Abstract
Introduction
The authors sought to evaluate cost differences between shoulder arthroplasties and lower-extremity joint replacements in the outpatient and inpatient setting within a large health-maintenance organization.
Methods
A cross-sectional study of 100 total hip arthroplasties (THA), 100 total knee arthroplasties (TKA), and 100 shoulder arthroplasties (50 anatomical total shoulder arthroplasties and 50 reverse shoulder arthroplasties [RTSA]) was performed at a single regional health care center within an integrated health care maintenance organization. A time-driven activity-based costing methodology was used to obtain total cost of each episode for outpatient (vs) inpatient surgery. Results are presented by procedure type.
Results
Compared to their respective inpatient procedure, outpatient surgery was less expensive by 20% for RTSA, 22% for total shoulder arthroplasties, 29% for THA, and 30% for TKA. The cost of implants was the highest proportion of cost for all joint procedures across inpatient and outpatient settings, ranging from 28% of the total cost for inpatient THA to 63% of the cost for outpatient RTSA.
Discussion
Although many factors influence the total cost for arthroplasty surgery, including rate of hospitalization, duration of stay, operative time, complexity of cases, patient factors, equipment, and resource utilization, the implant cost remains the most expensive factor, with hospital bed admission status being the second costliest contribution.
Conclusion
Outpatient total arthroplasty substantially reduced procedure expenses in a managed-care setting by 20%–30%, although savings for outpatient shoulder arthroplasty was lower than savings for THA or TKA. Implant costs remain the largest portion of shoulder arthroplasty procedure expenses.
Introduction
Value-based health care is increasingly important in the era of cost containment. A driving force behind recent trends toward outpatient surgery is a new focus on rising health care costs in the United States. Orthopedic surgery has seen a dramatic trend toward outpatient surgery from the inpatient setting in an effort to provide better value.
Total hip and knee joint arthroplasty have successfully made the transition to outpatient surgery, with several studies showing sustained quality when compared to inpatient surgery. 1,2 Studies have also reported cost savings in outpatient total hip and knee arthroplasty when compared to inpatient surgery. 3–5 With improvements in surgical techniques, implants, and pain-control modalities, outpatient shoulder arthroplasty has gained momentum. Implants have trended to smaller and less invasive designs on the humeral side, and expansion of regional anesthesia and multimodal pain control have reduced the need for inpatient hospitalization.
The value of outpatient shoulder arthroplasty remains to be proven. Quality of outpatient shoulder arthroplasty is similar to inpatient episodes across many outcome measures, including adverse events, complications, emergency room (ER) visits, readmissions, reoperations, and mortality. 6–14 Prior studies have found outcomes following outpatient shoulder arthroplasty match the outcomes of inpatient episodes. 15 Cost studies comparing this transition from inpatient to outpatient arthroplasty are few and limited to national database or retrospective studies with little granularity. 8,16,17 In fact, a recent systematic review argued that cost analysis through a comparative time-driven activity-based costing (TdABC) study is needed. 18
The purpose of this study was to evaluate cost differences between hip, knee, and shoulder arthroplasty in the outpatient and inpatient setting within a large health-maintenance organization. Factors driving the cost of arthroplasty surgery and the most expensive proportions of cost in an arthroplasty episode were determined. Our hypothesis was that although outpatient arthroplasty leads to notable cost savings, implant costs remained the leading financial burden to the care episode.
Methods
A cross-sectional study of primary elective joint arthroplasties performed at a single regional health care center in California within an integrated health care maintenance organization was conducted. All consecutive elective arthroplasty procedures were identified until 100 total hip arthroplasties (THA), 100 total knee arthroplasties (TKA), and 100 shoulder arthroplasties (including 50 anatomical total shoulder arthroplasties [TSR] and 50 reverse shoulder arthroplasties [RTSA]) were performed for a total sample size of 300 joint arthroplasty procedures (September 1, 2019 through June 30, 2021).
The health care organization’s integrated electronic health record was the primary data source. Patient characteristics at the time of the procedure included age (in years), body mass index (in kg/m2), and the American Society of Anesthesiologist’s (ASA) classification (≥ 3 vs < 3). Information on inhospital length of stay (LOS, in days), 30 day readmission, and 30 day ER visit was also obtained.
Outpatient (vs) inpatient stay was the exposure of interest. Outpatient THA and TKA were performed in a hospital operating room (OR) setting, and patients were recovered in the hospital postanesthesia care unit (PACU). Outpatient TSR and RTSA were performed in an outpatient surgery center and recovered in the outpatient PACU.
Total cost of the episode was determined for procedures included. For each procedure, the EHR was manually reviewed by clinical coauthors for exact time spent in the OR (in minutes), recovery room (RR, in minutes), and inpatient floor to allow for precise calculations of cost per resource per unit time. As many aspects of care were included for cost calculation as possible (Table 1). Resources included circulating registered nurse (RN), scrub technician, anesthesia personnel, OR cost, and RR RN. Other standard costs also included preoperative workup, supplies, regional anesthesia, assistants, imaging, implants, inpatient bed, pharmaceutical, physical therapy, and home health care costs. Costs of standard supplies, medications, and services were obtained through the organization’s internal system. Payroll expenses were obtained for certain cost factors (e.g., anesthesia block, fluoroscopy technician). The cost of time-based personnel was calculated based on the average hourly salary of the position multiplied by the time the patient spent in the OR or RR. OR cost was an average cost per procedure type based on estimates within the organization from 2019, increased 3% for inflation. Inpatient bed cost was calculated by subtracting all other factors from the internal diagnostic-related group for each type of case.
Table 1:
Components of costs considered in analysis
| Component | Item |
|---|---|
| Bed unit | Inpatient bed |
| Implant | Implant supplies |
| Medication | Bupivacaine |
| Cefazolin (Ancef) antibiotics | |
| Tranexamic acid | |
| Other supplies | Ice machine |
| Payroll—operating room | Certified RN anesthetist/medical doctor anesthesiologist |
| Fluoroscopy technician | |
| Physician assistant | |
| Operating room RN | |
| Operating room turnover cleaning | |
| Orthopedic surgeon | |
| Orthopedic technician | |
| Scrub technician | |
| Payroll—postoperative | Home health physical therapy |
| Home health RN | |
| Inpatient physical therapy | |
| Lab technician/tests | |
| Medical doctor anesthesiologist block | |
| Physician rounding | |
| Postanesthesia care unit RN | |
| Recovery x-rays | |
| Transport to car | |
| Transport to hospital floor |
Statistical analysis
Frequencies, proportions, means, standard deviations (SD), medians, and ranges were used to describe the sample. A TdABC methodology for cost analysis was performed for each procedure type to obtain the total cost of each episode. 19 Proportion of each cost component of the total cost was calculated, as was the percent difference between outpatient and inpatient surgery and procedure type. Results are stratified procedure type.
Results
Of the 100 THA and 100 TKA, 73% and 67% were outpatient procedures, respectively. Fifty percent of the 50 TSR and 40% of the 50 RTSA were included were outpatient procedures. Table 2 presents characteristics of patients included in the study sample by outpatient/inpatient status and procedure type. Mean OR time following THA and TKA ranged from 141.2 to 150 minutes. Although consistent across TSR and RTSA, OR time was longer than THA and TKA, ranging from 161.3 to 168.3 minutes. Mean RR time for outpatient and inpatient procedures was similar for THA (280.4 and 272.2 minutes) and TKA (253.3 and 246.7 minutes). However, RR time was shorter for inpatient RTSA (191.3 minutes) and TSR (196.2 minutes) than it was for outpatient RTSA (219.6 minutes) and TSR (219.3 minutes). Readmissions and ER visits within 30 days were infrequent across procedures (Table 2).
Table 2:
Characteristics of 300 joint arthroplasty procedures performed at a regional health care center
| Characteristic | Procedure | |||||||
|---|---|---|---|---|---|---|---|---|
| THA | TKA | TSR | RTSA | |||||
| Outpatient | Inpatient | Outpatient | Inpatient | Outpatient | Inpatient | Outpatient | Inpatient | |
| N | 73 | 27 | 67 | 33 | 25 | 25 | 20 | 30 |
| Age in years, mean (SD) | 66.1 (9.1) | 70.3 (9.0) | 67.7 (8.7) | 71.9 (8.9) | 67.6 (10.5) | 62.1 (15.4) | 73.0 (5.8) | 74.2 (8.3) |
| BMI, in kg/m2, mean (SD) | 28.7 (4.3) | 28.5 (4.8) | 29.9 (42) | 30.5 (5.4) | 29.8 (6.6) | 30.9 (5.2) | 30.1 (6.4) | 29.2 (5.5) |
| ASA ≥ 3, n (%) | 12 (16.4) | 11 (40.7) | 16(23.9) | 14 (42.4) | 11 (44.0) | 8 (33.3) | 9 (45.0) | 14 (46.7) |
| OR time, in minutes, mean | 144.8 | 150 | 141.2 | 143.6 | 162.8 | 168.3 | 163.7 | 161.3 |
| RR time, in minutes, mean | 280.4 | 272.2 | 253.3 | 246.7 | 219.6 | 191.3 | 219.3 | 196.2 |
| LOS, in days, mean (range) | 0 | 1.3 (1–2) | 0 | 1.5 (1–6) | 0 | 1.0 (1–2) | 0 | 1.2 (1-4) |
| Readmission/ER visit | 0 | 2 (0/2) | 0 | 4 (2/2) | 4 (1/3) | 0 | 2 (1/1) | 4 (0/4) |
ASA, American Society of Anesthesiologists; BMI, body mass index; ER, emergency room; LOS, length of stay; OR, operating room; RR, recovery room; RTSA, reverse total shoulder arthroplasty; SD, standard deviation; THA, total hip arthroplasty; TKA, total knee arthroplasty; TSR, total shoulder arthroplasty.
Compared to their respective inpatient procedure, outpatient surgery was 20% less expensive for RTSA, 22% less expensive for TSR, 29% less expensive for THA, and 30% less expensive for TKA (Table 3). RTSA carried the largest overall procedure cost for both inpatient and outpatient surgery, and inpatient RTSA was the most expensive procedure (Figure 1). Relative to this, THA was the least expensive outpatient (−52%) and inpatient (−27%) arthroplasty procedure.
Table 3:
Percent difference for outpatient (vs) inpatient joint arthroplasty
| Procedure | Difference |
|---|---|
| THA | 29% |
| TKA | 30% |
| TSR | 20% |
| RTSA | 22% |
RTSA, reverse total shoulder arthroplasty; THA, total hip arthroplasty; TKA, total knee arthroplasty; TSR, total shoulder arthroplasty.
Figure 1:
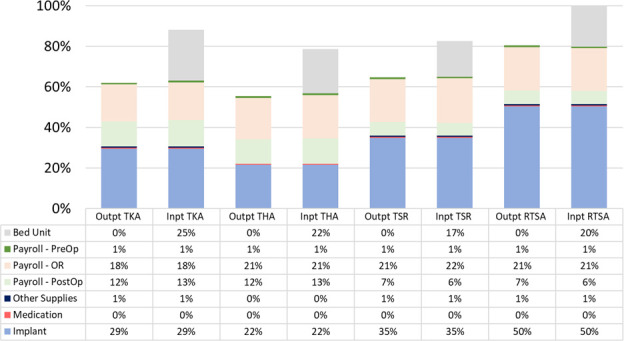
Proportion of outpatient and inpatient procedure costs relative to the most expensive procedure: inpatient RTSA. Inpt = inpatient; OR = operating room; Outpt = outpatient; PostOp = postoperative; PreOp = preoperative; RTSA = reverse total shoulder arthroplasty; THA = total hip arthroplasty; TKA = total knee arthroplasty; TSR = total shoulder arthroplasty.
The cost of implants was the highest proportion of cost for all joint procedures across both inpatient and outpatient settings. Implants made up 63% of the cost for outpatient RTSA and 54% of the costs for outpatient TSR. Hospitalization costs made up of 20% of the costs for inpatient RTSA and 21% overall costs for inpatient TSR (Figure 2).
Figure 2:
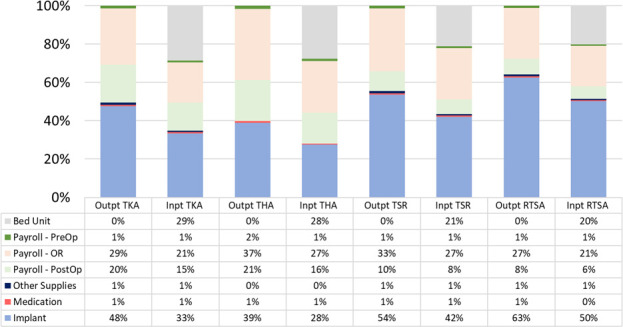
Proportion of cost for each component of the episode of care according to outpatient and inpatient surgery, by procedure type. Inpt = inpatient; OR = operating room; Outpt = outpatient; PostOp = postoperative; PreOp = preoperative; RTSA = reverse total shoulder arthroplasty; THA = total hip arthroplasty; TKA = total knee arthroplasty; TSR = total shoulder arthroplasty.
Discussion
When considering the cost for an episode of care according to outpatient and inpatient shoulder arthroplasty of care within a regional health-maintenance organization, a cost savings of 20% for outpatient RTSA and 22% for TSR relative to inpatient episodes was found. Outpatient to inpatient THA and TKA had slightly higher cost savings at 29% and 30%, respectively. Arthroplasty implants were the largest proportion of cost in either outpatient or inpatient setting, as high as 63% for outpatient RTSA.
THA and TKA have moved to the outpatient setting, with data showing maintained outcomes relative to an inpatient stay and at a lower cost. In a review of the literature, Pollock et al 1 reported maintained patient reported outcome measures and no increase in readmission rates or perioperative complications at a minimum 3-month follow-up across 17 studies. Lovald et al 4 showed similar rates of readmission between outpatient and inpatient TKA at multiple time intervals, including 3 months, 1 year, and 2 years. Using average Medicare payment for International Classification of Diseases, 9th revision Diagnosis and Current Procedural Terminology codes, they reported a cost savings around $8500 when moving TKA to the outpatient setting. 4 An outpatient THA evaluating preoperative, intraoperative, and postoperative costs using hospital charges, found a savings of around $2500. 20 Another study evaluating direct anterior THA moving to the outpatient setting used the total charges issued to payers and found a cost savings of $6000. 3 Discrepancies in the cost differences across studies may in part be because of the different methodologies used to determine cost of the episode.
Similar to THA and TKA, literature regarding outpatient TSR safety has also found maintained clinical outcomes relative to inpatient episodes. 6–10,12–14 In a matched cohort study, Brolin et al 7 reported a similar complication rate of 13% and 10% for outpatient and inpatient shoulder arthroplasty, respectively, with no difference in readmission (0% for both groups). The maintained outcomes have also been observed in large registry studies. Kramer et al 12 found no difference in 90 day readmission or ER visits, and no difference in 1-year mortality in a study of over 6500 shoulder arthroplasty patients. In a database study, Leroux et al 6 found improved 30 day readmission rates following outpatient shoulder arthroplasty when compared to inpatient procedures (1.74% vs 2.93%), as well as improved 30 day adverse event rates (2.31% vs 7.89%, respectively). Finally, a recent meta-analysis found lower complication rates for outpatient (vs) inpatient shoulder arthroplasty with no difference in 90 day readmission, revision, or infection rates. 15
Cost analyses focused on outpatient RTSA and TSR are limited. Cancienne et al 8 recently evaluated itemized 30 day postoperative reimbursements provided by a mixed insurance-based database of Medicare and private insurance companies and found a $3500 (19.7%) cost savings for outpatient (vs) inpatient TSR. This study relied on large administrative databases, which may carry inaccuracies with data quality or coding accuracy. 8 Using a public state health services database, Gregory et al 16 found the average charge for inpatient TSR was $76,109 compared to $22,908 for outpatient episodes, a savings of 70%. Further, inpatient RTSA was more expensive than inpatient anatomic TSR [$78,144 (vs) $66,293]. 16 Lastly Ode et al 21 reported that charges for outpatient shoulder arthroplasties were 40% less than inpatient procedures. However, this study did not differentiate between types of TSR and also included posttraumatic arthropathies and nonunions. 21
Although savings of the care episode has been shown, it is important to understand individual components of the total cost and what can be optimized. Kennon et al 11 evaluated standardized costs from a single academic institution using direct allocated costs (eg, materials, personnel, rent) and found a mean standardized cost for index inpatient surgical hospitalization of $14,501 for TSR and $17,407 for RTSA. The highest proportion of standardized cost was for the implant: 21.3% of overall cost for TSR and 27.5% of the total cost for RTSA. OR facility (24.6%), surgeon (12.6%), hospital room (12.0%), and preoperative/postoperative care (6.5%) were the drivers of total cost following the implant. 11 Menendez et al 19 used TdABC to calculate inpatient TSR cost in a private hospital using aggregated patient data and found the implant made up 57% of the inpatient costs (TSR 53%, RTSA 58%), and personnel (registration through OR) made up 20% of total costs (TSR 22% and 19% RTSA). Carducci et al 22 also found implant was the most important cost in a single center study, accounting for 60% and 57% of RTSA and TSR costs, respectively, compared to 40% for TKA and 52% for THA. 22 Lastly, in a single surgeon cost analysis for TSR at a single large academic medical center, Chalmers et al 23 found supply use (including implant) made up 82% of operative costs, and facility utilization (personnel) made up 18% of the operative costs. Similar to these previous studies evaluating inpatient shoulder arthroplasty, we found implant costs to be the most expensive component of total cost, up to 50% for inpatient RTSA and 42% for inpatient TSR. Personnel factors made up 28% of all costs for inpatient RTSA and 29% for inpatient TSR at our center.
This study differs from previous literature in that actual expense data from a health care maintenance organization with uniform system costs was used. Reviewing procedures from a single health care center allowed for more accurate representation regarding the actual cost within the organization rather than reimbursements or billed services from multiple centers. The TdABC analysis also allowed for more accurate assessment of cost to compare episodes of care across different arthroplasty types. Although actual cost numbers likely vary across institutions, percentages and proportions of cost in an episode of care are likely generalizable.
The present study found implant cost to be the greatest proportion of the total cost across all types of upper and lower arthroplasty, in both inpatient and outpatient settings, and as high as 63% of the cost of outpatient RTSA. Although there can be many factors associated with the cost of the implant, including the vendor, contract pricing, type of implant, region, size of the health care organization, volume of use, and consultant roles within industry organization, the prior literature and present study suggests implant cost is relatively immune to these factors. The implant is the most expensive proportion of cost across the literature no matter the health care setting (HMO, hospital employed, private practice, academic practice), surgery setting (inpatient, outpatient), or vendor, including within a large health-maintenance organization. Although many other factors influence the total cost for arthroplasty surgery, including rate of hospitalization, duration of stay, operative time, complexity of cases, patient factors, equipment, and resource utilization, implant cost remains the most expensive factor, with hospital bed admission status being the second costliest contribution. Facility personnel costs comprised 36%–44% of costs for outpatient shoulder arthroplasty episodes and 28%–36% for inpatient episodes. However, the OR time and RR time did not alter the cost of an episode of care to a large degree.
There are sparse studies identifying methods and pathways to reduce supply costs. Johnston et al 24 reported a 40% decrease in cost per implant for TKA and 18% decrease in implant cost for THA after implementing a 2-year contract with a 3-vendor system. Boylan et al 25 reported initiating a single vendor program for primary hip and knee replacements with mean costs per case decreasing by 23% in the first year. Our organization has utilized an implant vendor negotiation team formed by a hospital contracted consultant team and surgeon representatives. Organizational contract savings have been in line with past studies, producing more savings for lower-extremity joint replacements compared to shoulder arthroplasty. Despite these efficiencies, implant-related costs remain the single most expensive factor within the arthroplasty care episode. Future economic studies and adoptions of new strategies may benefit hospitals and organization to further increase cost savings.
The setting where outpatient surgery is performed will have an impact on cost. Currently in our organization, outpatient shoulder arthroplasty procedures are performed in an outpatient surgery center that is adjacent to the hospital. THA and TKA cases are performed in the main hospital OR, and these patients recover in the main operating room PACU prior to home discharge. In our institution, the payroll and OR costs are the same in these locations, but other institutions may find cost savings by changing the location of surgery. Many organizations have transitioned to outpatient joint arthroplasty in a freestanding outpatient surgery center. Efficiencies within such a setting may allow faster RR discharges, payroll savings, and other cost reductions. 26 This may be another future opportunity for cost savings for some organizations including our own. Conversely, the value of inpatient hospital admission has not been shown in the literature. Accurate patient selection for the optimal procedure setting will facilitate overall efficiency of care.
Study strengths include the evaluation of actual cost at a single institution using the TdABC method and prospective data collection. Uniform methodology was used across upper and lower joint arthroplasty procedures. Exact OR and RR times were obtained for each procedure to access different cost aspects of the episode accurately. Cost data were presented as percentages, which allows for more generalizability, and is more applicable to other institutions, compared to dollar amounts.
Limitations include the fact that negotiated contracts are specific only to our institution and staff costs are subject to pay structure, which is negotiated with a union and may differ between regions and organizations. Other differences from 1 site to another includes the setting of outpatient surgery, which may be variable depending on inherent efficiencies of the environment. Therefore, these findings may not be applicable to other systems that rely on different reimbursement models or payment contracts. However, it is likely that trends, percentages of cost, and areas to target for cost savings are universal.
Conclusion
Because of decreased hospitalization expenses, outpatient total joint arthroplasty reduced procedure expenses in a managed-care organization hospital setting by 20% to 30%. Cost savings associated with outpatient RTSA (22%) and TSR (20%) were substantial, although lower than savings for THA (29%) or TKA (30%). Implant costs remain the largest portion of shoulder arthroplasty procedure expenses, nearly twice as much as hospital bed charges.
Acknowledgments
The authors acknowledge the patient contributions for their deidentified data toward the completion of the study.
Footnotes
Author Contributions: Conceptualization: all authors; data curation: Edward H Yian, MD, Andrew M Schmiesing, MD, Heather A Prentice, PhD; Formal Analysis: Brandon D Kwong, MBA; supervision: Edward H Yian, MD; visualization: Brandon D Kwong, MBA; writing of original draft: Edward H Yian, MD, Andrew M Schmiesing, MD; writing, review, and editing: all authors.
Conflicts of Interest: Each author certifies that they have no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Funding: None declared
References
- 1. Pollock M, Somerville L, Firth A, Lanting B. Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: A systematic review of the literature. JBJS Rev. 2016;4(12):12. 10.2106/JBJS.RVW.16.00002 [DOI] [PubMed] [Google Scholar]
- 2. Scully RD, Kappa JE, Melvin JS. “Outpatient”-same-calendar-day discharge hip and knee arthroplasty. J Am Acad Orthop Surg. 2020;28(20):e900–e909. 10.5435/JAAOS-D-19-00778 [DOI] [PubMed] [Google Scholar]
- 3. Aynardi M, Post Z, Ong A, Orozco F, Sukin DC. Outpatient surgery as a means of cost reduction in total hip arthroplasty: A case-control study. HSS J. 2014;10(3):252–255. 10.1007/s11420-014-9401-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lovald ST, Ong KL, Malkani AL, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014;29(3):510–515. 10.1016/j.arth.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 5. Carey K, Morgan JR, Lin M-Y, Kain MS, Creevy WR. Patient outcomes following total joint replacement surgery: A comparison of hospitals and ambulatory surgery centers. J Arthroplasty. 2020;35(1):7–11. 10.1016/j.arth.2019.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leroux TS, Basques BA, Frank RM, et al. Outpatient total shoulder arthroplasty: A population-based study comparing adverse event and readmission rates to inpatient total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(11):1780–1786. 10.1016/j.jse.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 7. Brolin TJ, Mulligan RP, Azar FM, Throckmorton TW. Neer award 2016: Outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: A matched cohort study. J Shoulder Elbow Surg. 2017;26(2):204–208. 10.1016/j.jse.2016.07.011 [DOI] [PubMed] [Google Scholar]
- 8. Cancienne JM, Brockmeier SF, Gulotta LV, Dines DM, Werner BC. Ambulatory total shoulder arthroplasty: A comprehensive analysis of current trends, complications, readmissions, and costs. J Bone Joint Surg Am. 2017;99(8):629–637. 10.2106/JBJS.16.00287 [DOI] [PubMed] [Google Scholar]
- 9. Nwankwo CD, Dutton P, Merriman JA, Gajudo G, Gill K, Hatch J. Outpatient total shoulder arthroplasty does not increase the 90-day risk of complications compared with inpatient surgery in prescreened patients. Orthopedics. 2018;41(4):e563–e568. 10.3928/01477447-20180524-04 [DOI] [PubMed] [Google Scholar]
- 10. Charles MD, Cvetanovich G, Sumner-Parilla S, Nicholson GP, Verma N, Romeo AA. Outpatient shoulder arthroplasty: Outcomes, complications, and readmissions in 2 outpatient settings. J Shoulder Elbow Surg. 2019;28(6S):S118–S123. 10.1016/j.jse.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 11. Kennon JC, Songy CE, Marigi E, et al. Cost analysis and complication profile of primary shoulder arthroplasty at a high-volume institution. J Shoulder Elbow Surg. 2020;29(7):1337–1345. 10.1016/j.jse.2019.12.008 [DOI] [PubMed] [Google Scholar]
- 12. Kramer JD, Chan PH, Prentice HA, Hatch J, Dillon MT, Navarro RA. Same-day discharge is not inferior to longer length of in-hospital stay for 90-day readmissions following shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29(5):898–905. 10.1016/j.jse.2019.09.037 [DOI] [PubMed] [Google Scholar]
- 13. Erickson BJ, Shishani Y, Jones S, et al. Outpatient versus inpatient anatomic total shoulder arthroplasty: Outcomes and complications. JSES Int. 2020;4(4):919–922. 10.1016/j.jseint.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Antonacci CL, Cu BJ, Erickson BJ, Vazquez O, Alberta FG. Complications and readmissions after reverse and anatomic total shoulder arthroplasty with same-day discharge. J Am Acad Orthop Surg. 2021;29(3):116–122. 10.5435/JAAOS-D-20-00245 [DOI] [PubMed] [Google Scholar]
- 15. Cimino AM, Hawkins JK, McGwin G, Brabston EW, Ponce BA, Momaya AM. Is outpatient shoulder arthroplasty safe? A systematic review and meta-analysis. J Shoulder Elbow Surg. 2021;30(8):1968–1976. 10.1016/j.jse.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 16. Gregory JM, Wetzig AM, Wayne CD, Bailey L, Warth RJ. Quantification of patient-level costs in outpatient total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(6):1066–1073. 10.1016/j.jse.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 17. Calkins TE, Mosher ZA, Throckmorton TW, Brolin TJ. Safety and cost effectiveness of outpatient total shoulder arthroplasty: A systematic review. J Am Acad Orthop Surg. 2022;30(2):e233–e241. 10.5435/JAAOS-D-21-00562 [DOI] [PubMed] [Google Scholar]
- 18. O’Donnell EA, Fury MS, Maier SP, Bernstein DN, Carrier RE, Warner JJP. Outpatient shoulder arthroplasty patient selection, patient experience, and cost analyses: A systematic review. JBJS Rev. 2021;9(11):11. 10.2106/JBJS.RVW.20.00235 [DOI] [PubMed] [Google Scholar]
- 19. Menendez ME, Lawler SM, Shaker J, Bassoff NW, Warner JJP, Jawa A. Time-driven activity-based costing to identify patients incurring high inpatient cost for total shoulder arthroplasty. J Bone Joint Surg Am. 2018;100(23):2050–2056. 10.2106/JBJS.18.00281 [DOI] [PubMed] [Google Scholar]
- 20. Bertin KC. Minimally invasive outpatient total hip arthroplasty: A financial analysis. Clin Orthop Relat Res. 2005;435:154–163. 10.1097/01.blo.0000157173.22995.cf [DOI] [PubMed] [Google Scholar]
- 21. Ode GE, Odum S, Connor PM, Hamid N. Ambulatory versus inpatient shoulder arthroplasty: A population-based analysis of trends, outcomes, and charges. JSES Int. 2020;4(1):127–132. 10.1016/j.jses.2019.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Carducci MP, Gasbarro G, Menendez ME, et al. Variation in the cost of care for different types of joint arthroplasty. J Bone Joint Surg Am. 2020;102(5):404–409. 10.2106/JBJS.19.00164 [DOI] [PubMed] [Google Scholar]
- 23. Chalmers PN, Kahn T, Broschinsky K, et al. An analysis of costs associated with shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(7):1334–1340. 10.1016/j.jse.2018.11.065 [DOI] [PubMed] [Google Scholar]
- 24. Johnston DW, Beaupré LA, Davies DM, Hessels R. Reducing arthroplasty costs via vendor contracts. Can J Surg. 1999;42(6):445–449. [PMC free article] [PubMed] [Google Scholar]
- 25. Boylan MR, Chadda A, Slover JD, Zuckerman JD, Iorio R, Bosco JA. Preferred single-vendor program for total joint arthroplasty implants: Surgeon adoption, outcomes, and cost savings. J Bone Joint Surg Am. 2019;101(15):1381–1387. 10.2106/JBJS.19.00008 [DOI] [PubMed] [Google Scholar]
- 26. Fabricant PD, Seeley MA, Rozell JC, et al. Cost savings from utilization of an ambulatory surgery center for orthopaedic day surgery. J Am Acad Orthop Surg. 2016;24(12):865–871. 10.5435/JAAOS-D-15-00751 [DOI] [PubMed] [Google Scholar]


