Abstract
Geriatric medicine has evolved to an accepted specialty in 23 European countries. Despite much heterogeneity of postgraduate geriatric curricula, European societies have succeeded in defining a common core curriculum with a list of minimum training requirements for obtaining the specialty title of geriatric medicine. Geriatricians play a leading role in finding solutions for the challenges of health care of multimorbid older patients. One of these challenges is the demographic shift with the number of adults aged 80 years and older in Europe expected to double by 2050. Although geriatric units will play a role in the care of frail older patients, new care models are needed to integrate the comprehensive geriatric assessment approach for the care of the vast majority of older patients admitted to non-geriatric hospital units. Over the last few years, co-management approaches have been developed to address this gap. Innovative models are also in progress for ambulatory care, prevention and health promotion programs, and long-term care. Efforts to implement geriatric learning objectives in undergraduate training, and the generation of practice guidelines for geriatric syndromes may help to improve the quality of care for older patients.
Keywords: older people, geriatric medicine, geriatric assessment, postgraduate training, geriatric co-management
Key Points
The number of adults aged 80 years and older in Europe will approximately double until 2050—Geriatric medicine is now an accepted specialty field in 23 European countries.
Geriatricians may take a lead role on the individual patient level as well as in health policy.
Implementing geriatric learning objectives in undergraduate training of medical students is one important goal.
A call for action 30 years ago
Almost 30 years ago, a group of European Professors in Medical Gerontology called for action to promote geriatric medicine as a profession dedicated to maintain, improve and restore the health of older people [1]. They were concerned that a majority of European countries had not recognised the need for geriatric medicine: Their survey conducted in 1994 revealed that geriatric medicine was a recognised medical specialty in only 8 out of 25 countries. The group called for action in both undergraduate and postgraduate training to promote the recognition of geriatric medicine.
Geriatric medicine: a growing medical specialty
In the last 30 years, geriatric medicine has made large steps forward. It is now an accepted specialty in 23 European countries (Table 1), and in some additional countries, it is an established subspecialty. Only in a few remaining countries (e.g. Portugal, Greece), are efforts for obtaining national recognition for geriatric medicine still ongoing. In the context of the regulation of free movement of professionals in Europe, geriatric medicine is currently listed as a mutually accepted specialty in 21 European countries [2].
Table 1.
Duration of postgraduate training for obtaining the specialty title in geriatrics in 23 European countries with geriatrics as a recognised primary specialty
| Country | Official name of geriatrics | Duration (number of years) |
|---|---|---|
| Belgium | Gériatrie/Geriatrie | 6 |
| Bulgaria |
|
4 |
| Croatia | Gerijatrija | 5 |
| Czech Republic | Geriatrie | 4.5 |
| Germany | Geriatrie | 6a |
| Denmark | Intern medicin: geriatric | 7 |
| Finland | Geriatria/Geriatri | 5 |
| France | Gériatrie | 4 |
| Hungary | Geriátria | 5 |
| Iceland | Öldrunarlækningar | 8 |
| Ireland | Geriatric medicine | 8 |
| Italy | Geriatria | 4 |
| Lithuania | Geriatrija | 4 |
| Luxembourg | Gériatrie | 4b |
| Malta | Ġerjatrija | 8 |
| Netherlands | Klinische geriatrie | 5 |
| Norway | Geriatri | 6.5 |
| Poland | Geriatria | 5 |
| Romania | Geriatrie şi gerontologie | 5 |
| Slovakia | Geriatria | 5 |
| Spain | Geriatría | 4 |
| Sweden | Geriatrik | 6.5 |
| United Kingdom | Geriatric medicine | 9 |
aIn Germany, geriatric medicine is a recognised specialty in three federal states. In the remaining states, geriatrics is a subspecialty title.
bNo national programme for geriatric medicine, but geriatric medicine is recognised for physicians who do their postgraduate training abroad.
Table 1 documents the success of geriatric medicine as a specialty, but it also demonstrates much heterogeneity in postgraduate training curricula required for obtaining the specialty title with the length of training varying between 4 and 9 years. These differences are only the tip of an iceberg of diverse underlying organisational and training contents.
For example, in the UK, postgraduate training after medical school lasts a total of 9 years. Trainees have to undertake a 2-year basic medical training (Foundation Programme), followed by 3 years of Internal Medicine Training, and an additional 4 years’ higher level specialist training in combined Geriatric Medicine and Internal Medicine [3]. The latter curriculum is very comprehensive with trainees required to learn to manage the whole range of medical conditions at a generalist level for adults of all ages, and in addition, to cover all areas of Geriatric Medicine with experience in the acute ward, emergency care, acute stroke care, rehabilitation, ortho-geriatrics, old age psychiatry, specialist clinics (such as falls, osteoporosis, movement disorders), long-term care, community care and in other settings.
In comparison, postgraduate training for obtaining the specialty title of geriatric medicine in the Netherlands lasts only 5 years, with 2 years in internal medicine, 2 years in geriatric medicine, 3 months of neurology and 9 months in old age psychiatry [4]. Of note, long-term care is not part of the Dutch curriculum because nursing home care is the responsibility of a specialty called ‘Elderly Care Medicine’ requiring 3-year postgraduate training [5]. In Romania, postgraduate training has a duration of 5 years, but with a different structure compared with the Netherlands. It consists of 2.5 years of training in geriatrics and gerontology, with additional 12 rotations (lasting between 0.5 and 5 months each) in the fields of internal medicine; cardiology; emergency medicine; neurology; psychiatry; rheumatology; diabetes, nutrition and metabolic diseases; endocrinology; pneumology; bioethics; nephrology; and rehabilitation [6, 7].
Given this diversity, several organisations, including the European Geriatric Medicine Society, the UEMS-Geriatrics Section (European Union of Medical Specialists), the European Academy for Medicine and Ageing, and the International Association of Gerontology and Geriatrics - European region have been collaborating to try to harmonise training. A first step was to find agreement on the core definition of geriatrics. There is now an accepted definition in English, which has been translated into 20 languages [4]: ‘Geriatric Medicine is a specialty of medicine concerned with physical, mental, functional and social conditions in acute, chronic, rehabilitative, preventive and end of life care in older patients. This group of patients are considered to have a high degree of frailty and active multiple pathology, requiring a holistic approach. Diseases may present differently in old age, are often very difficult to diagnose, the response to treatment is often delayed and there is frequently a need for social support. Geriatric Medicine therefore exceeds organ orientated medicine offering additional therapy in a multidisciplinary team setting, the main aim of which is to optimise the functional status of the older person and improve the quality of life and autonomy. Geriatric Medicine is not specifically age defined but will deal with the typical morbidity found in older patients. Most patients will be over 65 years of age but the problems best dealt with by the specialty of Geriatric Medicine become much more common in the 80+ age group. It is recognised that for historic and structural reasons the organisation of geriatric medicine may vary between European Member Countries’.
This definition was then used as a basis for the development of a European standard curriculum for specialists in geriatric medicine. For developing the standard, a review of the status of geriatric medicine in Europe was conducted [8] and a Delphi process was used for finding a consensus on minimum training requirements to become a geriatrician at specialist level in European countries [9]. The resulting document entitled ‘Training requirements for the specialty of geriatric medicine’ was approved by the UEMS organisation in 2020, and was added to the 29 training requirements documents of other medical specialties available at that time [10].
Developing new approaches to hospital care
More than 30 years ago, specialised inpatient geriatric evaluation and management units were developed for ensuring optimal care of multimorbid older patients in the hospital setting, and have been shown to reduce nursing home admissions, mortality and improve functional outcomes in hospitalised older patients [11, 12]. This model of care is based on dedicated hospital units specially designed for the need of older patients at risk of functional limitations, with geriatricians in charge of patient care, and with a care process based on comprehensive geriatric assessment and an interdisciplinary approach. Today, such specialised geriatric units are an important element of hospital care.
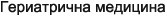
Figure 1 shows—based on the example of two countries—that geriatric units play a role in the care of hospitalised patients aged 80 years and older, but the large majority of multimorbid and frail patients are cared for in non-geriatric units. In the UK, geriatric medicine is the largest specialty doing general internal medicine and provides medical care of patients admitted acutely for almost 20% of patients aged 80 years and older, the care of rest of patients in that age group being the responsibility of physicians not specialised in geriatric medicine [13]. Germany introduced a special financial incentive for reimbursement of care in geriatric units [14]. In spite of this incentive, as a national average with large regional variations, only 6% of patients aged 80 years and older are treated in specialised units [15].
Figure 1.
Specialty with main responsibility for care in hospitalised patients aged 80 years and older in England (hospital admissions in 2019/2020) [13] and Germany (discharges from hospital in 2020) [15].
This situation stimulated the development of new approaches to ensure that patients in non-geriatric beds can also benefit from a geriatric approach. The following examples demonstrate recent innovations for health care of older patients in non-geriatric units.
In Germany, some hospitals have introduced models of collaborative care with geriatricians in orthopaedic or traumatology units for older patients with hip fracture, based on models originally developed in the UK. A descriptive study comparing patient outcomes in hospitals with and without collaborative care revealed that the collaborative approach reduced mortality rates [16]. A multicentre randomised controlled study conducted in Switzerland evaluated the effect of a nutritional intervention in patients at risk for malnutrition admitted to units of general internal medicine [17]. This study demonstrated that a standardised programme of individualised nutritional support improved important clinical outcomes, including survival compared with standard hospital food. In Belgium, a geriatric co-management programme for cardiology patients in hospital found encouraging acceptability, and identified critical factors for future success, including staffing, role of the geriatric nurse and leadership support [18].
A UK study on the effect of preoperative comprehensive geriatric assessment and optimisation prior to elective arterial vascular surgery demonstrated clinical and health economic benefits in older patients undergoing vascular surgery [19]. A review conducted in 2017 listed multiple other examples of new models for the delivery of comprehensive geriatric assessment in non-geriatric units of acute care hospitals, such as interventions based in the emergency departments, acute medical units, surgical wards or oncology settings [11].
Hospital care for older patients with dementia is especially challenging. A recent review identified 12 key items for improving care of older patients with cognitive impairment admitted to acute care wards, and 12 evidence-based recommendations for service change with the acronym DEMENTIA CARE [20].
New models for older adults in the community
One of the challenges of treating older adults in the community is the coordination of care. There is a growing awareness of fragmentation of care leading both to inefficiency and adverse outcomes in multimorbid older patients. For example, an Irish study observed ‘an absence of a shared and complete understanding of frailty amongst healthcare professionals’ and ‘a fragmented model of care for community-dwelling frail older patients’ [21]. Several recent studies addressed this issue. For example, a Swedish study tested the approach of comprehensive geriatric assessment integrated in primary care to ensure coordinated care, and found that this reduced unnecessary hospital admissions [22]. A UK study found that comprehensive geriatric assessment at home is an effective alternative for hospital admission for selected older people [23]. A Danish study of telephone-based support to assist older adults in managing their health problems found favourable effects in the subgroup of older patients with diabetes [24]. A review of innovations in France listed multiple examples of telemedicine as an additional approach for care coordination in older adults [25].
Recent research also informs on best practice in prevention and health promotion for older adults. For example, based on encouraging results of the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability, a worldwide network has been created to promote dementia prevention initiatives based on multidomain lifestyle interventions in older adults [26]. A large prospective Danish cohort study has contributed important data on cardiovascular risk and cholesterol in the understudied group of people between the ages of 70 and 100 years, leading to a better understanding of potential benefits of statin use in older age [27]. A study of health risk appraisal and counselling in older adults in Switzerland found favourable effects on risk factor modification in older adults [28], and was successfully replicated in Romania [29]. On the other hand, a large European-wide randomised controlled study found that a preventive approach based on high dose vitamin D3 strength training or Omega-3 s did not improve outcomes amongst older participants [30].
Several recent studies address the challenges of patient care in nursing homes. A randomised controlled trial conducted partly in UK care homes found no benefit and potential harm of mirtazapine in the treatment of patients with agitated behaviours with dementia, an often understudied patient group [31]. A multicentre UK trial demonstrated that a multifactorial falls prevention programme was cost-effective and resulted in a reduction in falls rate in nursing home settings [32]. A French study found that improving understanding in nursing home physicians on the treatment and management of dementia resulted in a reduction of unnecessary use of antipsychotics in older nursing home residents [33]. A survey covering 13 European countries found large interregional variations of COVID-19-related deaths amongst older adults living in nursing homes, emphasising the need for advancing best practice for this highly vulnerable patient group [34].
European guidelines and consensus papers
Over the last few years, many key issues related to health care in older adults have been synthesised on a European level, and new consensus reports help to guide clinical practice. Examples include guidelines for the diagnosis of sarcopenia [35], guidelines for the provision of care for older adults in emergency departments [36],or a consensus paper on core principles of geriatric rehabilitation [37]. Based on a European-wide Delphi consensus process, a screening tool for identifying fall-risk increasing drugs was developed for clinical use [38]. In a global initiative, European experts contributed to a world guideline on the prevention and management of falls [39].
Undergraduate training
Given that physicians of all specialties, with the exception of paediatrics, are involved in the treatment of care of older patients, it has been recognised that geriatric medicine should not be part of postgraduate training for specialty geriatricians alone, but should be part of undergraduate medical training for all future physicians. Several recent reviews demonstrate that there is still need for improvement, with key geriatric topics missing in many undergraduate curricula across Europe [40–42]. As an initial success, a European-wide consensus has been achieved for minimum requirements in undergraduate medical training [43]. There is ongoing work to refine this consensus and to advance its implementation [42, 44, 45].
Health care for older adults in the future
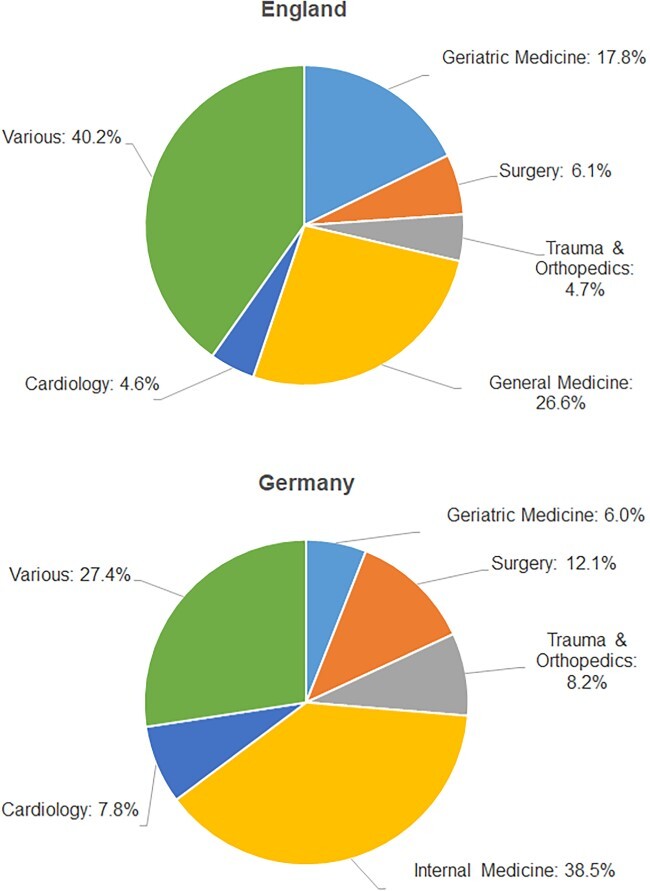
In their position paper published in 1994, the group of European Professors in Medical Gerontology emphasised that the number of adults aged 80 years and older was due to double by 2020. As we know, this prediction was more than correct, but we must realise that the demographic shift is ongoing [46]. Figure 2 depicts that the number of adults aged 80 years and older will approximately double again by 2050 in European countries.
Figure 2.
Demographic change from 2021 to 2050: percentage increase in the older population by the age group in selected European countries [46].
In contrast to other regions in the world, there will be no such increase in the younger age groups: even the number of ‘young-old’ adults will only minimally increase in Europe [Figure 2]. As a result, it will be even more challenging in the future to recruit a sufficiently high number of health and social care professionals. In countries with a small proportion of geriatricians, teaching and collaboration with other disciplines and development of new approaches of health care for older adults will become even more important.
In the future, medical progress will continue to open new options for the care of older people in European health care systems with limited resources, and address already existing challenges on how to ensure adequate quality of care for all older people. Geriatricians have the potential to take a lead role and contribute to solutions on all levels, from health policy to individual patient care. Further strengthening of the specialty field of geriatric medicine will therefore continue to be an important strategy. The goal is not to have uniform postgraduate training across Europe, but to ensure a common core competence for physicians specialised in older people. One step towards this goal is a currently ongoing effort to introduce a uniform European-level examination for specialists in geriatric medicine. Similarly, in undergraduate training, initiatives are needed to advance implementation of geriatric curricula in undergraduate education. A 4-year European Cooperation in Science and Technology-funded project called ``PROmoting GeRiAtric Medicine IN countries where it is still eMerGing (PROGRAMMING)’ has recently commenced with the aim of improving education and training in Geriatric Medicine for health care professionals in countries where the specialty is still emerging [47]. The need for action continues.
Contributor Information
Andreas E Stuck, Department of Geriatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Tahir Masud, Healthcare of Older People, Queens Medical Centre, Nottingham University Hospitals NHS Trust, Nottingham, UK; Medical Research Council and Versus Arthritis Centre for Musculoskeletal Ageing Research, University of Birmingham and University of Nottingham, Nottingham, UK; National Institute for Health and Care Research Nottingham Biomedical Research Centre for Musculoskeletal Disease theme, Nottingham, UK.
Declaration of Conflicts of Interest:
None.
Declaration of Sources of Funding:
None.
References
- 1. Stähelin HB, Beregi E, Duursma Set al. Teaching medical gerontology in Europe. Age Ageing 1994; 23: 179–81. [DOI] [PubMed] [Google Scholar]
- 2. Directive 2005/36/CE du Parlement Européen et du Conseil du 7 septembre 2005 relative à la reconnaissance des qualifications professionnelles. Date of last modification: Dec 12, 2021. Available at https://eur-lex.europa.eu/legal-content/FR/TXT/PDF/?uri=CELEX:02005L0036-20211210&from=EN (accessed 21 November 2022).
- 3. Joint Royal Colleges of Physicians Training Board . Specialty training curriculum for geriatric medicine curriculum. 2016. Available athttps://www.bgs.org.uk/resources/curriculum-specialty-training-curriculum-for-geriatric-medicine (accessed 24 October 2022).
- 4. European Union of Medical Specialists (UEMS) . Geriatric Medicine Section. 2022. Available athttps://uemsgeriatricmedicine.org/www/index.asp (accessed 24 October 2022).
- 5. Verenso (Dutch Association of Elderly Care Physicians and Social Geriatricians) . Elderly care physicians in the Netherlands, professional profile and competencies. Zwolle2015. Available athttps://www.verenso.nl/english/about-verenso/elderly-care-medicine.
- 6. Ministerul Sanatatii . Curriculum De Pregătire În Specialitatea GERIATRIE ŞI GERONTOLOGIE. 2019. Available at:https://emedic.ro/curriculum-de-pregatire-in-specialitatea-geriatrie-si-gerontologie (accessed 24 October 2022).
- 7. Kotsani M, Ellul J, Bahat Get al. Start low, go slow, but look far: the case of geriatric medicine in Balkan countries. Eur Geriatr Med 2020; 11: 869–78. 10.1007/s41999-020-00350-x. [DOI] [PubMed] [Google Scholar]
- 8. Fisher JM, Masud T, Holm EAet al. New horizons in geriatric medicine education and training: the need for pan-European education and training standards. Eur Geriatr Med 2017; 8: 467–73. [Google Scholar]
- 9. Roller-Wirnsberger R, Masud T, Vassallo Met al. European postgraduate curriculum in geriatric medicine developed using an international modified Delphi technique. Age Ageing 2019; 48: 291–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. European Union of Medical Specialists (UEMS) . Training requirements for the specialty of geriatric medicine. 2020. Available athttps://www.uems.eu/areas-of-expertise/postgraduate-training/european-standards-in-medical-training.
- 11. Parker SG, McLeod A, McCue Pet al. New horizons in comprehensive geriatric assessment. Age Ageing 2017; 46: 713–21. [DOI] [PubMed] [Google Scholar]
- 12. Stuck AE, Siu AL, Wieland GD, Rubenstein LZ, Adams J. Comprehensive geriatric assessment: a meta-analysis of controlled trials. The Lancet 1993; 342: 1032–6. [DOI] [PubMed] [Google Scholar]
- 13. NHS Digital, Hospital Episode Statistics for England . Admitted Patient Care statistics, 2019-2020. Version Oct 24, 2022. Available athttps://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 24 October 2022).
- 14. Kolb G, Breuninger K, Gronemeyer Set al. 10 Jahre geriatrische frührehabilitative Komplexbehandlung im DRG-System. Z Gerontol Geriat 2014; 47: 6–12. [DOI] [PubMed] [Google Scholar]
- 15. Statistisches Bundesamt Deutschland . Version Oct 24, 2022. Available athttps://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/_inhalt.html (accessed 24 October 2022).
- 16. Rapp K, Becker C, Todd Cet al. The association between orthogeriatric co-management and mortality following hip fracture: an observational study of 58 000 patients from 828 hospitals. Dtsch Arztebl Int 2020; 117: 53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schuetz P, Fehr R, Baechli Vet al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet 2019; 393: 2312–21. [DOI] [PubMed] [Google Scholar]
- 18. Van Grootven B, Jeuris A, Jonckers Met al. How to implement geriatric co-management in your hospital? Insights from the G-COACH feasibility study. BMC Geriatr 2022; 22: 386. 10.1186/s12877-022-03051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Partridge JS, Healey A, Modarai B, Harari D, Martin FC, Dhesi JK. Preoperative comprehensive geriatric assessment and optimisation prior to elective arterial vascular surgery: a health economic analysis. Age Ageing 2021; 50: 1770–7. [DOI] [PubMed] [Google Scholar]
- 20. Abbott RA, Rogers M, Lourida Iet al. New horizons for caring for people with dementia in hospital: the DEMENTIA CARE pointers for service change. Age Ageing 2022; 51: afac190. 10.1093/ageing/afac190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kennedy F, Galvin R, Horgan NF. Managing frailty in an Irish primary care setting: a qualitative study of perspectives of healthcare professionals and frail older patients. Journal of frailty, sarcopenia and falls 2021; 6: 1–8. 10.22540/JFSF-06-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nord M, Lyth J, Alwin J, Marcusson J. Costs and effects of comprehensive geriatric assessment in primary care for older adults with high risk for hospitalisation. BMC Geriatr 2021; 21: 263. 10.1186/s12877-021-02166-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Singh S, Gray A, Shepperd Set al. Is comprehensive geriatric assessment hospital at home a cost-effective alternative to hospital admission for older people? Age Ageing 2022; 51: afab220. 10.1093/ageing/afab220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Benthien KS, Rasmussen K, Nielsen CP, Kidholm K, Grønkjær M, Toft U. Proactive Health Support: a randomised controlled trial of telephone-based self-management support for persons at risk of hospital admission. Age Ageing 2022; 51: afac212. 10.1093/ageing/afac212. [DOI] [PubMed] [Google Scholar]
- 25. Zulfiqar AA, Hajjam A, Talha Set al. Telemedicine and geriatrics in France: inventory of experiments. Current Gerontol Geriatr Research 2018; 2018: 1–10. 10.1155/2018/9042180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kivipelto M, Mangialasche F, Snyder HMet al. World-Wide FINGERS Network: a global approach to risk reduction and prevention of dementia. Alzheimers Dement 2020; 16: 1078–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70–100 years: a contemporary primary prevention cohort. Lancet 2020; 396: 1644–52. [DOI] [PubMed] [Google Scholar]
- 28. Stuck AE, Moser A, Morf Uet al. Effect of health risk assessment and counselling on health behaviour and survival in older people: a pragmatic randomised trial. PLoS Med 2015; 12: 10, e1001889. 10.1371/journal.pmed.1001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Herghelegiu AM, Wenzel KM, Moser A, Prada GI, Nuta CR, Stuck AE. Effects of health risk assessment and counselling on fruit and vegetable intake in older people: a pragmatic randomised controlled trial. J Nutr Health Aging 2020; 24: 591–7. [DOI] [PubMed] [Google Scholar]
- 30. Bischoff-Ferrari HA, Vellas B Ret al. Effect of vitamin D supplementation, Omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: the DO-HEALTH randomized clinical trial. JAMA 2020; 324: 1855–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Banerjee S, High J, Stirling Set al. Study of mirtazapine for agitated behaviours in dementia (SYMBAD): a randomised, double-blind, placebo-controlled trial. The Lancet 2021; 398: 1487–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Logan PA, Horne JC, Gladman JRet al. Multifactorial falls prevention programme compared with usual care in UK care homes for older people: multicentre cluster randomised controlled trial with economic evaluation. BMJ 2021; 375: e066991. 10.1136/bmj-2021-066991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Philippe AS, Braunstein D, Clot-Faybesse Pet al. Impact d’une sensibilisation des médecins traitants sur la diminution des prescriptions d’antipsychotiques chez les résidents avec démence en Ehpad. Geriatr Psychol Neuropsychiatr Viel 2018; 16: 383–90. [DOI] [PubMed] [Google Scholar]
- 34. Aalto UL, Pitkälä KH, Andersen-Ranberg Ket al. COVID-19 pandemic and mortality in nursing homes across USA and Europe up to October 2021. Eur Geriatr Mec 2022; 13: 705–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cruz-Jentoft AJ, Bahat G, Bauer Jet al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lucke JA, Mooijaart SP, Heeren Pet al. Providing care for older adults in the Emergency Department: expert clinical recommendations from the European Task Force on Geriatric Emergency Medicine. Eur Geriatr Med 2022; 13: 309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Grund S, Gordon AL, Balen Ret al. European consensus on core principles and future priorities for geriatric rehabilitation: consensus statement. Eur Geriatr Med 2020; 11: 233–8. [DOI] [PubMed] [Google Scholar]
- 38. Seppala LJ, Petrovic M, Ryg Jet al. STOPPFall (screening tool of older persons prescriptions in older adults with high fall risk): a Delphi study by the EuGMS task and finish group on fall-risk-increasing drugs. Age Ageing 2021; 50: 1189–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Montero-Odasso M, Velde N, Martin FCet al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 2022; 51: afac205. 10.1093/ageing/afac205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Eglseer D, Visser M, Volkert D, Lohrmann C. Nutrition education on malnutrition in older adults in European medical schools: need for improvement? Eur Geriatr Med 2019; 10: 313–8. [DOI] [PubMed] [Google Scholar]
- 41. Gordon AL, Blundell A, Jugdeep Ket al. UK medical teaching about ageing is improving but there is still work to be done: the Second National Survey of Undergraduate Teaching in Ageing and Geriatric Medicine. Age Ageing 2014; 43: 293–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Streng PT, Masud Tet al. Geriatric medicine learning objectives and entrustable professional activities in undergraduate medical curricula: a scoping review. Age Ageing 2022; 51: 1–11. 10.1093/ageing/afac100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Masud T, Blundell A, Gordon ALet al. European undergraduate curriculum in geriatric medicine developed using an international modified Delphi technique. Age Ageing 2014; 43: 695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Copeland C, Fisher J, Teodorczuk A. Development of an international undergraduate curriculum for delirium using a modified Delphi process. Age Ageing 2018; 47: 131–7. [DOI] [PubMed] [Google Scholar]
- 45. Masud T, Ogliari G, Lunt Eet al. A scoping review of the changing landscape of geriatric medicine in undergraduate medical education: curricula, topics and teaching methods. Eur Geriatr Med 2022; 13: 513–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. OECD Population projections . Version Oct 24, 2022. Available athttps://stats.oecd.org/Index.aspx?DataSetCode=POPPROJ# (accessed 24 October 2022).
- 47. CA21122 - PROmoting GeRiAtric Medicine IN countries where it is still eMerGing (PROGRAMMING). 2022. Available at https://www.cost.eu/actions/CA21122/.


