Abstract
Telemental health (TMH) was an effective and relatively well-accepted way of delivering mental health care prior to the COVID-19 pandemic and has become widely adopted through the pandemic. Although recent findings show telehealth remains relatively well accepted across health care broadly, little is known about how patient experiences of TMH may have changed through the pandemic as many sectors were virtualized. These findings describe patient experiences with TMH at an outpatient mental health clinic approximately 1 year after the clinic rapidly transitioned to full TMH due to COVID-19. Respondents are 137 adult patients. Most patients reported TMH to be extremely or very effective (85.0%) and better than anticipated (76.8%). Most patients (74.6%) were interested in continuing at least some visits by TMH after the pandemic. A small subset of patients who rated their relationship with their provider as better in-person than by TMH also reported a preference for most or all visits in-person. Results provide preliminary support that TMH remains a well-accepted option for many patients. Mental health clinics may best serve patients by offering a hybrid model of care that includes both TMH and in-person services.
Keywords: telehealth, behavioral health, patient satisfaction, COVID-19
Introduction
The COVID-19 pandemic ushered in a new age for telemental health (TMH), the practice of using technology to provide mental health care at a temporal or geographic distance. TMH was demonstrated as an effective and acceptable alternative to in-person care prior to the pandemic (1–3). However, it became relatively ubiquitous during the pandemic due to the ability to provide mental health services while also following recommended pandemic precautions of minimizing in-person contact (4–6).
Research conducted prior to the pandemic has demonstrated a range of favorable outcomes for direct-to-consumer TMH including for safety, treatment adherence, patient satisfaction, provider satisfaction, and cost effectiveness (7,8). However, the pandemic may have changed the way patients and providers experience TMH. Pre-pandemic, TMH participation was typically available only through TMH research trials or rarely, in clinical settings offering a choice between TMH or in-person services. However, during the pandemic, many mental health services were virtualized and offered to patients solely by in-home TMH (9–12). Thus, patients who had been receiving in-person services, including a subset who may not have otherwise opted for TMH, were asked to abruptly switch to TMH visits. Others who may have transferred mental health treatment during the pandemic, or initiated services for the first time, were onboarded to services solely using TMH. Furthermore, little is known about how the vast increase in the use of videoconferencing and other virtual services across sectors during the pandemic (13) has impacted patient experience of TMH.
Telehealth in primary care (14) and across health care broadly (15) showed strong patient satisfaction during the pandemic and a recent survey suggests patients are open to continuing telehealth visits for general health care visits (16). However, there are unique considerations for telehealth application to mental health care in the increasingly virtualized world and they have implications for patient experience. For example, patient–provider relationships, are considered especially critical in mental health treatment (17), and are a critical element of the patient experience within mental health care. There may be differences between providers and patients in perceptions of rapport and impact of TMH on the patient/provider relationship. In addition, visit frequency is often greater in mental health care compared to many other specialties, which may make the convenience of telehealth particularly attractive for mental health visits. These factors have always been relevant to the patient experience of TMH. However, prior to the pandemic, real-world use of TMH was often based on a combination of availability and choice with providers often serving as the gatekeeper for modality of care. Because the pandemic created a much larger pool of patients who were using TMH to access mental health care, it is unknown how TMH has been experienced over time by this broader group of patients with more diverse baseline expectations of TMH.
Recent research found that TMH was well accepted by adult patients during a very early phase of the pandemic (18) and somewhat well accepted by adolescents and young adults (19). However, little is known about how adult patients have experienced TMH over a more extended period. TMH may have become more acceptable as patients are increasingly accustomed to virtual relationship formats, or conversely, less acceptable as patients experience fatigue from virtual formats and desire in-person connection (20). Patients who would not have otherwise utilized TMH but were nudged or required to use it during early phases of the pandemic may now appreciate the conveniences of the format for their regular visits. Thus, further examination of patient experiences with TMH during the COVID-19 pandemic can provide insight into how TMH s experienced by a broad group of patients in real-world clinical settings and further understanding of if/how TMH acceptability has changed through the dramatic shifts in daily life brought on by the pandemic. In this article, we describe survey results regarding patient experiences with TMH at an outpatient mental health clinic approximately 1 year after implementation of complete TMH.
Methodology
Design
Beginning in March 2020, all clinic services at an outpatient mental health clinic in an academic medical center located in the Denver, CO metro area were offered solely by TMH. TMH at this clinic consisted of synchronous, secure video conferencing in most cases and synchronous audio-only (ie, phone) communication in a few cases where technology issues prevented video conferencing. The clinic serves the full age range and specializes in mood and anxiety disorders, with psychiatric medication prescribing and psychotherapy services available. In March 2021, approximately 1 year after converting to offering only TMH, clinic patients were invited to complete an anonymous online survey regarding their experiences with TMH services during the pandemic. The survey was open for 2 weeks with a follow-up email invitation sent a week after the initial invitation. The survey was administered as a clinical quality improvement project and was deemed exempt from review by the relevant Institutional Review Board.
Participants
All patients who had a clinic visit in January or February 2021 and had an email address on file were sent an email invitation to complete the survey. In total, 596 people were sent the survey invitation which included 24 parents of child patients (aged 0-12 years), 22 parents of teenage patients (aged 13-17 years), 12 teenagers, and 536 adults. Due to the small sample size and low response rate of youth and their parents, we present results only for adult respondents.
Measures
The survey was a self-designed questionnaire that included items about demographics, patient experiences and satisfaction with TMH, relationships with providers, and future preferences for visit type (ie, TMH or in-person visits). The survey was estimated to take 5 to 6 min to complete. Patients were invited to respond to 33 items that included 21 multiple choice questions, 10 Likert scale ratings, and 2 open-ended questions with a free text response box. Two items asked patients to indicate notable positives and negatives to telehealth, by endorsing as many items as applicable for each of the listed positive and negative items. Listed items were derived from clinician input regarding frequent patient comments about TMH. Additional notable positives or negatives not listed could be indicated in a comment box. Respondents were not required to answer all questions. Analysis of questionnaire responses was primarily descriptive in nature and group comparisons were made using chi-square.
Results
Participant Characteristics
Survey responses were received from 137 of the 536 (25.6%) adult patients invited to participate1 . The sample included participants across adult age groups: 4.4% of the sample was 18–24 years (n = 6), 4.4% was 25 to 29 years (n = 6), 27.0% was 30 to 39 years (n = 37), 36.5% was 40 to –59 years (n = 50), 13.1% was 60 to 69 years (n = 18), and 14.6% was 70 years and older (n = 20). Sample gender was 71.9% female (n = 97), 27.4% male (n = 37), and 0.7% gender queer (n = 1).
Nearly all patients (n = 134; 97.8%) indicated they had received some form of mental health care prior to the start of the COVID-19 pandemic. In assessing whether patients had met their current providers in-person prior to full virtualization, 62.5% (n = 85) reported they had met at least one of their current clinic providers in person prior to COVID-19 lockdowns and 37.5% (n = 51) indicated they had met their provider(s) by TMH only. Many patients (75.2%; n = 103) reported receiving only in-person mental health services prior to the COVID-19 pandemic and 2.2% (n = 3) reported receiving no mental health services prior to the pandemic. Among those with pre-pandemic TMH experience, 10.9% (n = 15) reported occasional TMH use, 2.2% (n = 3) reported TMH about half the time and 9.5% (n = 13) reported TMH most or all of the time.
The most common TMH services received by patients during the pandemic included psychiatric medication management (76.6%; n = 105) and individual psychotherapy (62.0%; n = 85). A very small number of patients also indicated receiving couples therapy (2.9%; n = 4), family therapy (1.5%; n = 2), and group therapy (0.7%; n = 1). Patients reported they most often accessed TMH appointments by computer (68.6%; n = 94) followed by phone (21.2%; n = 29) and tablet (10.2%; n = 14).
Patient Experiences With TMH
Overall Impressions
About half of patients (50.4%; n = 68) reported they felt “very positive” or “positive” about TMH prior to using it; 35.6% (n = 48) felt “neither negative nor positive” and 14.1% (n = 19) reported they felt “negative” or “very negative”. Many patients rated their experience with TMH as “much better” (45.5%; n = 60) or “somewhat better” (31.8%; n = 42) than expected; 21.2% (n = 28) rated it “about as expected” and 1.5% (n = 2) rated it “somewhat worse” than expected. No patients rated TMH as “much worse” than expected.
Table 1 shows patient satisfaction with various aspects of virtualized clinic operations and care during the COVID-19 pandemic. Overall, patients were “Very satisfied” or “satisfied” with most aspects of care. Areas of most frequent dissatisfaction were appointment scheduling, communication with administrative staff and billing/payment issues, although dissatisfaction was less than 10% of responding patients even in those areas.
Table 1.
Patient Satisfaction With Specific Aspects of Telemental Health (TMH) During COVID-19.
| Very satisfied | Satisfied | Neither satisfied nor dissatisfied | Dissatisfied | Very dissatisfied | Not applicable | Total | |
|---|---|---|---|---|---|---|---|
| Establishing servicesa | 45 (33.6%) | 20 (14.9%) | 1 (0.8%) | 3 (2.2%) | 1 (0.8%) | 62 (47.8%) | 132 (100%) |
| Appointment scheduling | 71 (52.6%) | 51 (37.8%) | 4 (3.0%) | 4 (3.0%) | 4 (3.0%) | 1 (0.7%) | 135 (100%) |
| Getting Zoom links to appointments | 71 (52.6%) | 51 (37.8%) | 4 (3.0%) | 2 (1.5%) | 2 (1.5%) | 5 (3.7%) | 135 (100%) |
| Ease of use of videoconferencing platform | 77 (57.0%) | 44 (32.6%) | 7 (5.2%) | 2 (1.5%) | 1 (0.7%) | 4 (3.0%) | 135 (100%) |
| Providing clinical forms to your providers | 41 (30.4%) | 28 (20.7%) | 11 (8.1%) | 3 (2.2%) | 0 (0.0%) | 52 (38.5%) | 135 (100%) |
| Quality of therapy sessions | 68 (50.7%) | 37 (27.6%) | 6 (4.5%) | 1 (0.7%) | 0 (0.0%) | 22 (16.4%) | 134 (100%) |
| Quality of medication management sessions | 84 (62.2%) | 24 (17.8%) | 7 (5.2%) | 0 (0.0%) | 0 (0.0%) | 20 (14.8%) | 135 (100%) |
| Communication with administrative staff | 59 (43.7%) | 34 (25.2%) | 13 (9.6%) | 3 (2.2%) | 4 (3.0%) | 22 (16.3%) | 135 (100%) |
| Communication with your provider(s) (outside of appointments) | 71 (53.0%) | 30 (22.4%) | 7 (5.2%) | 1 (0.7%) | 0 (0.0%) | 25 (18.7%) | 134 (100%) |
| Billing/payment | 47 (35.9%) | 34 (26.0%) | 26 (19.8%) | 6 (4.6%) | 3 (2.3%) | 15 (11.5%) | 131 (100%) |
Patients who had established clinic services prior to implementation of full TMH were asked to mark not applicable.
Perceived Effectiveness
Patients perceived TMH to be effective overall. Eighty five percent of those (n = 113 of 133) who responded to the effectiveness question perceived TMH to be “extremely” (41.4%; n = 55) or “very” (43.6%; n = 58) effective; 14.3% (n = 19) perceived TMH as “somewhat” effective, 0.8% (n = 1) rated it as “not so effective” and no patients rated it as “not at all” effective.
Several exploratory chi-square analyses were performed to examine potential group differences in perceived effectiveness. Effectiveness ratings were compared among participants aged 70 and older versus those aged 18 to 69, χ2(1, n = 128) = 4.94, P = .026. Participants aged 18 to 69 were more likely to rate TMH as extremely or very effective than those aged 70 and older. In another exploratory analysis, TMH effectiveness ratings were compared among those who had previously met a clinic provider in person versus those who had met providers by TMH only, χ2(1, n = 132) = 1.67, P = .20. There was not a difference in perceived effectiveness of TMH based on whether patients had met providers in person.
Relationship With Providers
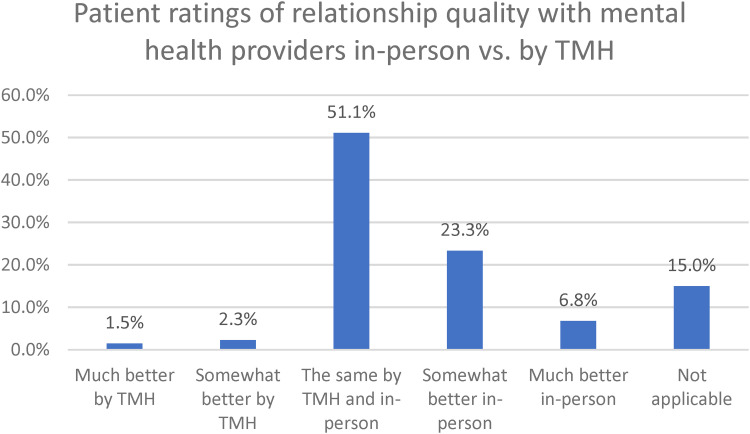
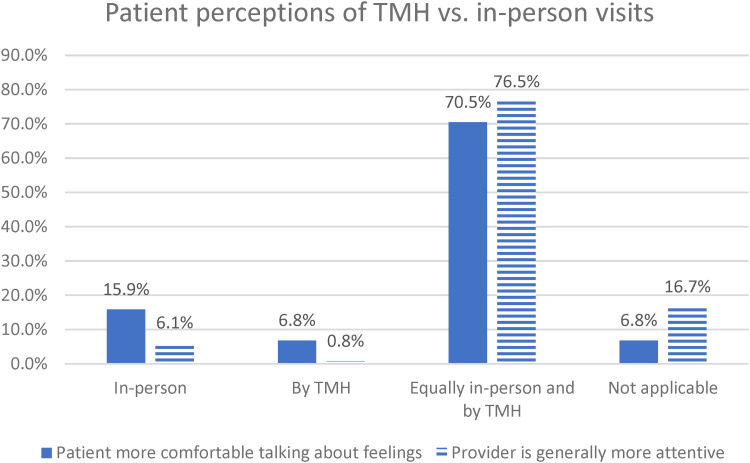
Figures 1 and 2 show responses regarding various aspects of the patient–provider relationship when comparing in-person visits prior to the pandemic with TMH visits during the pandemic. Many patients rated overall relationship quality, personal comfort talking about feelings, and provider attentiveness to be similar during in-person visits and TMH visits. Among patients who perceived a difference in relationship factors based on visit type, more people felt the relationship was better, felt more comfortable, and felt providers were more attentive in-person compared to TMH.
Figure 1.
Patient ratings of relationship quality with mental health providers in-person versus by telemental health (TMH).
Figure 2.
Patient perceptions of telemental health (TMH) versus in-person visits.
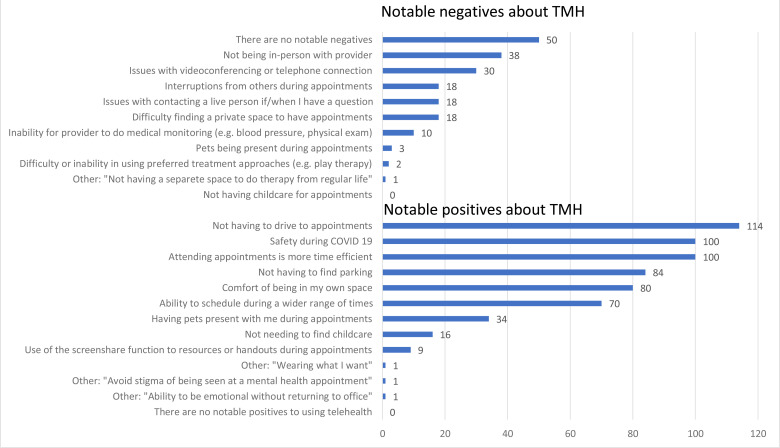
Notable Positives and Negatives
Frequency counts of patients’ notable positives and negatives about TMH are shown in Figure 3. Regarding negatives, the most common response was that there are not any notable negatives to TMH (40.3%; n = 50 of 124). The most frequently endorsed negatives included not being able to meet in person and issues with videoconferencing or connection. The most frequently endorsed positive factors included not having to drive to appointments, safety and time efficiency.
Figure 3.
Notable negative and positive factors in telemental health (TMH).
Future Preferences
Most patients expressed a preference to continue at least some TMH during an active period of the COVID-19 pandemic, especially while facial coverings are required for in-person visits. When face coverings are required during in-person visits, 55.9% (n = 71) preferred to keep all appointments by TMH, 18.1% (n = 23) preferred to continue mostly TMH visits and 15.7% (n = 20) preferred an equal mix of TMH and in-person visits. Only 10.2% (n = 13) preferred to have most or all visits in-person while facial coverings are required. More than half of patients (58.4%; n = 73) indicated receiving a vaccine would not impact their preference for TMH versus in-person visits. When asking patients to predict their preferences in a scenario where COVID-19 concerns may be a less significant factor in decision making (eg, community case counts are low and many people have been vaccinated), 74.6% (n = 94) indicated they would still prefer to keep at least half of their visits by TMH. An exception to this general finding was among the 6.8% (n = 9) who indicated that the relationship with their provider was much better in-person compared to TMH. In that case most (77.8%; n = 7) preferred all or most visits in-person when COVID-19 is less of a factor in decision making.
Discussion
TMH was viewed favorably by adult patients in this outpatient mental health specialty clinic. Patients were satisfied or very satisfied with most aspects of their mental health care, many patients found TMH services effective or very effective and many patients reported no notable negatives to TMH. One exception was exploratory analyses showing TMH was perceived as less effective by those aged 70 and older compared to younger patients. This finding is consistent with a recent large-scale study showing lower use of TMH among older patients (21) and warrants further study to understand the reasons for this difference in preference as it may suggest subgroups that will have better experience using TMH. Of note, most of the sample reported they had experienced in-person mental health visits prior to the pandemic. Thus, current findings support the notion that TMH was well received by patients who may not have utilized it if pandemic safety precautions had not required it. Indeed, many patients reported TMH services to be better than initially expected and rated qualities about the patient-provider relationship to be similar for in-person and TMH visits. It is often suspected by clinicians that patients may find TMH more acceptable if they have met a provider in-person previously. However, current findings did not find a difference in perceived effectiveness when comparing patients who had previously met a provider in person with those who had not.
Due to the particular importance of discerning nonverbals in mental health care, particularly in psychotherapy, it is not surprising that most patients indicated a preference to continue TMH while facial coverings are required for in-person appointments. Clinic providers have anecdotally reported that ability to conduct appointments without facial coverings by TMH has been a determining factor for both themselves and patients in continuing TMH appointments.
“Not having to drive to appointments” was the most frequently endorsed positive aspect of TMH. “Safety from the pandemic” and “time efficiency” were tied for the second most frequently endorsed positives. This indicates that patients experience a range of positive benefits to TMH care beyond factors specifically related to COVID-19. Indeed, when asking patients to consider their preferences if/when COVID-19 is less of a factor in their decision making, many patients indicated a preference for at least half of their appointments to be by TMH. An exception included the small subset of patients who perceived their relationship with their provider to be much better in-person; Not surprisingly, those patients indicated preference for mostly or all in-person visits when COVID-19 is less of a consideration in decision making. However, they comprised only a small proportion of the total sample. Current findings are consistent with research showing good patient acceptability of TMH early in the pandemic (13) as well as pre-pandemic data showing high patient satisfaction of TMH (1,2) and offer indications that patient interest in TMH has not waned due to videoconferencing fatigue.
The current results were obtained as part of a clinical quality program evaluation and thus are not generalizable. There are also limitations. Sample size and response rates from youth and their parents were so small they are not reported here. Thus, it is unknown if there are differences in TMH experience between youth and adults at the clinic. In addition, clinical outcome measures were not included and are obviously important to consider alongside experience metrics. Lastly, the sampling method invited patients who had a clinic visit in January or February 2021, more than 9 months after the clinic transitioned to full TMH. Thus, patients who may have disengaged in services or never initiated them due to dissatisfaction with TMH were not included, and this could have inflated positive impressions of TMH. Although providers at the clinic have generally reported that patient termination of services due to TMH has occurred at very low rates, this limitation should be considered.
These findings support the popular notion that TMH is maintaining lasting popularity and will likely do so well past the pandemic. Indeed, fast forwarding to more than 12 months after these data were collected, many places in the United States are normalizing operations. Although patients at the clinic where these data were collected are routinely offered a choice between TMH and in-person visits, many continue to opt for TMH visits. Anecdotally, clinicians have noted that many of the patients who were initially skeptical of TMH at the start of the pandemic may now actually prefer it. Research into why those people who initially resisted TMH now prefer it may be particularly enlightening in terms of ways to improve overall patient experience. For example, the most frequently noted positives to TMH were related to convenience and thus examination of diverse and innovative ways to make mental health care more convenient for patients has great potential to improve patient experience.
Given that TMH is likely here to stay, further research regarding TMH acceptability in specific patient populations (eg, rural, low socioeconomic status, and children) and with specific treatment modalities (eg, play therapy and couples therapy) will inform how to best apply and leverage TMH. Of note, recent findings regarding use of TMH with refugee populations during the pandemic (22) suggest that certain traditionally underserved groups continue to face structural barriers to using TMH (eg, lack of access to private space or internet). Thus, it will be important to maintain vigilance to these considerations to prevent perpetuating or even exacerbating health system inequities when using TMH.
In addition, prior to the pandemic providers were often the gatekeepers of care delivery modality. Decision making about modality now appears to be shifting more to patients due to the wide availability of TMH services. The current findings suggest that patients perceive hybrid care that includes TMH in combination with in-person visits, as a desirable, effective, and convenient solution moving forward. Further understanding how to optimize patient experience with hybrid services is an important next step. Ultimately, these and future findings can inform best practices for hybrid care and support thoughtful application that optimizes patient experience through this transformation in mental health treatment.
A portion of the reported data includes lower totals due to patients not completing all items.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This project was deemed exempt from review by the Institutional Review Board of the University of Colorado Anschutz Medical Campus.
ORCID iD: Dana Steidtmann https://orcid.org/0000-0003-3964-4439
References
- 1.Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The empirical evidence for telemedicine interventions in mental disorders. Telemed E-Health. 2016;22(2):87–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The Effectiveness of Telemental Health: A 2013 Review. Telemed J e-Health. 2013;19(6):444–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly BT. et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1595–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu D, Paige SR, Slone H, et al. Exploring telemental health practice before, during, and after the COVID-19 pandemic. J Telemed Telecare. 2021;0:1357633X211025943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zangani C, Ostinelli EG, Smith KA, et al. Impact of the COVID-19 pandemic on the global delivery of mental health services and telemental health: systematic review. JMIR Ment Health. 2022;9(8):e38600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fletcher TL, Hogan JB, Keegan F, et al. Recent advances in delivering mental health treatment via video to home. Curr Psychiatry Rep. 2018;20(8):56. [DOI] [PubMed] [Google Scholar]
- 8.Luxton DD, Sirotin AP, Mishkind MC. Safety of telemental healthcare delivered to clinically unsupervised settings: a systematic review. Telemed J E-Health. 2010;16(6):705–11. [DOI] [PubMed] [Google Scholar]
- 9.Kalin ML, Garlow SJ, Thertus K, Peterson MJ. Rapid implementation of telehealth in hospital psychiatry in response to COVID-19. Am J Psychiatry. 2020;177(7):636–7. https://ajp.psychiatryonline.org/doi/abs/10.1176/appi.ajp.2020.20040372 [DOI] [PubMed] [Google Scholar]
- 10.Steidtmann D, McBride S, Mishkind MC. Experiences of mental health clinicians and staff in rapidly converting to full-time telemental health and work from home during the COVID-19 pandemic. Telemed E-Health. 2021;27(7):785–91. [DOI] [PubMed] [Google Scholar]
- 11.Warren J, Smalley K. Using Telehealth to Meet Mental Health Needs During the COVID-19 Crisis. 2020 Retrieved from: https://www.commonwealthfund.org/blog/2020/using-telehealth-meet-mental-health-needs-during-covid-19-crisis
- 12.Kola L. Global mental health and COVID-19. Lancet Psychiatry. 2020; 7(8):655–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans B. The Zoom Revolution: 10 Eye-Popping Stats from Tech’s New Superstar [Internet]. 2020 [cited October 26, 2021]. Retrieved from: https://cloudwars.co/covid-19/zoom-quarter-10-eye-popping-stats-from-techs-new-superstar/
- 14.Hays RD, Skootsky SA. Patient experience with in-person and telehealth visits before and during the COVID-19 pandemic at a large integrated health system in the United States. J Gen Intern Med. 2022;37(4):847–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nanda M, Sharma M. A review of patient satisfaction and experience with telemedicine: a virtual solution during and beyond COVID-19 pandemic. Telemed J E-Health Off J Am Telemed Assoc. 2021;27(12):1325–31. https://pubmed.ncbi.nlm.nih.gov/33719577/ [DOI] [PubMed] [Google Scholar]
- 16.Predmore Z, Roth E, Breslau J, Fischer S, Uscher-Pines L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open. 2021;4(12):e2136405. https://pubmed.ncbi.nlm.nih.gov/34851400/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crits-Christoph P, Gibbons MBC, Hamilton J, Ring-Kurtz S, Gallop R. The dependability of alliance assessments: the alliance–outcome correlation is larger than you might think. J Consult Clin Psychol. 2011;79(3):267–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tse J, LaStella D, Chow E, et al. Telehealth acceptability and feasibility among people served in a community behavioral health system during the COVID-19 pandemic. Psychiatr Serv. 2021;72(6):654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wood S, Pickel J, Phillips A, et al. Acceptability, feasibility, and quality of telehealth for adolescent health care delivery during the COVID-19 pandemic: cross-sectional study of patient and family experiences. JMIR Pediatr Parent. 2021; 4(4):e32708. https://pubmed.ncbi.nlm.nih.gov/34779782/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiederhold BK. Connecting through technology during the coronavirus disease 2019 pandemic: avoiding “zoom fatigue.”. Cyberpsychology Behav Soc Netw. 2020;23(7):437–38. [DOI] [PubMed] [Google Scholar]
- 21.Connolly SL, Stolzmann KL, Heyworth L, et al. Patient and provider predictors of telemental health use prior to and during the COVID-19 pandemic within the department of veterans affairs. Am Psychol. 2022;77:249–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weith J, Fondacaro K, Khin PP. Practitioners’ perspectives on barriers and benefits of telemental health services: the unique impact of COVID-19 on resettled U.S. Refugees and asylees. Community Ment Health J. 2022:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]