Abstract
Background
Prior research has demonstrated that the needs of the disability community have not been met during public health emergencies. The COVID-19 pandemic has exacerbated existing inequities for many populations including people with disabilities, and data is needed to develop inclusive public health response policies.
Objective
To identify how COVID-19 has uniquely impacted the lives of adults with disabilities.
Methods
38 participants were recruited through disability advocacy groups and social media. Semi-structured virtual focus groups were conducted with adults (≥18 years) who self-identified as having a disability. Focus groups were conducted for each of six disability sub-groups: vision, hearing, mobility and physical, mental health, cognitive, intellectual, and developmental, and chronic illness. Using inductive coding, major themes were identified and compared across the disability sub-groups.
Results
Three major themes and thirteen sub-themes were identified from the focus groups. The three major themes comprised: new problems created by the pandemic, obstacles in daily life that were exacerbated by the pandemic, and broader changes to accessibility and disability identity. Sub-themes such as difficulty with COVID-19 testing and regular medical care were reported by participants of all disability sub-groups, while other sub-themes like direct care needs and medical rationing were reported by participants from a subset of the disability sub-groups.
Conclusions
These results indicate how the COVID-19 pandemic unequally impacts disabled people. The participants indicated that to fully address their needs, disability perspectives must be included in the public health pandemic response. As new research shows that COVID-19 can cause long-term disability, the urgency to ensure the disability community is part of public health policies will increase.
Keywords: COVID-19, Disability health, Disability equity, Qualitative, Emergency response
Introduction
One in four adults in the United States (U.S.) has a disability,1 and there is mounting evidence that the Novel Coronavirus SARS-Cov-2 (COVID-19) pandemic affects people with disabilities uniquely. Many people with disabilities have pre-existing conditions that place them at increased risk of COVID-19 infection and related mortality.2 In addition to the risk due to underlying medical conditions, people with disabilities are at increased risk due to barriers to accessing to healthcare. For example, disabled people are more likely to have unmet health needs due to cost,3 and many healthcare settings are physically inaccessible.4 These gaps in healthcare access may be exacerbated by the COVID-19 pandemic, a phenomenon that has been documented for other marginalized groups.5 , 6
Beyond biological factors and healthcare access, other aspects of life with a disability have been altered by the pandemic. COVID-19 prevention measures add difficulty to parts of daily life that are already modified by inaccessibility, such as: riding public transit,7 navigating a grocery store,8 and accessing information.9 Additionally, the pandemic has created a new set of obstacles for people with disabilities: social distancing conflicts with direct care needs,10 mask usage hinders communication,11 and hospital triage policies discriminate against patients with disabilities.12 These problems have been widely documented by journalists and disability advocates,13 but, as several commentary pieces point out,14 , 15 we lack data on how best to address them.
The COVID-19 pandemic has highlighted persistent health disparities for people with disabilities and underscores an urgent need to develop public health strategies that include people with disabilities, including emergency response. Although there has been work examining the impact of emergencies on the disability community, the majority focuses on natural disasters.3 , 16 Not only do we lack research on equitable pandemic policies, but current COVID-19 data collection efforts also fail to surveil disability.14 Existing data on disability and COVID-19 predominantly focuses on congregate care settings or on clinical outcomes for specific diagnoses.2 , 9 For example, one study found that people with intellectual and developmental disabilities are three times more likely to die from COVID-19 than patients without those conditions.17 This statistic raises the questions of why this disparity exists and whether the gap extends to people with other types of disabilities. Data on how the pandemic response affects people with all categories of disabilities living in the community does not yet exist. Without this data, we cannot craft a public health response that adequately takes into account the challenges faced by disabled people.
Additionally, there is a lack of data examining how the pandemic affects people with specific types of disabilities and the disability community as a whole. While there are systematic barriers impacting people with all types of disabilities, some of the obstacles created by the pandemic specifically impact people with a particular type of disability. For instance, d/Deaf people are suing over the lack of American Sign Language interpreters at government COVID-19 briefings,18 while people who cannot drive due to vision loss lack access to drive-through COVID testing.19 This approach to viewing disabled people as both a group with shared challenges and a heterogeneous population is unprecedented in COVID-19 research. This study aims to understand how challenges during the COVID-19 pandemic affected the disability community as a whole and differed between disability sub-groups.
The disability community has largely been left out of the public health response. However, disabled people’s unique life experiences could prove valuable in creating more inclusive pandemic policies for everyone. Qualitative data can begin to close this gap by identifying what problems the participants face in their own lives. Through virtual focus groups, this project assessed the needs and barriers for people with disabilities during the COVID-19 pandemic and amplified the lived experiences of disabled individuals by directly asking those most affected. The overall aim of this study is to identify how COVID-19 has uniquely impacted the lives of people with disabilities.
Methods
This study was approved by the Johns Hopkins Medical Institution Institutional Review Board (IRB #00249078), and informed oral consent was obtained prior to the study interviews. Qualitative methods were used in order to gather data on a wide range of issues impacting the disability community due to COVID-19. Focus groups were formed rather than individual interviews to allow participants to build off each other’s experiences. An ethnographic qualitative approach was selected in order understand how individual disabled people’s experiences represented the disability community as a whole.
The virtual focus groups were conducted from July to September of 2020, months after the pandemic spread to the U.S. and after the first coronavirus relief bill (the Coronavirus Aid, Relief, and Economic Security Act [CARES] Act) was passed. During this time, U.S. states fluctuated between various stages of reopening, and guidelines on COVID-19 prevention varied significantly from state to state.
Recruitment and participants
Recruitment materials were distributed to disability advocacy and support organizations across the U.S. via email. The recruitment text utilized broad language referring to adults with all disabilities. For accessibility, the recruitment materials included an image description and high-contrast and alternative text. We directly contacted 17 organizations, many of which distributed the recruitment information to their members via email, Twitter, Instagram, and/or Facebook. Individual members of the disability community and the research team also shared the recruitment information via personal social media and posted the recruitment material in disability advocacy Facebook groups.
The inclusion criteria for this study included: adults ages 18 and older, current resident in the U.S., self-identifying as having a disability, proficient in English or American Sign Language, and being able to provide informed consent. Although other people may have knowledge about issues facing people with disabilities, the study excluded non-disabled people to better focus on the perspectives of disabled people. In order to participate, interested individuals first completed an accessible survey (Qualtrics, Provo, UT) collecting their demographic information, including age range, racial or ethnic group, and gender pronouns, and verifying that they met the inclusion criteria. The survey asked participants to self-identify into one of six disability sub-groups, acknowledging that many people may fit into multiple categories: mobility and/or physical, cognitive, intellectual, and/or developmental, hearing, vision, mental health, and chronic illness.
From the pool of interested individuals, participants were grouped into 12 focus groups of 4 individuals who self-identified with the same type of disability. In selecting focus group members from the pool of interested participants, the goal was to represent a range of experiences. When possible, we worked to include no more than two people of the same age group, multiple racial/ethnic groups, and more than one gender. A research team member (S.E.) then followed up with the selected participants via email, and they completed a second survey (Qualtrics, Provo, UT) with their availability for the focus group. We contacted 5–6 individuals with the goal of forming focus groups of 4 people. In cases when the selected individuals did not respond, additional people with similar demographics were selected and sent a follow-up email. Four participants were scheduled for each call, but in many cases, only 2 or 3 of the participants scheduled to participate joined the call. Nine of the 48 selected participants did not participate. Reasons for not joining included emergent medical problems and changing family schedules. Consent to follow-up communication was collected in both surveys.
Out of the selected participants, we excluded one from the analysis because the participant indicated in the focus group interview that they were a parent of children with disabilities and did not have a disability themself.
Interview protocol
The semi-structured focus groups were conducted via Zoom (San Jose, CA). The sessions lasted 60–90 min with 5-min breaks every 30 min. Only audio, not video, of the focus groups was recorded. At the beginning of the call, the participants verbally consented to audio recording. To maintain privacy in Zoom, participants were given instructions prior to the focus group on how to change their Zoom name to a pseudonym and given the option to leave cameras off. During the focus group, the sensitive nature of the topic was acknowledged, and participants were instructed not to share information from other focus group members. The facilitator informed participants that they did not have to respond to every question and could take additional breaks or leave early for any reason. Participants did not receive compensation.
Communication Access Realtime Translation (CART) live-captioning was provided during all interviews in order to promote inclusion and accommodate the participants. The CART providers in the focus groups also signed a Health Insurance Portability and Accountability Act (HIPAA) waiver and were trained to keep all data confidential. As a further accommodation, participants were given the option to respond verbally or by typing in the chat.
This research team includes several researchers with a disability. One research team member (S.E.) facilitated all of the focus group interviews. An additional author observed (J.C. and C.C.) in two focus groups, in order to give them a better understanding of the transcripts they would later code. The facilitator also identifies as a person with a disability, which she disclosed to the participants in order to create a comfortable virtual environment. All members of the study team had qualitative interview training which included conducting a mock focus group and receiving feedback from other team members who have conducted several qualitative studies. Given that the facilitator is an active disability advocate, and because recruitment occurred through disability advocacy groups that she was connected to, three of the participants were familiar with her, but they were not people she contacted regularly.
The interview guide (Supplemental Materials) contained ten questions selected based on their relevance to both disability and the pandemic response. By reviewing issues that journalists and disability advocates were discussing, we identified topics that lacked data and wrote questions to fill that gap.
Analysis
A professional service (Landmark Associates, Phoenix, AZ) generated verbatim transcripts for analysis from the focus group audio recordings, and participant names were omitted. S.E. removed any further identifying information before sharing the transcripts with the other qualitative coders. The transcripts were not returned to the participants to check. The 12 focus group transcripts were analyzed by coding for themes in an accessible Excel (Microsoft, Seattle, WA) instrument created specifically for this study by J.C. which contained all transcripts and allowed coders to identify salient conversational excerpts and assign relevant codes. The analysis team consisted of S.E., J.C., and C.C., all trained in qualitative analysis and familiar with disability issues in both an academic and personal capacity. S.E., J.C., and C.C., independently coded focus group transcripts with two coders per transcript. A content analysis approach was used to identify themes from the participant comments. In instances of discrepancies between the two coders, the third team member served as the adjudicator. Inductive coding was used to identify codes based on the content of the transcripts. The three coders agreed upon a set list of codes based on each of their individual codes, then reviewed all of the transcripts and updated existing codes when necessary. Participants did not provide feedback in the analysis process.
After reviewing the resulting codes, 13 sub-themes were identified. The analysis team then grouped these 13 sub-themes into three major themes. For each sub-theme, the number of individuals that discussed each theme was determined and used to calculate the percentage of the entire study group and each disability sub-group discussing each theme. C.C. identified quotes from the coded portion of the transcripts that represented each sub-theme. The quotes were selected to be representative of the key issues discussed within each sub-theme while ensuring that the three selected quotes represented the range of disability experiences included in the study.
Results
Demographic characteristics
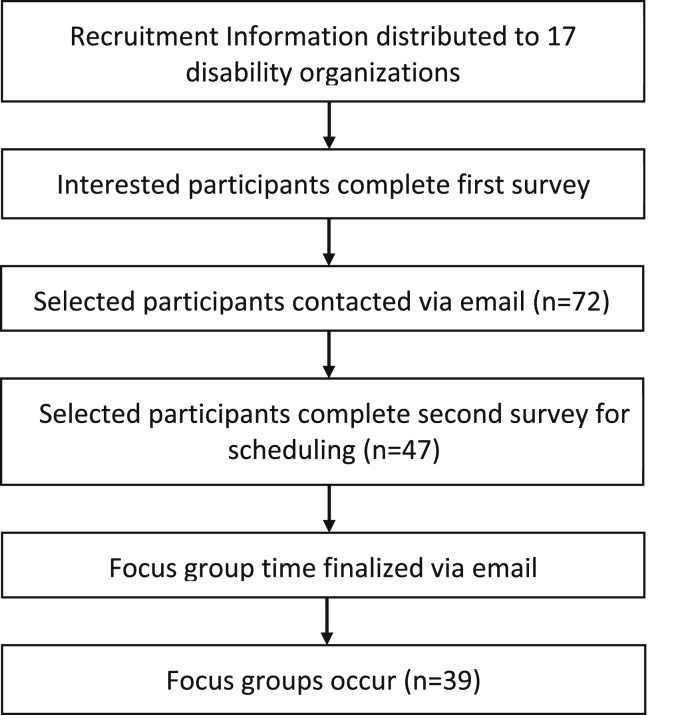
A total of 182 individuals responded to the recruitment survey, of which 39 joined twelve focus groups (Fig. 1 ). Two focus groups of 2–4 participants were conducted for each disability sub-group, which included a minimum of 4 and a maximum of 8 participants. One participant did not meet inclusion criteria because they indicated that they did not have a disability, leaving 38 participants in our analytic sample (Fig. 1). Out of the 38 participants, 5.3% reported their race as Asian, 10.5% Black or African American, 10.5% Hispanic or Latinx, 7.9% other, 63.2% white, and 2.6% Native American or Alaska Native. Table 1 reports the additional demographic information about the participants, including age group and gender pronouns.
Fig. 1.
Flow chart of recruitment process to form focus groups of participants with disabilities based on disability sub-type with the number of participants in each phase of the study.
Table 1.
Participant demographics comparing race/ethnicity, pronouns, and age group by disability sub-group.
| Disability Sub-Groups |
|||||||
|---|---|---|---|---|---|---|---|
| Demographic Characteristics | Vision |
Hearing |
Chronic Illness |
Cognitive, Intellectual, and/or Developmental |
Mobility and/or Physical |
Mental Health |
Total |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| 8 (21.1%) | 6 (15.8%) | 4 (10.5%) | 7 (18.4%) | 7 (18.4%) | 6 (15.8%) | 38 (100%) | |
| Race/Ethnicity | |||||||
| Asian | 1 (16.7%) | 1 (25%) | 2 (5.3%) | ||||
| Black or African American | 1 (12.5%) | 2 (28.6%) | 1 (16.7%) | 4 (10.5%) | |||
| Hispanic or Latinx | 1 (12.5%) | 2 (50%) | 1 (14.3%) | 4 (10.5%) | |||
| Other | 1 (12.5%) | 1 (25%) | 1 (14.3%) | 3 (7.9%) | |||
| White | 5 (62.5%) | 5 (83.3%) | 6 (85.7%) | 3 (42.9%) | 5 (83.3%) | 24 (63.2%) | |
| Native American | 1 (14.3%) | 1 (2.6%) | |||||
| Gender Identity (reported pronouns) | |||||||
| she/her | 6 (75%) | 4 (66.7%) | 2 (50%) | 3 (42.9%) | 4 (57.1%) | 3 (50%) | 22 (57.9%) |
| he/him | 2 (25%) | 2 (33.3%) | 1 (25%) | 3 (42.9%) | 3 (42.9%) | 2 (33.3%) | 13 (34.2%) |
| they/them | 1 (25%) | 1 (14.3%) | 2 (5.3%) | ||||
| multiple pronouns | 1 (16.7%) | 1 (2.6%) | |||||
| Age Group (years) | |||||||
| 18–29 | 1 (12.5%) | 1 (25%) | 3 (42.9%) | 1 (14.3%) | 4 (66.7%) | 10 (26.3%) | |
| 30–39 | 3 (37.5%) | 2 (33.3%) | 2 (50%) | 2 (38.6%) | 1 (14.3%) | 1 (16.7%) | 11 (28.9%) |
| 40–49 | 1 (12.5%) | 1 (16.7%) | 1 (25%) | 1 (14.3%) | 2 (28.6%) | 6 (15.8%) | |
| 50–59 | 2 (25%) | 1 (16.7%) | 1 (14.3%) | 1 (14.3%) | 1 (16.7%) | 6 (15.8%) | |
| 60–69 | 1 (12.5%) | 1 (16.7%) | 2 (28.6%) | 4 (10.5%) | |||
| 70+ | 1 (16.7%) | 1 (2.6%) | |||||
1Data from New obstacles and widening gaps: A qualitative study of the effects of the COVID-19 pandemic on U.S. adults with disabilities.
Focus group findings
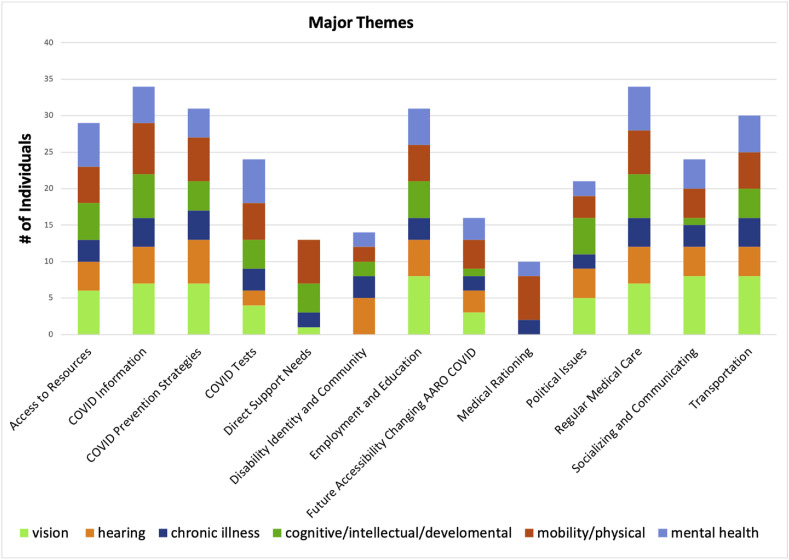
Three major themes and thirteen sub-themes were identified from the focus groups. Fig. 2 shows the sub-themes and how many individual participants mentioned them. As reported in Table 2 , the most commonly discussed sub-themes were access to COVID information, disruptions in regular medical care, employment and education, and transportation. Fig. 2 and Table 2 elaborate on how these 13 sub-themes differed across the six disability sub-groups represented in the study. Within each major theme and sub-theme, participants discussed a range of specific issues, as represented by the participant quotes in Table 3 .
Fig. 2.
Bar graph comparison of the number of participants who described each of the 13 sub-themes with colors of bars showing differentiation by disability sub-group.
Table 2.
Major themes described by participants across six disability sub-groups showing how many participants discussed each theme out of the 38 total participants and within each disability sub-group.
| Disability Sub-Groups |
|||||||
|---|---|---|---|---|---|---|---|
| Theme | Vision |
Hearing |
Chronic Illness |
Cognitive, Intellectual, and/or Developmental |
Mobility and/or Physical |
Mental Health |
Total |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Access to Resources | 29 (76.3%) | 6 (75%) | 4 (66.7%) | 3 (75%) | 5 (71.4%) | 5 (71.4%) | 6 (100%) |
| COVID Information | 34 (89.5%) | 7 (87.5%) | 5 (83.3%) | 4 (100%) | 6 (85.7%) | 7 (100%) | 5 (83.3%) |
| COVID Prevention Strategies | 31 (81.6%) | 7 (87.5%) | 6 (100%) | 4 (100%) | 4 (57.1%) | 6 (85.7%) | 4 (66.7%) |
| COVID Tests | 24 (63.2%) | 4 (50%) | 2 (33.3%) | 3 (75%) | 4 (57.1%) | 5 (71.4%) | 6 (100%) |
| Direct Support Needs | 13 (34.2%) | 1 (12.5%) | 0 (0%) | 2 (50%) | 4 (57.1%) | 6 (85.7%) | 0 (0%) |
| Disability Identity and Community | 14 (36.8%) | 0 (0%) | 5 (83.3%) | 3 (75%) | 2 (28.6%) | 2 (28.6%) | 2 (33.3%) |
| Employment and Education | 31 (81.6%) | 8 (100%) | 5 (83.3%) | 3 (75%) | 5 (71.4%) | 5 (71.4%) | 5 (83.3%) |
| Future Accessibility Changing as a result of COVID | 16 (42.1%) | 3 (37.5%) | 3 (50%) | 2 (50%) | 1 (14.3%) | 4 (57.1%) | 3 (50%) |
| Medical Rationing | 10 (26.3%) | 0 (0%) | 0 (0%) | 2 (50%) | 0 (0%) | 6 (85.7%) | 2 (33.3%) |
| Political Issues | 21 (55.3%) | 5 (62.5%) | 4 (66.7%) | 2 (50%) | 5 (71.4%) | 3 (42.9%) | 2 (33.3%) |
| Regular Medical Care | 34 (89.5%) | 7 (87.5%) | 5 (83.3%) | 4 (100%) | 6 (85.7%) | 6 (85.7%) | 6 (100%) |
| Socializing and Communicating | 24 (63.2%) | 8 (100%) | 4 (66.7%) | 3 (75%) | 1 (14.3%) | 4 (57.1%) | 4 (66.7%) |
| Transportation | 30 (78.9%) | 8 (100%) | 4 (66.7%) | 4 (100%) | 4 (57.1%) | 5 (71.4%) | 5 (83.3%) |
1Data from New obstacles and widening gaps: A qualitative study of the effects of the COVID-19 pandemic on U.S. adults with disabilities.
Table 3.
Thirteen sub-themes each accompanied by three representative quotes. Quotes were selected to represent the variety of issues discussed under that subtheme. Participant disability sub-group denoted in parentheses.
| Theme | Quote 1 | Quote 2 | Quote 3 |
|---|---|---|---|
| Access to Resources | Food access was as scary to me, if not scarier than COVID. (Mobility) | Trying to get shopper assistance—that’s been difficult. I know at some of the stores where they think, “Oh, well, we can’t do it ‘cause then we’re not social-distancing.” (Vision) | I was extremely concerned for a few weeks or so that I was going to run out of my medications, which not only keep me functioning, I actually get very sick if I miss any doses. (Mental Health) |
| COVID Information | I’ve seen press conferences that had no sign language interpreter, or broadcast like cable access channels that have no closed captioning. (Mobility) | I feel like just finding out what the stats are in my ZIP code is—I feel like Agatha Christie or some major sleuth, and maybe I’ll get it. (Vision) | The majority of my feedback about how to ride out this pandemic has come from other disabled people on the Internet because my team of medical professionals is just about as clueless as I am. (Chronic Illness) |
| COVID Prevention Strategies | When I approach someone […] that I’m going to have to speak to, and they’re wearing a mask, of course, […]—it’s almost like covering my eyes because I hear with my eyes when I speech-read. (Hearing) | I’ve literally had to stop taking [my service dog] in public with me because he’s cute, and he’s fluffy, and everybody flocks to him, and I cannot socially distance with him. (Chronic Illness) | Yeah, social distancing would not be bad if you could see how close somebody is, […] especially in noisy atmosphere or environments. It sounds like no one’s near you until they grab you or something, and it’s like, “Oh, geez.” (Vision) |
| COVID Tests | I’m really concerned for the focus on drive-through testing and how that doesn’t address people who don’t have cars. (Mobility) | I’ve tried to find testing that is not just drive-through testing in my area because I don’t have a car, and it’s been very difficult to find testing, as someone who is chronically ill, that I wouldn’t have to feel like I’m putting myself at risk for by taking a bus or public transport. (Mental Health) | I think that’s what I think of most in terms of my concerns about testing is just, some of us can’t even get to the point of testing because we’re just considered unworthy of care by virtue of our existence. (Chronic Illness) |
| Direct Support Needs | We need a backup system for home health workers because if they come down with the virus, what are we supposed to do? (Mobility) | I had to relieve one of my caregivers because that person thought it was all a bunch of baloney, didn’t believe in it, “I’m fine, you’ll be fine,” etcetera, etcetera. I said, “Okay, thank you for your service, but we’re gonna have to stop this.” (Mobility) | It’s difficult to get family and friends to take you anywhere they don’t have to. Fortunately, they’ve been really good about running some errands so if it doesn’t involve my going, it’s very doable. (Vision) |
| Disability Identity and Community | There’s been a lot of identity issues that have come up and having to advocate for myself and identify myself as somebody with a disability, and that’s not my normal experience in life, and I find that people don’t really know what to do with that information. (Hearing) | These preexisting conditions are literally segregating me out of this communal, collective human experience of suffering, and it feels like I’m not fully human in the same way, or not fully normal in that different way. (Hearing) | This pandemic is simulating to the non-disabled world what it’s like to be disabled and live with a disability, live with isolation, live with all the routine disruption, anxiety. (Cognitive/I/DD) |
| Employment and Education | I do not miss my commute at all, taking paratransit. I would sometimes be in-transit two, 3 h a day. (Mobility) | When I’ve had any issues with technical difficulties […] while in the office, there was usually somebody sighted around that I can say, “Can ya help with this?” […] I don’t have that now. (Vision) | As a visually impaired person teaching visual arts and dance and theater online, I can’t get my face really close to their painting anymore, […], or I can’t see the little details that they’re doing ‘cause I’m not able to get up close to them. I feel like half the teacher I was. (Vision) |
| Future Accessibility Changing as a result of COVID | Are we gonna be able to keep having Telehealth, or am I gonna be able to keep working from home when I need to? (Mental Health) | Outta this pandemic, I hope we move away from institution, shelter workshops, group homes. […] It’s like throwing somebody in the trash, disposable. It exposes our society. (Cognitive/I/DD) | The grocery delivery, the stronger radiuses, and the food delivery needs to be forever and not just because there’s a pandemic, and people want those services, by and large. Distance learning needs to be a forever option and not just an option because of the pandemic. (Chronic Illness) |
| Medical Rationing | I am concerned about medical rationing because I feel that it discredits the contribution that I have made to society as a whole. (Mobility) | At my hospital where I get all my care, they released a statement pretty early on saying that, if you’re disabled, you’re gonna get triaged out and left to die, essentially. (Chronic Illness) | Because of my age and my disability, I would probably be put back on the list if I needed lifesaving equipment, ventilator and such. […] I wouldn’t be considered worthy of saving. (Mobility) |
| Political Issues | No one has stepped up and brought us to the table and said, “What do you need? What do you need from us? How can we create policies that support you and support you in your lives?” (Chronic Illness) | It’s really annoying because plenty of dependent adults, especially college/grad students and disabled people, need that money [from the CARES Act stipend] because being a dependent on someone’s taxes doesn’t mean you can rely on them for everything. (Cognitive/I/DD) | People with chronic illness and disability have not been given prominent leadership roles to say, “We have already solved these problems as a collective. We already have answers. We already know how to redistribute and prioritize who needs resources. We can teach the rest of you who are suddenly finding yourself in a new normal what our regular normal looks like.” (Chronic Illness) |
| Regular Medical Care | It’s been just hoping every time that there’s been a new appointment, or procedure, or a visit to physical therapy that we don’t just accidently come into contact with somebody who might have the virus. (Chronic Illness) | I use telehealth also, and I liked it very much. I hope they let us do it after this [COVID-19]-- if this thing ever ends. (Mental Health) | I still don’t feel right telling—’cause these are people [nurses] who I rely on for medical care, so I don’t want to come across as rude to them by telling them to wear their mask properly or come across as snotty in such a way that I feel like it might impact the way that they treat me for the rest of the appointment. (Chronic Illness) |
| Socializing and Communicating | Captioning […] is the most important access to have. Even people with less hearing loss than I have, the masks also lower the amount of sound that they’re getting. (Hearing) | It’s lonely and isolating. I miss hugs. Touch is important, even for those with autism. (Cognitive/I/DD) | I know that my mental health is being severely compromised ‘cause I’m trying to keep myself safe, but I’ve had no real human interaction except for during medical procedures. (Chronic Illness) |
| Transportation | Social distancing with respect to transportation is obviously our real problem and not being sure what others around you are doing, whether they are practicing good social distancing and whether they are—whether or not they’re even wearing a mask or no, which is important to me. (Vision) | It has limited where I can shop, resulting in less transit access, since I’m scared to take public transit during this pandemic. (Cognitive/I/DD) | The paratransit systems in my area will not deliver you or pick you up from a testing site. If you can’t get there on the bus or on your own, you can’t do it. (Mobility) |
∗Parentheses denotes disability sub-group of participant.
1Data from New obstacles and widening gaps: A qualitative study of the effects of the COVID-19 pandemic on U.S. adults with disabilities.
COVID-19 impacts
Four sub-themes were identified that described new, disability-specific problems that have emerged due to the pandemic: COVID-19 testing, COVID-19 prevention strategies, access to COVID-19 information, and medical rationing. These issues were interrelated, as one participant described how their testing concerns were tied to medical rationing:
“I think that’s what I think of most in terms of my concerns about testing is just, some of us can’t even get to the point of testing because we’re just considered unworthy of care by virtue of our existence.” (they/them, Latinx or Hispanic, chronic illness)
A total of 34 participants reported obstacles in receiving information about the COVID-19 pandemic, including a lack of captions or alternative text, difficulty in finding information relevant to the disability experience, and overwhelming or confusing information. This sub-theme affected participants in all six disability sub-types. COVID-19 prevention strategies created new barriers for 31 participants. These barriers included mask usage causing difficulty communicating or obstructing residual sight, sanitizing precautions triggering allergic reactions, and social distancing measures clashing with personal assistance and healthcare needs. COVID-19 testing was challenging for 24 participants, with barriers such as inaccessibility of drive-through testing sites to participants who did not drive due to their disability. COVID-19 testing barriers, which had previously predominantly been reported for people with vision disabilities,19 were present for members of all six disability sub-groups.10 described fears of medical rationing and concerns that hospital triage systems would discriminate against them due to their disability if they were hospitalized due to the virus. Medical rationing was a concern for 6 out of 7 participants with mobility/physical disabilities and 2 out of 4 participants with chronic illnesses, but the theme was not discussed by the vision, hearing, and cognitive/intellectual/developmental groups.
Disruptions to daily life
Additionally, seven themes reflected how COVID-19 has disrupted daily life for participants. One participant captured this major theme with this succinct statement:
“If the gap exists before a major health crisis, you better believe that that’s gonna become the Grand Canyon when something like this happens to us.” (she/her, white, mobility/physical disability)
Access to resources refers to difficulties and changes in how participants acquired groceries and prescriptions during the pandemic. A total of 29 participants discussed these barriers, such as increased cost, item shortages, delivery wait times, and most commonly, difficulty receiving prescriptions. This sub-theme was similarly described by participants across the six disability sub-types. The pandemic brought about new challenges to meeting direct support needs for 13 participants, who struggled to receive daily assistance without greater risk for COVID-19. Direct support needs were discussed by 6 out of 7 participants with mobility/physical disabilities, 4 out of 7 of participants with cognitive/intellectual/developmental disabilities, and 2 out of 4 of participants with chronic illnesses. However, the hearing and mental health disabilities groups did not mention direct support needs. Employment and education were concerns for 31 participants, with similar concerns for participants across the disability sub-groups. Within that theme, telework and furlough, layoffs, or job searching were discussed the most. Political issues were discussed by 21 participants, including conversations about the stimulus check and specific state policies. Receiving regular medical care, meaning not COVID-19-specific medical care, was a challenge for 34 participants. Healthcare changes due to the COVID-19 pandemic included lapses in health insurance, disrupted or delayed care, additional barriers to accessing care, concerns about risks of receiving medical care, and transitions to telehealth. These healthcare access challenges were shared by members of all disability sub-groups. Socializing and communicating was a major topic of discussion, with 24 participants reporting both barriers to communication, such as inaccessible technology, and effects of social distancing, such as feeling isolated. Challenges to socializing and communicating were discussed by members of each disability type, but the theme was particularly prominent for the vision group, with all 8 participants with vision disabilities reporting these difficulties. Lastly, 30 participants discussed how the pandemic affected transportation access, referencing difficulties with and distrust in the safety of ride share, public transit, and paratransit. These transportation issues applied to participants from all six disability sub-groups.
Accessibility and identity
Two additional themes suggested how the pandemic broadly altered accessibility and disability identity across the six groups. 16 participants considered the lasting effects of the pandemic on accessibility, such as whether work from home accommodations and grocery delivery would outlast the pandemic. This sub-theme was reported by participants of all six sub-groups and was particularly prominent among participants in the mental health, cognitive, and chronic illness focus groups. Fourteen participants mentioned disability in the context of identity and community. This theme includes comments on how living with a disability afforded individuals’ unique knowledge for coping with the pandemic or how the disability community brought them assistance beyond what was available from medical professionals and news outlets. In the hearing disabilities group, 5 out of 6 of individuals discussed their relationship to disability identity and community changing due to the pandemic, while no one in the vision group brought up that topic. These two themes demonstrate the potential for the pandemic to spur positive changes for disabled people through increased virtual options and connection to the larger disability community. One participant expressed how she hoped that other people experiencing phenomena familiar to disability community could lead to change:
“This pandemic is simulating to the non-disabled world what it’s like to be disabled and live with a disability, live with isolation, live with all the routine disruption, anxiety.” (she/her, white, Cognitive/I/DD)
Discussion
The COVID-19 pandemic uniquely affected the disability community through the three major themes identified by this study- COVID-19 impacts, disruption to daily life, and accessibility and identity, which are major challenges that specifically affect people with disabilities. Although some sub-themes differed across the six disability sub-groups, the majority of the concerns were reported by members of all disability sub-groups, showing how the pandemic has affected the disability community as a whole. The results also highlight how disabled people may be at greater risk of contracting COVID-19, including: use of crowded public transit, need for close contact for personal assistance needs, barriers to COVID-19 tests, and lack of access to information about COVID-19 prevalence and prevention. Participants also discussed hope for potential positive outcomes from the pandemic, including work from home accommodations becoming commonplace, but expressed skepticism due to the lack of disability visibility in public health decision-making.
The findings from this study reinforce the need to examine the impact of COVID-19 more holistically, rather than just as morbidity and mortality, and consider impacts on daily life. From grocery shopping to taking public transit, participants indicated that these common barriers facing people with disabilities have been exacerbated by the pandemic. Many of these challenges are not new,4 , 16 , 20 , 21 and we must view the pandemic as a watershed moment for closing these gaps instead of letting these inequities continue to widen.
The results show the disability community’s unmet pandemic needs, implicating urgent public health policy action. Participants in all disability sub-groups experienced challenges in accessing COVID-19 tests, particularly due to drive-through testing. Mobile COVID-19 testing solutions must be implemented to equitably reach the disabled population. Participants shared experiences with direct support workers not having proper personal protective equipment or an understanding of the needed COVID-19 precautions. State and national COVID-19 relief policies should provide emergency funding and personal protective equipment for direct support workers. COVID-19 communications must serve the access needs of the disability community. Solutions proposed by participants include captions for video and audio content, alternative text for maps and diagrams, and plain language resources. Lapses in care, including mental healthcare, are dangerous for people with complex health needs, and public health policies need to ensure that disabled patients are able to manage their health without added risk of COVID-19. Participants discussed the need for clear guidance on how to go about their regular healthcare visits with the barriers added by COVID-19, such as masks hindering communication for individuals with hearing disabilities and policies prohibiting an accompanying person on their visits. Additionally, the participants’ perceived risk of COVID-19 was heightened by fears of medical rationing. Healthcare systems must adopt non-discrimination guidelines in their triage protocols to ensure that if people with disabilities are infected, they will receive equitable care. Participants reported mixed results with telehealth. Some felt optimistic that telehealth was finally being offered because it suits their access needs better, while other individuals found the technological obstacles burdensome. Telehealth should continue as an accommodation when possible, but an increased focus on accessibility and quality care is needed. The COVID-19 pandemic brought about accommodations that many participants wanted in the past, such as telework and telehealth. However, participants were frustrated that these needs were only met due to the widespread impact of the global pandemic on non-disabled people and were doubtful that the accommodations would continue into the future.
In contextualizing this study with the relevant literature, this study both supports existing research and demonstrates the need to include disability in broader work on COVID-19 in the US. Similar to the participants in this study, Boyle et al. also discuss information access as a key aspect of health protection for people with disabilities.15 Further, pre-pandemic research on disability health inequities was supported by participants’ discussion on how the barriers to healthcare that were present before COVID-19 were exacerbated.4 , 20 This finding suggests that further research on disability health inequities should take access issues from the COVID-19 pandemic into account. Currently, few major COVID-19 surveillance efforts collect disability information. One of the few that does found staggering disparities in mortality rates among individuals with developmental disabilities.17 By differentiating by disability sub-group, these results demonstrate that many of the issues facing people with intellectual and developmental disabilities also affect other disability groups, implicating the need to collect information on all disability sub-groups in COVID-19 surveillance. Emerging research shows that COVID-19 has lasting chronic illness symptoms for many survivors of the virus.21 With these long-term symptoms, many individuals will be newly disabled. Public health must include disabled people in the COVID-19 response now in order to prepare for emerging disability as the pandemic continues.
This study is one of the first to report the impact of COVID-19 among people with disabilities as a self-identified, heterogeneous population. This novel approach brought some challenges. Recruiting through disability advocacy groups yielded a sample of people already involved in disability advocacy. Because internet access was a requirement for participating, people with limited internet access are unlikely to participate, making the results not generalizable for the challenges faced by disabled people with limited internet access. Additionally, the recruitment did not collect information on education, which may affect participants’ access to social capital. Participants self-identified as one of the six disability sub-groups, but many participants had multiple disabilities. For example, deaf-blind people face unique challenges with COVID-19 prevention practices,22 but this study was unable to capture that perspective,2 nor other issues affecting people with multiple disabilities. The participants represented a wide range of disability types, so the results may not represent the full range of experiences of a particular disability type. A key strength of this study is that the use of virtual focus groups allowed for a geographically diverse sample. Participants unable to leave their homes due to the virus were able to participate. Another strength of the study was the range of accommodations offered, from accessible recruitment materials to captioned focus groups, which allowed people with disabilities who are often excluded from research to share their perspectives.
As a team of disabled researchers, we conducted this study about our own community. “Nothing about us without us” is the rallying cry of the disability rights movement, and we believe that this principle extends to research. We entered this work with a personal understanding of the population and designed a study that reflects the needs of our community. Navigating the heart-wrenching comments of fellow disabled people intensified our commitment to disability inclusion in the COVID-19 public health response. One participant put it best:
“We need to radically reimagine what type of person is a worthwhile person, and it needs to include all of us. […] People are not talking right now about the lives of people with disabilities. We’re just dying. We’re not being talked about. […] We’re not being seen.”
Disabled people are not being seen, and this work underscores an urgent need to change that. Our lives are worthwhile. When disabled people have a say in public health, from research to policy implementation, we can work towards health equity.
Conclusion
This study explored how the COVID-19 pandemic is uniquely affecting adults with disabilities in the U.S. These findings show how the pandemic has both created new challenges and exacerbated existing inequities for the disability community. Participants identified disability-specific obstacles to receiving COVID-19 testing, gaining information about the pandemic, and executing virus prevention strategies. Additionally, the participants’ daily access needs were made more difficult by COVID-19. This study demonstrates that to fully address these issues, disabled people’s needs must be considered in the pandemic response, and all public health policies and response strategies must be designed in partnership with the disability community.
Funding
This study was supported by NIA K01AG052640 and the Johns Hopkins University 10x20 Challenge Grant.
Declaration of competing interest
No known conflicts of interest.
Acknowledgments
Thank you to Dr. Tara Kirk Sell and Dr. Monica Schoch-Spana of the Johns Hopkins Center for Health Security.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.dhjo.2021.101103.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Okoro C.A., Hollis N.D., Cyrus A.C., Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults — United States, 2016. MMWR. Morbidity and mortality weekly report. 2018;67(32):882–887. doi: 10.15585/mmwr.mm6732a3. https://search.datacite.org/works/10.15585/mmwr.mm6732a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callender L.A., Curran M., Bates S.M., Mairesse M., Weigandt J., Betts C.J. The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front Immunol. 2020;11:1991. doi: 10.3389/fimmu.2020.01991. https://search.proquest.com/docview/2441610403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krahn G.L., Walker D.K., Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Publ Health. 1971;105(S2):S198–S206. doi: 10.2105/ajph.2014.302182. https://search.datacite.org/works/10.2105/ajph.2014.302182 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iezzoni L.I. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff. 2011;30(10):1947–1954. doi: 10.1377/hlthaff.2011.0613. https://search.datacite.org/works/10.1377/hlthaff.2011.0613 [DOI] [PubMed] [Google Scholar]
- 5.Kaufman H.W., Niles J.K., Nash D.B. Disparities in SARS-CoV-2 positivity rates: associations with race and ethnicity. Popul Health Manag. 2020 doi: 10.1089/pop.2020.0163. https://www.liebertpub.com/doi/abs/10.1089/pop.2020.0163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu J., Wang M., Lu F. COVID-19 and asian American pacific islanders. J Gen Intern Med : JGIM. 2020;35(9):2763–2764. doi: 10.1007/s11606-020-05953-5. https://search.proquest.com/docview/2438796819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams A.F. The Hill; June 13, 2020. COVID-19’s Transportation Implications for People with Disabilities. https://thehill.com/blogs/congress-blog/politics/502616-covid-19s-transportation-implications-for-people-with. Accessed October 8, 2020. [Google Scholar]
- 8.Hayes L.D.C. Washington City Paper; April 10, 2020. Residents with Disabilities Depend on Grocery Delivery Services. Now Everyone Wants a Slot. https://washingtoncitypaper.com/article/175501/dc-residents-with-disabilities-depend-on-grocery-delivery-now-everyone-wants-a-slot/. Accessed October 8, 2020. [Google Scholar]
- 9.Yap J., Chaudry V., Jha C.K., Mani S., Mitra S. World Development; 2020. Are Responses to the Pandemic Inclusive? A Rapid Virtual Audit of COVID-19 Press Briefings in LMICs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.What in-home social service providers and clients need to know about COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/in-home-social-services.html Accessed October 8, 2020.
- 11.Bryson Taylor D. The New York Times; June 4, 2020. For the Deaf, Social Distancing Can Mean Social Isolation. https://www.nytimes.com/2020/06/04/us/coronavirus-deaf-culture-challenges.html. Accessed October 8, 2020. [Google Scholar]
- 12.Scully J.L. Disability, disablism, and COVID-19 pandemic triage. J bioeth Inq. 2020:1–5. doi: 10.1007/s11673-020-10005-y. https://search.proquest.com/docview/2437128397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toward a disability-inclusive COVID19 response: 10 recommendations from the international disability alliance. International Disability Alliance. 2020:1–5. [Google Scholar]
- 14.Reed N.S., Meeks L.M., Swenor B.K. Disability and COVID-19: who counts depends on who is counted. The Lancet. Publ Health. 2020;5(8):e423. doi: 10.1016/S2468-2667(20)30161-4. 10.1016/S2468-2667(20)30161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyle C.A., Fox M.H., Havercamp S.M., Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disability and Health journal. 2020;13(3):100943. doi: 10.1016/j.dhjo.2020.100943. 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subramaniam P., Villeneuve M. Advancing emergency preparedness for people with disabilities and chronic health conditions in the community: a scoping review. Disabil Rehabil. 2019:1–9. doi: 10.1080/09638288.2019.1583781. https://search.datacite.org/works/10.1080/09638288.2019.1583781 [DOI] [PubMed] [Google Scholar]
- 17.Makary M. Fair Health; 2020. Risk Factors for COVID-19 Mortality Among Privately Insured Patients: A Claims Data Analysis. [Google Scholar]
- 18.Ortiz A. Lawsuit demands sign language at White House virus briefings. The New York Times. August 4, 2020. https://www.nytimes.com/2020/08/04/us/politics/asl-interpreter-lawsuit-coronavirus-trump.html Accessed October 18, 2020.
- 19.Berkon E. WAMU; March 2020. Coronavirus Tests Are Already Hard to Get. Having a Disability Makes it Harder. https://wamu.org/story/20/03/20/coronavirus-tests-are-already-hard-to-get-having-a-disability-makes-it-harder/. Accessed October 18, 2020. [Google Scholar]
- 20.Agaronnik N., Campbell E.G., Ressalam J., Iezzoni L.I. Exploring issues relating to disability cultural competence among practicing physicians. Disability and health journal. 2019;12(3):403–410. doi: 10.1016/j.dhjo.2019.01.010. https://www.ncbi.nlm.nih.gov/pubmed/30765256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaye H.S. Disability-related disparities in access to health care before (2008–2010) and after (2015–2017) the affordable care act. Am J Publ Health. 1971;109(7):1015–1021. doi: 10.2105/ajph.2019.305056. https://search.datacite.org/works/10.2105/ajph.2019.305056 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vargas T. They are deaf and blind, and social distancing has now taken their ability to touch. Wash Post. April 8, 2020 https://www.washingtonpost.com/local/they-are-deaf-and-blind-and-social-distancing-has-now-taken-their-ability-to-touch/2020/04/08/de5a9d42-79ae-11ea-9bee-c5bf9d2e3288_story.html Accessed November 27, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.