Abstract
Introduction:
Adverse childhood experiences (ACEs) and overdose are linked in a cycle that affects individuals and communities across generations. The Centers for Disease Control and Prevention’s (CDC) Overdose Data to Action (OD2A) cooperative agreement supports a comprehensive public health approach to overdose prevention and response activities across the United States. Exposure to traumatic events during childhood can increase the risk for a myriad of health outcomes, including overdose; therefore, many OD2A recipients leveraged funds to address ACEs.
Methods:
In 2021, an inventory of OD2A-funded activities implemented in 2019 and 2020 showed that 34 of the 66 recipients proposed overdose prevention activities that support people who have experienced ACEs or that focus on preventing the intergenerational transmission of ACEs. Activities were coded by ACE prevention strategy, level of the social ecology, and whether they focused on neonatal abstinence syndrome (NAS).
Results:
Most activities amongst OD2A recipients occurred at the community level of the social ecological model (SEM) and under the “intervene to lessen harms” ACE prevention strategy. Of the 84 ACE-related activities taking place across 34 jurisdictions, 44 are focused on NAS.
Conclusion:
Study results highlight the opportunities to expand the breadth of ACEs prevention strategies across the social ecology. Implementing cross-cutting overdose and ACEs-related activities that span the SEM are critical for population-level change and have the potential for broadest impact. Focusing on NAS also offers a unique intervention opportunity for both ACEs and overdose prevention.
INTRODUCTION
Drug overdose deaths continue to increase in the United States and predictions estimate their contributing to 92,183 deaths in 2020.1–3 Researchers and public health practitioners use the social ecological model (SEM) as one of the key frameworks for prevention and leverage it to understand how risk and protective factors contribute to childhood adversity.4 It describes the interplay between individual, relationship, community, and societal factors that put people at risk for or protect them from experiencing violence.4, 5 Risk and protective factors for overdose are found at multiple levels of the SEM and include physical and mental health, social connections, access to healthcare, and treatment for substance use disorder.6 An important correlate of experiencing overdose is adverse childhood experiences (ACEs). ACEs are preventable, potentially traumatic events that occur in childhood (0–17 years) including physical or emotional neglect or abuse, sexual abuse, experiencing or witnessing violence, growing up in a household with substance use or with household members in jail or prison, or having a family member attempt or die by suicide.7, 8 ACE exposure also increases the likelihood of substance use during adolescence and adulthood, including prescription opioid misuse,9, 10 marijuana and cocaine use,11 substance use disorder (SUD)12, 13 as well as overdose among adults with opioid use disorder (OUD).14 Exposure to a caregiver’s substance use is an ACE that may, in combination with socioeconomic, environment and genetic influences, continue the cycle of substance use15, 16 and related negative social and health outcomes, particularly in the absence of positive childhood experiences and in combination with other ACEs. ACEs and overdose are linked in a cycle that affects individuals and generations nested within communities and society. Additionally, the conditions in which people live, work, learn, and play– also known as social determinants of health – can contribute to health inequities and confer intergenerational risk for substance use and overdose. Specifically, exposure to parental substance use or losing a parent to overdose are ACEs that could contribute to increased risk of substance use and overdose in adulthood and impact a person’s ability to live a healthy life.
Another significant impact of SUDs is the increasing prevalence of neonatal abstinence syndrome (NAS). NAS is used to describe the signs and symptoms in infants who were exposed to substances, such as opioids, in utero.17 Increasing rates of NAS were attributed to opioid use during pregnancy between 2009 and 2014.18 Increased focus on NAS within prevention programming provides opportunities for women to learn about treatment options and for linkage to care, preventing future ACEs for multiple generations.19 The available evidence for prenatal exposure and substance use later in life is limited and does not reflect a cause-and-effect relationship.20, 21
CDC’s ACEs prevention resource, Preventing Adverse Childhood Experiences (ACEs): Leveraging the Best Available Evidence,10 identifies the best available evidence for programs, policies, and practices found in CDC’s technical packages that describe violence prevention strategies that work across the lifespan and have the greatest potential for impact.7, 22–26
Overdose Data to Action Cooperative Agreement
Recognizing the link between ACE-related trauma and substance use has led to development and implementation of programs spanning the social ecology. These programs work simultaneously to prevent ACEs, substance use, and overdose more broadly. CDC’s Overdose Data to Action (OD2A) cooperative agreement (CDC-RFA-CE19-1904) focuses on implementing an interdisciplinary and comprehensive public health approach using data to inform overdose prevention activities. There are two components of this four-year, $1.2 billion cooperative agreement: surveillance and prevention. This federally funded initiative began in 2019 and funds 66 jurisdictions, including 47 states, three territories, and 16 city or county health departments. OD2A encourages jurisdictions to focus activities on people who are at increased risk for overdose and SUD, including those who have experienced ACEs.12, 13 Each jurisdiction determines the combination of mandatory and optional activities that are funded through this cooperative agreement and ACEs-related activities are not mandatory. Jurisdictions with higher overdose burden may opt to implement interventions that directly reduce fatal and nonfatal overdoses as opposed to implementing more upstream prevention approaches. Given the potential for simultaneous prevention and intervention for both outcomes,12, 13 34 of the 66 OD2A funding recipients proposed activities that address the intersectionality of ACEs and substance use disorder.
Activities proposed and implemented by OD2A recipients were categorized using the ACEs prevention strategies and SEM level. Figure 1 depicts the OD2A logic model and strategies that can impact ACEs through intergenerational primary prevention or mitigation of trauma. The activities described fall under Strategy 3 which focuses on innovative surveillance, or the prevention component strategies (Strategies 5–10). This assessment uncovered gaps and opportunities for implementing ACEs-related overdose prevention activities across the SEM, and documents areas with potential for widespread implementation or evaluation.
Figure 1.
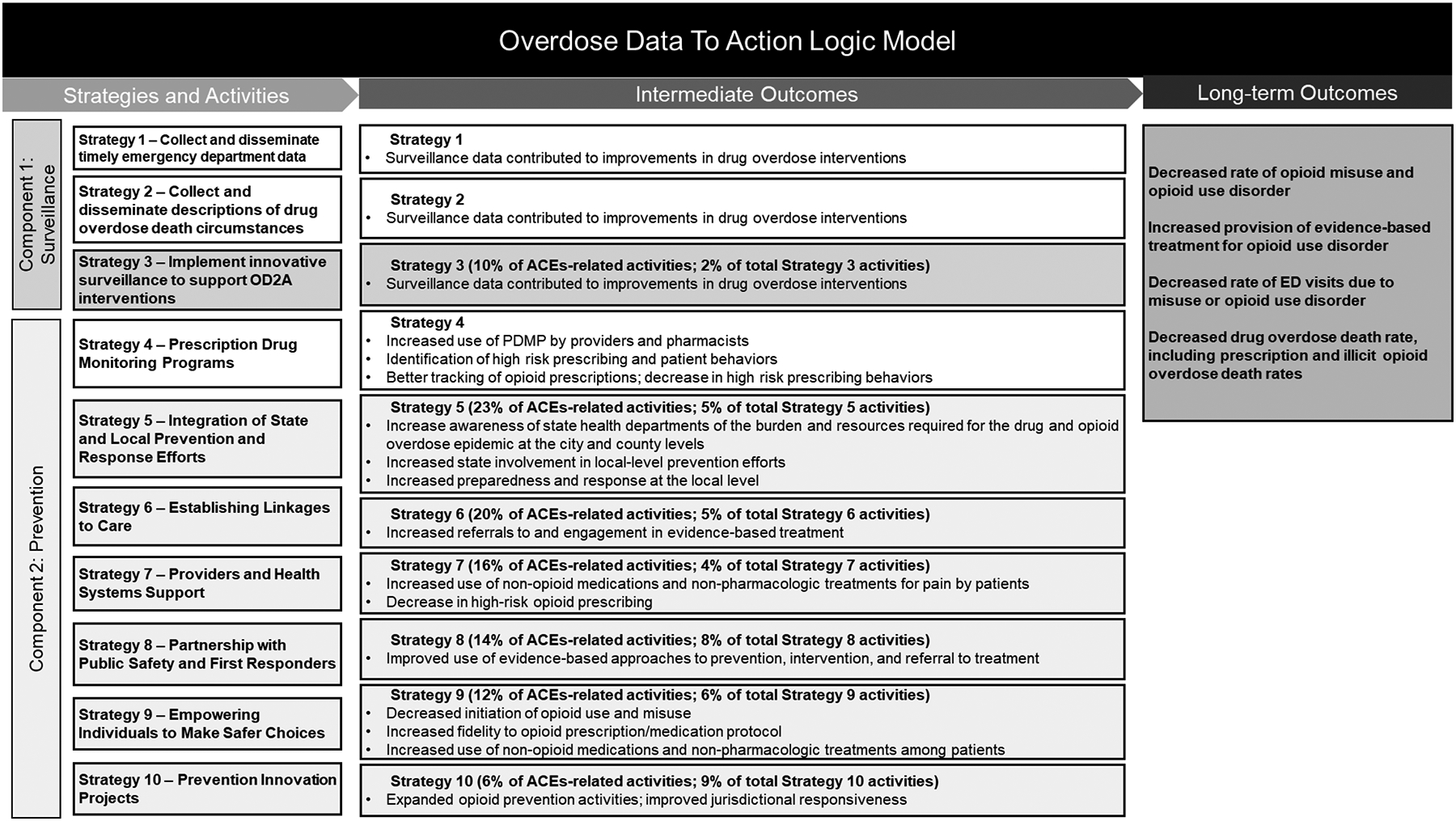
OD2A Logic Model with opportunities for ACEs work highlighted.a
a The Overdose Data to Action (OD2A) Notice of Funding Opportunity (NOFO) required applicants to consider of the populations at highest risk for overdose, including those with adverse childhood experiences. Strategies could target pregnant women, parents, and persons with Adverse Childhood Experiences (ACEs) in addition to other vulnerable populations. No ACEs-related activities were found in strategies 1, 2 or 4.
METHODS
ACEs Activity Inventory
All analyses took place in 2021. First, an activity inventory which describes ACE-related activities implemented by OD2A recipients in 2019 and 2020 was developed. The goals were to understand how OD2A jurisdictions are implementing both ACEs and SUD prevention, the level of the SEM in which the activities are implemented, and the gaps and opportunities for enhancing SUD prevention through an ACE lens. The jurisdictions provided information about strategies, activities, populations of focus, implementing sectors, and progress to date. A scan of the deliverables showed key search terms related to ACEs. Deliverables were reviewed using key search terms, and activity descriptions were extracted from program applications, year 1 performance reports, and year 2 workplans.
Coding and Analysis
Following data extractions, activities were coded by social ecology level4 by considering the targets of activities and whether the intervention was designed to stimulate change at the individual, relationship, community or societal level, ACEs prevention strategy described in the ACEs resource document, and by whether the activity focused on NAS.5, 7 For an activity to be coded as NAS-related, it had to mention NAS, substance-exposed newborns, Plans of Safe Care, which as of 2016, are required for states to receive Child Abuse Prevention and Treatment Act funds and are designed to ensure the safety and well-being of an infant with prenatal substance exposure,27 or pregnant women with SUD. A strategy was coded at the individual level if the activity intended to directly benefit only the population of focus. The relationship level corresponded to activities designed to improve individuals’ interactions with others, while community level impacted multiple entities and partnerships. Finally, activities intended to support guidelines or policies were considered societal.
The strategies described in the ACEs resource document are 1) strengthen economic supports to families; 2) promote social norms that protect against violence and adversity; 3) ensure a strong start for children; 4) teach prosocial skills; 5) connect youth to caring adults and activities; and 6) intervene to lessen immediate and long-term harms.
Thirty-nine of the jurisdictions included ACEs-related activities in their deliverables and 123 total were identified. Activities were removed from the inventory if they were discontinued (17), not directly related to ACEs (9), or did not fall under an ACEs prevention strategy (13). Each activity was coded by two members of the team and discrepancies were resolved through group consensus to identify one level of the SEM and one ACE prevention strategy.
RESULTS
Analysis showed that 34 of the 66 OD2A-funded jurisdictions are implementing at least one, and up to eight, ACE-related activities, amounting to 84 activities. Figure 2 shows the ACEs-related activities in OD2A jurisdictions. Forty-four of these activities have a NAS focus and are implemented in 18 jurisdictions. As seen in Figure 3, most activities were coded as the “intervene to lessen harms” (n=45) and “promoting social norms” (n=29) ACE-prevention strategies, and most addressed the community (n=68) level of the SEM.
Figure 2.

Map of Overdose Data to Action jurisdictions with Adverse Childhood Experiences (ACEs)-related activities by activity density
Figure 3.
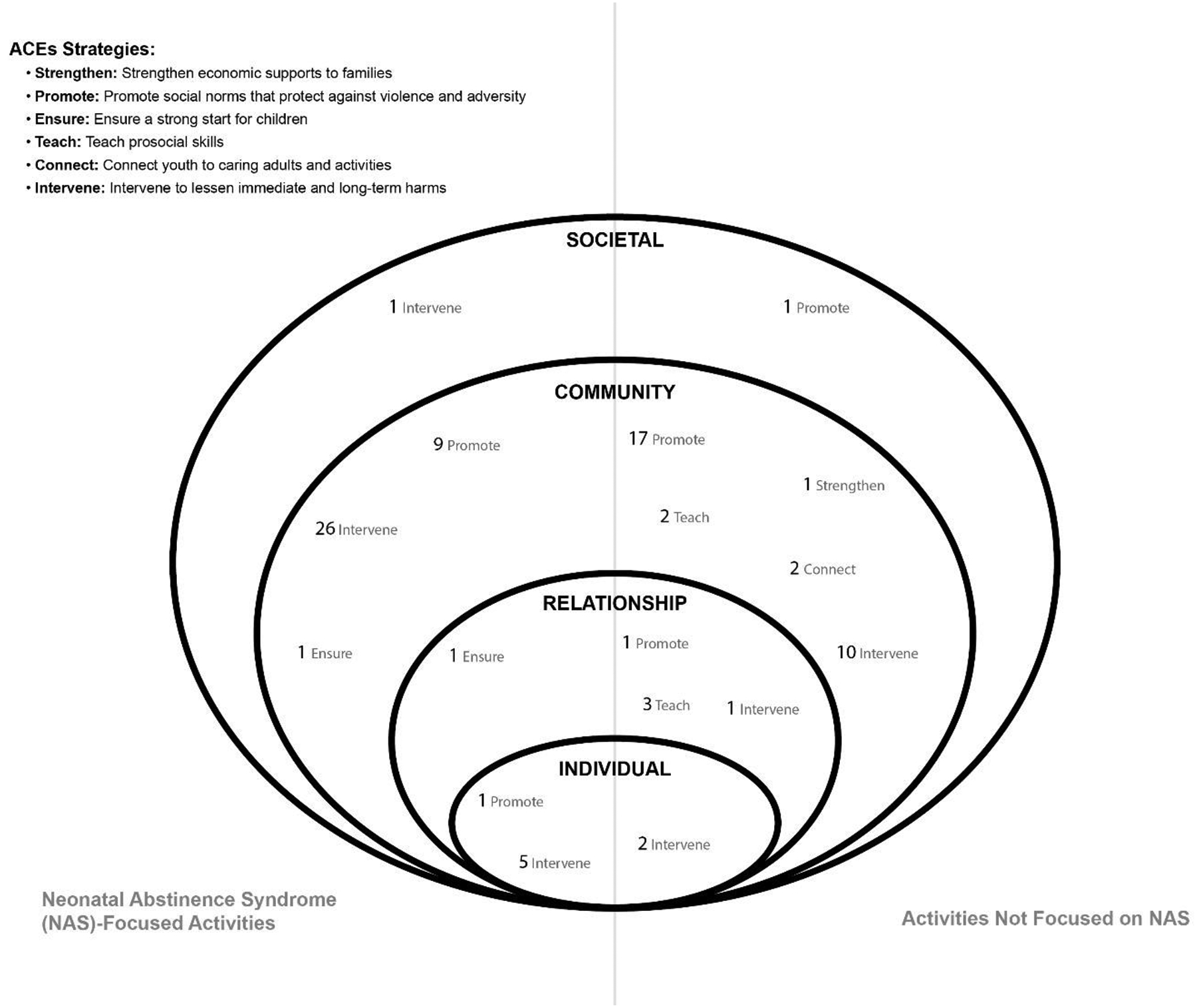
Distribution of Overdose Data to Action Adverse Childhood Experiences (ACEs)-related activities across the Social Ecological Model by ACE strategy
Characteristics of ACE-related activities implemented by jurisdictions
Table 1 describes the activities that were coded in each state. OD2A-funded jurisdictions are working across the lifespan and multiple sectors of service delivery for people with and at risk for SUD to implement programs across the SEM.
Most activities that do not address NAS fall under the ACE-prevention strategy “promoting social norms” and address the community level of the SEM, educating organizations across several sectors about the prevalence and impact of ACEs. Several of these activities involved training first responders (14) and school system staff (3) to implement trauma informed approaches and resiliency building.
Eight activities that focus on ACEs are under OD2A surveillance component’s Strategy 3 and most (7) involve using surveillance data to inform activities including linking pregnant and parenting women to services. These activities were coded under the “intervene to lessen harms” ACEs strategy and the relationship level of the SEM. Strategy 5 of the OD2A cooperative agreement focuses on integrating state and local overdose prevention and response efforts. Twenty of the ACEs-related activities fall under OD2A’s Strategy 5, accounting for 23 percent of the activities (see Figure 1). These activities were coded as the ACEs strategies “intervene to lessen harms,” “teach skills,” and “promote social norms.” They occur at the individual, relationship, and community levels of the SEM. Examples of Strategy 5 activities include providing trainings for caregivers of children whose parents are impacted by SUD and educating justice-system staff about trauma-informed interventions.
Eighteen activities fell under OD2A’s Strategy 6, which focuses on linking people to care. Most focus on ensuring that persons more susceptible to overdose are connected to appropriate services through creation, expansion, dissemination, and support of the infrastructure to increase linkages. Most Strategy 6 activities were coded as ACEs strategy “intervene to lessen harms” and all except one were coded as community level. The one exception was coded at the individual level and involved connecting mothers of infants born with NAS to treatment.
OD2A Strategy 7 activities focus on building the ACEs-related knowledge and capacity to respond to traumatic events across health systems. Several jurisdictions focus on implementing Plans of Safe Care, for infants with NAS and their families. Other jurisdictions are supporting the implementation of Screening, Brief Intervention and Referral to Services and developing guidelines for NAS screenings. All Strategy 7 activities were coded as the ACE strategies “intervene to lessen harms” or “promote social norms”. All except one Strategy 7 activity fell under the community level of the SEM; the one exception was coded as individual level and involved training school nurses in trauma-informed approaches.
OD2A Strategy 8 focuses on partnerships with public safety and other first responders. Jurisdictions identified opportunities to collaborate with the justice system on overdose, and all activities were coded as community level of the SEM. These activities were coded as either “promote social norms” or “intervene to lessen harms” and had two major foci: educating first responders about the potential harms and effects of trauma, including its relationship to substance use, and implementation of a trauma-informed approach. Handle with Care is a novel intervention, first implemented in West Virginia, designed to alert school personnel about a student’s interaction with police, either directly or in their home, so that school staff can support the student and understand possible causes of behaviors.
OD2A’s Strategy 9 activities focus on harm reduction services and communication campaigns. These activities were coded as “promote social norms,” “teach skills,” “ensure a strong start,” and “connect youth to caring adults.” These were coded into the relationship, community, and societal levels of the SEM. Examples of activities include training harm reduction and home visiting program staff about the impacts and frequency of trauma. Additional activities focus on connecting youth to caring adults through schools and community organizations.
OD2A’s Strategy 10 supports innovative activities that prevent overdose. The ACEs-related activities were coded as “promote social norms,” “ensure a strong start,” “intervene to lessen harms,” and “strengthen economic supports.” The activities were coded as community or relationship levels of the SEM. Activities include evaluating resources for pregnant and parenting women, implementing a home visiting program designed for families caring for substance-exposed infants, establishing a state-wide, trauma-informed workforce, and identifying barriers to enrolling in food and childcare assistance programs.
DISCUSSION
This paper is the first to document a federal initiative to fund activities that impact ACEs and substance use through strategies that address both. The connection between substance use in the home and the deleterious social and health risks to youth exposed to it is well established in the literature.28 There were more than 840,560 drug overdose deaths between 1999 and 20193 resulting in an estimated $1.02 trillion in societal costs associated with opioid use disorder and fatal opioid overdose in 2017 alone.29 The vast morbidity and mortality associated with the U.S. opioid crisis led to increased Congressional investment in opioid overdose prevention activities, allowing CDC to launch its Prevention for States initiative in 2015.30 More recently, OD2A was designed to continue to strengthen surveillance infrastructure for overdose morbidity and mortality and ensure that data were used to drive overdose prevention activities.
The findings show that the most common ACEs prevention strategies being implemented by OD2A recipients promote social norms and are primarily implemented at the community level. While prevention strategies that address community-level risk factors for ACEs31 and overdose32 have potential for effect, an ideal model would consist of programs or other interventions at each level of the SEM with integration of multiple ACE prevention strategies to ensure the largest, collective impact. This could include a combination of capacity and awareness building amongst the work force and general population implemented simultaneously with programs targeting community change and social norms while building or improving relationships through skill and resiliency building and addressing individuals’ needs. Eighteen OD2A recipients are implementing NAS-related activities. These strategies are designed to intervene among infants at high risk of ACEs as well as parenting women. Although the most common activities were similarly implemented at the community level, activities described here represent opportunities for intervention across multiple levels of the SEM. At the individual level, interventions include education, linkage to care, and obstetric care sessions for women and at the relational level, enhanced home visitation for families. Community-level interventions include implementing family screening and linkages to care and providing trainings for staff related to NAS and care for pregnant women with SUD. Finally, the development of state-level guidance for NAS screening represents a societal-level intervention. Maternal and infant outcomes can be improved through screening, intervention, and referral for treatment of pregnant women with opioid use and use disorder,19 and OD2A recipients are implementing activities that support these approaches and may also prevent future ACEs. Additionally, several other federally funded initiatives exist, including surge support to improve public health outreach to mothers and their infants, which serves pregnant and parenting women and babies born with NAS.33, 34
Many evidence-based programs are focused on either ACEs or SUD but have potential to address both. For example, peer recovery supporters are crucial to the success of those in recovery remaining in recovery;35, 36 this mirrors the ACE prevention strategy that focuses on connecting with positive role models (i.e., “connect youth to caring adults”). The roles of peer recovery supporters and caring adults are similar, and communities could use these supports simultaneously as child abuse and neglect and SUD prevention continue to overlap.
Limitations
Data shared here represent only activities funded through OD2A and described in the deliverables received from funded jurisdictions. The currently available deliverables do not include evaluation data. Other programs may be actively addressing overdose, substance use and ACEs at levels of the SEM and under ACEs strategies not included in OD2A-funded activities.
CONCLUSIONS
This analysis also revealed an opportunity to connect more caregivers experiencing SUD with parenting programs or other supportive interventions. Home visiting programs (HVPs) and parenting programs have shown benefits for families at risk for substance use/SUD and for babies born with NAS through enhanced parental skills training, facilitating the parent-child attachment, and identifying SUD-related problems before adverse outcomes can occur for the mothers or children.37, 38 As seen in Figure 3, no jurisdictions are implementing parenting programs that teach skills specific to parents of infants with NAS, revealing an opportunity to support the caregivers by teaching skills tailored for the children as they grow and develop. High-quality HVPs have shown returns on investments up to $5.70 for every dollar spent39 and focusing on families impacted by SUD with these interventions could show effects across the lifespan.
Finally, six OD2A jurisdictions are implementing school-based substance use prevention programming which may be considered primary prevention of ACEs because preventing substance use initiation in youth could theoretically prevent one form of ACEs—exposure to parental substance use—downstream. Resilience building and evidence-based programs improve protective factors amongst children from 4 years old through middle and high school while simultaneously increasing the knowledge and support of their parents and caregivers.40, 41 OD2A funds jurisdictions with high burdens of overdose morbidity and mortality, therefore upstream prevention programming may break the intergenerational cycle of substance use among many program participants.
This paper demonstrates that jurisdictions are implementing ACEs-related overdose prevention strategies at multiple levels of social ecology, which is critical for population-level change. The ACEs-related overdose prevention activities documented herein may help expand the reach and impact of overdose prevention activities by offering a holistic approach to prevention—integrating and addressing the multi-generational aspect of substance use and ACEs. Still, room exists to improve strategies that address both outcomes. Leveraging data collected through CDC’s Behavioral Risk Factor Surveillance System’s ACE module, the Youth Risk Behavior Surveillance System, and other federally and locally funded tools42 to further understand the burden of ACEs as a risk factor for SUD is one of the next steps. Data driven prevention and intervention across the SEM will enhance the collective impact in communities and synergized implementation is essential. Incorporating resilience building and positive childhood experiences across the levels of the social ecology and into many overdose prevention strategies is important to improve health outcomes in adulthood.43–46
We know from other reports that substance use and fatal and nonfatal overdoses and child abuse and neglect have increased during the COVID-19 pandemic; COVID-19 mitigation efforts also impacted support services to prevent and reduce these outcomes.47, 48 This underscores the importance of the work being done regarding these issues.
Supplementary Material
Footnotes
Conflict of Interest Statement: The authors whose names are listed above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Financial Disclosure: The authors whose names are listed above have no relevant financial interests in this article.
April Wisdom: conceptualization, methodology, writing, original draft, review and editing, visualization, formal analysis Madhumita Govindu: methodology, writing-original draft, formal analysis Stephen Liu: visualization Christina Meyers: formal analysis Jenelle Mellerson: formal analysis Derrick Gervin: formal analysis, Lara DePadilla: formal analysis, writing-review and editing Kristin Holland: formal analysis, writing-original draft, methodology
Publisher's Disclaimer: CDC Disclaimer: The findings and conclusions in this presentation are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Wilson N, Kariisa M, Seth P, Smith IV H, Davis NL. Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmad F, Rossen L, Sutton P. Data from: Provisional drug overdose death counts. 2021. National Center for Health Statistics. [Google Scholar]
- 3.Hedegaard H, Miniño A, Warner M. Drug Overdose Deaths in the United States, 1999–2019; NCHS Data Brief No. 394. https://www.cdc.gov/nchs/data/databriefs/db394-tables-508.pdf#1 [PubMed]
- 4.Division of Violence Prevention [DVP], National Center for Injury Control and Prevention [NCIPC], Centers for Disease Control and Prevention [CDC]. The Social-Ecological Model: A Framework for Violence Prevention. https://www.cdc.gov/violenceprevention/pdf/sem_framewrk-a.pdf
- 5.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. Oct 5 2002;360(9339):1083–8. doi: 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- 6.Jalali MS, Botticelli M, Hwang RC, Koh HK, McHugh RK. The opioid crisis: a contextual, social-ecological framework. Health Res Policy Syst. 2020;18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence (National Center for Injury Prevention and Control, Centers for Disease Control and Prevention) https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf (2019).
- 8.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 9.Swedo EA, Sumner SA, de Fijter S, et al. Adolescent Opioid Misuse Attributable to Adverse Childhood Experiences. J Pediatr. 2020;224:102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrick MT, Ford DC, Haegerich TM, Simon T. Adverse childhood experiences increase risk for prescription opioid misuse. J Prim Prev. 2020:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheidell JD, Quinn K, McGorray SP, et al. Childhood traumatic experiences and the association with marijuana and cocaine use in adolescence through adulthood. Addiction. 2018;113(1):44–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LeTendre ML, Reed MB. The Effect of Adverse Childhood Experience on Clinical Diagnosis of a Substance Use Disorder: Results of a Nationally Representative Study. Subst Use Misuse. 2017/05/12 2017;52(6):689–697. doi: 10.1080/10826084.2016.1253746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moss HB, Ge S, Trager E, et al. Risk for Substance Use Disorders in young adulthood: Associations with developmental experiences of homelessness, foster care, and adverse childhood experiences. Compr Psychiatry. 2020/07/01/ 2020;100:152175. doi: 10.1016/j.comppsych.2020.152175 [DOI] [PubMed] [Google Scholar]
- 14.Stein MD, Conti MT, Kenney S, et al. Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug Alcohol Depend. 2017;179:325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerr DCR, Tiberio SS, Capaldi DM, Owen LD. Paternal and maternal prescription opioid use and misuse: General and specific risks for early adolescents’ substance use. Addict Behav. Apr 2020;103:106248. doi: 10.1016/j.addbeh.2019.106248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jaaskelainen M, Holmila M, Notkola IL, Raitasalo K. Mental disorders and harmful substance use in children of substance abusing parents: A longitudinal register-based study on a complete birth cohort born in 1991. Drug Alcohol Rev. Nov 2016;35(6):728–740. doi: 10.1111/dar.12417 [DOI] [PubMed] [Google Scholar]
- 17.McQueen K, Murphy-Oikonen J. Neonatal Abstinence Syndrome. 2016;375(25):2468–2479. doi: 10.1056/NEJMra1600879 [DOI] [PubMed] [Google Scholar]
- 18.Atwell KA, Weiss HB, Gibson C, Miller R, Corden TE. Neonatal Abstinence Syndrome and Maternal Substance Use in Wisconsin, 2009–2014. WMJ. Dec 2016;115(6):287–94. [PubMed] [Google Scholar]
- 19.Mascola MA, Borders AE, Terplan M. Committee Opinion No. 711: Opioid Use and Opioid Use Disorder in Pregnancy. Obstet Gynecol. Aug 2017;130(2):e81–e94. doi: 10.1097/AOG.0000000000002235 [DOI] [PubMed] [Google Scholar]
- 20.Anbalagan S, Mendez M. Neonatal Abstinence Syndrome. StatPearls. 2021. [PubMed] [Google Scholar]
- 21.Maguire DJ, Taylor S, Armstrong K, et al. Long-Term Outcomes of Infants with Neonatal Abstinence Syndrome. Neonatal Netw. 2016;35(5):277–86. doi: 10.1891/0730-0832.35.5.277 [DOI] [PubMed] [Google Scholar]
- 22.Basile K, DeGue S, Jones K, et al. STOP SV: A technical package to prevent sexual violence. 2016.
- 23.David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, Marshall KJ, Rainford N & Hall JE A comprehensive technical package for the prevention of youth violence and associated risk behaviors.. 2016.
- 24.Fortson BL, Klevens J, Merrick MT, Gilbert LK, & Alexander SP Preventing child abuse and neglect: a technical package for policy, norm, and programmatic activities. 2016. [Google Scholar]
- 25.Niolon PH, Kearns M, Dills J, Rambo K, Irving S, Armstead T, & Gilbert L. Preventing intimate partner violence across the lifespan: a technical package of programs, policies, and practices.. 2017. [Google Scholar]
- 26.Stone DM, Holland KM, Bartholow B, Crosby AE, Davis S, & Wilkins N. Preventing suicide: a technical package of policies, programs, and practices. 2017. [Google Scholar]
- 27.Gateway CWI. Plans of safe care for infants with prenatal substance exposure and their families. 2020. https://www.childwelfare.gov/topics/systemwide/laws-policies/statutes/safecare/
- 28.Lander L, Howsare J, Byrne M. The Impact of Substance Use Disorders on Families and Children: From Theory to Practice. Soc Work Public Health. 2013;28(0):194–205. doi: 10.1080/19371918.2013.759005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Florence C, Luo F, Rice K. The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. Jan 1 2021;218:108350. doi: 10.1016/j.drugalcdep.2020.108350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robinson A, Christensen A, Bacon S. From the CDC: The Prevention for States program: Preventing opioid overdose through evidence-based intervention and innovation. J Safety Res. Feb 2019;68:231–237. doi: 10.1016/j.jsr.2018.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis JP, Ports KA, Basile KC, Espelage DL, David-Ferdon CF. Understanding the Buffering Effects of Protective Factors on the Relationship between Adverse Childhood Experiences and Teen Dating Violence Perpetration. J Youth Adolesc. Dec 2019;48(12):2343–2359. doi: 10.1007/s10964-019-01028-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thompson J, Creasy S, Mair C, Burke J. Drivers of opioid use in Appalachian Pennsylvania: Cross-cutting social and community-level factors. Int J Drug Policy. 2020;78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Center on Birth Defects and Developmental Disabilities [NCBDDD]. Prenatal Opioid and Substance Exposure. Accessed March 13th 2021, https://www.cdc.gov/ncbddd/aboutus/pregnancy/nas.html
- 34.Jilani SM, Frey MT, Pepin D, et al. Evaluation of State-Mandated Reporting of Neonatal Abstinence Syndrome - Six States, 2013–2017. MMWR Morb Mortal Wkly Rep. Jan 11 2019;68(1):6–10. doi: 10.15585/mmwr.mm6801a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kowalski MA. Mental Health Recovery: The Effectiveness of Peer Services in the Community. Community Ment Health J. Apr 2020;56(3):568–580. doi: 10.1007/s10597-019-00514-5 [DOI] [PubMed] [Google Scholar]
- 36.Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-Delivered Recovery Support Services for Addictions in the United States: A Systematic Review. J Subst Abuse Treat. Apr 2016;63:1–9. doi: 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 37.Dauber S, Ferayorni F, Henderson C, Hogue A, Nugent J, Alcantara J. Substance Use and Depression in Home Visiting Clients: Home Visitor Perspectives on Addressing Clients’ Needs. J Community Psychol. Apr 2017;45(3):396–412. doi: 10.1002/jcop.21855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumpfer KL, Fowler MA. Parenting skills and family support programs for drug-abusing mothers. Semin Fetal Neonatal Med. Apr 2007;12(2):134–42. doi: 10.1016/j.siny.2007.01.003 [DOI] [PubMed] [Google Scholar]
- 39.Harrison CL AM Home Visiting: Improving Children’s and Families’ Well-Being. 2018. [PubMed]
- 40.Spoth R, Trudeau L, Shin C, et al. Longitudinal effects of universal preventive intervention on prescription drug misuse: three randomized controlled trials with late adolescents and young adults. Am J Public Health. Apr 2013;103(4):665–72. doi: 10.2105/AJPH.2012.301209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spoth R, Trudeau L, Redmond C, Shin C. Replication RCT of early universal prevention effects on young adult substance misuse. J Consult Clin Psychol. Dec 2014;82(6):949–63. doi: 10.1037/a0036840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anderson KN, Swedo EA, Clayton HB, Holditch-Niolon P, Shelby D, Harrison KM. Building Adverse Childhood Experiences Surveillance Infrastructure: Integrated, Multi-Method Approaches to Generate Data for Prevention Action Am J Prev Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonanno GA, Diminich ED. Annual Research Review: Positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry. Apr 2013;54(4):378–401. doi: 10.1111/jcpp.12021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gartland D, Riggs E, Muyeen S, et al. What factors are associated with resilient outcomes in children exposed to social adversity? A systematic review. BMJ Open. Apr 11 2019;9(4):e024870. doi: 10.1136/bmjopen-2018-024870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leung DYL, Chan ACY, Ho GWK. Resilience of Emerging Adults After Adverse Childhood Experiences: A Qualitative Systematic Review. Trauma Violence Abuse. Jun 26 2020:1524838020933865. doi: 10.1177/1524838020933865 [DOI] [PubMed] [Google Scholar]
- 46.Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive Childhood Experiences and Adult Mental and Relational Health in a Statewide Sample: Associations Across Adverse Childhood Experiences Levels. JAMA Pediatr. Nov 1 2019;173(11):e193007. doi: 10.1001/jamapediatrics.2019.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Swedo E, Idaikkadar N, Leemis R, et al. Trends in U.S. Emergency Department Visits Related to Suspected or Confirmed Child Abuse and Neglect Among Children and Adolescents Aged <18 Years Before and During the COVID-19 Pandemic - United States, January 2019-September 2020. MMWR Morb Mortal Wkly Rep. Dec 11 2020;69(49):1841–1847. doi: 10.15585/mmwr.mm6949a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Czeisler ME, Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. Aug 14 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


