Abstract
Background
Medical subspecialties including neurosurgery have seen a dramatic shift in operative volume in the wake of the coronavirus disease 2019 (COVID-19) pandemic. The goal of this study was to quantify the effects of the COVID-19 pandemic on operative volume at 2 academic neurosurgery centers in New Orleans, Louisiana, USA from equivalent periods before and during the COVID-19 pandemic.
Methods
A retrospective review was conducted analyzing neurosurgical case records for 2 tertiary academic centers from March to June 2020 and March to June 2019. The records were reviewed for variables including institution and physician coverage, operative volume by month and year, cases per subspecialty, patient demographics, mortality, and morbidity.
Results
Comparison of groups showed a 34% reduction in monthly neurosurgical volume per institution during the pandemic compared with earlier time points, including a 77% decrease during April 2020. There was no change in mortality and morbidity across institutions during the pandemic.
Conclusions
The COVID-19 pandemic has had a significant impact on neurosurgical practice and will likely continue to have long-term effects on patients at a time when global gross domestic products decrease and relative health expenditures increase. Clinicians must anticipate and actively prepare for these impacts in the future.
Key words: Coronavirus, COVID-19, Length of stay, Morbidity, Mortality, Neurosurgery, Pandemic, Patient outcomes, Surgical volume
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; GDP, Gross domestic product; ICU, Intensive care unit; LOS, Extended length of hospital stay; RVU, Relative value unit
Introduction
Since its recognition in December 2019, coronavirus disease 2019 (COVID-19) has been confirmed in just less than 40 million individuals and is responsible for more than 1 million deaths globally.1 , 2 The disease had spread to 214 countries 8 months after being declared a pandemic by the World Health Organization.2 Before the emergence of COVID-19, the economic impact of health care spending had become a recent major point of discussion in the United States,3 , 4 with national health expenditure percentage relative to gross domestic product (GDP) projected to increase from 17.7% in 2018 to 19.9% in 2028.1 The pandemic has put further strain on an already unfavorable trend, with GDP decreasing globally as health expenditures increase, with hospitals becoming increasingly populated with critically ill, aged, and medically complex patients requiring emergent procedures and extended stays for multidisciplinary care despite disproportionate volume reductions in multiple medical subspecialties.5 , 6 The pandemic has increased the complexity of the medical insurance interfaces and reimbursement calculation, resulting in increased numbers of out-of-pocket costs, particularly for those with consumer-directed health plans.7
Regarding neurosurgery, case volume and weekly work relative value units (RVUs) have steeply declined, and populations have seen disproportionate increases in critical patients requiring emergency procedures secondary to both restrictions in elective cases and unexpected neurologic sequelae of severe COVID-19.8, 9, 10, 11 Rapid shifts in hospital patient characteristic proportions fueled by sharp increases in patients requiring multidisciplinary care in intensive care units (ICUs) and emergent procedures along with cessation and later restricted continuation of elective procedures put further strain on the system, requiring resource and personnel reallocation, and overnight flips in reimbursements garnered according to specialty. Facilities became dominated by a novel patient population with demographics similar to those reported to be at risk of extended length of hospital stay (LOS) beyond medical readiness for discharge, with major repercussions on hospital finances.12, 13, 14, 15, 16, 17
The pandemic has affected all forms of medical education, requiring medical student, nursing, residency, and fellowship programs to find alternative didactic measures to prevent indefinite delays in education.15 , 18 , 19 Spanning 2 major tertiary academic and comprehensive stroke centers in New Orleans, Louisiana, the Tulane-Ochsner neurosurgical residency program has faced similar challenges secondary to both social distancing restrictions as well as logistical strain mounting on the individual departments of each contributing institution.18 , 19 However, the effects of these changes on patient outcomes and service productivity have yet to be quantified. We report findings from a retrospective 2-center series comparing neurosurgical patients treated from March to June 2020 during as of yet height of the pandemic with patients treated in the same period in the previous year in an attempt to better characterize the effect of COVID-19 on operative volume, resident training, and patients.
Methods
Weekly operative neurosurgical volume at Ochsner Medical Center and Tulane Medical Center in New Orleans, Louisiana was retrospectively analyzed for the period from March to June 2020 compared with the average for the same period in the prepandemic years 2017–2019. Further analysis was then performed for this study period comparing 2019 with 2020, in which the records of all identified patients were reviewed for demographics, characteristics of performed procedures, resident involvement, individual surgeon volume, and outcomes as defined by morbidity and mortality. Procedures were categorized by subspecialty and Current Procedural Terminology codes into subgroups including craniotomy for trauma, craniotomy for tumor, endonasal approach for tumor, craniotomy for vascular pathology, endovascular treatment for vascular pathology, cerebrospinal fluid diversion, functional and epilepsy surgery, pediatrics surgery (including both cranial and spinal surgeries), stereotactic radiosurgery, spinal surgery, and minor procedures, the last including diagnostic digital subtraction angiography, ventriculostomy, lumbar puncture, muscle biopsy, peripheral nerve, and wound washout. Analysis regarding specific physicians and cases conducted was excluded if the surgeon was not employed during the entirety of both study periods. Outcomes changes in case rates, coverage characteristics, and subspecialties, as well as morbidity and mortality, were assessed. Univariate analysis was conducted via t tests for means, Fisher exact or χ2 tests for proportions, and the Mann-Whitney U test for LOS data. Statistical significance for all tests was taken as α ≥0.05.
Results
Prepandemic Operative Volume
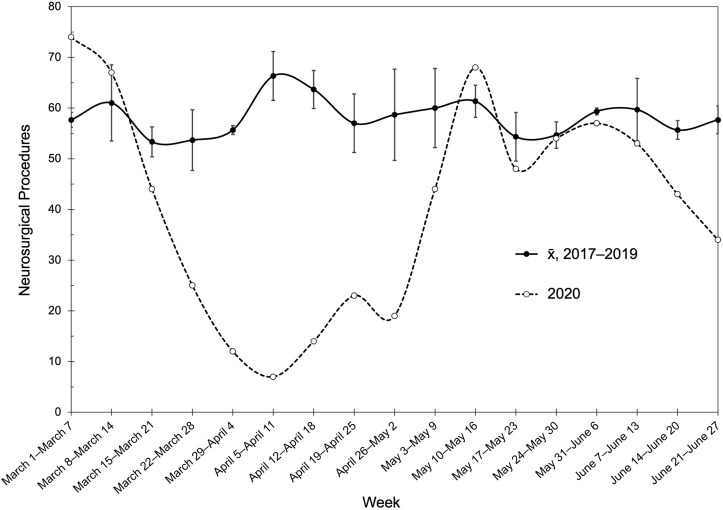
For the prepandemic period of March–June in 2017–2019, the average combined institutional operative volume was 58 procedures per week (range 53–66, Figure 1 ). Year-to-year variability remained low, with monthly average operative volumes of 243.7 (standard error, ±15.9) procedures in March, 259.3 (±11.5) in April, 264.7 (±8.4) in May, and 240.3 (±8.1) in June.
Figure 1.
Average weekly combined operative neurosurgical volume for Ochsner and Tulane Medical Centers from March 1 to June 27 in prepandemic years 2017–2019.
Operative Volume, Outcomes, and Coverage
Combined mean cases per month were significantly increased in the 2019 calendar period compared with 2020 (135 vs. 89 cases/month; P = 0.031). This trend was most pronounced in April, which saw a 77% reduction in operative procedures from 282 in 2019 to just 64 in 2020 (Figure 1). Cases were conducted by 11 full-time attending neurosurgeons active throughout the entire study period; 4 physicians (2 who left after the 2019 study period and 2 who began working during the 2020 study period) were excluded during subgroup analysis. All 4 excluded physicians worked at the same facility with departing staff fellowship-trained in complex minimally invasive spinal and peripheral neurosurgery and dual cerebrovascular surgery and incoming faculty in dual cerebrovascular and functional neurosurgery. Included physicians averaged significantly higher case volume in the 2019 window compared with that of 2020 (19.6 vs. 13.9 cases/month; P = 0.0025; Table 1 ) with again the most drastic discrepancy noted in April, which saw a case reduction of 74% per attending in 2020 compared with 2019.
Table 1.
Operative Outcome and Coverage Characteristics
| Variable | Year |
P Value | |
|---|---|---|---|
| 2019 | 2020 | ||
| Service output | |||
| Procedures per institution per month, average (standard deviation) | 135 (55) | 89 (49) | 0.031∗ |
| Procedures per attending neurosurgeon per month, average (standard deviation) | 19.6 (7.7) | 13.9 (9.3) | 0.0025∗ |
| Procedures not covered by a resident neurosurgeon, n (%) | 217 (20.1) | 83 (11.7) | <0.0001∗ |
| Procedures covered by 1 resident neurosurgeon, n (%) | 814 (75.4) | 576 (81.0) | 0.0064∗ |
| Procedures covered by ≥2 resident neurosurgeons, n (%) | 48 (4.5) | 52 (7.3) | 0.0114∗ |
| Adverse outcomes | |||
| Mortalities, n (%) | 23 (2.1) | 15 (2.1) | 1.0000 |
| Morbidities, n (%) | 33 (3.1) | 33 (4.6) | 0.0954 |
Normally distributed data compared with t tests and proportions compared with Fisher exact tests.
Significant difference with α = 0.05.
A combined 1079 cases (61.3%) were conducted during the 2019 study window, of which 20.1% (217/1079) went uncovered by a neurosurgery resident compared with 11.7% (83/711) in that of 2020 (P < 0.0001; Table 1). In addition, further analysis showed significant increased incidence of multiple residents scrubbing the same case in the pandemic window versus that of 2019 (7.3%, 52/711 vs. 4.5%, 48/1079; P = 0.0114) as well as single resident coverage across the same windows from 75.4% (814/1079) to 81.0% (575/711) (P = 0.0064). No significant differences were found in morbidity or mortality between groups.
Volume by Subspecialty
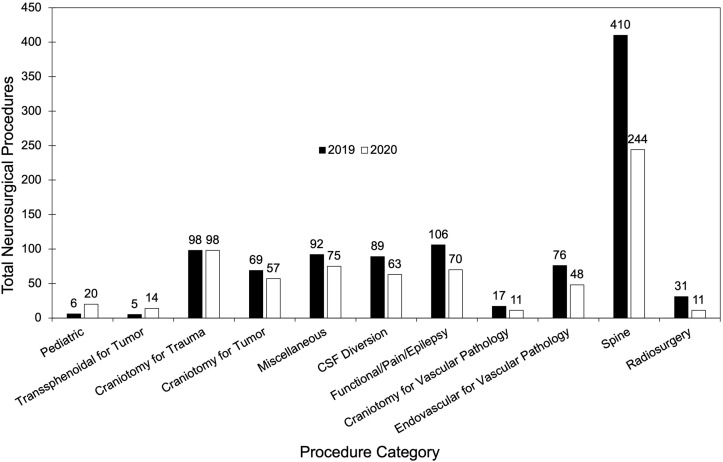
Subgroup analysis comprised 999 cases from the 2019 and 711 cases from the 2020 study windows (Figure 2 ). Nonsignificant changes were noticed in multiple subspecialties, including increases in pediatric and endonasal cases in 2020 and decreases in craniotomies for tumor, minor procedures, cerebrospinal fluid diversion, functional and epilepsy surgery, open and endovascular vascular cases, spinal surgeries, and radiosurgical procedures (Table 2 ). A significant relative increase in cases designated craniotomy for trauma was noted in the 2020 study window compared with the 2019 period (13.7%, 98/711 vs. 9.8%, 98/999; P = 0.0125). Significant relative decreases were noted with spinal surgery (41.0%, 410/999 vs. 34.3%, 244/711; P = 0.0050) and radiosurgery (3.1%, 31/999 vs. 1.5%, 11/711; P = 0.0344).
Figure 2.
Breakdown of all combined procedures performed at Ochsner and Tulane Medical Centers from March to June 2019 and 2020 by procedure category.
Table 2.
Distribution of All Combined Neurosurgical Procedures Performed Based on Subspecialty from March to June 2019 and 2020
| Code | Number of Cases by Year |
Difference (% Difference) | |
|---|---|---|---|
| 2019 | 2020 | ||
| Pediatric | 6 | 20 | 14 (233) |
| Transsphenoidal for tumor | 5 | 14 | 9 (180) |
| Craniotomy for trauma | 98 | 98 | 0 (0) |
| Craniotomy for tumor | 69 | 57 | −12 (−17) |
| Miscellaneous | 92 | 75 | −17 (−18) |
| Cerebrospinal fluid diversion | 89 | 63 | −26 (−29) |
| Functional/pain/epilepsy | 106 | 70 | −36 (−34) |
| Craniotomy for vascular pathology | 17 | 11 | −6 (−35) |
| Endovascular for vascular pathology | 76 | 48 | −28 (−37) |
| Spine | 410 | 244 | −166 (−40) |
| Radiosurgery | 31 | 11 | −20 (−65) |
| Total | 999 | 711 | −368 (−34) |
Patient Characteristics
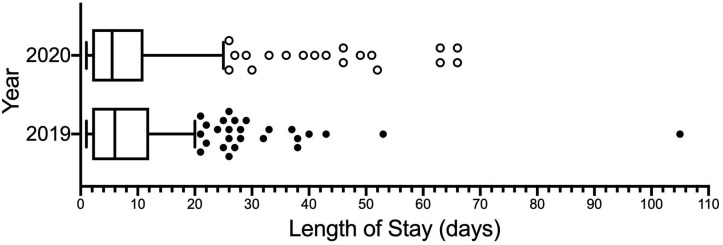
Treated patients in both calendar periods average in the mid-50s for age and were most often male. Regarding race, patients were most often white, followed by black, in both study windows (Table 3 ). The most common comorbidities in both periods were hypertension, current or former smoker, diabetes mellitus, and dyslipidemia (Table 4 ). No significant differences were found in LOS between study groups (Figure 3 ).
Table 3.
Results of Demographic Analysis and Length of Stay From One Institution
| Variable | Year |
P Value | |
|---|---|---|---|
| 2019 (N = 270) | 2020 (N = 200) | ||
| Demographics | |||
| Age (years), average (standard deviation) | 56.0 (15.7) | 56.8 (15.1) | 0.5832 |
| Sex, n (%) | |||
| Male | 109 (40.4) | 93 (46.5) | 0.1886 |
| Female | 161 (59.6) | 107 (53.5) | 0.1886 |
| Race, n (%) | |||
| White | 157 (58.1) | 106 (53.0) | 0.3014 |
| Black | 98 (36.3) | 79 (39.5) | 0.5012 |
| Other/unspecified | 15 (5.6) | 15 (7.5) | 0.4472 |
| Number of comorbidities, n (%) | |||
| None | 17 (6.3) | 17 (8.5) | 0.3735 |
| ≥3 | 137 (50.7) | 116 (58.0) | 0.1345 |
| ≥5 | 50 (18.5) | 37 (18.5) | 1.0000 |
| Length of stay | |||
| Median (interquartile range) | 6 (2–12) | 5.5 (2–11) | 0.5317 |
| Patients with length of hospital stay >30 days, n (%) | 9 (3.3) | 14 (7.0) | 0.0839 |
Normally distributed data compared with t tests, proportions compared with Fisher exact tests, and length of stay data compared with Mann-Whitney U test; significance determined with α = 0.05.
Table 4.
List of Comorbidities at One Institution Between March and June for 2019 and 2020
| Comorbidity | Number of Cases by Year |
|
|---|---|---|
| 2019 | 2020 | |
| Hypertension | 162 | 117 |
| Current or former smoker | 75 | 85 |
| Dyslipidemia | 64 | 54 |
| Diabetes mellitus | 50 | 46 |
| Previous neurosurgery | 55 | 41 |
| Previous cerebrovascular accident/stroke/subarachnoid hemorrhage/intracerebral hemorrhage | 26 | 29 |
| Thyroid disorder | 26 | 20 |
| Gastrointestinal disorder | 26 | 15 |
| Coronary artery disease | 25 | 12 |
| Depression/anxiety | 20 | 16 |
| Atrial fibrillation | 19 | 14 |
| Heart failure | 18 | 13 |
| Neuromusculoskeletal disorder | 21 | 11 |
| Non-CNS malignancy | 16 | 14 |
| Kidney disease | 17 | 10 |
| Chronic obstructive pulmonary disease | 13 | 13 |
| Substance abuse | 9 | 13 |
| Asthma | 10 | 8 |
| Seizure disorder | 8 | 9 |
| Hematologic disorder | 7 | 9 |
| CNS tumor/mass/abscess | 9 | 5 |
| Peripheral vascular disease | 5 | 7 |
| Nondepression/anxiety psychiatric disorder | 7 | 3 |
| Hepatitis C positive | 5 | 5 |
| Intravenous drug use | 4 | 6 |
| Non-CNS malignancy, known metastatic | 5 | 4 |
| Gout | 5 | 4 |
| Autoimmune disorder | 6 | 3 |
| Human immunodeficiency virus positive | 6 | 1 |
| Obstructive sleep apnea | 3 | 3 |
| Transient ischemic attack | 3 | 3 |
| Chiari malformation | 6 | 0 |
| Deep vein thrombosis | 2 | 3 |
| Dementia | 2 | 3 |
| Cardiac valvular disease/endocarditis/myopathy | 4 | 1 |
| Previous myocardial infarction | 3 | 2 |
| Previous pulmonary embolism | 2 | 2 |
| Morbid obesity | 2 | 2 |
| Traumatic brain injury | 1 | 2 |
| Pacemaker | 2 | 1 |
CNS, central nervous system.
Figure 3.
Length of stay duration for operative neurosurgical patients treated at Tulane Medical Center from March to June 2019 and 2020. Box, interquartile range; line, median; whiskers, 10th, 90th percentiles. CSF, cerebrospinal fluid.
Discussion
The COVID-19 pandemic has had a direct primary impact on the global economy, disrupting supply chains and trading routes, increasing unemployment, and decreasing consumer spending to cumulatively markedly decrease national GDPs.20, 21, 22 Secondary impacts stemming from increased health care expenditures may render this trend unsustainable without intervention.3, 4, 5, 6, 7 Reports investigating potential inefficiencies in the logistics of patient care as it pertains to neurosurgery before the advent of the pandemic identified that patients discharged beyond perceived medical readiness resulted in a significant economic impact to the health care facility.16 , 17 Such patients were found to be insured via a public plan and recipients of emergent interventions, hold multiple systemic medical comorbidities, and require prolonged ICU care and a discharge disposition to a specialized inpatient facility.16 , 17 This patient population has a high degree of overlap with critically ill patients requiring extended care associated with the COVID-19 pandemic.17 Such patients often require emergent procedures, many in the context of neurosurgical practice, with prolonged ICU stays.18 These trends were evident in our study as well, in which we noted significant proportional increases in emergent procedures and decreases in spinal and radiosurgical procedures, the latter of which have many elective patients. Simultaneously, public health coverage was projected to relatively increase, particularly with expansions in the Medicare sector, and overall numbers of uninsured patients were expected to increase before the pandemic.3 Hospital resource allocation has put increasing importance on the maintenance of isolated respiratory ICUs with staff and trainee reassignments as well as in providing constant availability of appropriate personal protective equipment in the wake of an increasingly limited supply.7 Despite overall increases in health expenditures, the pandemic has also drastically shifted proportional case volumes according to specialty, with the biggest declines noted in diseases often managed on an outpatient basis, further complicating the economic picture, particularly regarding subspecialty fields such as neurosurgery.8 , 9
Effects on Neurosurgical Volume
Pertaining to our academic program, which spans 2 major tertiary academic comprehensive stroke centers, we likewise noted a significant reduction in total operative volume in the calendar period straddling the outbreak of COVID-19 in Louisiana compared with the equivalent period in the previous year. Such findings are consistent with literature from other neurosurgical and clinical neuroscience institutions within the same time frame.23 , 24 Elective cases were prohibited outright at both institutions for the latter part of March and the entirety of April during the pandemic, and later time points saw the resumption of elective cases albeit with decreased capacity given reallocation of operating room availability to allow for a COVID-19–designated room. Both facilities saw decreases in the number of first start cases, forcing elective procedures to follow one another, often leading to cases being delayed until late at night, postponement thereby rolling the volume burden over onto a following day or resulting in outright cancellation. Many such cases were further delayed to accommodate proportional increases in emergent procedures. The trend reported has been likewise noted in previous studies, citing drastic declines in RVUs.8 , 9
Accordingly, the greatest reduction in procedures performed per institution occurred in April, which saw 1 week in which <10 procedures were performed across both our institutions combined. This period corresponded with the time frame immediately after the implementation of local shelter-in-place in Louisiana and social distancing ordinances, which, in addition to a concurrently imposed moratorium on many surgical procedures, may have inadvertently deterred symptomatic individuals from seeking neurosurgical treatment.14 , 23 , 25 , 26
As previously mentioned, the reduction in operative volume was not distributed evenly among the procedures, with the most significant decrease noted in spinal surgery. Spinal surgery represents an economic staple for neurosurgery, being reported as the disease condition with the highest rate of relative annual health expenditure.3 , 4 Instrumented spinal fusions have a significant population of elective procedures and have been increasingly performed, with annual reimbursement steadily increasing before the emergence of COVID-19.27, 28, 29 Speculatively, decreasing numbers of elective or nonemergent spinal procedures, secondary to both imposed restrictions as well as decreased likelihood of patients presenting or following up on an outpatient basis, provides a primary cause for reported decreases in weekly RVUs. Decreasing spinal volume does not only imply economic consequences, because it has been shown that delays in surgery are strongly associated with increased long-term mortality and morbidity,30, 31, 32 an effect shared among several nonurgent operative neurosurgical diseases.33
Spinal and cranial surgeries in addition to operations for polytrauma have also declined during the pandemic, likely as an indirect result of the modified population behavior that has been affected by recent social distancing restrictions, whereby individuals are at a relatively reduced risk of sustaining injuries that necessitate these types of intervention compared with previous years.34, 35, 36 Given that neither of our facilities are level 1 trauma centers, the volume of complex neurosurgical trauma was steady but relatively low compared with more specialized facilities. Consistent with the American Council for Graduate Medical Education,37 all emergent cranial procedures, including nontraumatic decompressive craniectomies and craniotomies for intracranial hypertension brought on by hemorrhage or large territory infarct were categorized in our report as “craniotomy for trauma.” As previously described, many critically ill patients with COVID-19 at both facilities correlated significantly with emergent neurologic procedures, consistent with disease histories and practice patterns described in previous reports.8 , 9 , 18
In addition, although we noted significant relative increases in pediatric (2.8%, 20/711 vs. 0.6%, 6/999; P = 0.0002) and endonasal procedures (1.4%, 14/711 vs. 0.5%, 5/999; P = 0.0489), there were few cases coded in each of these categories for both periods. Therefore, the perceived differences between years are likely to be a reflection of small sample size or coding factors. Although it remains to be seen how severe the true long-term disease burden caused by pandemic-related surgical delays will be, we believe that active anticipation of these effects will be essential in mitigating their impacts on patients in the future.
Effects on Resident Education
Along with decreasing trends in operative volume, the COVID-19 pandemic has had a pronounced effect on resident and medical student education, in some cases prompting temporary rearrangements in teaching structure secondary to shifts in available procedures and increased personnel requirements in newly developed respiratory ICUs.13 , 18 In an already changing training environment with work hour restrictions and a shift in treatment paradigms leading to changes in resident autonomy, it is becoming more difficult for residents to achieve the necessary practical case exposure that is needed to become proficient to a degree that would otherwise necessitate further fellowship training in many areas of subspecialization.38, 39, 40 Accentuated by the pandemic as evident in our findings by increased numbers of double scrubbed cases, decreased resident exposure to various techniques limits resident participation in available cases, creating a restrictive feedback loop. The advent of expensive simulation modalities for multiple areas of neurosurgery holds promise in increasing technical knowledge so that trainees may be more likely to rapidly gain manual skills when exposed to live cases; however, there is no evidence that such devices may replace or substitute live practice in resident education.41 Furthermore, such systems are less likely to be purchased by programs in a declining economy if not already secured.
Subspecialty training via fellowship will likely be increasingly necessary to obtain the necessary skill sets for practice. This speculated consequence is not necessarily deleterious, because, with most pandemic-driven effects, it is simply an acceleration of a preexisting eventuality, particularly for those seeking positions in academia.42 The ever-increasing subspecialization of medicine has made fellowship training a factor in job-market competitiveness regarding employment.43 More importantly, fellowships themselves provide an invaluable aspect of training, a unique period in which a trained participant can intensively study and practice in an extremely complicated specialized field of their desire. This period of intense subspecialty focus also provides an opportunity for clinical apprenticeship in which they learn first hand from the surgical experts of their field.38, 39, 40, 41, 42, 43
The concerning challenge elicited by COVID-19 is how to ensure that potential fellowship participants and those wishing to directly enter practice are adequately pretrained. Recent survey findings querying North American neurosurgical residents showed subjective concerns of senior residents regarding educational experiences in the COVID-19 era.44 Although whether or not their fears are valid remains to be determined, it would be wise for educational administrators to increase their priorities regarding operative training, particularly for midlevel and senior residents who may not see a full normalization in case volume until after graduation. Lower-level residents will still be able to benefit from increased proportional volumes in emergent cranial procedures given their relative technical simplicity, assuming that they are not boxed out because of increased demand for experience among their seniors. However, it is also likely that situations will arise in which multiple residents will be required to participate in a single procedure concurrently for the sake of obtaining adequate operative experiences per American Council for Graduate Medical Education requirements, despite the fact that their direct participation will be severely limited given the lack of a need for so many participants in the procedure, and this may further affect resident education.
Effect of Relative Hospital COVID-19 Censuses
Investigations into the differential impact secondary to regional and interfacility discrepancies in COVID-19 burden may further characterize the effect of the pandemic.8 , 9 , 24 Studies comparing decreasing case volumes across academic institutions in separate geographic regions in the United States showed substantial decreases in volume from monthly averages in April 2020, likely secondary to government restrictions that appeared in nearly all states after the initial outbreaks.24 At this time, the response of state governments in immediately imposing moderate practice restrictions was felt by nearly all facilities in all states simultaneously.
Because such actions were quickly determined to be economically unsustainable and, in many cases, transient, further investigations into lasting effects secondary to the prevalence of COVID-19 infection in a given region are warranted. Furthermore, the infection rates noted in the early days of the COVID-19 outbreak in the United States were preemptively analyzed and not illustrative of future trends in relative burden. For example, in the first few months of the pandemic, Louisiana, and specifically New Orleans, was considered a pandemic epicenter before being overshadowed by increasing case numbers in multiple states.45 After national dissemination and an unstable equilibrium brought on by long-term changes to attempt to control the spread of the virus and enable a continued functional economy and necessary services, Louisiana remains second in total cases per capita.46 Therefore, it would be interesting to compare long-term effects on relative case volume with regions with fewer afflicted citizens. Furthermore, correlations with other aspects of epidemiologic trends, such as new cases per day and remaining proportions of naive vulnerable populations, would be of interest.
Patient Characteristics and Outcomes
Combined institutional analysis showed no significant differences in periprocedural mortality or morbidity between periods in our study, consistent with similar reports.8 Surprisingly, we also found no significant differences in mean or proportional extended LOS, potentially circumventing further financial strain.16 , 17 These results provide reassurance that despite severe resource shortages and reallocation of medical personnel, indicated patients were adequately and safely treated with ostensibly no repercussions in hospital logistics.
Concerning patient demographics, we found no differences in the number of comorbidities per patient in 2020 compared with 2019. The most common comorbidities in both periods were hypertension, diabetes mellitus, and dyslipidemia, conditions increasingly associated with poor prognosis in COVID-19,47 which was not reflected in our mortality and morbidity findings. Further ongoing studies will help to clarify the continuously changing pattern of the COVID-19 pandemic as it relates to neurosurgical practice.
Limitations
This study is limited by nature as a 2-center retrospective analysis in which only in-hospital outcomes were assessed. As discussed earlier, the impact of delayed or cancelled operative management of progressive neurosurgical diseases such as cranial neoplasms and elective or nonemergent spinal disease requires long-term follow-up and analysis. The involved centers, Ochsner and Tulane Medical Centers, are private academic institutions and comprehensive stroke centers, and findings may not necessarily be representative of other neurosurgery departments. Assessment of the impact beyond institutional experience of the COVID-19 pandemic on operative volume, residency training, and patient outcomes necessitates multicenter involvement.
Conclusions
We retrospectively characterize impacts of the COVID-19 pandemic in the initial months of the 2020 outbreak compared with the same calendar period in prepandemic times on our neurosurgical residency program in New Orleans, Louisiana. We report significant reductions in operative case volume, with significant impact on residency training. In addition, we report no changes in patient morbidity and mortality; however, the delay or postponement of elective neurosurgical cases may put affected patients at increased risk of long-term complications. Because the impact on health expenditure trends by the pandemic in the United States is economically unsustainable, further investigations into various aspects of changes and challenges and how they are countered in academic centers is of vital importance.
CRediT authorship contribution statement
Mitchell D. Kilgore: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing, Software. Tyler Scullen: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing. Mansour Mathkour: Conceptualization, Methodology, Data curation, Writing - review & editing, Software. Rishawn Dindial: Data curation, Writing - original draft, Writing - review & editing. Christopher Carr: Writing - review & editing, Software. Tyler Zeoli: Writing - review & editing. Cassidy Werner: Writing - review & editing. Lora Kahn: Writing - review & editing, Supervision. Cuong J. Bui: Writing - review & editing, Supervision. Joseph R. Keen: Writing - review & editing, Supervision. Christopher M. Maulucci: Writing - review & editing, Supervision. Aaron S. Dumont: Writing - review & editing, Supervision.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2019;2020:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease 2019 (COVID-19): situation report, 96. (2020) https://www.who.int/docs/default-dsource/coronaviruse/situation-dreports/20200415-sitrep-86-covid-19.pdf?fsfvrsn1/4c615ea20_2 Available at: Updated October 16, 2020. Accessed October 16, 2020.
- 3.Centers for Medicare and Medicaid Services (CMS) National Health Expenditure Projections 2019-2028. https://www.cms.gov/ Available at:
- 4.Orr J.M., Leider J.P., Singh S., et al. Regarding investment in a healthier future: impact of the 2012 Institute of Medicine Finance Report [e-pub ahead of print] https://doi.org/10.1097/PHH.0000000000001209 J Public Health Manag Pract. [DOI] [PubMed]
- 5.The Lancet Oncology COVID-19 and the US health insurance conundrum. Lancet Oncol. 2020;21:733. doi: 10.1016/S1470-2045(20)30286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glied S., Levy H. The potential effects of coronavirus on national health expenditures. JAMA. 2020;323:2001–2002. doi: 10.1001/jama.2020.6644. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg M.D., Barry C.L., Schilling C.L., Kennedy-Hendricks A. Financial risk for COVID- 19-like respiratory hospitalizations in consumer-directed health plans. Am J Prev Med. 2020;59:445–448. doi: 10.1016/j.amepre.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajunaid K., Alqurashi A., Alatar A., et al. Neurosurgical procedures and safety during the COVID-19 pandemic: a case-control multicenter study. World Neurosurg. 2020;143:e179–e187. doi: 10.1016/j.wneu.2020.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sivakanthan S., Pan J., Kim L., Ellenbogen R., Saigal R. Economic impact of COVID-19 on a high-volume academic neurosurgical practice. World Neurosurg. 2020;143:e561–e566. doi: 10.1016/j.wneu.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicola M., Alsafi Z., Sohrabi C., et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanne J.H., Hayasaki E., Zastrow M., Pulla P., Smith P., Rada A.G. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090. doi: 10.1136/bmj.m1090. [DOI] [PubMed] [Google Scholar]
- 12.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 13.Keesara S., Jonas A., Schulman K. Covid-19 and health care's digital revolution. N Engl J Med. 2020;382:e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 14.Søreide K., Hallet J., Matthews J.B., et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107:1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dedeilia A., Sotiropoulos M.G., Hanrahan J.G., Janga D., Dedeilias P., Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(3 suppl):1603–1611. doi: 10.21873/invivo.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers C.M., Busch C.M., Cuoco J.A., Elias Z., Simonds G.R. Economic impact of hospitalization past maximal neurosurgical inpatient benefit. Cureus. 2018;10:e3567. doi: 10.7759/cureus.3567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linzey J.R., Kahn E.N., Shlykov M.A., Johnson K.T., Sullivan K., Pandey A.S. Length of stay beyond medical readiness in neurosurgical patients: a prospective analysis. Neurosurgery. 2019;85:E60–E65. doi: 10.1093/neuros/nyy440. [DOI] [PubMed] [Google Scholar]
- 18.Scullen T., Keen J., Mathkour M., Dumont A.S., Kahn L. Coronavirus 2019 (COVID-19)- associated encephalopathies and cerebrovascular disease: the New Orleans experience. World Neurosurg. 2020;141:e437–e446. doi: 10.1016/j.wneu.2020.05.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scullen T., Mathkour M., Maulucci C.M., Dumont A.S., Bui C.J., Keen J.R. Letter to the Editor. Impact of the COVID-19 pandemic on neurosurgical residency training in New Orleans. World Neurosurg. 2020;139:718–719. doi: 10.1016/j.wneu.2020.04.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guerriero C., Haines A., Pagano M. Erratum: Author Correction: Health and sustainability in post-pandemic economic policies. Nat Sustain. 2020;3:494–496. doi: 10.1038/s41893-020-0575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuzemko C., Bradshaw M., Bridge G., et al. Covid-19 and the politics of sustainable energy transitions. Energy Res Soc Sci. 2020;68:101685. doi: 10.1016/j.erss.2020.101685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lenzen M., Li M., Malik A., et al. Global socio-economic losses and environmental gains from the Coronavirus pandemic. PLoS One. 2020;15:e0235654. doi: 10.1371/journal.pone.0235654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma M., Lioutas V.A., Madsen T., et al. Decline in stroke alerts and hospitalisations during the COVID-19 pandemic. Stroke Vasc Neurol. 2020;5:403–405. doi: 10.1136/svn-2020-000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aljuboori Z.S., Young C.C., Srinivasan V.M., et al. Early effects of COVID-19 pandemic on neurosurgical training in the United States: a case volume analysis of eight programs. World Neurosurg. 2021;145:e202–e208. doi: 10.1016/j.wneu.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jayakumar N., Kennion O., Villabona A.R., Paranathala M., Holliman D. Neurosurgical referral patterns during the coronavirus disease 2019 pandemic: a United Kingdom experience. World Neurosurg. 2020;144:e414–e420. doi: 10.1016/j.wneu.2020.08.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.State of Louisiana Executive Department Proclamation number 33 JBE 2020: additional measures for COVID-19 stay at home. https://gov.louisiana.gov/assets/Proclamations/2020/JBE-33-2020.pdf Available at:
- 27.Alhourani A., Sharma M., Ugiliweneza B., et al. Ninety-day bundled payment reimbursement for patients undergoing anterior and posterior procedures for degenerative cervical radiculopathy. Neurosurgery. 2019;85:E851–E859. doi: 10.1093/neuros/nyz123. [DOI] [PubMed] [Google Scholar]
- 28.Al Jammal O.M., Delavar A., Maguire K.R., et al. National trends in the surgical management of lumbar spinal stenosis in adult spinal deformity patients. Spine (Phila Pa 1976) 2019;44:E1369–E1378. doi: 10.1097/BRS.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 29.Sheikh S.R., Thompson N.R., Benzel E., et al. Can we justify it? trends in the utilization of spinal fusions and associated reimbursement. Neurosurgery. 2020;86:E193–E202. doi: 10.1093/neuros/nyz400. [DOI] [PubMed] [Google Scholar]
- 30.Wagner S.C., Butler J.S., Kaye I.D., Sebastian A.S., Morrissey P.B., Kepler C.K. Risk factors for and complications after surgical delay in elective single-level lumbar fusion. Spine (Phila Pa 1976) 2018;43:228–233. doi: 10.1097/BRS.0000000000002282. [DOI] [PubMed] [Google Scholar]
- 31.vanTol F.R., Choi D., Verkooijen H.M., Oner F.C., Verlaan J.J. Delayed presentation to a spine surgeon is the strongest predictor of poor postoperative outcome in patients surgically treated for symptomatic spinal metastases. Spine J. 2019;19:1540–1547. doi: 10.1016/j.spinee.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 32.Kim E.J., Wick J.B., Stonko D.P., et al. Timing of operative intervention in traumatic spine injuries without neurological deficit. Neurosurgery. 2018;83:1015–1022. doi: 10.1093/neuros/nyx569. [DOI] [PubMed] [Google Scholar]
- 33.Noorani I., Sanai N. Surgical management of incidental gliomas. Neurosurg Clin North Am. 2017;28:397–406. doi: 10.1016/j.nec.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 34.Kamine T.H., Rembisz A., Barron R.J., Baldwin C., Kromer M. Decrease in trauma admissions with COVID-19 pandemic. West J Emerg Med. 2020;21:819–822. doi: 10.5811/westjem.2020.5.47780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nuñez J.H., Sallent A., Lakhani K., et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51:1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pinggera D., Klein B., Thomé C., Grassner L. The influence of the COVID-19 pandemic on traumatic brain injuries in Tyrol: experiences from a state under lockdown [e-pub ahead of print] https://doi.org/10.1007/s00068-020-01445-7 Eur J Trauma Emerg Surg. [DOI] [PMC free article] [PubMed]
- 37.Accreditation Counsel for Graduate Medical Education (ACGME). Neurological surgery case log defined case categories and required minimum numbers. Available at: https://www.acgme.org/Specialties/Documents-and-Resources/pfcatid/10/Neurological%20Surgery. Accessed October 16, 2020.
- 38.Sarkiss C.A., Riley K.J., Hernandez C.M., et al. Academic productivity of US neurosurgery residents as measured by H-Index: program ranking with correlation to faculty productivity. Neurosurgery. 2017;80:975–984. doi: 10.1093/neuros/nyx071. [DOI] [PubMed] [Google Scholar]
- 39.Lipsman N., Khan O., Kulkarni A.V. "The actualized neurosurgeon": a proposed model of surgical resident development. World Neurosurg. 2017;99:381–386. doi: 10.1016/j.wneu.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 40.Karsy M., Henderson F., Tenny S., et al. Attitudes and opinions of US neurosurgical residents toward research and scholarship: a national survey. J Neurosurg. 2018;131:252–263. doi: 10.3171/2018.3.JNS172846. [DOI] [PubMed] [Google Scholar]
- 41.Badash I., Burtt K., Solorzano C.A., Carey J.N. Innovations in surgery simulation: a review of past, current and future techniques. Ann Transl Med. 2016;4:453. doi: 10.21037/atm.2016.12.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson T.A., Langston R.G., Wong K.H., Rodriguez A. Characteristics and career outcomes of Neurosurgery Research and Education Foundation research fellowship recipients. J Neurosurg. 2019;132:802–808. doi: 10.3171/2018.10.JNS18859. [DOI] [PubMed] [Google Scholar]
- 43.Ronna B., Guan J., Karsy M., Service J., Ekins A., Jensen R. A survey of neurosurgery residency program coordinators: their roles, responsibilities, and perceived value. Cureus. 2019;11:e4457. doi: 10.7759/cureus.4457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pelargos P.E., Chakraborty A., Zhao Y.D., Smith Z.A., Dunn I.F., Bauer A.M. An Evaluation of Neurosurgical Resident Education and Sentiment During the Coronavirus Disease 2019 Pandemic: A North American Survey. World Neurosurg. 2020;140:e381–e386. doi: 10.1016/j.wneu.2020.05.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention Coronavirus Disease 2019, Cases in the US. https://www.cdc.gov/coronavirus/2019-ncov/cases-us.html Available at:
- 47.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]