Abstract
Purpose
During the COVID-19 pandemic, there is a large unmet need for follow-up services, particularly for chronic diseases such as epilepsy. Alternative methods to reach these people have become necessary. We assessed the feasibility, satisfaction, and effectiveness of video teleconsultation using mobile phones for managing persons with epilepsy (PWEs) on follow-up at a tertiary care center in the southern part of India.
Patients and methods
We included PWEs aged 18 years and over who have been evaluated in person within the past six months, with details available in electronic health records (EHRs), and advised regular follow-up after getting telephonic consent. We excluded those requiring emergency care and those seeking teleconsultation for new symptoms. Participants were sent a message in English and in the local language about the possibility of a video teleconsultation. If willing, they were informed about the date, time, and technical requirements such as smartphones, browsing facilities, etc. Feasibility and effectiveness were assessed. Satisfaction/acceptability was assessed using Telemedicine Satisfaction Questionnaire.
Results
From June 2020 to October 2020, we selected 336 PWEs after screening 1100 records, and we tried video teleconsultation in 141 (41.8%) PWEs. We achieved successful video connections in 95 (28.2%) and audio consultations in 46 (13.6%). The median duration for calling the participants, making successful connections, and consultation was 8 (5–14) min. The majority required two (47.4%) or three (32.6%) attempts. Sixty-five PWEs (68.4%) used caretaker’s mobile phones. We gave prescriptions to all, and 18 received new drugs. Out of 95 PWEs, 90% either ‘agreed’ or ‘strongly agreed’ on 12 out of 14 telemedicine satisfaction questions.
Conclusion
Although we need to make video teleconsultation more feasible, our synchronous mobile video teleconsultation model is an effective and acceptable method to follow up PWEs. This real-time model has the advantage that it does not require any mobile application to be downloaded and installed. Further studies are needed to evaluate methods to improve the reach of these services particularly to vulnerable groups of the population.
Abbreviations: PWEs, Persons with epilepsy; MoHFW, Ministry of health and family welfare
Keywords: Epilepsy, Synchronous methods, Mobile video teleconsultation, Feasibility, Acceptability, Effectiveness
1. Introduction
Telemedicine has been defined as the use of information and communication technologies to provide medical services from a distance [1]. Telemedicine services may use the synchronous method where patients and doctors connect in the real-time or asynchronous mode which is non-real time, “store and forward” communication method such as email [2], [3]. In India, some institutes provide synchronous telemedicine services with real-time video conferencing (RTV) services using a hub-and-spoke model. Here the district and taluk hospitals work as spokes and institutes as the hub, and an electronic health record (EHR)-based synchronous video conference collaborative care model is used [4]. Many countries offer outpatient tele neurology. After the initial detailed evaluation utilizing a person to person meeting, patients are followed up by teleconferencing [5], [6], [7], [8]. Tele-neurology to rural veterans was found to provide quality neurological care, with patient satisfaction, as well as time and cost savings [9], [10]. Epilepsy affecting more than 1% of the world population is a common neurological illness requiring long-term care. For follow-up of persons with epilepsy (PWEs), teleconsultation has been used for focused examination such as nystagmus, gait, speech, tremor, etc. Telemedicine clinics showed similar rates of seizures, hospitalizations, and emergency room (ER) visits as compared to conventional epilepsy clinics, while reducing the costs incurred by the patient [5], [11], [12].
In India, the first case of novel coronavirus (SARS CoV-2) was reported on January 30, 2020. In mid-March 2020, the Government of India announced a complete lockdown followed by stepwise relaxation of restrictions. Hospitals had started to restrict the number of OPD consultations and routine services to reduce the spread of COVID-19, and with the introduction of lockdown, these services came to a near-complete halt. Though some services have resumed with the relaxation of the restrictions, there is still a large unmet need for follow-up services, particularly for those with chronic non-communicable diseases like epilepsy. Thus, alternative methods to reach these patients have become necessary. This is where telemedicine may play a significant role.
Internet and telecommunication services are available in many rural and semi-urban areas in our country. As such, teleconsultation is expanding its role to reach out to patients with limited access to healthcare. Teleconsultation becomes all the more important where there is an imposed limitation for almost all the patients to access regular health care. With the given scenario, it is essential to assess teleconsultation’s overall acceptability for the patients, the barriers to its implementation, maintenance as an alternative health delivery mechanism, and finally, the effectiveness. There are few synchronous teleconsultation models in India that use direct patient specialist video interactions using mobile phones.
If proven feasible, acceptable to the participants and caregivers, and effective, we may utilize this model to manage the PWE during restricted mobility of the population. Besides, we may use this method to manage PWEs who do not require detailed examination during follow-up visits, mainly if they are coming from far-off places. Therefore in this study, we aimed to assess the feasibility, effectiveness, and acceptability/satisfaction of video teleconsultation using mobile phones to manage PWEs on follow-up during COVID-19 pandemic in a public tertiary care hospital.
2. Patients and methods
In this descriptive study, we included PWEs (aged 18 years and above) registered for care with our tertiary care center and had been evaluated in person with details available in EHR within the past six months and advised regular follow-up.
We included PWEs from three districts (Villupuram, Kallakurichi, and Cuddalore) of Tamilnadu, a state situated in southern India. The people from three districts form the catchment population of our hospital. PWEs who primarily contacted the department of neurology for telemedicine services and those PWEs identified from records and approached by the department for providing telemedicine services for follow-up were eligible.
We excluded those PWEs requiring emergency care and those seeking teleconsultation for new symptoms that were not in the spectrum of the same health condition.
We provided teleconsultation services as per the Telemedicine practice guidelines released on 25.03.2020 by the Government of India(MoHFW). We recruited participants after getting the informed telephonic consent (as per the telemedicine guidelines). Eligible participants were sent messages (SMS) in English and Tamil (local language) about the possibility of a video teleconsultation and, if willing, were informed about the date, time, and technical requirements as smartphones, browsing facilities, etc. If they did not carry a smartphone with browsing facility, they were asked whether they would give an alternate number with these facilities. We updated the alternate numbers in our electronic medical records. In addition, we sent a short video to all participants describing the steps to register the request for teleconsultation, achieving the connection, and the method by which they can access the latest prescription. The Institutional ethics committee approved the study (JIP/IEC/2020/144).
2.1. Telemedicine equipment/facility
Our teleconsultation system uses an end-to-end secure encryption algorithm that ensures privacy and low-latency image processing for video consultation using the Transmission Control Protocol/Internet Protocol (TCP/IP). The video consultation application is a custom made application developed using Active Server Pages (ASP.NET) framework with Visual Basic (VB) as the code behind the language. The application uses a very minimal bandwidth of 500 kbps to facilitate low bandwidth video consultation so that any patient with inadequate network coverage too can utilize the teleconsultation service. When a clinician initiates a call, he has features like zoom in and out the patient’s video for better medical observation. The system also ensures that the secure channel for video consultation is closed, and the patient cannot use the same channel again once the clinician marks the call as ended. The two-way communication can also be used for audio consultation only and the clinician has the freedom to choose between audio and video.
During teleconferencing, they were inquired about their illness, any new complaints, whether they had any difficulty in procuring medication during the lockdown period, whether the disease had worsened, or was stable, etc. We analyzed the following points for assessing the feasibility of video teleconsultation. How many PWEs could be contacted, and how many of them registered? How many PWEs had smartphones with video facilities? How many did not have smartphones but connected through caregiver numbers? How many were not willing to do video conferencing? How many PWEs had internet connectivity issues? How many were successful connections? How many attempts had to be made before a successful connection? How much time was spent by a doctor on a consult? On a day, how many appointments were made, and how many of them were completed? Was there any additional cost for staff, technology, licensing etc.? How easy was it for the team to use?
For assessing the acceptability/satisfaction, a 14-point Telemedicine Satisfaction Questionnaire was used in local language [13]. A separate person different from the teleconsultation service provider administered this questionnaire.
We analyzed the following points for assessing the effectiveness: Any new symptoms/exacerbation reported? Able to diagnose based on history/video? Able to prescribe treatment (New vs. Old)? The number of referrals made to other departments?
2.2. Statistical methods
We entered the data collected in Epicollect5 into SPSS 19 software. Descriptive analysis based on each indicator was done (the questions of satisfaction questionnaire, feasibility assessment, and effectiveness assessment) and expressed as proportions
3. Results
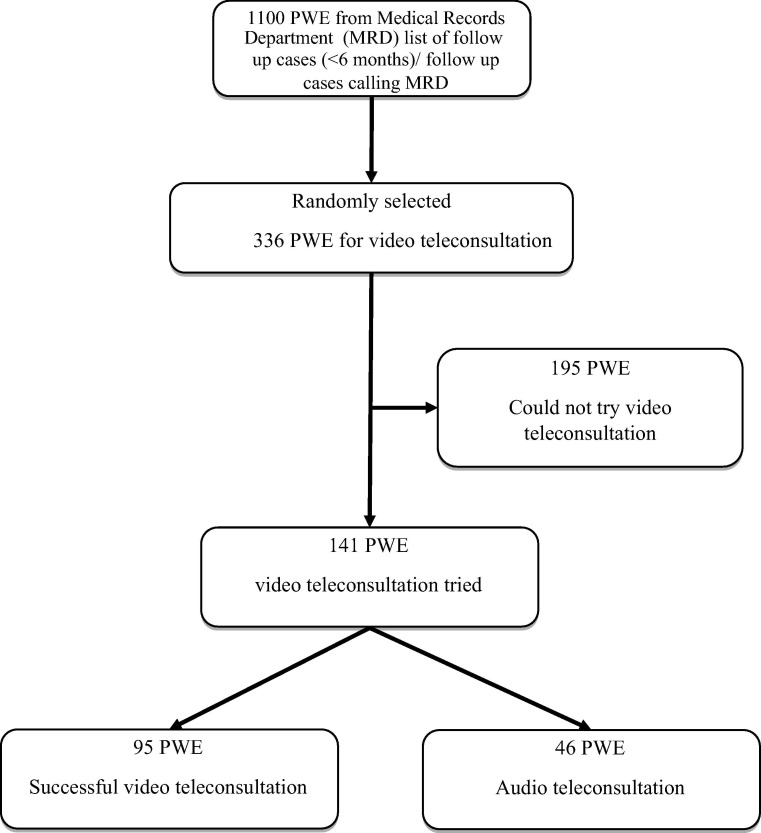
From June 2020 to October 2020, we screened 1100 PWEs and we recruited 336 participants who fulfilled inclusion and exclusion criteria. Out of 336, we attempted video teleconsultation in 141 (41.9%) participants Fig. 1 . The reasons for not attempting video consultation in the remaining participants are depicted in Fig. 2 . Two significant reasons were lack of smartphones in 75 (39%) and inability to contact participants in 71 (36%) due to various reasons such as out of coverage area, phone being switched off, and not responding to calls.
Fig. 1.
Flow diagram showing recruitment of participants for video teleconsultation.
Fig. 2.

Details of PWEs in whom video teleconsultation could not be tried.
We could achieve a successful video connection in 95 (28.3%) PWEs, and only audio consultation in 46 (13.7%). There were no significant differences in age, gender, the educational status between those who had successful video teleconsultation and those who had failed video teleconsultation. Table 1 .
Table 1.
Comparison of demographic and clinical characteristics of Persons with Epilepsy (PWEs) who had successful video teleconsultation and those who had failed video consultation.
| Characteristics | Video consultation successful (n = 95) Number (%) |
Video consultation Failed (n = 46) Number (%) |
p value |
|---|---|---|---|
| Age groups (years) | |||
| <20 years | 27(28.4) | 17(37.0) | |
| 20–39 years | 50(52.6) | 25(54.3) | |
| 40–59 years | 14(14.7) | 4(8.7) | |
| ≥60 years | 4(4.2) | 0(0) | |
| Mean (SD) age | 28.4(13.2) | 24.9(9.9) | 0.08 |
| Gender | 0.21 | ||
| Male | 56(58.9) | 22 (47.8) | |
| Female | 39(41.1) | 24 (52.2) | |
| Years of schooling | 0.54 | ||
| No formal education | 10(10.5) | 2(4.3) | |
| <5 years | 7(7.4) | 4(8.7) | |
| 5–10 years | 41(43.2) | 26(56.5) | |
| 11–15 years | 33(34.7) | 13(28.3) | |
| >15 years | 4(4.2) | 1(2.2) | |
| Diagnosis- Epilepsy etiology | 0.02 | ||
| Structural | 44(46.3) | 19(41.3) | |
| Genetic | 35(36.8) | 9(19.6) | |
| Post infectious | 2(2.2) | 3(6.5) | |
| Immune | 1(1.1) | 0 | |
| Unknown | 13(13.7) | 15(32.6) | |
| Access to smart phone | |||
| Own | 30(31.6) | 12(26.1) | 0.74 |
| Care giver | 65(68.4) | 34(73.9) |
On a day, we made 5–10 registrations and completed them on the same day. We took a median time of 8 (5–14) minutes from initiating teleconsultation to completion of the interaction. There were 11 participants who required more than 30 min for a successful connection, and four of them required more than an hour. Only 19 (20%) participants could connect successfully in the first attempt itself, whereas remaining people required two (47.4%) or three (32.6%) attempts. The main reason for more than one attempt and extra time for consultation was the difficulty in teaching the participants how to enable the video facility in their smartphones. Out of 95 participants who had successful video teleconsultation, only 30 (31.6%) used their mobile phones, and the remaining people used the caretaker's phones. Ninety (95%) had continued their anti-seizure medication during the lockdown, 47 (49.5%) received it from government hospitals and primary health centers (PHCs). Except for the registration and the assessment of the satisfaction, the entire teleconsultation was managed by two physicians, and no additional training for staff was involved neither extra cost, as the Institute provided it as an extension of the existing Hospital Information System.
After teleconsultation, we could provide prescriptions to all 95 PWEs, and for 18 (18.9%) of them, we could even add new medications. The physician felt that the video quality was good in 68 (71.6%), average in 22 (23.2%) and bad in five (5.3%), and audio quality was good in 62 (65.3%), average in 24 (25.3%), and bad in 9 (9.5%) connections. For two participants, we identified new symptoms and referred them to other specialties. Six of them were post epilepsy surgery cases, and we could advise regarding the drug tapering.
During the assessment of satisfaction of video teleconsultation, more than 90% of participants either ‘agreed’ or ‘strongly agreed’ on 12 out of 14 questions such as – they could easily see, hear, talk, communicate, get enough attention, fulfill their healthcare needs, and save time. They also opined that they would like to receive teleconsultation again in the future and were overall satisfied with teleconsultation Table 2 . Forty-six (48.4%) participants either disagreed or strongly disagreed that assistance is needed for teleconsultation.
Table 2.
Satisfaction regarding teleconsultation among persons with epilepsy (N = 95).
| Indicator | Strongly disagree/disagree | Neutral | Strongly agree/agree |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Could you easily talk to your healthcare provider | 0 (0.0) | 1 (1.1) | 94 (98.9) |
| Could you hear your healthcare provider clearly? | 0 (0.0) | 2 (2.1) | 93 (97.9) |
| Whether your healthcare provider is able to understand your healthcare condition? | 0 (0.0) | 2 (2.1) | 93 (97.9) |
| Could you see your healthcare provider as if you met in person? | 1 (1.1) | 9 (9.5) | 85 (89.5) |
| Do you need assistance while using the system? | 46 (48.4) | 0 (0.0) | 49 (51.60 |
| Do you feel comfortable communicating with your healthcare provider? | 0 (0.0) | 2 (2.1) | 93 (97.9) |
| Do you think that the healthcare provided via telemedicine is consistent? | 0 (0.0) | 5 (5.3) | 90 (94.7) |
| Do you think that you obtain better access to healthcare services by use of telemedicine? | 0 (0.0) | 0 (0.0) | 95 (100.0) |
| Does Telemedicine save your time traveling to hospital or a specialist clinic? | 0 (0.0) | 0 (0.0) | 95 (100.0) |
| Do you receive adequate attention? | 0 (0.0) | 1 (1.1) | 94 (98.9) |
| Does Telemedicine fulfill your healthcare need? | 0 (0.0) | 3 (3.2) | 92 (96.8) |
| Do you find telemedicine an acceptable way to receive healthcare services? | 0 (0.0) | 4 (4.2) | 91 (95.8) |
| Will you use telemedicine services again? | 0 (0.0) | 1 (1.1) | 94 (98.9) |
| Overall, are you satisfied with the quality of service being provided via telemedicine? | 0 (0.0) | 2 (2.1) | 93 (97.9) |
4. Discussion
In this observational study, we assessed the feasibility, effectiveness, and acceptability/satisfaction of the newly introduced video teleconsultation module for managing the follow-up PWE. Out of the 336 participants included in study 95 (28.3%) PWEs had successful video teleconsultation, and another 46 (13.7%) had audio consultation. Of the 95 PWEs, majority were satisfied with the video teleconsultation modality.
Tele-stroke is a well-established telemedicine technique with equivalence to the person to person consultation [14]. Teleconsultation has also been studied for the management of conditions such as headache, parkinsonism, multiple sclerosis, etc. [6], [7], [15]. There have been studies on telemedicine in epilepsy care. Still, most of them used dedicated satellite centers with telemedicine facilities and a central coordinating center [16], [17]. For this, considerable infrastructure is required and people have to travel and reach the offices rather than staying at their home. For RTV (synchronous), various methods have been used, such as carts attached with Pan-tilt zoom camera, robots, or PCs [14].
mHealth (or mobile health) is commonly defined as the provision of health services through mobile technologies. The mHealth application as a consultation modality is rare [8]. Most of the mHealth applications in epilepsy care are for educational purposes, seizure tracking, and social support rather than real-time consultation [18]. We used mobile communication technology for real-time video consultation. The institution did not have to set up satellite centers in the periphery, and the healthcare seekers did not have to download any specific applications. Lack of adequate infrastructure has been a significant challenge in India. Some of the rural areas may experience poor network connectivity. Most of the low-income population cannot afford to buy a decent smartphone, which will give them access to mHealth. However, as of October 2020, the global average for mobile Internet traffic as a percentage of the total web traffic is 50%. India ranks second on this parameter at 64.37% [19].
Despite all these, we were able to have successful video teleconsultation with 27% of our participants, in a situation where the personal visit was impossible and at no additional cost to the participant. Even though only 1/3rd of the participants had their smartphones, we could have successful consultations with the remaining people using caregivers’ smartphones. A recent study from the same region reported a similar finding that only 22% reported having a smartphone [20]. In around 195 (58%) PWEs, no audio or video teleconsultation could be done. A definite reason was available in 81 of them. The primary reason in this group was the lack of smartphones in 75 (39%), with them or with the caregiver. Four PWEs were not interested in a consultation and two had expired during this period. We could not contact 71 PWEs as the phones were either switched off, not ringing, or ringing but not answering. If we could reach them, a proportion of them probably could have had successful consultation, and if we exclude them, the success rate of video teleconsultation becomes 40.25%. A sizable proportion, 48 PWEs (22%), could not pick up the calls when we contacted, which also contributed to the failure of the video consultation. One method by which we may overcome this situation is by collecting alternate mobile phone numbers including that of the caregiver at the time of initial registration and asking them to update the EHR whenever they are changing their mobile phone numbers.
The time taken for getting video connected and consultation done was a factor that might require improvement. Besides, the failure to get the video facility connected was the sole reason for the failure of consultation in those in whom it was tried. Since such a facility was not existing previously and was introduced during the lockdown, the participants could not be trained about the method in person. The training was given using the SMS service and voice call. Further, since this was a cross-sectional study, we have not assessed the ease of use during subsequent calls.
This indicates that we need to improve the infrastructure to make video teleconsultations more feasible to the rural population, but it is not impossible. Smartphones may be made available at more affordable prices, the network coverage should be improved, and the public should be taught about the internet usage. Recent proposal of the central government to introduce free Wi-Fi facilities for the rural population will be a giant leap toward better mHealth care.
All consultations were follow-up consultations and according to the national teleconsultation guidelines. Except for minor issues in audio and video qualities, all these consultations resulted in a prescription generation and in around 18 of them new drugs were added. We could contact six post epilepsy surgery cases successfully and we could advise regarding the tapering of drugs. A few of the PWEs were referred to other departments for additional evaluation, and overall physicians could effectively convey the advice.
In mobile health, even if the infrastructure is present, security and privacy are major concerns. More than 1.5 lakh mHealth applications are available, and there is no way to know if the application developer has taken appropriate measures to ensure security and protect his/her application against malicious attacks. The advantage of the system we tried was that the participants did not have to download and install the application on their smartphones. The link for teleconsultation was sent as a message to them. There were no additional costs incurred for the participants.
More than 90% of participants were satisfied with the video teleconsultation using mobile phones. The satisfaction was similar to that observed in studies from Northern India and Canada [8], [21], [22]. The current study is different from those two studies in that real-time video consultation using mobile phones was utilized in our research.
The limitation of our study is the cross-sectional nature with its inherent drawbacks. We did not have a control group to compare, but in the current scenario where in-person consultations are impossible, due to pandemic, we could not have found one. The strong points of the present study are the assessment of real-time video teleconsultation using mobile phones in rural populations without any prior training, and the participants did not have to download and install the application in their smartphones
5. Conclusion
Although we need to make video teleconsultation more feasible, our synchronous mobile video teleconsultation model is an effective and acceptable method to follow up PWEs. This real-time model has the advantage that it does not require any mobile application to be downloaded and installed. Further studies are needed to evaluate methods to improve the reach of these services particularly to vulnerable groups of the population.
Acknowledgments
Acknowledgements
Nil.
Declarations of interest
None.
Authors have no disclosures to declare.
References
- 1.Ganapathy K. Telemedicine and neurosciences. J Clin Neurosci. 2005;12:851–862. doi: 10.1016/j.jocn.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Balasinorwala V.P., Shah N.B., Chatterjee S.D., Kale V.P., Matcheswalla Y.A. Asynchronous telepsychiatry in Maharashtra, India: study of feasibility and referral pattern. Indian J Psychol Med. 2014;36:299–301. doi: 10.4103/0253-7176.135384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allely E.B. Synchronous and asynchronous telemedicine. J Med Syst. 1995;19:207–212. doi: 10.1007/BF02257174. [DOI] [PubMed] [Google Scholar]
- 4.Gowda G.S., Kulkarni K., Bagewadi V., Rps S., Manjunatha B.R., Shashidhara H.N., et al. A study on collaborative telepsychiatric consultations to outpatients of district hospitals of Karnataka, India. Asian J Psychiatry. 2018;37:161–166. doi: 10.1016/j.ajp.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal S., Warburton E.A. Teleneurology: is it really at a distance? J Neurol. 2011;258:971–981. doi: 10.1007/s00415-011-5920-5. [DOI] [PubMed] [Google Scholar]
- 6.Dorsey E.R., Deuel L.M., Voss T.S., Finnigan K., George B.P., Eason S., et al. Increasing access to specialty care: a pilot, randomized controlled trial of telemedicine for Parkinson’s disease. Mov Disord. 2010;25:1652–1659. doi: 10.1002/mds.23145. [DOI] [PubMed] [Google Scholar]
- 7.Kane R.L., Bever C.T., Ehrmantraut M., Forte A., Culpepper W.J., Wallin M.T. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J Telemed Telecare. 2008;14:190–194. doi: 10.1258/jtt.2008.070904. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed S.N., Mann C., Sinclair D.B., Heino A., Iskiw B., Quigley D., et al. Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient’s perspective. Epilepsia. 2008;49:573–585. doi: 10.1111/j.1528-1167.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 9.Davis L.E., Coleman J., Harnar J., King M.K. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J e-Health Off J Am Telemed Assoc. 2014;20:473–477. doi: 10.1089/tmj.2013.0217. [DOI] [PubMed] [Google Scholar]
- 10.Davis L.E., Harnar J., LaChey-Barbee L.A., Pirio Richardson S., Fraser A., King M.K. Using teleneurology to deliver chronic neurologic care to rural veterans: analysis of the first 1,100 patient visits. Telemed J e-Health Off J Am Telemed Assoc. 2019;25:274–278. doi: 10.1089/tmj.2018.0067. [DOI] [PubMed] [Google Scholar]
- 11.Velasquez S.E., Chaves-Carballo E., Nelson E.-L. Pediatric teleneurology: A model of epilepsy care for rural populations. Pediatr Neurol. 2016;64:32–37. doi: 10.1016/j.pediatrneurol.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Patterson V. Teleneurology in Northern Ireland: a success. J Telemed Telecare. 2002;8(Suppl 3):46–47. doi: 10.1258/13576330260440835. [DOI] [PubMed] [Google Scholar]
- 13.Yip M.P., Chang A.M., Chan J., Mackenzie A.E. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: A preliminary study. J Telemed Telecare. 2003;9:46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 14.Wechsler L.R. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72:349–354. doi: 10.1001/jamaneurol.2014.3844. [DOI] [PubMed] [Google Scholar]
- 15.Müller K.I., Alstadhaug K.B., Bekkelund S.I. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017;89:153–162. doi: 10.1212/WNL.0000000000004085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Craig J., Patterson V., Russell C., Wootton R. Interactive videoconsultation is a feasible method for neurological in-patient assessment. Eur J Neurol. 2000;7:699–702. doi: 10.1046/j.1468-1331.2000.00133.x. [DOI] [PubMed] [Google Scholar]
- 17.Rasmusson K.A., Hartshorn J.C. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia. 2005;46:767–770. doi: 10.1111/j.1528-1167.2005.44804.x. [DOI] [PubMed] [Google Scholar]
- 18.Escoffery C., McGee R., Bidwell J., Sims C., Thropp E.K., Frazier C., et al. A review of mobile apps for epilepsy self-management. Epilepsy Behav. 2018;81:62–69. doi: 10.1016/j.yebeh.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Mobile internet traffic share in selected countries 2020 | Statista n.d. https://www.statista.com/statistics/430830/share-of-mobile-internet-traffic-countries/ (accessed December 21, 2020).
- 20.Sreejith G., Menon V. Mobile phones as a medium of mental health care service delivery: perspectives and barriers among patients with severe mental illness. Indian J Psychol Med. 2019;41:428–433. doi: 10.4103/IJPSYM.IJPSYM_333_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bahrani K., Singh M.B., Bhatia R., Prasad K., Vibha D., Shukla G., et al. Telephonic review for outpatients with epilepsy—A prospective randomized, parallel group study. Seizure. 2017;53:55–61. doi: 10.1016/j.seizure.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Panda P.K., Dawman L., Panda P., Sharawat I.K. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]