Abstract
Background:
The SARS-CoV-2 (COVID-19) pandemic brought the public overwhelming and conflicting information. Rates of trust in healthcare professionals have been declining among laypersons over the past five decades. In this setting, we sought to evaluate the use of medications, both with or without a prescription, to prevent and treat SARS-CoV-2 as well as trust in healthcare among patients in a primary care clinic.
Design:
We surveyed 150 veterans in primary care clinic waiting rooms at a large southwestern tertiary care Veterans Affairs hospital. This survey was performed in March–November 2021.
Methods:
The survey asked about respondents’ demographics, use of medications, nutritional supplements, and other remedies for the prevention and treatment of COVID-19, perceived access to care using Agency for Healthcare Research and Quality (AHRQ) Consumer Assessment of Healthcare Providers and System (CAHPS), overall health status, and barriers to medical appointments in the last 12 months. Distrust was measured using the Revised Health Care Distrust scale. We used univariate and multivariate linear regression analyses to study predictors of distrust to healthcare.
Results:
Forty-two (28%) of 150 respondents reported taking an agent for the prevention of COVID-19, while 4% reported storing antibiotics for the treatment of COVID-19, if diagnosed. Medications were obtained from medical providers, US stores or markets, the Internet, home stockpiles, and other countries. Medications with potentially harmful effects taken for the prevention and treatment of COVID-19 included hydroxychloroquine, pseudoephedrine, and antibiotics. Among those surveyed, the mean (SD) on the health system distrust score was 2.2 (0.6) on a scale of 1–5, with 5 indicating higher distrust. Younger age, self-reported poor health, lack of a regular physician, and self-reported poor access to care were independently associated with distrust in healthcare.
Conclusion:
Self-medication to prevent COVID-19 infection with unproven therapies was common among respondents, as was some level of distrust in the healthcare system. Access to care was one of the modifiable factors associated with distrust. Future studies may explore whether improving trust may moderate self-treatment behavior and storage of potentially harmful medications.
Plain Language Summary
Self-Medication Habits and Trust in Healthcare Among Patients in a Primary Care Setting in the United States
The public has received information from many different sources on COVID-19. Trust in healthcare leadership has also been impacted. We studied self-medication habits to prevent or treat COVID-19 among a group of primary care patients in a large hospital system in the Southwest United States. We also explored these patients’ trust in their healthcare system.
We asked people waiting in primary care clinic waiting rooms whether they had taken any medications, nutritional supplements, or other remedies to prevent or treat COVID-19. We also asked people whether they stored medications in the event that they were diagnosed with COVID. The survey explored patients’ trust in the healthcare system through a validated trust survey tool. The survey also assessed basic demographic information, health literacy, access to care, and self-reported health status. These survey answers were analyzed to see whether there was an association between trust in healthcare and other factors including self-medication habits, access to care, demographics, or perceived health.
This study found that over 25% of the 150 people surveyed had taken a medication, nutritional supplement, or remedy in an attempt to prevent COVID. We found that some people were taking potentially harmful medications, including hydroxychloroquine, pseudoephedrine, and antibiotics. We found that patients’ distrust score was 2.2 on a scale of 1–5 (5 is associated with higher distrust). Self-medication for the prevention or treatment of COVID was not associated with distrust; however, younger age, self-perceived lack of access to healthcare, self-perceived poor overall health, and not having a regular doctor were predictors for lower trust. This information provides a basis to further study self-medication habits as well as ways to improve trust in the healthcare system.
Keywords: COVID-19, self-medication, distrust, ambulatory care, Veterans Health Services
Introduction
Since March 2020, the US public has been confronted with dual outbreaks, one from SARS-CoV-2 (COVID-19), the other from the overwhelming and often conflicting information about COVID-19. The World Health Organization (WHO) has defined this latter phenomenon as an infodemic.1 Infodemic, or the spread of both accurate and inaccurate information about a world event, was first coined in 2003 by David Rothkopf2 of the Washington Post to describe the SARS outbreak in China. Misinformation or conflicting information may lead to anxiety and mistrust and may also cause people to feel a need to take charge of their own health, leading to self-medication and vaccine hesitancy.3–5
Self-medication is well documented among individuals with limited access to healthcare and has been studied among lower, middle-income countries.3,6,7 Poor access to care and distrust may be associated with use of medications without medical guidance.6,8 A systematic review by Ayosanmi et al. on self-medication practices for prevention and treatment of COVID-19 found that prevalence of self-medication ranged widely (from 3% to 96% in various countries and different study populations), but this review did not include any studies from the United States.
Trust has proven to be an essential component of effective healthcare delivery.9,10 Even prior to the pandemic, a decline in trust occurred, with rates of trust among individuals in healthcare professionals and leaders in the United States decreasing from 73% in 1966 to 34% in 2013.11 Distrust in the healthcare system has been associated with lower utilization of recommended screening tests as well as preventive health services.12,13
As misinformation surrounding the COVID-19 pandemic and distrust in healthcare are both associated with harmful clinical outcomes, including vaccine hesitancy and refusal,14–17 we examined pandemic perspectives and experiences among patients in a primary care clinic on two related topics: self-medication and trust in healthcare. For self-medication, we surveyed individuals’ use of medications, nutritional supplements, or remedies both with or without a prescription, to self-prevent and self-treat COVID-19. In the same survey, we measured individuals’ level of trust in the healthcare system and what factors were associated with distrust in healthcare. At the time of this survey, no oral medication had been approved for the prevention or treatment of COVID-19.
Methods
Participants
Participants were recruited from the Michael E. DeBakey Veterans Affairs Medical Center primary care clinic waiting rooms. The Veterans Health Administration is the largest integrated health system in the United States that cares for 9 million Veterans yearly. US adults who had served in active military duty for 24 months are eligible for care at the Veterans Affairs (VA). Between March–November 2021, members of the research team approached patients in the primary care waiting rooms and provided information about the present study. Interested individuals were then given the opportunity to perform the survey in person with a member of the research team or undergo the survey via telephone at a later date. The survey was read aloud to participants, and responses were logged by the research coordinator. All individuals were offered $25 for their participation. The Baylor College of Medicine Institutional Review Board approved this study, and patients provided informed consent to participate in the study.
Measures
Participants completed a 33-question survey including basic sociodemographic information, including age, race and ethnicity, education level, number of children (under the age of 18) in the household, income, and self-reported mental health disorders.
COVID-19 survey questions
Three sections consisted of questions pertaining to the use, storage of medications for the prevention and treatment of COVID-19 (see supplemental materials for the complete survey instrument). The three key survey questions were (1) Have you used a medication, nutritional supplement, or other remedy to prevent COVID-19? (2) Have you used a medication, nutritional supplement, or other remedy to treat COVID-19? (3) Do you store medicines at home right now because of COVID-19, excluding medicines you are currently using? If the answer was yes to any of the above questions, they were asked for the reason for medication use as well as where they obtained the medication (Supplemental Table 1). Any medication, nutritional supplement, or remedy that was reported as used for the prevention of COVID was coded as inappropriate. For the treatment of COVID-19, medications prescribed by a doctor, nurse, dentist, or hospital and over-the-counter medications for symptom relief were coded as appropriate, and other nutritional supplement, remedy, or prescription medications not prescribed by a licensed provider were coded as inappropriate. Over-the-counter medications for symptoms of COVID-19 stored were coded as appropriate, and any prescription medication, nutritional supplement, or remedy stored for the treatment of COVID-19 was coded as inappropriate.
Distrust, access to care survey questions
To study distrust, the Revised Health Care Distrust scale was employed. It is a nine-question survey that asks participants to rate on 5-point Likert-type scale different aspects of trust in the healthcare system with a total maximum score of 45 (higher distrust) and minimum score of 9 (Supplemental Table 2). The survey, developed and validated for the general public in the United States, consists of two subscales of distrust with five questions associated with competence distrust and four questions associated with value distrust with maximum scores of 25 and 20, respectively.18 To assess health literacy, we used Chew’s three health literacy screening questions that are scored on a 5-point Likert-type scale and have a maximum score of 15 and a minimum score of 3 with high scores correlating to poor health literacy and low scores to high health literacy19 (Supplemental Table 3). This scale has been validated for the veteran population.20 Access to care and self-perceived overall health was measured using the validated Agency for Healthcare Research and Quality (AHRQ) Consumer Assessment of Healthcare Providers and System (CAHPS), four questions rated on a 4-point Likert-type scale (1–4) with higher scores associated with more favorable outcomes21 (Supplemental Table 4). Additional barrier to care questions were formulated to help identify any additional factors that may be contributing to access to care and were measured using the following question: ‘In the past 12 months, how much of a problem is each of the following for you: transportation, long wait times in clinic, high costs of doctor’s visits, and/or lack of a regular doctor’. The scale to answer each question about access to care was: Not a Problem, Minor Problem, Major Problem, or Not Applicable (Supplemental Table 5).
Statistical analysis
We performed descriptive statistics on all study variables. Data were checked for normality. The effect of sociodemographic factors [age, race and ethnicity, education level, number of children (under the age of 18) in the household, income, and self-reported mental health disorders], CAHPS overall health status and access to care, health literacy on distrust of healthcare system was studied using a simple linear regression analysis. Candidate independent variables for multiple linear regression were those that exhibited simple bivariate relationship with the outcome at p < 0.10. For multiple linear regression analysis, the alpha level was set to 0.05.
Data analysis was performed using SPSS version 28 (SPSS Inc., Chicago, IL) software.
Results
Demographics
A total of 292 individuals were approached to participate in the survey, with 150 (51%) agreeing to participate. A total of 134 (89%) of surveys were performed in person, with the remainder occurring over the phone. The majority of the 150 respondents were male (86%) with a mean age of 57.8 ± 14.6 years. Those surveyed self-reported their race with 56% identifying as Black or African American, 13.3% identifying as Hispanic or Latina/Latino, and 29.3% identifying as White. Our survey participants reported high levels of advanced education with 71.3% reporting some college or above. Health literacy was high among surveyed individuals with 83.3% meeting adequate health literacy on the Chew’s three health literacy screening questions. Of surveyed veterans, 60% self-reported some type of a mental health disorder including depression, general anxiety disorder, and post-traumatic stress disorder (PTSD). The mean overall health status reported was 2.1 (standard deviation of 0.9), with lower scores being more favorable and a possible range of 0–4 (Table 1).
Table 1.
Characteristics of respondents (n = 150).
| Characteristic | Value |
|---|---|
| Mean age (years) (standard deviation) | 57.8 (14.6) |
| No. (%) of male respondents | 129 (86.0) |
| No. (%) of respondents of race and ethnicity | |
| African American or Black | 84 (56.0) |
| Hispanic or Latina/Latino | 20 (13.3) |
| Othera | 2 (1.3) |
| White | 44 (29.3) |
| No. (%) of respondents with education level | |
| Less than high school | 2 (1.3) |
| High school or GED | 41 (27.3) |
| Some college and above | 107 (71.3) |
| Median number of children under 18 years in the household (range) | 0 (0–4) |
| No. of respondents with income/total no. of respondents (%) | |
| <$20,000 | 31 (20.7) |
| ⩾$20,000 but <$40,000 | 29 (19.3) |
| ⩾$40,000 but <$60,000 | 35 (23.3) |
| ⩾$60,000 but <$100,000 | 14 (9.3) |
| ⩾$100,000 | 20 (13.3) |
| Don’t know/prefer not to say | 21 (14.0) |
| No. (%) of respondents with self-reported mental health disordersb | 90 (60.0) |
| Overall health status,c mean (standard deviation) | 2.1 (0.9) |
Includes 1 Asian, and 1 multiracial.
Includes 63 depression, 50 generalized anxiety disorder, 8 mania or bipolar disorder, 2 dysthymic disorder, 6 obsessive compulsive disorder, 26 panic attack, 9 phobia, 53 post-traumatic stress disorder, 1 gender dysphoria, 1 insomnia 1 mood swings, 1 MST, and 1 schizophrenia.
Score ranges from 0 to 4 (excellent = 0; poor = 4), with lower scores being more favorable.
Use of medications for the prevention and treatment of COVID
Of the 150 respondents, 41 (27%) reported use of medications, nutritional supplements, or other remedies to prevent COVID. At the time of this survey, no oral medication had been approved for the prevention or treatment of COVID-19, and none of these agents that patients reported taking had been prescribed by a doctor, nurse, dentist, or hospital. Of the 41 reporting self-dosing for COVID prevention, 40 (95%) took vitamins and/or herbal supplements, 1 took pseudoephedrine, and 1 took hydroxychloroquine (a 30-day course, obtained from the Internet). Forty-one Veterans took a total of 90 medication, nutritional supplement, or other remedies with some respondents taking up to five medications. Supplements taken included vitamin C, zinc, elderberry, garlic oil, and ginger. Reasons cited for taking these agents to prevent COVID included 52% to support the immune system (47 of 90), 19% as a health supplement (17 of 90), 12% to ensure getting enough Vitamin C (11 of 90), 9% to prevent COVID (8 of 90), 4% for digestive health (4 of 90), 2% as anti-inflammatory (2 of 90), and 1% for circulation support (1 of 90). The sources of obtaining these agents included 5% from the Internet (5 of 90) and 94% directly from a market or store in the United States (86 of 90).
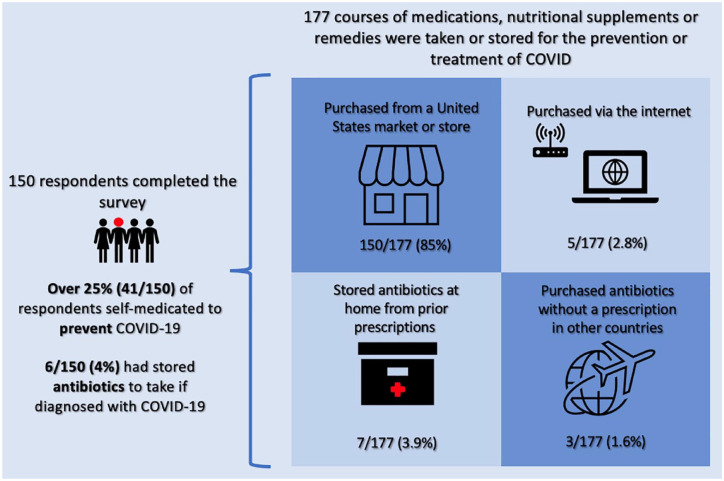
Among the 150 respondents, 22 (15%) reported that they had been diagnosed with COVID by a medical professional. Seventeen of 22 (77% of those with COVID, 11% of total respondents) had taken a medication, nutritional supplement, or other remedy to treat COVID. Of these 17 patients with COVID who took some remedy to treat it, 5 had taken antibiotics (4 took a prescribed course of antibiotics, and 1 took leftovers from prior course of antibiotics). Six of 22 (27%) patients took vitamins and supplements including zinc, Vitamin C, multivitamin, and elderberry to treat COVID. Eighteen respondents (12%) reported storing medications because of COVID. Six of 150 (4%) had stored antibiotics (4 stored leftovers from prior prescriptions, while 2 stored antibiotics that had been purchased from another country without a prescription) and 1 respondent had stored previously prescribed prednisone. The other stored agents were vitamins, herbal supplements, and over-the-counter cold medications (Figure 1).
Figure 1.
A selection of survey results on the self-medication habits to prevent or treat COVID-19 among veterans in a large tertiary care Veterans Affairs hospital.
Distrust in the healthcare system and access to care
For the distrust scale, the question categories are divided into subscales of competence and value (Table 2). The mean (SD) health system distrust score was 2.2 (0.6), or a composite score of 19.9 (15.9). Ranges for these domains are 1–5 and 9–45, respectively, with higher scores indicating higher levels of distrust. The total mean competence domain was 2.1 (0.7) and value domain was 2.3 (0.7). Distrust scores were not different between those who used self-medication [median = 2.2 (IQR = 1.9–2.7)] and those who did not [median = 2.2 (IQR = 1.7–2.6)].
Table 2.
Healthcare system distrust scale questions (n = 150).
| Domain | Mean (SD) | |
|---|---|---|
| Veterans Health Administration (VHA) does its best to make patients health bettera | Competence | 1.8 (0.7) |
| Veterans Health Administration covers up its mistakesb | Value | 2.9 (1.0) |
| Patients receive high quality medical care from Veterans Health Administrationa | Competence | 2.0 (0.9) |
| VHA makes too many mistakesc | Competence | 2.4 (0.8) |
| VHA puts making money above patients’ needs | Value | 2.2 (0.9) |
| VHA gives excellent medical carea | Competence | 2.2 (1.0) |
| Patients get the same medical treatment from VHA, no matter what the patient’s race or ethnicitya,d | Value | 2.1 (1.0) |
| VHA lies to make moneye | Value | 2.2 (0.8) |
| VHA experiments on patients without them knowing | Value | 2.4 (1.0) |
Items are answered on a scale where 1 = strongly disagree and 5 = strongly agree. Higher scores indicate greater distrust.
Item is reverse scored, meaning that strongly disagree = 5 and strongly agree = 1.
Five patients responded ‘N/A’ and were excluded from the analysis.
Four patients responded ‘N/A’ and were excluded from the analysis.
One patient responded ‘N/A’ and was excluded from the analysis.
Three patients responded ‘N/A’ and were excluded from the analysis.
Respondents reported their experience with access to care in the past 12 months through the CAHPS access to care survey and the additional barriers to healthcare access questions that was created for this survey. For both surveys, higher scores are more favorable, with a range of 0–3. The mean (SD) of ease in making doctor’s appointments was 2.06 (0.98), obtaining needed tests and treatment was 2.07 (0.86), accessing emergency care was 1.8 (1.14), and timely routine care was 1.6 (1.1). For barriers to access to care in the past 12 months, 87.3% reported that transportation was either not a problem or a minor problem. Likewise, 89.3% of participants reported that long wait times were either not problem or a minor problem. High cost of medical visit was reported as a major problem by 6%; however, 77.3% reported cost was not applicable as their healthcare costs are covered by the VA. About 12% of those surveyed reported that not having a regular doctor was a major problem, and 32% reported this was not applicable.
Univariate analysis of distrust
In a univariate analysis using simple linear regression (Table 3), younger age was associated with greater distrust [β (95% CI) = −0.010 (−0.017; −0.003), p = 0.03]. The presence of a mental health disorder was found to be associated with higher distrust [β = −0.261 (−0.466; −0.56), p = 0.013]. Likewise, lower self-reported overall health status was associated with higher levels of distrust [β = 0.206 (0.098; 0.315), p < 0.001]. Each individual question on the CAHPS Access to Care Questions showed a significant negative correlation between decreased access to care and increased distrust [β = −0.239 (−0.337; −0.141), −0.366 (−0.465; –.266), −0.187 (−0.259; −0.116), −0.258 (−0.342; −0.174), respectively, p < 0.001 for all]. Not having a regular doctor was correlated to higher levels of distrust. We did not observe a statistically significant association between race, education level, health literacy, or income and distrust [β = −0.643 (–1.019; −0.267), p < 0.001].
Table 3.
Univariate analysis of healthcare system distrust (n = 150).
| Simple linear regression analysis | ||
|---|---|---|
| Predictor | β (95% CI) | P valuea |
| Age (years) | −0.010 (−0.017; −0.003) | 0.03 |
| Sex | ||
| Female | 1 (reference)b | |
| Male | −0.171 (–4.465; 0.124) | 0.254 |
| Race and ethnicityc | ||
| Hispanic or Latino | 1 (reference) | |
| African American or Black | 0.029 (−0.278; 0.336) | 0.852 |
| White | −0.266 (−0.598; 0.067) | 0.117 |
| Educationd | ||
| College and more | 1 (reference) | |
| High school or GED | −0.135(−0.413; 0.142) | 0.337 |
| Some college (1–3 years) | 0.015 (−0.235; 0.266) | 0.903 |
| Incomee | ||
| ⩾$100,000 | 1 (reference) | |
| <$20,000 | −0.010 (−0.374; 0.354) | 0.956 |
| ⩾$20,000 but <$40,000 | 0.100 (−0.269; 0.469) | 0.593 |
| ⩾$40,000 but <$60,000 | 0.074 (−0.281; 0.430) | 0.680 |
| ⩾$60,000 but <$100,000 | −0.172 (−0.614; 0.270) | 0.442 |
| Presence of mental health disorderf | ||
| Yes | 1 (reference) | |
| No | −0.261 (−0.466; −0.56) | 0.013 |
| Overall health status | 0.206 (0.098; 0.315) | <0.001 |
| Health literacy | ||
| Inadequate | 1 (reference) | |
| Adequate | −0.029 (−0.304; 0.246) | 0.834 |
| CAHPS Access to Care Questions | ||
| How often was it easy to get an appointment with a doctor? | −0.239 (−0.337; −0.141) | <0.001 |
| How often was it easy to get the care, tests, or treatment you thought you needed through your health plan? | −0.366 (−0.465; –.266) | <0.001 |
| When you needed care right away, how often did you get care as soon as you thought you needed? | −0.187 (−0.259; −0.116) | <0.001 |
| Not counting the times you needed care right away, how often did you get an appointment for your healthcare at a doctor’s office or clinic as soon as you thought you needed? | −0.258 (−0.342; −0.174) | <0.001 |
| Not having a regular doctorb | ||
| Major problem | 1 (reference) | |
| Not a problem or minor problem | −0.643 (–1.019; −0.267) | <0.001 |
CAHPS, Consumer Assessment of Healthcare Providers and System; CI, confidence interval.
Results shown in boldface type have a p value of <0.10 in univariate analyses.
Forty-eight patients responded ‘not applicable’ and were excluded from the analysis.
Two patients with other races were excluded.
One patient with middle class education and 1 patient with some high school were excluded.
Twenty patients who responded ‘don’t know/prefer not say’ were excluded.
Mental health disorders include 63 depression, 50 generalized anxiety disorder, 8 mania or bipolar disorder, 2 dysthymic disorder, 6 obsessive compulsive disorder, 26 panic attack, 9 phobia, 53 post-traumatic stress disorder, 1gender dysphoria, 1 insomnia 1 mood swings, 1 MST, and 1 schizophrenia.
Multivariate analysis of distrust
A multivariate analysis was performed (Table 4) with four factors identified as significantly correlated with distrust in the VA healthcare system: self-reported difficulty in accessing care [β = −0.343 (−0.449;−0.236), p < 0.001], lack of a regular doctor [β = −0.350 (−0.661; −0.039), p = 0.028], self-reported poor overall health status [β = 0.127 (0.034; 0.220), p = 0.008], and younger age [β = −0.006 (−0.023; −0.001), p = 0028]. The model including all four factors explained 36% of variance for distrust in the healthcare system.
Table 4.
Multivariate analysis of mistrust of healthcare system (n = 150).
| Final multivariate model | ||
|---|---|---|
| Predictor | β (95% CI) | P valuea |
| Intercept | 3.322 (2.841; 3.804) | <0.001 |
| CAHPS Access to Care Scalea | −0.343 (−0.449; −0.236) | <0.001 |
| Not having a regular doctorb | ||
| Major problem | 1 (reference) | |
| Not a problem or minor problem or NA | −0.350 (−0.661; −0.039) | 0.028 |
| Overall health status | 0.127 (0.034; 0.220) | 0.008 |
| Age | −0.006 (−0.023; −0.001) | 0.028 |
CAHPS, Consumer Assessment of Healthcare Providers and System; CI, confidence interval.
Presence of mental disorders was not significant in the multivariate analysis.
Mean score was calculated based on four items in the scale.
Adjusted R squared = 0.364, which means that our factors explain 36% of variance for mistrust in healthcare system.
Answers of ‘not applicable’ were combined with ‘not a problem’ and ‘minor problem’ for this variable.
Discussion
We found that survey respondents were taking medications, nutritional supplements, or other remedies to prevent or treat COVID-19, although at the time of the survey, no oral medications had been approved for either prevention or treatment. Some of these agents had been purchased on the Internet. Stockpiled medications at home were another source. Patients reported taking several medications with potentially harmful side effects including hydroxychloroquine, pseudoephedrine, and antibiotics. The reasons for taking these agents were wide ranging and included to support the immune system, to prevent COVID, and as an anti-inflammatory. The use of agents for the prevention of COVID was not correlated with distrust in the healthcare system. Multivariate analysis revealed that self-perceived lack of access to care, younger age, self-perceived poor health, and lack of a regular doctor were independent risk factors for higher levels of distrust in healthcare.
A number of medications or supplements that had been taken for the prevention of COVID-19 have potentially harmful side effects. Taking supplements and prescription medications without medical supervision puts individuals at risk for suffering adverse effects. For example, elderberry may promote hypoglycemia and have an additive effect to medications for diabetes.22 Both ginger and garlic oil may increase bleeding risk in patients taking anti-coagulation.23,24 Storing or obtaining antibiotics without a prescription also confers a risk to the individual and to society of fostering antibiotic-resistant infections.25–27 These findings suggest that larger studies are needed to better assess the use of self-medication for the prevention and treatment of COVID-19 as well as for other conditions and ultimately to better understand the prevalence of these behaviors.
The use of agents for the prevention or treatment of COVID was not correlated with distrust in healthcare, potentially related to the small sample size surveyed. In contrast, a link between self-medication with antibiotics and distrust in healthcare was seen in a cohort of 4243 Swedish survey respondents.8 Other studies have documented an association between trust in the healthcare provider and delay of antibiotics; however, there is limited data on the link between trust in the healthcare system and the use of antibiotics.28,29
The overall distrust score among our survey respondents was a mean (SD) of 2.2 (0.6) or a composite score of 19.9 (15.9), which is moderate and falls between rates reported in studies in the United States.16,17,30,31 In the multivariate analysis, younger age, lower self-reported overall health status, perceived limited access to care, and not having a regular doctor were independently associated with distrust. We did not find a significant correlation between patients’ race, education level, health literacy, and income with distrust.
Access to care was an independent risk factor for healthcare distrust. Access to care also contributes to the practice of self-prescribing antibiotics.6 Taken together, self-perceived lack of access to care may lead to both distrust in the healthcare system and ultimately to the use of self-prescribed agents. COVID may have had both direct and indirect effects on distrust. For example, access to many in-person healthcare activities were limited, which indirectly might lead to higher levels of distrust. Further studies are needed to understand the causes of self-perceived access to care and its effects on practice of self-medication as well as distrust.
Limitations
Limitations of this study include that survey respondents were taken from a single primary care clinic center, although it is the largest VA medical center in the United States and is located in one of the most diverse cities in the United States.32 The sample size was relatively small, and the number of women participating was low, as reflects the veteran patient population. Participants were approached in primary care clinics and thus their response may not reflect the perspectives of people with no access to primary care. Our survey estimates of self-medication for COVID may underestimate the true prevalence rate. Respondents might deny practicing self-medication, especially if they are aware that this is inappropriate behavior and if they are interviewed in a healthcare setting. This survey was performed mostly in person, which may increase the risk of acquiescence bias or the bias to be agreeable when asked questions in person.
Conclusion
Our surveyed primary care population was taking medications, nutritional supplements, or other remedies purchased on the Internet, prescription medications not prescribed by a licensed provider, and in some instances stored prescription medications to prevent or treat COVID-19. These habits may confer risk for adverse events as well as contribute to antibiotic resistance. These self-prescribing habits were not correlated with distrust in healthcare, although our sample size was small. Independent risk factors for distrust included self-perceived lack of access to care, lack of a regular doctor, self-reported poor overall health status, and younger age. These findings are hypothesis generating and encourage us to sample a larger population of primary care patients about their self-medication habits, both during the pandemic and beyond, as a means to inform patient safety interventions.
Supplemental Material
Supplemental material, sj-docx-1-taw-10.1177_20420986221143265 for A survey on self-medication for the prevention or treatment of COVID-19 and distrust in healthcare of veterans in a primary care setting in the United States by Eva Amenta, Larissa Grigoryan, Laura Dillon, Casey Hines-Munson, John Van and Barbara Trautner in Therapeutic Advances in Drug Safety
Supplemental material, sj-png-2-taw-10.1177_20420986221143265 for A survey on self-medication for the prevention or treatment of COVID-19 and distrust in healthcare of veterans in a primary care setting in the United States by Eva Amenta, Larissa Grigoryan, Laura Dillon, Casey Hines-Munson, John Van and Barbara Trautner in Therapeutic Advances in Drug Safety
Acknowledgments
Not applicable.
Footnotes
ORCID iD: Eva Amenta  https://orcid.org/0000-0002-9224-7056
https://orcid.org/0000-0002-9224-7056
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Eva Amenta, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), Houston, TX, USA; Section of Infectious Diseases, Department of Medicine, Baylor College of Medicine, Houston, TX, USA.
Larissa Grigoryan, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), Houston, TX, USA; Department of Family and Community Medicine, Baylor College of Medicine, Houston, TX, USA.
Laura Dillon, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), Houston, TX, USA.
Casey Hines-Munson, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), Houston, TX, USA.
John Van, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), Houston, TX, USA.
Barbara Trautner, Michael E. DeBakey Veteran Affairs Medical Center, Center for Innovations in Quality, Effectiveness, and Safety (IQuESt), 2002 Holcombe Boulevard (152), Houston, TX 77030, USA; Section of Health Services Research, Department of Medicine, Baylor College of Medicine, Houston, TX, USA.
Declarations
Ethics approval and consent to participate: The Baylor College of Medicine Institutional Review Board approved this study (H-48466). The anonymous surveys were performed under waiver of informed consent, as approved by the Baylor College of Medicine IRB, H-48466.
Consent for publication: Not applicable.
Author contributions: Eva Amenta: Investigation; Project administration; Writing – original draft; Writing – review & editing.
Larissa Grigoryan: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Supervision; Writing – review & editing.
Laura Dillon: Project administration.
Casey Hines-Munson: Project administration.
John Van: Project administration.
Barbara Trautner: Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Supervision; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Veteran’s Affairs HSR&D Small Award Initiative for Impact (SWIFT) awards to Centers of Innovation (COINs).
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: The full survey instrument is available as supplemental materials.
References
- 1. Tangcharoensathien V, Calleja N, Nguyen T, et al. Framework for managing the COVID-19 infodemic: methods and results of an online, crowdsourced WHO technical consultation. J Med Internet Res 2020; 22: e19659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rothkopf D. When the buzz bites back. The Washington Post, 2003, https://www.washingtonpost.com/archive/opinions/2003/05/11/when-the-buzz-bites-back/bc8cd84f-cab6-4648-bf58-0277261af6cd/
- 3. Ayosanmi OS, Alli BY, Akingbule OA, et al. Prevalence and correlates of self-medication practices for prevention and treatment of COVID-19: a systematic review. Antibiotics 2022; 11: 808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang A, Hobman EV, De Barro P, et al. Self-medication with antibiotics for protection against COVID-19: the role of psychological distress, knowledge of, and experiences with antibiotics. Antibiotics 2021; 10: 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Larson HJ. The biggest pandemic risk? Viral misinformation. Nature 2018; 562: 309–310. [DOI] [PubMed] [Google Scholar]
- 6. Do NTT, Vu HTL, Nguyen CTK, et al. Community-based antibiotic access and use in six low-income and middle-income countries: a mixed-method approach. Lancet Glob Health 2021; 9: e610–e619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Batista AD, Rodrigues DA, Figueiras A, et al. Antibiotic dispensation without a prescription worldwide: a systematic review. Antibiotics 2020; 9: 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Munthe C, Malmqvist E, Rönnerstrand B. Non-prescription acquisition of antibiotics: prevalence, motives, pathways and explanatory factors in the Swedish population. Plos One 2022; 17: e0273117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall MA, Dugan E, Zheng B, et al. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q 2001; 79: 613–639, v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. Jama 1996; 275: 1693–1697. [PubMed] [Google Scholar]
- 11. Blendon RJ, Benson JM, Hero JO. Public trust in physicians – U.S. medicine in international perspective. New England Journal of Medicine 2014; 371: 1570–1572. [DOI] [PubMed] [Google Scholar]
- 12. Katapodi MC, Pierce PF, Facione NC. Distrust, predisposition to use health services and breast cancer screening: results from a multicultural community-based survey. Int J Nurs Stud 2010; 47: 975–983. [DOI] [PubMed] [Google Scholar]
- 13. Musa D, Schulz R, Harris R, et al. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 2009; 99: 1293–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Turhan Z, Dilcen HY, Dolu İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Current Psychology 2022; 41: 8147–8156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kricorian K, Civen R, Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother 2022; 18: 1950504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schenker Y, White DB, Asch DA, et al. Health-care system distrust in the intensive care unit. J Crit Care 2012; 27: 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vandergrift LA, Christopher PP. Do prisoners trust the healthcare system? Health Justice 2021; 9: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shea JA, Micco E, Dean LT, et al. Development of a revised health care system distrust scale. J Gen Intern Med 2008; 23: 727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004; 36: 588–594. [PubMed] [Google Scholar]
- 20. Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008; 23: 561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Crofton C, Darby C, Farquhar M, et al. The CAHPS® hospital survey: development, testing, and use. Jt Comm J Qual Patient Saf 2005; 31: 655–659. [DOI] [PubMed] [Google Scholar]
- 22. Christensen KB, Petersen RK, Kristiansen K, et al. Identification of bioactive compounds from flowers of black elder (Sambucus nigra L.) that activate the human peroxisome proliferator-activated receptor (PPAR) γ. Phytother Res 2010; 24(Suppl. 2): S129–S132. [DOI] [PubMed] [Google Scholar]
- 23. Ang -Lee MK, Moss J, Yuan C-S. Herbal medicines and perioperative care. Jama 2001; 286: 208–216. [DOI] [PubMed] [Google Scholar]
- 24. Shalansky S, Lynd L, Richardson K, et al. Risk of warfarin-related bleeding events and supratherapeutic international normalized ratios associated with complementary and alternative medicine: a longitudinal analysis. Pharmacotherapy 2007; 27: 1237–1247. [DOI] [PubMed] [Google Scholar]
- 25. Aslam A, Gajdács M, Zin CS, et al. Public awareness and practices towards self-medication with antibiotics among the Malaysian population. A development of questionnaire and pilot-testing. Antibiotics 2020; 9: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bell BG, Schellevis F, Stobberingh E, et al. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infectious Diseases 2014; 14: 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morgan DJ, Okeke IN, Laxminarayan R, et al. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis 2011; 11: 692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carlsson F, Jacobsson G, Jagers SC, et al. Who is willing to stay sick for the collective? – Individual characteristics, experience, and trust. SSM Popul Health 2019; 9: 100499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rönnerstrand B, Andersson Sundell K. Trust, reciprocity and collective action to fight antibiotic resistance. An experimental approach. Soc Sci Med 2015; 142: 249–255. [DOI] [PubMed] [Google Scholar]
- 30. Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between Blacks and Whites. J Gen Intern Med 2008; 23: 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jones AL, Fine MJ, Taber PA, et al. National media coverage of the Veterans Affairs waitlist scandal: effects on veterans’ distrust of the VA Health Care System. Medical Care 2021; 59: S322–S326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McCann A. Most diverse cities in the U.S. https://wallethub.com/edu/most-diverse-cities/12690 (2021, accessed 12/21 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-taw-10.1177_20420986221143265 for A survey on self-medication for the prevention or treatment of COVID-19 and distrust in healthcare of veterans in a primary care setting in the United States by Eva Amenta, Larissa Grigoryan, Laura Dillon, Casey Hines-Munson, John Van and Barbara Trautner in Therapeutic Advances in Drug Safety
Supplemental material, sj-png-2-taw-10.1177_20420986221143265 for A survey on self-medication for the prevention or treatment of COVID-19 and distrust in healthcare of veterans in a primary care setting in the United States by Eva Amenta, Larissa Grigoryan, Laura Dillon, Casey Hines-Munson, John Van and Barbara Trautner in Therapeutic Advances in Drug Safety