ABSTRACT
As more healthcare is provided in non-hospital settings, it is essential to support clinicians in recognising early signs of clinical deterioration to enable prompt intervention and treatment.
There are intuitive reasons why the use of the National Early Warning Score 2 (NEWS2) in out-of-hospital settings may enhance the community response to acute illness by using a common language across healthcare. An additional advantage of the use of NEWS2 in community settings is that it is not disease specific and requires no expensive technology or great expertise to take a full set of observations that can be an indicator of clinical acuity.
However, concerns have been expressed as NEWS2 was developed in acute hospital settings that it may not be applicable in community settings; this review shares some of the practical ways that NEWS2 can support clinical practice along with the emerging published evidence.
KEYWORDS: NEWS2, out-of-hospital settings, ambulance, emergency department
Introduction
As more healthcare is provided in non-hospital settings, it is essential to support clinicians in recognising early signs of clinical deterioration to enable prompt intervention and treatment. In Time to act, the ombudsman recommended ‘timely history and examination on admission or referral’ and ‘regular physiological monitoring using track and trigger systems’ to aid recognition and monitoring of potential deterioration.1 The National Confidential Enquiry into Patient Outcomes and Deaths (NCEPOD) Just Say Sepsis report recommended ‘An early warning score (EWS), such as the National Early Warning Score (NEWS) should be used in both primary care and secondary care for patients where sepsis is suspected’.2
More recently, the Royal College of Physicians (RCP) has recommended that ‘NEWS should be used in the pre-hospital assessment of acutely ill patients by ‘first responders’, eg ambulance services, primary care and community hospitals, to identify and improve the assessment of acute illness, triage and the communication of acute-illness severity to receiving hospitals.’3
One of the potential advantages of the use of NEWS2 in community settings is that it requires no expensive technology or great expertise to take a full set of observations that can be an indicator of clinical acuity but is not disease specific. Despite this, there has been reluctance to use early warning scores (EWS), such as NEWS2, in settings such as pre-hospital care.
The evidence for NEWS2 in out-of-hospital settings
There are intuitive reasons why the use of NEWS2 in out-of-hospital settings may enhance the community response to acute illness by using a common language across healthcare settings, and there is an emerging evidence base to support this.
Concerns had been expressed that EWS would have a different predictive value in different settings but a systematic review of 17 studies in 157,878 patients demonstrated that measurement of EWS in community settings correlates with short-term outcomes, which would be expected if a EWS is just an objective measure of physiology.4
Another concern regarding the use of NEWS in community settings is its value as a track and trigger tool to identify deterioration. In hospital settings, repeated observations are used to detect deterioration and the aggregated score for NEWS2 triggers a specific category of intervention in terms of speed of intervention and the experience and clinical competency of the responder(s). However, in pre-hospital settings, the track and trigger element relates to the system response to illness, such as a change in NEWS2 between patient assessments, rather than a requirement to perform repeated observations. In this way, NEWS2 can aid communication about the severity of acute illness between clinicians such as the general practitioner (GP) and the out-of-hours service. There is also the added potential for NEWS2 to be a standardised measure of clinical acuity across the healthcare system and, by using a common language, the subsequent healthcare response can be tailored to NEWS2; for example, in patients with a high NEWS2, the ambulance response and conveyance time can be prioritised and faster, the emergency department (ED) can be pre-alerted and patients at the highest risk of further deterioration can be assessed by more senior clinicians. This means that the patient is seen in the right place at the right time by the right grade of clinician. A change in NEWS2 from referral to arrival can also indicate deterioration.
NEWS2 is most useful in the undifferentiated unwell patient. Although NEWS2 can identify patients at the highest risk of deterioration due to any cause, it does not override existing pathways for specific conditions, such as stroke or chest pain.3
Experience in using aggregated score across a health system
In 2015, the West of England region standardised the use of NEWS (the project pre-dated the introduction of NEWS2) across a region of a 5 million population. It was decided that clinicians would either refer acutely ill patients to hospital with a NEWS, or share a full set of observations at the point of referral, enabling the admitting team to calculate the NEWS. Once community clinicians became familiar with NEWS, they spontaneously started to use the tool to support their clinical judgement.
After this widespread implementation of NEWS across the system, the West of England region had the lowest mortality in patients with suspicion of sepsis (SOS) across England. Suspicion of sepsis is based on a group of 200 coded conditions that can lead to sepsis, and data from the national dashboard for SOS for the West of England were examined over time and compared with the rest of England.5,6 There was a reduction in mortality in the SOS cohort in the West of England, which was not seen in the rest of England over the time period of the project (Fig 1). Moreover, hospital admissions did not increase. While cause and effect cannot be assumed in a complex health system, the timing of the mortality reduction aligns closely with the point at which most organisations across the health system had adopted NEWS and were communicating it consistently and effectively.7
Fig 1.
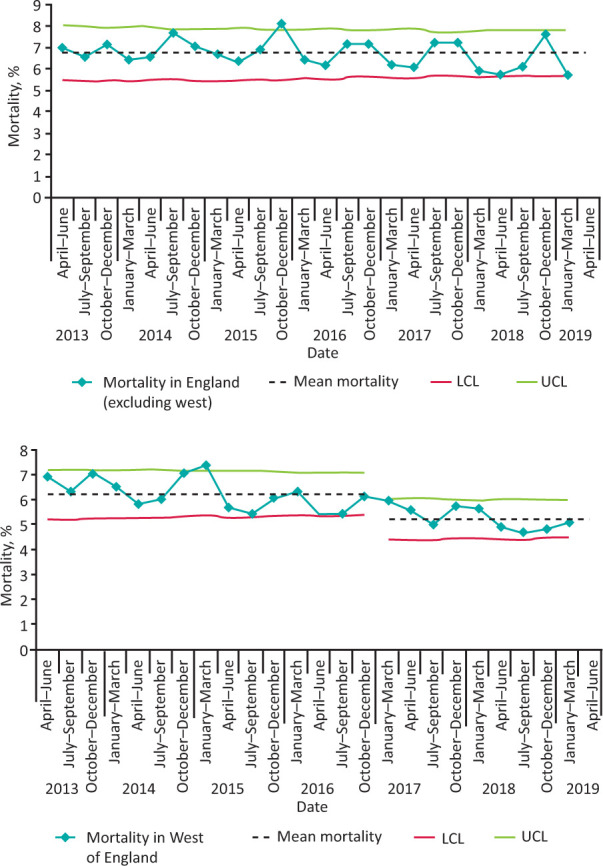
Mortality of patients with suspicion of sepsis across Academic Health Science Networks. a) Crude mortality of patients with suspicion of sepsis in all 14 Academic Health Science Networks excluding the West of England. b) Crude mortality of patients with suspicion of sepsis in the West of England. LCL = lower control limit; UCL = upper control limit.
As part of the same project in the West of England, NEWS for patients at point of referral in primary care, in the GP admissions unit and in ED were demonstrated to correlate with short-term outcomes, such as length of stay (LOS), intensive care unit admission and mortality.8 More importantly, evidence from 13,047 GP referrals into acute care demonstrated that a higher NEWS was associated with faster conveyance for patients travelling by ambulance and faster time from hospital arrival to medical review, demonstrating how the system response was informed by and reacted appropriately to a higher NEWS.4
Silcock et al found that an elevated NEWS among unselected pre-hospital patients was associated with increased adverse outcomes and suggested that calculation of a EWS prior to transfer to hospital could facilitate earlier recognition of at-risk or deteriorating patients and enabling the alerting of ED.9 Inada Kim et al found that elevated NEWS in the community during the process of emergency admission is associated with adverse outcomes.10 They concluded that:
A clear relationship between elevated scores and mortality at 5 and 30 days was observed. While there is no consensus on the absolute positive predictive value that would encourage use of the score, its relative simplicity makes it a potentially useful and convenient method of communicating risk to the next immediate provider of care in a care chain from community to hospital. 10
Practical considerations in the use of NEWS in community settings
NEWS2 and decisions regarding escalation
When NEWS2 is used in the acute sector, there are escalation protocols delivered within specific time frames. In the community, the opportunities for ‘tracking’ NEWS2 are different as a clinician may see an unwell patient with a low NEWS2 but if the same patient is reviewed later by another health professional, a NEWS2 of 7 can provide objective evidence of clinical deterioration. This tracking of a change in NEWS2 is of particular value if a health professional does not know a patient or if the patient is being reviewed in another healthcare setting, such as ‘out of hours’.
NEWS2 and clinical judgement
Concerns have also been expressed that linking actions to specific NEWS values in the community could negatively impact patients; for example, if a clinician or other healthcare provider was falsely reassured by a low NEWS value. However, the RCP guidance is clear in that ‘any concern about a patient's clinical condition should prompt an urgent clinical review, irrespective of the NEWS.’3 The Health and Safety Investigation Branch (HSIB) observed that ‘NEWS2 is not intended to be a stand-alone tool. Instead, it is intended to be combined with other relevant charts, clinical investigation results and notes together with clinical observations of the patient.’11 Clinical judgement is always paramount and a patient with central crushing chest pain or evidence of a stroke should clearly be admitted to hospital whatever the NEWS2. The acute cardiac cohort may elicit a low NEWS2, despite being potentially gravely unwell; therefore, clinical judgement is key to management and there needs to be consideration of how this is accommodated within the protocol driven response of, for example, the ambulance service.
Another issue was that patients at the end of their life could have a raised NEWS, that could prompt an inappropriate admission. Again, clinical judgement is key. This scenario prompted parallel work on the use of advance care plans, such as ReSPECT, so that NEWS2 contributes to the holistic assessment of the patient and not just a blanket response to a particular score.12
Baseline NEWS2 scores
As NEWS was developed in the acute sector, another concern was that many people with long-term conditions could have raised ‘baseline’ NEWS and, therefore, if a NEWS of 5 were chosen as a trigger to consider admission, the system could be overwhelmed. This hypothesis was refuted as 92% (n=122,000) of patients seen in the ED, 83% (n=1.1 million) of patients under ambulance service care and 90% (n=21,000) of those assessed by the community nursing teams had a NEWS of less than 5. It is of interest that, of the patients who had been referred to the hospital for further clinical assessment after a review by a primary care clinician, 31% had a NEWS of ≥5, demonstrating that the sickest patients were being admitted.13
Use of NEWS2 in care homes
In the care home context, NEWS2 measurement often forms part of composite deterioration tools, such as RESTORE2.14 The philosophy, driven predominantly from an intuitive clinical perspective, is that care home staff can use NEWS2 as an adjunct to their intuition, to identify residents earlier in their acute illness trajectory.
For further discussion on the use of NEWS in the older person please see Vardy et al's paper.15
Practical considerations in the use of NEWS in the ambulance service and the ED
Ambulance services provide care for the broadest possible range of patients in terms of age, complexity and disease groups, as well as, importantly, a range of acuity. The use of NEWS2 aligns well with the predominantly protocol-driven approach advocated for assessing patients presenting to the 999 service with high-acuity presentations and is now included in the risk assessment for speed of transfer.16 Data from NHS England state that all ambulance services in England have adopted the NEWS2 scoring system.17 This has been reinforced by a national patient safety alert issued in 2018 when it was recommended that ‘all acute hospital trusts and ambulance trusts to fully adopt NEWS2 for adult patients’.18
There is increasing evidence that the use of NEWS2 in the ambulance service can support paramedics in decision making and the prioritisation of the sickest patients for transfer.19 Inada-Kim et al suggested that communicating NEWS could enable downstream care to be ‘better calibrated to risk’.10
However, for the potential of NEWS2 to be maximised, information (such as previous observations or NEWS2 values) should to be available in the electronic patient care records used by the attending crew. There must also be adequate training, such as the correct choice of the use of oxygen saturation scale 1 and scale 2 in patients, to correctly identify patients at risk of hypercapnic respiratory failure. Another priority is to recognise that, although NEWS2 is useful in pre-hospital settings, it is not appropriate for all patient groups, such as pregnant women, and the key is modification of some of the clinical pathways.
NEWS2 can be used as a common language to communicate patient acuity between the ambulance service and the ED, and support both with the use of pre-alerts.20 At times of ED overcrowding, NEWS2 can help to identify which patients waiting in an ambulance may be sickest or at greatest risk of deterioration. Within the ED when NEWS2 is measured as part of the initial triage process, it provides valuable information in addition to the presenting complaint, which supports the ED team to assign the correct triage category to the patient. The triage category determines the order in which patients are seen and is a vital safety process in busy and often crowded departments.
A NEWS2 of 5 at triage also triggers consideration of sepsis as a potential cause for the acute illness and sepsis screening, leading to earlier diagnostic tests and subsequent treatment when appropriate.
Serial measurements of NEWS also helps the ED team to recognise deteriorating patients in crowded departments. It is a component of the ED safety checklist, which has been spread nationally to all EDs and is designed to keep patients safe, especially at the busiest times.21 This helps the ED team to prioritise the most unwell patients, ensuring that the patients are admitted to the most appropriate clinical area and referred earlier to critical care if needed.
Clinicians' experience of using NEWS2
Although there is evidence that numbers correlate with outcomes, what do clinicians think? A qualitative study in staff from primary care, ambulance service, community and mental health settings in the West of England region demonstrated that NEWS was effective at supporting clinical decision making, prioritisation and escalation of care.22
Although emergency departments understand if a blood pressure or heart rate is deteriorating, [NEWS] encapsulates all those baseline observations, so that we know that, actually, somebody who, originally, 20 minutes ago, had a NEWS score of 4, now has a NEWS score of 7, and this is clearly identifiable as somebody who may need to go to the front of the queue. – a paramedic22
It improved communication across systems and professional roles.
I think it's difficult to convey a patient's condition over the phone and sometimes in the past I have been saying, ‘They have got tachycardia and they don't look well.’ If you say, ‘Actually they have got a NEWS score of six.’ Suddenly they say, ‘Well I think we better see them.’ – a nurse22
Some felt it was easier to arrange admissions as NEWS provided objective evidence of physiological deterioration.
One of the nurses saw somebody with a NEWS score of 7. She thought he was septic ... She said that before, she'd have had to speak to one of us before she got the approval for doing the admission. But because he had got a NEWS of 7, she was able to phone the ambulance service, phone the ED, and get it sorted out. – a GP22
Conversely, NEWS also provided a degree of validation if a decision was made not to admit.
Making the decision not to admit someone or not to refer someone, which we have to do most of the time, there's potentially a lot of comeback on you for not doing that, so anything that covers you and helps protect you or back up your decision making is potentially useful. – a GP22
By recording NEWS at the time of seeing a patient, it can provide evidence of a considered assessment. If a patient re-presents to a different colleague later in the day with a higher NEWS2, this objective evidence of physiological deterioration can support clinicians in their decisions, which is of additional value in a healthcare service where it is not possible to provide continuity of clinician.
Conclusion
While there is increasing evidence for the value of NEWS2 in clinical practice for both the patient and the clinician, uncertainties remain. The Royal College of General Practitioners supports the use of physiological measurements in a general practice setting for all patients at risk of deterioration but has stopped short of recommending widespread uptake of NEWS2 without more research and evidence.23
There are still areas where the practical impact of NEWS2 in pre-hospital settings needs further research and clarification, such as the use of NEWS2 to inform ambulance despatches to ensure decisions be balanced with clinical need. Finnikin et al found that NEWS was poorly related to hospital referral, but these were retrospectively calculated scores with no detail on diagnosis in a system that was not using, or responding to, NEWS in patients outside hospital.24 The observations were also taken by healthcare assistants and not the admitting clinicians, so NEWS was not used as a tool to support decisions to admit.
The delivery of care in the NHS is also changing to include new models, such as virtual wards and same-day emergency care, delivered in non-hospital settings.25 Digital technology and the remote monitoring of patient observations underpin many of these pathways, particularly as NEWS2 is often one of the entry criteria as an indicator of clinical acuity. Remote monitoring may be used to support these ‘virtual wards’ and an increased understanding of changes in patient physiology can provide objective evidence of both when the patient deteriorates but also when they improve.
NEWS2 is a common language in the acute sector, it is becoming a more common language in pre-hospital settings, and it has great potential to provide a common language supporting shared decision making with our patients.
References
- 1.Parliamentary and Health Service Ombudsman . Time to act: Severe sepsis: rapid diagnosis and treatment saves lives. Parliamentary and Health Service Ombudsman, 2013. www.ombudsman.org.uk/sites/default/files/Time_to_act_report.pdf [Google Scholar]
- 2.National Confidential Enquiry into Patient Outcome and Death . Just Say Sepsis! A review of the process of care received by patients with sepsis. NCEPOD, 2015. www.ncepod.org.uk/2015report2/downloads/JustSaySepsis_Summary.pdf [Google Scholar]
- 3.Royal College of Physicians . National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. RCP, 2017. www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 [Google Scholar]
- 4.Patel R, Nugawela MD, Edwards HB, et al. Can early warning scores identify deteriorating patients in pre-hospital settings? A systematic review. Resuscitation 2018;132:101–11. [DOI] [PubMed] [Google Scholar]
- 5.Inada-Kim M, Page B, Maqsood I, Vincent C. Defining and measuring suspicion of sepsis: an analysis of routine data. BMJ Open 2017;7:e014885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Academic Health Science Networks Network . Suspicion of Sepsis (SOS) Insights Dashboard. The AHSN Network. www.sos-insights.co.uk [Google Scholar]
- 7.Pullyblank A, Tavaré A, Little H, et al. Implementation of the National Early Warning Score in patients with suspicion of sepsis: evaluation of a system-wide quality improvement project. British Journal of General Practice 2020;70:e381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott LJ, Redmond NM, Tavaré A, et al. Association between National Early Warning Scores in primary care and clinical outcomes: an observational study in UK primary and secondary care. Br J Gen Pract 2020;70:e374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silcock DJ, Corfield AR, Gowens PA, Rooney KD. Validation of the National Early Warning Score in the prehospital setting. Resuscitation 2015;89:31–5. [DOI] [PubMed] [Google Scholar]
- 10.Inada-Kim M, Knight T, Sullivan M, et al. The prognostic value of national early warning scores (NEWS) during transfer of care from community settings to hospital: a retrospective service evaluation. BJGP Open 2020;4:bjgpopen20X101071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healthcare Safety Investigation Branch . Recognising and responding to critically unwell patients. HSIB, 2019. www.hsib.org.uk/investigations-and-reports/recognising-and-responding-to-critically-unwell-patients [Google Scholar]
- 12.Resuscitation Council UK . ReSPECT. Resuscitation Council UK. www.resus.org.uk/respect [Google Scholar]
- 13.Scott LJ, Redmond NM, Garrett J, et al. Distributions of the National Early Warning Score (NEWS) across a healthcare system following a large-scale roll-out. Emergency Medicine Journal 2019;36:287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hampshire and Isle of Wight . RESTORE2 official. Hampshire and Isle of Wight. www.hantsiowhealthandcare.org.uk/your-health/restore2 [Google Scholar]
- 15.Vardy E, Lasserson D, Barker R, Hanratty B. National Early Warning Score (NEWS) 2 and the older person. Clin Med 2022;22:522–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NHS England, NHS Improvement . National Framework for Healthcare Professional Ambulance Responses. NHS, 2021. www.england.nhs.uk/publication/healthcare-professional-ambulance-responses-framework [Google Scholar]
- 17.NHS England . National Early Warning Score (NEWS). NHS, 2017. www.england.nhs.uk/ourwork/clinical-policy/sepsis/nationalearlywarningscore [Google Scholar]
- 18.NHS England . Patient Safety Alert: Resources to support the safe adoption of the revised National Early Warning Score (NEWS2). NHS, 2018. www.england.nhs.uk/publication/patient-safety-alert-safe-adoption-of-news2 [Google Scholar]
- 19.Shaw J, Fothergill RT, Clark S, Moore F. Can the prehospital National Early Warning Score identify patients most at risk from subsequent deterioration? Emergency Medicine Journal 2017;34:533–7. [DOI] [PubMed] [Google Scholar]
- 20.West of England Academic Health Science Network . Watch our film to see NEWS in practice. WEAHSN, 2017. www.weahsn.net/news/watch-film-see-news-practice [Google Scholar]
- 21.Redfern E, Hoskins R, Gray J, et al. Emergency department checklist: an innovation to improve safety in emergency care. BMJ Open Quality 2018;7:e000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brangan E, Banks J, Brant H, et al. Using the National Early Warning Score (NEWS) outside acute hospital settings: a qualitative study of staff experiences in the West of England. BMJ Open 2018;8:e022528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Royal College of General Practitioners . NEWS2 score for assessing the patient at risk of deterioration. RCGP. www.rcgp.org.uk/policy/rcgp-policy-areas/news2-score-for-assessing-the-patient-at-risk-of-deterioration.aspx [Google Scholar]
- 24.Finnikin S, Hayward G, Wilson F, Lasserson D. Are referrals to hospital from out-of-hours primary care associated with National Early Warning Scores? Emergency Medicine Journal 2020;37:279–85. [DOI] [PubMed] [Google Scholar]
- 25.NHS England . Virtual wards. NHS. www.england.nhs.uk/virtual-wards [Google Scholar]


