The pathophysiological mechanisms underlying olfactory dysfunction are not well known but can be triggered in neurodegenerative diseases and after viral infection.1 We report a patient whose case could provide interesting insights into the neurophysiology of smell.
A woman aged 35 years was referred in July, 2019, to the Department of Radiation Oncology for radiotherapy of residual tumour tissue located in the olfactory region. Full details of the patient's medical history are in the appendix (pp 1–4).
The patient had previously undergone two surgical procedures to resect olfactory neuroblastoma. The first operation was a frontal craniotomy done 1 year before referral (July, 2018). After this surgical procedure had been performed, the patient reported that she had lost all olfaction, although this loss of sensation was not confirmed objectively. The second operation was done 1 year after the first operation (July, 2019) and entailed transnasal resection of recurrent tumour tissue. At the time of this second surgery, the patient had not recovered any olfaction. The olfactory epithelium was resected completely during these two operations, and the tumour could not be detected on CT 3 months after the second surgery (appendix p 5) or at the 21-month follow-up (appendix p 6).
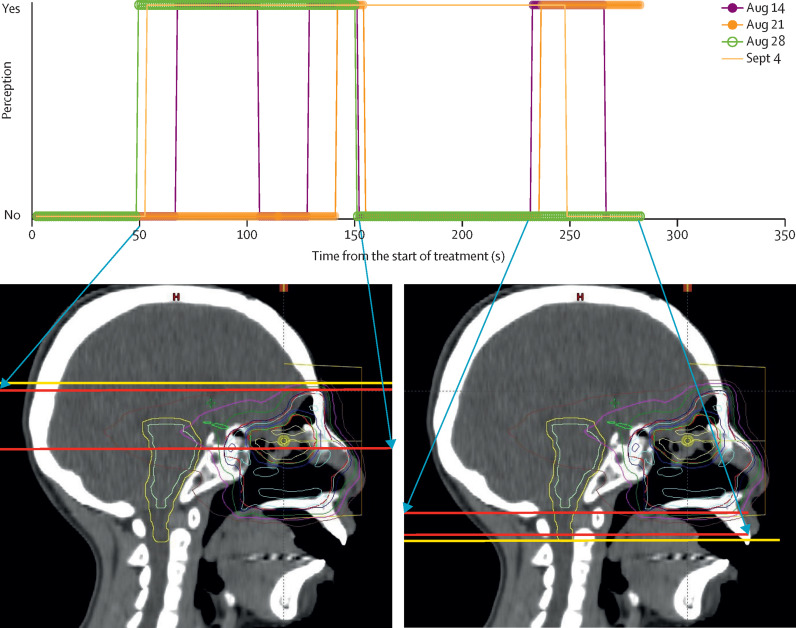
21 days after the second surgery, we treated the patient with helical tomotherapy, a type of intensity-modulated radiotherapy, administered as 60 Gy in 30 fractions over 43 days. A dosimetric analysis is presented in the appendix (p 7). During radiotherapy sessions, the patient complained of a foul odour. Olfaction was reported when the x-rays were directed through the frontal lobe and the lower part of the nasal cavity outside the olfactory epithelial level (figure ).
Figure.
Analysis of odour perception in the patient during radiotherapy sessions
The upper graph indicates periods when the patient perceived the foul odour; the different coloured lines represent results for days in which odour perception was measured. The lower images indicate the beam positions that overlapped the sagittal views of treatment-planning CT: yellow lines indicate the start (cranial; left panel) and end (caudal; right panel) of the full session; red lines indicate the beam positions during the start and end of olfaction for each period of perception. Part of this figure was reproduced, with permission, from Hara et al (2021).2
During radiotherapy sessions to treat brain tumours, other patients have also reported experiencing foul smells.2, 3 We did a prospective study in which 13 (34%) of 38 patients who received radiotherapy for brain or near-orbital tumours reported olfactory perceptions.2 Two (5%) of the 38 patients had no olfactory epithelium, including the individual described here. The cause or causes of these reported olfactory sensations remain undetermined. Patients might have either smelled substances such as ozone generated by the radiation or they might have had phantosmia.4 Moreover, temporal lobe seizures have been associated with a reported foul odour, such as that of burning tyres.5
It is possible that terminal sensors of cranial nerves, such as the trigeminal nerve, can detect the smell of substances generated by radiation. However, the patient we report here perceived an odour when the x-ray passed through the frontal lobe. Therefore, it could be concluded that the CNS of the patient detected the x-rays during radiation sessions, although this hypothesis remains to be proven.
KS reports a grant from Hitachi. All other authors declare no competing interests.
Supplementary Material
References
- 1.Xydakis MS, Albers MW, Holbrook EH, et al. Post-viral effects of COVID-19 in the olfactory system and their implications. Lancet Neurol. 2021;20:753–761. doi: 10.1016/S1474-4422(21)00182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hara N, Isobe A, Yamada K, et al. Unusual visual and olfactory perceptions during radiotherapy sessions: an investigation of the organs responsible. J Radiat Res (Tokyo) 2021;62:718–725. doi: 10.1093/jrr/rrab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Obinata M, Yamada K, Sasai K. Unusual olfactory perception during radiation sessions for primary brain tumors: a retrospective study. J Radiat Res (Tokyo) 2019;60:812–817. doi: 10.1093/jrr/rrz060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang JC, Khakoo Y, Lightner DD, Wolden SL. Phantosmia during radiation therapy: a report of 2 cases. J Child Neurol. 2013;28:791–794. doi: 10.1177/0883073812450616. [DOI] [PubMed] [Google Scholar]
- 5.Berkowitz AL. In: Clinical neurology and neuroanatomy: a localization-based approach. Berkowitz AL, editor. McGraw-Hill; New York: 2017. Cranial nerves 1, 9, 10, 11, and 12; pp. 125–128. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.