ABSTRACT
This year is the 10th anniversary since the launch of the National Early Warning Score (NEWS) by the Royal College of Physicians in 2012. This review reflects on the journey, from the nascent concept of a standardised system to detect acute illness severity and clinical deterioration through to the adoption of NEWS2 by the NHS and, ultimately, its incorporation into quality indicators of acute care provision. The impact of NEWS/NEWS2 on the transformation of provision and configuration and training of acute care teams in hospitals is reviewed. User feedback has been key in iterating guidance on the use of NEWS/NEWS2 and key elements of this are discussed. The ultimate aim of NEWS was to improve patient outcomes with acute illness or deterioration and the impact on outcomes is now becoming apparent but, paradoxically, an effective response can eliminate the link between the score and the ultimate outcome. This review concludes with a reflection on what the next 10 years may bring, particularly with the digital transformation of healthcare and its potential impact on scoring systems, as well as the necessary permeation of NEWS2 beyond the acute hospital setting into emergency response triage in primary and community care settings.
Ten years on, via NEWS/NEWS2, the NHS is the first healthcare system globally with a ‘common language’ of illness severity and a standardised early warning system for acute clinical illness and deterioration, a system that is now being replicated in many other areas of the world.
KEYWORDS: NEWS, NEWS2, implementation, NHS, early warning scores
Why was the National Early Warning Score developed?
A number of national reports in the years, preceding the development and subsequent launch of the National Early Warning Score (NEWS) in 2012, had highlighted the poor performance of NHS in the timely detection and response to acute illness.1–4 In its report in 2007, the Royal College of Physicians (RCP) Acute Medicine Task Force recommended a template for the development of acute medicine units in acute hospitals across the NHS, underpinned by a new specialist discipline of acute medicine.2 Alongside, one of our recommendations was the need for a national early warning score to improve the detection and response to acute medical illness, whether it be at presentation of an acute illness or timely detection of acute clinical deterioration in patients already under care.2 A recommendation founded on the observation that to improve the outcomes of patients with acute illness/deterioration, time is of the essence; with a triad of factors determining clinical outcomes: early detection; speed of response; and the nature of that response (ie the competencies of the responder(s)). Early warning systems have the potential to drive improvements in the first two factors and complementary guidance on how to configure clinical teams 24/7 can assure the latter.
Of interest, the ‘N’ in NEWS originally referred to the ‘NHS’ (the NHS Early Warning Score) but we were advised against using the NHS moniker as this would need to be approved by a process that wasn't well defined and would take an unspecified amount of time. The ‘N’ was, thus, changed to ‘National’. This was fortuitous, as NEWS would eventually permeate beyond the NHS to be used in many healthcare settings in the UK and across the world.
NEWS was developed by the National Early Warning Score Development and Implementation Group (NEWSDIG), comprising physicians, nurses, ambulance services and patients, hosted by the Royal College of Physicians (RCP).1 The concept and development were clinically led, with a vision to develop a standardised methodology to grade acute illness severity and to detect patient deterioration, to be applied across the whole NHS, with system-wide instantly recognisable documentation to facilitate recording, scoring and responding to changes in routinely measured physiological parameters.
While there were already multiple early warning scores (EWS) in existence, they were often not validated and/or locally modified from the original, compromising any prior validation.5 There were also variations in the scoring process. In most early iterations of EWS systems, a high score was bad and, in others, it was good. Moreover, across scoring systems, the magnitude of the score didn't correlate with the same level of clinical deterioration. Furthermore, while many hospitals had no EWS system, others had multiple different systems, in different clinical areas or, sometimes, even in the same clinical area. This variation was undesirable, dysfunctional and potentially dangerous, with potential for miscommunication of illness severity, especially when staff are working across different hospitals or ward areas, or move to new roles in different hospitals with different EWS systems.5 This lack of a standardised approach also bedevilled attempts to provide consistent education and training in the assessment of acute illness. Thus, a priority from the many recommendations of the acute medicine task force report was a system-wide standardisation of our approach to acute illness assessment and response, recognising that standardising the use of a single system would yield much greater patient safety and outcome benefits than any potential small differences in the performance of the many existing scoring systems. Crucially, it would also allow everyone in the NHS to speak a common language, and facilitate a standardised system for education, accreditation and training. Moreover, standardisation was the key philosophy underpinning NEWS because it is fundamental to safety processes, across many industries; thus, why not the same for the NHS? This was noted by the NHS medical director, Sir Bruce Keough, commenting on the widespread adoption of NEWS2 by the NHS in 2017:
Systems operating with similar levels of risk use universal means of communication to reduce the chance of failure ... Air traffic control systems the world over adhere to common standards and language to prevent disasters ... Imagine what would happen if each airport pursued its own way of working? 6
Developing NEWS
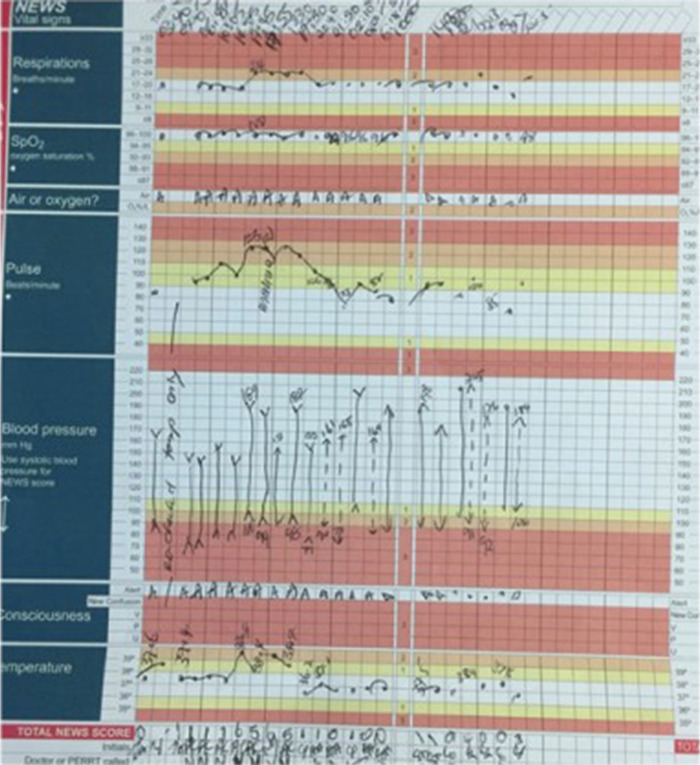
EWS systems assess the magnitude of physiological disturbance from the norm in response to acute illness and are generally based on allocating scores to routinely measured physiological parameters in a clinical setting. A score of zero representing no physiological disturbance and higher scores reflecting greater disturbance. By scoring multiple physiological parameters simultaneously and aggregating the score, the sensitivity and specificity of the score to detect acute deterioration earlier is enhanced.7 This is because changes in physiological parameters track with each other in response to acute illness; for example, when temperature begins to rise due to infection, there is invariably a concomitant rise in heart rate and respiratory rate, which might be barely noticeable in isolation, but the changes are magnified through aggregate scoring of the change in all parameters. This phenomenon is illustrated in Fig 1 from a bedside vital signs chart from a patient who developed a urinary tract infection in hospital.
Fig 1.
An early iteration of the National Early Warning Score chart showing the repeated scoring of physiological parameters from a patient who developed a urine infection in hospital. Note the coincidence of the rise in respiratory rate, pulse rate and temperature as the patient developed a fever and the marked escalation of the aggregate score from 1 to 5–6. Followed by a similar time pattern of rapid resolution after prompt treatment of the patient with antibiotics.
An important consideration was to ensure that the parameters included in the score (Box 1) were easily measured at the point of routine care, without requirement for blood or urine tests, or any other specialised testing or equipment.
Box 1.
Physiological vital sign parameters that form the basis of the National Early Warning Score and National Early Warning Score 2
|
The only parameter that was potentially controversial at the time of the original development of NEWS was the inclusion of oxygen saturation; while this seems somewhat ironic now, with the COVID-19 pandemic having led to many patients having their own pulse oximeters at home, at the time, oxygen saturation was not being measured universally across the health service or routinely by ambulance services.
The NEWS chart guided the user though the process of measuring and recording the score for each physiological parameter, before adding up the numbers and adding a binary score of two for any use of oxygen to give the final NEWS score. The chart allowed tracking of the score over time, making any change immediately obvious.
The scoring system is designed to trigger an appropriate response in terms of time and responder(s), and accompanying guidance was provided on how the score should be used to inform decisions for ongoing care: whether care escalation was required and how urgently, what level of clinician competency was required to respond to the patient, the intensity of ongoing care, the frequency of monitoring, and the appropriate setting for ongoing care to take place (ie whether higher dependency or intensive care unit (ICU) care was required).
As evidence of use of NEWS emerged, it became apparent that a score of <5 usually indicated that a patient was reasonably stable and lower risk, and that clinical management would usually be ward-based, while a score of 5 or more was medium–high risk and should trigger concern requiring a more urgent response by those with competencies in assessing and treating acutely ill patients. A score of 7 was high risk and should prompt major concern, with emergency transfer to hospital usually being indicated for patients in a community setting.8–16 In contrast, a high score in a single parameter is much more unusual in response to acute clinical deterioration and requires a clinician to promptly determine the cause. An important point emphasised in the original NEWS report, and reiterated subsequently, is that a low score should never override a healthcare professional or carer's concern about a patient's clinical condition if they feel it is necessary to escalate care. NEWS is a powerful aid to assessment, not medicine by numbers, and it doesn't replace the ill-defined sense that experienced nurses and clinicians develop that something just isn't right. There are also circumstances in which a patient may be acutely ill with a condition that doesn't always markedly disturb vital sign physiology in proportion to their need for urgent or emergency care; for example, an acute stroke or acute myocardial infarction might present with a NEWS <5 but with other signs and symptoms that make the need for urgent care obvious.
NEWS was launched by the RCP on 27 July 2012, with a press conference, gaining some media attention, despite the launch coinciding with opening ceremony of Olympic games in London.
Concerns from the time that NEWS was launched
There was inevitably some resistance and criticism following the initial launch of NEWS. NEWS was a disruptive but appropriate challenge to the widespread variation in acute care across the NHS. The concept of system-wide standardisation is rarely met with enthusiasm from professional groups often wedded to bespoke models of care. The challenges were frequent and vociferous. Without the persistence and determination of the NEWS development team, and the unrelenting support of the senior leadership of the RCP, it would have faltered. The fact that NEWS was clinically led, and was not imposed from on high, was undoubtedly a factor in its successful deployment, embraced by a silent majority of clinicians and nurses who recognised the benefits of standardisation and a common language for clinical deterioration. The many lessons learned were important in aiding the subsequent development of standardised national paediatric and maternity EWS in the tailwind of NEWS.17,18
A legitimate concern was the organisational implications of implementing NEWS at an individual hospital level. This was manifest in some initial criticism of the standards set down for responding to higher NEWS and ongoing care; not all hospitals had sufficient staff with the required competency levels to provide the required response, especially overnight or at weekends. This would prove to be an important and necessary driver of change. The criticism was reflective of an inadequate acute care system, rather than inadequacies of NEWS; an acute care system incapable of providing a universal high standard of response to acute clinical deterioration.
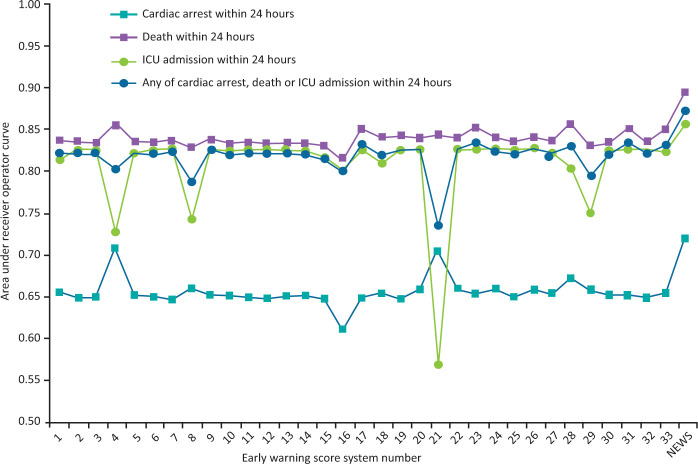
Another line of resistance was whether NEWS was ‘validated’, irrespective of the fact that most of the existing systems in use, were not. There were two approaches taken to validation: a desktop evaluation of the scoring system proposed for NEWS using a large clinical database that linked baseline physiological variables recorded in routine care to outcomes; and recognition that once launched, user feedback would provide a powerful tool to modify the scoring system if needed. This latter approach led to the update of NEWS to NEWS2 in 2017. With regard to the former, given that the likely standardisation benefits of NEWS were widely accepted, the main aim had been to demonstrate that the proposed NEWS scoring system was at least non-inferior to the other EWS that were available at the time. To this end, a key study by Smith et al, published in 2013, compared NEWS with 33 other EWS systems being used in the NHS at the time regarding the ability to predict the outcomes of death, cardiac arrest or ICU admission.19 This study showed that NEWS2 was better at predicting these outcomes than any of the other EWS, probably because of the inclusion of oxygen saturation among the parameters (Fig 2).
Fig 2.
Area under the receiver operating curves for the National Early Warning Score and 33 other early warning score systems previously evaluated using the system scores relative to each outcome studies. 35,585,patient episodes and 198,755 vital signs datasets. ICU = intensive care unit; NEWS = National Early Warning Score. Adapted with permission from Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013;84:465–70.
Subsequently, many studies have evaluated and validated the utility of NEWS in a variety of clinical settings.8–16 However, there remains a challenge in validating these EWS systems, principally centred around the measure of validity. Typically, the measure of validation is the prediction of outcomes based on the initial score. Outcomes in this context are usually either an escalation of care (eg to more intensive care), in-hospital cardiac arrest or mortality. The problem with this approach is that the outcome is not only determined by the physiological score but also by the speed and nature of the clinical response, according to the individual patient treatment escalation plan. The irony is that if NEWS works and the clinical response is optimal, then the link between the original NEWS and adverse outcomes would begin the break down, with anticipated adverse outcomes reduced or averted, which is itself the primary objective of the score.
Progression of NEWS to NEWS2
With the widespread and growing use of NEWS, regular feedback was forwarded to the RCP by users and reviewed by the chair of the NEWS Development Group. It soon became clear that improvements could be made, and work began on NEWS2, which was released in December 2017.6
The NEWS2 vital signs chart
When NEWS was originally launched, alongside a standardised scoring system, we also proposed a standardisation of the vital signs chart used in all hospitals to provide a familiar interface for all users of NEWS so that clinical deterioration and documentation of the response were easily recognisable. The vital signs chart was updated for NEWS2 because of user reports that the red/amber/green scale in the original NEWS chart was problematic for those with red–green colour-blindness. The chart colour scheme was updated for NEWS2 and the recording of vital signs were also reordered to reflect the Resuscitation Council UK ABCDE (airway, breathing, circulation, disability and exposure) format.
New-onset confusion added to NEWS2 scoring system
Consciousness in the original chart used the familiar AVPU (alert, verbal, pain and unresponsive) scale. In the updated NEWS2 chart, ‘new-onset confusion’ was added, recognising that this is an important sign of physiological decompensation, even if patients are alert, especially in older patients.20 This is discussed in more detail in by Vardy et al.21
Improvements in care for hypercapnic respiratory failure
Another important change was to update guidance on the use of the chart for patients with hypercapnic respiratory failure to avoid NEWS driving a potentially harmful overuse of oxygen in these patients. Work in collaboration with the British Thoracic Society led to the NEWS2 chart having two scales for scoring oxygen saturations; Scale 1, the original NEWS scale, and a new Scale 2, reserved for patients with confirmed hypercapnic respiratory failure where the desired oxygen saturations are set at a lower level (88%–92% and the NEWS2 scoring scale was adjusted accordingly for these patients). This is discussed further by Juniper.22
NEWS2 and the suspicion of sepsis
A final important change resulted from a national focus on the better early detection and treatment of sepsis. A number of scoring systems to detect sepsis were being proposed, many requiring additional testing beyond routine vital signs. There was also a concern that too many acute disease-specific scoring systems would prevent their effective deployment. Thus, the focus turned to whether use of NEWS would be effective at raising suspicion of potential sepsis. This was logical as the clinical presentation of sepsis is highly variable but invariably associated with changes in baseline physiology that NEWS would be able to detect. In 2014, a study by Corfield et al had validated the approach of suspecting sepsis with a NEWS of ≥5 (Table 1), a score associated with a step-change in risk of ICU admission or mortality in patients with sepsis, confirmed in multiple subsequent studies.23,24 This positioned NEWS2 at the heart of national guidance for the early detection of sepsis whereby sepsis should be considered as a potential diagnosis in any acutely ill patient with a NEWS ≥5, and care escalated; with the campaign, ‘NEWS2 5 or more – think sepsis’.25
Table 1.
Data from 20 UK emergency departments showing the first National Early Warning Score in patients presenting to acute hospitals with sepsis and subsequent outcomes, n=2,00323
| Initial National Early Warning Score | Intensive care unit admission and/or mortality, % |
|---|---|
| <5 | 8 |
| 5–6 | 23 |
| 7–8 | 27 |
| 9–20 | 35 |
The launch and adoption of NEWS2 by NHS England
By 2017, there was widespread utilisation of NEWS by acute hospitals and ambulance services across the NHS, growing use in pre-hospital settings and increasing use across the world. There had been evidence of healthcare professional enthusiasm for NEWS since launch, as indicated by voluntary undertaking of non-mandatory training and accreditation in NEWS by over 150,000 NHS staff by 2017.26 The chair of the NEWS Development Group presented the success of the NEWS deployment to the NHS England (NHSE) leadership in 2017, emphasising the emerging evidence of the impact of the NEWS deployment in reducing cardiac arrest rates and in-hospital mortality from acute illness.27,28 This was in recognition that NHSE endorsement would drive full hospital implementation and extension to the pre-hospital community setting, enabling the NHS to become the first healthcare system in the world with a standardised national early warning system for acute clinical deterioration. The NHS formally adopted NEWS2 upon its release in December 2017.29 Adoption by the devolved nations of the UK soon followed. Since, NEWS has completed the full cycle of clinical translation from initial concept, development and early evaluation, through to clinical adoption and audit evaluation via its own Commissioning for Quality and Innovation (CQUIN). The NHSE CQUIN guidance 2021/2022 included indicator CCG3, auditing acute hospital performance in recording NEWS2, and response and escalation time for unplanned acute admissions to critical care.30
Additional NEWS2 guidance released in March 2020
In March 2020, additional implementation guidance was released by the RCP.31 This clarified what was meant by ‘new confusion’, provided new guidance on recommended assessment times of acutely ill patients, ie within 60 minutes for patients with a score of 5 or 6, and within 30 minutes for those with a score of 7 or more. The guidance also advised on how to handle incomplete or unrecordable physiological scores, and clarified the use of the two oxygen saturation scales in patients with chronic obstructive pulmonary disease (COPD); emphasising that not everybody with COPD has type 2 hypercapnic respiratory failure.
This update also coincided with the beginning of the COVID-19 pandemic in the UK. Patients with COVID-19 were unusual in their rapidly escalating requirement for oxygen, and there were concerns that this deterioration in respiratory function might not be adequately captured by the binary variable used by NEWS2 to capture oxygen use (ie yes/no). Despite this, studies subsequently confirmed that NEWS2 was effective at identifying/stratifying acutely ill patients with COVID-19 and their deterioration.32–36
Training the healthcare workforce in NEWS2
We recognised at the launch of NEWS and NEWS2 that easy to access, online educational resources were essential. An e-learning platform was developed pro bono by colleagues at OCB Media who have worked closely with the NEWS chair and development team throughout.26,37 The NEWS/NEWS2 e-learning module has had remarkable uptake, now approaching 350,000 completed modules, with 3,000 – 4,000 NHS staff currently completing training modules per month, and a completion rate around 86%. There is also an increase in staff completing the mental health (10%) and community (5%) variants of the training modules, equivalent to approximately 46,000 users in these areas, and growing. 55 NHS trusts have now migrated from the national NHS platform and are accessing NEWS2 modules directly through their local learning management systems or Electronic Staff Record / Oracle Learning Management as detailed Blackwell et al.26 Beyond the healthcare system, NEWS2 is now incorporated in medical and nursing school curricula. Furthermore, once NEWS2 was formally adopted by the NHS, NHS improvement also provided an excellent set of resources to support the use of NEWS2 by the workforce.25
The impact of NEWS/NEWS2
The uptake of NEWS2 has been extremely successful. Since its launch, NEWS and now NEWS2, has been consistently the highest-viewed page on the RCP website.
As discussed earlier, despite training on the e-learning platform not being mandatory in most hospitals (it is now becoming so, in some), almost 400,000 NHS staff have voluntarily undertaken the training since launch. These users are no longer just from acute hospital care but also from primary, community, ambulance and mental health services, showing that NEWS2 has permeated the whole system. Ninety-nine point five per cent of acute hospital trusts and 100% of ambulance services now use NEWS2 across the NHS, with increasing uptake in primary and community care settings.38
NEWS and NEWS2 have had a significant impact on patient care and safety, with reports from many regions of significant reductions (around 20%) in mortality from sepsis and acute illness after implementation of NEWS, and reports of around 50% reductions in cardiac arrest rates in hospitals after adoption. There have also been reports of reduced hospitals lengths of stay.24
Impact on system transformation
An important driver of the aforementioned impact has come from the role of NEWS2 in driving transformation. It has raised the profile of acute illness assessment and the importance of monitoring to detect clinical deterioration and sepsis. It has set clearer expectations around response times and staff competency levels, in some cases prompting hospitals to reorganise their 24/7 care. It has improved the awareness and recording of vital signs, and has driven more expedient triage and decision-making, prompting completion of treatment escalation plans in those with elevated scores. It has also improved the recording of oxygen saturations and appropriate prescribing of oxygen. NEWS has supported the prioritisation of resources, with a more objective assessment of clinical workload in different areas, facilitating better deployment of staff to clinical areas with the highest proportion of deteriorating patients. Finally, the success of NEWS has inspired other fields to standardise their approaches to acute care and it has been gratifying to witness and support the development of the NHS paediatric and maternity early warning scores (PEWS and MEWS, respectively), modelled on but necessarily physiologically distinct from NEWS.
Looking forward to the next 10 years
A lot has been achieved in the past 10 years towards our primary aim of improving patient safety and outcomes. Improvements in healthcare is an iterative process and developing NEWS has been a constant process of evolution and that will continue. The inevitable inclination of individuals or organisations to independently iterate with their own versions of NEWS has been a constant challenge and resisted, to preserve the overwhelmingly important concept of system-wide standardisation for patient safety. Nevertheless, we are on the cusp of major changes in the way we collect and use healthcare data, as in many other facets of life. Many healthcare systems are migrating to electronic health records, which provides its own unique challenges in how to standardise the way information is presented, as bedside vital signs charts will eventually disappear. How to resist alert fatigue from such systems and target alerts appropriately is already a challenge.39 Digitisation also presents opportunities to provide higher fidelity assessment of all available data across the time course of an acute illness, tracking trends and using continuous rather than binary variables to quantify change in a patient's condition and automatically aggregate additional data as it is acquired, adjusting the score for the patient's individual trends and comorbidities, providing a richer and more real-time score, using advanced computing and machine learning techniques. Furthermore, the collection of vital signs will eventually become automated and more routinely continuous, providing even richer data. Of course, the envisioning a future digital, AI-enabled EWS is easier than it will be to deliver it, with the need to ensure interoperability across multiple different electronic health record systems, integration of monitoring systems, alerting the responders and better understanding the anthropology of the human–computer interface, ensuring it is human-gated; aiding decisions, not making them. The key, as with the development of NEWS, will be to ensure that the development is clinically led. After that, everything is possible, and much of it will happen, after all, I was told many times that a system-wide deployment of a single EWS system could never happen in the NHS.
Conclusion
The NHS is the first healthcare system in the world to have a system-wide common language for acute clinical illness severity and clinical deterioration. NEWS was designed as a common language of acute illness severity. It is a language that all of us in clinical practice now understand, having entered the medical lexicon, although I am not sure about references to patients ‘NEWSing’ that are now frequently overheard on the wards. It has been an extraordinary journey, highly informative, at times challenging, but a largely positive experience in leading it. It has been humbling to witness its adoption by the NHS and the hugely significant impact on patient care and safety, an achievement of which I, the rest of the NEWS development group and the RCP are extremely proud.
In this issue, marking the 10-year anniversary of NEWS, we collate contributions from diverse groups who have taken on various roles in supporting the development, implementation or assessment of NEWS and NEWS2, providing personal perspectives or covering many key aspects in greater depth than has been possible here. I thank the colleagues who have contributed articles to this special edition of the journal, and the many who have supported the development and deployment of the NEWS/NEWS2 over the past 10 years.
Acknowledgements
There are so many people who provided guidance and support to me in leading the development and subsequent NHS adoption of NEWS/NEWS2. They are too numerous to list but they know who they are and we all owe them a huge debt of gratitude. I must, however, acknowledge Prof Derek Bell who worked closely with me from the start and was an endless source of wisdom and encouragement.
References
- 1.Royal College of Physicians . National Early Warning Score (NEWS): standardising the assessment of acute-illness severity in the NHS. RCP, 2012. [Google Scholar]
- 2.Royal College of Physicians . Acute medical care: the right person, in the right setting – first time. RCP, 2007. [Google Scholar]
- 3.National Institute for Health and Care Excellence . Acutely ill adults in hospital: recognising and responding to deterioration: Clinical guideline [CG50]. NICE, 2007. www.nice.org.uk/guidance/cg50 [Accessed 9 August 2017]. [Google Scholar]
- 4.National Confidential Enquiry into Patient Outcome and Death . Emergency admissions: A journey in the right direction? NCEPOD, 2007. www.ncepod.org.uk/2007ea.html [Accessed 9 August 2017]. [Google Scholar]
- 5.Patterson C, Maclean F, Bell C, et al. Early warning systems in the UK: variation in content and implementation strategy has implications for a NHS early warning system. Clin Med 2011;11:424–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Royal College of Physicians . National Early Warning Score 2 (NEWS2): standardising the assessment of acute-illness severity in the NHS. RCP, 2017. www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 [Google Scholar]
- 7.Jarvis S, Kovacs C, Briggs J, et al. Aggregate National Early Warning Score (NEWS) values are more important than high scores for a single vital signs parameter for discriminating the risk of adverse outcomes. Resuscitation 2015;87:75–80. [DOI] [PubMed] [Google Scholar]
- 8.Spångfors M, Bunkenborg G, Molt M, Samuelson K. The National Early Warning Score predicts mortality in hospital ward patients with deviating vital signs: a retrospective medical record review study. J Clin Nurs 2019;28:1216–22. [DOI] [PubMed] [Google Scholar]
- 9.Keep JW, Messmer AS, Sladden R, et al. National early warning score at Emergency Department triage may allow earlier identification of patients with severe sepsis and septic shock: a retrospective observational study. Emerg Med J 2016;33:37–41. [DOI] [PubMed] [Google Scholar]
- 10.Silcock DJ, Corfield AR, Gowens PA, Rooney KD. Validation of the National Early Warning Score in the prehospital setting. Resuscitation 2015;89;31–5. [DOI] [PubMed] [Google Scholar]
- 11.Shaw J, Fothergill RT, Clark S, Moore F. Can the prehospital National Early Warning Score identify patients most at risk from subsequent deterioration? Emerg Med J 2017;34:533–7. [DOI] [PubMed] [Google Scholar]
- 12.Bilben B, Grandal L, Søvik S. National Early Warning Score (NEWS) as an emergency department predictor of disease severity and 90-day survival in the acutely dyspneic patient – a prospective observational study. Scand J Trauma Resusc Emerg Med 2016;24:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farenden S, Gamble D, Welch J. Impact of implementation of the National Early Warning Score on patients and staff. Br J Hosp Med 2017;78:132–6. [DOI] [PubMed] [Google Scholar]
- 14.Hodgson LE, Dimitrov BD, Congleton J, et al. A validation of the National Early Warning Score to predict outcome in patients with COPD exacerbation. Thorax 2017;72:23–30. [DOI] [PubMed] [Google Scholar]
- 15.Kovacs C, Jarvis SW, Prytherch DR, et al. Comparison of the National Early Warning Score in non-elective medical and surgical patients. Br J Surg 2016;103:1385–93. [DOI] [PubMed] [Google Scholar]
- 16.Abbott TE, Torrance HD, Cron N, Vaid N, Emmanuel J. A single-centre cohort study of National Early Warning Score (NEWS) and near patient testing in acute medical admissions. Eur J Intern Med 2016;35:78–82. [DOI] [PubMed] [Google Scholar]
- 17.Roland D, Stilwell PA, Fortune PM, Alexander J, Clark SJ, Kenny S. Case for change: a standardised inpatient paediatric early warning system in England. Arch Dis Child 2021;106:648–51. [DOI] [PubMed] [Google Scholar]
- 18.Patient Safety Learning . NHS England - Maternity early warning score podcasts (14 July 2022). Patient Safety Learning, 2022. www.pslhub.org/learn/patient-safety-in-health-and-care/high-risk-areas/maternity/nhs-england-maternity-early-warning-score-podcasts-14-july-2022-r7213 [Google Scholar]
- 19.Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013;84:465–70. [DOI] [PubMed] [Google Scholar]
- 20.Williams B. The National Early Warning Score and the acutely confused patient. Clin Med 2019;19:190–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vardy E. National Early Warning Score (NEWS) 2 and the older person. Clin Med 2022;22:522–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juniper M. NEWS2, patient safety and hypercapnic respiratory failure. Clin Med 2022;22:518–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corfield AR, Lees F, Zealley I, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emerg Med J 2014;31:482–7. [DOI] [PubMed] [Google Scholar]
- 24.Inada-Kim M. NEWS2 and improving outcomes from sepsis. Clin Med 2022;22:514–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NHS England . National Early Warning Score (NEWS). NHS. www.england.nhs.uk/ourwork/clinical-policy/sepsis/nationalearlywarningscore [Google Scholar]
- 26.Blackwell N. The development and introduction of a national e-learning programme to support the dissemination of NEWS2. Clin Med 2022;22:530–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute for Health and Care Research . Are track and trigger systems linked to rates of in-hospital cardiac arrest? Health And Social Care Services Research; 2019. https://evidence.nihr.ac.uk/alert/are-track-and-trigger-systems-linked-to-rates-of-in-hospital-cardiac-arrest [Google Scholar]
- 28.Haegdorens F, Van Bogaert P, Monsieurs K. 1301: The National Early Warning Score improves patient monitoring practice and reduces mortality. Critical Care Medicine 2019;47:627. https://journals.lww.com/ccmjournal/Citation/2019/01001/1301__THE_NATIONAL_EARLY_WARNING_SCORE_IMPROVES.1256.aspx [DOI] [PubMed] [Google Scholar]
- 29.Royal College of Physicians . NHS England approves use of National Early Warning Score (NEWS) 2 to improve detection of acutely ill patients. RCP. www.rcplondon.ac.uk/news/nhs-england-approves-use-national-early-warning-score-news-2-improve-detection-acutely-ill [Google Scholar]
- 30.NHS England . Commissioning for Quality and Innovation (CQUIN): Guidance for 2020 –2021. NHS, 2020. www.england.nhs.uk/wp-content/uploads/2020/01/FINAL-CQUIN-20-21-Core-Guidance-190220.pdf [Google Scholar]
- 31.Royal College of Physicians . National Early Warning Score 2 (NEWS2): standardising the assessment of acute-illness severity in the NHS: Additional implementation guidance. RCP, 2020. www.rcplondon.ac.uk/projects/outputs/news2-additional-implementation-guidance [Google Scholar]
- 32.Baker KF, Hanrath AT, Schim van der Loeff I, et al. National Early Warning Score 2 (NEWS2) to identify inpatient COVID-19 deterioration: a retrospective analysis. Clin Med 2021;21:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scott LJ, Tavaré A, Hill EM, et al. Prognostic value of National Early Warning Scores (NEWS2) and component physiology in hospitalised patients with COVID-19: a multicentre study. Emergency Medicine Journal 2022;39:589–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carr E, Bendayan R, Bean D, et al. Evaluation and improvement of the National Early Warning Score (NEWS2) for COVID-19: a multi-hospital study. BMC Med 2021;19:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kostakis I, Smith GB, Prytherch D, Meredith P, Price C, Chauhan A; Portsmouth Academic ConsortIum For Investigating COVID-19 (PACIFIC-19) . The performance of the National Early Warning Score and National Early Warning Score 2 in hospitalised patients infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Resuscitation 2021;159:150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams B. Evaluation of the utility of NEWS2 during the COVID-19 pandemic. Clin Med 2022;22:539–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.OCB Media . NEWS2: Standardising the assessment of acute-illness severity in the NHS: elearning programme. OCB Media. https://news.ocbmedia.com [Google Scholar]
- 38.Tavare A, Gibson A, Barker R. NEWS2 in out-of-hospital settings: the ambulance and the emergency department. Clin Med 2022;22:525–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Subbe CP, Bramley R. Digital NEWS? How to amplify the benefits of NEWS in a digital health care system. Clin Med 2022;22:534–8. [DOI] [PMC free article] [PubMed] [Google Scholar]