Abstract
Objective
The COVID-19 pandemic and its socio-economic impacts have disrupted our health systems and society. We sought to examine informatics and digital health strategies that supported the primary care response to COVID-19 in Australia. Specifically, the review aims to answer: how Australian primary health care responded and adapted to COVID-19, the facilitators and inhibitors of the Primary care informatics and digital health enabled COVID-19 response and virtual models of care observed in Australia.
Methods
We conducted a rapid scoping review complying with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for scoping reviews guidelines. Two reviewers independently performed the literature search, data extraction, and synthesis of the included studies. Any disagreement in the eligibility screening, data extraction or synthesis was resolved through consensus meeting and if required. was referred to a third reviewer. Evidence was synthesised, summarised, and mapped to several themes that answer the research question s of this review.
Results
We identified 377 papers from PubMed, Scopus, Web of Science and Embase. Following title, abstract and full-text screening, 29 eligible papers were included. The majority were “perspectives” papers. The dearth of original research into digital health and COVID-19 in primary care meant limited evidence on effectiveness, access, equity, utility, safety, and quality. Data extraction and evidence synthesis identified 14 themes corresponding to 3 research questions. Telehealth was the key digital health response in primary care, together with mobile applications and national hotlines, to enable the delivery of virtual primary care and support public health. Enablers and barriers such as workforce training, digital resources, patient experience and ethical issues, and business model and management issues were identified as important in the evolution of virtual primary care.
Conclusions
COVID-19 has transformed Australian primary care with the rapid adaptation of digital technologies to complement “in-person” primary care with telehealth and virtual models of care. The pandemic has also highlighted several literacy, maturity/readiness, and micro, meso and macro-organisational challenges with adopting and adapting telehealth to support integrated person-centred health care. There is a need for more research into how telehealth and virtual models of care can improve the access, integration, safety, and quality of virtual primary care.
Abbreviations: COVID-19, Coronavirus Disease of 2019; EMRs, Electronic Medical Records; GP, General Practitioner/General Practice; MBS, Medicare Benefits Schedule; OMOP, Observational Medical Outcomes Partnership; PBS, Pharmaceutical Benefits Schedule; PCI, Primary care informatics; PRISMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews; RQ, Research question; SNOMED, Systematized Nomenclature of Medicine Clinical Terms; WHO, World Health Organisation
Keywords: COVID-19 response, Australia, Primary care response, Primary care informatics, Australian digital health, Digital health response, Digital health, COVID-19
1. Introduction
World Health Organisation (WHO) defines primary care as, “the entry point to personal health services for most health problems. An essential component of the health system, it also provides services with a family and community orientation, linking public health and personal health” [1]. On the other hand, public health is often described as, “the science and art of preventing disease, prolonging life and promoting health through the organized efforts of society” [2]. The link between individual health, public health and primary care is an important aspect that primary care informatics (PCI) and digital health can enable. PCI is the academic discipline and science focused on the special attributes and needs of primary care [3]. The WHO defines digital health as, “broad umbrella term encompassing eHealth (including mobile health), as well as emerging areas such as [the] use of advanced computing sciences in ‘big data’, genomics, and artificial intelligence” [4]. PCI science underpins digital health in the community, empowering patients, carers, citizens, health professionals and health organisations in the delivery of safe, effective, and integrated patient-centred care.
The novel coronavirus SARS-CoV-2 was declared a pandemic by the WHO in March 2020. The pandemic (COVID-19) and its socio-economic impacts have disrupted our lives, health systems and wider society, and exposed the weaknesses in Australia’s response to the pandemic. Melbourne’s COVID-19 s wave highlighted the lack of ethnicity and social history data to target interventions towards vulnerable populations [5]. Lack of mature digital health and PCI capabilities has resulted in various impediments to implementation of an effective response. Unfortunately, this has also been observed with previous pandemics such as H1N1 flu. PCI and digital health are powerful tools during pandemics. They can provide quick and effective response in the form of “telehealth”, virtual care, contact tracing, capturing timely information and connecting all stakeholders including but not limited to patients, carers, and health professionals.
The Australian healthcare system is complex, multi-tiered and follows a hybrid model. The government provides basic universal health insurance coverage through the Medicare Benefits Schedule (MBS) and the Pharmaceutical Benefits Schedule (PBS). Individuals can obtain optional private insurance for additional coverage. The Australian healthcare system has had problems in effectively responding to national health emergencies, partly due to the fragmented health information systems which are not completely interoperable, and often have differing levels of digital health maturity [6,7]. Like the rest of the world, Australia had to “fast-forward” its telehealth capabilities to support the prompt and ongoing response to COVD-19 [8]. In addition to the priorities of personal protective equipment, the need for hand hygiene, social distancing, and contact tracing apps, primary care had other barriers to overcome. In addition to technical challenges (network connectivity & user interfaces), there were clinical challenges, such as limited ability to perform physical examinations; and social challenges such as privacy and other ethical issues, participants' digital and health literacy, cost, reimbursement, and regulatory barriers [9].
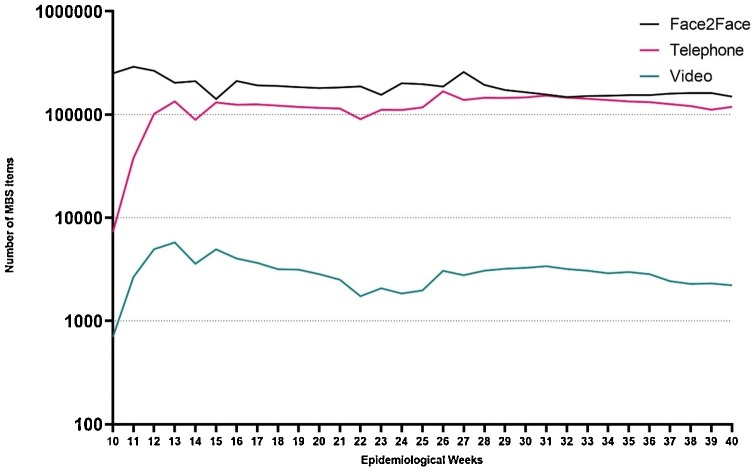
The Australian National COVID-19 Primary Care Response is an integral component of Australia’s COVID-19 response across all sectors. This primary care response allowed digital health to play a major role not only in delivery of general practice care but also in virtual training of healthcare workers and health information dissemination through national hotlines [10]. Telehealth, a key component of this primary care response, has been allocated new funding. In 2020, from the beginning of the COVID-19 pandemic, a significant increase in uptake of telehealth in primary care has been observed. Fig. 1 presents the weekly telehealth consultations performed in the first 40 weeks of the pandemic (mainly by telephone with a small proportion of video consultations) by approximately 1000 Australian GPs from New South Wales and Victoria [11]. However, the scope of PCI and digital health extend beyond primary care into public health. Consequently, the objective of this rapid scoping review is to examine the use of PCI and digital health in COVID-19 across sectors and communities in Australia, considering the variable resources available and levels of digital health maturity of the participants. We reviewed how PCI and digital health supported the Australian primary care response to the pandemic. We addressed the following specific research questions (RQ):
Fig. 1.
Weekly trends of telehealth consultations in Australian general practice. We only included in-person items where there is an equivalent MBS telehealth item. For instance, antenatal care, which has no equivalent MBS telehealth item. (Fig. 1 was generated from data reported in Pearce C et al. The GP Insights Series no 7. 26 Oct 2020 (www.polargp.org.au) [11]).
RQ1: How has Australian PCI and digital health responded and adapted to the COVID-19?
RQ2: What virtual models of care are observed in Australia during the COVID-19?
RQ3: What are the facilitators and inhibitors of the PCI and digital health enabled COVID-19 response?
2. Methods
2.1. Study design
We conducted a rapid scoping review, using the preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) guidelines [12], to answer our research questions [13]. A rapid scoping review was selected to enable a rapid synthesis of existing evidence, which is evolving very rapidly [[12], [13], [14]].
2.2. Search strategy
The literature search was performed on 4th of January 2021, by searching PubMed, Scopus, Web of Science and Embase OVID databases from 1st January to 31st December 2020. The search strategy was developed iteratively beginning with the Scopus database and subsequently adapted to the others. The final search strategy included four key word groups with a combination of Medical Subject Headings and text key words. We only included English language articles related to human participants. The complete search strategy is available in Appendix A.
2.3. Inclusion and exclusion criteria
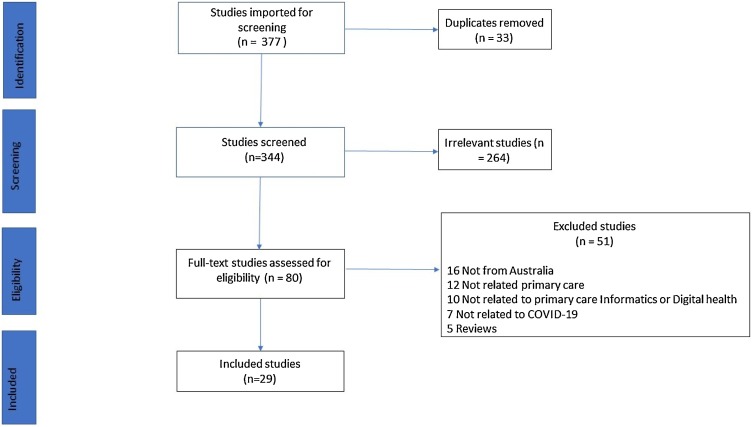
We included original research, opinions, editorials, letters, perspectives, and short communications. We only included society and professional statements about COVID-19 if they added new information. We also screened the reference lists of all eligible studies to find papers that might be eligible. For this review, we adopted the WHO’s definition of primary care [1]. We included papers that relate to general practice, family medicine, psychology, mental health, and physiotherapy. We excluded: reviews and meta-analyses; non-English papers, conference abstracts, and papers with insufficient information; where full texts were not available; and, grey literature or preprint publications. Reasons for exclusion were documented (Fig. 2 ).
Fig. 2.
PRISMA flow chart of the literature search with number of included and excluded studies.
2.4. Data extraction and quality assessment
Two reviewers (JJ, MAG) independently screened all the titles and abstracts. Disagreements in screening were sent to full-text review. Any disagreements after the full-text review were resolved by discussion with a third reviewer (STL). The data extraction template included key PCI and digital health responses and COVID-19 response characteristics.
2.5. Evidence synthesis
Extracted data was summarised, synthesised into themes which were mapped to conceptual frameworks addressing the research questions [7,15,16]. Themes described the landscape of Australian PCI and digital health response to the COVID-19. The WHO classification of Digital Health Interventions was used to map PCI and digital health tools [15]. The WHO framework on Integrated People-Centered Health Services (IPCHS) was used to describe the virtual models of primary care observed [16]. Likewise, the enablers and challenges related themes were synthesised using the Digital Health Maturity framework [7].
3. Results
We identified 377 papers from the four databases, of which 33 were duplicates. The title and abstract screening of the 344 papers identified 80 studies. Full-text screening identified 29 eligible papers (excluding 51 papers). Fig. 2 describes this process.
The data extraction and evidence synthesis phases identified various themes for each research question. Themes for RQ1 included Telehealth, national hotline, mobile applications, and health information dissemination themes. Similarly, themes for RQ2 included General Practice, Psychiatry, Physiotherapy, Pharmacy, Nursing and Cancer care themes. Themes for RQ3 included workforce training, digital resources in rural and remoted areas, patient experiences, and ethical issues. Table 1 summarises the literature and themes identified.
Table 1.
Thematic synthesis of reviewed literature.
| Study (reference) | Type | Research question | Theme identified |
|---|---|---|---|
| Andrikopoulos 2020 [17] | Perspective | RQ1, RQ2 | Telehealth, General practice, Mental health |
| Arnold 2020 [18] | Perspective | RQ3 | Ethical issues, patient experiences |
| Bell 2020 [19] | Perspective | RQ2 | Pharmacy |
| Chan 2020 [20] | Original research | RQ1, RQ2, RQ3 | Cancer care, Telehealth, ethical issues, Patient experiences |
| Desborough 2020 [10] | Perspective | RQ1, RQ3 | Telehealth, National hotline, health information dissemination, Workforce training, Mobile Applications |
| Duckett 2020 [21] | Perspective | RQ1, RQ2, RQ3 | General Practice, Telehealth, Business model & management issues, Workforce training, National Hotline |
| Fisk 2020 [22] | Original research | RQ1 | Telehealth, Mobile applications |
| Freedman 2020 [23] | Perspective | RQ2 | General practice, Telehealth |
| Halcomb 2020 [24] | Original research | RQ2 | Nursing |
| Henderson 2020 [25] | Perspective | RQ3 | Health information dissemination, Ethical issues, patient experiences, Mobile applications |
| Hull 2020 [26] | Original research | RQ1, RQ2 | Child Health, National Hotline |
| Janda 2020 [27] | Perspective | RQ1, RQ2, RQ3 | Cancer care, Telehealth, ethical issues, Patient experiences |
| Kelly 2020 [28] | Position Statement | RQ2, RQ3 | Telehealth, Nutrition |
| Kippen 2020 [29] | Original research | RQ1, RQ2, RQ3 | General Practice, Business model & management issues |
| Koczwara 2020 [30] | Perspective | RQ2, RQ3 | Cancer care, Patient Experience, Workforce Training, Telehealth |
| Liu 2020 [31] | Perspective | RQ2, RQ3 | Telehealth, patient experiences, general practice |
| Looi 2020 [32] | Perspective | RQ1, RQ2 | Telehealth, Mental health |
| Marshall 2020 [33] | Perspective | RQ1, RQ2 | Mobile applications, Mental health |
| Mazza 2020 [34] | Perspective | RQ1, RQ2 | Telehealth, General Practice |
| Nankervis 2020 [35] | Perspective | RQ1 | Information dissemination, Workforce training |
| Oh 2020 [36] | Original research | RQ1, RQ2, RQ3 | Cancer care, |
| O'Sullivan 2020 [37] | Perspective | RQ3 | Digital resources in rural and remoted areas |
| Rasalam 2020 [38] | Original research | RQ1, RQ3 | Workforce training, General practice |
| Shadmi 2020 [39] | Perspective | RQ1 | Telehealth, Ethical issues, Patient experiences, Digital resources |
| ShafieeHanjani 2020 [40] | Perspective | RQ 2, RQ3 | Telehealth, General Practice, Pharmacy, Workforce training, Digital resources in rural and remoted areas |
| Snoswell 2020 [41] | Original research | RQ1 | Telehealth |
| Stanhope 2020 [42] | Perspective | RQ2, RQ3 | Physiotherapy, Telehealth, Patient experiences |
| Thomas 2020 [43] | Perspective | RQ1, RQ3 | Telehealth, Workforce training |
| Wright 2020 [44] | Perspective | RQ1 | Telehealth, Information dissemination |
Table 2 summarises the themes synthesised, and the relevant conceptual frameworks. More details are available in Appendix B.
Table 2.
Summary of Themes by RQ.
| Research Question (RQ) | Themes | Conceptual frameworks used to deduce the themes |
|---|---|---|
| RQ1: How has primary health care responded and adapted to COVID-19 with a focus on PC informatics and digital health in Australia? |
|
These themes were derived using the WHO classification of Digital health interventions: Client communication (health information dissemination), Citizen-based reporting (mobile apps), On-demand information (national hotline) and Telemedicine (telehealth). [15] |
| RQ2: What virtual models of care are observed in Australia during the COVID-19? |
|
These virtual models of primary care operationalize the WHO framework on Integrated people-centered health services (IPCHS) by integrating care at the primary-secondary interface (e.g., between GPs and specialists), integrating health and social care (e.g. between primary care, allied health and social services) and orienting care provision around peoples’ needs (i.e., people-centered). [16] |
| RQ3: What are the facilitators and inhibitors of the Primary care informatics and digital health enabled COVID-19 response? |
|
These themes were synthesised using the Digital Health Maturity framework. [7] Superficially, ICT infrastructure, essential digital tools, information sharing and adoption components of the framework. |
The following sections present the evidence synthesised from these 29 papers.
3.1. RQ1: PCI and digital health response to COVID-19
Telehealth was the most widely reported PCI and digital health response to the COVID-19 in Australia [10,17,22,28,31,32,34,[39], [40], [41],43,44]. Before the pandemic, telehealth funding by the Government was restricted to general practice, mental health, and a few other specialities. However, by the end of 2020, telehealth funding was extended to psychiatry, psychology, primary care nurses, dentists, and some allied health services. A similar pattern of telehealth items funded was noted among the private health insurer [11,45]. This has enabled rapid uptake of telehealth by patients and health care professionals, allowing them to manage over 85 % of the patients in the community [41]. The majority of the papers included in our synthesis reported an exponential uptake of telehealth in primary care. This uptake was mainly telephone calls, with video-based telehealth services remaining almost unchanged [41,46].
Like many other countries, Australia set up a national hotline specifically for COVD-19 in February 2020 [10,21,26]. Initially, the hotline provided COVID-19 related information but later was expanded to provide more services such as triage by health professionals. However, our review did not find any evidence of utility and effectiveness of this hotline, but it was believed to be lower than expected [21]. The Australian federation and its jurisdictions both established call centres to provide advice on COVID-19 [21]. Some professional organisations also surveyed and advised citizens on COVID-19, related to their professional discipline. For example, the National Breastfeeding Helpline volunteers were surveyed regarding concerns of breastfeeding mothers during the pandemic, who identified several concerns such as insufficient supply of milk, and stressing reducing breast milk production in mothers [26].
In April 2020, the Australian government introduced COVIDSafe, a mobile application based on the Singapore government’s contact tracing app. Though promoted heavily to the public, the app did not reach the targeted downloads required for its successful implementation [25]. Subsequently, this app was replaced by QR code-based check-in applications such as ServiceNSW. The HealthDirect initiative provided an online COVID-19 symptom checker through its mobile application and website [10]. During the pandemic, patients and citizens have used mobile applications to access information and services related to mental health, raising concerns regarding regulations, efficiency, safety, and underlying guidelines [33]. Elsewhere, primary health networks and aged care facilities in Australia have leveraged existing self-care mobile applications in dealing with similar issues during COVID-19 [22].
Health information dissemination to healthcare professionals was also one of the key response areas during COVID-19 [10,25]. Previous pandemics have highlighted the role of accurate, quality, and rapid information dissemination to the health care professionals. The Australian government has conducted several webinars, targeted emails, and social media campaigns to this end, as well as for citizens, patients and carers [10]. Information dissemination on digital health interventions, such as the COVIDSafe app and sharing of electronic health records, was critical in building trust among consumers [25].
3.2. RQ2: virtual models of care
New funding arrangements (such as the Australian MBS telehealth items) to support a ‘digital-first’ response to COVID-19 led to a significant increase in ‘tele-consultations’, and a corresponding decrease in in-person consultations. These were mainly via telephone, with less than 3% using videoconferencing. This was associated with accelerated development of digital provider order entry applications, especially e-Prescribing, e-Pathology and e-imaging requests. Regulations have also been amended to allow pharmacists to supply full Australian Pharmaceutical Benefits Schedule (PBS) quantity of long-term medications in selected cases.
There were also parallel developments in child health with a focus on national planning for infant and young child feeding in emergencies [26]. Similarly, Dietitians Australia have recommended that policy makers and healthcare funders include telehealth-delivered dietetic consultations as a cost-effective alternative or complement to in-person delivery of dietetic services. Studies have shown that telehealth-delivered dietetic consultations are comparable to those delivered in-person, without requiring higher levels of additional training nor compromising quality of service provision [47].
Telepsychiatry was already available for ongoing care before COVID-19. Telepsychiatry and telepsychology may not be effective with new patients and is also not a long-term replacement for in-person consultations. Privacy and cybersecurity, especially with small practices, was a particular issue in mental health [32,33]. Patients were increasingly using mobile apps to deal with psychological trauma related to COVID-19. However, there is limited evidence on the effectiveness of these largely unregulated apps [33].
Tele-management of acute painful conditions by the GP may also be augmented by tele-physiotherapy for early management or subsequent follow-up. This is particularly important for people living in remote areas or those who are otherwise isolated [42]. Delivery of Tai Chi and Qi Gong by telehealth was feasible and resulted in increased overall patient satisfaction with cancer care services during the lockdown [36].
COVID-19 induced changes in lifestyle behaviours, including a reduction in physical activity, sleep quality, mental health, and healthy diet; and an increase in alcohol and smoking intake, producing adverse health impacts over the long term [36]. Increased access to telehealth-delivered preventive care and health promotion counselling is essential [39]. With increasing use, equity and access issues in telehealth utilisation were observed, for example, challenges for women accessing early medical abortion services through MBS telehealth services [34,39].
Closures of, and delays to cancer screening services due to COVID-19 resulted in fewer referrals for cancer prevention, screening, and diagnostic services [48]. The care of cancer survivors requires needs assessment and delivery of ongoing care through telehealth-enabled models of care, and practice management strategies. The transfer of survivorship care from secondary to primary care should also be accelerated, including the development of virtual models of shared care [20].
3.3. RQ3: facilitators and inhibitors
Several studies highlighted the importance of adequately preparing the workforce to engage in safe and appropriate usage of telehealth. The rapid uptake of telehealth highlighted gaps in staff knowledge and capacity required for using telehealth technologies [41], as well as the need for good communication among the care providers themselves [40], enabled by approaches like networking, co-location and consolidation [21]. Studies emphasized the importance of professional bodies’ guidelines to ensure best practice [10]. Other studies have demonstrated that virtual simulations of general practice clinics provided appropriate learning environments for developing key telehealth competencies [38]. Trained staff, validated apps, patient privacy protocols, relevant and usable technology suited to the local context, and good communication between healthcare professionals are required to conduct effective virtual medication reviews [39,40]. Looking forward, there is potential to transfer more types of care (e.g. cancer survivorship) to primary care using telehealth and other digital health services, freeing up hospital staff to handle the more ill patients in a timely manner. Workforce development remains key to achieve this [30].
Barriers to virtual care included limited access to affordable technology, lack of long-term policies for funding of telehealth, and safety/privacy concerns [20]. There were also concerns that Electronic Medical Records (EMRs) did not completely capture clinical thinking and patient experience, leading to the possibility of acontextual clinical management, and even the erosion of ethics in care provision [18]. Studies recognised the need for plain language explanations, ethical oversight and mandatory inclusion of experienced, informed personnel in the governance of health information [25]. In remote and rural settings, where primary care (rather than hospital care) played a greater role in COVID-19 response, the availability of digital resources were highlighted as particularly important [37], and implementers should ensure that technology is suitable for the context of use [40].
Shifting to virtual care provision inevitably resulted in changes to the patient experience. For example, the prevention, screening, referral, and diagnosis of cancer were delayed, and there were challenges to the management of lifestyle-related cancer risk factors [20,27]. Nonetheless, telehealth was noted to be of particular importance for chronic disease management, with studies highlighting the potential for tele-physiotherapy to prevent acute injuries from becoming chronic [42]. Moreover, user-centric approaches to virtual care, such as ‘co-presence-enhanced design’ have the potential to reduce patients’ anxiety and increase their confidence in managing their chronic disease condition, possibly reducing unwarranted demand for services during a time when health care resources are being stretched [31].
The viability of GP practices was compromised by the rapid increase in administrative requirements, reduced billable time, staffing adjustments, and the change management associated with pivoting to telehealth service provision; most practices experienced an increased workload and reduced income [29]. Considerable realignment of business models (networking, co-location and consolidation; new funding arrangements) was necessary to manage resources more efficiently, and coordinate different cohorts of patients to ensure safety and quality of care [21].
4. Discussion
Telehealth became the flagship of Australia’s COVID-19 response. Despite the lack of evidence for its potential benefits for access, equity, utility, safety and quality, it has become mainstream policy with generous funding [49]. However, could we have been better prepared? Could we have had better infrastructure, capacity, and evidence well ahead of time? Australian health and technology organisations have advocated for telehealth in primary care for decades. However, before COVID-19, there has been very little progress due to a lack of funding for telehealth items in general practice and primary care. Reasons for the government’s risk averse approach to funding telehealth services in general practice included provider over-servicing, fraud and individual over-utilisation [21]. However, this lack of funded telehealth activities has led to a lack of ICT infrastructure to support telehealth; a lack of research into the effective implementation of telehealth services and virtual models of care; limited understanding of the socio-technical barriers to telehealth implementation; and limited understanding of the safety and quality of telehealth.
The accelerated uptake of telehealth observed is consistent with what seen in countries with range of levels of ICT developments from well-developed (UK, USA, South Korea) to lesser developed (India, Pacific Islands) [50]. Challenges include little increase in the already very low levels of video consultations, despite a very significant increase in telephone consultations. This is primarily due to the lack of ICT infrastructure due to poor funding, but also a perceived lack of patient and provider comfort with video consultation. Further research is required into the process and impacts of video consultations, including the role of ‘co-presence’ for increasing patient confidence [51]. Another challenge is the low utilisation of telehealth among the elderly and rural populations, for similar reasons [22].
There were reported concerns about the reduced role of primary care nurses, and decreasing employment opportunities, due to increasing telehealth uptake [18,37]. Subsequently, nursing MBS service items were included in Australia. Similarly, Diabetes Educators can also access MBS telehealth items for virtual activities such as regular monitoring of lifestyle, medication use, diabetes, and mental health indicators [17,26,32,33].
EMRs are an integral component of PCI and digital health and play a crucial role, especially during and after pandemics. Healthcare workers rely heavily on EMRs when providing virtual consultations. At the same time, they are also invaluable sources of real-world data. Lack of timely access to this data for management of COVID-19 has impeded rapid implementation and evaluation of primary care response policies. Population-level data on telehealth and other PCI and digital health responses are available through sources like MBS, PBS, and other data sources [52]. However, the data formats (including standards used), governance and access processes to these sources vary significantly making it difficult to link and analyse swiftly in public health emergencies [8]. There is a need for centralised data discovery, harmonisation, access, monitoring of real-world primary care data sources which can play a key role in managing pandemics and designing effective policies to build resilience [53,54]. Primary care data sources need to consider adopting unified syntactic common data model standards such as Observational Medical Outcomes Partnership (OMOP) and semantic vocabulary standard such as Systematized Nomenclature of Medicine Clinical Terms (SNOMED).
Public health strategies, delivered through general practice and primary care are less likely to result in adverse consequences such as contacting and sharing confidential information with wrong people [55]. Partially developed contact tracing systems, such as Australia’s current hybrid method of contact tracing — manual and assisted by computer spreadsheets and generic customer relationships management solutions — are problematic in regard to accuracy, safety, and security standards for the storage of sensitive personal health information.
Inconsistent policy decisions and information dissemination in Australia were identified in the early months of COVID-19 [44]. There were inconsistencies in clinical guidelines and protocols at national, state and local levels. Eventually, these will be overcome by more effective coordination. It is important to anticipate these inconsistencies in information dissemination and have a response plan in place for effective management of pandemics.
COVID-19 is transforming health service delivery. The various virtual models of care observed in general practice, pharmacy, mental health, nursing, and physiotherapy demonstrates that virtual care will be an integral part of the Australian health system. This review has identified new ways of working with telehealth that has evolved through a process of substitution and augmentation of existing work practices. For instance, clinicians need to be equipped to recognise and respond to patients affected by mental health issues or are at risk of domestic violence [23].
In addition to health systems, patients, carers, communities, and societies also adapted to the pandemic in their own way. Patient experience is important in building resilience and strength. Their needs and concerns need to be studied and considered in adapting to new models of care. For example, “participant presence” in video consultations is believed to reduce patients’ anxiety and increase their confidence in managing their chronic disease condition, possibly reducing unwarranted demand for services during a time when health care resources are being stretched [51].
The first 9 months of COVID-19 saw a significant decline in service utilisation in primary, secondary and tertiary care [11]. For example, the decrease in cancer screening in primary care has had a downstream effect on the utilisation of pathology services and available specimens for biobanking [48]. The long-term effects of this on individual health outcomes is unclear and require further research. However, PCI-enabled services through virtual models of care provide opportunities for research and development to improve healthcare service utilisation during health emergencies in general [21,48].
The need to create a more equitable and accessible primary care system is more urgent now than ever. Like most countries globally, the portrayal of COVID-19 response in Australian media has revolved around hospital-based and public health strategies right from the beginning in March 2020. However, it is gradually moving to emphasise the importance of primary care and equitable access, especially to sustain and improve the response over the long term. For example, the sequelae of COVID-19 – a.k.a “long COVID” – needs to be monitored. Primary care played a key role in COVID-19 response especially with equitable access to care in remote and rural settings. The shift to telehealth and virtual care by primary care organisations need to be strengthened with a focus on integrated person-centred care models and a biopsychosocial approach over the long term. This shift from disease-centred to patient-centred services [16] in the virtual environment is essential for sustainable improvements in safety, quality and access to care. Primary care needs to embrace these innovations and adaptations and support to enable safe, efficient, and integrated delivery of virtual care during and beyond COVID-19. This will ultimately redefine general practice and primary care during and after COVID-19 to meet the aspirations implicit in the WHO definition of the health, public health and digital health [4].
4.1. Limitations
Whilst there is sufficient baseline evidence that these PCI responses are beneficial, this review is subjected to several limitations observed in rapid scoping reviews. These include lack of quality appraisal, risk of bias and inclusion of all study types including perspectives may weaken the evidence synthesised. Additionally, the themes synthesised as part of this review can be categorized differently. For example, contact tracing, information dissemination and national hotline can be public health responses rather than primary care response. However, it is important to note that our synthesis was based on the included studies and the interrelationship of PCI and digital with primary care and public health. For example, “Australia’s National COVID-19 Primary Care Response” included health information dissemination and the national hotline [11]. Though these PCI and digital health responses were included as part of primary care in these studies, it is important to note that they are not just for primary care. Despite these limitations, there is an urgent need to understand, monitor and evaluate PCI and digital health responses to COVID-19 from clinical and economical point of view. To date there is very limited review of evidence related to PCI and digital health in Australia. Our findings provide a baseline pandemic response related to PCI for the March 2020 to December 2020 period. Furthermore, our findings provide an opportunity to compare with other countries. Further work is needed to systematically review some of our findings such as telehealth effectiveness in improving COVID-19 outcomes. Challenges include identifying appropriate metrics and outcomes to synthesize robust evidence across heterogenous populations.
5. Conclusions
Most of the literature was in the form of perspectives, highlighting the limited evidence on effectiveness, access, equity, utility, safety, and quality of these technologies at the time of this review. Despite this lack of evidence before and during the pandemic, COVID-19 has strengthened the position of telehealth, and facilitated the development of virtual models of primary care into the future. It also highlighted the importance of more integration and information sharing between primary care and public health.
Digital technologies were adopted and adapted across the spectrum of primary care beyond conventional general practice and into the domain of public health. Enablers and barriers identified, mainly determined by the changing care delivery landscape, included workforce training, digital resources, patient experience and ethical issues, and business model and management issues. EMRs provided more agility for primary care to adapt to the pandemic but lack of standards and timely information are ongoing issues. Patient and provider experience should not be overlooked and need to be at the centre of all types of care and further research into PCI post-pandemic. The future of telehealth and virtual models of care require more robust evidence.
Authorship contributions
Category 1
Conception and design of study: Jitendra Jonnagaddala, Siaw-Teng Liaw.
Acquisition of data: Jitendra Jonnagaddala, Myron A Godinho, Siaw-Teng Liaw.
Analysis and/or interpretation of data: Jitendra Jonnagaddala, Myron A Godinho, Christopher Pearce, Siaw-Teng Liaw.
Category 2
Drafting the manuscript: Jitendra Jonnagaddala, Myron A Godinho, Siaw-Teng Liaw.
Revising the manuscript critically for important intellectual content: Jitendra Jonnagaddala, Myron A Godinho, Christopher Pearce, Siaw-Teng Liaw.
Category 3
Approval of the version of the manuscript to be published: Jitendra Jonnagaddala, Myron A Godinho, Christopher Pearce, Siaw-Teng Liaw.
Ethics approval
This review did not require ethics approval.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
We would like to acknowledge Associate Professor Christopher Pearce for providing us with the telehealth utilisation report from the POLAR dataset.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijmedinf.2021.104470.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.WHO, U . Technical Series on Primary Health Care; 2018. A Vision for Primary Health Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals. [DOI] [PubMed] [Google Scholar]
- 2.Function, G.B.C.O.I.I.T.F.D.O.T.P.H . H.M. Stationery Office; 1988. Public Health in England: The Report of the Committee of Inquiry Into the Future Development of the Public Health Function. [Google Scholar]
- 3.de Lusignan S. What is primary care informatics? J. Am. Med. Inform. Assoc. 2003;10(4):304–309. doi: 10.1197/jamia.M1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization, W.H . World Health Organization; 2019. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. [PubMed] [Google Scholar]
- 5.Mccredie J. 2020. Data Hole.https://insightplus.mja.com.au/2020/25/melbournes-covid-19-second-wave-exposes-multicultural-data-hole/ [cited 2021 4 January]; Available from: [Google Scholar]
- 6.Jonnagaddala J., et al. Adoption of enterprise architecture for healthcare in AeHIN member countries. BMJ Health Care Inform. 2020;27(1) doi: 10.1136/bmjhci-2020-100136. p. e100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liaw S.-T., et al. A digital health profile & maturity assessment toolkit: cocreation and testing in the Pacific Islands. J. Am. Med. Inform. Assoc. 2021;28(3):494–503. doi: 10.1093/jamia/ocaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webster P. Virtual health care in the era of COVID-19. The Lancet (World Report) 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maldonado J.M.S.D.V., Marques A.B., Cruz A. Telemedicine: challenges to dissemination in Brazil. Cadernos de Saúde Pública. 2016;32(Suppl 2) doi: 10.1590/0102-311X00155615. [online] [DOI] [PubMed] [Google Scholar]
- 10.Desborough J., et al. Australia’s national COVID‐19 primary care response. Med. J. Aust. 2020;213(3):104–106. doi: 10.5694/mja2.50693. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearce C., et al. The GP Insights Series. 2020. Primary care and SARS-CoV-2: the first 40 weeks of the pandemic year. [Google Scholar]
- 12.PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 13.Munn Z., et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters M.D.J., et al. Guidance for conducting systematic scoping reviews. JBI Evid. Implement. 2015;13(3) [Google Scholar]
- 15.World Health Organisation; 2018. Classification of Digital Health Interventions V 1.0. [Google Scholar]
- 16.Godinho M.A., et al. mHealth for integrated people-centred health services in the Western Pacific: a systematic review. Int. J. Med. Inform. 2020:104259. doi: 10.1016/j.ijmedinf.2020.104259. [DOI] [PubMed] [Google Scholar]
- 17.Andrikopoulos S., Johnson G. The Australian response to the COVID-19 pandemic and diabetes – lessons learned. Diabetes Res. Clin. Pract. 2020;165 doi: 10.1016/j.diabres.2020.108246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnold M., Kerridge I. Accelerating the de-personalization of medicine: the ethical toxicities of COVID-19. J. Bioethical Inq. 2020 doi: 10.1007/s11673-020-10026-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bell J.S., et al. Strategies to promote access to medications during the COVID-19 pandemic. Aus. J. Gen. Prac. 2020;49(8):530–532. doi: 10.31128/AJGP-04-20-5390. [DOI] [PubMed] [Google Scholar]
- 20.Chan A., et al. Cancer survivorship care during COVID-19—perspectives and recommendations from the MASCC survivorship study group. Support. Care Cancer. 2020;28(8):3485–3488. doi: 10.1007/s00520-020-05544-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duckett S. What should primary care look like after the COVID-19 pandemic? Aust. J. Prim. Health. 2020;26(3):207–211. doi: 10.1071/PY20095. [DOI] [PubMed] [Google Scholar]
- 22.Fisk M., Livingstone A., Pit S.W. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020;22(6) doi: 10.2196/19264. p. e19264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedman E., Bateson D. Recognising and responding to domestic violence during COVID-19: how telehealth can help. Med. Today. 2020;21(8):33–36. [Google Scholar]
- 24.Halcomb E., et al. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J. Nurs. Scholarsh. 2020;52(5):553–563. doi: 10.1111/jnu.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henderson J. Patient privacy in the Covid-19 era: data access, transparency, rights, regulation and the case for retaining the status quo. Health Inf. Manag. J. 2020;50(1–2):6–8. doi: 10.1177/1833358320966689. [DOI] [PubMed] [Google Scholar]
- 26.Hull N., Kam R.L., Gribble K.D. Providing breastfeeding support during the COVID-19 pandemic: concerns of mothers who contacted the Australian breastfeeding association. Breastfeed. Rev. 2020;28(3):25–35. [Google Scholar]
- 27.Janda M., et al. Changes in cancer preventive behaviours, screening and diagnosis during COVID-19. Psycho-Oncol. 2020 doi: 10.1002/pon.5575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly J.T., et al. Dietitians Australia position statement on telehealth. Nutr. Diet. 2020;77(4):406–415. doi: 10.1111/1747-0080.12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kippen R., et al. A national survey of COVID-19 challenges, responses and effects in Australian general practice. Aust. J. Gen. Pract. 2020;49(11):745–751. doi: 10.31128/AJGP-06-20-5465. [DOI] [PubMed] [Google Scholar]
- 30.Koczwara B. Cancer survivorship care at the time of the COVID-19 pandemic. Med. J. Aust. 2020;213(3):107–108. doi: 10.5694/mja2.50684. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu N., et al. Telehealth for noncritical patients with chronic diseases during the COVID-19 pandemic. J. Med. Internet Res. 2020;22(8) doi: 10.2196/19493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Looi J.C.L., Pring W. Private metropolitan telepsychiatry in Australia during Covid-19: current practice and future developments. Australas. Psychiatry. 2020;28(5):508–510. doi: 10.1177/1039856220930675. [DOI] [PubMed] [Google Scholar]
- 33.Marshall J.M., Dunstan D.A., Bartik W. Treating psychological trauma in the midst of COVID-19: the role of smartphone apps. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazza D., Deb S., Subasinghe A. Telehealth: an opportunity to increase access to early medical abortion for Australian women. Med. J. Aust. 2020;213(7):298–299. doi: 10.5694/mja2.50782. e1. [DOI] [PubMed] [Google Scholar]
- 35.Nankervis R., et al. COVID-19: perspectives from the experience of one australian primary health network. Asia Pacific J. Heal. Manag. 2020;15(3) [Google Scholar]
- 36.Oh B., et al. An innovative Tai Chi and qigong telehealth service in supportive Cancer care during the COVID-19 pandemic and beyond. Am. J. Lifestyle Med. 2020 doi: 10.1177/1559827620983762. p. 1559827620983762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Sullivan B., et al. Rural pandemic preparedness: the risk, resilience and response required of primary healthcare COMMENT. Risk Manag. Healthc. Policy. 2020;13:1187–1194. doi: 10.2147/RMHP.S265610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rasalam R., Bandaranaike S. Virtual WIL clinics in medicine: overcoming the COVID-19 challenge. Int. J. Work-Integrated Learn. 2020;21(5):573–585. [Google Scholar]
- 39.Shadmi E., et al. Health equity and COVID-19: global perspectives. Int. J. Equity Health. 2020;19(1) doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shafiee Hanjani L., Bell J.S., Freeman C. Undertaking medication review by telehealth. Aust J. Gen. Pract. 2020;49(12):826–831. doi: 10.31128/AJGP-06-20-5461. [DOI] [PubMed] [Google Scholar]
- 41.Snoswell C.L., et al. Telehealth uptake in general practice as a result of the coronavirus (COVID-19) pandemic. Aust. Health Rev. 2020;44(5):737–740. doi: 10.1071/AH20183. [DOI] [PubMed] [Google Scholar]
- 42.Stanhope J., Weinstein P. Learning from COVID-19 to improve access to physiotherapy. Aust. J. Prim. Health. 2020;26(4):271–272. doi: 10.1071/PY20141. [DOI] [PubMed] [Google Scholar]
- 43.Thomas E.E., et al. Building on the momentum: sustaining telehealth beyond COVID-19. J. Telemed. Telecare. 2020 doi: 10.1177/1357633X20960638. [DOI] [PubMed] [Google Scholar]
- 44.Wright M., Versteeg R., Hall J. General practice’s early response to the COVID-19 pandemic. Aust. Health Rev. 2020;44(5):733–736. doi: 10.1071/AH20157. [DOI] [PubMed] [Google Scholar]
- 45.Medicare Australia; 2020. Medicare Benefits Schedule (MBS) Online.http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home [08 Nov 2020]; Available from: [Google Scholar]
- 46.Snoswell C., et al. 2020. Telehealth and Coronavirus: Medicare Benefits Schedule (MBS) Activity in Australia.https://coh.centre.uq.edu.au/telehealth-and-coronavirus-medicare-benefits-schedule-mbs-activity-australia May 19, 2020 [cited 2020 08 Nov]; Available from: [Google Scholar]
- 47.Kelly J.T., et al. Dietitians Australia position statement on telehealth. Nutr. Diet. 2020;77(4):406–415. doi: 10.1111/1747-0080.12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Helsper C.W., et al. Cancer has not gone away: a primary care perspective to support a balanced approach for timely cancer diagnosis during COVID-19. Eur. J. Cancer Care. 2020;29(5) doi: 10.1111/ecc.13290. p. e13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grönqvist H., et al. Fifteen challenges in establishing a multidisciplinary research program on eHealth research in a university setting: a case study. J. Med. Internet Res. 2017;19(5):e173. doi: 10.2196/jmir.7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liaw S.-T., et al. Primary care informatics response to Covid-19 pandemic: adaptation, progress, and lessons from four countries with high ICT development. IMIA Yearbook Med. Inform. 2021;30(01) doi: 10.1055/s-0041-1726489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thangavelu K., et al. Designing virtual reality assisted psychotherapy for anxiety in older adults living with parkinson’s disease: integrating literature for scoping. Clin. Gerontol. 2020:1–17. doi: 10.1080/07317115.2019.1709597. [DOI] [PubMed] [Google Scholar]
- 52.The University of Queensland Centre for Online Health; 2020. Telehealth and Coronavirus: Medicare Benefits Schedule (MBS) Activity in Australia.https://coh.centre.uq.edu.au/telehealth-and-coronavirus-medicare-benefits-schedule-mbs-activity-australia [cited 2020 14 Nov]; Available from: [Google Scholar]
- 53.Wilkinson M.D., et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data. 2016;3:160018. doi: 10.1038/sdata.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liaw S.-T., et al. Quality assessment of real-world data repositories across the data life cycle: a literature review. J. Am. Med. Inform. Assoc. 2021 doi: 10.1093/jamia/ocaa340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Richardson T. 2020. SA Health Sent Bungled COVID Alerts After "pausing" Private Provider.https://indaily.com.au/news/2020/08/28/sa-health-sent-bungled-covid-alerts-after-pausing-private-provider/ Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.