Abstract
Restricted access to healthcare during COVID-19 pandemic warranted an urgent adaptation of telemedicine practice. We describe a synchronous, stepwise (telephonic, video, and in-person consultation) direct-care model. From 18th May to 31st August 2020, 128 new and 198 follow-up patients received consultation. Eighty-nine percent of new patients required video-consultation. Sixty-eight percent of follow-up cases were managed by telephonic consultation. A third of new and a fifth of the follow-up patients had to be called for physical consultation. Limited access to and understanding of the technologies, potential breach in privacy, and restrictions imposed on online prescription of medications posed significant challenges.
Keywords: Telemedicine, Stepwise approach, Video conferencing, In person care
1. Background
A nation-wide complete lockdown was implemented in India on 25th March 2020 to combat the coronavirus disease 2019 (COVID-19) pandemic. Since then, the out-patient services in many institutes including ours were either completely shut down or heavily restricted. The travel restrictions resulted in difficult access to the already limited number of treatment services. The stay-at-home orders and advisory to maintain physical distance might also have deterred patients to seek in-person medical help except for emergencies.
The nation-wide lockdown and resultant restrictions further widened the already existing significant unmet treatment need for substance use disorders (SUD) (Ambekar et al., 2019). Telemedicine might play a pivotal role in reducing the treatment gap by improving the access and availability of evidence-based care, not only during this time of crisis but also in usual times (Lurie and Carr, 2018; Wosik et al., 2020).
Telepsychiatry was in practice since around two decades in various parts of India. The mobile telepsychiatry initiative in Pudukotti, Tamilnadu by Schizophrenia Research Foundation, and the telepsychiatry service as a part of Maharashtra State Telemedicine project suggested the feasibility of incorporation of both synchronous and asynchronous telepsychiatry into existing clinical practice (Rangaswamy, 2012; Balasinorwala et al., 2014). Malhotra et al. (2017) created a Clinical Decision Support System as an accurate and valid screening and diagnostic tool in telepsychiatry. Another study in National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru have shown efficacy of teleconsultation in collaboration with the primary care physician for providing psychiatric services to the homeless people in a rehabilitation centre (Kulkarni et al., 2020). The telemedicine centre of NIMHANS also follows a synchronous telepsychiatry model for non-emergency aftercare in a section of patient. In a pilot study, the acceptability and satisfaction were found to be higher in the telepsychiatry consultation than in-person consultation (Das et al., 2020). During the early stage of COVID-19 pandemic, the same group of researchers proposed expansion of the services (Manjunatha et al., 2020). In sum, the existing evidence suggests the acceptability and feasibility of telepsychiatry services in India. Nonetheless, none of these afore-mentioned services were particularly designed to deliver care to patients with substance use disorders, which might have a different set of clinical, social, legal, and service-related needs. Moreover, most of these services were designed before the publication of the Telemedicine Practice Guideline (TPG) of India.
The TPG was released on 25th March 2020 (the same day the lockdown was imposed) and was formally notified in the Gazette of the Government of India on 14th May 2020 (Telemedicine Practice Guidelines, 2020). Telepsychiatry guidelines were also released in May 2020.The aim of both the guidelines were to give practical advice to clinicians regarding the ‘setting up, implementation, administration and provision’ of teleconsultation service, so that it can be integrated to the usual clinical practice (Bada Math et al., 2020).
Although the need for adopting TPG in the addiction healthcare services in order to adapt with the current situation in India has been highlighted (Arya and Gupta, 2020; Kar et al., 2020; Dubey et al., 2020), to our knowledge there is dearth of published detailed model of healthcare delivery services for SUD in India utilizing telemedicine. A wider application of smartphone based teleconsultation for patients with substance use disorders started during the lockdown due to COVID-19 pandemic (Ganesh et al., 2020). We have earlier published interim standard operating procedures for running opioid substitution therapy service (Basu et al., 2020) but that is an in-person service by definition because of the necessity to dispense buprenorphine in person.
Here we describe the telemedicine model adopted by the Drug De-addiction & Treatment Centre of the Postgraduate Institute of Medical Education & Research, Chandigarh. This publicly funded addiction treatment and research center is one of the three centers of excellence in the country and caters to several northern and western states of India. It has a multi-disciplinary out-patient service consisting of psychiatrists, medical doctors, nurses, clinical psychologists, psychiatric social workers, and counselors. It has an integrated dual diagnosis clinic and opioid agonist treatment clinic as components of the out-patient services. Psychoeducational group therapy is an essential component of these special clinics. The challenge was to incorporate and integrate the practice of telemedicine within the TPG framework but also in a stepwise hierarchical logistics service model depending upon the need and contingencies of the situation. This brief communication addresses how we responded to the challenge and what we learnt so that others may apply or further refine this model.
2. The PGI stepwise direct care model
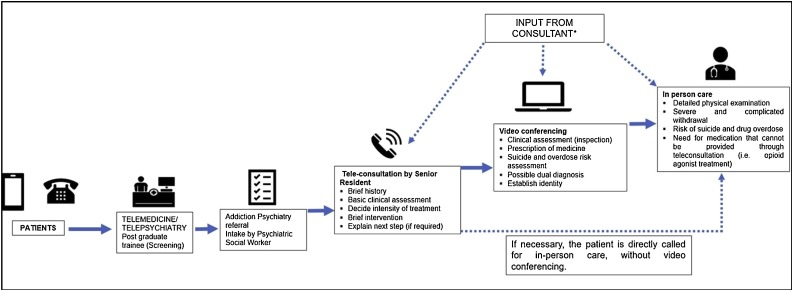
We adopted a synchronous and stepwise direct care model with three hierarchical steps of service delivery: telephonic, video, and in-person consultation. This was a stand-alone model for our addiction treatment centre, conceived (a) to address the varying needs and legal mandates for the treatment of SUD; (b) for the optimal use of the limited resources. Fig. 1 shows the structural and functional elements of the model in a schematic way.
Fig. 1.
Flow-chart showing the step-wise approach for tele addiction service.
Registration can be done by the patient either telephonically or online. The information regarding the telephone numbers and online procedure is circulated through advertisements on the newspapers, prominent displays on the hospital’s website, and sending text messages to the already registered patients. The telemedicine and the telepsychiatry units operated by undergraduate doctors and postgraduate trainees, respectively, act as gatekeepers and transfer the patients’ information to appropriate specialties. The senior residents (SR) working in addiction psychiatry (psychiatrist) contact the registered patients on telephone within 24 h of their initial registration.
2.1. STEP 1: telephonic care
All consultations start with an initial intake by a psychiatric social worker. Telephonic consultation is provided by the SR on the contact number provided by the patient. The patients’ identity is corroborated (with the registered details) at the beginning of the consultation. The aims of the telephonic consultation are to: (a) take a brief history and do basic clinical assessment, (b) decide about the intensity of treatment needed, (c) provide brief psychological interventions, and (d) explain the next step and its logistics, if required. TPG does not permit prescription of medications for first audio-consultation. Therefore, exclusive telephonic consultation is feasible only for a subgroup of patients who would not require any medications.
2.2. STEP 2: care through videoconferencing (VC)
Following the telephonic consultation, VC is considered in the following scenario: (a) clinical assessment suggests possibility of severe withdrawal symptoms, which warrant at least an inspection (e.g., tremor for alcohol withdrawal), (b) for prescribing new medications or continuation of previous medications, (c) for suicide or overdose risk-assessment, (d) for possible dual diagnosis, and (e) a mismatch between the identity of the registered person and the individual contacted on phone. However, this step (VC) may be skipped and patients can be advised for in-person consultation directly following telephonic consultation in case the SR is reasonably certain that the patient would require medication which cannot be prescribed even after a VC (e.g., benzodiazepines other than clonazepam and clobazam are currently not permitted under TPG).
2.3. STEP 3: in-person care
In-person consultation is required in the following cases: (a) need for detailed physical examination due to suspected medical comorbidities, (b) presence of severe and complicated withdrawal syndrome, (c) potential risk of suicide and drug overdose, and (d) need for medication which cannot be prescribed through teleconsultation. Examples of such treatment include opioid agonist treatment and treatment of alcohol withdrawal with benzodiazepines (except clonazepam). Although the prescription of maintenance treatment with naltrexone and disulfiram not particularly prohibited by the TPG, online prescription of these medications are fraught with the possible risk of precipitated withdrawal (in opioid use disorders) and disulfiram-ethanol reaction, respectively.
In all three steps, consultant psychiatrists inputs were sought for patients with: (a) multiple and complex comorbidities, (b) medico-legal concerns, and (c) clinical discretion of the senior residents based on diagnostic and treatment aspects.
3. Sharing our initial experience
We performed a retrospective chart review for this study. The ethical clearance was obtained from institutional ethical committee (reference no: INT/IEC/2020 SPL 1391).
3.1. Preliminary data of service utilization
Although initial exploratory experience was gained using telemedicine since April 2020, the formal telemedicine-assisted stepped-care outpatient service for SUD started on 18th of May 2020. Till 31 st August 2020, 160 new and 219 follow-up patients (who were already on treatment prior to 24th March 2020) were registered in the tele-addiction service.
Among the newly registered, we provided telephonic consultation to 128 (80 %) patients. Consultation could not be done for 32 patients because of wrong contact information and consultation initiated by family members without patient’s consent. The clinical and demographic details of the service users are provided in Table 1 . All audio-consultations were delivered within 24 h (largely within 12 h) of registration. Out of the 128 patients, VC had to be done in 115 (89 %) patients. VC was done on the same day. Therefore, telephonic consultation as the sole modality was used only for 13 (11 %) patients. Finally, forty (31.3 %) patients were called for physical consultation, and 28 (70 %) of them actually turned up for the same. Among the 88 patients consulted either through phone or video, 48 (54.5 %) followed-up at least once through the telemedicine services.
Table 1.
Socio-demographic and clinical data of the patients.
| Parameter | Follow-up patients; Number (%) | Newly-registered patients; Number (%) | |
|---|---|---|---|
| Mean age ± SD (range) | 37.1 ± 12.1 (16−78) | 33.4 ± 9.8 (18−70) | |
| Sex | Male | 193 (97.6) | 124 (96.8) |
| Female | 5 (2.4) | 4 (3.2) | |
| Residence | Urban | 119 (59.9) | 78 (60.9) |
| Rural | 79 (40.1) | 50 (39.1) | |
| Substance use disorder | Alcohol | 103 (52.5) | 51 (40) |
| Opioid | 97 (48.9) | 80 (62.4) | |
| Cannabis | 43 (21.8) | 17 (13.6) | |
| Sedative | 13 (6.6) | 4 (3.2) | |
| Tobacco | 101 (50.8) | 55 (42.8) | |
| Physical illness | Present | 13 (6.6) | 4 (3.2) |
| Absent | 185 (93.4) | 124 (96.8) | |
| Psychiatric illness | Absent | 172 (87.1) | 112 (87.8) |
| Present | 26 (12.9) | 16 (12.2) | |
| Psychiatric diagnosis | Depressive disordera | 9 (34.6) | 6 (37.5) |
| Bipolar affective disorderb | 7 (26.9) | 2 (12.5) | |
| Psychotic disordersc | 6 (23.1) | 3 (18.8) | |
| Anxiety disorderd | 3 (11.5) | 5 (31.3) | |
| Conduct disorder | 1 (3.8) | 0 (0) | |
Note: Total number of follow up patients were 198, and total number of newly registered patients were 128. SD- Standard Deviation.
Depressive disorders include unipolar depression, dysthymia and recurrent depressive disorders.
Bipolar affective disorders include manic, hypomanic and depressive episodes (with past history of mania or hypomania).
Psychotic disorders include schizophrenia, schizoaffective disorder, substance induced psychotic disorders.
Anxiety disorders include generalised anxiety disorder, panic disorder with and without agoraphobia and social anxiety disorder.
Among the 219 follow-up patients, we could provide teleconsultation to 198 (90.4 %). Consultation could not be provided to 21 patients because of wrong contact information and unavailability of patients’ explicit consent. The demographic and clinical details of service users who sought follow up care are provided in Table 1. Out of the 198 patients, majority 134 (67.7 %) received only audio-consultations. VC done in 12 cases (5.5 %) following the audio-consultations. Fifty two (23.7 %) patients were called for physical consultation, and 32 (14.6 %) of them actually followed up. Fifty six patients (25.6 %) followed up telephonically at least once after the initial consultation.
In comparison to last year, the number of new OPD registrations dropped drastically. From 18th till 31 st May 2019, the number of new OPD registration was 170, which dropped to 22 during this year’s tele-consultation during the same period. In the same manner, the new registration in the months of June, July and August in 2019 were 351, 467 and 436 respectively in 2019, which dropped to 43, 44 and 51 for the respective months in 2020. The smaller numbers suggested limited awareness, acceptability, availability, and affordability of telemedicine based service. On a positive note, a slight increasing trend was visible in the tele-registration.
Telemedicine based treatment delivery for SUD is feasible and apparently acceptable to patients. It has assumed greater importance and relevance during the time of the pandemic. To say the least, with a severe restriction of the availability and access to routine care, telemedicine has created a new window of opportunity. However, we would like to share some concerns and lessons from the perspectives of both the service users and service providers.
3.2. Perspectives from service users
Firstly, a large majority (nearly 90 %) of patients needed VC, which required availability of android or i-os devices like smartphones or computers, good internet connectivity, and a minimum technical expertise. We found that many patients struggling with one or all of these. Secondly, sometimes patients used devices of family and friends, which could threaten the privacy and confidentiality of information. Besides, family members were seen to be mostly around during the VC, even when it was done from patients’ personal devices. This feature is unique to India, where the concept of personal space and privacy is blurred in the family context. Thirdly, one-third of the patients had to be called for in-person consultation. The main reason was the restriction of prescribing buprenorphine and benzodiazepines other than clonazepam through online consultation. Although in usual times the need for an in-person consultation before starting these medications could not be contested, insistence of physical consultation during the pandemic appears to be restrictive. Several countries including the US and UK have lifted the limitations of online prescriptions of opioid agonists and benzodiazepines (SAMHSA, 2020; ACMD, 2020). However, a continued restriction in India could increase (a) the risk of infection both in patients and doctors, (b) chances of drop-out from treatment (as evidenced by one-third not taking the in-person consultation), and (c) the burden on the limited human resources available for treatment. Finally, the follow-up care was easier to deliver through telemedicine as a majority required only telephonic consultation.
3.3. Perspectives from service providers
From the service providers’ view-point, we experienced the following difficulties: (a) in more than 16 percent cases patients could not be contacted due to technical difficulties such as wrong numbers, line-busy, and non-response; VCs were often interrupted by the difference of bandwidths between the service users and providers, poor network connection, patients non-familiarity with the technology; in sum, the quality of interaction through VC was only modestly satisfactory. (b) The restrictions imposed on telemedicine-based prescription of benzodiazepines had posed a conflict between the legal responsibility and ethical obligation of beneficence, especially for patients who had to travel long distance to seek in-person consultation. (c) Inability to perform a thorough physical examination in the presence of medical comorbidities with a need for immediate treatment presented the dilemma of non-maleficence and beneficence. Currently virtual physical examination ‘on rest’ and ‘on instruction’ is proposed to avoid this shortcoming (Thirthalli et al., 2020). It is an inspection-based procedure, and cannot possibly replace the need for a proper physical examination especially in patients with systemic complications due to substance use.
Finally from the aspects of service delivery, we encountered the following limitations: (a) the multidisciplinary team engaged in routine in-person care was difficult to be integrated in the existing telemedicine based care model, (b) conducting group psychotherapy, an integral component of in-person care, too, was difficult through telemedicine.
The future will tell us whether the interest in the telemedicine would persist even after the availability of unrestricted in-person care.
4. Comparing the PGI’s and the NIMHANS telemedicine model for substance use disorder
NIMHANS, Bengaluru has a tele-psychiatry aftercare (TAC) model for follow up care delivery to the patients including those with substance use disorder (Das et al., 2020). During lockdown another smartphone-based e-consultation portal was initiated by the Centre for Addiction Medicine to aid the treatment of patients with substance use disorder, delivered by trained healthcare workers (Ganesh et al., 2020). Here, we would like to compare this model (Ganesh et al., 2020) with the PGI model because both these models have been specifically designed for SUDs. The NIMHANS’s “consultation” model was possible because of the continuous capacity building exercise for the treatment of SUD since 2014, and, consequent presence of trained human resources at the primary care. Therefore, this model is difficult to replicate. On the contrary, the PGI model can be adopted under most of the circumstances. However, the PGI model would require continuous presence of a specialist and contingent upon the availability of technology among service users. Therefore, it is more resource intensive. We believe an ideal telemedicine-based care for substance use disorder should combine both the models for their complementarity. It would be worthwhile to compare the two models to further enhance the utility of both.
5. Limitations
Some of the limitations of this study are (a) retrospective study design and post hoc analysis of the data, (b) lack of qualitative analysis of the experience of the service users and providers.
6. Conclusion and future directions
The pandemic has brought about a welcome and unprecedented growth of telemedicine globally, across medical disciplines (Song et al., 2020; Hollander and Carr, 2020). Telemedicine might prove to be a boon to address the unmet treatment need for substance use disorders, and it is likely to continue even after the pandemic, to complement the existing healthcare delivery. At the same time, telemedicine must acknowledge and try to minimize the drawbacks related to logistic obstacles (like poor connectivity, audio and video quality) and legal restrictions (like restriction to prescribe benzodiazepines) for a seamless integration to the current system. The two different models of telehealth care for SUD, practiced in two different institutes of India, could encourage others to adopt, adapt, and share their experience. We need studies comparing feasibility, acceptability, efficacy, and cost-effectiveness of these models and comparison of telemedicine-based and in-person care. There should also be efforts to deliver psychosocial interventions with patient or family members and clinical psychology assessments utilizing tele-platform for patients with SUD. Till that time the service providers, based on their resources and context, should continue to explore and experiment with various models, within the framework of the telemedicine guideline, to minimize the impact of the service disruption.
Financial disclosure
None to disclose.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
We want to acknowledge the contribution of Mr Geetesh Kumar Singh, Junior Research Fellow in data collation and analysis.
References
- ACMD . 2020. COVID-19: ACMD Advice on Proposed Legislative Changes to Enable Supply of Controlled Drugs during a Pandemic.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/878524/COVID19_ACMD_advice_on_proposed_legislative_changes_to_enable_supply_of_controlled_drugs_during_a_pandemic1.pdf [Google Scholar]
- Ambekar A., Agrawal A., Rao R., Mishra A., Khandelwal S., Chadda R., on behalf of the group of investigators, editors. Ministry of Social Justice and Empowerment, Government of India and NDDTC, AIIMS, New Delhi. National Survey on Extent and Pattern of Substance Use in India; New Delhi: 2019. [Google Scholar]
- Arya S., Gupta R. COVID-19 outbreak: challenges for addiction services in India. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bada Math S., Manjunatha N., Naveen Kumar C., Basavarajappa C., Gangadhar B.N. NIMHANS; Bengaluru, India: 2020. Telepsychiatry Operational Guidelines-2020. [Google Scholar]
- Balasinorwala V.P., Shah N.B., Chatterjee S.D., Kale V.P., Matcheswalla Y.A. Asynchronous telepsychiatry in Maharashtra, India: study of feasibility and referral pattern. Indian J. Psychol. Med. 2014;36(3):299–301. doi: 10.4103/0253-7176.135384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu D., Ghosh A., Subodh B.N., Mattoo S.K. Opioid substitution therapy with buprenorphine-naloxone during COVID-19 outbreak in India: sharing our experience and interim standard operating procedure. Indian J. Psychiatry. 2020;62(3):322–326. doi: 10.4103/psychiatry.IndianJPsychiatry_295_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S., Manjunatha N., Kumar C.N., Math S.B., Thirthalli J. Tele-psychiatric after care clinic for the continuity of care: a pilot study from an academic hospital. Asian J. Psychiatr. 2020;48 doi: 10.1016/j.ajp.2019.101886. [DOI] [PubMed] [Google Scholar]
- Dubey M.J., Ghosh R., Chatterjee S., Biswas P., Chatterjee S., Dubey S. COVID-19 and addiction. Diabetes Metab. Syndr. 2020;14:817–823. doi: 10.1016/j.dsx.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesh A., Sahu P., Nair S., Chand P. A smartphone based e-Consult in addiction medicine: an initiative in COVID lockdown. Asian J. Psychiatr. 2020;51:102120. doi: 10.1016/j.ajp.2020.102120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Kar S.K., Arafat S.Y., Sharma P., Dixit A., Marthoenis M., Kabir R. COVID-19 pandemic and addiction: current problems and future concerns. Asian J. Psychiatr. 2020;51:102064. doi: 10.1016/j.ajp.2020.102064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni K.R., Shyam R., Bagewadi V.I., Gowda G.S., Manjunatha B.R., Shashidhara H.N., et al. A study of collaborative telepsychiatric consultations for a rehabilitation centre managed by a primary healthcare centre. Indian J. Med. Res. 2020;152(4):417–422. doi: 10.4103/ijmr.IJMR_676_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N., Carr B.G. The role of telehealth in the medical response to disasters. JAMA Intern. Med. 2018;178:745–746. doi: 10.1001/jamainternmed.2018.1314. [DOI] [PubMed] [Google Scholar]
- Malhotra S., Chakrabarti S., Shah R., Sharma M., Sharma K.P., Malhotra A., et al. Telepsychiatry clinical decision support system used by non-psychiatrists in remote areas: validity & reliability of diagnostic module. Indian J. Med. Res. 2017;146(2):196–204. doi: 10.4103/ijmr.IJMR_757_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manjunatha N., Kumar C.N., Math S.B. Coronavirus disease 2019 pandemic: time to optimize the potential of telepsychiatric aftercare clinic to ensure the continuity of care. Indian J. Psychiatry. 2020;62(3):320–321. doi: 10.4103/psychiatry.IndianJPsychiatry_236_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangaswamy T. Using mobile telepsychiatry to close the mental health gap. Curr. Psychiatry Rep. 2012;14(3):167–168. doi: 10.1007/s11920-012-0267-x. [DOI] [PubMed] [Google Scholar]
- SAMHSA . Substance Abuse and Mental Health Administrations (SAMHSA); 2020. COVID-19 and Opioid Treatment Programs.https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf (Last Accessed on 10 September 2020) [Google Scholar]
- Song X., Liu X., Wang C. The role of telemedicine during the COVID-19 epidemic in China-experience from Shandong province. Crit. Care. 2020;24:178. doi: 10.1186/s13054-020-02884-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telemedicine Practice Guidelines, Ministry of Health & Family Welfare; New Delhi . 2020. Telemedicine Practice Guidelines.https://www.mohfw.gov.in/pdf/Telemedicine.pdf (Last Accessed on 10 September 2020) [Google Scholar]
- Thirthalli J., Manjunatha N., Math S.B. Unmask the mind! Importance of video consultations in psychiatry during COVID-19 pandemic. Schizophr. Res. 2020;222:482–483. doi: 10.1016/j.schres.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J., Fudim M., Cameron B., Gellad Z.F., Cho A., Phinney D., et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020;27:957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]