Background:
The tuberous breast is a rare malformation that can affect psychosocial well-being in young women. Its management represents a great challenge to plastic surgeons. Many surgical procedures have been described to correct different grades of tuberous breast deformity (TBD). The authors describe their one-stage technique for correcting grade 2 TBD.
Methods:
Sixteen women affected by grade 2 TBD treated with glandular flaps, silicone gel prosthesis, and only an hemiperiareolar incision between January 2018 and January 2019 were reviewed. The age range was 19–27 years (mean age was 25). Follow-up average was 25 months (range 16–33 months). To evaluate the results, we used two analogic scales with values from 1 to 3, where the lower value was the worst result. First, an independent medical team of three plastic surgeons evaluated two parameters: correction of deformity and symmetry. Then, patients were asked to judge the result obtained.
Results:
The resulting breast has a normal-shaped areola without bulging, a natural shape, a volume matching the contralateral breast, and no evidence of “double-bubble” deformity or irregularities of the lower pole shape.
Conclusion:
We propose this one-stage approach with hemiperiareolar incision, to minimize time interval to obtain final results in TBD correction, with reduced scar dimensions to avoid all the possible complications related to the round block suture.
Takeaways
Question: Is it possible to treat TBD in a one-stage procedure, improving cosmetic results compared to other techniques?
Findings: Yes, it is possible by using technical details, like glandular flap, radial incision of inferior quadrants, and retroglandular silicone gel implants, with only a small emiperiareolar scar.
Meaning: Many patients with TBD, who did not require an areolar reduction, could benefit from a minimally invasive emiperiareolar incision approach.
INTRODUCTION
In 1976, Rees and Aston1 described for the first time the tuberous breast deformity (TBD), asserting that this complex breast asymmetry and shape deformity cannot usually be corrected satisfactorily by standard augmentation mammoplasty or mastopexy. The tuberous aberration of breast shape could include a constricted breast base, hypoplastic breast tissue, herniated nipple-areola complex, deficient skin envelope inferiority, and elevated inframammary fold.2 The exact incidence of TBD is unknown, as is its etiology, but a high prevalence in the general population and in women seeking breast augmentation or breast reduction (about 50%) is well established.3 This malformation presents itself at the age of puberty, causing remarkable psychological repercussions and altering personal rapports within young patients. Various classifications were reported to grade tuberous breasts deformity. The first classification of Von Heimburg et al in 19964 divided the entity of deformity in four types. We prefer to use the Grolleau classification to review our patients. Grolleau et al5 proposed a classification modifying the Von Heimburg classification, but they retained only three of their four types because the difference between their types II and III has no objective anatomic or clinical reality. Grolleau used a three-type classification:
Type I: only the lower medial quadrant is deficient. Whatever the volume of the breast, its lower medial edge is characteristically shaped like an italic S, and its lateral part appears oversized in comparison.
Type II: both lower quadrants are deficient. The areola points downward and the subareolar cutaneous segment is short.
Type III: all four quadrants are deficient, and the breast base is constricted both horizontally and vertically.
In typical forms, the breast is shaped like a tubercle, but in certain cases, the gland is so underdeveloped that its appearance is that of major hypoplasia. Numerous surgical techniques have been described, reflecting the reconstructive challenge of this variable deformity (See table, Supplemental Digital Content 1, which displays a review of surgical techniques for TBD treatment, http://links.lww.com/PRSGO/C313.) As reported by Foustanos et al,6 more than 15 authors describe surgical techniques to manage this deformity through one-stage or two-stage procedures. Many authors use periareolar mastopexy associated with the use of a mammary implant, others use skin expanders,7–11 and still others use a complete autologous reconstruction rearranging the inferior pole of the breast, using glandular plasty, cutaneous flaps, or Z-plasty.12–17
Fat grafting recently has been proposed to correct the cleavage and the remaining constricting ring.18–21 All techniques described up to now provide minimum a complete scar around the areola, even closed with a round block suture using permanent material. (See table, Supplemental Digital Content 1, http://links.lww.com/PRSGO/C313.) The aim of this current study is to show the reliability of our new technique refinement to manage grade 2 tuberous breast. We reserved this technique for patients who did not require an areolar reduction. We achieve correction of the deformity in a one-stage surgery by glandular flap, radial incision of inferior quadrants, and retroglandular silicone gel implants, with only a small hemiperiareolar scar.
MATERIAL AND METHODS
Between 2018 and 2019, 16 patients affected by type II TBD were included in this study. The age range was 19–27 years (mean age was 25). Follow-up average was 25 months (range 16–33 months). All patients had pre- and postoperative standardized pictures of the anterior chest wall. To evaluate the results, we used two analogic scales with values from 1 to 3, where 1 corresponds to poor; 2, good; and 3, excellent. An independent medical team of three plastic surgeons who did not participate in surgery administered one that evaluated two parameters: correction of deformity and symmetry. Moreover, all patients were asked to judge the result obtained, using the other analogic scale.
SURGICAL TECHNIQUE
The procedure begins with a single inferior hemiperiareolar incision on the edge of the areola; next, we make a dissection in the extraparenchymal subcutaneous tissue until fascial plane in the lower pole. We dissect the entire base of the mammary gland, detaching the gland from the pectoral fascia to perform a suitable pocket; we make a vertical and horizontal scoring of lower pole, principally on old inframammary fold where the breast is more constricted. A subareolar superior pedicle glandular flap is harvested from the upper pole of the areola, where bulging is evident, then it is transferred to the lower pole. The flap is elevated through an “inverted V” glandular incision performed in the upper pole of areola where bulging of the nipple-areola complex is more evident. Following this, we split the distal portion of the glandular flap into three or four little tongues (Fig. 1). Before inserting the definitive breast implant, we use inflatable sizers to estimate the required volume and to stretch the pocket by hyperexpansion. The use of inflatable sizers is particularly useful in the case of breast asymmetry that is frequently associated with this breast deformity.
Fig. 1.
Intraoperative view of the subareolar superior pedicled glandular flap that it is harvested from the upper pole of the areola, where bulging is evident; then, it is transferred to the lower pole. The flap is elevated through an “inverted V” glandular incision performed in the upper pole of areola where nipple-areola complex bulging is more evident. Following this, we then split the distal portion of the glandular flap into three or four little tongues.
After implantation of the prosthesis, the inferior hypoplasic breast pole is filled with the glandular flap, anchoring the three or four tongues of distal portion with subcutaneous stitches based on the old inframammary folds. Therefore, the glandular tissue that causes the areola bulging is sliced vertically to fill the inferior pole, avoiding the double bubble.
Although many authors use transcutaneous stitches to fix the glandular flaps differently, we prefer not to use transcutaneous stitches to avoid possible skin necrosis or maceration phenomena and to reduce the risk of infection. We fix the flap with absorbable subcutaneous stitches; then we suture the hemiperiareolar incision. A micropore dressing is always inserted to immobilize the prosthesis. The patient should not exert herself during the week after surgery and should sleep in the supine position. We use mammary prostheses of different volume and projection, thus obtaining the highest degree of symmetry.
RESULTS
At 12 months after surgery the medical team rated 38% of cases as excellent, 57% as good and 5% as poor. After 12 months of follow-up, the judgment of patients was 43% excellent, 53% good, and 4% poor. The results of three patients treated by our team are shown in Figures 2–4. The achieved breast has a normal-shaped areola without bulging, a natural shape, a volume matching the contralateral breast, and no evidence of the “double-bubble” deformity or irregularities of the lower pole shape (Figs. 2–4). All the results were obtained with our single-step technique without a complete periareolar incision or round block suture. No early or delayed postsurgical complications have been recorded for any patients.
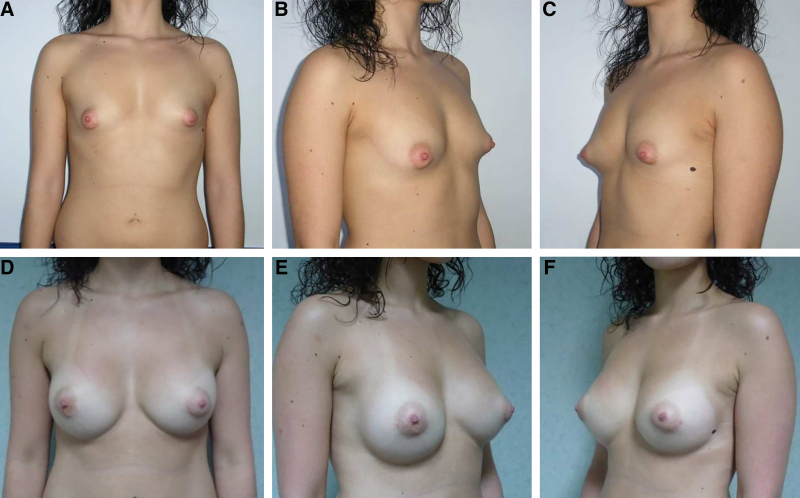
Fig. 2.
Pre- and postoperative views. A–C, Frontal and lateral views of a 23-year-old patient consulting for correction of her TBD (grade 2) and the asymmetry. D–F, Results after 12 months of follow-up, frontal and lateral views.
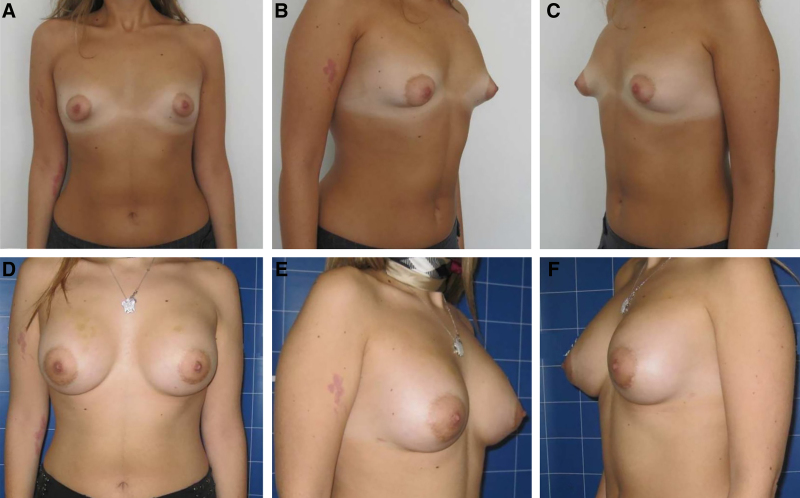
Fig. 4.
Pre- and postoperative views. A–C, Frontal and lateral views of a 25-year-old patient with a different grade of TBD (right breast grade 2, left breast grade 1) and asymmetry of inframammary folds and volume. D–F, Results after 18 months of follow-up, frontal and lateral views.
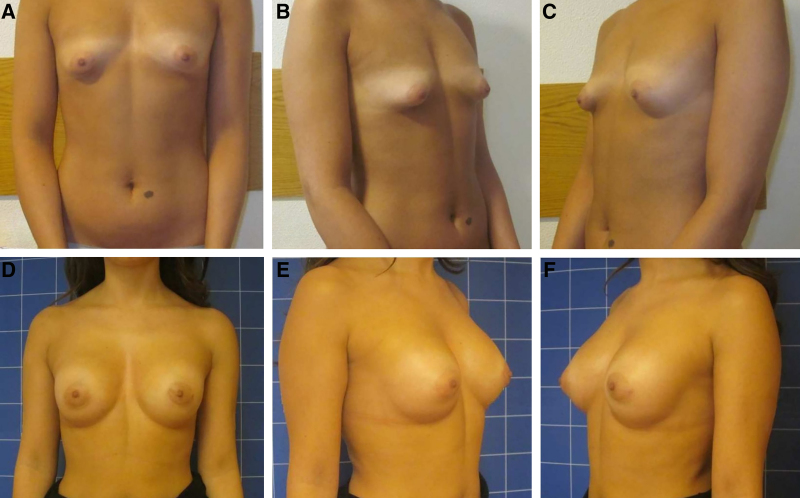
Fig. 3.
Pre- and postoperative views. A–C, Frontal and lateral views of a 19-year-old patient consulting for correction of her TBD (grade 2) and the asymmetry. Note the enlarged areolas; this young patient refused to reduce her areolas because she did not accept a complete periareolar scar. D–F: Results after 12 months of follow-up, frontal and lateral views.
DISCUSSION
Numerous procedures have been described to correct the variety of forms of TBD with their advantages and disadvantages. (See table, Supplemental Digital Content 1, http://links.lww.com/PRSGO/C313.) In our experience, the simple augmentation with silicone implants is not the right technique for the correction of tuberous breasts.22 The reduction of the normal side is easy, but it does not correct the basic problem, and it is possible only in cases with a unilateral breast deformity.23 Many of the techniques described consist of two surgical stages to achieve the result. We believe that two surgical stages and 3 to 6 months or more to obtain a final result are ambitious for these young patients. Other authors perform periareolar mastopexy associated with a mammary implant achieving the results through a one-stage approach. As proposed by the Muti technique, the areolar elevation and its dimensional reduction are achieved by periareolar deepithelialization and by vertical rhomboid deepithelialization in the central part of the lower pole from the nipple to the existing sulcus associated with the glandular flap.15 This technique results in a complete periareolar scar and a little vertical scar from the nipple to the inframammary fold. Other authors perform a completely autologous reconstruction using different glandular plasty and various cutaneous flaps to rearrange the inferior pole of the breast, consequently with very extended scars. (See table, Supplemental Digital Content 1, http://links.lww.com/PRSGO/C313.) To date, all the techniques described to treat type II tuberous breasts result in a minimum complete periareolar scar, sometimes associated with a vertical scar, “Z scar” or “L scar.” (See table, Supplemental Digital Content 1, http://links.lww.com/PRSGO/C313.) In our experience, these large scars are not well accepted by young patients, and they more willingly agree to large or asymmetric areolas rather than extended scars. In the past, we performed a complete periareolar approach, as described in 1990 by Benelli,24 with nonoptimal results. We have experienced that the round block technique to confine the scar in the areola creates several problems: scar widening, suture infection (especially using braided suture), decubitus phenomena, changes in areola shape, and rupturing of necessary nonabsorbable suture.25–27 Indeed, the periareolar technique usually entails the closure of the defect under tension for the inevitable discrepancy between the areola diameter and the outer edge of the wound circumference; this problem occurs also when some of the discrepancy is compensated by vertical skin take-out. This often leads to areolar distortions, scar widening, and hypertrophic scarring,27 and it is a well-known setup for litigation with an unfavorable outcome for the surgeon.10 This unfortunate complication is highlighted even more when volume is added by an implant, thus increasing tension on the suture. For all these reasons, we believe that the best option for these patients should be the technique baring minimal scars in minimal time to join the definitive result with the best cosmetic long-term outcome and low complication rate. Some recent authors have described the fat grafting application for TBD.20,21 We consider fat grafting only as an addition to the routine surgery if it is necessary. Using lipofilling with patients having distinctive severe deformation may not achieve satisfactory aesthetic results without parenchyma modification of the gland. Moreover, these methods often require two or more stages for TBD correction. These drawbacks may lead to complications to consider for reaching an optimal aesthetic outcome. Other authors have described techniques, with their strengths and weaknesses, where they avoid a periareolar approach.28–30 In this study, we present our one-stage approach with a minimal hemiperiareolar incision, to minimize the time interval for achieving the final result, with reduced scar dimensions, avoiding all the possible complications related to the round block suture. We preferred not to use transcutaneous stitches to replace the flaps in the inframammary fold, but we used internal subcutaneous stitches to anchor the glandular flap, avoiding the possible infection facts that could occur during the removal of stitches or maceration phenomena in the inframammary fold.
CONCLUSIONS
The aim of this study is to determine whether these encouraging results could translate to long-term benefits for treatment of TBD, reducing the common complications of periareolar surgery. Although our experience to date with this technique has been limited in number, we have been pleased with the postoperative results.
PATIENT CONSENT
Written informed consent was obtained.
Supplementary Material
Footnotes
Published online 15 December 2022.
The study was approved by the Institutional Review Board of University of Campania Luigi Vanvitelli and performed in accordance with the principles of the Declaration of Helsinki.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg. 1976;3:339–347. PMID: 1261187 [PubMed] [Google Scholar]
- 2.Kolker AR, Collins MS. Tuberous breast deformity: classification and treatment strategy for improving consistency in aesthetic correction. Plast Reconstr Surg. 2015;135:73–86. [DOI] [PubMed] [Google Scholar]
- 3.Klinger M, Caviggioli F, Giannasi S, et al. The prevalence of tuberous/constricted breast deformity in population and in breast augmentation and reduction mammaplasty patients. Aesthetic Plast Surg. 2016;40:492–496. [DOI] [PubMed] [Google Scholar]
- 4.von Heimburg D, Exner K, Kruft S, et al. The tuberous breast deformity: classification and treatment. Br J Plast Surg. 1996;49:339–345. [DOI] [PubMed] [Google Scholar]
- 5.Grolleau JL, Lanfrey E, Lavigne B, et al. Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg. 1999;104:2040–2048. [DOI] [PubMed] [Google Scholar]
- 6.Kanos A, Zavrides H. Surgical reconstruction of tuberous breasts. Aesthetic Plast Surg. 2006;30:294–300. [DOI] [PubMed] [Google Scholar]
- 7.Kneafsey B, Crawford DS, Khoo CT, et al. Correction of developmental breast abnormalities with a permanent expander/implant. Br J Plast Surg. 1996;49:302–306. [DOI] [PubMed] [Google Scholar]
- 8.Scheepers JH, Quaba AA. Tissue expansion in the treatment of tubular breast deformity. Br J Plast Surg. 1992;45:529–532. [DOI] [PubMed] [Google Scholar]
- 9.Sohet C, Heymans O. Expansion tissulaire et seins tubéreux: à propos de dix cas [Tissular expansion and tuberous breasts: 10 cases report]. [French]. Ann Chir Plast Esthet. 2007;52:187–195. [DOI] [PubMed] [Google Scholar]
- 10.Versaci AD, Rozzelle AA. Treatment of tuberous breasts utilizing tissue expansion. Aesthetic Plast Surg. 1991;15:307–312. [DOI] [PubMed] [Google Scholar]
- 11.Toranto IR. Two-stage correction of tuberous breasts. Plast Reconstr Surg. 1981;67:642–646. [DOI] [PubMed] [Google Scholar]
- 12.Argenta LC, VanderKolk C, Friedman RJ, et al. Refinements in reconstruction of congenital breast deformities. Plast Reconstr Surg. 1985;76:73–82. [DOI] [PubMed] [Google Scholar]
- 13.Bruck HG. Hypoplasia of the lower medial quadrant of the breast. Aesthetic Plast Surg. 1992;16:283–286. [DOI] [PubMed] [Google Scholar]
- 14.Dinner MI, Dowden RV. The tubular/tuberous breast syndrome. Ann Plast Surg. 1987;19:414–420. [DOI] [PubMed] [Google Scholar]
- 15.Muti E. Personal approach to surgical correction of the extremely hypoplastic tuberous breast. Aesthetic Plast Surg. 1996;20:385–390. [DOI] [PubMed] [Google Scholar]
- 16.Puckett CL, Concannon MJ. Augmenting the narrow-based breast: the unfurling technique to prevent the double-bubble deformity. Aesthetic Plast Surg. 1990;14:15–19. [DOI] [PubMed] [Google Scholar]
- 17.Ribeiro L, Canzi W, Buss A, Jr, et al. Tuberous breast: a new approach. Plast Reconstr Surg. 1998;101:42–50; discussion 51–52. [DOI] [PubMed] [Google Scholar]
- 18.Serra-Renom JM, Muñoz-Olmo J, Serra-Mestre JM. Treatment of grade 3 tuberous breasts with Puckett’s technique (modified) and fat grafting to correct the constricting ring. Aesthetic Plast Surg. 2011;35:773–781. [DOI] [PubMed] [Google Scholar]
- 19.Ho Quoc C, Piat JM, Michel G, et al. Apport du transfert graisseux dans les formes sévères de seins tubéreux [Fat grafting to improve severe tuberous breast]. [French]. J Gynecol Obstet Biol Reprod (Paris). 2015;44:503–509. [DOI] [PubMed] [Google Scholar]
- 20.Brault N, Stivala A, Guillier D, et al. Correction of tuberous breast deformity: a retrospective study comparing lipofilling versus breast implant augmentation. J Plast Reconstr Aesthet Surg. 2017;70:585–595. [DOI] [PubMed] [Google Scholar]
- 21.Claudio Silva-Vergara C, Fontdevila J, Weshahy O. Fat grafting technique, a paradigm shift in the treatment of tuberous breast. World J Plast Surg. 2018;7:72–77. PMCID: PMC5890369 [PMC free article] [PubMed] [Google Scholar]
- 22.Pacifico MD, Kang NV. The tuberous breast revisited. J Plast Reconstr Aesthet Surg. 2007;60:455–464. [DOI] [PubMed] [Google Scholar]
- 23.Corso PF. Plastic surgery for the unilateral hypoplastic breast. A report of eight cases. Plast Reconstr Surg. 1972;50:134–141. [DOI] [PubMed] [Google Scholar]
- 24.Benelli L. A new periareolar mammaplasty: the “round block” technique. Aesthetic Plast Surg. 1990;14:93–100. [DOI] [PubMed] [Google Scholar]
- 25.Azzawi K, Humzah MD. Mammaplasty: the “Modified Benelli” technique with de-epithelialisation and a double round-block suture. J Plast Reconstr Aesthet Surg. 2006;59:1068–1072. [DOI] [PubMed] [Google Scholar]
- 26.Ferraro GA, Lanzano G, Gentile C, et al. The “five-flap” technique for nipple-areola complex reconstruction. Plast Reconstr Surg Glob Open. 2021;9:e3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffman S. Some thoughts on augmentation/mastopexy and medical malpractice. Plast Reconstr Surg. 2004;113:1892–1893. [DOI] [PubMed] [Google Scholar]
- 28.Palacín Casal JM. Mamoplastia transversal en mamas tuberosas. Cirugía Plástica Ibero-Latinoamericana. 2011;37:205–214. [Google Scholar]
- 29.Galych SP, Dabizha OY, Kostenko AA, et al. Surgical treatment of tubular breast type II. Plast Reconstr Surg Glob Open. 2016;4:e1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Servaes M, Mahaudens P, Sinna R, et al. Avantages de la voie hémi-aréolaire supérieure pour la correction par implants des seins tubéreux de types II et III. Annales de Chirurgie Plastique Esthétique. 2011;56:342–350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.