Abstract
Background
Telemedicine has been a useful healthcare alternative in the fight to contain the recent Covid-19 global pandemic. Yet the extent of its application and efficacy as an alternative route for healthcare provision remains a major concern for clinicians and patients.
Objective
This study sought to identify barriers to the successful implementation of telemedicine in Sub-Saharan African (SSA) countries.
Method
A systematic review of the literature was conducted by applying the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for identifying, selecting, evaluating and interpreting findings.
Results
Our results from 66 empirical studies revealed a wide usage of telemedicine technology across SSA countries but also showed insufficient evidence of usage for fighting Covid-19 infection. Further, technological, organisational, legal and regulatory, individual, financial, and cultural aspects were identified as the major barriers to the successful implementation of telemedicine in SSA. A list of recommendations was produced for each telemedicine barrier.
Conclusion
Our review shows current trends in telemedicine application, as well as highlighting critical barriers for consideration by healthcare decision makers. This review offers a number of recommendations to support wider implementation and sustainable usage of telemedicine in SSA.
Keywords: Telemedicine, Covid-19, Sub-Saharan Africa, Healthcare readiness
1. Introduction
Sub-Saharan African (SSA) countries have witnessed some improvement in healthcare provision through the use of telemedicine [1]. It has played a significant role in increasing access, speed and quality of healthcare services through varied forms of telecommunication technologies. Previous studies have outlined significant progress in the adoption of telemedicine in healthcare practice in SSA. For example, variants of telemedicine such as teleeducation, teleconsultation, teledermatology, teleradiology, telecardiology, teleophtamology, teleoncology, and telepsychiatry [[2], [3], [4], [5], [6], [7]] have been successfully implemented in medical education and practice. Ratna et al. [8] records successful implementation of telemedicine through robotic assisted surgeries. Moreover, telemedicine has been considered as a useful alternative healthcare provision, in particular towards effort to containing (testing and treating) the recent global Covid-19 pandemic [[9], [10], [11]]. Despite the much-demonstrated importance of telemedicine, the extent of wider implementation and usage remains slow. Issues regarding the continuity of telemedicine systems are of great concern, especially since the majority of such systems were trailed on pilot projects [12].
Although previous reviews have attempted to describe telemedicine adoption in SSA, very few studies provided a comprehensive review with a focus on telemedicine adoption and barriers to successful implementation in the wake of the global Covid-19 pandemic. For example, Farag [13] identified the socio-cultural factors that could hinder the acceptance of telemedicine among patients. The study’s focus on the interaction between socio-cultural dynamics and systems offer some insights into other potential barriers. In addition, Mars [12] reviewed activities and barriers hindering successful implementation of telemedicine. However, there is a need for further review that expands insight into current issues on factors associated with the slow implementation of telemedicine. Our objectives are in two-folds: (a) describe major barriers to the successful implementation of telemedicine for Covid-19 in SSA; and (b) outline policy recommendations to tackle these barriers. We consider our review very significant, since the outcome will expose current trends in telemedicine applications in SSA as well as highlight critical barriers for consideration by healthcare decision makers.
2. Methods
This review included quantitative, qualitative, and mixed methods studies published in peer-review journals. The reviewed studies examined healthcare users’ experiences (e.g., clinicians, nurses, and patients) of using telemedicine in SSA. The systematic review protocol was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [14].
2.1. Articles search and inclusion criteria
Our search of the literature was performed using PubMed, IEEE Xplore Digital Library, Cochrane, ProQuest, Web of Science, Scopus, Global Health, ERIC, and Google Scholar. A number of research keywords were used to retrieve relevant articles for this study. For example, we used: ("challenges" OR "factors" OR "covid-19" OR "coronavirus" OR "affect" OR "impact" OR "influence" OR "utilized" OR "adopt" OR "implement") AND ("telemedicine" OR "e-health" OR "telehealth" OR "electronic health" OR "electronic health record") AND ("Africa" OR "African countries" OR “Country name"). Our search of the literature started on May 2020 and ended on September 2020.
2.2. Screening and coding of the retrieved articles
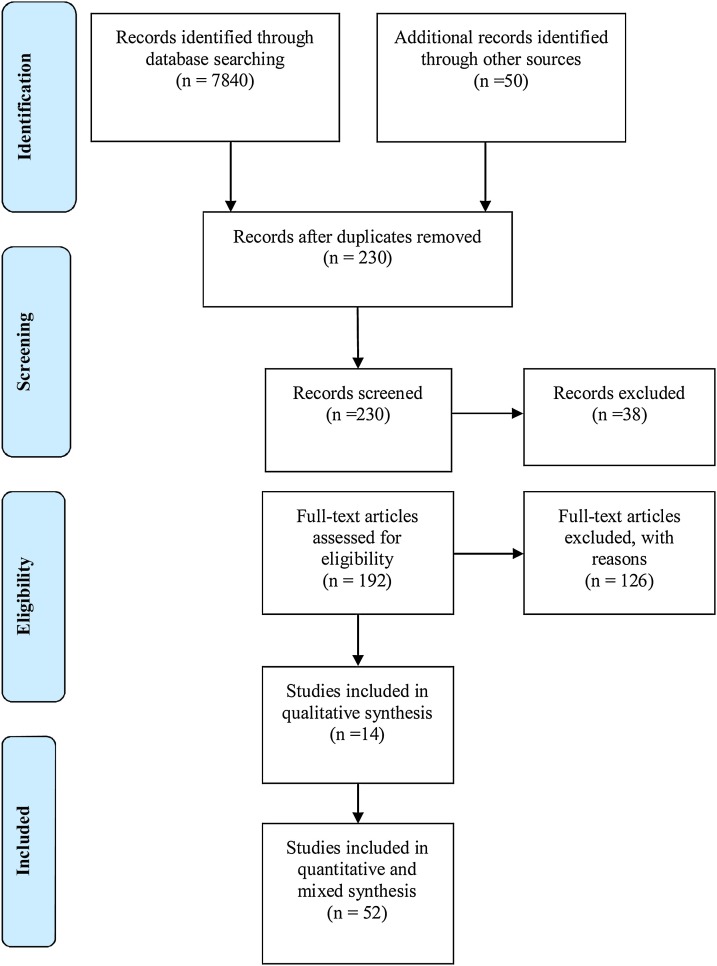
Our search of the literature resulted in 7840 studies. We screened the titles and abstracts of these studies and retained for further review. We only included articles if they met certain inclusion criteria that we developed. For example, an article was included if it was: 1) empirically based; 2) published in a scholarly journal; 3) studying barriers or challenges of telemedicine within specific SSA countries. All the included articles were scanned for duplicates, thus leaving us with 230 studies. Some articles were also excluded upon reading the titles and abstracts because they were not directly studying barriers related to telemedicine utilization within the SSA context. The full text of 192 studies was reviewed by the authors according to the same inclusion criteria. The examination of the full text of these articles led to a further exclusion of 126 articles, either because the articles covered theoretical and conceptual aspects, review-based studies, or the articles were non-peer-reviewed research reports. The finalized 66 studies were then fully reviewed to identify key challenges related to telemedicine use in SSA countries. We carefully read and evaluated these studies by all the authors. A series of meetings was held weekly to compare notes and to reach an agreement on the main challenges in the SSA region. The total number of articles that met the standard of inclusion and quality check was 66 (see Fig. 1 ). The first two authors evaluated independently the final list of articles. We used four criteria to assess the quality of publications by the experts:
-
1
Appropriateness of the research region (SSA).
-
2
Relevance of the study objectives in addressing the research questions raised in this review.
-
3
Appropriateness of the study type and relevance to the focus of the review (empirical quantitative and qualitative studies).
-
4
Reliability of the results in relation to focus of this review.
Fig. 1.
Study selection flowchart.
The interrater reliability measure was used to assess and obtain the quality of indicators. The interrater reliability was estimated using an item-by-item method and was calculated by dividing the number of agreements by the total number of agreements plus disagreements divided by 100. The average value for the interrater agreement was 86 %. The identified challenges (based on the country where the research was conducted) were placed into six categories/dimensions: organisational, technological, financial, individual, culture, and legal barriers.
3. Barriers to telemedicine adoption in SSA countries
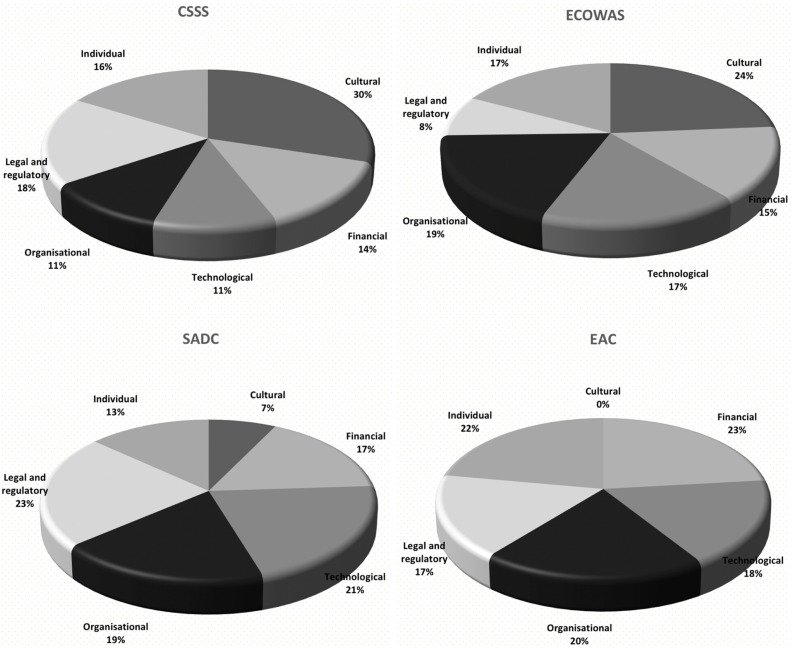
In order to simplify the discussion, we classified SSA into five-main regional blocks (based on United Nations Regional Statistics): Community of Sahel-Saharan States (CSSS); Economic Community of West African States (ECOWAS); Economic Community of Central African States (ECCAS) (there were no studies exploring barriers to telemedicine adoption in this regional block); East African Community (EAC); and Southern African Development Community (SADC) (see Table I, supplementary material). Fig. 2 shows the regional blocks, barriers and the rate of occurrence in the literatures. We present findings on barriers for each of the regional blocks under the key categories mentioned above. In the CSSS regional block, we found that the majority of research studies on barriers were concentrated in Ethiopia (92.3 %) and Djibouti (7.7 %). In the ECOWAS regional block, studies were found mostly in countries such as Mali (27.8 %), Ghana (27.8 %), Nigeria (27.8 %), Burkina Faso (11.1 %) and Togo (5.5 %). In EAC, we identified studies from Kenya (27.3 %), Rwanda (27.3 %), Tanzania (9 %) and Uganda (36.4 %). In SADC, we identified studies from Angola (13 %), Botswana (26.1 %), Mauritius (8.7 %), South Africa (43.5 %), and Zambia (8.7 %). We devote the following subsections to discussing in detail the identified barriers.
Fig. 2.
Barriers affecting telemedicine use in SSA countries.
3.1. Technological barriers
3.1.1. Community of Sahel-Saharan States (CSSS)
The literature reported that poor quality of internet connectivity (low speed and poor connectivity) and unstable electricity power supply were the main barriers for user adoption of telemedicine in Ethiopia [5,[15], [16], [17]]. Efficient and quality supply of internet and electricity are critical necessities for the successful implementation of any telemedicine service. Research suggests that these challenges were mostly prevalent in remote areas [17] that need telemedicine services the most. Such barriers are likely to affect both clinicians’ and patients’ interest in using telemedicine systems.
3.1.2. Economic Community of West African States (ECOWAS)
Technological barriers to using telemedicine in the ECOWAS countries were mostly related to the insufficient IT infrastructure in terms of the quality of system and service quality. The literature showed that the deficiency in system quality was the main challenge to the successful implementation and use of telemedicine in countries such as Mali, Burkina Faso, Ghana and Nigeria. Issues with the quality of internet (e.g., poor connectivity and low quality of bandwidth) have been reported in the literature [[18], [19], [20]]. Research suggests that poor internet connectivity can impact negatively on the quality of consultations [21], due to delay in the transmission of information from primary healthcare worker to other clinical collaborators [22]. This dimension is most likely to influence clinicians’ interest in using the system, as many consider it as counterproductive based on the fact that most of them are already burdened with additional workloads.
3.1.3. East African Community (EAC)
Technological barriers in this region were mostly related to inadequate telemedicine infrastructure, unreliable internet connectivity, and quality of service. Our review showed that in countries such as Rwanda, Uganda, Kenya barriers were mostly related to inadequate and inappropriate telemedicine infrastructure in terms of the readiness of medical equipment, tools and training [[23], [24], [25]], and software availability [26,27] in the majority of healthcare facilities. Lack of telemedicine infrastructure impedes the wide usage and full benefit of the technology.
3.1.4. Southern African Development Community (SADC)
Our review of literature showed that the lack of adequate telemedicine and ICT infrastructure in countries such as South Africa, Zambia, Mauritius, Botswana, and Angola, were the main barriers for user adoption of telemedicine [20,[28], [29], [30]]. This was due to the paucity of integrated ICT infrastructure [31] and the high cost of telecommunication equipment [32]. Such cases can considerably hinder the efficiency of teleconsultation and negatively influence work efficiency. In addition, issues related to the quality of internet connectivity (e.g., poor connectivity in rural areas, low speed and high cost of utility) were reported across all the countries as remaining challenges [[33], [34], [35]].
3.2. Organisation barriers
3.2.1. Community of Sahel-Saharan States (CSSS)
Healthcare organisations play a critical role in ensuring that any new health technology is seamlessly implemented to create an efficient value chain system. Our review demonstrated that the lack of expertise with telemedicine system, issues of balancing stakeholder interest and efficient work-structure were significant constraints to the successful implementation and adoption of telemedicine in the CSSS region. Although the literature reports the presence of telemedicine infrastructure in countries such as Ethiopia, Somaliland, and Djibouti, yet they are inadequate. The lack of clinicians with hybrid expertise in telemedicine application was a crucial barrier [3]. This was due to inadequate training and knowledge on telemedicine, which led to unstandardized application of the system [36]. These tend to generate issues of parity relative to quality of service and potentially influence successful implementation of telemedicine systems.
3.2.2. Economic Community of West African States (ECOWAS)
In the ECOWAS region, we found that the lack of adequate telemedicine infrastructure [37] was the main barrier. It emerged from the review that most medical organisations in the region were lacking healthcare professionals with hybrid expertise and use of telemedicine medical equipment [38,39]. We further identified the lack of initial-buy in from clinicians as a major barrier in countries such as Mali, Ghana, and Nigeria [4,40]. This could be attributed to the limited engagement of stakeholder and other medical institutions. Clinicians viewed the use of telemedicine as an imposition, due to no or minimal consultation by management. This often resulted in low motivation to use the system [40,41], and thus resistance to change [42]. In addition, the literature noted that the location of telemedicine set-up in the health facility did not support the workflow of clinicians. It was often viewed as counter efficient [43] which resulted in low usage of the technology.
3.2.3. East African Community (EAC)
Our review of the literature in this region showed that the majority of the challenges were mostly related to lack of healthcare professional competency, strategic planning, service quality, low buy-ins from healthcare professionals and institutions. The lack of professional competency was also highlighted as a major barrier in Uganda, Kenya [23,24,26]. This was reflected in a number of mistakes in data entry [44] and quality of service provided [45]. Also, the lack of strategic planning in the operationalisation of the telemedicine system was another challenge in countries such as Rwanda, Kenya. Our review revealed that the lack of strategic insight by management to fully anticipate future challenges and provide proactive solutions potentially contributed to issues such as implementation gaps, employee turn-over, ineffective internal communication, lack of e-readiness of healthcare professionals and commitment [25,27].
3.2.4. Southern African Development Community (SADC)
In this region, the major barriers were related to healthcare professional competence (e.g., lack of training, concerns of inaccurate medical decisions in the application of telemedicine system, and low e-awareness/readiness [28,32,[46], [47], [48]] in countries such as South Africa, Zambia, Mauritius, Botswana and Angola. These were reflected in the low-buy ins by healthcare professionals, especially by the South Africa Health Professional Council [49,50]. It is also important to note that the reluctance of the healthcare professionals to fully endorse the usage of telemedicine could be attributed to the lack of trust in the ability of users (clinicians) to properly handle medical cases and ensure quality management of patients. In addition, our review showed that duplication and fragmented implementation of telemedicine projects was a major barrier in South Africa [29,51]. These often resulted in challenges related to identifying progress and pathways to sustainability.
3.3. Legal and regulatory barriers
3.3.1. Community of Sahel-Saharan States (CSSS)
The barriers centre around the need for governmental support, policy and regulatory framework, privacy and confidentiality in the application of the telemedicine system. The literature suggests that low buy-in from government and their representing institutions was the major challenge to telemedicine use among clinicians, which lead to a low perceived support [52] by medical professionals in Ethiopia. These can be attributed to the lack of complete understanding of telemedicine and its benefits to the healthcare sector by the government and other allied institutions. In addition, we found that the majority of barriers addressed in the literature were related to the need for context-specific policy and framework to regulate the implementation and usage of telemedicine, especially in Ethiopia and Djibouti [3,53,54]. Since telemedicine is not part of the conventional healthcare practice, most existing healthcare regulations or policies do not support its implementation and operationalisation.
3.3.2. Economic Community of West African States (ECOWAS)
Legal and regulatory barriers were commonly focused on various security issues and lack of e-policy framework in countries such as Ghana and Nigeria. The review found that the majority of clinicians and patients are in doubt about how telemedicine could have a negative effect on patients privacy and confidentiality of medical data [40]. The use of internet for transmission of health information was found to pose some concerns about information security. Owing to the seeming lack of e-policy in regulating the usage of telemedicine technology, patients may show unwillingness to use it for fear of disclosing their health information. The fear was even legitimate due to the limited government commitment [38] for telemedicine adoption. In addition, the seeming lack of a concerted national policy framework to regulate the system [41] can further influence the successful adoption of telemedicine in ECOWAS.
3.3.3. East African Community (EAC)
Our review showed that issues regarding policy and security were the major barriers in countries such as Rwanda, Uganda, and Tanzania. Since telemedicine practice is very contemporary, existing healthcare policy and regulatory frameworks are not ready for this change. The lack of policy and regulations/framework to support e-system usage across healthcare sectors have been reported as barriers to user adoption of telemedicine [55]. In addition, issues regarding patients security, privacy and protection of medical data were highlighted as further challenges [23,44] to the adoption of health technology. The foregoing may create doubt for both clinicians and patients in terms of protection against potential abuse of patients and disclosure of confidential medical records.
3.3.4. Southern African Development Community (SADC)
A number of legal and regulatory concerns were found to hinder the adoption and implementation of telemedicine in countries such as South Africa, Zambia, Mauritius, Botswana and Angola. Concerns ranged from lack of ethical principles to the lack of specific e-health legislations. The literature pointed the lack of ethical and legal framework–that regulate telemedicine– as a major challenge [29,49,56]. The absence of such regulations may raise concerns about the legitimacy of health technology and successful adoption. In particular, issues about health information and data retrieval, security, privacy and patient confidentiality, and supervision [50] were found to limit the benefits of telemedicine and by implication its adoption.
3.4. Individual barriers
3.4.1. Community of Sahel-Saharan States (CSSS)
Our review identified two key individual-related barriers (perceived threat to professional control and insufficient training and skills) to telemedicine adoption in countries such as Ethiopia and Djibouti. Previous studies reports that healthcare professionals perceived telemedicine practice as a threat to their autonomy [52] and possibly may lead to lack of control over patient management [53]. This is due to the fact that telemedicine system requires that healthcare professional consult with other domain experts to arrive at a consensus on how to properly diagnose, treat and manage patient. Thus, perceived threat to autonomy can hinder the effective use of the technology.
3.4.2. Economic Community of West African States (ECOWAS)
Our review showed that individual barriers consisted of conflict of interest, resistance to change, job demand, and illiteracy rate. It was reported that clinicians in Mali perceived the telemedicine technology as a substitute to some of the advantages that the conventional healthcare practice offered (such as travelling for training and refresher courses), and possibly limit the recruitment of additional staff [39]. These aspects were obviously perceived as a disincentive to clinicians’ intrinsic motivation and may influence their resistance and usage of the system. The review also showed that some clinicians in Ghana resisted the use of telemedicine [43]. This can be attributed to the lack of buy-ins, which is common when new changes are introduced. In addition, clinicians in Nigeria viewed the use of telemedicine system as an additional workload which does not add any added incentives to motivate them [42].
3.4.3. East African Community (EAC)
Individual-related barriers were identified on two levels, namely: healthcare professionals and clients. Barriers related to healthcare professionals were mostly related to the limited IT readiness [25], especially in countries such as Rwanda, Uganda. This was due to lack of adequate knowledge and training on telemedicine system, which led to resistance to change [57]. Since, technical knowledge and skills for telemedicine is important, limited expertise may still negatively influence doctors’ and clients’ confidence and adoption of the technology. On the other hand, barriers related to the use of personal telemedicine equipment for individual usage in countries such as Rwanda and Uganda were reported.
3.4.4. Southern African Development Community (SADC)
Our review of the literature found that individual barriers were mostly related to insufficient IT knowledge and resistance to change. The limited electronic skills and insufficient knowledge to navigate the health technology were major barriers to both clinicians and patients alike [35], especially in countries such as South Africa and Angola. Capable human resource is a major asset for any effective initiative. Thus, a limitation in relation to professionals with hybrid knowledge and skills may impose an additional challenge to the success of telemedicine technology.
3.5. Financial barriers
3.5.1. Community of Sahel-Saharan States (CSSS)
Quality healthcare delivery is intricately linked with reliable financial support. In the case of Ethiopia, the literature suggests that the healthcare sector relied mostly on government for financial support. We found four key financial barriers to the success of telemedicine adoption: limited medical budget, high cost of telemedicine and ICT infrastructure, high tariffs on telecommunication and import duties, and high cost of electricity supply. It emerged from our study that budget allocated to support telemedicine implementation was often limited [58]. In addition, literature reports of high tariffs on telecommunication and import duties on ICT equipment [16].
3.5.2. Economic Community of West African States (ECOWAS)
The review showed that the primary financial barrier across all the countries in this region was linked to the cost of telemedicine and ICT infrastructure [4,59] and the cost of maintenance of the technology [43]. We noted from the literature that healthcare provision in this region, especially in Ghana and Nigeria, was dominated by the public healthcare. Due to the fact that most of health systems are generally under-resourced with limited budget and funding [41]. This ultimately hinders the capacity of public healthcare to finance the operational cost of telemedicine set-up. Our review showed that the high operational cost can contribute to increased charge of services, thus posing another challenge for telemedicine implementation. Moreover, the majority of the population who needed the telemedicine services are mostly low-income earners located in remote areas.
3.5.3. East African Community (EAC)
Our review of the literature showed that high operational cost for running telemedicine systems was a major financial barrier, especially in Rwanda and Uganda [25,45]. We also found that the high operational cost of telemedicine may contribute to the high cost of telemedicine services [24] in EAC. Murererehe et al. [44] found that high cost of telemedicine services can affect the interest of patients in Rwanda, since the majority of them are low income earners and could not afford to pay for the service charge.
3.5.4. Southern African Development Community (SADC)
The literature showed that financial barriers were mostly related to the high cost of telemedicine services and equipment. For example, in South Africa, the majority of financial issues were related to the operational cost of telemedicine systems set-up [35,46]. Also, the high-cost of telemedicine services (e.g., excessive billing) was viewed as a major barrier for patients [60,61], hence negatively affecting technology usage. Lack of funding among service providers and financial constraints [49,51] in countries such as Botswana and Angola were viewed as a major barrier to implementing telemedicine. Since most patients are financially constrained, the likelihood of expanding telemedicine services is low, hence the interest in its adoption and usage.
3.6. Cultural barriers
3.6.1. Community of Sahel-Saharan States (CSSS)
Resistance to change and language differences were the main barriers for the implementation of telemedicine. The socio-demographic and cultural dynamics in some countries like Ethiopia are very diverse. The literature suggests that the majority of the population live outside the city and do not have formal education and minimal access to ICT infrastructure, electricity and internet connectivity. This can potentially impose knowledge and awareness gap in the use of technology for healthcare by patients and healthcare workers. Our review suggests that the lack of knowledge about alternative healthcare practices can results in low buy-ins (resistance to change) by the majority of people [5,16].
3.6.2. Economic Community of West African States (ECOWAS)
In countries like Mali, Ghana, and Nigeria, we identified that the commonly reported issues were due to socio-cultural differences which led to resistance to change among clinicians, nurses, and patients. In general, the social and cultural dynamics can potentially influence patients’ decision to use telemedicine systems [40]. For example, the literature reported that in Mali the socio-cultural differences between collaborators (clinicians) and local expertise [19] was a major challenge. It resulted in some forms of resistance in terms of change from old practice to the adoption of the new system [39,41,43].
3.6.3. Southern African Development Community (SADC)
Cultural barriers were found in a study contextualised in Botswana. It related to utility of technology in healthcare and resistance to change. Our review showed that resistance to change [62] of patients and their perceptions about the sanctity of human life and relevance of technology in treating illness were the main barriers to successful adoption of the technology. These perceived threats may potentially affect the wide acceptance of telemedicine technology, in particular among patients in the rural areas.
4. Recommendations
Application of telemedicine has gained wide acceptance in Africa, in particular for managing healthcare in the Covid-19 era. Our review suggests that while telemedicine policy remains relatively same across the continent, access and usage remains varied. To maintain relevance of telemedicine in SSA, healthcare providers and government policy makers need to develop their own implementation strategies that are in tandem with individual country needs (for example, culture and governance systems). We identified some recommendations for consideration by both researchers and decision-makers (see Table II, supplementary material). These are categorised as follows: technological, organisational, legal and regulatory, financial, individual, and cultural.
-
1
Technological: This study recommends a consideration of the design of telemedicine systems. For example, in countries such as Ethiopia, Somaliland, Djibouti, Rwanda, Nigeria, and South Africa, developers of telemedicine systems may consider designing simple, user-friendly and cost-effective solutions that can support both patients and healthcare members. In view of the high operational cost of telemedicine set-up highlighted in our review, a consideration of a simple, yet effective telemedicine technology will optimise its usage. This study also recommends a careful consideration of parity in content and visual representation of the systems, in particular for those designed for personal usage. This will ensure that patients are able to understand and clearly communicate covid-19 symptoms for better patient management. Another noteworthy recommendation cited across all the studies was the need for improvement in ICT infrastructure. Provision of adequate and appropriate ICT infrastructure is critical for adoption of the health technology. For example, healthcare providers should incorporate real-time network model in addition to the store-and-forward practice, especially in remote areas. This will promote patients’ confidence in the system since they could observe and interact with both their immediate care provider and experts. In addition, it may help mitigate issues of resistance due to cultural and social values, thus enhancing the adoption of the system.
-
2
Organisational: We noted that a significant number of studies from countries such as Mali, Ghana, Nigeria, Uganda, South Africa, and Botswana have recommended the need for staff training on ICT and telemedicine technology. In addition, the lack of expertise on telemedicine practice was found to negatively influence user motivation and usage of the system. Therefore, institutionalised regular training can potentially enhance the knowledge and skills of clinicians and patients by increasing work efficiency and effective utilization of the technology. It was suggested that training on telemedicine technology should also be incorporated in the curricula of medical education, particularly for the mainstream Universities. Also, studies from countries such as Djibouti, Mali, Ghana, Uganda, Kenya, and Botswana, are advised to pay more attention to quality exchanges and collaborations to support adoption of the telemedicine technology. We found that there is a need for a sustained quality collaboration with external parties such as international partners, national ICT providers, government representing institutions, and private-public sector partnership. Enhancing such exchange relationships will not only widen the usage of the system but also increase its image and acceptance among all stakeholders. This study also recommends to the management of health institutions to adopt a more inclusive strategy prior to implementing telemedicine. Also, the review found that establishing a monitoring system to look at the use of telemedicine, in particular nurses, is critical. Healthcare providers may also consider a balance of both face-to-face and technology based medical provision. This will reduce the number of perceived threats related to the loss of human touch in healthcare provision as a result of technology integration.
-
3
Legal and regulatory: Providing a comprehensive e-policy framework that regulate the adoption and implementation of telemedicine in SSA is highly recommended. Governments and policy makers may consider establishing relevant policies, legislations and ethical standards to govern the usage of telemedicine in healthcare. This will be particularly relevant for addressing issues of security, confidentiality and privacy that slows down adoption. Providing the appropriate legal and policy environment will be useful for developing quality partnerships, balanced stakeholder interests, wider application of affordable telemedicine service, technical support and continued funding. Based on our review of the literature, we noted that government support and commitment are key for successful and sustained adoption of telemedicine. This review also recommends establishing strict protocols to monitor and evaluate telemedicine practices.
-
4
Financial: The financial barriers highlighted earlier in this study may be reduced through the development of easily adaptable systems that can meet the local needs. In addition, developers should consider value-for-money telemedicine systems. Since the primary agents of telemedicine healthcare are located mostly in the remote areas (low-income earners), ensuring value-for-money systems can increase the acceptance of patients. Lastly, we noted that most of the healthcare sectors in SSA are limited in their ability to financially support the adoption and implementation of telemedicine technology. This review recommends increasing budgetary allocation to support telemedicine implementation, as well as increasing collaborations between public and private health sectors in order to widen funding sources of telemedicine projects.
-
5
Individual: Our review highlights the need for increased awareness about the potential benefits of telemedicine technology to medical practice. This can be achieved through the implementation of systems with both medical and social values to the broader society. Health decision makers are advised to ensure a proper balance of telemedicine usage without dismissing the human touch, which is mostly valued by the society of SSA countries. In addition, increasing education and training can be also considered to improve the knowledge and skills of both clinicians and patients. It will also support the breaking of resistance to change highlighted earlier among nurses, clinicians and patients.
-
6
Cultural: The noted cultural barriers can be mitigated through an integrated and targeted training approach. A consideration of prevailing social and economic dynamics of patients, clients and other significant stakeholders. Meanwhile, providing the appropriate training can help create awareness and motivation to use the telemedicine system among clinicians and patients.
Author’s contribution
All authors conceived and designed the study. All authors conducted the search for articles considered for the study and prepared an initial draft of the manuscript, which was subsequently revised by Ahmed. All authors participated in the synthesis and analysis, read and approved the final manuscript.
Summary points
What was already known on the topic:
-
•
The use of telemedicine in SSA can offer a great approach to healthcare provision, in particular to under-resourced areas.
-
•
Various telemedicine systems were used in SSA countries to monitor and manage diseases across specific dimensions.
-
•
The use of telehealth/telemedicine technologies have been separately studied in specific SSA countries for managing healthcare information.
What this study adds:
-
•
The main challenges of utilizing telemedicine in SSA countries were outlines and discussed.
-
•
To overcome these challenges, we provided a number of recommendations to ensure an effective use of telemedicine in SSA countries.
;1;
Declaration of Competing Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Acknowledgments
This work was funded by the Researchers Supporting Project (RSP2020/157), King Saud University, Riyadh, Saudi Arabia.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijmedinf.2021.104467.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Bervell B., Al-Samarraie H. A comparative review of mobile health and electronic health utilization in sub-Saharan African countries. Soc. Sci. Med. 2019;232:1–16. doi: 10.1016/j.socscimed.2019.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Kamulegeya L.H., Bwanika J.M., Musinguzi D., Bakibinga P. Continuity of health service delivery during the COVID-19 pandemic: the role of digital health technologies in Uganda. Pan Afr. Med. J. 2020;35(43):1–3. doi: 10.11604/pamj.supp.2020.35.2.23115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kifle M., Mbarika V.W., Datta P. Telemedicine in sub-Saharan Africa: the case of teleophthalmology and eye care in Ethiopia. J. Am. Soc. Inf. Sci. Technol. 2006;57(10):1383–1393. [Google Scholar]
- 4.Mars M. Health capacity development through telemedicine in Africa. Yearb. Med. Inform. 2010;19(01):87–93. [PubMed] [Google Scholar]
- 5.Weldegebrial T.T., Berhie G. Marshall University; 2016. Telehealth in Ethiopia–The Barriers Vs. The Success Factors. no. December, 2017. [Google Scholar]
- 6.Dodoo J.E., Al-Samarraie H. Factors leading to unsafe behavior in the twenty first century workplace: a review. Manag. Rev. Q. 2019;69(4):391–414. [Google Scholar]
- 7.Dodoo J.E., Al-Samarraie H. A systematic review of factors leading to occupational injuries and fatalities. J. Public Health. 2021:1–15. [Google Scholar]
- 8.Ratna C.P., Juwaheer R., Pudaruth S. Assessing the impact of technology adoption on human touch aspects in healthcare settings in Mauritius. Stud. Bus. Econ. 2018;13(2):164–178. [Google Scholar]
- 9.Behar J.A., Liu C., Tsutsui K., Corino V.D., Singh J., Pimentel M.A., Karlen W., Warrick P., Zaunseder S., Andreotti F. 2020. Remote Health Monitoring in the Time of COVID-19. arXiv preprint arXiv:2005.08537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Samarraie H., Ghazal S., Alzahrani A.I., Moody L. Telemedicine in middle eastern countries: progress, barriers, and policy recommendations. Int. J. Med. Inform. 2020;141 doi: 10.1016/j.ijmedinf.2020.104232. [DOI] [PubMed] [Google Scholar]
- 12.Mars M. Telemedicine and advances in urban and rural healthcare delivery in Africa. Prog. Cardiovasc. Dis. 2013;56(3):326–335. doi: 10.1016/j.pcad.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Farag J. Cross cultural telemedicine: sub-saharan africa. Intersect. 2015;9(1):23–56. [Google Scholar]
- 14.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abera A.A., Mengesha G.H., Musa P.F. Assessment of Ethiopian health facilities readiness for implementation of telemedicine. Commun. Assoc. Inf. Syst. 2014;34(1):67. [Google Scholar]
- 16.Kifle M., Mbarika V.W., Bradley R.V. Global diffusion of the internet x: the diffusion of telemedicine in ethiopia: potential benefits, present challenges, and potential factors. Commun. Assoc. Inf. Syst. 2006;18(1):30–43. [Google Scholar]
- 17.Sagaro G.G., Battineru G., Amenta F. Research Square; 2019. A Review on Barriers to Sustainable Telemedicine Implementation in Ethiopia. 1021203/rs 215424/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnaert A., Ponzoni N., Sanou H., Nana N.G. Using the BELT framework to implement an mhealth pilot project for preventative screening and monitoring of pregnant women in Rural Burkina Faso, Africa. Telehealth Med. Today. 2019;2019:1–10. [Google Scholar]
- 19.Geissbuhler A., Ly O., Lovis C., L’Haire J.F. Telemedicine in Western Africa: lessons learned from a pilot project in Mali, perspectives and recommendations. American Medical Informatics Association; 2003. p. 249. [PMC free article] [PubMed] [Google Scholar]
- 20.Mars M. Telerehabilitation in South Africa–is there a way forward? Int. J. Telerehabil. 2011;3(1):11–18. doi: 10.5195/ijt.2011.6069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Annan R.K., Agyepong J.T. Pragmatic Teleconsultation network model to address the bandwidth deficiency inhibiting real-time telemedicine implementation in the Sub-Saharan Africa. Int. J. Innov. Res. Dev. 2018;7(1):203–209. [Google Scholar]
- 22.Olayiwola J.N., Udenyi E.D., Yusuf G., Magaña C., Patel R., Duck B., Sajanlal S., Potapov A., Kibuka C. Leveraging electronic consultations to address severe subspecialty care access gaps in Nigeria. J. Med. Assoc. 2020;112(1):97–102. doi: 10.1016/j.jnma.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Isabalija S.R., Mayoka K.G., Rwashana A.S., Mbarika V.W. Factors affecting adoption, implementation and sustainability of telemedicine information systems in Uganda. J. Health Inform. Dev. 2011;5(2) [Google Scholar]
- 24.Mulwa J., Kihara A. Factors influencing implementation of telemedicine in Kenya: a case of the Aga Khan University Hospital. Int. J. Hum. Resour. Procure. 2017;6(3):38–56. [Google Scholar]
- 25.Nchise A., Boateng R., Mbarika V., Saiba E., Johnson O. The challenge of taking baby steps—preliminary insights into telemedicine adoption in Rwanda. Health Policy Technol. 2012;1(4):207–213. [Google Scholar]
- 26.Kiberu V.M., Scott R.E., Mars M. Assessment of health provider readiness for telemedicine services in Uganda. Health Inf. Manag. J. 2019;48(1):33–41. doi: 10.1177/1833358317749369. [DOI] [PubMed] [Google Scholar]
- 27.Randu K.K., Nambiro A., Kilwake J. 2019. A Technological Infrastructure Assessment Framework for Telemedicine Adoption in Kenyan Level Four Hospitals.http://erepository.kibu.ac.ke/handle/123456789/1871 Retrieved July 2020 from. [Google Scholar]
- 28.Bholah L.A., Beharee K. Mauritius eHealth-trust in the healthcare revolution. 2015 ITU Kaleidoscope: Trust in the Information Society (K-2015); IEEE; 2015. pp. 1–8. December. [Google Scholar]
- 29.Fortuin J., Molefi M. Telemedicine in South Africa. Int. Telemed. eHealth. 2006;2(1):9–11. [Google Scholar]
- 30.Wamala D.S., Augustine K. A meta-analysis of telemedicine success in Africa. J. Pathol. Inform. 2013;4(6):23–53. doi: 10.4103/2153-3539.112686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coleman A., Herselman M.E., Potass D. E-health readiness assessment for e-health framework for Africa: a case study of hospitals in South Africa. International Conference on Electronic Healthcare; Springer, Berlin, Heidelberg; 2011. pp. 162–169. November. [Google Scholar]
- 32.Dinis M., Santiago F., Silva L., Ferreira R., Machado J., Castela E. Telemedicine as a tool for Europe-Africa cooperation: a practical experience. International Conference on e-Infrastructure and e-Services for Developing Countries; Springer, Berlin, Heidelberg; 2009. pp. 86–94. December. [Google Scholar]
- 33.Chavez A., Littman-Quinn R., Ndlovu K., Kovarik C.L. Using TV white space spectrum to practise telemedicine: A promising technology to enhance broadband internet connectivity within healthcare facilities in rural regions of developing countries. J. Telemed. Telecare. 2016;22(4):260–263. doi: 10.1177/1357633X15595324. [DOI] [PubMed] [Google Scholar]
- 34.Fischer M.K., Kayembe M.K., Scheer A.J., Introcaso C.E., Binder S.W., Kovarik C.L. Establishing telepathology in Africa: lessons from Botswana. J. Am. Acad. Dermatol. 2011;64(5):986–987. doi: 10.1016/j.jaad.2010.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petersen F., Brown A., Pather S., Tucker W.D. Challenges for the adoption of ICT for diabetes self‐management in South Africa. Electron. J. Inf. Syst. Dev. Countries. 2019;86(5) [Google Scholar]
- 36.Biruk K., Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: a cross-sectional study in North West Ethiopia. J. Healthc. Eng. 2018;2018 doi: 10.1155/2018/2389268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bagayokoa C., Anneb A., Fieschi M., Geissbuhlera A. Can ICTs contribute to the efficiency and provide equitable access to the health care system in Sub-Saharan Africa? The Mali experience. Yearb. Med. Inform. 2011;20(01):33–38. [PubMed] [Google Scholar]
- 38.Abodunrin O., Akande T. Knowledge and perception of e-health and telemedicine among health professionals in LAUTECH teaching hospital, Osogbo, Nigeria. Int. J. Health Res. 2009;2(1):51–58. [Google Scholar]
- 39.Bagayoko C.-O., Gagnon M.-P., Traoré D., Anne A., Traoré A.K., Geissbuhler A. E-Health, another mechanism to recruit and retain healthcare professionals in remote areas: lessons learned from EQUI-ResHuS project in Mali. BMC Med. Inform. Decis. Mak. 2014;14(1):120–132. doi: 10.1186/s12911-014-0120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kissi J., Dai B., Dogbe C.S., Banahene J., Ernest O. Predictive factors of physicians’ satisfaction with telemedicine services acceptance. Health Inf. J. 2019;26(3):1866–1880. doi: 10.1177/1460458219892162. [DOI] [PubMed] [Google Scholar]
- 41.Ajala F., Adetunji A., Akande N. Telemedicine acceptability in South Western Nigeria: its prospects and challenges. Int. J. Adv. Comput. Technol. 2015;4(9):1970–1976. [Google Scholar]
- 42.Adenuga K.I., Iahad N.A., Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int. J. Med. Inform. 2017;104:84–96. doi: 10.1016/j.ijmedinf.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 43.Nyame-Asiamah F. Improving the ‘manager-clinician’collaboration for effective healthcare ICT and telemedicine adoption processes–a cohered emergent perspective. Inf. Technol. Dev. 2020;26(3):525–550. [Google Scholar]
- 44.Murererehe J., Uwambaye P., Isyagi M., Nyandwi T., Njunwa K. Knowledge, attitude and practices of dental professionals in Rwanda towards the benefits and applications of teledentistry. Rwanda J. 2017;4(1):39–47. [Google Scholar]
- 45.Kiberu V.M., Scott R.E., Mars M. Assessing core, e-learning, clinical and technology readiness to integrate telemedicine at public health facilities in Uganda: a health facility–based survey. BMC Health Serv. Res. 2019;19(1):266. doi: 10.1186/s12913-019-4057-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gulube S., Wynchank S. Telemedicine in South Africa: success or failure? J. Telemed. Telecare. 2001;7(2_suppl):47–49. doi: 10.1258/1357633011937100. [DOI] [PubMed] [Google Scholar]
- 47.Mauco K.L. eHealth readiness of health care institutions in Botswana. J. Int. Soc. Telemed. eHealth. 2014;2:43–49. [Google Scholar]
- 48.Parham G.P., Mwanahamuntu M.H., Pfaendler K.S., Sahasrabuddhe V.V., Myung D., Mkumba G., Kapambwe S., Mwanza B., Chibwesha C., Hicks M.L. eC3—a modern telecommunications matrix for cervical cancer prevention in Zambia. J. Low. Genit. Tract Dis. 2010;14(3):1–14. doi: 10.1097/LGT.0b013e3181cd6d5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Correia J.C., Lapão L.V., Mingas R.F., Augusto H.A., Balo M.B., Maia M.R., Geissbühler A. Implementation of a telemedicine network in Angola: challenges and opportunities. J. Health Inform. Dev. 2017;12(1):1–14. [Google Scholar]
- 50.Gregory M., Tembo S. Implementation of e-health in developing countries challenges and opportunities: a case of Zambia. Sci. Technol. 2017;7(2):41–53. [Google Scholar]
- 51.Ncube B. 2019. Adoption and Adaptation of e-health Systems for Developing Nations: the Case of Botswana.https://www.diplomacy.edu/sites/default/files/IGCBP2010_2011_Ncube_0.pdf Retrieved December 2020 from. [Google Scholar]
- 52.Xue Y., Liang H., Mbarika V., Hauser R., Schwager P., Getahun M.K. Investigating the resistance to telemedicine in Ethiopia. Int. J. Med. Inform. 2015;84(8):537–547. doi: 10.1016/j.ijmedinf.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 53.Bertani A., Launay F., Candoni P., Mathieu L., Rongieras F., Chauvin F. Teleconsultation in paediatric orthopaedics in Djibouti: evaluation of response performance. Orthop. Traumatol. Surg. Res. 2012;98(7):803–807. doi: 10.1016/j.otsr.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 54.Shiferaw F., Zolfo M. The role of information communication technology (ICT) towards universal health coverage: the first steps of a telemedicine project in Ethiopia. Glob. Health Action. 2012;5(1):1–8. doi: 10.3402/gha.v5i0.15638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kajirunga A., Kalegele K. Analysis of activities and operations in the current E-Health landscape in Tanzania: focus on interoperability and collaboration. Int. J. Comput. Sci. Inf. Secur. 2015;13(6):49–54. [Google Scholar]
- 56.Chipps J., Mars M. Readiness of health-care institutions in KwaZulu-Natal to implement telepsychiatry. J. Telemed. Telecare. 2012;18(3):133–137. doi: 10.1258/jtt.2012.SFT103. [DOI] [PubMed] [Google Scholar]
- 57.Isabalija S.R., Mbarika V., Kituyi G.M. A framework for sustainable implementation of e-medicine in transitioning countries. Int. J. Telemed. Appl. 2013;2013 doi: 10.1155/2013/615617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lemma F., Atnafu+ S., Kassegne+ S.K. 2004. Survey of Current Efforts and Potentials in Application of Telemedicine in Ethiopia.http://www.digitaladdis.com/ Retrieved November 2020, from. [Google Scholar]
- 59.Frimpong K.O., Asare S., Nomah D.K., Antwi-Asante D.O. Knowledge and perception of telemedicine among health professionals at the koforidua regional hospital, Ghana. Int. J. Healthcare Sci. 2017;4(2):96–103. [Google Scholar]
- 60.Colven R., Shim M.-H.M., Brock D., Todd G. Dermatological diagnostic acumen improves with use of a simple telemedicine system for underserved areas of South Africa. Telemed. e-health. 2011;17(5):363–369. doi: 10.1089/tmj.2010.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kekana M., Noe P., Mkhize B. The practice of telemedicine and challenges to the regulatory authorities. S. Afr. J. Bioeth. Law. 2010;3(1):33–37. [Google Scholar]
- 62.Ndlovu K., Littman-Quinn R., Park E., Dikai Z., Kovarik C.L. Scaling up a mobile telemedicine solution in Botswana: keys to sustainability. Front. Public Health. 2014;2:275. doi: 10.3389/fpubh.2014.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.