe employment and service changes for white, economically and educationally privileged females with disabilities and chronic health conditions. However, readers should be cautious in generalizing our results to other populations, as individuals with disabilities who also identify with an underserved racial or ethnic group may experience an additive effect of unmet health care needs.34
The lack of representation of minority populations in health research is a long standing problem35 and this is not the first study on COVID-19 that has oversampled white and female individuals.11 However, racial, gender, and disability representation are essential for understanding the impact of COVID-19 as the health and economic effects of the COVID-19 pandemic are not distributed equally, further widening existing structural inequities in the United States.36, 37, 38 Barriers to achieving representative participation via survey methods may also be exacerbated by the personal and organizational stressors posed by the pandemic. Organizations did not consistently provide feedback about distribution of the survey and their reach, we were not able to calculate response rate for our overall recruitment efforts. Thus, attending to the issues of representation in COVID-19 research may require additional efforts, including financial compensation,39 use of social media to targeted groups,40 paper-based (mailed) surveys to reach those without access to technology, and use of a community-based participatory research approach.41 , 42 Future research must include a more representative sample to inform policy making, including the distribution of financial resources. If this is not done, the circumstances and experiences of marginalized communities will continue to go undocumented, further perpetuating disparities in this time of great need and turmoil. Finally, as participants perceived positive impacts of remote work, additional research should explore benefits and challenges of remote work for a more diverse group of individuals with disabilities, across multiple employment sectors, including those that have not previously implemented remote work (e.g., service industry, education, etc.).
Ethical review
All procedures were reviewed by the Boston University Institutional Review Board and designated as exempt.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dhjo.2021.101090.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Turk M.A., Landes S.D., Formica M.K., Gross K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disability Health J. 2020:100942. doi: 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antonini A., Leta V., Teo J., Chaudhuri K.R. Outcome of Parkinson’s disease patients affected by COVID-19. Mov Disord. 2020;35(6):906–908. doi: 10.1002/mds.28104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mares J., Hartung H. Multiple sclerosis and COVID-19. Biomed Pap. 2020;164(3):217–225. doi: 10.5507/bp.2020.033. [DOI] [PubMed] [Google Scholar]
- 4.Boyle C.A., Fox M.H., Havercamp S.M., Zuber J. The public health response to the COVID-19 pandemic for people with disabilities. Disability Health J. 2020:100943. doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Constantino J.N., Sahin M., Piven J., Rodgers R., Tschida J. The impact of COVID-19 on individuals with intellectual and developmental disabilities: clinical and scientific priorities. Aust J Pharm. 2020 Aug 28;177(11):1091–1093. doi: 10.1176/appi.ajp.2020.20060780. https://ajp.psychiatryonline.org/doi/pdf/10.1176/appi.ajp.2020.20060780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabatello M., Blankmeyer Burke T., McDonald K.E., Appelbaum P.S. Disaiblity, ethics, and health care in the COVID-19 pandemic. Am J Publ Health. 2020;110(10):1523–1527. doi: 10.2105/AJPH.2020.305837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turk M.A., McDermott S. The Covid-19 pandemic and people with disability. Disability Health J. 2020:100944. doi: 10.1016/j.dhjo.2020.100944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fullard M.E., Thibault D.P., Hill A., et al. Utilization of rehabilitation therapy services in Parkinson disease in the United States. Neurology. 2017 Sep 12;89(11):1162–1169. doi: 10.1212/WNL.0000000000004355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magaña S., Parish S., Morales M.A., Li H., Fujiura G. Racial and ethnic health disparities among people with intellectual and developmental disabilities. Intellect Dev Disabil. 2016;54(3):161–172. doi: 10.1352/1934-9556-54.3.161. [DOI] [PubMed] [Google Scholar]
- 10.Reichard A., Stolzle H., Fox M.H. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disability Health J. 2011;4(2):59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Drum C.E., Oberg A., Cooper K., Carlin R. American Association on Health and Disability; Rockville, MD: 2020. COVID-19 & Adults with Disabilities: Health and Health Care Access Online Survey Summary Report. [Google Scholar]
- 12.Cortis N., van Toorn G. Social Policy Research Centre: UNSW Sydney; Sydney: 2020. The Disability Workforce and COVID-19: Initial Experiences of the Outbreak. [Google Scholar]
- 13.Ameis SH, Mulsant BH, Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol Autism. 11(61). [DOI] [PMC free article] [PubMed]
- 14.Courtenay K., Perera B. COVID-19 and people with intellectual disability: impacts of a pandemic. Ir J Psychol Med. 2020;37:231–236. doi: 10.1017/ipm.2020.45. https://www.cambridge.org/core/journals/irish-journal-of-psychological-medicine/article/covid19-and-people-with-intellectual-disability-impacts-of-a-pandemic/EE2156045429D885B49CBBBEBA5A96C5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhai Y. A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom. 2021;90(1):64–66. doi: 10.1159/000509000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith J.A., Judd J. Health Promotion Journal of Australia; 2020. COVID-19: Vulnerability and the Power of Privilege in a Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Negrini S., Grabljevec K., Boldrini P., et al. Up to 2.2 million people experiencing disability suffer collateral damage each day of Covid-19 lockdown in Europe. Eur J Phys Rehabil Med. 2020;56(3):361–365. doi: 10.23736/S1973-9087.20.06361-3. [DOI] [PubMed] [Google Scholar]
- 18.Kraus L., Lauer E., Coleman R., Houtenville A. University of New Hampshire; Durham, NH.: 2018. Disability Statistics Annual Report. [Google Scholar]
- 19.Social Security Administration . 2019. Annual Statistical Report on the Social Security Disability Insurance Program, 2018.https://www.ssa.gov/policy/docs/statcomps/di_asr/index.html [Internet] Available from. [Google Scholar]
- 20.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 21.Creswell J.W., Plano Clark V.L., Gutmann M.L., Hanson W.E. In: Handbook of Mixed Methods in Social and Behavioral Research. Tashakkori A., Teddlie C., editors. Sage; Thousand Oaks: 2003. Advanced mixed methods research designs; pp. 209–240. [Google Scholar]
- 22.Wu Y.P., Deatrick J.A., McQuaid E.L., Thompson D. A primer on mixed methods for pediatric researchers. J Pediatr Psychol. 2019;44(8):905–913. doi: 10.1093/jpepsy/jsz052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bureau of Labor Statistics . Bureau of Labor Statistics; Washington, D.C.: 2020. Civilian Unemployment Rate.https://www.bls.gov/charts/employment-situation/civilian-unemployment-rate.htm [Internet] Available from. [Google Scholar]
- 24.Office of Disability Employment Policy . U.S. Department of Labor; Washington, D.C.: 2020. Disability Employment Statistics.https://www.dol.gov/agencies/odep/research/statistics [Internet] Available from. [Google Scholar]
- 25.Ersoy K., Altin B., Sarikaya B.B., Ozkardas O.G. The comparison of impact of health anxiety on dispositional hope and psychological well-being of mothers who have children diagnosed with autism and mothers who have normal children, in Covid-19 pandemic. Sosyal Bilimler Araştırma Dergisi. 2020;9(2):117–126. [Google Scholar]
- 26.Patrick S.W., Henkhaus L.E., Zickafoose J.S., et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020 Oct 1;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- 27.Factor A., Heller T., Janicki M. Institute on Disability and Human Development, University of Illinois at Chicago; Chicago, IL: 2012. Bridging the Aging and Developmental Disabilities Service Networks: Challenges and Best Practices. [Google Scholar]
- 28.Au M., Simon S., Chen A., Lipson D., Gimm G., Rich E. Mathematic Policy Research; 2011. Comparative Effectiveness of Care Coordination for Adults with Disabilities. [Google Scholar]
- 29.Division of Labor Force Statistics . United States Bureau of Labor Statistics; Washington, D.C.: 2020. Supplemental Data Measuring the Effects of the Coronavirus (COVID-19) Pandemic on the Labor Market [Internet]https://www.bls.gov/cps/effects-of-the-coronavirus-covid-19-pandemic.htm#highlights Available from. [Google Scholar]
- 30.Houtenville A., Boege S. University of New Hampshire, Institute on Disability; Durham, NH: 2019. Annual Report on People with Disabilities in America: 2018. [Google Scholar]
- 31.Bosua R., Kurnia S., Gloet M., Moza A. In: Social Inclusion and Usability of ICT-Enabled Services. Choudrie J., Tsatsou P., Kurnia S., editors. Routledge; New Delhi: 2017. Telework impact on productivity and well-being: an Australian study; pp. 201–223. [Google Scholar]
- 32.Bloom N., Liang J., Roberts J., Ying Z.J. Does working from home work? Evidence from a Chinese experiment. Q J Econ. 2015;130(1):165–218. [Google Scholar]
- 33.Baudot L., Kelly K. Social Science Research Network; Rochester, NY: 2020 Jul. A Survey of Perceptions of Remote Work and Work Productivity in the United States during the COVID-19 Shutdown. [Internet] [cited 2021 Jan 14]. Report No.: ID 3646406. Available from. [DOI] [Google Scholar]
- 34.Horner-Johnson W., Dobbertin K. Usual source of care and unmet health care needs: interaction of disability with race and ethnicity. Med Care. 2014:S40–S50. doi: 10.1097/MLR.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 35.Chen M.S., Lara P.N., Dang J.H.T., Paterniti D.A., Kelly K. Twenty years post-NIH Revitalization Act: enhancing minority participation in clinical trials (EMPaCT): laying the groundwork for improving minority clinical trial accrual: renewing the case for enhancing minority participation in cancer clinical trials. Cancer. 2014 Apr 1;120(Suppl 7):1091–1096. doi: 10.1002/cncr.28575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Artiga S., Corallo B., Pham O. Kaiser Family Foundation; 2020. Racial Disparities in COVID-19: Key Findings from Available Data and Analysis.https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-covid-19-key-findings-available-data-analysis/ [Internet] Available from. [Google Scholar]
- 37.Artiga S., Garfield R., Orgera K. Kaiser Family Foundation; 2020. Communities of Color at Higher Risk for Health and Economic Challenges Due to COVID-19.https://www.kff.org/coronavirus-covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/ [Internet] Available from. [Google Scholar]
- 38.Sehra S.T., Fundin S., Lavery C., Baker J.F. Differences in race and other state-level characteristics and associations with mortality from COVID-19 infection. J Med Virol. 2020;92(11) doi: 10.1002/jmv.26095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Largent E.A., Lynch H.F. Paying research participants: regulatory uncertainty, conceptual confusion, and a path forward. Yale J Health Pol Law Ethics. 2017;17(1):61–141. [PMC free article] [PubMed] [Google Scholar]
- 40.Ali S.H., Foreman J., Capasso A., Jones A.M., Tozan Y., DiClemente R.J. Social media as a recruitment platform for a nationwide online survey of COVID-19 knowledge, beliefs, and practices in the United States: methodology and feasibility analysis. BMC Med Res Methodol. 2020 13;20(1):116. doi: 10.1186/s12874-020-01011-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frerichs L., Lich K.H., Dave G., Corbie-Smith G. Integrating systems science and community-based participatory research to achieve health equity. Am J Publ Health. 2016 Feb;106(2):215–222. doi: 10.2105/AJPH.2015.302944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harris D.A., Pensa M.A., Redlich C.A., Pisani M.A., Rosenthal M.S. Community-based participatory research is needed to address pulmonary health disparities. Ann Am Thorac Soc. 2016;13(8):1231–1238. doi: 10.1513/AnnalsATS.201601-054PS. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.