ABSTRACT
Physician associates (PAs) are currently unable to prescribe in the UK due to the absence of statutory regulation and prescribing legislation. This is likely to change with the introduction of regulation by the General Medical Council (GMC) set to start from 2023. Currently, there are working groups looking into what needs to be done to enable them to prescribe.
In this paper, we explored the views of PAs that qualified in the UK on prescribing and ordering investigations via an online questionnaire. Almost all PAs would prefer to be able to prescribe and request radiological investigations. Inability to perform these basic duties has a negative impact on patient care, patient flow, PAs' contribution to healthcare and career progression.
KEYWORDS: prescribing, NHS, physician associate, GMC regulation
Introduction
Physician associates (PAs) are a continuously growing profession in the UK. PAs are generalist healthcare professionals who've trained within the medical model to provide patient care under supervision.1 The profession originally emerged in the USA in the 1960s, and was introduced to the NHS in 2003 to help with workforce shortages.1 This was followed by establishment of training programmes for PAs and, currently, 35 universities offer PA studies in the UK.2 As of October 2020, there were 1,788 PAs registered with the Faculty of PAs at the Royal College of Physicians.3 This number has grown further and will continue to increase in the future because of their invaluable support to the NHS.
Even though PAs are able to carry out a range of tasks from history taking, examination, diagnosis and making management plans, they are currently unable to prescribe medications or order investigations containing ionising radiation due to a lack of regulation.4,5 In 2019, the General Medical Council (GMC) was selected as the regulatory body for the PAs and this may open several doors for the PAs, one in particular is the legal right to prescribe.6,7 In the USA, PAs were first given prescribing authority in 10 states in 1980 and, by 2007, PAs had prescribing rights in all 50 states.8 With GMC regulations set to start from 2023, we wanted to explore the views of PAs working in the UK on prescribing and ordering radiological investigations.
Methods
We devised an online questionnaire (Google Forms) that could be easily answered either via a mobile phone or a computer. The questionnaire was anonymous and did not seek any identifiable personal data. It had nine questions: three required specific answers as a free text (when did they qualify, do they work in primary or secondary care, and what is their current specialty), four had yes/no answers, one had a yes/no/not sure answer and one had a multiple-choice answer, there was also a free-text box for additional comments (the questionnaire is available in supplementary material S1). The questionnaire was shared to qualified PAs working in the UK through the authors' professional contacts (via PAs' WhatsApp groups) and Twitter.
Results
We had 123 responses, of which, three (2.5%) were blank submissions. One was incomplete where the respondent had missed just one question, but we included this in the analysis. The results from yes/no and yes / no / not sure questions are given in Table 1. Thirty-nine used the additional comment section to express their views, from which we selected a few based on the theme of their messages including any contrasting comments (Box Box 1.).
Table 1.
Answers to questions from the physician associate survey on prescribing rights
| Yes | No | Not sure | |
|---|---|---|---|
| Q4. Would you like to be an independent prescriber? n=120, n (%) | 117 (97.5) | 1 (0.8) | 2 (1.7) |
| Q6. Do you think that your inability to prescribe has had a negative impact on your work, colleagues and/or patients? n=120, n (%) | 104 (86.7) | 16 (13.3) | N/A |
| Q7. Do you think that you would be able to work more productively and efficiently if you could prescribe? n=120, n (%) | 119 (99.2) | 1 (0.8) | N/A |
| Q8. Do you think that your inability to prescribe is limiting your career progression? n=120, n (%) | 108 (90.0) | 12 (10.0) | N/A |
| Q9. Would you like to be able to request radiological investigations, eg CT, MRI and X-rays? n=119, n (%) | 117 (98.3) | 2 (1.7) | N/A |
CT = computed tomography; MRI = magnetic resonance imaging.
Box 1.
Selected illustrative free-text comments from the questionnaire
Views on prescribing
|
Views on requesting radiological investigations:
|
CT = computed tomography; GP = general practitioner; NICE = National Institute for Health and Care Excellence; PA = physician associate.
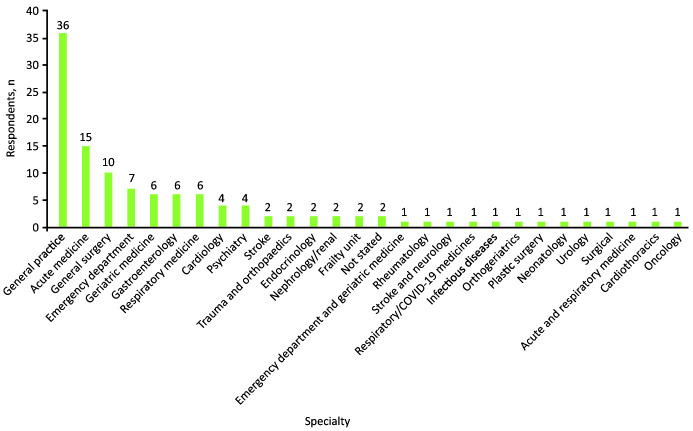
Most of the PAs who had responded (77.8%) had qualified in the previous 3 years (between 2019 and 2021), with the earliest in 2013. Sixty-six per cent were working in secondary care, 34% in primary care, and one was between secondary care and a university. The most common specialties where they worked included acute medicine, general practice, surgery and the emergency department (Fig 1).
Fig 1.
Specialty/department in which physician associate respondents work.
Almost all PAs (98%) would like to be independent prescribers and also be able to request radiological investigations. Eighty-seven per cent felt that their inability to prescribe has had a negative impact on their work, colleagues and patients, and 90% believed that their inability to prescribe was limiting their career progression. Almost everyone (99%) felt that they would be more efficient and contribute more to patient care if they could prescribe.
There was a mixed response regarding their competencies gained during their course to become independent prescribers (Fig 2). More than a third (37%) stated that even though they had adequate training, they would still prefer to have additional experience before becoming independent prescribers. Another 38% felt that they did not receive adequate training and would prefer further training, and only about a quarter (23%) felt that they had adequate training to prescribe independently. The majority (75%) of those who felt that they had received adequate training had qualified more recently (between 2019 and 2021) and almost all of them were based in secondary care.
Fig 2.
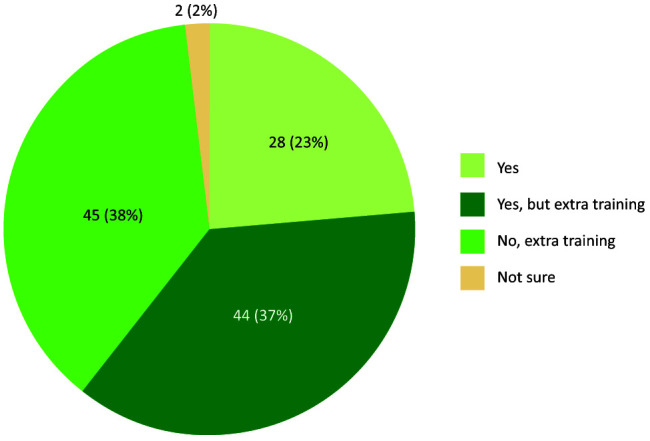
The views of physician associate respondents on whether they received adequate training from their degree to become independent prescribers.
The themes from the free text (Box 1) showed that a majority could contribute more towards patient care and be more efficient if they were able to prescribe and order investigations, and that a lack of prescribing is an hinderance on patient care and prohibits their development and career opportunities.
Discussion
Our results confirm that PAs would like to be independent prescribers and should be able to request radiological investigations after appropriate training. This is probably due to a number of factors including enhanced clinical training, willingness to contribute more effectively and a desire to work with increased autonomy. Currently, despite having the ability to take detailed histories, perform examinations competently, and come up with a diagnosis and a management plan, particularly for conditions within their competency, they would still need to rely on someone who could prescribe.4
In some general practices, a PA can message a general practitioner (GP) for a prescription, and they, in turn, can issue an electronic prescription for the patient, thus maintaining workflow. However, it is more difficult in secondary care because a prescriber may not always be immediately available and, disappointingly, in many hospitals, PAs are not even allowed to transcribe medications. A vast majority (87%) said that their inability to prescribe had not only a negative impact on their work but also affected their career progression; their frustration is evident in the free-text comments (Box 1). One PA even mentioned about changing specialty because of their inability to prescribe in primary care, while others found that the lack of prescribing is deterring some employers from recruiting them.
These issues were recognised nearly a decade ago in a study from 2014 involving 62 doctors, where they indicated that PAs' inability to prescribe (82%) and inability to request radiography (50%) limited the effectiveness of a PA.4 A survey involving 119 clinical and non-clinical healthcare professionals found overwhelmingly positive feedback on the role of PAs.9 But, it also identified a few negative comments by junior doctors that the PAs were taking away their learning opportunities and also increase their workload because the junior doctors had to re-review the patients before then prescribing.9
There were mixed responses on whether PAs had received adequate training during their course to become an independent prescriber (Fig 2). Many felt that their course had not prepared them for prescribing but the experience that they've had since qualifying has provided them with more confidence to prescribe. This is similar to studies involving junior doctors that found that many do not feel prepared to prescribe following qualification despite years of in-depth training but their confidence had grown with first-hand experience.10
When PAs are embedded in a team, they bring additional assets and share their clinical and institutional knowledge with newer members of the multidisciplinary team.11 It has been recently shown that PAs in the UK are a stable workforce, many are being established in the same position when they feel well supported by their supervisors.12 It is a well-recognised fact that opportunities for professional growth is critically associated with job satisfaction and retention, so it is time to act without any further delay to empower the PAs to extend their duties and responsibilities.13
So, what needs to be done for PAs to be able to prescribe? Our results showed that only a quarter felt that they had adequate training to prescribe independently. Most of this group had qualified in the previous few years, which suggests that the training for PAs regarding applied pharmacology has improved recently. A few suggestions made by PAs include some more years of experience after qualification and also to complete the prescribing safety assessment as part of their national qualifying exams.
A recent paper gives clear guidance and suggestions for preparing PAs to prescribe.5 They draw comparison from the USA where PAs are given prescribing rights upon passing their national certifying examination. Similarly, PAs in the UK should be given prescribing rights after passing the PA National Certifying Exam (PANE). Other options would include allowing the PAs to take the V300 prescribing course that is currently available to all non-physician healthcare professionals.14 This would allow the already qualified PAs to gain prescribing rights. These recommendations could be extrapolated to ordering radiological investigations after completing the Ionising Radiation (Medical Exposure) Regulations 2017 training and any necessary additional local training relevant to their practice.
Additionally, if PAs are to have prescribing rights upon qualification, several course providers may need to update their pharmacy modules.5,15 With this in mind, St George's, University of London recently took the initiative to improve their curriculum in pharmacology for PA students by introducing a drug formulary and encouraging self-directed learning. This not only improved the student feedback on engagement and quality but also found that PA students could be ready to prescribe when they finish their qualification.15
Limitations of our survey include a possible bias where the PAs who had responded may be keener than others towards prescribing and a selection bias by using the social networks that don't include all PAs working in the UK. Despite this, we feel that the answers from our survey is a fair representation of the views of the PAs in general as our results are consistent with previous studies that had a similar theme.
Conclusion
PAs have a keen interest in becoming independent prescribers as indicated by the survey. This will allow them to work autonomously and efficiently, increase their contribution, and improve the quality of care for patients. Also, it would consolidate their role in healthcare, increase their job satisfaction, cause less frustration in their roles and improve retention.
There are several established courses that could be integrated into the PA programme to develop them as competent prescribers. It has already been proven in the USA that PAs have the capability to prescribe safely.5,15 We strongly believe that it is absolutely essential for PAs to prescribe independently and have the ability to order appropriate investigations within their professional framework after achieving the necessary competencies.
There is, sadly, now going to be a further delay to the legislation that will make PAs a regulated profession. The legislation is now set to be completed by summer 2023, which was previously when regulation was estimated to begin.16
Supplementary material
Additional supplementary material may be found in the online version of this article at www.rcpjournals.org/fhj:
S1 – Physician associates' views on prescribing survey questions.
References
- 1.Farmer J, Currie M, Hyman J, West C, Arnott N. Evaluation of physician assistants in National Health Service Scotland. Scottish Medical Journal 2011;56:130–4. [DOI] [PubMed] [Google Scholar]
- 2.NHS England . Interim NHS people plan. NHS, 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf [Accessed 08 May 2022]. [Google Scholar]
- 3.Royal College of Physicians . Focus on physician associates: census 2020. RCP, 2021. www.fparcp.co.uk/about-fpa/fpa-census [Accessed 02 April 2022]. [Google Scholar]
- 4.Williams LE, Ritsema TS. Satisfaction of doctors with the role of physician associates. Clin Med 2014;2:113–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guest BN, Chandrakanthan C, Bascombe K, Watkins J. Preparing physician associates to prescribe: evidence, educational framework and pathways. FHJ 2022;9:21–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown ME, Laughey W, Tiffin PA, Finn GM. Forging a new identity: a qualitative study exploring the experiences of UK-based physician associate students. BMJ Open 2020;10:e033450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.General Medical Council . Bringing physician associates and anaesthesia associates into regulation. GMC, 2022. www.gmc-uk.org/pa-and-aa-regulation-hub/map-regulation [Accessed 07 April 2022]. [Google Scholar]
- 8.American Academy of Physician Associates . Milestones in PA history. AAPA, 2017. www.aapa.org/wp-content/uploads/2017/01/History_Milestones.pdf [Accessed 07 May 2022]. [Google Scholar]
- 9.Theodoraki M, Hany TS, Singh H, Khatri M. Multisource feedback for the physician associate role. The Bulletin of the Royal College of Surgeons of England 2021;103:206–10. [Google Scholar]
- 10.Newby DA, Stokes B, Smith AJ. A pilot study of a pharmacist-led prescribing program for final-year medical students. BMC Med Educ 2019;19:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chenevert L, Bascombe K. Cornerstones to progressing the physician associate profession: post-qualification training and development. FHJ 2022;9:3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts K, Drennan VM, Watkins J. Physician associate graduates in England: a cross-sectional survey of work careers. FHJ 2022;9:5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arkwright L, Edgar S, Debenham J. Exploring the job satisfaction and career progression of musculoskeletal physiotherapists working in private practice in Western Australia. Musculoskeletal Science and Practice 2018;35:67–72. [DOI] [PubMed]
- 14.Cope LC, Abuzour AS, Tully MP. Nonmedical prescribing: where are we now? Ther Adv Drug Saf 2016;7:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guest BN, Chandrakanthan C, Bascombe K, Watkins J. Pharmacology for physician associate programmes: a collaborative, flexible and responsive approach to curriculum design. FHJ 2021;8:e580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Royal College of Physicians . Update on progress towards regulation. RCP. https://fparcp.co.uk/about-fpa/news/update-on-progress-towards-regulation [Accessed 16 May 2022]. [Google Scholar]